Abstract
Purpose
COVID‐19 and other recent infectious disease outbreaks have highlighted the urgency of robust, resilient health systems. We may now have the opportunity to reform the flawed health care system that made COVID‐19 far more damaging in the United States (U.S.) than necessary.
Design and Methods
Guided by the World Health Organization (WHO) Health System Building Blocks framework (WHO, 2007) and the socio‐ecological model (e.g., McLeroy et al., 1988), we identified challenges in and strengths of the U.S.’ handling of the pandemic, lessons learned, and policy implications for more resilient future health care delivery in the U.S. Using the aforementioned frameworks, we identified crucial, intertwined domains that have influenced and been influenced by health care delivery in the U.S. during the COVID‐19 pandemic through a review and analysis of the COVID‐19 literature and the collective expertise of a panel of research and clinical experts. An iterative process using a modified Delphi technique was used to reach consensus.
Findings
Four critically important, inter‐related domains needing improvement individually, interpersonally, within communities, and for critical public policy reform were identified: Social determinants of health, mental health, communication, and the nursing workforce.
Conclusions
The four domains identified in this analysis demonstrate the challenges generated or intensified by the COVID‐19 pandemic, their dynamic interconnectedness, and the critical importance of health equity to resilient health systems, an effective pandemic response, and better health for all.
Clinical relevance
The novel coronavirus is unlikely to be the last pandemic in the U.S. and globally. To control COVID‐19 and prevent unnecessary suffering and social and economic damage from future pandemics, the U.S. will need to improve its capacity to protect the public's health. Complex problems require multi‐level solutions across critical domains. The COVID‐19 pandemic has underscored four interrelated domains that reveal and compound deep underlying problems in the socioeconomic structure and health care system of the U.S. In so doing, however, the pandemic illuminates the way toward reforms that could improve our ability not only to cope with likely future epidemics but also to better serve the health care needs of the entire population. This article highlights the pressing need for multi‐level individual, interpersonal, community, and public policy reforms to improve clinical care and public health outcomes in the current COVID‐19 pandemic and future pandemics, and offers recommendations to achieve these aims.
INTRODUCTION
The outbreak of the novel coronavirus SARS‐CoV‐2 was declared a Public Health Emergency of International Concern by the World Health Organization (WHO) on January 30, 2020, and a pandemic on March 11, 2020 (World Health Organization, 2020a). Now, nearly three years into the pandemic, COVID‐19, an acute illness in humans caused by SARS‐CoV‐2, has presented the world with many well‐documented challenges including death, disability, and socioeconomic damage. In May 2022, the WHO reported the grim statistic that an estimated 15 million persons worldwide have died of COVID‐19, with one million of these deaths occurring in the U.S. (World Health Organization, 2022).
Throughout the world, health systems were unprepared for the pandemic despite the warnings of public health experts. Health crises, such as the Ebola epidemic and now the Covid‐19 pandemic, acutely illustrate the need for resilient systems that can prepare for and effectively respond to crises while maintaining core functions and reorganizing if needed (Haldane et al., 2021). A robust, resilient health system provides the right services, both personal and population‐based, in the right places, at the right times, to all who need those services. Although the U.S. spends far more on health care than any other country in the world, the COVID‐19 pandemic severely strained hospitals and health systems across the nation and undermined the health of the U.S. population (Crowley et al., 2020; Haldane et al., 2021).
While the U.S. is not the only country to endure painful challenges and losses from COVID‐19, the pandemic highlighted the deep socioeconomic inequities, communication and workforce challenges, and weaknesses in U.S. healthcare delivery systems present before the start of the pandemic. It also brought into focus the important and unique role of nurses. Nurses, the largest group of health professionals in the U.S., have been a critical component of health care delivery in the U.S. throughout the pandemic (ANA, 2022). Yet, because of their frontline roles and mission, they have also acutely experienced and borne witness to the ravages of COVID‐19.
Although the COVID‐19 pandemic has reified and compounded deep underlying problems in health care in the U.S., it also offers an opportunity to reflect and consider how to facilitate improvements. Guided by the World Health Organization (WHO) Health System Building Blocks framework (WHO, 2007) and the socio‐ecological model (Centers for Disease Control and Prevention, n.d.; Kilanowski, 2017; McLeroy et al., 1988; Sallis et al., 2008; Wold & Samdal, 2012), we use an expanded model to consider challenges and strengths in addressing the pandemic, lessons learned, and policy implications for more resilient health care delivery in the U.S. in the future.
GUIDING MODEL AND METHODS
Socio‐ecological model, health system framework, COVID‐19 and nursing
Health systems that can deliver services equitably and efficiently are critical for achieving improved population health. In an effort to support health system strengthening, the WHO formulated a health system framework that identified six foundational building blocks of a strong, functional health care system: (1) service delivery, (2) health workforce, (3) information, (4) medical products, vaccines, and technologies, (5) financing, and (6) leadership/governance (WHO, 2007). In considering health system strengthening within the context of COVID‐19, the WHO health systems framework can be viewed from a broad socio‐ecological context as delineated in a socio‐ecological model (Centers for Disease Control and Prevention, n.d.; Kilanowski, 2017; McLeroy et al., 1988; Sallis et al., 2008; Wold & Samdal, 2012). Within this framework, dynamic interrelations among various personal and environmental factors are represented with the recognition that no single factor can explain or predict a particular phenomenon (Baron et al., 2014). As such, lessons of the COVID‐19 pandemic can be viewed as the outcome of dynamic interactions between discrete but interrelated dimensions at the individual (patient, families, and nurses), interpersonal (relationship between patients, family, and healthcare providers, including nurses and their co‐workers), organizational (context of healthcare practice within the organization), community (nursing communities, professional and educational regulation, and standards), and public policy (socio‐political and economic) levels (Figure 1).
FIGURE 1.
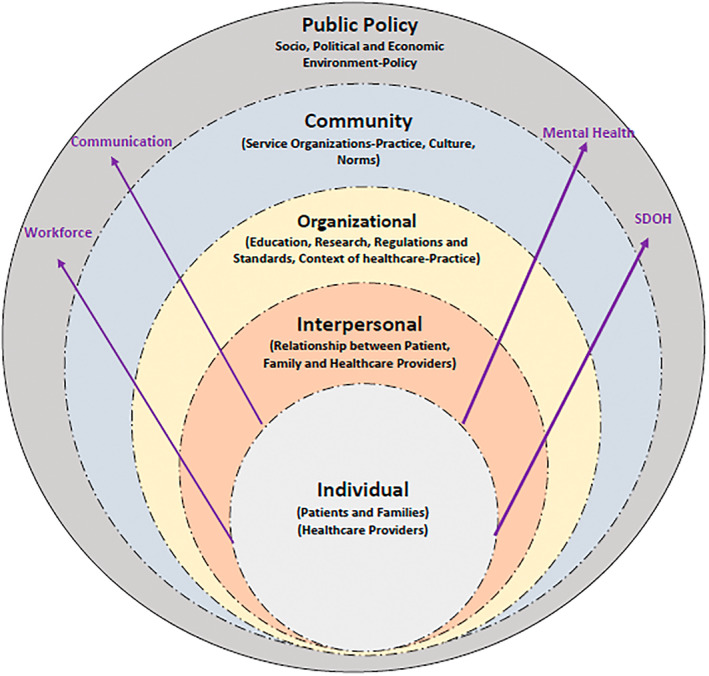
Socio‐ecological model, nursing and COVID‐19
METHODS
Grounded in the WHO health systems framework and the socio‐ecological model, we identified four crucial, intertwined domains that have influenced and been influenced by health care delivery in the U.S. during the COVID‐19 pandemic. A modified Delphi technique was used (Dalkey & Helmer, 1963). We convened a panel of experts with relevant research and clinical backgrounds to define and discuss the problem area, analyze the literature and bring together explicit and implicit knowledge with the goal of reaching a group consensus on the domains, lessons learned and policy implications.
The domains of interest were identified based on a review of relevant literature across nursing, public health and policy journals followed by extensive discussion and triangulation with the integrated frameworks. A facilitator led discussions with the panel. After each round, the facilitator summarized the range of the experts' judgments and rationale provided. At the start of the next round, the discussion from the previous round and the rationale for the experts' earlier judgments were reviewed. This information was then provided to the expert panelists, who could revise their previous responses based on the replies of other members of the panel. The process continued to reduce the range of responses with the aim that the group would ultimately converge toward a consensus. This process concluded when convergence of opinion on four domains and their interface with the integrated model was reached. The team recognizes that this is a non‐exhaustive list of potential topics, but concurred that these domains were the most salient in the literature and nursing clinical practice to date and offered opportunities to highlight intersecting concerns for policy change. The four domains are elaborated in the results section followed by a discussion of lessons learned and policy implications for each domain. While implications for practice, education, and research are also important, this project is focused on policy implications, though these have relevance to practice, education, and research.
RESULTS
We identified four crucial, intertwined domains that have influenced and been influenced by health care delivery in the U.S. during the COVID‐19 pandemic: (1) social determinants of health, (2) mental health, (3) communication, and, (4) the nurse workforce. These domains demonstrate the challenges generated or intensified by the COVID‐19 pandemic, their dynamic interconnectedness, and the critical importance of health equity to resilient health systems, an effective pandemic response and better health for all.
Social determinants of health and vulnerable populations
Social determinants of health (SDOH) are defined by the WHO as the non‐medical factors that influence health outcomes, the conditions in which people are born, live, work, and age, and the wider set of forces and systems shaping the conditions of daily life (WHO, n.d.). These conditions are typically grouped according to economic stability, education access and quality, healthcare access and quality, neighborhood and built environment, and social and community context (Healthy People, 2030). Social and other health determinants occur in feedback loops throughout the life course, intergenerationally, and at individual, population, and community levels (McGovern et al., 2014). Adding to this complexity is the importance of the intersections of environmental and socioeconomic determinants, which results in greater disadvantage. For example, lower socioeconomic urban neighborhoods (an economic determinant) have considerably higher pollution levels (an environmental determinant), which partially account for the higher rates of respiratory diseases such as asthma seen in children growing up in these settings (Kreger et al., 2011).
Over the past few decades, the study of these SDOH have revealed stark health‐related disparities by race and ethnicity, age, gender, and ability. Unfortunately, in the U.S., the COVID‐19 pandemic further exacerbated existing health disparities, which are rooted in the U.S.' history of colonialism, and continue to be reinforced by structural racism (Bailey et al., 2017). Most notably, in the first year of the pandemic (2020–2021), Indigenous peoples (American Indian/Alaskan Native), Hispanic, Americans, and Black Americans had 3.5, 2.4, and 2 times higher COVID‐related mortality rates than White Americans, respectively. Communities that were already experiencing the compounding effects of structural racism and historical trauma faced a higher burden of existing co‐morbidities, unsafe work conditions, unstable housing, poverty, unsafe neighborhoods, and substandard education were disproportionately affected by COVID‐19 (Moreno et al., 2020; Panchal et al., 2021).
Although mortality rates have now decreased for all racial and ethnic groups, inequities persist (Centers for Disease Control and Prevention, 2022a). Moreover, Indigenous, Black, and Hispanic Americans have also experienced a disproportionate risk of non‐COVID‐19‐related mortality during this time (e.g., heart disease, diabetes; Luck et al., 2022). Health infrastructure in Native American communities, provided through the Indian Health Service, is often under‐resourced and understaffed, Native Americans are more likely to be uninsured and the pandemic has disproportionally affected mental health in many Indigenous communities (Hatcher et al., 2020). Black and Hispanic adults in the U.S. were 3 and 2 times more likely to report increased household food insecurity and were more likely to report job loss and difficulty paying household bills compared to White adults. Recent rises in inflation have also disproportionately affected the finances of communities of color. These metrics were exacerbated by structural inequities related to the pandemic including decreased COVID‐19 testing sites in communities with more Black and Hispanic residents (Dalva‐Baird et al., 2021) and less access to life‐saving monoclonal antibody treatment for minoritized groups, those underinsured, or those with language barriers with active COVID‐19 infection (Wiltz et al., 2022; Wu et al., 2022). Additionally, patients in the U.S. are more likely to face higher out‐of‐pocket costs and to be uninsured than those in other comparable countries (Kearney et al., 2021). Among Indigenous communities, elevated incidence might also reflect differences in reliance on shared transportation, limited access to running water, household size, and other factors that might facilitate COVID‐19 community transmission (Hatcher et al., 2020).
The pandemic also compounded physiological and social vulnerabilities of those at high risk from the virus across the lifespan. For example, older adults faced disproportionate mortality during the pandemic, which was unequally distributed by race, ethnicity, and indices of social vulnerability (Garcia et al., 2021). Further, the required social isolation that aimed to protect older adults from infection was also linked to loneliness and depressive symptoms, especially in long‐term care facilities that shut the doors to family and required residents to quarantine in their rooms (Hwang et al., 2020). Older adults, who were more likely to experience co‐morbid conditions, delayed seeking health care services for non‐COVID‐related health problems or were unable to access these services because of overwhelmed providers and health systems (Lei & Maust, 2022).
While children experienced comparatively lower mortality compared to adults, COVID‐19 was a leading cause of death and severe outcomes for this population as well, with significant racial disparities (Shi et al., 2022). Pregnant and postpartum persons and their infants are another group whose physiological vulnerabilities to the virus were compounded by a fragmented policy environment that failed to adequately consider their unique needs, leading to barriers to care and labor support and mother‐infant separation, which has negative psychosocial impacts and disrupts lactation (Tomori et al., 2020, 2022). Pregnant and recently pregnant persons were also excluded from initial vaccination trials, causing a delay in information when vaccinations became available (Rawal et al., 2022), and leading to confusion, misinformation, and comparatively lower vaccination uptake. Coupled with insufficient investment in community‐based outreach, these delays also deepened racial, ethnic and socioeconomic vaccination inequities within this group (Tomori et al., 2022).
Inequities for incarcerated people, who are disproportionately racialized minorities, were exceptionally heightened during the pandemic (LeMasters et al., 2022). Inadequate mitigation measures and delayed vaccination rollout facilitated the rapid COVID‐19 spread through overcrowded prisons, leading to much higher incidence, morbidity and mortality than the general population (Altibi et al., 2021; American Association of Public Health, 2021; Marquez et al., 2021). The Coronavirus Aid Relief and Economic Security (CARES) Act, passed in 2020, allowed the Bureau of Prisons to release nonviolent, pretrial prisoners to expanded home confinement, which alleviated COVID‐related risks for some. However, rapid release without assurance of continuity of care placed released prisoners who struggled with opioid use disorder at risk of relapse (Bandara et al., 2022; Dadiomov et al., 2022).
Together, existing inequities in the U.S. were greatly exacerbated by the COVID pandemic and the inadequate policy response to it, resulting in a life expectancy decline of 2.7 years between 2019 and 2021—setting the U.S. apart from all other wealthy nations (Arias et al., 2022). These impacts disproportionately affected racial minorities, reflecting the ongoing effects of structural racism, with a 6.6 year decline for Indigenous Americans (American Indian/Alaskan Native), a 4.2 year decline for Hispanic Americans, and a 4 year decline in life expectancy for Black Americans (Arias et al., 2022).
Mental health
The pandemic created a mental health crisis in the U.S. due to numerous factors, such as the disruption of care for persons with mental health needs and substance use disorders (SUD) and the creation of conditions that exacerbated or catalyzed mental disorders. By February 2021, over 40% of adults reported anxiety or depressive symptoms and 25% reported that they were not receiving needed care (Vahratian et al., 2021). Deaths from drug overdose increased by 28.5% over the 12‐month period ending April 2021, primarily due to opioids (Centers for Disease Control and Prevention, 2021). While mental health symptoms were often brought on or worsened by the pandemic environment, an actual diagnosis of COVID‐19 and difficulty coping with symptoms of the virus were also associated with depression, anxiety, and traumatic stress (Houben‐Wilke et al., 2022). In particular, adverse psychological symptoms of traumatic stress, depression, and anxiety may persist for months (Houben‐Wilke et al., 2022) and cognitive symptoms (e.g., brain fog) may persist for two years or more (Taquet et al., 2021). As approximately 30% of adults hospitalized with COVID‐19 complained of symptoms lasting at least 6 months (Centers for Disease Control and Prevention, 2022b), the increased need for COVID‐related mental health services may persist long term (Havervall et al., 2021; Panchal et al., 2021; Schou et al., 2021).
The pandemic adversely impacted the mental health of all age groups in the U.S. Children and youth who were most at‐risk were those with the greatest exposure to pandemic‐related stressors, including a COVID‐related death in the family (Fegert et al., 2020), lack of reprieve from abuse or relationship conflicts in the home (Magson et al., 2021), financial strain (Adegboye et al., 2021), prolonged isolation from peers (Loades et al., 2020), challenges with remote learning (Magson et al., 2021), and pandemic‐related racial discrimination (Cheah et al., 2020). A recent nationally representative sample of U.S.‐based adolescent students found that 37.1% experienced poor mental health during the pandemic, 19.9% had seriously considered suicide, and 9% had attempted suicide (Jones et al., 2022).
As discussed above, social distancing protocols of older adults were linked to loneliness and depressive symptoms, particularly for residents of long‐term care facilities that restricted family access and required residents to quarantine in their rooms (Hwang et al., 2020). Eighty percent of deaths from COVID‐19 occurred in adults aged 65 and above (Lekamwasam & Lekamwasam, 2020).
Essential workers (healthcare providers, grocery store, package delivery workers) risked exposure and had higher rates of psychiatric symptoms. Frontline healthcare workers were exposed to unprecedented stress, burnout, and moral injury due to the suffering and death of patients and colleagues; emotionally difficult situations with patients and patients' family members; conflicting loyalties to self and family, and employers and patients; ethical dilemmas regarding rationing of supplies and resources; and personal risk for COVID‐19 infection (Giorgi et al., 2020; Panchal et al., 2021). Approximately 22% of healthcare workers experienced at least moderate depression, anxiety, or PTSD symptoms during the pandemic (Li et al., 2021). Nurses were at higher risk of infection and death than any other healthcare profession, and over 20% reported wanting to leave the profession (The National Institute for Occupational Safety and Health, 2021a, 2021b). Research suggests this was more prevalent among minority frontline healthcare workers due to the apparent increased health risks associated with COVID‐19 (Van Beusekom, 2020). Even when psychiatric symptoms were identified, support and mental healthcare were frequently inaccessible (Pollock et al., 2020).
The increased need for mental health and substance use disorder services in the U.S. was accompanied by multiple barriers to access, including the overwhelming need for emergency departments to provide beds to patients with life‐threatening symptoms, temporary cessation of mobile crisis units that could be deployed to homes or streets for evaluation and treatment, decreased clinical hours, and reduced access to long‐acting injectables and medication for opioid use disorders (Khatri & Perrone, 2020; Moreno et al., 2020; Panchal et al., 2021). Underscoring the social and environmental inequities in the U.S., racial and ethnic minorities experienced greater stress, worry, mental disorders, and substance use conditions (McKnight‐Eily et al., 2021). Communities with unstable housing, low income, unsafe neighborhoods, and substandard education were disproportionately affected by COVID‐19 as were incarcerated persons as noted above (Golembeski et al., 2020).
Barriers to access were exacerbated by challenges in preparation of providers. The shift to online education was rapid and many nursing educational systems and educators were untrained in online best practices. Healthcare systems turned their focus to acute patient care and psychiatric clinical placements for mental healthcare students were extremely hard to find. Telepsychiatry clinical placements were offered to some healthcare students; however, many clinicians were not prepared to precept students via telepsychiatry.
Communication
Responding to COVID‐19 requires critical preparedness and action, which includes effective communication as an essential strategy. As COVID‐19 spread, health systems in the U.S. aggressively stepped up response measures such as finding, isolating, testing, treating, and tracing transmission. Media and social conversations were dominated by large amounts of information about COVID‐19, of which there was initially little known. Public health information communicated through social networks and traditional media was inconsistent, and messages conveyed were sometimes not well‐received (Cheng et al., 2022; Clemente‐Suárez et al., 2022). America's vast size and decentralized governance structure resulted in uneven implementation of often‐conflicting recommendations coming from epidemiologists, media influencers and government officials. Policies varied by region and mask wearing and other preventive behavior became highly politicized. Conspiracy theories spread on social media, undercutting trust in vaccines, with many persons turning to unproven treatments. On the one hand, nurses were lauded for their heroic efforts in providing care under extremely demanding circumstances, while on the other hand they experienced feelings of disrespect when members of the population balked at masking despite public health recommendations and high rates of COVID‐related hospitalizations and deaths.
Nurses and other health care providers in both primary and acute care health settings also faced challenges of disrupted communication. Protective measures against the virus, such as facemasks, hindered the interpersonal connection with patients (Mheidly et al., 2020). Patients in hospitals were isolated from families and providers needed to limit the frequency of entry into rooms, which placed added stress on nurses in their patient care role. The restricted visitation policies required innovative communication structures and care for nurses, patients, and their family members. Telehealth or telemedicine became a method of choice for most consultations (Klapper et al., 2021; Newman‐Casey et al., 2021; Williams et al., 2021). “Drive‐thru” and curbside clinics were used to provide care for patients who needed in‐person treatment (Halalau et al., 2020; Zobeck et al., 2021).
In nursing education, traditional in‐class lectures, the usual structure of clinicals, and the experience of being with patients were replaced with online education, recorded lectures, practice in a computer simulation, virtual reality, and technology‐enhanced nursing laboratories. One of the most important challenges for this online education was ensuring appropriate learning activities to meet the learning objectives, encouraging students' engagement, and developing clinical reasoning, competency, and a positive attitude toward the profession (Konrad et al., 2021). For students without reliable internet access, the pivot to online education became a source of disparity in access to educational content.
Nursing workforce
The nursing workforce experienced challenges prior to the COVID‐19 pandemi, and health care leaders predicted that hospitals would face a nursing shortage (Buerhaus et al., 2017; Zhang et al., 2018). Between 2016 and 2030, a shortfall of over 500,000 nurses in the U.S. was predicted with a state‐by‐state analysis indicating that the most intense shortage would be in the South and West (Zhang et al., 2018). The main reasons for the anticipated shortage included the number of nurses reaching retirement age, an aging population that requires more medical and health care services, attrition of hospital nurses from direct patient care to other settings or roles or leaving the profession altogether due to occupational stress, and nursing faculty shortages that limit the capacity of nursing schools to accept qualified students (Buerhaus et al., 2017).
The duration, intensity, and repeated surges of the COVID‐19 pandemic have deepened the nursing workforce shortage and cost hospitals an estimated $24 billion to mitigate the staffing shortage (Yang & Mason, 2022). Contributing factors have included an increased demand related to COVID‐19 hospitalizations and critical care needs, an inadequate number of new nursing graduates, and increased attrition. The nursing attrition has been significant as COVID‐19 accentuated pre‐existing nurse burnout and concerns related to well‐being, adequate staffing, working conditions, and salary compensation (Chan et al., 2021). In a recent survey by the American Association of Critical Care Nurses of more than 6500 critical care nurses, 92% of respondents reported that that pandemic had depleted nurses at their hospitals, creating significant challenges and, as a result, their careers will be shorter than they intended (American Association of Critical Care Nurses, 2021). In addition, 66% indicated that they were considering leaving the profession because of dissatisfaction with working conditions and may seek other employment options that provides them with more control over where and when they work. Furthermore, 76% report that unvaccinated patients contribute adversely to nurses' risk for physical and mental well‐being (American Association of Critical Care Nurses, 2021, Yang & Mason, 2022).
Even as COVID‐19 cases fluctuate, U.S. healthcare providers continue to experience the workforce and operational challenges exacerbated by the pandemic (McKinsey & Company, 2022). Patient demand is expected to rise, given the growing and aging population of the U.S. Without addressing this potentially wider divide between patient demand and the clinical workforce, with a specific focus on nurses, the U.S. health sector could face substantial repercussions, including workforce shortages impacting access to health services such as elective surgery (McKinsey & Company, 2022).
Unfortunately, as discussed above, the impact of COVID‐19 on nursing education exacerbated pre‐existing challenges including faculty shortages and problems securing clinical learning experiences. Clinical placement opportunities for students were difficult to arrange due to limited clinical sites, the additional workload student presence can place on healthcare providers, and the growing number of nursing programs (Berry & Bitton, 2020). The pandemic made the clinical placement of nursing students, which has long been a challenging aspect of nursing education, even more complicated.
In the U.S., entry into the nursing profession may include earning a diploma, an Associate Degree in Nursing (ADN), a Bachelor of Science in Nursing (BSN) degree, an accelerated, second‐bachelor's nursing degree where students already have a baccalaureate degree in another discipline, or an entry‐level master's degree from a program designed for students with a bachelor's or graduate degree in a non‐nursing discipline (U.S. Department of Health and Human Services, 2018). While bachelor's degrees account for nearly half of degree types among R.N.s between ages 19 and 23, associate degrees account for more than half of degree types among those who obtained the degree after age 24 (USDHHS, 2018). These findings become an important consideration as new models are identified to address the nursing workforce education pipeline and models of care to address temporary needs.
Lessons learned, opportunities for policy reform and discussion
The novel coronavirus is unlikely to be the last pandemic in the U.S. and globally. To control COVID‐19 and prevent unnecessary suffering and social and economic damage from future pandemics, the U.S. government will need to improve its capacity to protect public health. Complex problems require multi‐level solutions across critical domains. Reforms across levels (individual to community and public policy) and the interacting domains are needed as summarized in Table 1 and elaborated below.
TABLE 1.
Theory and evidence‐based recommendations to address SDOH, mental health, communication and nursing workforce
| Service delivery, health workforce, information, medical products, vaccines, and technologies, financing, leadership/governance | |
|---|---|
| Individual | Physical and mental health preventative self‐care strategies |
| Interpersonal | Development of stronger nursing leadership in healthcare settings • Healthcare provider team support strategies including communication skills • Use of telehealth best practices • Crisis/pandemic communication using best practices • Health care provider use of anti‐bias/health equity language |
| Community | Improve agency‐community intersectoral collaboration • Preparation of nurse providers and CHW for primary care/community‐based roles • Messaging to the public that considers health literacy and other characteristics to meet the diverse community needs • Prioritization of social connectedness and communication with mental health services • Provision of comprehensive, integrated mental health and social care services in community based settings • Implementation and maintenance of rapid evaluation/screening of health, comprehensive treatment of mental health and substance use disorders • Inclusion of screening for SDOH in primary care |
| Public policy | Require health care organizations to compare the quality of care for patients of different races and ethnic groups • Safety standards and oversight locally and/or nationally to protect nurses and other healthcare workers • Improve access to primary and preventive care services with Universal coverage • Investment in preparation of nurse providers/CHWs • Institution of policies and interventions to support the psychological well‐being and resilience of healthcare workers • Investment to improve registered nurse educational pathways and training and tuition support • Federal mandate on expanded telehealth access • Proper education and best practices in providing telehealth • Coordinated trustworthy/reliable public health information • Nursing leadership on integrated pandemic preparedness policies • Nursing advocacy for policies that directly address the social determinants of health • Greater investment in community‐level interventions • Require health care organizations to compare the quality of care for patients of different races and ethnic groups |
Measures must be taken to address social determinants of health and health disparities
As discussed above, disparities in access and health outcomes are entrenched features of the U.S. health care system. When nurses recognize health inequities, they are obligated to address those needs at all appropriate levels including the individual, organizational, and community levels. Social justice, holistic care, and patient advocacy are historically fundamental principles in nursing (National Academies of Sciences, Engineering, and Medicine, 2021a). These principles include addressing the SDOH, particularly among marginalized populations. The effect of the pandemic on communities of color and other vulnerable populations shines a light on systemic inequities in health care. The problem, however, cannot be solved within the health care system alone. Much of the heightened vulnerability of persons of color to COVID‐19 originates outside of health care—in differential access to education, employment, housing, and social justice. Nevertheless, the pandemic refocuses attention on how the health care system can provide stronger, equitable health care while also attending to broader policies that address upstream determinants of health.
Improve agency‐community intersectoral collaboration. Promotion of multiagency collaboration among health, housing, education, and employment services is needed to mobilize social support networks and better access to integrated health care services.
Improve access to primary and preventive care services with Universal Coverage, which, in turn, could reduce the prevalence and severity of chronic illnesses that exacerbate the multi‐dimensional health effects of COVID‐19 and disasters of all types.
Require health care organizations to compare the quality of care for patients of different races and ethnic groups and report these data as a condition for eligibility for Medicare and Medicaid funding.
Improve anti‐bias and health equity training in the education and licensing of health professionals.
Include screening for SDOH in primary care as a routine expectation of high‐quality health care. Improving this screening is critical for identifying and then addressing areas of patient need. Screening can take place in the waiting room using hard copy or electronic forms, or patients can complete screening forms online prior to the visit. In some clinical practices, clinical staff assist with completing a SDOH screening at the visit. During the height of the pandemic, providers and practices quickly transitioned to providing some primary care via telemedicine to decrease COVID‐19 transmission risk for all. Quick and convenient screening tools can be readily embedded in Electronic Health Records.
Greater investment in community‐level interventions. Improved support for safety‐net facilities and small community providers, including inner‐city and rural hospitals and community health centers, could improve access to basic and advanced services for populations of color. These providers would also need support to transition to value‐based care and make contributions to research and evaluation programs in multiple settings (Nkimbeng et al., 2022; Ver Hoeve et al., 2022). Other examples of community focused responses include food delivery for vulnerable community members, access to emergency funds raised by volunteer organizations, virtual mutual support meetings, community conversations and online meetings, local community‐led, user‐led, and family‐led initiatives to provide immediate help and guidance, and the presence of community health workers (CHWs) (Moreno et al., 2020; U.S. Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Professions, 2007)
Nursing advocacy for policies that directly address the social determinants of health. Nursing organizations should take up calls to action from nursing leaders in health equity and engage in the development, advocacy, and implementation of social policies that impact health (National Academies of Sciences, Engineering, and Medicine, 2021a). This includes policies that address equitable housing, labor, and food and social welfare policies which have a direct impact on health and are also key drivers of racial health inequities (American Public Health Association, 2021).
Nursing leadership on integrated pandemic preparedness policies. As experts in holistic models of care that situate patients in the context of their specific circumstances, nurses should lead in the development and implementation of pandemic preparedness policies that explicitly incorporate SDOH and center the unique needs of vulnerable populations. This is also consistent with WHO guidance on human rights principles and the right to health. These models will be particularly salient as we face intersecting emergencies from future pandemics as well as the escalating impacts of climate change (IPCC Sixth Assessment Report, 2022).
Action is urgently needed to strengthen prevention and access to mental health and substance use disorder care
The WHO's Mental Health Action Plan 2013–2030 (2021a) recommends improved general mental health care that includes:
More effective leadership for mental health care;
Provision of comprehensive, integrated mental health and social care in community‐based settings; and,
Implementation of strategies for mental health promotion and prevention
In addition, accelerated strategies during times of crisis are needed including:
Implementation and maintenance of rapid evaluation/screening for comprehensive treatment of mental health and SUD, including the integration of harm reduction programs with other treatment modalities such as walk‐in clinics, mobile crisis units, emergency centers, and alternate field hospital settings. During times of hospital overcapacity, alternative field hospitals should be prepared to evaluate and treat common mental health symptoms and disorders, and to continue care for patients treated by outside providers. Ideally, alternative hospitals should have a system for obtaining outside medical records. Crisis response plans should include coordination with local healthcare educational institutions to provide rapid deployment of faculty and their students to provide service.
Expanded coverage for telehealth and remote coverage and include telemedicine training for outpatient and inpatient healthcare workers to allow a rapid switch from face‐to‐face to virtual visits through telepsychiatry, assuring that alternative mechanisms are in place for those who do not have telephones, fixed addresses, or insurance.
Prioritization of social connectedness and communication with mental health services for all age groups, families, providers, and long‐term care residents. For youth and older adults, maintaining social connectedness is crucial to mental health, and school connectedness is key to addressing youth adversity (Centers for Disease Control and Prevention, 2022a, 2022b). Schools need to develop plans for rapid shifts to reduce risks yet continue to provide opportunities for social connectedness. Planning is necessary to maintain social and familial connections for older adults, manage emotions and psychiatric symptoms to relieve the adverse effects of loneliness and isolation (Hwang et al., 2020). Rosen et al. (2021) and colleagues found that maintaining a structured daily routine, reducing passive screen time, minimizing consumption of pandemic‐related news media, spending more time in nature, and getting adequate sleep were associated with better mental health outcomes for youth during the pandemic. In addition, maintaining ongoing, in‐person socialization when possible is recommended. These strategies are accessible and achievable to many families and should be implemented while the pandemic persists and in the event of future pandemics. Moreno et al. (2020) recommend that the public health response include clear concise and accurate information; and culturally congruent public service messaging to increase mental health literacy. The How Right Now (Centers for Disease Control and Prevention, How Right Now, n.d., 2022a) online website is an example of culturally appropriate resources to help persons cope with severe stress, loss, and the emotional sequelae.
Communication must be improved
Responding to COVID‐19 requires critical preparedness and response which includes effective communication as an essential strategy. It is clear that communication must be strengthened across several dimensions.
Create trustworthy/reliable sources of well‐coordinated public health information. Whether it is at the health systems level or governmental level, communication is crucial to establish trust in the information provided (Hyland‐Wood et al., 2021). While inconsistent messaging is inevitable in a rapidly changing healthcare environment, efforts should be made to coordinate messages that maximize consistency. Although heavily relied upon, there is not robust evidence that explaining the science of a disease and its risks will directly change behavior related to that disease, nor is it likely to alter preexisting habits. The Societal Experts Action Network (SEAN) of the National Academies of Sciences, Engineering, and Medicine's Standing Committee on Emerging Infectious Diseases and 21st Century Health Threats conducted a rapid analyses of COVID‐19 messaging strategies. These analyses found that people are most likely to adhere to health‐protecting guidelines when they experience gratification instantly or shortly thereafter, when they have a sense of self‐efficacy, when they are equipped with information about the appropriate way to implement the recommended behaviors, and when there are minimal barriers to modifying their behavior (National Academies of Sciences, Engineering, and Medicine, 2021b). The SEAN group suggested five habit‐promoting strategies to normalize the use of protective measures and increase the likelihood of behavior change: (1) Make the behavior easy to start and repeat; (2) Make the behavior rewarding to repeat; (3) Tie the behavior to an existing habit; (4) Alert people to behaviors that conflict with existing habits and provide alternative behaviors; and (5) Provide specific descriptions of desired behaviors. The SEAN group also recommended 10 risk communication strategies: (1) Use clear, consistent, and transparent messaging; (2) Avoid undue attention to the frequency of socially undesirable behaviors; (3) Foster a sense of efficacy and avoid fatalism; (4) Appeal to the collective good of one's community; (5) Use messengers trusted by the target audience; (6) Tailor the framing of the message to the audience; (7) Link prevention behaviors to people's identities; (8) Highlight social disapproval of a target audience member's failure to comply when it occurs; (9) Highlight the growing prevalence of behavior change within the target audience when it occurs; and (10) Avoid repeating misinformation, even to debunk it.
Combat misinformation with use of effective, evidence‐based messaging strategies.
Combating misinformation has been particularly challenging during the COVID‐19 pandemic, but it is critical for increasing COVID‐19 vaccination as well as managing any subsequent pandemics or health issues that may be politicized/weaponized in the future. Wen‐Ying Sylvia Chou, program director of the Health Communication and Informatics Research Branch at the National Cancer Institute (NCI) of the National Institutes of Health (NIH), identified six major COVID‐19 misinformation topics (National Academies of Sciences, Engineering, and Medicine, 2020): (1) disease characteristics, (2) origins and spread of the virus, (3) federal, state, and local government and organization responses, (4) individuals' prevention behaviors, (5) unproven treatments, and (6) vaccine attitudes. Communication strategies for combating misinformation include the following: (1) induce skepticism toward disinformation agents (similar to the discrediting of tobacco marketing); (2) develop tools to help identify and access credible information sources and resources for debunking myths and misinformation; (3) cultivate science literacy: understanding the uncertain and evolving nature of science; (4) combat conspiracy theories by partnering with former members and trusted influencers; (5) mobilize the public health majority to counter online misinformation; (6) proactively monitor, flag, down rank, and remove content or accounts that promote misinformation; and (7) reconfigure platform features that amplify misinformation (e.g., Twitter's handling of QAnon and Facebook's and Google's removal of misinformation).
Nurses, the most trusted profession in the U.S. for the 20th consecutive year (Saad, 2022), should be active in providing factual and current information to the public.
Messaging to the public should consider health literacy to meet the diverse community needs. There should be coordination between intersectoral groups to develop programs to improve health literacy and resources and amplify public health messages (National Academies of Sciences, Engineering, and Medicine, 2020).
Use telehealth best practices. Even though the federal government took steps to ensure telehealth could be used to improve communication with patients and access to care, it is important to mandate proper education on best practices in providing telehealth. Funding is also needed for nursing schools to purchase immersive learning technologies to account for limited access to clinical placements during pandemics.
There must be greater investment in and support of the nursing and healthcare workforce
The COVID‐19 pandemic has had a significant and negative impact on the nursing workforce and exacerbated workforce challenges that existed prior to COVID‐19 as discussed above. Short‐ and long‐term strategies must be taken to mitigate the adverse effects of the pandemic and pre‐existing underlying conditions affecting the nursing workforce (World Health Organization, 2020b, 2021b). Key recommendations include actions to enhance the supply of nurses for roles in primary care as well as acute care settings while at the same time enacting reforms to improve workplace conditions.
Establish safety standards to protect nurses and other healthcare workers relative to safe staffing models and prevention of workplace violence for healthcare workers including violence by patients and families. Such policies are best established at the institutional/organizational level with review by regulatory agencies such as The Joint Commission on Accreditation of Healthcare Organizations. There are legislative policies under consideration nationally such as the Nurse Staffing Standards for Hospital Patient Safety https://www.congress.gov/bill/117th‐congress/house‐bill/3165 and the Quality Care Act and the Workplace Violence Prevention for Health Care and Social Service Workers Act https://www.congress.gov/bill/117th‐congress/house‐bill/1195
Develop nursing leadership to maintain an environment of trust, psychological safety, and empowerment.
Implement team support strategies including communication skills and protocols to address with workplace violence, suffering, and death. For example, team members should be encouraged to monitor and support each other, identify serious issues, provide peer support (Bartels et al., 2020), and develop a buddy system that trains workers to watch out for each other in crisis situations has been useful in prior disaster situations (NIOSH, 2020a, 2020b).
Institute policies and interventions to support the psychological well‐being and resilience of healthcare workers in disease outbreaks, including work scheduling and time off policies, supportive services for staff (rooms for rest), and access to more support without stigma or punishment if needed.
Hospitals and other clinical agencies should address workforce stress, violence and mental health concerns. Institutional changes and programs that foster a healthy and safe work environment are crucial. Prioritize the need for nursing and other staff for downtime. Consider offering mental health programs, fitness programs or childcare assistance. Although many hospitals offer employee assistance programs, consider expanding resources to on‐site or virtual counseling, mental health self‐screening, and wellness workshops. Resiliency training provide nurses with the knowledge and strategies to address moral and soul distress from the realities of healthcare and in particular, pandemic related challenges such as patient mortality, concern for risk to families, and equipment shortages.
Develop educational materials and supportive learning environments for nurses and other frontline workers to develop accurate knowledge and beliefs about symptoms of anxiety, depression, acute stress, and the resources available to help them and educate healthcare workers in psychological first aid (Blake & Bermingham, 2020, Blake et al., 2020; Everly, 2020).
Decrease reliance on travel or agency nursing. The demand for travel or agency nursing in the U.S. has exploded during the pandemic as hospitals struggled to meet unprecedented workforce shortages. Decreasing the use of travel nurses is critical to provide a stable expert nursing workforce and continuity for hospitals. Improving conditions that retain the nurse workforce is critically important to reduce reliance on travel nurses.
Reset nurses' relationships with hospitals to provide them with more predictability and control (Buerhaus, 2021) and encourage use of staff council and shared governance to address nurse identified needs and include them in the process.
Support continuing education programs that allow nurses to pursue areas of interest and contribute to satisfaction. Likewise, promoting internal career paths and promotions will retain nurses within an institution. To address immediate workforce shortages, new models of care that create a team led by a registered nurses along with an LPN and/or nursing aide/tech to provide care for patients. This option helps hospitals address immediate needs while simultaneously addressing long term solutions to recruit and retain nurses (Maryland Higher Education Commission I & II, n.d.).
Maintain R.N. residency programs to facilitate the transition for new graduates through education, mentoring, and service‐based projects (MHEC NSP [Link], [Link]).
-
Improve registered nurse educational pathways and training. The Future of Nursing 2020–2030 report (NASEM, 2021a) advocates for seamless education pathways for registered nursing for unlicensed personnel (e.g., medics and nursing aides and licensed practical nurses), improving retention and well‐being of existing nurses through improved conditions, staffing, and compensation, and creating new models of nursing care to address immediate workforce needs. Creating efficiencies in prerequisite and pre‐licensure nursing education taps into an existing pool of potential nursing applicants by generating options and efficiencies in education programs pathways for health professionals leading to the B.S. in nursing, which the research demonstrates is associated with improved patient morbidity and outcomes (Aiken, Cimiotti, et al., 2011, Aiken, Sloane, et al., 2011; Aiken et al., 2012). Second degree programs in nursing have been in existence for over 25 years, yet many programs require that students complete similar prerequisite courses and nursing curricular programs to non‐degree nursing students. This increases the time and cost for registered nurse education.
The pandemic accelerated the use of distance‐based learning and virtual simulation to create educational continuity and flexible access for prerequisite nursing education and pre‐licensure education. At the Johns Hopkins School of Nursing, the prerequisite program for health professions offers rigorous online education and virtual laboratory learning. In addition, distance‐based education degree programs, coupled with occasional immersive onsite learning, offer flexible options as schools adapt to clinical site availability. However, access to reliable internet access remains a challenge for rural areas, home internet services, and environments not conducive to learning such as multi‐generational home and inadequate housing (Chan et al., 2021).
Improvement of student tuition support is crucial, through loan forgiveness programs or employment based tuition support, to attract qualified applicants to nursing at a time of a nursing workforce crisis that impacts access to care.
Schools and practice should partner to identify new models of supervision that may provide incentives for experienced nurses to serve as preceptors and clinical instructor quality so that the burden on practice is decreased.
Invest in preparation of nurses for primary health care and community‐based roles to advance access to care especially in underserved areas.
Strengthen information systems, evidence, and research to guide policies. Funding and research are needed to evaluate general population needs during and after the pandemic, the impact of quarantine, media exposure, decreased ability to obtain in‐person services, social distancing, and uncertainty. Research is also needed to evaluate the effectiveness of and barriers and facilitators to interventions that support the resilience of frontline workers and vulnerable populations (Pollock et al., 2020), and to examine emerging roles and functions that work (Buerhaus et al., 2019). Observational studies and natural experiments can help to provide necessary evidence to guide policies aimed at containing the spread of the infection, while safeguarding mental health (Taquet & Harrison, 2022).
CONCLUSIONS
COVID‐19 and other recent infectious disease outbreaks have highlighted the urgentcy for robust, resilient health systems. We now have the opportunity to reform the flawed health care system that made COVID‐19 far more damaging than necessary in the U.S. SDOH, mental health, nurse workforce, and communication are four inter‐related, critically important domains for improvement individually, interpersonally, within communities, and in public policy reform.
AUTHOR CONTRIBUTIONS
All authors made substantial contributions to the conception and design, acquisition, analysis, and interpretation of data for the work. Additionally, they drafted the work and revised it critically for important intellectual content and approved the final version to be published.
CONFLICT OF INTEREST
No conflict of interest has been declared by the author(s).
CLINICAL RESOURCES
WHO Global Community of Nursing and Midwifery Practice. Global Community of Practice for Nursing and Midwifery (nursingandmidwiferyglobal.org)
National Academies of Sciences, Engineering, and Medicine (2021a). The Future of Nursing 2020–2030: Charting a path to achieve health equity. https://nap.nationalacademies.org/catalog/25982/the‐future‐of‐nursing‐2020‐2030‐charting‐a‐path‐to
American Psychiatric Nurses Association. Expanding mental health care services in America. https://www.apna.org
American Nurse. Preventing the spread of misinformation. https://www.myamericannurse.com/preventing‐the‐spread‐of‐misinformation/
International Council of Nurses. https://www.icn.ch/
American Academy of Nursing. https://www.aannet.org/home
American Association of Critical Care Nurses. Policy and Advocacy. https://www.aacn.org/policy‐and‐advocacy
Reynolds, N. R. , Baker, D. , D’Aoust, R. , Docal, M. , Goldstein, N. , Grubb, L. , Hladek, M. D. , Koirala, B. , Kverno, K. , Ling, C. , Lukkahatai, N. , McIltrot, K. , Pandian, V. , Regier, N. G. , Sloand, E. , Tomori, C. & Wenzel, J. (2023). COVID‐19: Implications for nursing and health Care in the United States. Journal of Nursing Scholarship, 55, 187–201. 10.1111/jnu.12853
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study
REFERENCES
- Adegboye, D. , Williams, F. , Collishaw, S. , Shelton, K. , Langley, K. , Hobson, C. , Burley, D. , & van Goozen, S. (2021). Understanding why the COVID‐19 pandemic‐related lockdown increases mental health difficulties in vulnerable young children. JCPP Advances, 1, e12005. 10.1111/jcv2.12005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken, L. H. , Cimiotti, J. , Sloane, D. M. , Smith, H. L. , Flynn, L. , & Neff, D. (2011). The effects of nurse staffing and nurse education on patient deaths in hospitals with different nurse work environments. Medical Care, 49(10), 1047–1053. 10.1097/MLR.0b013e3182330b6e [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken, L. H. , Sermeus, W. , van den Heede, K. , Sloane, D. M. , Busse, R. , McKee, M. , Bruyneel, L. , Rafferty, A. M. , Griffiths, P. , Moreno‐Casbas, M. T. , Tishelman, C. , Scott, A. , Brzostek, T. , Kinnunen, J. , Schwendimann, R. , Heinen, M. , Zikos, D. , Sjetne, I. S. , Smith, H. L. , & Kutney‐Lee, A. (2012). Patient safety, satisfaction, and quality of hospital care: Cross‐sectional surveys of nurses and patients in 12 countries in Europe and the United States. British Medical Journal, 344, e1717. 10.1136/bmj.e1717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken, L. H. , Sloane, D. M. , Clarke, S. , Poghosyan, L. , Cho, E. , You, L. , Finlayson, M. , Kanai‐Pak, M. , & Aungsuroch, Y. (2011). Importance of work environments on hospital outcomes in 9 countries. Quality Assurance in Health Care, 23(4), 357–364. 10.1093/intqhc/mzr022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altibi, A. M. , Pallavi, B. , Liaqat, H. , Slota, A. A. , Sheth, R. , Al Jebbawi, L. , George, M. E. , LeDuc, A. , Abdallah, E. , Russell, L. R. , Jain, S. , Shirvanian, N. , Masri, A. , & Kak, V. (2021). Characteristics and comparative clinical outcomes of prisoner versus non‐prisoner populations hospitalized with COVID‐19. Scientific Reports, 11(1), 1–9. 10.1038/s41598-021-85916-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Association of Critical Care Nurses . (2021). Hear us out campaign reports Nurses' COVID‐19 reality. https://www.aacn.org/newsroom/hear‐us‐out‐campaign‐reports‐nurses‐covid‐19‐reality
- American Nurses Association . (2022). Nurses in the workforce. https://www.nursingworld.org/practice‐policy/workforce/
- American Association of Public Health . (2021). Call for urgent actions to address health inequities in the U.S. Coronavirus disease 2019 pandemic and response. Policy Statement 20218. https://apha.org/?Policies‐and‐Advocacy/Public‐Health‐Policy‐Statements/
- Arias, E. , Tejada‐Vera, B. , Kochanek, K. D. , & Ahmad, F. B. (2022). Provisional life expectancy estimates for 2021. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System, Report 23. https://www.cdc.gov/nchs/products/index.htm
- Bailey, Z. D. , Krieger, N. , Agénor, M. , Graves, J. , Linos, N. , & Bassett, M. T. (2017). Structural racism and health inequities in the USA: Evidence and interventions. The Lancet, 389(10077), 1453–1463. 10.1016/S0140-6736(17)30569-X [DOI] [PubMed] [Google Scholar]
- Bandara, S. , Maniates, H. , Hulsey, E. , Smith, J. S. , DiDomenico, E. , Stuart, E. A. , Saloner, B. , & Krawczyk, N. (2022). Opioid treatment program safety measures during the COVID‐19 pandemic: A statewide survey. BMC Health Services Research, 22(1), 418. 10.1186/s12913-022-07832-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron, S. L. , Beard, S. , Davis, L. K. , Delp, L. , Forst, L. , Kidd‐Taylor, A. , Liebman, A. K. , Linnan, L. , Punnett, L. , & Welch, L. S. (2014). Promoting integrated approaches to reducing health inequities among low‐income workers: Applying a social ecological framework. American Journal of Industrial Medicine, 57, 539–556. 10.1002/ajim.22174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartels, S. J. , Baggett, T. P. , Freudenreich, O. , & Bird, B. L. (2020). COVID‐19 emergency reforms in Massachusetts to support behavioral health care and reduce mortality of people with serious mental illness. Psychiatric Services, 71(10), 1078–1081. 10.1176/appi.ps.202000244 [DOI] [PubMed] [Google Scholar]
- Berry, D. M. , & Bitton, J. R. (2020). Not working well: Clinical placement for nursing students in an era of a pandemic world. Oregon Center for Nursing. https://oregoncenterfornursing.org/wp‐content/uploads/2020/09/COVID‐Era‐Clinical‐Placement‐Assessment.pdf
- Blake, H. , Bermingham, F. (2020). Psychological wellbeing for healthcare workers: Mitigating the impact of COVID‐19. The University of Nottingham, version 2.0. https://www.nottingham.ac.uk/toolkits/play_22794
- Blake, H. , Bermingham, F. , Johnson, G. , & Tabner, A. (2020). Mitigating the psychological impact of COVID‐19 on healthcare workers: A digital learning package. International Journal of Environmental Research and Public Health, 17(9), 2997. 10.3390/ijerph17092997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buerhaus, P. , Martsof, G. , Donelan, K. , Clarke, S. , Barnes, H. , Cohen, C. C. , & Cooley, H. T. (2019). Nursing health services research agenda for the 2020 s. https://www.montana.edu/nursing [DOI] [PubMed]
- Buerhaus, P. I. (2021). Creating the 21st century nursing workforce needed by society: Building on our strengths to address post pandemic health needs of society. Virginia Lee Franklin Lecture. https://www.nursing.umaryland.edu/media/son/academics/professional‐education/FINAL‐UMaryland‐Buerhaus‐Nov‐9.pdf
- Buerhaus, P. I. , Skinner, L. E. , Auerbach, D. I. , & Staiger, D. O. (2017). State of the registered nurse workforce as a new era of health reform emerges. Nursing Economics, 35(5), 229–237. [Google Scholar]
- Centers for Disease Control and Prevention . (2021). Drug overdose deaths top 100,000 annually. https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2021/20211117.htm
- Centers for Disease Control and Prevention . (2022a). COVID‐19 weekly cases and deaths per 100,000 population by age, race/ethnicity, and sex March 1, 2020 to May 28, 2022. https://covid.cdc.gov/covid‐data‐tracker/#demographicsovertime [Google Scholar]
- Centers for Disease Control and Prevention . (2022b). Long‐COVID or post‐COVID conditions. https://www.cdc.gov/coronavirus/2019‐ncov/long‐term‐effects/index.html
- Centers for Disease Control and Prevention . (n.d.). The socio‐ecological model: A framework for prevention. https://www.cdc.gov/violenceprevention/about/social‐ecologicalmodel.html
- Centers for Disease Control and Prevention . (n.d.). How right now. https://www.cdc.gov//howrightnow//
- Chan, G. K. , Bitton, J. R. , Allgeyer, R. L. , Elliott, D. , Hudson, L. R. , & Moulton Burwell, P. (2021). The impact of COVID‐19 on the nursing workforce: A National Overview. OJIN: The Online Journal of Issues in Nursing, 26(2). 10.3912/OJIN.Vol26No02Man02 [DOI] [Google Scholar]
- Cheah, C. S. L. , Wang, C. , Ren, H. , Zong, X. , Cho, H. S. , & Xue, X. (2020). COVID‐19 racism and mental health in Chinese American families. Pediatrics, 146(5), e2020021816. 10.1542/peds.2020-021816 [DOI] [PubMed] [Google Scholar]
- Cheng, Y. , Wang, Y. , & Zhao, W. (2022). Shared virtual reality experiences during the COVID‐19 pandemic: Exploring the gratifications and effects of engagement with immersive videos. International Journal of Environmental Research and Public Health, 19(9), 5056. 10.3390/ijerph19095056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clemente‐Suárez, V. J. , Navarro‐Jiménez, E. , Simón‐Sanjurjo, J. A. , Beltran‐Velasco, A. I. , Laborde‐Cárdenas, C. C. , Benitez‐Agudelo, J. C. , Bustamante‐Sánchez, Á. , & Tornero‐Aguilera, J. F. (2022). Mis‐dis information in COVID‐19 health crisis: A narrative review. IJERPH, 19(9), 5321. 10.3390/ijerph19095321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowley, R. , Daniel, H. , Cooney, T. G. , & Engel, L. S. (2020). Envisioning a better U.S. health care system for all: Coverage and cost of care. Annals of Internal Medicine, 172, S7–S32. 10.7326/M19-2415 [DOI] [PubMed] [Google Scholar]
- Dadiomov, D. , Trotzky‐Sirr, R. , Shooshtari, A. , & Qato, D. M. (2022). Changes in the availability of medications for opioid use disorder in prisons and jails in the United States during the COVID‐19 pandemic. Drug and Alcohol Dependence, 232, 109291. 10.1016/j.drugalcdep.2022.109291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalkey, N. , & Helmer, O. (1963). An experimental application of the Delphi method to the use of experts. Management Science, 9(3), 458–467. 10.1287/mnsc.9.3.458 [DOI] [Google Scholar]
- Dalva‐Baird, N. P. , Alobuia, W. M. , Bendavid, E. , & Bhattacharya, J. (2021). Racial and ethnic inequities in the early distribution of U.S. COVID‐19 testing sites and mortality. European Journal of Clinical Investigation, 51(11), e13669. 10.1111/eci.13669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everly, G. S. (2020). Psychological first aid to support healthcare professionals. Journal of Patient Safety and Risk Management, 24(4), 159–162. 10.1177/2516043520944637 [DOI] [Google Scholar]
- Fegert, J. M. , Vitiello, B. , Plener, P. L. , & Clemens, V. (2020). Challenges and burden of the coronavirus 2019 (COVID‐19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child and Adolescent Psychiatry and Mental Health, 14, 20. 10.1186/s13034-020-00329-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia, M. A. , Homan, P. A. , García, C. , & Brown, T. H. (2021). The color of COVID‐19: Structural racism and the disproportionate impact of the pandemic on older black and Latinx adults. The Journals of Gerontology: Series B, 76(3), e75–e80. 10.1093/geronb/gbaa114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giorgi, G. , Lecca, L. I. , Alessio, F. , Finstad, G. L. , Bondanini, G. , Lulli, L. G. , & Mucci, N. (2020). COVID‐19‐related mental health effects in the workplace: A narrative review. International Journal of Environmental Research and Public Health, 17(21), 7857. 10.3390/ijerph17217857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golembeski, C. A. , Irfan, A. , & Dong, K. R. (2020). Food insecurity and collateral consequences of punishment amidst the COVID‐19 pandemic. World Medical & Health Policy, 12(4), 357–373. 10.1002/wmh3.378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halalau, A. , Ditkoff, J. , Hamilton, J. , Sharrak, A. , Vanood, A. , Abbas, A. , & Ziadeh, J. (2020). Emergency center curbside screening during the COVID‐19 pandemic: Retrospective cohort study. JMIR Public Health Surveillance, 6(3), e20040. 10.2196/20040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haldane, V. , de Foo, C. , Abdalla, S. M. , Jung, A. S. , Tan, M. , Wu, S. , Chua, A. , Verma, M. , Shrestha, P. , Singh, S. , Perez, T. , Tan, S. M. , Bartos, M. , Mabuchi, S. , Bonk, M. , McNab, C. , Werner, G. K. , Panjabi, R. , Nordström, A. , & Legido‐Quigley, H. (2021). Health systems resilience in managing the COVID‐19 pandemic: Lessons from 28 countries. Nature Medicine, 27, 964–980. 10.1038/s41591-021-01381-y [DOI] [PubMed] [Google Scholar]
- Hatcher, S. M. , Agnew‐Brune, C. , Anderson, M. , Zambrano, L. D. , Rose, C. E. , Jim, M. A. , Baugher, A. , Liu, G. S. , Patel, S. V. , Evans, M. E. , Pindyck, T. , Dubray, C. L. , Rainey, J. J. , Chen, J. , Sadowski, C. , Winglee, K. , Penman‐Aguilar, A. , Dixit, A. , Claw, E. , … McCollum, J. (2020). COVID‐19 among American Indian and Alaska native persons—23 states, January 31–July 3, 2020. Morbidity and Mortality Weekly Report, 69, 1166–1169. 10.15585/mmwr.mm6934e1externalicon [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havervall, S. , Rosell, A. , Phillipson, M. , Mangsbo, S. M. , Nilsson, P. , Hober, S. , & Thålin, C. (2021). Symptoms and functional impairment assessed 8 months after mild COVID‐19 among health care workers. JAMA, 325(19), 2015–2016. 10.1001/jama.2021.5612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healthy People . (2030). U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. https://health.gov/healthypeople/objectives‐and‐data/social‐determinants‐health
- Houben‐Wilke, S. , Goërtz, Y. M. , Delbressine, J. M. , Vaes, A. W. , Meys, R. , Machado, F. V. , van Herck, M. , Burtin, C. , Posthuma, R. , Franssen, F. M. , Vijlbrief, H. , Spies, Y. , van't Hul, A. , Spruit, M. A. , & Janssen, D. J. (2022). The impact of long COVID‐19 on mental health: Observational 6‐month follow‐up study. JMIR Mental Health, 9(2), e33704. 10.2196/33704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang, T. J. , Rabheru, K. , Peisah, C. , Reichman, W. , & Ikeda, M. (2020). Loneliness and social isolation during the COVID‐19 pandemic. International Psychogeriatrics, 32(10), 1217–1220. 10.1017/S1041610220000988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyland‐Wood, B. , Gardner, J. , & Ecker, U. K. H. (2021). Toward effective government communication strategies in the era of COVID‐19. Humanities and Social Sciences Communications, 8(1), 30. 10.1057/s41599-020-00701-w [DOI] [Google Scholar]
- IPCC Sixth Assessment Report . (2022). Climate change 2022: Impacts, adaptation, and vulnerability. https://www.ipcc.ch/report/ar6/wg2/
- Jones, S. E. , Ethier, K. A. , Hertz, M. , DeGue, S. , Le, V. D. , Thornton, J. , & Geda, S. (2022). Mental health, suicidality, and connectedness among high school students during the COVID‐19 pandemic – Adolescent behaviors and experiences survey, United States, January – June 2021. MMWR, 71, 16–21. 10.15585/mmwr.su7103a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kearney, A. , Hamel, L. , Stokes, M. , & Brodie, M. (2021). Americans' challenges with health care costs. KFF. https://www.kff.org/health‐costs/issue‐brief/americans‐challenges‐with‐health‐care‐costs/
- Khatri, U. G. , & Perrone, J. (2020). Opioid use disorder and COVID‐19: Crashing of the crises. Journal of Addiction Medicine, 14(4), e6–e7. 10.1097/ADM.0000000000000684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilanowski, J. F. (2017). Breadth of the socio‐ecological model. Journal of Agromedicine, 22(4), 295–297. 10.1080/1059924X.2017.1358971 [DOI] [PubMed] [Google Scholar]
- Klapper, J. , Bardakjian, T. , Sigal, I. , Muralidharan, K. , & Gonzalez‐Alegre, P. (2021). Healthcare delivery via telehealth during the COVID‐19 pandemic: The experience of a Huntington's disease clinic. Clinical Parkinsonism & Related Disorders, 4, 100093. 10.1016/j.prdoa.2021.100093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konrad, S. , Fitzgerald, A. , & Deckers, C. (2021). Nursing fundamentals – Supporting clinical competency online during the COVID‐19 pandemic. Teaching and Learning in Nursing, 16(1), 53–56. 10.1016/j.teln.2020.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreger, M. , Sargent, K. , Arons, A. , Standish, M. , & Brindis, C. D. (2011). Creating an environmental justice framew, ork for policy change in childhood asthma: A grassroots to treetops approach. American Journal of Public Health, 101(Suppl. 1), S208–S216. 10.2105/AJPH.2011.300188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lei, L. , & Maust, D. T. (2022). Delayed care related to COVID‐19 in a nationally representative sample of older Americans. Journal of General Internal Medicine, 37(5), 1337–1340. 10.1007/s11606-022-07417-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lekamwasam, R. , & Lekamwasam, S. (2020). Effects of COVID‐19 pandemic on health and wellbeing of older people: A comprehensive review. Annals of Geriatric Medicine and Research, 24(3), 166–172. 10.4235/agmr.20.0027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeMasters, K. , Brinkley‐Rubinstein, L. , Maner, M. , Peterson, M. , Nowotny, K. , & Bailey, Z. (2022). Carceral epidemiology: Mass incarceration and structural racism during the COVID‐19 pandemic. The Lancet Public Health, 7(3), e287–e290. 10.1016/S2468-2667(22)00005-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, Y. , Scherer, N. , Felix, L. , & Kuper, H. (2021). Prevalence of depression, anxiety and post‐traumatic stress disorder in health care workers during the COVID‐19 pandemic: A systematic review and meta‐analysis. PLoS One, 16(3), e0246454. 10.1371/journal.pone.0246454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loades, M. E. , Chatburn, E. , Higson‐Sweeney, N. , Reynolds, S. , Shafran, R. , Brigden, A. , & Crawley, E. (2020). Rapid systematic review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID‐19. Journal of the American Academy of Child and Adolescent Psychiatry, 59(11), 1218–1239.e3. 10.1016/j.jaac.2020.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luck, A. N. , Preston, S. H. , Elo, I. T. , & Stokes, A. C. (2022). The unequal burden of the Covid‐19 pandemic: Capturing racial/ethnic disparities in U.S. cause‐specific mortality. SSM – Population Health, 17, 101012. 10.1016/j.ssmph.2021.101012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magson, N. R. , Freeman, J. Y. A. , Rapee, R. M. , Richardson, C. E. , Oar, E. L. , & Fardouly, J. (2021). Risk and protective factors for prospective changes in adolescent mental health during the COVID‐19 pandemic. Journal of Youth and Adolescence, 50, 44–57. 10.1007/s10964-020-01332-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marquez, N. , Ward, J. A. , Parish, K. , Saloner, B. , & Dolovich, S. (2021). COVID‐19 incidence and mortality in federal and state prisons compared with the U.S. population, April 5, 2020, to April 3, 2021. JAMA, 326(18), 1865–1867. 10.1001/jama.2021.17575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maryland Higher Education Commission . Nurse Support Program, Nurse Support I. https://nursesupport.org/nurse‐support‐program‐i/
- Maryland Higher Education Commission Nurse Support Program, Nurse Support II. https://nursesupport.org/nurse‐support‐program‐ii/
- McGovern, L. , Miller, G. , & Hughes‐Cromwick, P. (2014). Health policy brief. The relative contribution of multiple determinants to health outcomes. Health Affairs. 10.1377/HPB20140821.404487 [DOI]
- McKinsey & Company . (2022). Survey: U.S. hospital patient volumes move back towards 2019 levels. https://www.mckinsey.com/industries/healthcare‐systems‐and‐services/our‐insights/survey‐us‐hospital‐patient‐volumes‐move‐back‐towards‐2019‐levels
- McKnight‐Eily, L. R. , Okoro, C. A. , Strine, T. W. , Verlenden, J. , Hollis, N. D. , Njai, R. , Mitchell, E. W. , Board, A. , Puddy, R. , & Thomas, C. (2021). Racial and ethnic disparities in the prevalence of stress and worry, mental health conditions, and increased substance use among adults during the COVID‐19 pandemic – United States April and May 2020. Morbidity and Mortality Weekly Report, 70, 162–166. 10.15585/mmwr.mm7005a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeroy, K. R. , Bibeau, D. , Steckler, A. , & Glanz, K. (1988). An ecological perspective on health promotion programs. Health Education Quarterly, 15(4), 351–377. 10.1177/1090198188015004 [DOI] [PubMed] [Google Scholar]
- Mheidly, N. , Fares, M. Y. , Zalzale, H. , & Fares, J. (2020). Effect of face masks on interpersonal communication during the COVID‐19 pandemic. Frontiers in Public Health, 8, 582191. 10.3389/fpubh.2020.582191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreno, C. , Wykes, T. , Galderisi, S. , Nordentoft, M. , Crossley, N. , Jones, N. , Cannon, M. , Correll, C. U. , Byrne, L. , Carr, S. , Chen, E. Y. H. , Gorwood, P. , Johnson, S. , Kärkkäinen, H. , Krystal, J. H. , Lee, J. , Lieberman, J. , López‐Jaramillo, C. , Männikkö, M. , … Arango, C. (2020). How mental health care should change as a consequence of the COVID‐19 pandemic. The Lancet Psychiatry, 7(9), 813–824. 10.1016/S2215-0366(20)30307-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine . (2020). Addressing health misinformation with health literacy strategies: Proceedings of a workshop—in brief. The National Academies Press. 10.17226/26021 [DOI] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine . (2021a). The future of nursing 2020–2030: Charting a path to achieve health equity. The National Academies Press. 10.17226/25982 [DOI] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine . (2021b). Critical findings on COVID‐19: Select publications from the National Academies of sciences, engineering, and medicine. The National Academies Press. 10.17226/26100 [DOI] [PubMed] [Google Scholar]
- Newman‐Casey, P. A. , De Lott, L. , Cho, J. , Ballouz, D. , Azzouz, L. , Saleh, S. , & Woodward, M. A. (2021). Telehealth‐based eye care during the COVID‐19 pandemic: Utilization, safety and the patient experience. American Journal of Ophthalmology, 230, 234–242. 10.1016/j.ajo.2021.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nkimbeng, M. , Han, H. , Szanton, S. L. , Alexander, K. A. , Davey‐Rothwell, M. , Giger, J. T. , Gitlin, L. N. , Joo, J. H. , Koeuth, S. , Marx, K. A. , Mingo, C. A. , Samuel, L. J. , Taylor, J. L. , Wenzel, J. , & Parisi, J. M. (2022). Exploring challenges and strategies in partnering with community‐based organizations to advance intervention development and implementation with older adults. The Gerontologist, 62(8), 1104–1111. 10.1093/geront/gnab190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panchal, N. , Kamal, R. , Cox, C. , & Garfield, R. (2021). The implications of COVID‐19 for mental health and substance use. https://www.kff.org/coronavirus‐covid‐19/issue‐brief/the‐implications‐of‐covid‐19‐for‐mental‐health‐and‐substance‐use/#:~:text=The%20KFF%20Health%20Tracking%20Poll,eating%2C%20increases%20in%20alcohol%20consumption
- Pollock, A. , Campbell, P. , Cheyne, J. , Cowie, J. , Davis, B. , McCallum, J. , McGill, K. , Elders, A. , Hagen, S. , McClurg, D. , Torrens, C. , & Maxwell, M. (2020). Interventions to support the resilience and mental health of frontline health and social care professionals during and after a disease outbreak, epidemic or pandemic: A mixed methods systematic review. Cochrane Review, 11(11), CD013779. 10.1002/14651858.CD013779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rawal, S. , Tackett, R. L. , Stone, R. H. , & Young, H. N. (2022). COVID‐19 vaccination among pregnant people in the U.S: A systematic review. American Journal of Obstetrics & Gynecology MFM, 4(4), 100616. 10.1016/j.ajogmf.2022.100616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen, M. L. , Rodman, A. M. , Kasparek, S. W. , Mayes, M. , Freeman, M. M. , Lengua, L. J. , Meltzoff, A. N. , & McLaughlin, K. (2021). Promoting youth mental health during the COVID‐19 pandemic: A longitudinal study. PLoS One, 16(8), e0255294. 10.1371/journal.pone.0255294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saad, L. (2022). Gallup, January 12, 2022 Military brass, judges, among professions at new image low. https://news.gallup.com/poll/388649/military‐brass‐judges‐among‐professions‐new‐image‐lows.aspx
- Sallis, J. F. , Owen, N. , & Fisher, E. B. (2008). Ecological models of health behavior. In Glanz K., Rimer B. K., & Viswanath K. (Eds.), Health behavior and health education: Theory, research, and practice (pp. 465–485). Jossey‐Bass. [Google Scholar]
- Schou, T. M. , Joca, S. , Wegener, G. , & Bay‐Richter, C. (2021). Psychiatric and neuropsychiatric sequelae of COVID‐19 ‐ a systematic review. Brain, Behavior, and Immunity, 97, 328–348. 10.1016/j.bbi.2021.07.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi, D. S. , Whitaker, M. , Marks, K. J. , Anglin, O. , Milucky, J. , Patel, K. , Pham, H. , Chai, S. J. , Kawasaki, B. , Meek, J. , Anderson, E. J. , Weigel, A. , Henderson, J. , Lynfield, R. , Ropp, S. L. , Muse, A. , Bushey, S. , Billing, L. M. , Sutton, M. , … COVID‐NET Surveillance Team . (2022). Hospitalizations of children aged 5‐11 years with laboratory‐confirmed COVID‐19 – COVID‐NET, 14 states, March 2020‐February 2022. Morbidity and Mortality Weekly Report, 71(16), 574–581. 10.15585/mmwr.mm7116e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taquet, M. , Geddes, J. R. , Husain, M. , Luciano, S. , & Harrison, P. J. (2021). 6‐month neurological and psychiatric outcomes in 236 379 survivors of COVID‐19: a retrospective cohort study using electronic health records. The Lancet Psychiatry, 8(5), 416–427. 10.1016/s2215-0366(21)00084-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taquet, M. , & Harrison, P. J. (2022). Restricting the spread of SARS‐CoV‐2 or safeguarding mental health: A false dichotomy? The Lancet. Public Health, 7(5), e392–e393. 10.1016/S2468-2667(22)00091-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The National Institute for Occupational Safety and Health . (2021a). Protecting health worker mental health: A call to action. https://www.cdc.gov/niosh/topics/healthcare/workstress.html
- The National Institute for Occupational Safety and Health . (2021b). Mental health initiative for healthcare workers. https://www.cdc.gov/niosh/bsc/pdfs/MentalHealthInitiativeForHealthWorkers_508.pdf
- Tomori, C. , Gribble, K. , Palmquist, A. E. , Ververs, M. T. , & Gross, M. S. (2020). When separation is not the answer: Breastfeeding mothers and infants affected by COVID‐19. Maternal & Child Nutrition, 16(4), e13033. 10.1111/mcn.13033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomori, C. , Penta, B. , & Richman, R. (2022). Centering the right to health of childbearing people in the U.S. during the COVID‐19 pandemic. Frontiers of Public Health, 10. 10.3389/fpubh.2022.862454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services . (2018). 2018 national sample survey of registered nurses summary report. U.S. Department of Health and Human Services Health Resources and Services Administration Bureau of Health Workforce National Center for Health Workforce Analysis. https://bhw.hrsa.gov/sites/default/files/bureau‐health‐workforce/data‐research/nssrn‐summary‐report.pdf
- U.S. Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Professions . (2007). https://bhw.hrsa.gov/sites/default/files/bureau‐health‐workforce/data‐research/community‐health‐workforce.pdf
- Vahratian, A. , Blumberg, S. J. , Terlizzi, E. P. , & Schiller, J. S. (2021). Symptoms of anxiety or depressive disorder and use of mental health care among adults during the COVID‐19 pandemic – United States, august 2020‐February 2021. Morbidity and Mortality Weekly Report, 70(13), 490–494. 10.15585/mmwr.mm7013e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Beusekom, M. (2020) Health workers, especially minorities, at high risk for COVID, even with PPE. CIDRAP News (Center for Infectious Disease Research and policy). https://www.cidrap.umn.edu/news‐perspective/2020/08/health‐workers‐especially‐minorities‐high‐risk‐covid‐even‐ppe
- ver Hoeve, E. , Simon, M. A. , Danner, S. M. , Washington, A. J. , Coples, S. D. , Percac‐Lima, S. , Whited, E. C. , Paskett, E. D. , Naughton, M. J. , Gray, D. M. , Wenzel, J. A. , Zabora, J. R. , Hassoon, A. , Tolbert, E. E. , Calhoun, E. , Barton, D. L. , Friese, C. R. , Titler, M. G. , & Hamann, H. A. (2022). Implementing patient navigation programs: Considerations and lessons learned from the Alliance to advance patient‐centered cancer care. Cancer, 128(14), 2806–2816. 10.1002/cncr.34251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams, A. , Walsh, C. G. , & Griffith, M. L. (2021). Telehealth for endocrinology: Experience and effect on utilization in the Prepandemic era. Journal of the Endocrine Society, 5(suppl. 1), A844–A1021. 10.1016/j.eprac.2021.06.009 [DOI] [PubMed] [Google Scholar]
- Wiltz, J. L. , Feehan, A. K. , Molinari, N. M. , Ladva, C. N. , Truman, B. I. , Hall, J. , Block J. P., Rasmussen S. A., Denson J. L., Trick W. E., Weiner M. G., Koumans E., Gundlapalli A., Carton T. W., Boehmer T. K. (2022). Racial and ethnic disparities in receipt of medications for treatment of COVID‐19 – United States, March 2020‐August 2021. DHEW Publication, 71(3), 96–102. 10.15585/mmwr.mm7103e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wold, B. , & Samdal, O. (2012). An ecological perspective on health promotion systems, settings, and social processes. Bentham Books. [Google Scholar]
- World Health Organization . (2007). Everybody's business—Strengthening health systems to improve health outcomes: WHO's framework for action. World Health Organization; https://apps.who.int/iris/handle/10665/43918 [Google Scholar]
- World Health Organization (2020a). WHO Director‐General's opening remarks at the media briefing on COVID‐19 – 11. https://www.who.int/director‐general/speeches/detail/who‐director‐general‐s‐opening‐remarks‐at‐the‐media‐briefing‐on‐covid‐19‐‐‐11‐march‐2020. Accessed May 30, 2022.
- World Health Organization . (2020b). State of the world's nursing 2020: Investing in education, jobs and leadership. https://www.who.int/publications/i/item/9789240003279
- World Health Organization . (2021a). Comprehensive mental health action plan 2013‐2030. (who.int)
- World Health Organization . (2021b). The WHO global strategic directions for nursing and midwifery (2021–2025). https://www.who.int/publications/i/item/9789240033863
- World Health Organization (2022). WHO Coronavirus Dashboard. [WHO Coronavirus (COVID‐19) Dashboard|WHO Coronavirus (COVID‐19) Dashboard With Vaccination Data].
- World Health Organization (n.d.). Social determinants of health. https://www.who.int/health‐topics/universal‐health‐coverage/social‐determinants‐of‐health#tab=tab_1
- Wu, E. L. , Kumar, R. N. , Moore, W. J. , Hall, G. T. , Vysniauskaite, I. , Kim, K. A. , Angarone, M. P. , Stosor, V. , Ison, M. G. , Bba, A. F. , Achenbach, C. J. , & Gates, K. L. (2022). Disparities in COVID‐19 monoclonal antibody delivery: A retrospective cohort study. Journal of General Internal Medicine, 37(10), 2505–2513. 10.1007/s11606-022-07603-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang, T & Mason, D . (2022). COVID‐19's impact on nursing shortages, the rise of travel nurses and price gouging. Health Affairs Forefront. https://www.healthaffairs.org/do/10.1377/forefront.20220125.695159/#:~:text=In%20a%20survey%20of%20more.%E2%80%9D%20Sixty%2Dsix%20percent%20said [Google Scholar]
- Zhang, X. , Tai, D. , Pforsich, H. , & Lin, V. W. (2018). United States registered nurse workforce report card and shortage forecast: A revisit. American Journal Medical Quality, 33(3), 229–236. 10.1177/1062860617738328 [DOI] [PubMed] [Google Scholar]
- Zobeck, B. , Carson, E. , MacDowell, M. , Hunt, A. , & Reeder, A. (2021). Appointment attendance and patient perception of drive‐up INR testing in a rural anticoagulation clinic during the COVID‐19 pandemic. ACCP Journal of the American College of Clinical Pharmacy, 3(8), 1536–1537. 10.1002/jac5.1390 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study


