Abstract
Parents of children diagnosed with autism spectrum disorder (ASD) report higher levels of stress than parents of typically developing children. Few studies have examined factors associated with parental stress in early childhood. Even fewer have investigated the simultaneous influence of sociodemographic, clinical, and developmental variables on parental stress. We examined factors associated with stress in parents of young children with ASD. Multiple regression models were used to test for associations between socioeconomic indices, developmental measures, and parental stress. Externalizing behaviors, communication, and socialization skills accounted for variance in parental stress, controlling for ASD diagnosis. Results highlight the importance of interventions aimed at reducing externalizing behaviors in young children as well as addressing stress in caregivers of children with ASD.
Keywords: ASD, Parental stress, Externalizing behaviors, Early childhood
Introduction
Parents of children with autism spectrum disorder (ASD) commonly report experiencing higher levels of stress in comparison to parents of children with other neurodevelopmental disorders or children who are typically developing (Davis & Carter, 2008; DesChamps et al., 2020; Estes et al., 2013; Zablotsky et al., 2013). Broadly, factors contributing to parental stress may include child characteristics (e.g., presence of behavioral challenges; Lecavalier et al., 2006) as well as societal and sociodemographic circumstances (e.g., low income, living in a low-resource community, limited access to resources; Iadarola et al., 2019; Zablotsky et al., 2013). Higher rates of parenting stress in mothers of children with ASD have been associated with less favorable maternal mental health (Zablotsky et al., 2013), which in turn can have an impact on child mental health and behavior (Rodriguez et al., 2019).
Child Characteristics Contributing to Parental Stress
While the core symptoms of autism include deficits in social communication and restricted and repetitive behaviors and interests (American Psychiatric Association, 2013), many children with autism also display co-occurring behavioral problems, such as externalizing behaviors, including aggression, tantrums, and non-compliance (Hill et al., 2014). There is evidence that child problem behaviors in general, and externalizing behaviors in particular, predict parental stress in caregivers of children with ASD, over and above the influence of core ASD symptoms (Estes et al., 2009, 2013; Firth & Dryer, 2013; Lecavalier et al., 2006). For instance, in children with ASD between 3 and 18 years of age, externalizing behavior problems showed the largest associations with parental stress, followed by the child’s internalizing problems (Lecavalier et al., 2006). Similarly, in parents of children with ASD between 4 and 12 years of age, children’s behavioral and emotional problems—but not social impairments associated with ASD—were predictive of parental mental distress (self-reported stress, anxiety, and depression; Firth & Dryer, 2013). These findings suggest that externalizing behavior problems may be more distressing overall and may have a larger impact on parental mental health than the social deficits characteristic of ASD.
Although the implication of these findings is that the externalizing behaviors contribute to increased parental stress, the relationship between these variables may be bidirectional (Rodriguez et al., 2019; Zaidman-Zait et al., 2014). In a longitudinal study of children with ASD between 5 and 12 years of age, parenting stress both impacted, and was impacted by child behavior (Rodriguez et al., 2019). The nature and timing of these transactional relationships between parental stress and child behavioral problems depended upon the behavioral domain, with the child internalizing behaviors being driven by parental stress across middle to late childhood, while child externalizing behaviors were predicted by parenting stress early on, but also led to increased parental stress with increasing age, and especially in fathers (Rodriguez et al., 2019).
Complementary to these findings, other studies have shown associations between other characteristics associated with ASD and parental stress. Communication impairments, cognitive skills, and problems with socialization in children with ASD have all been associated with stress among caregivers (Davis & Carter, 2008). Additionally, greater ASD symptoms (Hastings & Johnson, 2001) and low levels of adaptive behavior skills (Hall & Graff, 2011) have also been linked with higher levels of parental stress.
While most studies have focused on stress in parents of school-aged children and adolescents with ASD, some have examined these relationships in early childhood (DesChamps et al., 2020; Estes et al., 2009, 2013; Zaidman-Zait et al., 2014). Investigating longitudinal trajectories of parenting stress among parents of 1.5–3.5 years old children with ASD concerns, prior to a formal diagnosis of ASD, Deschamps et al. (2020) reported higher levels of stress across six months of their child’s early development, in comparison to caregivers of children with no developmental (or non-ASD) concerns. These authors also found associations between impaired social communication and parenting stress in the sample. These findings suggest that autism-related behaviors may contribute to parenting stress even prior to a child receiving a formal diagnosis of autism. For example, ASD-associated challenges with social communication could interfere with parents’ abilities to connect with their children, in turn contributing to higher parenting stress (DesChamps et al., 2020). Critically, however, most studies in young children (DesChamps et al., 2020; Estes et al., 2009, 2013) did not include measures of externalizing behaviors, which have previously been shown to relate to stress in parents of older children with ASD, preventing direct comparisons and inferences about the effect of externalizing behaviors on parental stress in early childhood.
Sociodemographic and Societal Contributors to Parental Stress
In addition to relationships between children’s behavioral characteristics and parental stress, socioeconomic status, broadly construed, may also relate to stress in parents of children with ASD. Having a child with autism can place a heavy financial burden on parents (Bonis, 2016). Indeed, the additional healthcare and intervention costs for raising a child with ASD are estimated to be nine times higher than the costs of raising a child without ASD (Bonis, 2016; CDC, n.d.). At the same time, families of children on the autism spectrum often face lost wages and lower incomes as a result of one parent (most often, a mother) leaving the workforce in order to manage their child’s care (Bonis, 2016).
The links between socioeconomic status (SES) and developmental outcomes in autism as well as in typical development are well documented (Romeo et al., 2018). Having access to fewer resources (e.g., having low family income or of living in a low-resource neighborhood) may place additional stress on parents, which could be even more burdensome for parents of children with ASD. Indeed, mothers of children with ASD from lower-income households and mothers of Black children with ASD report higher rates of mental distress than mothers of white children from higher-resource households (Zablotsky et al., 2013). Additionally, findings from a qualitative study using focus groups with parents of children with ASD who are under-represented in ASD research (e.g., non-white, Spanish-speaking, lower income individuals, or people living in rural communities) showed several distinct sources of parental stress that may be uniquely experienced by these families, including their children’s autism-related symptoms interfering with family activities; misperceptions about ASD among family and community members; and system-level factors contributing to access to services (e.g., health insurance coverage, availability of language interpretation services in medical settings; Iadarola et al., 2019).
Low utilization of services among many families with children with ASD has been linked to public stigma associated with ASD diagnosis (Kinnear et al., 2016; Zuckerman et al., 2018) which can further compound parental stress (Bonis, 2016; Lutz et al., 2012). Indeed, because ASD is most often an “invisible disability” (i.e., it has no outwardly recognizable physical characteristics associated with it), some parents report feeling a great deal of negative criticism and stigmatization from others, with no physical characteristic to account for their child’s potentially problematic or challenging behaviors (Myers et al., 2009). Some parents report avoiding social encounters in order to prevent negative experiences with onlookers in public or at family or community events (Lutz et al., 2012). Feelings associated with isolation or shame can contribute to elevated stress levels among caregivers of individuals with ASD. Further, perceived stigma experienced by caregivers could negatively impact mental healthcare seeking (Golberstein et al., 2008), further exacerbating the already heightened parental stress in this population.
Overall, the growing literature on stress in caregivers of children with ASD provides compelling evidence for higher levels of parenting stress, associated with child’s clinical and behavioral characteristics and family’s sociodemographic and socioeconomic circumstances. However, most extant studies reporting links between parenting stress and child behavior problems in young children with ASD have not examined concurrent influence of sociodemographic factors or SES on parental stress. To our knowledge, this is the first study to examine patterns of parenting stress in caregivers of young children (i.e., 1.5–5 year-old toddlers and preschoolers) with early diagnosis of ASD, supported by gold-standard diagnostic sample characterization, allowing for measurement of simultaneous influences of behavior problems, ASD symptoms, and sociodemographic variables on parental stress.
Methods
Participants
Participants were enrolled in the ongoing longitudinal study of early brain markers of ASD. Toddlers and preschoolers with a diagnosis of ASD or behavioral concerns consistent with ASD symptoms were referred to the study from specialty autism clinics, state-funded early education and developmental evaluation programs, local pediatricians, service providers, and community clinics. Typically developing (TD) children were recruited from the community, including early head start programs, and via print and social media advertisements. Participants in either group were screened and excluded for any comorbid neurological disorders (e.g., cerebral palsy), history of perinatal Central Nervous System (CNS) infection or gross CNS injury, non-febrile seizures, and contraindications for MRI. Participants with known syndromic forms of ASD (e.g., fragile X or Rett syndrome), as ascertained from parent report, were also excluded, given the study’s focus on idiopathic ASD (i.e., with no known genetic causes). To limit known risk factors for developmental delays among children enrolled in the TD group, TD participants were also screened and excluded for prematurity (< 36 weeks of gestation), family history (in first degree relatives) of ASD, intellectual disability, or other heritable psychiatric or neurological disorders. Upon enrollment, diagnoses of ASD (also referred to as clinical best estimate [CBE] in children younger than age three; Ozonoff et al., 2015) were established in all participants in the ASD group in a specialty clinic based on the DSM-5 criteria (Diagnostic and Statistical Manual of Mental Disorders, 2013), supported by Autism Diagnostic Observation Schedule, 2nd Edition (ADOS-2; Lord et al., 2012) administered by research-reliable clinicians, the Autism Diagnostic Interview-Revised (ADI-R; Lord et al., 1994) administered to caregivers of children older than 36 months, and expert clinical judgment. Informed written consent was obtained from caregivers under protocols approved by the Institutional Review Board. This report includes cross-sectional data from 42 children with ASD (12 females) and 36 TD children (19 females; see Table 1 for participant characteristics).
Table 1.
Participant characteristics
| ASD (n = 42) |
TD (n = 36) |
p value | |||
|---|---|---|---|---|---|
| Mean ± SD | Range | Mean ± SD | Range | ||
|
| |||||
| Age (months) | 31.9 ± 12.2 | 17–67 | 27.6 ± 13.8 | 15–64 | 0.18 |
| % Femalea | 25% | 52% | 0.01 | ||
| % Hispanica | 43% | 18% | 0.02 | ||
| % Mothers with college educationa | 47% | 79% | 0.001 | ||
| Income-to-needs ratio | 4.6 ± 2.6 | 0.2–9.4 | 4.5 ± 3.2 | 0.3–9.3 | 0.15 |
| MSEL ELC | 73.6 ± 18.0 | 49–107 | 105.4 ± 16.2 | 80–143 | < 0.001 |
| SCQ total | 16.0 ± 7.5 | 3–35 | 4.5 ± 3.2 | 0–11 | < 0.001 |
| ADOS-2 total | 15.9 ± 5.5 | 6–22 | – | – | – |
Income-to-Needs Ratio (INR) was derived by dividing the household income by the federal poverty threshold defined by family size; an INR of one indicates living at the federal poverty line, which according to the 2019 US government official poverty definition was $25,750/year for a family of four
MSEL Mullen Early Learning Scale ELC Early Learning Composite, Standard Score SCQ Social Communication Scale ADOS-2 Autism Diagnostic Observation Schedule, 2nd Edition
Values denote counts and corresponding χ2 p values. Remaining comparisons reflect two-sample t tests and corresponding p values
Measures
Parental Stress
Parental stress was assessed with the Parenting Stress Index, 4th Edition (PSI-4; Abidin, 2012), a 120-item self-report scale designed to measure stress experienced by parents of children between the ages of one month and twelve years, including specific aspects of parental stress arising from the child’s behavior, from within the parent, and from the parent–child relationship. Parents rate their agreement with statements on a 5-point Likert scale ranging from “strongly disagree’” to “strongly agree”. The PSI-4 yields three overarching scores indexing stress related to Child- and Parent-characteristics, and the overall parental experience of stress (Total Stress). The Child Domain includes six subscales summarizing sources of stress related to child mood, demandingness, acceptability (or extent to which child’s characteristics meet parental expectations), adaptability, distractibility/hyperactivity, and the extent to which the parent experiences interactions with the child as reinforcing. The Parent Domain measures seven sources of stress related to parent characteristics, including competence, parents’ sense of role restriction and constrained personal identity, perceived emotional and physical support from the spouse or parenting partner, affective status, isolation and social support, sense of attachment to the child, and overall health.
Child Developmental and Behavioral Measures
All children were administered the Mullen Scales of Early Learning (MSEL; Mullen, 1995), a clinician-administered assessment of language, cognitive, and motor development, which yields age-corrected standardized scores. The Vineland Adaptive Behavior Scales, 2nd Edition, Survey Interview (Sparrow et al., 2005), a semi-standardized interview yielding age-normed standard scores, was administered to caregivers to assess the child’s adaptive communication, daily living, social, and motor skills. Caregivers also completed the Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2000) for ages 1.5–5 years (CBCL 1½–5), a measure designed to assess broadband behavioral and emotional problems, and the Social Communication Questionnaire, Current (SCQ; Rutter et al., 2003) a screener for social delays associated with ASD administered primarily to rule out ASD-like symptoms in TD children. All TD participants’ scores on the CBCL Total Problems, Internalizing Problems, and Externalizing Problems subscales fell within the normal range (all T scores < 63), and no TD participants exceeded the SCQ cut-off score of 15 (all scores < 11).
Socioeconomic and Sociodemographic Variables
Household-level SES was assessed based on the demographic information provided by caregivers, including household income, number of individuals in the household, and highest level of education attained by either parent. Gross annual income was reported on a following scale: < $10,000, $10,001–20,000, $20,001–30,000, $30,001–40,000, $40,001–50,000, $50,001–60,000, $60,001–80,000, $80,001–100,000, $100,001–150,000, $150,001–200,000, $200,001–250,000 and > $251,000. Income measurements were converted to income-to-needs ratio (INR) to account for family size (INR was derived by dividing the household income by the federal poverty threshold defined by family size; an INR of one indicates living at the federal poverty line, which according to the 2019 US government official poverty definition was $25,750 per year for a family of four). Maternal education was rated on a six-point scale: less than high school, completed high school, vocational or technical school, some college, completed college, professional or doctoral training beyond college.
Analytic Strategy
Independent sample t tests were used to examine group differences (ASD v. TD) in parental stress. Pearson’s correlations and multiple regression models were used to examine relationships among clinical, developmental, and demographic variables and parental stress (child- and parent-related parental stress). The effects of covariates (age, gender, ethnicity: Hispanic vs. Non-Hispanic, and number of children in the household) were also examined and retained in regression models when significantly associated with parental stress outcome variables. Regression model specification was achieved by first including all variables that showed significant bivariate associations with parental stress (child- and parent-related parental stress, respectively) as explanatory variables, and then iteratively removing from the models those variables that were not significant predictors of parental stress when controlling for the influence of other variables. Finally, given some previous findings suggesting that parental reporting of stress may differ between mothers and fathers (Davis & Carter, 2008), all analyses were also conducted with a subset of the dataset that excluded parent-report measures provided by fathers (n = 13). Results from the mothers-only subset were nearly identical to those from the full sample (i.e., yielded no differences in statistical inference), and thus all subsequent analyses are reported on the full sample.
Results
Diagnostic Group Differences in Parental Stress
Parents of young children with ASD reported significantly higher levels of child-related stress than parents of TD children (t(76) = − 8.0, Cohen’s d = − 2.0, p < 0.001; see Fig. 1a). Parents of children with ASD also reported higher levels of parent-related stress, although the effect of diagnosis on parent-related stress was considerably smaller than that on child-related stress, while still relatively substantial (t(76) = − 2.0, Cohen’s d = − 0.6, p = 0.02; see Fig. 1b).
Fig. 1.
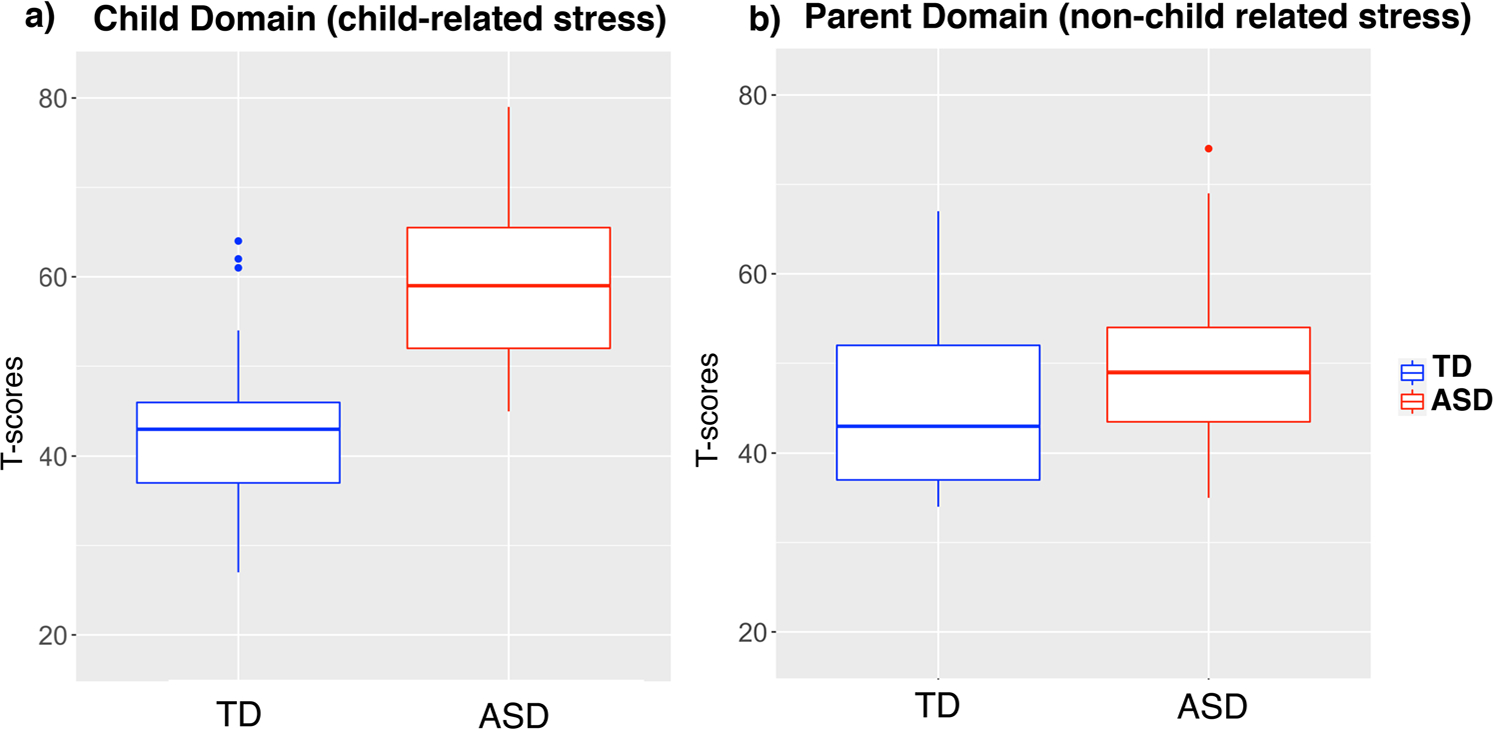
Boxplots displaying PSI Child (a) and Parent (b) domain T scores by diagnostic group. a t = − 8.0, p < 0.001, b t = − 2.0, p < 0.02
Bivariate Correlations Between Clinical and Developmental Variables and Parental Stress
Relationships between parental stress indices and clinical, developmental, and demographic variables were first examined with zero-order correlational analyses conducted separately in each diagnostic group, as summarized in Fig. 2. The results revealed that, in the ASD group, child-related parental stress (PSI-4 Child Domain T score) was significantly associated with parent-rated externalizing behavior problems (r = 0.72), oppositional behavior, ADHD-related and ASD-related behaviors as measured with CBCL, social communication deficits (SCQ Total score), communication skills measured with Vineland, as well as non-child-related stress indexed with the PSI-4 Parent Domain (all rs >|0.38|, all ps < 0.009; see Fig. 2a). For parents of TD children, child-related stress was associated with similar CBCL indices, including externalizing behaviors (r = 0.66), oppositional behaviors, ADHD-related behavior, and behaviors associated with ASD, as well as communications and socialization skills measured with Vineland (all rs >|0.36|, all ps < 0.003; see Fig. 2b).
Fig. 2.
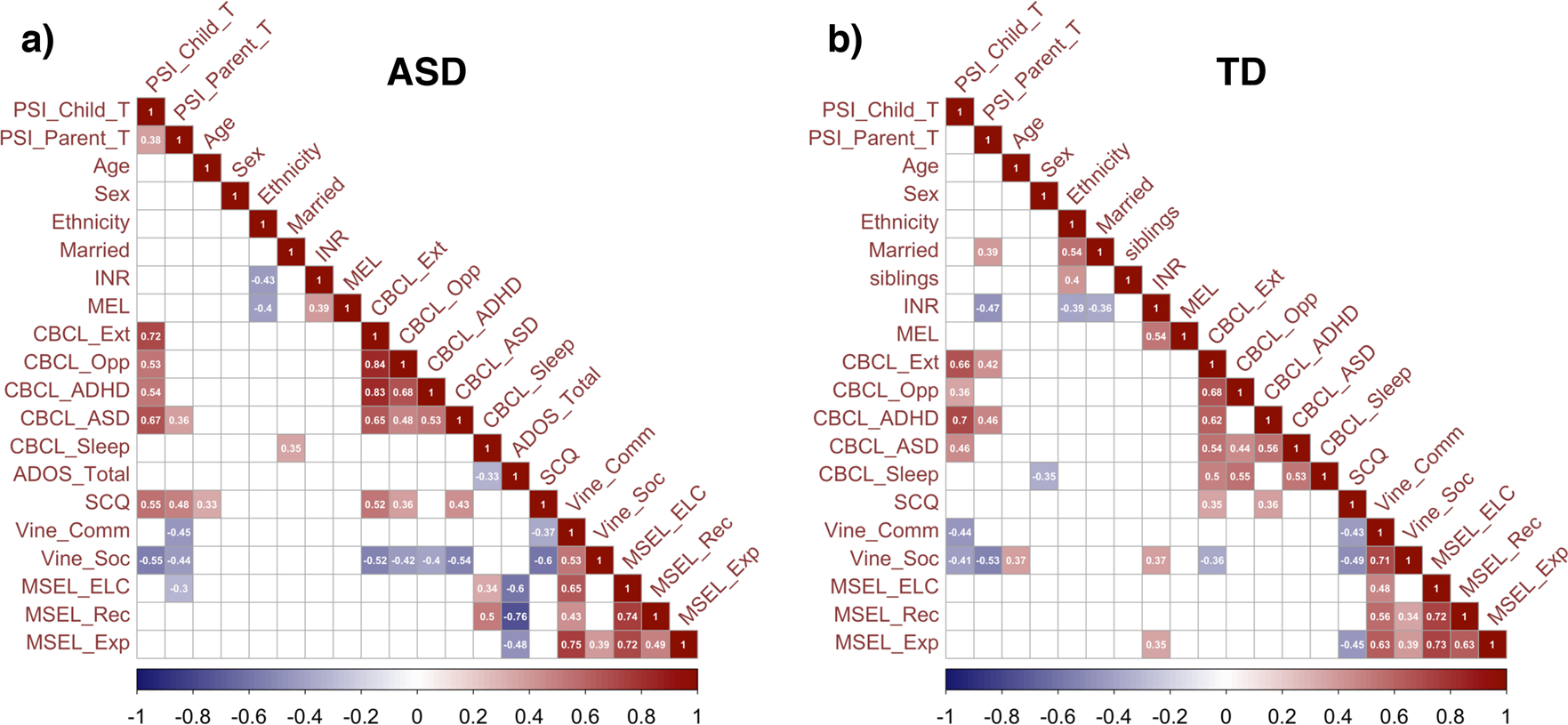
Correlation heat maps. Bivariate Pearson’s correlations between the PSI-4 Child and Parent domain scores and developmental, clinical, and demographic variables in a participants with ASD and b TDparticipants. Only significant correlations (at p < 0.05, uncorrected) are displayed in color. INR income-to-needs ratio, MEL maternal education level, CBCL Ext externalizing problems, CBCL Opp oppositional defiance, Vine Comm Vineland Communica-tion, Vine Soc Vineland Socialization, MSEL ELC Mullen Scales of Early Learning, Early Learning Composite score, MSEL Rec receptive language, MSEL Exp expressive language. Higher scores on ADOS, CBCL, and SCQ represent greater ASD symptoms and behavioral problems, while higher scores on Vineland and MSEL represent greater or more advanced developmental skills. Higher T scores on PSI-4 represent greater levels of stress
Notably, non-child related parental stress, indexed with the PSI-4 Parent Domain score, was also associated with child developmental variables. Namely, in parents of children with ASD, non-child related parental stress was associated with parent-rated autism symptoms (CBCL ASD-related behaviors), parent-rated communication and socialization skills (SCQ, Vineland Communication and Socialization), and overall developmental skills (MSEL Early Learning Composite; all rs >|0.3|, all ps < 0.04; see Fig. 2a), with higher skills and lower symptoms associated with lower levels of stress. In the TD group, non-child related parental stress was significantly associated with income-to-needs ratio, and parent-rated externalizing, oppositional, ADHD, and ASD-related behaviors as measured with CBCL, as well as with marital status, with single parents reporting higher levels of stress (all rs >|0.39|, all ps < 0.02; see Fig. 2b).
Child and SES Predictors of Parental Stress
Given the observed bivariate associations between clinical and developmental measures, and parent- and child-related parental stress, we used multiple regression models to examine unique variance in parental stress associated with each predictor variable, considering all the variables together. For a summary of all explanatory variables tested in multiple regression models at the model specification stage, see Table S1. Because none of the relevant covariates (e.g., age, ethnicity, number of children in the home) were significantly associated with parent- or child-related stress, they were removed from the final regression models. For child-related parental stress, externalizing behavior problems emerged as the strongest predictor (t = 8.02, r2 = 0.50, p < 0.001), controlling for the significant associations of ASD diagnosis (t = 2.33, r2 = 0.07, p = 0.02) and parent-rated communication skills (t = − 2.75, r2 = 0.09, p = 0.007; see Table 2; Fig. 3a, b). Overall, greater externalizing behavior problems, diagnosis of ASD, and lower communication skills, all significantly predicted higher levels of child-related stress. For non-child-related stress, lower socialization skills (as perceived by parents) were significantly associated with greater parent-related stress (Vineland Socialization t = − 3.98, r2 = 0.19, p = 0.0001; see Table 2; Fig. 3c). Further, there was a significant diagnosis by income-to-needs ratio interaction effect on non-child-related stress, such that higher income-to-needs ratio was associated with lower parental stress in the TD group, but not for parents of children with ASD (t = 2.74, r2 = 0.09, p = 0.01; see Table 2; Fig. 3d).
Table 2.
Summary of final regression models of demographic and behavioral predictors of child-related and non-child related parental stress
| Estimated parameters | PSI child domain (child-related stress) | PSI parent domain (non-child-related stress) |
|---|---|---|
| β (standard error) | β (standard error) | |
|
| ||
| Intercept | 34.8 (6.0) | 77.75 (7.16) |
| Diagnosis | 4.5 (1.9) | −8.45 (3.3) |
| CBCL externalizing behavior | 0.47 (0.05) | – |
| Vineland communication | −0.12 (0.04) | – |
| Vineland socialization | – | −0.30 (0.1) |
| INR (income to needs ratio) | – | −1.01 (0.5) |
| INR × diagnosis interaction | – | 1.79 (0.7) |
| Overall model fit (F, R2, p value) | 78.0, 0.76, p < 0.0001 | 9.28, 0.36, p < 0.0001 |
Fig. 3.
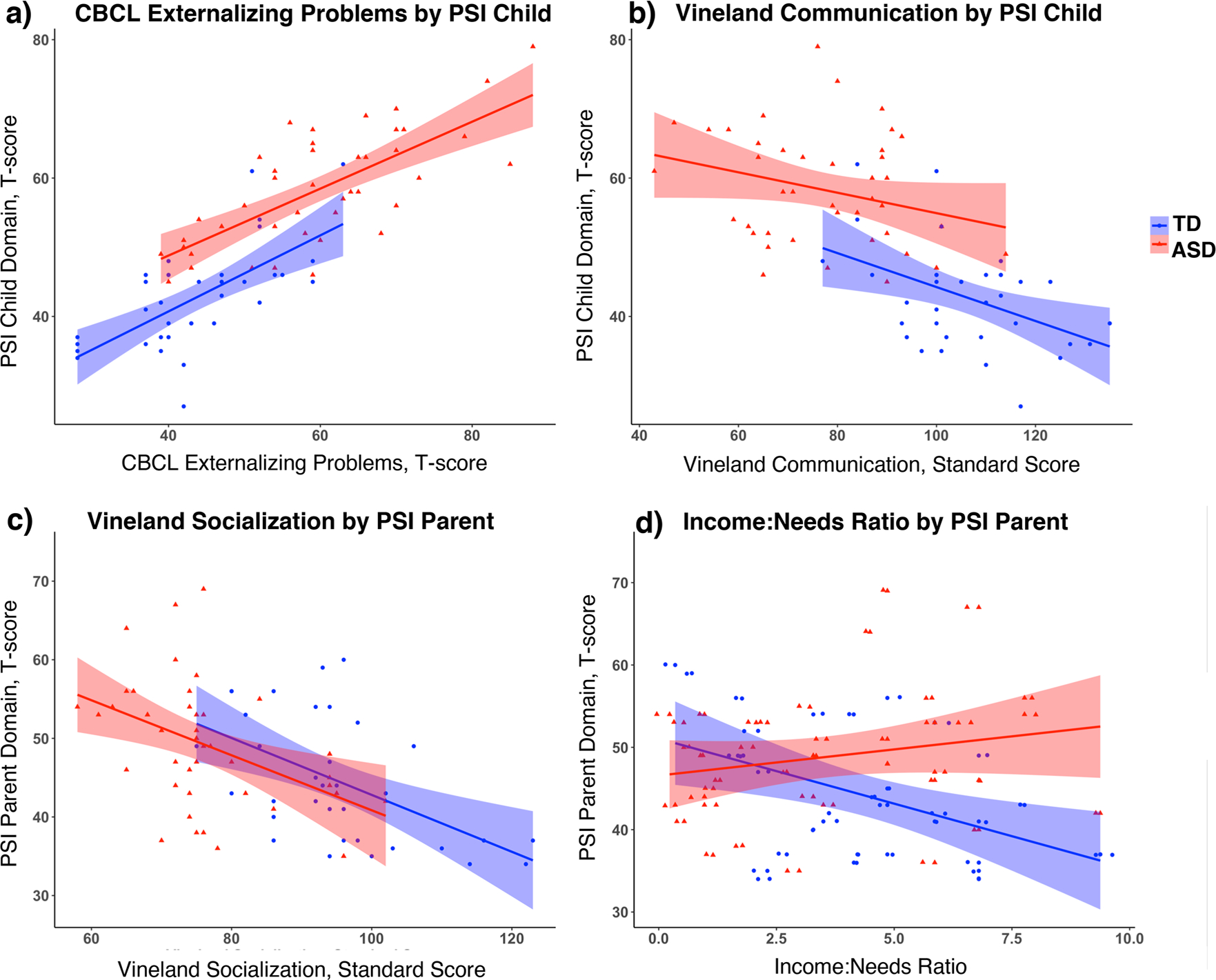
a, b Scatterplots depicting significant associations between PSI-Child domain T scores and scores on a parent-rated externalizing behaviors (CBCL) and b parent-rated communication skills (Vineland). Associations were significant when controlling for one another and for the effect of diagnosis on child-relatedstress. c, d Scatterplots depicting significant associations between PSI-Parent domain T scores and c parent-rated socialization skills (Vineland) and d income-to-needs ratio by diagnosis interaction. Associations were significant when controlling for one another and for the effect of diagnosis
Two Subgroups Determined by the Profiles of Parental Stress
Given that child developmental and clinical characteristics predicted both child-related and non-child related parental stress, we applied k-means clustering to further explore patterns of parent-related stress. Fourteen PSI child- and parental-stress subscale scores for all (TD and ASD) children were submitted to k-means clustering using a squared Euclidean distance measure. The elbow method suggested that the two-cluster solution provided the best fit for the data (both three- and four-cluster solutions yielded a cluster with size n = 2; see Supplemental Fig. 1). The two resulting clusters were compared on their values of each PSI subscale, as well as on the proportion of children with ASD and overall PSI Child- and Parent-Domain scores (see Fig. 4). Cluster 1 (n = 44) was characterized by lower levels of both child- and parent-related stress and included a higher proportion of TD children (nTD = 31, nASD = 13; see Fig. 4). Cluster 2 (n = 39) was characterized by higher levels of both parent- and child-related stress and a higher proportion of children with ASD (nTD = 5, nASD = 34; see Fig. 4). Although Cluster 2 showed significantly higher levels of stress in both child- and non-child domains (Fig. 4c), the difference between the two clusters was particularly large in the child domain (Child Domain: t(76) = − 12, Cohen’s d = − 3, p < 0.001; Parent Domain: t(76) = − 7, Cohen’s d = − 1, p < 0.001).
Fig. 4.
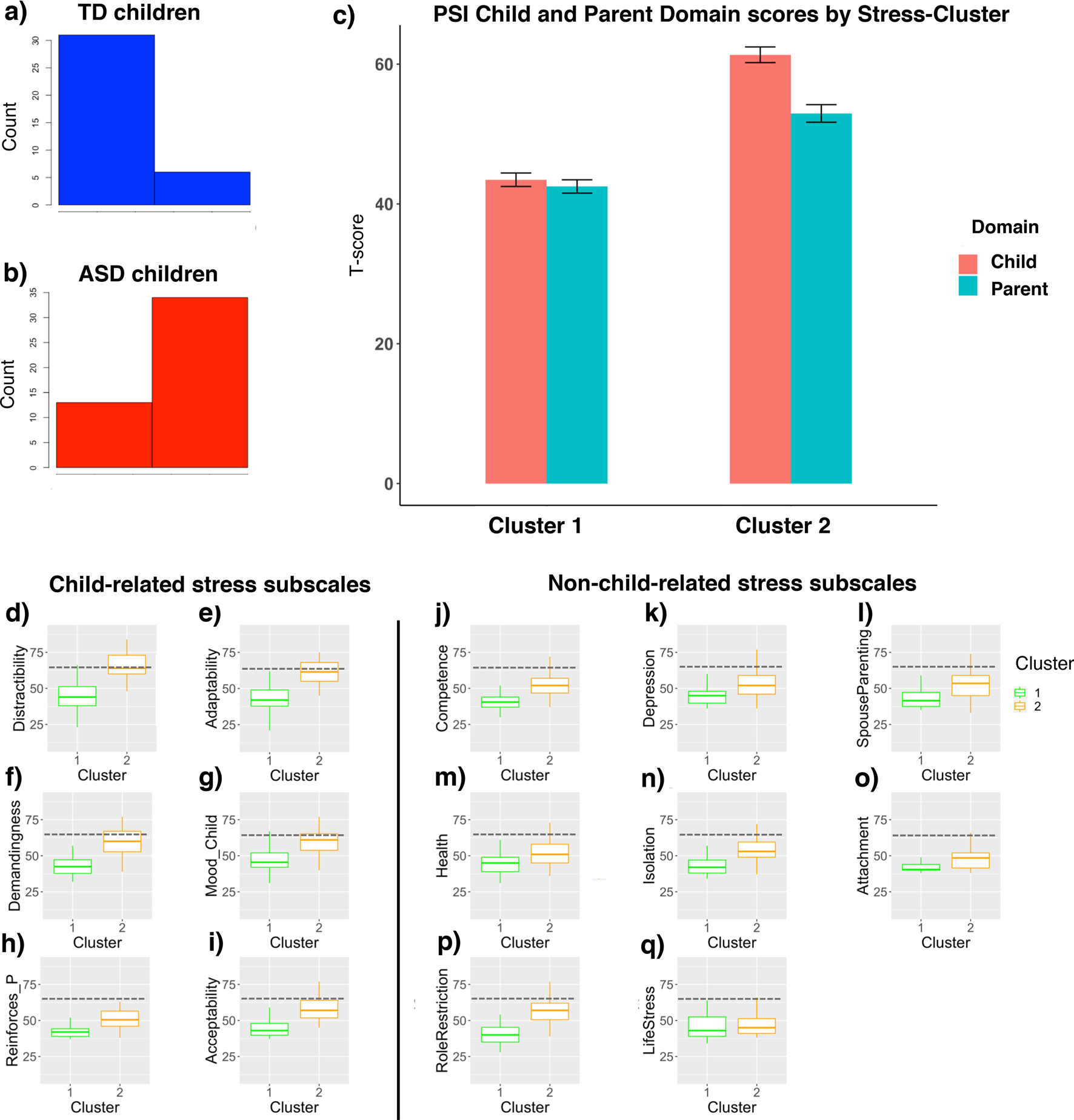
a, b Parental stress cluster membership in a TD children and b children with ASD. c Bar plots depicting PSI Child and Parent domain T scores (y-axis) by Stress Cluster (x-axis) with standard error bars. d–i Boxplots displaying scores for each PSI child-related subscale, in each cluster. j–q Boxplots displaying scores for each PSI parent-related subscale, in each cluster. Child-related stress subscales include: child’s d distractibility/hyperactivity, e adaptability, f demandingness, g child mood, h the extent to which the parent experiences interactions with the child as reinforcing, and i the extent to which child’s characteristics meet parental expectations (acceptability). Non-child-related stress subscales include: parent’s sense of j competence, k parent’s affective status, l perceived emotional and physical support from the parenting partner, m parent’s overall health, n sense of isolation and social support, o sense of attachment to the child, p sense of role restriction and constrained personal identity, and q overall life stress. For d–q, dashed lines indicate clinically significant threshold (at 90th percentile)
Point-biserial correlations were conducted to examine associations between cluster membership and clinical, developmental, and demographic variables in the ASD group only (as there were only 5 TD participants in cluster 2). Cluster membership was significantly correlated with externalizing, oppositional, ADHD, and ASD-related behaviors on the CBCL (all rs > 0.32, all ps < 0.03), such that membership in Cluster 2 (representing higher levels of parental stress) was associated with higher levels of reported behavioral problems in these domains. Cluster 2 was also associated with higher impairments in parent-rated communication skills measured with both SCQ (r = 0.40, p = 0.009) and Vineland Communication (r = − 0.34, p = 0.02). When the effects of developmental and clinical variables on cluster membership in the ASD group were considered simultaneously, using logistic regression, externalizing behaviors were the only significant explanatory variable in the logistic regression model (CBCL Externalizing z-score = 2.65, p = 0.007).
Discussion
We examined associations between developmental, clinical, and sociodemographic variables and parental stress in parents of young children with and without autism spectrum disorders. We found that parents of children with early diagnosis of ASD report higher levels of stress than parents of typically developing children of the same age. However, controlling for ASD diagnosis, externalizing behavior problems were even more strongly associated with child-related parental stress than diagnosis, with higher levels of externalizing behaviors associated with higher levels of stress. Additionally, parent-rated child’s communication and socialization skills were also associated with parental stress. In parents of typically developing young children, but not of those with ASD, income-to-needs ratio was negatively associated with non-child related stress. Finally, when all children in the sample (those with a diagnosis of ASD and TD children) were considered together, a clustering analysis of parental stress profiles revealed two subgroups: one with the preponderance of parents of TD children who reported lower levels of stress, and the other one consisting of mostly of parents of children with ASD who reported higher levels of stress, with the externalizing behaviors again emerging as the strongest predictor of membership in the higher-stress cluster.
Our study adds to the growing literature demonstrating associations between child externalizing behavior problems and parental stress in caregivers of young children with early diagnosis of ASD. These findings highlight the need to address stress in parents and caregivers of young children with autism, and to target externalizing behavior problems in early intervention for ASD, especially given the remarkable continuity of externalizing behavior problems across childhood (Campbell, 2002).
These results align well with those from previous studies in older, school-age children with ASD demonstrating strong associations between externalizing behavior problems and parental stress (e.g., Firth & Dryer, 2013; Lecavalier et al., 2006). Notably, the links between externalizing behavior in early childhood and parental stress have been also documented in caregivers of children without ASD (McKee et al., 2008; Morgan et al., 2002; Williford et al., 2007). Although with these cross-sectional data we were unable to examine the directionality of the relationship between externalizing behaviors and parental stress, previous findings in children and adolescents with and without ASD indicate that this relationship may be bidirectional (Neece et al., 2012; Rodriguez et al., 2019; Woodman et al., 2015). Our findings may, thus, represent the earliest phases of the cascading transactional process that unfolds between parents and their children, highlighting an important window for early intervention.
We also observed associations between early socialization and communication skills and parental stress. These results are also consistent with reports by others (DesChamps et al., 2020; Firth & Dryer, 2013), and suggest that ASD-related social communication deficits may contribute to parental stress, perhaps by impacting parents’ sense of connectedness to their children. Surprisingly, however, parent-rated socialization skills were associated with parent-related stress, but not child-related stress (when controlling for the diagnosis by income-to-needs ratio interaction, and simple main effects of each of these variables). One possible explanation for this counterintuitive finding is that parent’s concern for their children’s development carries over into parental experience of stress in other areas of life. Alternatively, it is possible that higher levels of parental stress contribute to over-endorsing response biases on parent-report measures and developmental interviews (Stokes et al., 2011), such that parents experiencing more stress may report higher levels of deficits or problems for their children. The latter would indicate the need to control for parental stress in analyses using parent-report measures of child development. Not-withstanding, child social communication behaviors appear to be significant predictors of parenting stress among all parents, regardless of their child’s diagnosis.
Remarkably, lower income was associated with higher levels of stress only among parents of typically developing children. Although this finding is well in line with a robust body of evidence on links between income and parental stress (e.g., Gupta, 2007; Hurt & Betancourt, 2017; Neppl et al., 2016; Santiago et al., 2011), this association did not emerge in the ASD group. One possibility accounting for the lack of observed association between income and parental stress in the ASD group is that the stressors associated with raising a child with ASD may outweigh those associated with having limited economic resources. Further, it is possible that the relatively young age of the participants studied may have impacted the extent to which parents of children with ASD experienced finance-related stress, as the cumulative cost of services and potential loss of income due to disrupted routines increases over time for these families (Cidav et al., 2012).
Notably, results did not differ when conducting analyses using a subset of the data provided by mothers only (vs. the full dataset where information was provided by mothers or fathers). Although discussed heretofore as ‘parental stress,’ it is important to note that these results have been obtained primarily from mothers, and reflect stress experienced mainly by mothers. Previous work suggests that parental reporting of stress may differ between mothers and fathers (Davis & Carter, 2008; Moes et al., 1992). Findings suggest that mothers of children with ASD experience higher levels of stress than fathers (Moes et al., 1992), perhaps due to the higher responsibility mothers have taken on in raising children. However, others have shown that mothers and fathers report comparable levels of stress (Hastings et al., 2005), but may experience stress based on different aspects of their children’s development (Davis & Carter, 2008). Finally, although not directly measured or examined in the present study, stigma associated with ASD diagnosis may also contribute to parental stress (Kinnear et al., 2016). Research and programs aimed to reduce the stigma associated with ASD diagnosis may also subsequently help reduce parental stress in this population.
Findings from the present study need to be interpreted in the context of several limitations. Due to the lack of longitudinal data, we were unable to test directional hypotheses regarding relationships between developmental and clinical variables and parental stress, although previous work has shown that relationships between these variables are bidirectional (e.g., Rodriguez et al., 2019). Future work should aim to examine these associations longitudinally beginning in very early childhood (or even infancy) to contribute knowledge on how these constructs interact over time. Additionally, the lack of data on parent characteristics in our study (e.g., parental mental health, parenting style) has further limited the inferences regarding what gives rise to associations between child behavior and parental stress. Although we had limited data regarding caregiver characteristics, those who participated in our study represented a broad range of the socioeconomic strata (see Table 1) and were recruited through diverse avenues, including direct referrals from specialty autism clinics, state-funded early education and developmental evaluation programs, autism service providers, community clinics, and via print, digital, and social media advertisements.
Further, the majority of the relationships between parental stress and child characteristics were observed for measures relying on parent report (vs. those derived from clinician observation or objective performance-based testing, such as autism symptoms measured with ADOS-2 or early learning abilities measured with Mullen Scales of Early Learning, all of which were available and included in our analyses). Although parents provide invaluable information on their children’s development and behavior in home, parent-report measures are not immune to biases that are present in any type of self-report measure (Gough & Madill, 2012). Additionally, self-report data may be less valid among people from lower SES backgrounds (Lee et al., 2016). Therefore, we cannot completely rule out confounding effects of parental reporting style as it relates to observed associations between parental stress and parent-reported child behaviors. Given that parental stress may relate to reporting style regarding child development, we recommend that researchers control for the impact of parental stress when using parent-report measures in developmental studies. Families who sought participation in a research study on child development and autism may show different response patterns than caregivers who are reluctant to seek medical diagnoses or other services for their children. Because our participants self-selected into this research study, our findings may not generalize to caregivers who do not seek diagnosis or services. Finally, the generalizability of the study findings may be limited by a relatively modest sample size.
Overall, these results show that child externalizing behavior problems account for the largest proportion of variance in parental stress in young children with and without ASD, when controlling for the significant effect of ASD diagnosis on parental stress. These findings highlight the need to address stress in caregivers of very young children with ASD, and to target externalizing behavior problems in this population in particular.
Supplementary Material
Funding
This work was supported by Grants from the National Institutes of Health (R01 MH107802 to I. Fishman) and Autism Speaks (predoctoral fellowship to L. Olson)
Footnotes
Declarations
Conflict of interest The authors declared that they have no conflicts of interest.
Supplementary Information The online version contains supplementary material available at https://doi.org/10.1007/s10803-021-04995-w.
References
- Abidin RR (2012). Parenting stress index, fourth edition (PSI-4). Lutz, Fl: Psychological Assessment Resources. [Google Scholar]
- Achenbach T, & Rescorla L (2000). Child behavior checklist. Retrieved from https://books.google.com/books?hl=en&lr=&id=YxCXh5ZvTksC&oi=fnd&pg=PA372&dq=child+behavior+checklist&ots=uGdWaO_eYv&sig=vfDaj5C2N4v19lKIsWvQJsYISYY
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders. (5th ed.). American Psychiatric Association. [Google Scholar]
- Bonis S (2016). Stress and parents of children with autism: A review of literature. Issues in Mental Health Nursing, 37(3), 153–163. 10.3109/01612840.2015.1116030. [DOI] [PubMed] [Google Scholar]
- Campbell S. (Ed.). (2002). Behavior problems in preschool children: Clinical and developmental issues- PsycNET. (2nd ed.). Guilford Press. [Google Scholar]
- Cidav Z, Marcus SC, & Mandell DS (2012). Implications of childhood autism for parental employment and earnings. Pediatrics, 129(4), 617–623. 10.1542/peds.2011-2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Data & Statistics on Autism Spectrum Disorder | CDC. (n.d.). Retrieved August 17, 2020, from https://www.cdc.gov/NCBDDD/autism/data.html
- Davis NO, & Carter AS (2008). Parenting stress in mothers and fathers of toddlers with autism spectrum disorders: Associations with child characteristics. Journal of Autism and Developmental Disorders, 38(7), 1278–1291. 10.1007/s10803-007-0512-z. [DOI] [PubMed] [Google Scholar]
- DesChamps TD, Ibañez LV, Edmunds SR, Dick CC, & Stone WL (2020). Parenting stress in caregivers of young children with ASD concerns prior to a formal diagnosis. Autism Research, 13(1), 82–92. 10.1002/aur.2213. [DOI] [PubMed] [Google Scholar]
- Estes A, Munson J, Dawson G, Koehler E, Zhou XH, & Abbott R (2009). Parenting stress and psychological functioning among mothers of preschool children with autism and developmental delay. Autism, 13(4), 375–387. 10.1177/136236130905658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estes A, Olson E, Sullivan K, Greenson J, Winter J, Dawson G, & Munson J (2013). Parenting-related stress and psychological distress in mothers of toddlers with autism spectrum disorders. Brain and Development, 35(2), 133–138. 10.1016/j.braindev.2012.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Firth I, & Dryer R (2013). The predictors of distress in parents of children with autism spectrum disorder. Journal of Intellectual and Developmental Disability, 38(2), 163–171. 10.3109/13668250.2013.773964. [DOI] [PubMed] [Google Scholar]
- Golberstein E, Eisenberg D, & Gollust SE (2008). Perceived stigma and mental health care seeking. Psychiatric Services, 59(4), 392–399. 10.1176/ps.2008.59.4.392. [DOI] [PubMed] [Google Scholar]
- Gough B, & Madill A (2012). Subjectivity in psychological science: From problem to prospect. Psychological Methods, 17(3), 374–384. 10.1037/a0029313. [DOI] [PubMed] [Google Scholar]
- Gupta VB (2007). Comparison of parenting stress in different developmental disabilities. Journal of Developmental and Physical Disabilities, 19(4), 417–425. 10.1007/s10882-007-9060-x. [DOI] [Google Scholar]
- Hall HR, & Graff JC (2011). The relationships among adaptive behaviors of children with autism, family support, parenting stress, and coping. Comprehensive Child and Adolescent Nursing, 34(1), 4–25. 10.3109/01460862.2011.555270. [DOI] [PubMed] [Google Scholar]
- Hastings RP, & Johnson E (2001). Stress in UK families conducting intensive home-based behavioral intervention for their young child with autism. Journal of Autism and Developmental Disorders, 31(3), 327–336. 10.1023/A:1010799320795. [DOI] [PubMed] [Google Scholar]
- Hastings RP, Kovshoff H, Ward NJ, Degli Espinosa F, Brown T, & Remington B (2005). Systems analysis of stress and positive perceptions in mothers and fathers of pre-school children with autism. Journal of Autism and Developmental Disorders, 35(5), 635–644. 10.1007/s10803-005-0007-8. [DOI] [PubMed] [Google Scholar]
- Hill AP, Zuckerman KE, Hagen AD, Kriz DJ, Duvall SW, Van Santen J, & Fombonne E (2014). Aggressive behavior problems in children with autism spectrum disorders: Prevalence and correlates in a large clinical sample. Research in Autism Spectrum Disorders, 8(9), 1121–1133. 10.1016/j.rasd.2014.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurt H, & Betancourt LM (2017). Turning 1 year of age in a low socioeconomic environment: A portrait of disadvantage. Journal of Developmental and BehavioralPediatrics, 38(7), 493–500. 10.1097/DBP.0000000000000469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iadarola S, Pérez-Ramos J, Smith T, & Dozier A (2019). Understanding stress in parents of children with autism spectrum disorder: A focus on under-represented families. International Journal of Developmental Disabilities, 65(1), 20–30. 10.1080/20473869.2017.1347228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinnear SH, Link BG, Ballan MS, & Fischbach RL (2016). Understanding the experience of stigma for parents of children with autism spectrum disorder and the role stigma plays in families’ lives. Journal of Autism and Developmental Disorders, 46(3), 942–953. 10.1007/s10803-015-2637-9. [DOI] [PubMed] [Google Scholar]
- Lecavalier L, Leone S, & Wiltz J (2006). The impact of behaviour problems on caregiver stress in young people with autism spectrum disorders. Journal of Intellectual Disability Research, 50(3), 172–183. 10.1111/j.1365-2788.2005.00732.x. [DOI] [PubMed] [Google Scholar]
- Lee SJ, Gopalan G, & Harrington D (2016). Validation of the parenting stress index-short form with minority caregivers. Research on Social Work Practice, 26(4), 429–440. 10.1177/1049731514554854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord C, Rutter M, Dilavore P, Risi S, Gotham K, & Bishop S (2012). Autism Diagnostic Observation Schedule, Second Edition (ADOS-2) Manual (Part I): Modules 1–4. Western Psychological Services. [Google Scholar]
- Lord C, Rutter M, & Le Couteur A (1994). Autism Diagnostic Interview-Revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders, 24(5), 659–685. [DOI] [PubMed] [Google Scholar]
- Lutz HR, Patterson BJ, & Klein J (2012). Coping with autism: A journey toward adaptation. Journal of Pediatric Nursing, 27(3), 206–213. 10.1016/j.pedn.2011.03.013. [DOI] [PubMed] [Google Scholar]
- McKee L, Colletti C, Rakow A, Jones DJ, & Forehand R (2008). Parenting and child externalizing behaviors: Are the associations specific or diffuse? Aggression and Violent Behavior. 10.1016/j.avb.2008.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moes D, Koegel RL, Schreibman L, & Loos LM (1992). Stress profiles for mothers and fathers of children with autism. Psychological Reports, 71(3 Pt 2), 1272–1274. 10.2466/pr0.1992.71.3f.1272. [DOI] [PubMed] [Google Scholar]
- Morgan J, Robinson D, & Aldridge J (2002). Parenting stress and externalizing child behaviour. Child and Family Social Work, 7(3), 219–225. 10.1046/j.1365-2206.2002.00242.x. [DOI] [Google Scholar]
- Mullen E (1995). Mullen Scales of Early Learning Manual. American Guidance Service. Circle Pines, MN. Retrieved from https://books.google.com/books/about/Mullen_Scales_of_Early_Learning_Manual.html?id=ZYYQAQAAMAAJ [Google Scholar]
- Myers BJ, Mackintosh VH, & Goin-Kochel RP (2009). “My greatest joy and my greatest heart ache:” Parents’ own words on how having a child in the autism spectrum has affected their lives and their families’ lives. Research in Autism Spectrum Disorders, 3(3), 670–684. 10.1016/j.rasd.2009.01.004. [DOI] [Google Scholar]
- Neece CL, Green SA, & Baker BL (2012). Parenting stress and child behavior problems: A transactional relationship across time. American Journal on Intellectual and Developmental Disabilities, 117(1), 48–66. 10.1352/1944-7558-117.1.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neppl TK, Senia JM, & Donnellan MB (2016). Effects of economic hardship: Testing the family stress model over time. Journal of Family Psychology, 30(1), 12–21. 10.1037/fam0000168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozonoff S, Young GS, Landa RJ, Brian J, Bryson S, Charman T, Chawarska K, Macari SL, Messinger D, Stone WL, & Zwaigenbaum L (2015). Diagnostic stability in young children at risk for autism spectrum disorder: A baby siblings research consortium study. Journal of Child Psychology and Psychiatry, 56(9), 988–998. 10.1111/jcpp.12421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez G, Hartley SL, & Bolt D (2019). Transactional relations between parenting stress and child autism symptoms and behavior problems. Journal of Autism and Developmental Disorders, 49(5), 1887–1898. 10.1007/s10803-018-3845-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romeo RR, Leonard JA, Robinson ST, West MR, Mackey AP, Rowe ML, & Gabrieli JDE (2018). Beyond the 30-million-word gap: Children’s conversational exposure is associated with language-related brain function. Psychological Science, 29(5), 700–710. 10.1177/0956797617742725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter M, Bailey A, & Lord C (2003). Social Communication Questionnaire (SCQ). Western Psychological Services. Retrieved from https://www.wpspublish.com/scq-social-communication-questionnaire [Google Scholar]
- Santiago CDC, Wadsworth ME, & Stump J (2011). Socioeconomic status, neighborhood disadvantage, and poverty-related stress: Prospective effects on psychological syndromes among diverse low-income families. Journal of Economic Psychology, 32(2), 218–230. 10.1016/j.joep.2009.10.008. [DOI] [Google Scholar]
- Sparrow S, Cicchetti D, & Balla D (2005). Vineland adaptive behavior scales. (2nd ed.). Pearson Clinical. [Google Scholar]
- Stokes J, Pogge D, Wecksell B, & Zaccario M (2011). Parentchild discrepancies in report of psychopathology: The contributions of response bias and parenting stress. Journal of Personality Assessment, 93(5), 527–536. 10.1080/00223891.2011.594131. [DOI] [PubMed] [Google Scholar]
- Williford AP, Calkins SD, & Keane SP (2007). Predicting change in parenting stress across early childhood: Child and maternal factors. Journal of Abnormal Child Psychology, 35(2), 251–263. 10.1007/s10802-006-9082-3. [DOI] [PubMed] [Google Scholar]
- Woodman AC, Mawdsley HP, & Hauser-Cram P (2015). Parenting stress and child behavior problems within families of children with developmental disabilities: Transactional relations across 15 years. Research in Developmental Disabilities, 36, 264–276. 10.1016/j.ridd.2014.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zablotsky B, Bradshaw CP, & Stuart EA (2013). The association between mental health, stress, and coping supports in mothers of children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 43(6), 1380–1393. 10.1007/s10803-012-1693-7. [DOI] [PubMed] [Google Scholar]
- Zaidman-Zait A, Mirenda P, Duku E, Szatmari P, Georgiades S, Volden J, Zwaigenbaum L, Vaillancourt T, Bryson S, Smith I, & Fombonne E (2014). Examination of bidirectional relationships between parent stress and two types of problem behavior in children with autism spectrum disorder Ann Thompson the Pathways in ASD Study Team. Journal of Autism and Developmental Disorders, 44, 1908–1917. 10.1007/s10803-014-2064-3. [DOI] [PubMed] [Google Scholar]
- Zuckerman KE, Lindly OJ, Reyes NM, Chavez AE, Cobian M, Macias K, Reynolds AM, & Smith KA (2018). Parent perceptions of community autism spectrum disorder stigma: Measure validation and associations in a multi-site sample. Journal of Autism and Developmental Disorders, 48(9), 3199–3209. 10.1007/s10803-018-3586-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


