Abstract
Contrast-induced encephalopathy (CIE) is an uncommon complication associated with contrast exposure during angiographic procedures that is usually transient but occasionally leads to permanent complications or death. Due to the low incidence of CIE, there are still insufficient reports. This study was used to summarize the clinical features of CIE through a case report and systematic review. We summarized and reviewed 127 patients with CIE, and we found that the total incidence of CIE between men and women had no difference (49.61 and 50.39%, respectively), but the average age in female patients with CIE was older than that in male patients (62.19 and 58.77 years, respectively). Interestingly, the incidence of female patients with CIE in the poor prognosis group was significantly higher than that in the good prognosis group (62.50 and 36.51%, respectively), and the average age of these female patients in the poor prognosis group was younger than that in the good prognosis group (61.39 and 62.82 years, respectively). The contrast medium types were mainly nonionic (79.69 and 73.02%, respectively) and low-osmolar (54.69 and 71.43%, respectively) in both groups. Importantly, the total contrast media administrated in patients with poor prognoses was greater than that administrated in patients with good prognoses (198.07 and 188.60 ml, respectively). In addition, comorbidities in both groups included hypertension (55.91%), diabetes mellitus (20.47%), previous contrast history (15.75%), renal impairment (11.81%), and hyperlipidemia (3.15%). The percentage of patients with cerebral angiography was significantly higher in the poor prognosis group than that in the good prognosis group (37.50 and 9.52%, respectively), whereas the percentage of patients with coronary angiography in both groups had the opposite results (35.94 and 77.78%, respectively). In conclusion, CIE may not always have a benign outcome and can cause permanent deficits. Female gender, younger age, the higher dose of contrast medium, and the procedure of cerebral angiography may be related to the patient’s poor prognosis.
Keywords: cerebral angiography, contrast-induced encephalopathy, neurological deficit, prognosis, risk factor
Introduction
Contrast-induced encephalopathy (CIE) is an uncommon complication associated with intravenous or intra-arterial exposure to iodinated contrast media during angiographic procedures. The incidence of CIE ranges between 0.3 and 4.0% (de Bono, 1993; Potsi et al., 2012; Liu et al., 2020). Since the first description in 1970, the clinical features of CIE have included headache, memory loss, confusion, visual and speech impairment, seizures, hemiparesis, and even coma. The underlying mechanisms and causes of iodine-based CIE remain unclear. Studies suggest that this may be related to transient blood–brain barrier (BBB) breakdown and increased permeability, which may subsequently contribute to extravasation of contrast medium into the central nervous system, resulting in cerebral edema and altered neuronal excitability (Dangas et al., 2001; Babalova et al., 2021). In addition, some high concentrations of contrast media may cause the clumping of red blood cells and, consequently, occlusion of arterial branches, which may play a role in permanent neurological deficits (Cristaldi et al., 2021). Most patients with CIE have a good prognosis and resolve quickly within 1–2 days (Spina et al., 2017). A minority (approximately 15% of CIE) may develop permanent neurological deficits or fatal cerebral edema (Hamra et al., 2017; Donepudi and Trottier, 2018; Zhao et al., 2019). However, the development of an evidence-based consensus on CIE has been hindered by the low incidence of CIE. Although the current literature on CIE is extensive, only case reports in the literature describe CIE and further analyses on the risk factors of CIE prognosis have been rarely performed. Here, we provided a case report as a reference and summarized existing reports about CIE, aiming to explore pathogenesis, risk factors, diagnosis, treatment strategy, and future exploration direction of the disease.
Case report
A 51-year-old woman was admitted to our hospital with a suspected intracranial aneurysm. The patient had a history of hypertension. On admission, a physical examination showed no signs of neurological deficits. Cerebral angiography was urgently performed through the right femoral approach. The procedure lasted for 60 min. A total of 50 ml iodixanol (Jiangsu Hengrui Pharmaceutical Co., Ltd., China), an iso-osmolar non-ionic dimeric hydrophilic contrast medium, was injected. Notably, 1% lignocaine was administered for local anesthesia prior to cerebral angiography. This was the patient’s first exposure to a contrast medium, and no obvious aneurysm or vascular malformation was found.
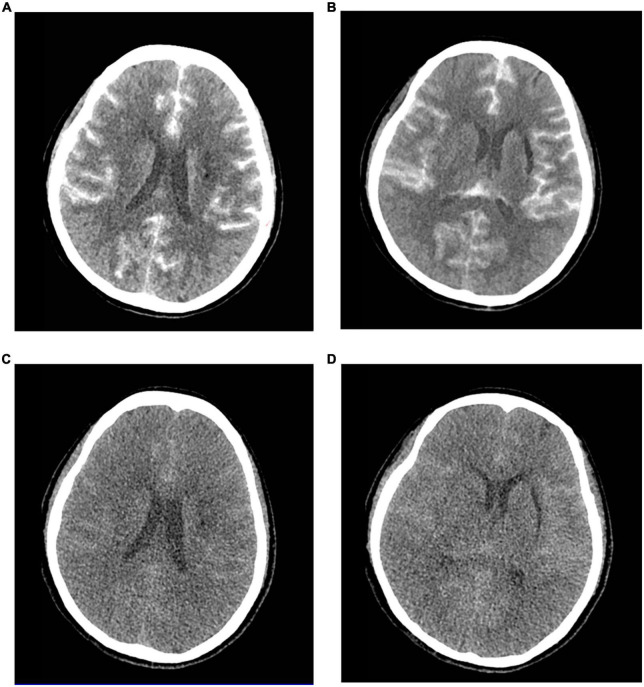
Approximately 5 h after surgical completion, the patient developed a decrease in the upper and lower extremity motor strength, and the pupils were symmetric and reactive. The left muscle strength was grade 2, and the right muscle strength was grade 3. An emergency brain computed tomography (CT) scan was requested and revealed the diffuse contrast enhancement in brain sulci, fissures, cisterns, third ventricle, fourth ventricle, and subarachnoid space with mild global brain edema, and softening foci in the left basal ganglia-insular area (Figures 1A,B). On the second day, the patient’s clinical symptoms further deteriorated and the upper and lower muscle strength was grade 0 with positive pathological signs. Brain CT was reviewed and showed diffuse enhancement disappeared, but the brain parenchyma was diffusely swollen and the lateral ventricles were slightly more compressed than that in the previous scan (Figures 1C,D). A diagnosis of CIE was suspected given the worsening of the clinical manifestations and symptoms compatible with higher functional impairment following the administration of the contrast medium.
FIGURE 1.
Contrast-induced encephalopathy in brain computed tomography (CT) scans. (A,B) Emergency brain CT 5 h after the procedure showed diffuse contrast enhancement in the brain parenchyma and subarachnoid space with mild global brain edema and the softening foci in the left basal ganglia-insular area. (C,D) Brain CT 2 days after the procedure indicated diffuse enhancement disappeared, and the brain parenchyma was diffusely swollen and the lateral ventricle was slightly more compressed.
The patient routinely received fluids to accelerate the excretion of contrast medium, 1,000 mg of intravenous methylprednisolone once daily for 2 days to mitigate inflammation, 250 ml of mannitol every 8 h to dehydrate and reduce intracranial pressure, 10 mg of nimodipine once daily to prevent vasospasm, 120 mg of sodium valproate once daily to prevent epilepsy, as well as strengthen nutrition to improve clinical symptoms. Furthermore, lumbar cistern drainage was performed to reduce intracranial pressure, and cerebrospinal fluid (CSF) was clear with increased white blood cell count and glucose level and decreased chloride level. In the following hours, the patient experienced further deterioration in mental status and fell into a coma with respiratory insufficiency. Therefore, the patient was transferred to the intensive care unit (ICU) where she underwent tracheal intubation with ventilator-assisted breathing, dehydration, anti-epileptic therapy, body temperature and blood pressure control, and close neurological observation.
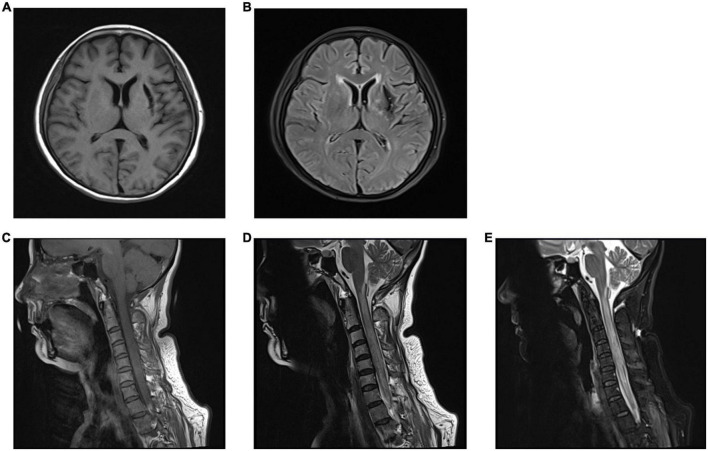
On the second day after being admitted to the ICU, the patient regained consciousness, but her motor deficit was unchanged. A neurological examination showed muscle weakness in the upper and lower limbs and sensory loss below the T2 sensory level, which may be related to spinal cord edema. Considering that the patient was temporarily unable to remove the tracheal tube, a tracheotomy was performed 4 days later. A magnetic resonance imaging (MRI) performed at 2 weeks revealed a diffuse hyperintense signal on FLAIR sequences in the cervical cord, which may be consistent with the patient’s motor deficits and sensory disturbances, as well as a softening foci formation in the left basal ganglia-insular area (Figure 2). Dramatically, the patient suffered from a lung infection during hospitalization and was eventually discharged from the neurosurgery ward to another hospital for hyperbaric oxygen therapy after 20 days. A telephone follow-up after 2 months revealed that the patient’s persistent neurological deficits had not improved.
FIGURE 2.
The brain and cervical spine magnetic resonance imaging (MRI) performed at 2 weeks. (A,B) Brain MRI showed the left basal ganglia-insular softening foci in T1 (A) and T2 (B) weighted image. (C–E) Cervical spine MRI showed diffuse hyperintense signal in the cervical cord in T2-weighted image (D) and fluid-attenuated inversion recovery (FLAIR) images (E), and normal findings were observed in T1-weighted image (C).
Literature review
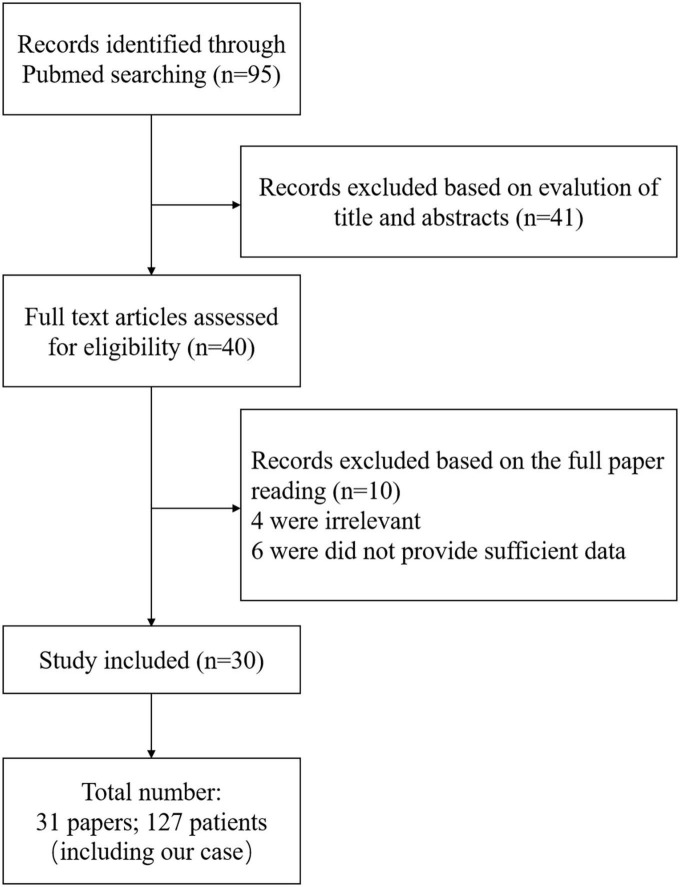
In searching for the keywords “Contrast-induced encephalopathy” and “Angiography” in PubMed, 95 relevant articles were found. A total of 54 papers were selected after screening abstracts and titles. After reading through the whole paper, the reviews, editorial, and duplicate cases were excluded, and 40 papers were left. However, four of them were excluded because it was defined as allergic reactions, vasospasm, and posterior reversible encephalopathy syndrome, and complete data were not available in the other six papers. Finally, we accurately summarized 30 papers (Leong and Fanning, 2012; Yan and Ramanathan, 2013; Kocabay et al., 2014; Nagamine et al., 2014; Hamra et al., 2017; Park et al., 2017; Spina et al., 2017; Dattani et al., 2018; Heemelaar et al., 2018; Hirata et al., 2018; Kahyaoğlu et al., 2018; Tong et al., 2018; Renault and Rouchet, 2019; Riahi et al., 2019; Şimşek et al., 2019; Zhao et al., 2019, 2021; Fernando et al., 2020; Harada et al., 2020; Lei et al., 2020; Liu et al., 2020; Andone et al., 2021; Cristaldi et al., 2021; García-Pérez et al., 2021; Kamimura et al., 2021; Li et al., 2021; Vigano et al., 2021; Yao et al., 2021; Zhang et al., 2021; Rashid et al., 2022). A total of 127 patients were enrolled. Figure 3 shows the screening process. Table 1 shows the basic information of 31 studies (including our case).
FIGURE 3.
Screening process.
TABLE 1.
Basic information of all patients.
| Study | Number | Gender/Age (year) | Procedure | Risk factor | Previous angio- graphy |
Contrast medium | Contrast medium class | Volume (ml) | Presentation | Neuroimaging | Symptom duration | Complete resolution |
| Andone et al., 2021 | 1 | M/70 | Diagnostic coronary angiography | HT, DM | No | Ioversol | Non-ionic, monomer, low osmolar | 100 | Headache, behavioral changes and aggressive tendencies | CT: a mild hyper-density in the frontal lobes; MRI: normal |
72 h | Yes |
| Dattani et al., 2018 | 2 | M/76 | Coronary angiography | HT, DM | No | Iohexol | Non-ionic, monomer, low osmolar |
120 | Confused and aggressive, expressing verbal profanities | CT: normal | 9 days | Yes |
| 3 | M/65 | Diagnostic coronary angiography | Previous CIE, HT, Dyslipidaemia, Smoking. | Yes | Iopromide | Non-ionic, monomer, low osmolar |
110 | Global aphasia, bilateral limb weakness | CT and MRI: normal; | 24 h | Yes | |
| 4 | M/49 | Coronary angiography | – | – | Iopromide | Non-ionic, monomer, low osmolar |
205 | Confusion, decreased GCS | – | 12 h | Yes | |
| 5 | M/32 | Coronary angiography | – | – | Iopromide | Non-ionic, monomer, low osmolar |
100 | Cortical blindness | CT: normal | 24 h | Yes | |
| 6 | F/39 | Coronary angiography | – | No | Iopamidol | Non-ionic,monomer, low osmolar | 100 | Cortical blindness | CT: normal | 1 h | Yes | |
| 7 | M/74 | Coronary angiography + aortogram | HT, Obse | No | Iomeprol | Non-ionic, monomer, low osmolar |
320 | Cortical blindness | CT: normal | 24 h | Yes | |
| 8 | M/73 | Coronary angiography + PCI | Sleep apnea, Hypoventilation, Obese | – | None reported | N/A | 240 | Cortical blindness | CT: normal | 7 h | Yes | |
| 9 | M/53 | Coronary angiography | – | – | Ioversol | Non-ionic, monomer, low osmolar |
100 | Cortical blindness, catatonia | – | 12 h | Yes | |
| 10 | M/45 | Coronary angiography + PCI | HT | No | Ioversol | Non-ionic, monomer, low osmolar |
167 | Cortical blindness | – | 24 h | Yes | |
| 11 | M/59 | Coronary angiography + PCI | HT | No | Ioversol | Non-ionic, monomer, low osmolar |
220 | Cortical blindness | – | 12 h | Yes | |
| 12 | M/68 | Coronary angiography + PCI | HT | No | Ioversol | Non-ionic, monomer, low osmolar |
262 | Homonymous hemianopia | – | 15 min | Yes | |
| 13 | M/55 | Coronary angiography | – | Yes | Diatrizoate | Ionic, monomer, high osmolar |
280 | Cortical blindness | CT: both occipital lobes enhancement | 24 h | Yes | |
| 14 | M/61 | Coronary angiography | – | Yes | Diatrizoate | Ionic, monomer, high osmolar |
145 | Cortical blindness | CT: normal | 36 h | Yes | |
| 15 | M/44 | Coronary angiography | – | No | Diatrizoate | Ionic, monomer, high osmolar |
50 | Cortical blindness | No brain CT | 12 h | Yes | |
| Kamimura et al., 2021 | 16 | F/70 | Diagnostic erebral angiography | Not reported | No | Iopamidol | Non-ionic, monomer, low osmolar |
43 | Confusion and generalized tonic-clonic seizures | CT: high-density signaling in the cortex; MRI: high signal intensity in temporal lobe |
24 h | Yes |
| 17 | M/71 | Cerebral angiography | Not reported | No | Iohexol | Non-ionic, monomer, low osmolar |
46 | Cortical blindness, confusion, and Ophthalomoplegia | No brain CT | 10 days | N/A | |
| 18 | F/68 | Cerebral angiography | Not reported | No | Iohexol | Non-ionic, monomer, low osmolar |
24 | Cortical blindness, confusion, and amnesia | No brain CT | 6 days | N/A | |
| 19 | F/71 | Cerebral angiography | HT, Transient ischemic attack | No | Iopromide | Non-ionic, monomer, low osmolar |
25 | Confusion, disorientation, and hemiparesis | CT: edema, right diffuse cortical hyperattenuation | 24 h | Yes | |
| Fernando et al., 2020 | 20 | F/52 | Coronary angiography | HT | N/A | Iopromide | Non-ionic, monomer, low osmolar |
130 | Left sided hemiparesis, disorientation, and decreased GCS | CT: cortical and subarachnoid hyper-densities |
5day | Yes |
| Cristaldi et al., 2021 | 21 | F/54 | Cerebral angiography | HT, Cerebral ischemia |
N/A | Iobitridol | Non-ionic, monomer, low osmolar |
Not reported | Severe right hemiparesis and complete aphasia | CT: edema, abnormal subarachnoid contrast enhancement zone | >6 months | No |
| 22 | M/10 | Angiocardio- graphy |
Fallot’s tetralogy | Not stated | Urografin 76% |
Ionic, monomer, high osmolar |
76 | Apnoea and cardiac arrest | No CT brain (autopsy showed brain edema) | During | Death | |
| 23 | F/7 | Aortography | HT | No | Renografin 76% |
Ionic, monomer, high osmolar |
340 | Seizures | CT: contrast enhancement of cortex, basal ganglia and thalamus | During | Death | |
| 24 | M/68 | Bypass graft angiography | HT, DM | Yes | Iohexol | Non-ionic, monomer, low osmolar |
180 | Confusion, amnesia, aphasia, cortical blindness | CT: contrast enhancement of occipital lobes, temporal lobes, thalami | During | No | |
| 25 | F/73 | Coronary angiography | HT | No | Iohexol | Non-ionic, monomer, low osmolar |
1150 | Seizures, gait instability, postural tremor, dysphasia | CT: abnormal signal in bilateral frontal and occipital | During | No | |
| 26 | F/62 | Cerebral angiography | None reported | No | Not specified | Non-ionic | 297 | Confusion, cortical blindness | CT: abnormal signal in bilateral occipital, basal ganglia, frontal | During | No | |
| 27 | M/41 | Cerebral angiography | None reported | Yes | Not specified | Non-ionic | 225 | Bilateral visual loss, agitation | CT: right parietal abnormal signal | 3 h | No | |
| 28 | F/54 | Cerebral angiography | None reported | Yes | Not specified | Non-ionic | 62 | Cortical blindness with only light perception | MRI: bilateral occipital | 1 months | Yes | |
| 29 | M/46 | Cerebral angiography | None reported | Yes | Not specified | Non-ionic | 225 | Right homonymous hemianopia | CT and MRI: normal | 1 months | Yes | |
| 30 | M/47 | Cerebral angiography | None reported | No | Not specified | Non-ionic | 384 | Right homonymous hemianopia | CT: normal | 7 days | Yes | |
| 31 | F/67 | Coronary angiography | Angina, DM, HT | – | Iodixanol | Non-ionic, dimer, iso-osmolal |
Not reported | Gradually GCS 3 | N/A | During | Yes | |
| 32 | F/71 | Cerebral angiography | HT, hyperlipidemia, Angina | – | Iopamidol | Non-ionic, monomer, low osmolar |
110 | Dizziness, nausea, vomiting; then respiratory distress, deep coma, GCS 3 | CT: cerebral edema | 56 days | Death | |
| 33 | F/51 | Carotid artery angioplasty | HT, DM, Coronary artery disease |
– | Iohexol | Non-ionic, monomer, low osmolar |
Not reported | Seizures, unconsciousness | N/A | During | Death | |
| Spina et al., 2017 | 34 | F/44 | Diagnostic coronary angiography + PCI | End-stage kidney disease, HT, DM | – | Iohexol | Non-ionic, monomer, low osmolar |
190 | Left-sided weakness, seizure activity | CT: contrast enhancement of right cerebral hemisphere | 72 h | Yes |
| 35 | M/69 | Diagnostic coronary angiography + PCI | HT, DM | – | Not reported | N/A | N/A | Aphasia, left-sided hemiparesis | CT: contrast enhancement of right cerebral hemisphere | 12 h | Yes | |
| 36 | F/63 | Diagnostic coronary angiography | HT, DM | – | Iopramide | Non-ionic, low osmolar | 250 | Cortical blindness | CT: contrast enhancement of occipital lobes; MRI: normal | 72 h | Yes | |
| 37 | F/60 | Diagnostic coronary angiography | HT | – | Not reported | N/A | N/A | Abrupt decrease in GCS score to 6/15 | CT: cerebral edema confined to the right cerebral hemisphere; MRI: normal |
10 days | Yes | |
| 38 | F/76 | Diagnostic coronary angiography | HT, DM | – | Ioversol | Non-ionic, monomer, low osmolar |
125 | Aphasia, cortical blindness, right sided weakness | MRI: hyperintensity in frontoparietal regions |
48 h | Yes | |
| 39 | F/69 | Diagnostic coronary angiography + PCI | CKD, DM, Previous contrast reaction |
Yes | Iodixanol | Non–ionic, dimer, iso-osmolal |
320 | Partial seizure, homonymous hemianopia, hemisensory loss, hemiparesis | CT: cerebral edema | 24 h | Yes | |
| 40 | M/64 | Diagnostic coronary angiography + PCI | HT, DM | – | Iopromide | Non-ionic, monomer, low osmolar |
160 | Confusion, irritability, limb paralysis, aphasia | CT: hyperdensity of sagittal sinus |
28 h | Yes | |
| 41 | M/68 | Diagnostic coronary angiography + PCI | HT | – | Iopromide | Non-ionic, monomer, low osmolar |
250 | Left lower extremity weakness and sensory loss |
CT: contrast enhancement in sagittal sinus and occipital lobe |
12 h | Yes | |
| 42 | M/47 | Diagnostic coronary angiography + PCI | None reported | – | Iopromide | Non-ionic, monomer, low osmolar |
150 | Confusion, agitation, nausea, headache | CT: contrast enhancement in right occipital lobe | 8 h | Yes | |
| 43 | M/70 | Diagnostic coronary angiography + PCI | DM | – | Iopromide | Non-ionic, monomer, low osmolar |
120 | Confusion; nausea | CT: contrast enhancement in occipital lobe | 12 h | Yes | |
| 44 | F/76 | PCI + carotid artery stenting | CKD, DM | – | Iodixanol | Non-ionic, dimer, iso-osmolal |
200 | Stupor, aphasia, hemiparesis | CT: hyperdensity of cerebral sulci and subarachnoid spaces | 48 h | Yes | |
| 45 | F/39 | Diagnostic coronary angiography | – | – | Iopamidol | Non-ionic, monomer, low osmolar |
80 | Cortical blindness | CT and vertebral angiogram: normal | 1 h | Yes | |
| 46 | F/70 | Diagnostic coronary angiography + PCI | – | – | None reported | N/A | N/A | Left-sided hemiparesis, conjugate gaze deviation to the right | CT: hyperdensity of cerebral sulci and right frontal lobe | 72 h | Yes | |
| 47 | F/70 | Diagnostic coronary angiography + PCI | – | – | Not specified | Ionic | 1500 | Myoclonus | CT: hyperdensity of cerebral sulci | <1 h | Yes | |
| 48 | F/52 | Diagnostic coronary angiography | – | – | Iomeprol | Non-ionic, monomer, low osmolar |
150 | Cortical blindness | CT: contrast enhancement of occipital lobes | 5 h | Yes | |
| 49 | F/70 | Diagnostic coronary angiography | DM, HT | – | Iobitridol | Non-ionic, monomer, low osmolar |
75 | Cortical blindness | CT: contrast enhancement of occipital lobes | 72 h | Yes | |
| 50 | M/56 | Diagnostic coronary angiography | – | – | Iopromide | Non-ionic, monomer, low osmolar |
135 | Confusion, dysarthria, cortical blindness | CT: contrast enhancement of right occipital lobe | 24 h | Yes | |
| 51 | F/82 | Diagnostic coronary angiography + PCI | CKD, HT | – | Iomeprol | Non-ionic, monomer, low osmolar |
500 | Aphasia, right-sided hemiparesis | CT: hyperdensities filling the sulci of both cerebral hemispheres |
40 h | Yes | |
| 52 | M/82 | Diagnostic coronary angiography | CKD, DM, HT | – | Iopromide | Non-ionic, monomer, low osmolar |
150 | Right-sided hemiparesis, aphasia | CT: Left hemisphere cerebral edema and extravascular local contrast media | 6 h | Yes | |
| 53 | M/63 | Diagnostic coronary angiography + Aortogram | – | – | Iopremol | Non-ionic, monomers | 450 | Amnesia, numbness, right upper extremity numbness | CT: contrast enhancement of right occipital lobe | 12 h | Yes | |
| 54 | F/63 | Diagnostic coronary angiography | DM, HT | – | Iopromide | Non-ionic, monomer, low osmolar |
160 | Cortical blindness, right homonymous hemianopia | CT and MRI: contrast enhancement of occipital lobes |
48 h | Yes | |
| 55 | F/52 | Diagnostic coronary angiography + PCI | HT | Yes | Ioversol | Non-ionic, monomer, low osmolar |
280 | Cortical blindness | CT: contrast enhancement of occipital lobes | 36 h | Yes | |
| 56 | M/55 | Diagnostic coronary angiography | – | – | Iomeprol | Non-ionic, monomer, low osmolar |
280 | Cortical blindness | CT: contrast enhancement of occipital lobes | 5 days | Yes | |
| 57 | M/58 | Diagnostic coronary angiography | HT | – | Ioglaxate | Ionic, dimer, low osmolar |
260 | Cortical blindness | CT: normal | 32 h | Yes | |
| 58 | M/64 | Diagnostic coronary angiography | – | – | Ioglaxate | Ionic, dimer, low osmolar |
400 | Cortical blindness | N/A | 30 h | Yes | |
| 59 | M/49 | Diagnostic coronary angiography | CKD, HT | – | Diatrizoate | Ionic, monomer, high osmolar |
610 | Seizures, encephalopathy | CT: contrast enhancement of left frontal gyri | 4 h | Yes | |
| 60 | M/62 | Diagnostic coronary angiography + PCI | CKD, HT | – | Iopamidol | Non-ionic, monomer, low osmolar |
170 | Headache, confusion, cortical blindness | CT: contrast enhancement of cerebellum, thalamus | 12 h | Yes | |
| 61 | M/62 | Diagnostic coronary angiography | HT | – | Iopamidol | Non-ionic, monomer, low osmolar |
270 | Cortical blindness, loss of coordination right arm | CT: contrast enhancement of occipital lobes | 72 h | Yes | |
| 62 | F/57 | Diagnostic coronary angiography | HT, Previous contrast reaction |
Yes | Ioglaxate | Ionic, dimer, low osmolar |
200 | Cortical blindness | CT: mild attenuation in occipital poles |
48 h | Yes | |
| 63 | F/52 | Diagnostic coronary angiography + aortogram | HT | – | Diatrizoate | Ionic, monomer, high osmolar |
100 | Cortical blindness | N/A | 18 h | Yes | |
| Hamra et al., 2017 | 64 | M/62 | Coronary angioplasty | HT | – | Iohexol | Non-ionic, monomer, low osmolar |
200 | Right-sided homonymous hemianopia | CT: contrast enhancement of the venous sinuses and cerebral arteries |
48 h | Yes |
| Vigano et al., 2021 | 65 | F/56 | Cerebral angiography | Migraine, Renal colic, Smoking, Previous heroin abuse | – | Iomeprol | Non-ionic, monomer, low osmolar |
70 | Global aphasia and right hemiplegia | CT: left cerebral edema | 10 days | Yes |
| 66 | F/74 | Abdominal aorta and renal artery angiography + angioplasty | Renal impairment; HT | No | Diatrizoate | Ionic, monomer, high osmolar |
250 | Cortical blindness, left hemiparesis | CT: bilateral occipital and basal ganglia alterations | 4–5 days | Yes | |
| 67 | M/64 | Carotid artery and aorta angiography | HT | No | Iothalamate meglumine | Ionic, monomer, high osmolar |
12 | Cortical blindness, fluent aphasia | CT: left temporo-parieto-occipital alterations | 3 days | N/A | |
| 68 | F/71 | Spinal angiography | – | No | Ioxaglate | Ionic dimer low osmolar |
360 | Right-sided visual neglect and Wernicke’s aphasia | CT: bilateral occipital and left parietal lobe alterations | 4 days | Yes | |
| 69 | M/82 | Carotid artery angiography + stenting | HT | Yes | Ioxaglate | Ionic, dimer, low osmolar |
50 | Confusion, left hemiparesis, neglect | CT: right frontoparietal cortical enhancement and edema | 2 days | Yes | |
| 70 | M/72 | Carotid artery angiography + coiling anterior aneurysm | – | No | Iopamidol | Non-ionic, monomer, low osmolar |
260 | Right hemiparesis and motor aphasia | CT: enhancement throughout the left cerebral cortex and left basal ganglia, diffuse swelling of the left cerebral hemisphere | 7 days | Yes | |
| 71 | M/80 | Carotid and coronary angiography + stenting | HT | No | Iohexol | Non-ionic, monomer, low osmolar |
250 | Right hemiparesis | CT: left frontoparietal-occipital cortical enhancement | 2 days | Yes | |
| 72 | M/51 | Carotid artery angiography + right internal carotid artery | HT | No | Iopromide | Non-ionic, monomer, low osmolar |
300 | Gerstmann’s left visual field deficit, hemiparesis, right gaze deviation | CT: cortical enhancement and edema in the right cerebral hemisphere | 2 days | Yes | |
| 73 | M/69 | Coronary angiography + PCI | – | – | Iohexol | Non-ionic, monomer, low osmolar |
100 | Stupor, disorientation, left hemiplegia | CT: hyperdense lesion in the right frontoparietal region, parietal lobe and basal ganglia | 6 h | Yes | |
| 74 | F/73 | Aortic angiography + thoracic aortic aneurysm repair | Chronic kidney disease; HT | Yes | Iodixanol | Non-ionic, dimer, iso-osmolal |
248 | Seizure and left-sided hemiplegia | CT: hyperdensity of the right cortex, subarachnoid space and basal ganglia | 7 days | N/A | |
| 75 | F/67 | Cerebral angiography | HT | Yes | N/A | N/A | N/A | Right-sided hemiparesis and aphasia | CT: cortical edema of the left cerebral hemisphere and contrast medium leakage to the subarachnoid space | 24 h | N/A | |
| Liu et al., 2020 | 76 | F/84 | Coronary angiography | HT, Paroxysmal atrial fibrillation, Chronic bronchitis | – | Iopromide | Non-ionic, monomer, low osmolar |
20 | Lost consciousness, and exhibited left limb hemiplegia with muscle strength level 0 and eyes staring to the right, seizure | CT: high-density regions in the subarachnoid space | 2 months | Yes |
| 77 | F/57 | Diagnostic coronary angiography + PCI | CKD, HT, DM | – | Iodixanol | Non-ionic, dimer, iso-osmolal | 130 | Tonic–clonic seizures | CT: right parenchymal edema | 72 h | Yes | |
| 78 | M/6 | Diagnostic coronary angiography | HT, DM | – | Iohexol | Non-ionic, monomer, low osmolar | 120 | Confused, aggressive, expressing verbal profanities | CT: normal | 9 days | Yes | |
| 79 | M/62 | Diagnostic coronary angiographyc + PCI | HT | – | Iohexol | Non-ionic, monomer, low osmolar | 300 | Right-sided homonymous hemianopia | CT: slight enhancement of the venous sinuses |
48 h | Yes | |
| 80 | M/49 | Diagnostic coronary angiography | – | – | Iopromide | Non-ionic, monomer, low osmolar |
205 | Confusion, decrease in level of consciousness | CT and MRI: normal | 12 h | Yes | |
| 81 | M/69 | Diagnostic coronary angiography + PCI | – | – | Iohexol | Non-ionic, monomer, low osmolar | 100 | Confusion, headache, vomiting, left hemiplegia, | CT: focal hyperdense lesions | 6 h | Yes | |
| 82 | M/74 | Diagnostic coronary angiography + aortogram | – | Iomeprol | Non-ionic, monomer, low osmolar | 320 | Cortical blindness | CT: normal | 24 h | Yes | ||
| Riahi et al., 2019 | 83 | F/71 | Coronary angiography | HT, DM | – | Iodixanol | Non-ionic, dimer, iso-osmolal | 80 | Aphasia, GCS score to 7/15 | CT: normal | 24 h | Yes |
| Rashid et al., 2022 | 84 | F/76 | Coronary angiography | DM, HT, Hyperlipidemia, Coronary artery disease | – | N/A | N/A | N/A | Confusion and aggressive behavior | CT and MRI: normal | 16 days | Yes |
| Zhang et al., 2021 | 85 | M/42 | Coronary angiography | – | – | Iopromide | Non-ionic, monomer, low osmolar |
200 | Severe headache, cortical blindness and neuropsychiatric symptom | CT: normal | 5 days | Yes |
| Park et al., 2017 | 86 | F/58 | Cerebral angiography | HT, Hypothyroidism, Peripheral artery occlusive disease, Depressive disorder | – | Iodixanol | Non-ionic, dimer, iso-osmolal | 220 | Tonic-clonic seizure, left hemiparesis involving face, arm and leg(grade 3/5), sensory loss, and left-sided neglect with drowsy mentality | CT:sulcal obliteration of right cerebral hemisphere; MRI: gyral swelling and hyperintensity in the right cerebral hemisphere |
6 days | Yes |
| Kocabay et al., 2014 | 87 | F/58 | Diagnostic coronary angiography + PCI | HT, Hyperlipidemia | – | Iopromide | Non-ionic, monomer, low osmolar |
220 | Bilateral oculomotor ophthalmoplegia |
N/A | >30 days | No |
| 88 | M/68 | Diagnostic coronary angiography + PCI | HT | – | Iopromide | Non-ionic, monomer, low osmolar | 250 | Monoplegia | N/A | 12 h | Yes | |
| 89 | M/68 | Diagnostic coronary angiography + PCI | HT, DM | – | Iopromide | Non-ionic, monomer, low osmolar | 180 | Unilateral oculomotor monoplegia |
N/A | 1 h | Yes | |
| 90 | M/70 | Diagnostic coronary angiography + PCI | HT | – | Iopromide | Non-ionic, monomer, low osmolar | 130 | Cerebellar dysfunction | N/A | 14 h | Yes | |
| Kahyaoğlu et al., 2018 | 91 | M/66 | Lower extremity angiography | – | – | Iohexol | Non-ionic, monomer, low osmolar | Not reported | Confusion and cortical blindness, seizure | CT: normal | 24 h | Yes |
| Zhao et al., 2019 | 92 | F/71 | Digital subtraction angiography | HT, Hyperlipemia, Angina | – | Iopamidol | Non-ionic, monomer, low osmolar | 110 | Headache, dizziness, nausea and vomiting, deep coma | CT: cerebral edema | 56 days | Death |
| Li et al., 2021 | 93 | F/77 | Digital subtraction angiography | HT, Coronary heart disease | Yes | Visipaque | Non-ionic | 200 | Right hemiplegia, aphasia, and epilepsy | CT: hyperdensity in the left subarachnoid space | 6 days | Yes |
| Zhao et al., 2021 | 94 | F/50 | Cerebral angiography | – | – | Iopromide | Non-ionic, monomer, low osmolar |
6 | Disturbance of consciousness, seizures, frequent blinking, and stiffness | CT: normal; MRI: swelling of the left cerebral cortex |
10 days | Yes |
| Heemelaar et al., 2018 | 95 | F/67 | Coronary angiography | DM, HT, Adenocarcinoma of the left breast | – | Iso-osmolar iodinated contrast | Iso-osmolar | 100 | Acute-onset coma and respiratory insufficiency | CT: bilateral cerebral edema | 23 days | Yes |
| García-Pérez et al., 2021 | 96 | F/61 | Diagnostic digital subtraction angiography | Migraine | – | Iodixanol | Non-ionic, dimer, iso-osmolar | 70 | Confused and drowsy, agitated and vomiting | MRI: lesions in the cerebellar hemispheres and parieto-occipital lobes; | 36–48 h | Yes |
| 97 | M/22 | Diagnostic digital subtraction angiography | Left parietooccipital arteriovenous malformation | – | None reported | N/A | None reported | Disoriented, bilateral amaurosis and presented amnesia | CT and MRI: normal | 48–72 h | Yes | |
| Harada et al., 2020 | 98 | F/72 | Coronary angioplasty | HT, Hyperlipidemia | – | Iodinated contrast | None reported | 210 | Left hemiparesis, left sensory and visual hemineglect, and right gaze preference | CT: mild cerebral edema | 2 days | Yes |
| Renault and Rouchet, 2019 | 99 | M/49 | Renal artery angiography | Chronic renal failure | – | Iohexol | Non-ionic, monomer, low osmolar | Cortical blindness, global amnesia disappeared | MRI: normal | 6 days | Yes | |
| Hirata et al., 2018 | 100 | M/75 | Coronary angioplasty | DM | – | None reported | N/A | None reported | No neurological symptoms were observed because the patient was intubated | CT: high-density areas in the cortex, putamen, caudate nucleus and subarachnoid space of the right cerebral hemisphere |
12 days | Yes |
| Yao et al., 2021 | 101 | M/68 | Contrast-enhanced chest CT examination | Rheumatoid arthritis | – | Iso-osmolar iodinated contrast | Iso-osmolar | 70 | Lost consciousness and experienced cardiorespiratory arrest | CT: abnormal cortical contrast enhancement and cerebral sulci hyperdensity |
>17days | Yes |
| Leong and Fanning, 2012 | 102 | F/50 | Cerebral angiography | HT | No | Iopramide | Non-ionic, low osmolar | 220 | Right hemisyndrome | CT: edema in the left cerebral hemisphere | During | No |
| 103 | F/59 | Aortic arch angiography | Renal impairment; HT | Yes | Diatrizoate | Ionic, monomer, high osmolar |
150 | Cortical blindness; headache, myoclonus or seizure | CT: bilateral parieto-occipital contrast enhancement | 3 days | Yes | |
| 104 | F/53 | Carotid artery angiography | Not reported | No | Diatrizoate meglumine |
Ionic, monomer, high osmolar |
60 | Partial motor seizure | CT: right temporo-parietal contrast enhancement | 24 h | Yes | |
| 105 | M/70 | Arch, Carotid & Vertebral arteries angiography | None reported | No | Diatrizoate | Ionic, monomer, high osmolar |
72 | Cortical blindness | CT: bilateral Occipital hyperdensity |
2 days | Yes | |
| 106 | F/74 | Abdominal aorta angiography | HT, Renal impairment | No | Iopamidol | Non-ionic, monomer, low osmolar | 415 | Visuospatial disorder | CT: bilateral parieto-occipital hyperdensity | 4 days | Yes | |
| 107 | F/74 | Diagnostic cerebral angiography | HT | No | Iohexol | Non-ionic, monomer, low osmolar | None reported | Complete bilateral blindness; confusion | CT: left parieto-occipital hyperdensity; MRI: left occipita hyperdensity |
24 h | Yes | |
| 108 | F/45 | Diagnostic cerebral angiography | HT | No | Iohexol | Non-ionic, monomer, low osmolar | None reported | Complete bilateral blindness; confusion | CT: normal; MRI: bilateral occipital hyperdensity |
7 days | Yes | |
| 109 | F/73 | Diagnostic cerebral angiography | HT | No | Iohexol | Non-ionic, monomer, low osmolar | None reported | Cortical blindness | CT: normal; MRI: bilateral occipita hyperdensity |
5 days | Yes | |
| 110 | F/70 | Coronary artery angiography | HT | Yes | None reported | N/A | 1500 | Seizure | CT: hyperdensity of right frontal | 24 h | Yes | |
| 111 | M/56 | Coronary artery | None reported | Yes | Iohexol 350 | Non-ionic, monomer, low osmolar | 220 | Bilateral cortical blindness | CT: high-density areas in the bilateral occipital and frontal lobes |
4 days | Yes | |
| Nagamine et al., 2014 | 112 | F/58 | Cerebral angiography | Unknown | N/A | Iohexol | Non-ionic, monomer, low osmolar | – | Agraphia, right hemiparesis | N/A | >20 days | No |
| Tong et al., 2018 | 113 | F/64 | Diagnostic cerebral angiography | HT | No | ioversol | Non-ionic, monomer, low osmolar | 300 | Lateral blindness | MRI: normal | 6 days | Yes |
| 114 | M/53 | Diagnostic cerebral angiography | HT | Yes | Omnipaque | Non-ionic, monomer, high osmolar | 155 | Lateral blindness | CT: bilateral brain edema on frontal and occipital lobe | 5 days | Yes | |
| 115 | F/61 | Diagnostic cerebral angiography | HT | – | Omnipaque | Non-ionic, monomer, high osmolar | 10 | Lateral blindness | MRI: right occipital cerebellar infarction | 3 months | Yes | |
| 116 | M/58 | Carotid artery + vertebral artery angiography | – | Yes | Iopromide | Non-ionic, monomer, low osmolar |
350 | Cortical blindness | CT: cortical hyperdensity and vasogenic edema | 10 days | Yes | |
| 117 | M/57 | Vertebral artery angiography | – | Yes | Omnipaque | Non-ionic, monomer, high osmolar | 20 | Bilateral cortical blindness | CT: normal; MRI: abnormal bilateral parieto-occipital lobes |
24 h | Yes | |
| Lei et al., 2020 | 118 | M/76 | Coronary angiography | HT, DM, Transient ischemic attacks | Yes | Iodixanol | Non-ionic, dimer, iso-osmolar | 150 | Epileptic seizures | N/A | 6 months | Yes |
| Yan and Ramanathan, 2013 | 119 | M/63 | Cerebral angiogram | HT, DM, Rheumatoid arthritis, End-stage renal disease | – | Iodixano | Non-ionic, dimer, iso-osmolar | 910 | Left-sided blindness and ophthalmoplegia | CT: bilateral subarachnoid hyper-attenuation over the cerebral sulci, and diffuse cerebral edema | 72 h | Yes |
| 120 | F/58 | Cerebral arteriogram | – | – | Iodixanol | Non-ionic, dimer, iso-osmolar | 193 | Left hemiparesis | CT: hyperdensity of right frontoparietal lobe | 4 days | Yes | |
| 121 | F/61 | Cerebral arteriogram | – | – | Iodixanol | Non-ionic, dimer, iso-osmolar | 212 | Left hemiparesis | CT: hyperdensity of right frontoparietal lobe | 3 days | Yes | |
| 122 | F/58 | Transfemoral cerebral angiography | – | – | Ioversol | Non-ionic, monomer, low osmolar | N/A | Global aphasia, right sided hemiparesis |
CT: abnormal enhancement in left cerebral cortex and thalamus | 3 days | Yes | |
| 123 | F/63 | Right middle cerebral angiography | – | – | Iopromide | Non-ionic, monomer, low osmolar |
150 | N/A | CT: diffuse subarachnoid hyperdensity |
2 days | Yes | |
| 124 | M/16 | Angiography of the circle of Willis | – | – | Iopromide | Non-ionic, monomer, low osmolar |
50 | Cortical blindness | CT: occipital lobe hyperdensity | 24 h | Yes | |
| 125 | F/69 | Coronary angioplasty | – | – | Iopamidol 370 | Non-ionic, monomer, low osmolar | 260 | Seizure, right hemiparesis. | CT: left cerebral cortex, left basal ganglia hyperdensity |
18 h | Yes | |
| Şimşek et al., 2019 | 126 | M/68 | Coronary angiography | HT, DM, Coronary artery disease, Severe renal impairment | No | Iohexol | Non-ionic, monomer, low osmolar | 230 | seizure | CT: hyperdense fields at the vertex and at the right frontal lobe | 60 h | Yes |
| Our case | 127 | F/51 | Cerebral angiography | HT | No | Iodixanol | Non-ionic, dimer, iso-osmolal | 50 | Dyskinesia, coma | CT:the diffuse hyperdensity in brain sulci, fissures, cisterns, third ventricle, fourth ventricle and subarachnoid space, and global brain edema | >3 months | No |
From the search results, we found that the total incidence of CIE between women and men has no difference. A total of 63/127 (49.61%) patients were women and 64/127 (50.39%) patients were men, and the average age in women was older than that in men (62.19 and 58.77 years, respectively). More importantly, we classified the statistical results according to prognosis, and patients who recovered less than or equal to 48 h were included in the good prognosis group and the remaining patients were included in the poor prognosis group. Eventually, 63 patients were included in the good prognosis group and 64 patients were included in the poor prognosis group, and the results are shown in Table 2. We found that the incidence of female patients with CIE in the poor prognosis group was significantly higher than that in the good prognosis group (62.50 and 36.51%, respectively), and the average age of these female patients in the poor prognosis group was younger than that in the good prognosis group (61.39 and 62.82 years, respectively). Furthermore, the poor prognosis group had a wider age range, ranging from 6 to 84 years.
TABLE 2.
The relationship between prognosis with variable.
| ≤2 days (n = 63) | >2 days (n = 64) | |
| Gender | ||
| Female (%) | 23 (36.51) | 40 (62.50) |
| Male (%) | 40 (63.49) | 24 (37.50) |
| Age (year) | 62.82 ± 1.41 | 61.39 ± 1.45 |
| Contrast types | ||
| Non-ionic (%) | 46 (73.02) | 51 (79.69) |
| Ionic (%) | 12 (19.05) | 6 (9.38) |
| Low-osmolar (%) | 45 (71.43) | 35 (54.69) |
| High-osmolar (%) | 8 (12.70) | 7 (10.94) |
| Iso-osmolal (%) | 4 (6.35) | 11 (17.19) |
| Contrast doses (ml) | 188.60 ± 13.99 | 198.07 ± 14.23 |
| Non-ionic (ml) | 193.39 ± 15.59 | 199.19 ± 14.73 |
| Ionic (ml) | 167.70 ± 37.91 | 235.20 ± 54.49 |
| Low-osmolar (ml) | 195.10 ± 16.18 | 207.83 ± 19.85 |
| High-osmolar (ml) | 117.83 ± 35.31 | 194.20 ± 45.73 |
| Iso-osmolal (ml) | 167.50 ± 58.79 | 152.56 ± 23.40 |
| Comorbidities | ||
| Hypertension (%) | 32 (50.79) | 39 (60.93) |
| Diabetes mellitus (%) | 10 (15.78) | 16 (25.00) |
| History of angiography (%) | 9 (14.29) + 1 | 11 (17.19) |
| Renal impairment (%) | 6 (9.52) | 9 (14.06) |
| Dyslipidaemia (%) | 2 (3.17) | 3 (4.69) |
| Angiography types | ||
| Coronary angiography (%) | 49 (77.78) | 23 (35.94) |
| Cerebral angiography (%) | 6 (9.52) | 24 (37.50) |
| Carotid and vertebral angiography (%) | 6 (9.52) | 4 (6.25) |
| Abnormal CT or MRI (%) | 40 (63.49) | 44 (68.75) |
In interventional procedures, the contrast types included non-ionic and ionic, or low-osmolar, high-osmolar, and iso-osmolar in our present study, and we found that both groups were mainly non-ionic (79.69 and 73.02%, respectively) and low-osmolar (54.69 and 71.43%, respectively). Importantly, the total contrast media administrated and the non-ionic, ionic, low-osmolar, or high-osmolar contrast media administrated in patients with poor prognosis were greater than that administrated in patients with good prognosis (198.07 and 188.60 ml, 199.19 and 193.39 ml, 235.20 and 167.70 ml, 207.83 and 195.10 ml, and 194.20 and 117.83 ml, respectively), whereas the iso-osmolar contrast media administrated was lower in patients with poor prognosis compared to patients with good prognosis (152.56 and 167.50, respectively).
The comorbidities in the present study mainly included hypertension (55.91%), diabetes mellitus (20.47%), previous contrast history (15.75%), renal impairment (11.81%), and hyperlipidemia (3.15%). Although there was no significant difference in comorbidities between the two groups, the percentages of hypertension, diabetes mellitus, previous contrast history, renal impairment, and hyperlipidemia in the poor prognosis group were higher than those in the good prognosis group (60.93 and 50.79%, 25.00 and 15.78%, 17.19 and 4.29%, 14.06 and 9.52%, and 4.69 and 3.17%, respectively). The angiography types, mainly coronary angiography (56.69%), cerebral angiography (23.62%), and carotid and vertebral angiography (7.87%), in both groups, were also analyzed. We found that the percentage of patients with cerebral angiography in the poor prognosis group was significantly higher than that in the good prognosis group (37.50 and 9.52%, respectively), whereas the percentage of patients with coronary angiography in both groups had the opposite results (35.94 and 77.78%, respectively). Moreover, brain CT or MRI abnormalities were found in most patients in both groups (68.83 and 62.00%, respectively).
Discussion
Contrast-induced encephalopathy is a rare and reversible complication that can cause neurotoxicity with a favorable prognosis and resolves within 24–48 h in most cases. Based on previous studies (Yan and Ramanathan, 2013; Spina et al., 2017; Cristaldi et al., 2021), the renal elimination of contrast medium, the regression of cerebral edema, and the recovery of BBB function were assumed to play an important role in the pathophysiology of neurological recovery. Here, we described a case of permanent neurological deficit after cerebral angiography and provided a summary and analysis of a series of CIE cases to explore the probable reasons for permanent neurological deficit. Given that most patients resolved completely within 48 h, we performed a prognostic analysis using 48 h as the node. We found that the total incidence of CIE between female patients and male patients had no difference, but female patients were more likely to have a poor prognosis. In addition, the average age of patients with poor prognoses was younger than that of patients with good prognoses. Surprisingly, no reports are currently available on risk factors associated with prognosis in patients with CIE. Only two reports were found to analyze the relationship between the incidence of CIE and gender or age, and the conclusions of the two reports were inconsistent. One report found that the adverse drug reaction incidence of iodinated contrast medium (e.g., CIE) seemed to be associated with gender, with a significantly higher incidence in female patients than in male patients, and it was also associated with age, with a lower occurrence in older (>44 years) patients compared to younger patients (Jiang et al., 2021). The other report summarized 9 CIE cases in 2013 and proposed that male gender and advanced age are the greatest risk factors for developing CIE. These two reports just provide a reference for us, and further research and a more in-depth analysis are necessary.
Studies showed a correlation between contrast medium dose and CIE (Yu and Dangas, 2011; Vigano et al., 2021), and whether the more contrast medium used is related to the poor prognosis of patients has not been directly reported. Although our study showed that the patients with poor prognosis used more contrast medium among different types of contrast media, including the non-ionic, ionic, low-osmolar, and high-osmolar contrast media, as well as the total contrast media used, the results are not absolute. Because in our reported case and 4 other summarized cases, the patient presented with permanent neurological deficits (more than 10 days) after administrating only a low quantity of contrast medium (no more than 50 ml) for angiography. Among these cases, the contrast medium types included non-ionic, low-osmolar, high- osmolar, and iso-osmolar, suggesting that severe neurotoxic symptoms may occur in response to low doses and different types of contrast agents. A previous study has shown that a 49-year-old man developed CIE and completely resolved within 4 h after receiving 610 ml diatrizoate (an ionic high-osmolar contrast medium) for diagnostic coronary angiography (Muruve and Steinman, 1996), indicating that high-dose contrast media do not cause permanent neurological dysfunction. Therefore, we speculated that, in addition to volume, the poor prognosis is generally related to the route and number of administrated, type of contrast medium, and individual patient characteristics.
Previous research has shown that demographic risk factors for CIE are chronic hypertension, diabetes mellitus, renal insufficiency, and previous reactions to contrast media (Yu and Dangas, 2011; Zhao et al., 2019; Cristaldi et al., 2021). Our study showed that the majority of patients (55.91%) had hypertension, 20.47% had diabetes mellitus, 15.75% had a contrast history, and 11.81% had renal insufficiency. Although there is no statistical difference between the poor prognosis group and the good prognosis group, these risk factors have a higher proportion in patients with poor prognosis, suggesting they may be related to worse prognosis, and further research is needed by increasing the sample size.
For the types of angiographic procedures, the present study showed that the proportion of patients with cerebral angiography was significantly higher in the poor-prognosis group than in the good-prognosis group, whereas patients with coronary angiography had the opposite results. Whether the cerebral angiography procedure itself is more likely to aggravate the prognosis than coronary angiography is unclear. This study demonstrated that 170 ml is recommended as the maximum threshold level of toxicity for coronary angiography procedure, and a smaller volume of contrast media may damage the BBB during selective intracranial injection (Kocabay et al., 2014), suggesting that cerebral angiography may be more likely to damage the BBB than coronary angiography. Furthermore, it is unclear whether procedure-related factors and patient-related factors are involved.
The diagnosis of CIE often requires the exclusion of cerebrovascular accidents such as cerebral hemorrhage and cerebral infarction. Neuroimaging plays an important role in distinguishing CIE from other neurological pathologies such as thromboembolism and hemorrhage following angiography. Our research showed that the most common abnormalities on brain CT included cortical or subcortical contrast enhancement, cerebral edema, focal hyperdense lesions, and hyper-density in the cerebral sulci. MRI abnormalities included hyperintensity on T2, FLAIR, and DWI. This study has suggested that CSF examination is also useful to rule out subarachnoid hemorrhage through the absence of xanthochromia or red blood cells (Shahan et al., 2021). The simultaneous detection of high concentrations of iodinated contrast medium in CSF and serum supports contrast medium extravasation rather than hemorrhage. In addition, the exclusion of contrast allergy or allergic-like reactions is also essential for the diagnosis of CIE. A recent study showed that allergic-like or allergic reactions caused by contrast media are rare, which can be severe or even life-threatening (Fusco et al., 2022). It is important to obtain a history of immediate or delayed reactions to a specific contrast medium, which may contribute to predicting the risk for future reactions. Clinical manifestations such as throat tightness, facial edema, and bronchospasm are helpful in distinguishing.
For the treatment of CIE, most patients with CIE have a good prognosis and a rapid recovery. Therefore, supportive care and observation are generally considered sufficient. Based on the literature summarized in the present study, it is recommended that appropriate hydration, steroids, and mannitol can be given immediately after surgery, and benzodiazepines can be used for epileptic seizures.
Conclusion
A contrast-induced encephalopathy is a form of neurotoxicity caused by contrast media that is usually transient but occasionally leads to permanent complications or death. We summarized a series of cases and found that the female gender, younger age, higher contrast medium dose, and cerebral angiography procedure were associated with poor prognosis in patients with CIE. However, the contrast medium types were not associated with the prognosis. In addition, there was no statistical difference between the poor prognosis group and the good prognosis group; hypertension, diabetes mellitus, renal insufficiency, and previous reactions to contrast media were also important risk factors for CIE. Our case and literature review highlight that CIE may not always have a benign outcome and has the potential to cause permanent neurological dysfunction, even with low-dose contrast media. We should not be overlooked, especially following procedures that use contrast medium.
Author contributions
YZ wrote the manuscript. JZ analyzed the data. HS and SY critically revised and edited the manuscript. All authors discussed the content and read and approved the final version.
Funding
This study was supported by the National Key Research and Development Program of China (2021YFC2501800) and the National Key Research and Development Program of China (2021YFC2501804).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- Andone S., Balasa R., Barcutean L., Bajko Z., Ion V., Motataianu A., et al. (2021). Contrast medium-induced encephalopathy after coronary angiography- case report. J. Crit. Care Med. 7 145–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babalova L., Ruzinak R., Ballova J., Sivak S., Kantorova E., Kurca E., et al. (2021). Contrast-induced encephalopathy. Bratisl. Lek. Listy 122 618–620. [DOI] [PubMed] [Google Scholar]
- Cristaldi P. M. F., Polistena A., Patassini M., de Laurentis C., Giussani C., Remida P. (2021). Contrast-induced encephalopathy and permanent neurological deficit: A case report and literature review. Surg. Neurol. Int. 12:273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dangas G., Monsein L. H., Laureno R., Peterson M. A., Laird J. R., Jr., Satler L. F., et al. (2001). Transient contrast encephalopathy after carotid artery stenting. J. Endovasc. Ther. 8 111–113. [DOI] [PubMed] [Google Scholar]
- Dattani A., Au L., Tay K. H., Davey P. (2018). Contrast-induced encephalopathy following coronary angiography with no radiological features: A case report and literature review. Cardiology 139 197–201. [DOI] [PubMed] [Google Scholar]
- de Bono D. (1993). Complications of diagnostic cardiac catheterisation: Results from 34,041 patients in the United Kingdom confidential enquiry into cardiac catheter complications. The joint audit committee of the british cardiac society and royal college of physicians of london. Br. Heart J. 70 297–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donepudi B., Trottier S. (2018). A seizure and hemiplegia following contrast exposure: Understanding contrast-induced encephalopathy. Case Rep. Med. 2018:9278526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernando T. G., Nandasiri S., Mendis S., Senanayake S., Gooneratne I. K., Navinan R., et al. (2020). Contrast-induced encephalopathy: A complication of coronary angiography. Pract. Neurol. 20 482–485. [DOI] [PubMed] [Google Scholar]
- Fusco A., Pucci L., Pierre K., Wolberg A., Small C., Cerillo J., et al. (2022). Contrast allergies for neurological imaging: When to proceed. AIMS Allergy Immunol. 6 216–227.36285334 [Google Scholar]
- García-Pérez D., Parra-Serrano J., Panero I., Moreno L. M., Campollo J., Alén J. F. (2021). Transient cortical blindness secondary to contrast-induced encephalopathy following diagnostic cerebral angiography: Report of 2 cases. Acta Neurol. Belg. 121 585–589. [DOI] [PubMed] [Google Scholar]
- Hamra M., Bakhit Y., Khan M., Moore R. (2017). Case report and literature review on contrast-induced encephalopathy. Future Cardiol. 13 331–335. [DOI] [PubMed] [Google Scholar]
- Harada Y., Kairamkonda S. R., Ilyas U., Pothineni N. V. K., Samant R. S., Shah V. A., et al. (2020). Pearls & Oy-sters: Contrast-induced encephalopathy following coronary angiography: A rare stroke mimic. Neurology 94 e2491–e2494. [DOI] [PubMed] [Google Scholar]
- Heemelaar J. C., van der Hoeven N. W., Muller F. F., Appelman Y. (2018). Acute-onset coma after iso-osmolar iodinated contrast injection: A case report of contrast-induced encephalopathy after elective coronary angiography. Eur. Heart J. Case Rep. 2:yty132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirata S., Koga M., Iseki H. (2018). Contrast-induced encephalopathy after coronary angioplasty in a patient with ST-elevation myocardial infarction. Heart Asia 10:e010987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang C., Li J., Huang Y., Huang D., Lin J., Jiang X. (2021). Clinical safety evaluation of contrast agents based on real-world evidence. J. Clin. Pharm. Ther. 46 1600–1605. [DOI] [PubMed] [Google Scholar]
- Kahyaoğlu M., Ağca M., Çakmak E., Geçmen Ç., Izgi I. A. (2018). Contrast-induced encephalopathy after percutaneous peripheral intervention. Turk Kardiyol. Dern. Ars. 46 140–142. [DOI] [PubMed] [Google Scholar]
- Kamimura T., Nakamori M., Imamura E., Hayashi Y., Matsushima H., Mizoue T., et al. (2021). Low-dose contrast-induced encephalopathy during diagnostic cerebral angiography. Intern. Med. 60 629–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kocabay G., Karabay C. Y., Kalayci A., Akgun T., Guler A., Oduncu V., et al. (2014). Contrast-induced neurotoxicity after coronary angiography. Herz 39 522–527. [DOI] [PubMed] [Google Scholar]
- Lei P., He W., Shi Q., Sun M., Sun Z. (2020). Recurrent epileptic seizures following cardiac catheterization with iodixanol: A case report. BMC Cardiovasc. Disord. 20:79. 10.1186/s12872-020-01341-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leong S., Fanning N. F. (2012). Persistent neurological deficit from iodinated contrast encephalopathy following intracranial aneurysm coiling. A case report and review of the literature. Interv. Neuroradiol. 18 33–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., Qi G., Zhang H., Chen G., Wang S., Yan M., et al. (2021). Contrast-induced encephalopathy mimicking stroke after a second cerebral DSA: An unusual case report. BMC Neurol. 21:430. 10.1186/s12883-021-02457-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu M. R., Jiang H., Li X. L., Yang P. (2020). Case report and literature review on low-osmolar, non-ionic iodine-based contrast-induced encephalopathy. Clin. Interv. Aging 15 2277–2289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muruve D. A., Steinman T. I. (1996). Contrast-induced encephalopathy and seizures in a patient with chronic renal insufficiency. Clin. Nephrol. 45 406–409. [PubMed] [Google Scholar]
- Nagamine Y., Hayashi T., Kakehi Y., Yamane F., Ishihara S., Uchino A., et al. (2014). Contrast-induced encephalopathy after coil embolization of an unruptured internal carotid artery aneurysm. Intern. Med. 53 2133–2138. [DOI] [PubMed] [Google Scholar]
- Park J. C., Ahn J. H., Chang I. B., Oh J. K., Kim J. H., Song J. H. (2017). A case of unusual presentation of contrast-induced encephalopathy after cerebral angiography using iodixanol. J. Cerebrovasc. Endovasc. Neurosurg. 19 184–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potsi S., Chourmouzi D., Moumtzouoglou A., Nikiforaki A., Gkouvas K., Drevelegas A. (2012). Transient contrast encephalopathy after carotid angiography mimicking diffuse subarachnoid haemorrhage. Neurol. Sci. 33 445–448. [DOI] [PubMed] [Google Scholar]
- Rashid H., Brown J., Nix E., Fisher Covin A. (2022). Contrast-Induced encephalopathy following diagnostic coronary angiography. Clin. Case Rep. 10:e05624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renault P., Rouchet S. (2019). Transient global amnesia and transient cortical blindness secondary to contrast induced encephalopathy after renal artery angiography. Rev. Neurol. 175 335–336. [DOI] [PubMed] [Google Scholar]
- Riahi L., Mediouni M., Messelmani M., Fehri W. (2019). A singular manifestation of contrast-induced encephalopathy following coronary angiography. Neurol. India 67 1525–1527. [DOI] [PubMed] [Google Scholar]
- Shahan B., Choi E. Y., Nieves G. (2021). Cerebrospinal fluid analysis. Am. Fam. Phys. 103 422–428. [PubMed] [Google Scholar]
- Şimşek E., Ertürk E., Uçar R., Yilmaz A. O., Ekmekçi C., Mutlu I., et al. (2019). Transient contrast neurotoxicity after percutaneous coronary intervention mimicking subarachnoid hemorrhage in a patient with chronic kidney disease. Clin. Med. Insights Case Rep. 12:1179547619867671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spina R., Simon N., Markus R., Muller D. W., Kathir K. (2017). Contrast-induced encephalopathy following cardiac catheterization. Catheter. Cardiovasc. Interv. 90 257–268. [DOI] [PubMed] [Google Scholar]
- Tong X., Hu P., Hong T., Li M., Zhang P., Li G., et al. (2018). Transient Cortical Blindness Associated with Endovascular Procedures for Intracranial Aneurysms. World Neurosurg. 119 123–131. [DOI] [PubMed] [Google Scholar]
- Vigano M., Mantero V., Basilico P., Cordano C., Sangalli D., Reganati P., et al. (2021). Contrast-induced encephalopathy mimicking total anterior circulation stroke: A case report and review of the literature. Neurol. Sci. 42 1145–1150. [DOI] [PubMed] [Google Scholar]
- Yan J., Ramanathan V. (2013). Severe encephalopathy following cerebral arteriogram in a patient with end-stage renal disease. Semin. Dial. 26 203–207. [DOI] [PubMed] [Google Scholar]
- Yao L. D., Zhu X. L., Yang R. L., Zhang M. M. (2021). Cardiorespiratory arrest after iso-osmolar iodinated contrast injection: A case report of contrast-induced encephalopathy following contrast-enhanced computed-tomography. Medicine 100:e24035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu J., Dangas G. (2011). Commentary: New insights into the risk factors of contrast-induced encephalopathy. J. Endovasc. Ther. 18 545–546. [DOI] [PubMed] [Google Scholar]
- Zhang W., Huang H., Jiang B., Liu Z. Y., He Y. (2021). Iopromide-induced encephalopathy: A case report and literature review. Sichuan Da Xue Xue Bao Yi Xue Ban 52 528–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao W., Zhang J., Song Y., Sun L., Zheng M., Yin H., et al. (2019). Irreversible fatal contrast-induced encephalopathy: A case report. BMC Neurol. 19:46. 10.1186/s12883-019-1279-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Z., Huang L., Chen J., Zhu H. (2021). Rapid contrast-induced encephalopathy after a small dose of contrast agent: Illustrative case. J. Neurosurg. Case Lessons 1:Case2052. [DOI] [PMC free article] [PubMed] [Google Scholar]