Background:
Coronavirus disease 2019, known as a widespread, aerosol spreading disease, has affected >549 000 000 people since 2019. During the lockdown period, dramatic reduction of elective endoscopic procedures, including endoscopic retrograde cholangiopancreatography, had been reported worldwide, leading to delayed diagnosis and treatment. Nevertheless, whether patients’ hospital stays and complication rate of endoscopic retrograde cholangiopancreatography (ERCP) during the lockdown period were influenced by the pandemic still remains controversial.
Methods:
Patients who diagnosed with obstructive jaundice and acute cholangitis in the lockdown period, May 16 to July 26, 2021, were compared to the same prepandemic period in 2019.
Results:
A total of 204 patients in 2019 and 168 patients in 2021 were diagnosed with acute biliary cholangitis or obstructive jaundice, and 82 of the patients in 2019 and 77 patients in 2021 underwent ERCP (p = 0.274). Patients whose quick Sequential Organ Failure Assessment (qSOFA) score was ≥ 2 occurred more during the lockdown period than during the normal period (24/77, 31.1% vs 12/82, 14.6%; p = 0.013). The initial laboratory data, including, total bilirubin (4.12 in 2021 vs 3.08 mg/dL in 2019; p = 0.014), gamma-glutamyl transferase (378 in 2021 vs 261 U/L in 2019; p = 0.009), and alkaline phosphatase (254 in 2021 vs 174 U/L in 2019; p = 0.002) were higher during the lockdown period compared to 2019. Hospital stay was statistically significant longer in the lockdown period (11 days [7.00–22.00] in 2021 vs 8 days in 2019 [6.00–12.00]; p value = 0.02). Multivariate analysis showed that qSOFA ≥ 2 (hazard ratio [HR] = 3.837, 95% confidence interval [CI] = 1.471–10.003; p = 0.006), and malignant etiology (HR = 2.932, 95% CI = 1.271–6.765; p = 0.012) were the statistically significant factors for a prolonged hospital stay, which was defined as hospital stay >21 days. ERCP-related complications and mortality rate were not statistically different between the two periods.
Conclusion:
Patients from May 16 to July 26, 2021, the lockdown period, had longer hospital stays and higher biliary tract enzyme levels, which indicated more severe disease. Nevertheless, ERCP could be safely and successfully performed even during the medical level 3 alert lockdown period without causing an increase in procedure-related complications and mortality.
Keywords: Coronavirus disease 2019, Endoscopic retrograde cholangiopancreatography, Endoscopic papillotomy, Quick Sequential Organ Failure Assessment
1. INTRODUCTION
Since late 2019 to July 2022, the coronavirus disease 2019 has affected >549 000 000 people and devastated approximately >6 000 000 people’s lives. The ravaging disease has changed people’s lives and behaviors in many aspects in addition to affecting the way clinical practice is being conducted. Invasive and high-risk procedures, such as endoscopic procedures that may spread aerosol droplets containing the coronavirus 2019 (COVID-19), have raised a great deal of concern about avoiding viral transmission during the pandemic.1–3 Elective procedures, such as esophagogastroduodenoscopy, colonoscopy, and endoscopic ultrasound, were reduced dramatically during the pandemic, particularly during the lockdown.2–6
Unlike other endoscopic procedures, endoscopic retrograde cholangiopancreatography (ERCP), which is considered an advanced endoscopic procedure that is used to treat biliary tract obstruction, is a relatively emergent intervention. Previous studies had been reported that ERCP cases reduced during the lockdown period. A delay in performing procedures may have occurred during lockdown periods.6–12 Whether patients’ hospital stays and complication rate of ERCP during the lockdown period were influenced by the pandemic, which still remains controversial.
Taiwan, unlike most other countries, had undertaken strict control of the spreading of this disease. Daily clinical practice was maintained until May 2021. An outbreak of COVID-19 was reported. A national level 3 alert13–16 was announced on May 16, 2021. Elective or scheduled medical service were scaled back because of the COVID-19 outbreak, and the alert was implemented nationwide under the command of National Health Command Center. Fortunately, the COVID-19 outbreak was controlled, and on July 26, 2021, the national level 3 alert was downgraded to level 2. The endoscopic center of Taipei Veterans General Hospital restored normal endoscopic service capacity as pre-COVID-19 era under a strict check of COVID-19 reverse-transcriptase polymerase chain reaction (RT-PCR) test before the procedures.
This study is aimed to study patients’ hospital stay and complication rates associated with ERCP during the lockdown period in Taiwan.
2. METHODS
2.1. Study population and design
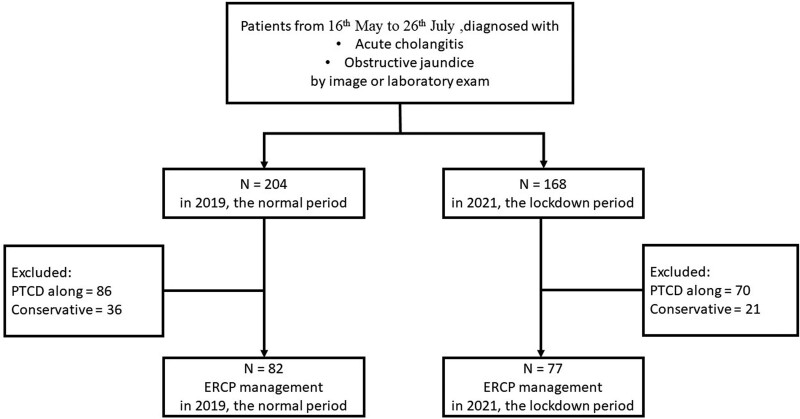
This study was a single Taiwanese tertiary center, retrospective, and cohort study. Patients with whose ages were ≥20 years and who had indications, including acute biliary cholangitis and obstructive jaundice, for undergoing ERCPs from May to July 26, 2021, were compared to the same prepandemic period in 2019 (Fig. 1). These specific intervals were chosen because that the Taiwanese government had announced national level 3 alert since May 16 to July 26, 2021. The pre-COVID era in 2019 was defined as the control group. This study was approved by the Institutional Review Board of Taipei Veterans General Hospital. Informed consent was waived because this study was retrospective.
Fig. 1.
Patient selection flowchart.
The initial clinical presentations were assessed using the quick Sequential Organ Failure Assessment (qSOFA) score. Laboratory test data including white blood cell (WBC) and neutrophil counts, hemoglobin (Hb) levels, platelet count, alanine transaminase (ALT), aspartate transaminase (AST), total and direct bilirubin levels, alkaline phosphatase (ALKP), gamma-glutamyl transferase (GGT), and C-reactive protein (CRP) were analyzed when patient initially presented to our hospital and before he she was discharges. Besides, hospital stays of the patients undergoing ERCP and the procedure-related complications during normal period, 2019, and the lockdown period, 2021, were compared.
2.2. ERCP procedures
Before undergoing ERCP, all patients were sedated with Midazolam (1–5 mg), Tramadol 100 mg. Fentanyl (0.025–0.1 mg) was administrated by doctors intravenously in a select population of those who were ≤80 years old, had a stable respiratory pattern, and stable vital signs. All ERCP procedures were performed with side viewing endoscopes (JF-260V or TJF-260V Olympus Optical Corporation).
2.3. Protective equipment
In 2019, before the COVID-19 pandemic, ERCPs were performed by endoscopists equipped with surgical masks, surgical gloves, and waterproof gowns. During the outbreak period in 2021, N95 masks, waterproof shoe covers, and facial shields were added to the list.
2.4. PCR test for COVID
All patients undergoing ERCPs were admitted for the procedure and further management. During the COVID-19 outbreak, the patient would undergo nasal swab test of COVID-19 for reverse-transcriptase polymerase chain reaction (RT-PCR). Once a result was negative, a patient was then allowed to have the endoscopic procedure at Taipei Veterans General Hospital. The COVID-19 RT-PCR test would take around 6 hours to yield the results. From May 16 to July 26, 2021, no patient nor ERCP staffs were diagnosed with COVID-19.
2.5. Statistical analyses
The case numbers, initial presentations, pre- and post-ERCP laboratory data, post-ERCP complications, time to ERCP, and hospital stays were analyzed. To compare the variables between 2019 and 2021, the Mann–Whitney U test and the chi-squared test were used to compare continuous and categorical variables, respectively. Cox regression was used to analyze the variable that may influence the Inpatient days in 2021. A Kruskal–Wallis test was used to compare lab data between different patient origins in 2021. A p value <0.05 indicated statistical significance. Statistical analysis was conducted using IBM SPSS version 25.0.
3. RESULTS
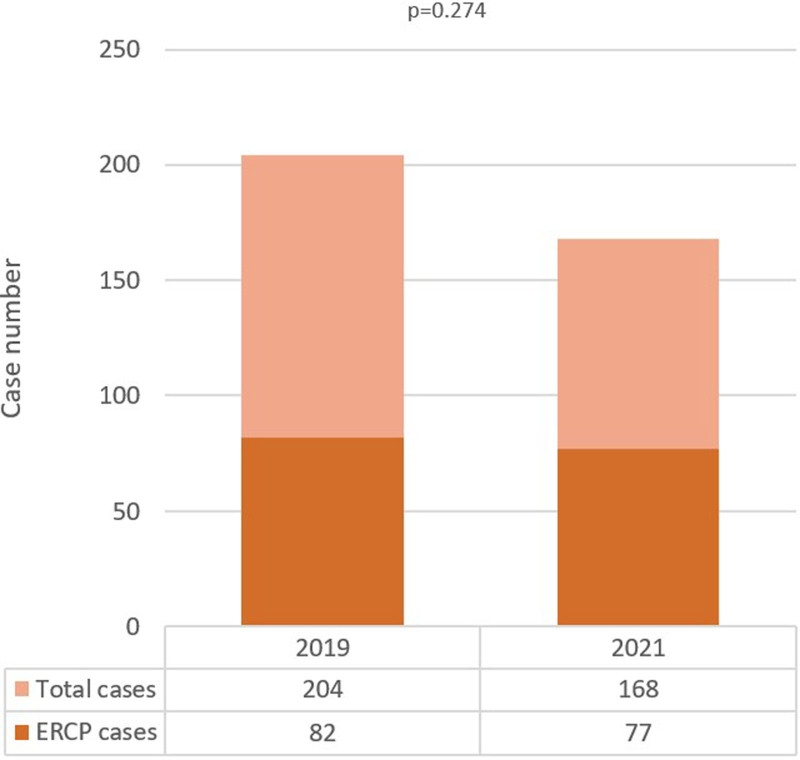
A total of 204 patients in 2019 and 168 patients in 2021 were diagnosed with acute biliary cholangitis or obstructive jaundice, and 82 of the patients in 2019 and 77 patients in 2021 underwent ERCP (p = 0.274, Fig. 2). Comparison of age, gender, and malignant etiologies between the two groups showed no statistically significant differences. More patients referred from other hospitals was found, eight patients (9.8%) in 2019 and 20 (26%) in 2021(p = 0.022). The rest of baseline characteristics are listed in Table 1.
Fig. 2.
Total case number and ERCP case number during the normal period and lockdown period. ERCP = endoscopic retrograde cholangiopancreatography.
Table 1.
Demographic data of patient undergoing ERCP during the normal and lockdown periods
| 2019 (the normal period) (n = 82) | 2021 (the lockdown period) (n = 77) | p | |
|---|---|---|---|
| Male (%) | 44 (53.7) | 42 (54.5) | 1 |
| Age, y (median [IQR]) | 67.50 (60.25, 77.00) | 69.00 (59.00, 82.00) | 0.492 |
| Charlson comorbidity index ≥ 2 (%) | 67 (81.7) | 64 (83.1) | 0.816 |
| Malignancy (%) | 9 (11.0) | 14 (18.2) | 0.287 |
| Diabetes mellitus (%) | 18 (22.0) | 23 (29.9) | 0.337 |
| Hypertension (%) | 35 (42.7) | 33 (42.9) | 1 |
| History of biliary stone (%) | 27 (32.9) | 29 (37.7) | 0.646 |
| Congestive heart failure (%) | 14 (17.1) | 16 (20.8) | 0.693 |
| COPD (%) | 2 (2.4) | 4 (5.2) | 0.621 |
| Chronic kidney disease (%) | 10 (12.2) | 7 (9.1) | 0.707 |
| Chronic liver disease (%) | 9 (11.0) | 8 (10.4) | 1 |
| Indications of ERCP | 0.573 | ||
| Biliary stone-related cholangitis | 68 (62.5) | 52 (67.5) | |
| Malignant obstructive jaundice | 8 (9.8) | 15 (19.5) | |
| Benign obstructive jaundice | 6 (7.3) | 10 (13.0) | |
| Procedure during ERCP | 0.153 | ||
| EPT (%) | 20 (24.4) | 27 (35.0) | |
| EPBD/EPLBD (%) | 36 (43.9) | 24 (31.2) | |
| Stent (%) | 12 (14.6) | 15 (19.5) | |
| Cannulation method | 0.569 | ||
| Selective catheter cannulation | 77 (93.9) | 74 (96.1) | |
| Guidewire-assisted | 1 (1.2) | 1 (1.2) | |
| Precut papillotomy | 4 (4.8) | 2 (2.6) | |
| Patient origin (%) | 0.022 | ||
| Emergent room | 56 (68.3) | 46 (59.7) | |
| Out-patient department | 18 (22.0) | 11 (14.3) | |
| Referral | 8 (9.8) | 20 (26.0) |
COPD = chronic obstructive pulmonary disease; EPT = endoscopic papillotomy; EPLBD = endoscopic papillary large balloon dilation; ERCP = endoscopic retrograde cholangiopancreatography; IQR= interquartile range.
The initial lab data, including blood urea nitrogen ([BUN] 15.00 in 2021 vs 11.5 mg/dL in 2019; p = 0.029), total bilirubin (4.12 in 2021 vs 3.08 mg/dL in 2019; p = 0.014), GGT (378 in 2021 vs 261 U/L in 2019; p = 0.009), and ALKP (254 in 2021 vs 174 U/L in 2019; p = 0.002) were higher during lockdown compared to the normal period in 2019. Patients whose qSOFA score was ≥2 occurred more during the lockdown period than during the normal period (24 patients [31.1%] in the lockdown periods versus 12 patients [14.6 %] in the normal period; p = 0.013). The detailed information is listed in Table 2.
Table 2.
Laboratory data and clinical presentation of patients undergoing ERCP during 2019 (the normal period) and 2021 (the lockdown period)
| 2019 (the normal period) (n = 82) | 2021 (the lockdown period) (n = 77) | p | |
|---|---|---|---|
| WBC (/µL) (median [IQR]) |
9200.00 [6140.00, 13 775.00] | 10 100.00 [7100.00, 14 000.00] | 0.227 |
| Hb (g/dL) (median [IQR]) |
13.10 [11.90, 14.67] | 13.10 [11.90, 14.20] | 0.461 |
| Plt (/µL) (median [IQR]) |
204 500.00 [159 250.00, 258 000.00] | 220 000.00 [164 000.00, 264 000.00] | 0.881 |
| BUN (mg/dL) (median [IQR]) |
11.50 [9.00, 14.00] | 15.00 [9.00, 23.00] | 0.029 |
| Cr (mg/dL ) (median [IQR]) |
0.94 [0.77, 1.15] | 0.86 [0.65, 1.15] | 0.184 |
| ALT (U/L) (median [IQR]) |
167.50 [60.00, 365.50] | 186.00 [98.00, 358.00] | 0.376 |
| AST (U/L) (median [IQR]) |
139.00 [49.00, 307.00] | 156.50 [73.25, 288.50] | 0.531 |
| Tbil (mg/dL) (median [IQR]) |
3.08 [1.23, 4.49] | 4.12 [2.17, 7.24] | 0.014 |
| GGT (U/L) (median [IQR]) |
261.00 [116.50, 467.75] | 378.00 [248.00, 595.00] | 0.009 |
| ALKP (U/L) (median [IQR]) |
174.00 [131.00, 301.00] | 254.00 [168.50, 393.00] | 0.002 |
| Lipase (median [IQR]) | 434.28 (1433.04) | 496.64 (1577.64) | 0.807 |
| CRP (mg/dL) (median [IQR]) |
4.77 [1.54, 8.50] | 6.16 [1.93, 13.07] | 0.055 |
| Acute kidney injury (%) | 15 (18.3) | 17 (22.1) | 0.691 |
| PTCD/PTGBD (%) | 12 (14.6) | 15 (19.5) | 0.547 |
| Pancreatitis (%) | 17 (20.7) | 17 (22.1) | 0.989 |
| qSOFA ≥ 2 (%) | 12 (14.6) | 24 (31.1) | 0.013 |
ALKP = alkaline phosphatase; ALT = alanine aminotransferase; AST = asparate aminotransferase; BUN = blood urea nitrogen; CRP = C-reactive protein; ERCP = endoscopic retrograde cholangiopancreatography; Hb = hemoglobin; PTCD = percutaneous transhepatic cholangiography and drainage; PTGBD = percutaneous transhepatic gallbladder drainage; qSOFA = quick Sequential Organ Failure Assessment; Tbil = total bilirubin; WBC = white blood cell count.
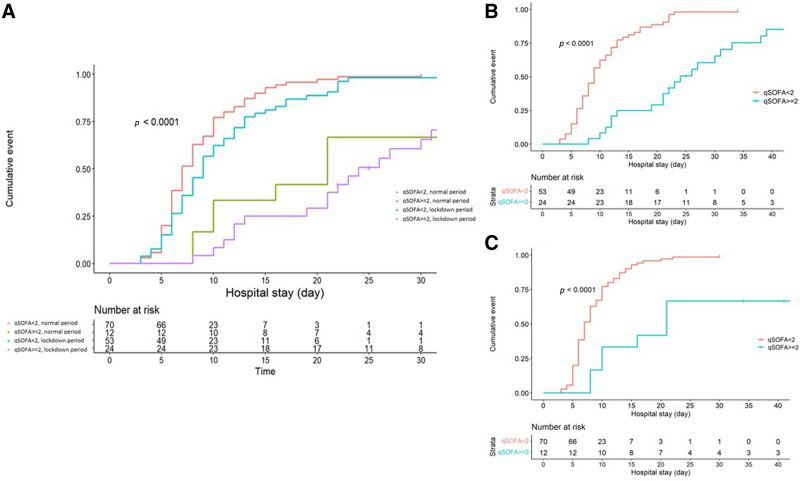
Time interval including from symptom onset to discharge was analyzed, Table 3. Only hospital stay showed statistically significant longer values in the lockdown period than in the normal period (11 days [7.00–22.00] vs 8 days [6.00–12.00]; p = 0.02, Fig. 3A).Cumulative incidence of discharge of patients during lockdown, stratified by qSOFA ≥ 2 showed at Fig. 3B, while the normal period was shown in Fig. 3C. Both periods showed the statistical significance of hospital stay when stratified by qSOFA score, p < 0.001.
Table 3.
Time intervals during the clinical course of patients undergoing ERCP during the normal period (2019) and lockdown period (2021)
| 2019 (the normal period) (n = 82) | 2021 (the lockdown period) (n = 77) | p | |
|---|---|---|---|
| Symptom onset to ER | 1.00 | 2.00 | 0.298 |
| (median [IQR]) | [0.00, 6.25] | [0.00, 6.00] | |
| ER registration to image evaluation | 0.50 | 0.00 | 0.15 |
| (median [IQR]) | [0.00, 2.00] | [0.00, 1.00] | |
| Image diagnosis to ERCP | 5.00 | 6.00 | 0.351 |
| (median [IQR]) | [4.00, 7.75] | [3.00, 11.00] | |
| Hospital admission to ERCP | 4.00 | 4.00 | 0.341 |
| (median [IQR]) | [3.00, 6.00] | [3.00, 8.00] | |
| Hospital stays (median [IQR]) | 8.00 | 11.00 | 0.002 |
| [6.00, 12.00] | [7.00, 22.00] |
ER = emergency room; ERCP = endoscopic retrograde cholangiopancreatography; IQR = interquartile range.
Fig. 3.
A, Cumulative incidence of discharge of the patient received ERCP during the normal and lockdown period, stratified by qSOFA ≥ 2. B, During 2019, the lockdown period. C, During 2021, the normal period. ERCP = endoscopic retrograde cholangiopancreatography; qSOFA = quick Sequential Organ Failure Assessment.
Multivariate analysis showed that qSOFA ≥ 2 (hazard ratio [HR] = 3.837, 95% confidence interval [CI] = 1.471–10.003; p = 0.006) and malignant etiology (HR = 2.932, 95% CI = 1.271–6.765; p = 0.012) were the statistically significant factors for a prolonged hospital stay, which is defined as hospital stay >21 days according to the local Health Ministry’s operational definition (Table 4).
Table 4.
Risk factors of prolonged hospital stay, defined as >21 days hospital stay
| Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|
| Variable | N | Hazard ratio | p | Hazard ratio | p |
| Lockdown period | 77/82 | 0.697 (0.304–1.599) | 0.395 | ||
| Y/N | |||||
| Gender | 86/73 | 1.298 (0.164–10.288) | 0.805 | ||
| M/F | |||||
| Referral | 28/131 | 0.824 (0.149–4.548) | 0.824 | ||
| Y/N | |||||
| Malignant etiology | 23/136 | 35.109 (2.017–611.034) | 0.015 | 2.932 (1.271–6.765) | 0.012 |
| Y/N | |||||
| qSOFA | 36/123 | 21.484 (3.557–129.751) | 0.001 | 3.837 (1.471–10.003) | 0.006 |
| ≥2/<2 | |||||
| Post-EPT bleeding | 5/154 | 0.172 (0.026–1.160) | 0.071 | ||
| Y/N | |||||
| Post-ERCP pancreatitis | 14/145 | 8.935 (0.134–593.675) | 0.306 | ||
| Y/N | |||||
| Charlson Comorbidity index ≥2/<2 | 131/28 | 67.284 (0.100–45192.978) | 0.205 | ||
| WBC (/10−9 L−1) | 1.031 (0.989–1.075) | 0.155 | |||
| BUN (mg/dL) | 1.011 (0.941–1.087) | 0.761 | |||
| Total bilirubin (mg/dL) | 0.839 (0.733–0.960) | 0.010 | 0.946 (0.895–1.000) | 0.051 | |
| GGT (mg/dL) | 1.003 (1.000–1.005) | 0.036 | |||
| ALKP (mg/dL) | 1.003 (0.999–1.007) | 0.156 | |||
| CRP (mg/dL) | 0.964 (0.883–1.054) | 0.422 | |||
BUN = blood urea nitrogen; ALKP = alkaline phosphatase; CRP = C-reactive protein; EPT = endoscopic papillotomy; ERCP = endoscopic retrograde cholangiopancreatography; GGT = gamma-glutamyl transferase; qSOFA = quick Sequential Organ Failure Assessment; WBC = white blood cell. .
Further analysis was conducted based on patients’ origin during the lockdown period in 2021. A total of 77 patients in 2021 were stratified into three groups: (1) patients admitted from the emergency room (ER), (2) those from the out-patient department (OPD), and (3) those referred from other hospitals. Forty-six patients (59.7%) were admitted from ER, 11 patients from OPD (14.3%), while 20 patients (26.0%) were referred from other hospitals. Patients referred from the OPD had longer hospital stay although it was not statistically different. More patients had a medical history of hepatobiliary tract malignancy compared patients referred from OPD to those who were admitted from ER or referred from other hospitals (90.90%, 17.39%, and 25%, respectively; p = 0.003). On the contrary, these patients had lower WBC and CRP level (p = 0.015 and p = 0.006, respectively). The detailed data are listed in Table 5.
Table 5.
Comparison of laboratory data according to patients’ origin during the lockdown period in 2021
| ER (n = 46) | OPD (n = 11) | Referral (n = 20) | p | |
|---|---|---|---|---|
| Malignant etiology (%) | 8 (17.39) | 10 (90.90) | 5 (25) | 0.003 |
| EPT (%) | 17 (36.9) | 3 (27.2) | 7 (35.0) | 0.833 |
| WBC (/µL) (median [IQR]) | 10 550.00 | 5900.00 | 11 100.00 | 0.015 |
| [7767.50, 14 000.00] | [4700.00, 8785.00] | [7175.00, 15 850.00] | ||
| Tbil (mg/dL) (median [IQR]) | 3.63 | 8.58 | 4.65 | 0.177 |
| [2.13, 6.11] | [2.42, 13.58] | [2.49, 8.02] | ||
| ALT (U/L) (median [IQR]) | 188.00 | 235.00 | 181.00 | 0.976 |
| [105.50, 359.25] | [76.00, 422.50] | [74.50, 339.25] | ||
| GGT (U/L) (median [IQR]) | 347.50 | 581.00 | 384.00 | 0.463 |
| [248.25, 566.75] | [281.50, 807.50] | [230.25, 572.75] | ||
| ALKP (U/L) (median [IQR]) | 258.00 [186.00, 376.00] |
442.00 [142.50, 531.00] |
188.00 [150.75, 284.00] |
0.263 |
| CRP (mg/dL) (median [IQR]) | 7.15 | 1.76 | 9.42 | 0.006 |
| [4.63, 13.41] | [0.47, 2.29] | [2.01, 16.28] | ||
| qSOFA ≥ 2 (%) | 14 (30.4) | 3 (27.2) | 7 (35.0) | 0.226 |
| Hospital stays (d) (median [IQR]) | 10.50 | 17.00 | 12.00 | 0.103 |
| [7.00, 19.50] | [8.00, 33.000] | [8.25, 26.00] |
BUN = blood urea nitrogen; ALKP = alkaline phosphatase; CRP = C-reactive protein; EPT = endoscopic papillotomy; ERCP = endoscopic retrograde cholangiopancreatography; GGT = gamma-glutamyl transferase; IQR= interquartile range; qSOFA = quick Sequential Organ Failure Assessment; WBC = white blood cell.
Post-ERCP complications including post-EPT bleeding, perforation, and post-ERCP pancreatitis were compared between 2019 and 2021. No statistical significance was revealed between these two periods in our study (Table 6).
Table 6.
Comparison of post-ERCP complications and cannulation failure rates between the normal period (2019) and lockdown period (2021)
| 2019 (the normal period) (n = 82) | 2021 (the lockdown period) (n = 77) | p | |
|---|---|---|---|
| Post-EPT bleeding (%) | 3 (3.7) | 2 (2.6) | 1 |
| Post-ERCP pancreatitis (%) | 5 (6.1) | 9 (11.7) | 0.335 |
| Perforation (%) | 0 (0) | 0 (0) | 1 |
| Cannulation failure rate (%) | 6 (7.3) | 3 (3.9) | 0.556 |
EPT = endoscopic papillotomy; ERCP = endoscopic retrograde cholangiopancreatography.
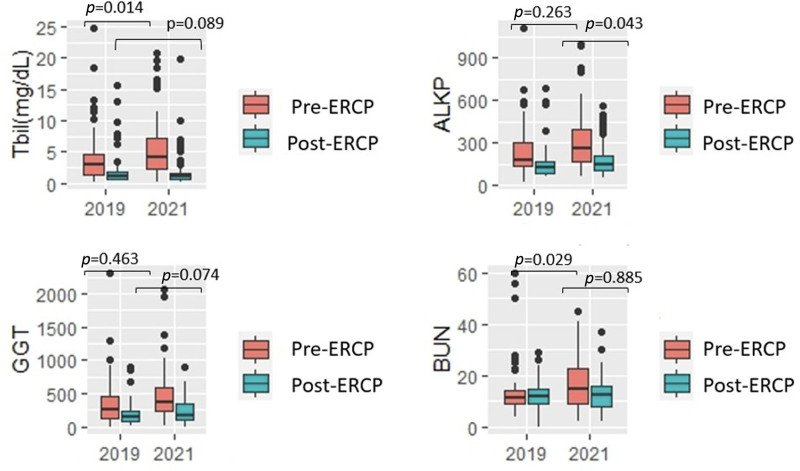
Post-treatment lab data before discharge showed no statistical difference between 2019 and 2021, except for ALKP, which was higher in 2021 rather than 2019 (144 vs 128 U/L; p = 0.043, Supplementary Table 1, http://links.lww.com/JCMA/A171). Biomarkers representing biliary tract and liver function improved after the treatment. The improvement in the total bilirubin level (1.94 mg/dL in 2019 vs 2.76 mg/dL in 2021; p = 0.018) was significantly higher in 2021 than that in 2019 (Fig. 4). Detailed data are listed in Supplementary Table 2, http://links.lww.com/JCMA/A171.
Fig. 4.
The improvement of laboratory examinations before and after ERCP during the lockdown and normal period. ERCP = endoscopic retrograde cholangiopancreatography.
4. DISCUSSION
During the pandemic era, especially the lockdown period, many previous studies reported a reduction in cases of endoscopic procedure including upper gastrointestinal endoscopy, colonoscopy, and endoscopic ultrasound. The reduction of elective endoscopic procedures was found to have led to the reduction in the malignancy detection rates,17,18 which may have delayed diagnosis and treatment.
Whether ERCP procedure would be delayed during the lockdown period seems to be controversial. One Italian study reported urgent EGD was significantly higher during the pandemic than before.3 Another retrospective study in Korea reported a significant reduction in ERCP during the pandemic.6 A similar result was obtained in a study from Ireland. However, another single-center retrospective study in Spain implied that no significant ERCP reduction during the pandemic had occurred, and the procedure could be performed safely even during the pandemic.11 Our study revealed no significant reduction in both patients diagnosed with acute cholangitis or obstructive jaundice and the patients receiving ERCP during the lockdown period, compatible with the previous study in Spain.
Time from symptom onset to hospital visit, hospital registration to image evaluation, and admission date to date of ERCP showed no differences between 2019 and 2021. The results implied that the medical evaluation and ERCP intervention were not delayed during the lockdown period. However, the hospital stay was longer in the lockdown period than in 2019, which might have indicated a more severe disease condition. The much higher total bilirubin, GGT, and ALKP level during the lockdown period could reflect this finding. More patients, whose qSOFA score ≥2, were noticed in the lockdown period than in the normal period in our study. Multivariate analysis also showed that qSOFA ≥2 and malignant etiology were statistically significant factors for a prolonged hospital stay, which was defined as hospital stay >21 days.
Although prolonged hospital stay was found in the lockdown period in our study, the complication and mortality rates were not different during the lockdown period.
Previous studies have been reported the incidences of ERCP complications. The incidence of post-ERCP pancreatitis is ranging from 2% to 16%.19–21 Post-EPT bleeding and perforation varied from 0.02% to 11% and 0.06% to 0.72%, respectively.21–23 Finally, the failure rate of cannulation is reported as ranging from 16% to 24%.24–26 The performance indicators, including cannulation and complication rates, were similar between 2019 and 2021 and compatible with the previous studies. In fact, in Taipei Veteran General Hospital, the preventive strategy of post-ERCP pancreatitis was not different during normal and lockdown periods. During both periods, preprocedure rectal indomethacin administration and pancreatic stenting were applied for the prevention of post-ERCP pancreatitis, especially for those who had risk factors of post-ERCP pancreatitis, including recurrent pancreatitis, difficult cannulation, or precut papillotomy. The fact implies that the procedure could be safely performed during the lockdown period. The result was concordant with the previous studies.6,14 Also, a more severe reduction of total bilirubin and CRP level in 2021 indicates that the procedure could efficiently manage the patients with the indications of ERCP during the lockdown period.
Further analysis based on patients’ origin was conducted. Our study found that patients who were referred from OPD tended to have malignant etiology and longer hospital stays than patients referred from ER or other hospitals. The patients from the OPD tended to have higher total bilirubin and biliary tract enzyme levels although this difference was not statistically significant. The patients from the OPD had more insidious and ambiguous symptoms, which may not obvious enough to urge the patient to seek for medical help immediately. This finding was compatible with the previous study, which reported higher total bilirubin and biliary tract enzyme in patients with obstructive jaundice induced by malignant etiology.27,28 On the other hand, patients from the ER or those referred from other hospital had higher qSOFA scores and inflammatory markers upon admission. These patients, having abrupt abdominal pain, fever, or gastrointestinal upset, would have sought medical help in a timely manner even during the lockdown period, leading to shorter hospital stays.
Several studies and guidelines have offered the endoscopist safe and efficient self-protection methods to performed endoscopic procedure.29,30 The more serious the clinical condition before the procedure and the more improvements of laboratory data after the procedure during the lockdown era suggests that the ERCP should not be delayed even during the medical lockdown period. Early referral to hospital equipped with ERCP equipment and timely ERCP intervention are highly suggested based on our analysis.
Our study has some limitations. First, small case numbers were a limitation since this study is a single-center observational study. For more case numbers, nationwide information is necessary. Second, although our analysis reports were no significant reduction in urgent ERCP case numbers, the real reduction in elective ERCP, since there was no document nor registration if patients canceled the procedure or doctors did not order the ERCP procedure during the lockdown period. The effects of reduction or delay of elective ERCP need more time to evaluate.
In conclusion, patients from May 16 to July 26, 2021, had longer hospital stays and higher biliary tract enzyme levels, which indicated more severe disease. Nevertheless, ERCP could be safely and successfully performed even during the medical level 3 alert lockdown period without causing an increase in procedure-related complications.
Footnotes
Conflicts of interest: Dr. Ming-Chih Hou, Dr. Yi-Hsiang Huang, and Dr. Fa-Yuah Lee, editorial board members at Journal of the Chinese Medical Association, have no roles in the peer-review process of or decision to publish this article. The authors declare that they have no conflicts of interest related to the subject matter or materials discussed in this article.
Supplementary data related to this article can be found at http://links.lww.com/JCMA/A171.
References
- 1.Chiriac S, Stanciu C, Cojocariu C, Sfarti C, Singeap AM, Girleanu I, et al. The impact of the COVID-19 Pandemic on gastrointestinal endoscopy activity in a tertiary care center from northeastern Romania. Healthcare 2021;19:100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mahadev S, Aroniadis OC, Barraza LH, Agarunov E, Smith MS, Goodman AJ, et al. Gastrointestinal endoscopy during the coronavirus pandemic in the New York area: results from a multi-institutional survey. Endo Inter Open 2020;8:E1865–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Salerno R, Conti CB, De Silvestri A, Campbell Davies SE, Mezzina N, Ardizzone S. The impact of COVID-19 pandemic on urgent endoscopy in Italy: a nation-wide multicenter study. Scand J Gastroenterol 2020;55:870–6. [DOI] [PubMed] [Google Scholar]
- 4.Lisotti A, Fusaroli P. EUS-guided gallbladder drainage during a pandemic crisis—How the COVID-19 outbreak could impact interventional endoscopy. Dig Liver Dis 2020;52:613–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang K, Zhao X, Chen X, Gao Y, Yu J, Wu L. Analysis of digestive endoscopic results during COVID-19. J Transl Int Med 2021;9:38–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim KH, Kim SB. Comparison of the impact of endoscopic retrograde cholangiopancreatography between pre-COVID-19 and current COVID-19 outbreaks in South Korea: retrospective survey. World J Clin Cases 2021;9:8404–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.An P, Huang X, Wan X, Xiao Y, Zhang J, Kang J, et al. ERCP during the pandemic of COVID-19 in Wuhan, China. Gastrointest Endosc 2020;92:448–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Donato G, Forti E, Mutignani M, Laterra M, Arese D, Coppola F, et al. A multicenter survey on endoscopic retrograde cholangiopancreatography during the COVID-19 pandemic in northern and central Italy. Endosc Int Open 2021;9:E629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Layton GR, Chung WY, Isherwood J, Fraser RE, Issa E, Robertson GS, et al. Endoscopic retrograde cholangiopancreatography in the COVID era: considerations for hepatobiliary and pancreatic surgery units. Br J Surg 2021;108:e290–1. [DOI] [PubMed] [Google Scholar]
- 10.Machicado JD, Papachristou GI, Cote GA, Wani S, Groce JR, Conwell DL, et al. Pancreaticobiliary endoscopy in the COVID-19 pandemic era. Pancreas 2020;49:729–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tag-Adeen M, Yousef M, Osman HA, Abdel-Gawad M, Elsayed Hassan M, Ozawa E, et al. Impact of Covid-19 pandemic on endoscopic retrograde cholangiopancreatography: a single center experience. Rev Esp Enferm Dig 2022;114:455–60. [DOI] [PubMed] [Google Scholar]
- 12.Voiosu T, Voiosu A, Boškoski I, Arvanitakis M, Bronswijk M, Hollenbach M, et al. Technical and clinical outcomes of endoscopic retrograde cholangiopancreatography (ERCP) procedures performed in patients with COVID-19. Therap Adv Gastroenterol 2020;13:1756284820980671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Central Epidemic Command Center. CECC raises epidemic alert level for Taipei City and New Taipei City to Level 3 and strengthens national restrictions and measures, effective from May 15 to May 28, in response to increasing level of community transmission. Available at https://www.cdc.gov.tw/En/Bulletin/Detail/R1K7gSjoYa7Wojk54nW7fg?typeid=158. Accessed December 13, 2021.
- 14.Central Epidemic Command Center. CECC raises epidemic warning to Level 3 nationwide from May 19 to May 28; strengthened measures and restrictions introduced across Taiwan to reduce community transmission. Available at https://www.cdc.gov.tw/En/Bulletin/Detail/VN_6yeoBTKhRKoSy2d0hJQ?typeid=158. Accessed December 13, 2021.
- 15.Central Epidemic Command Center. In response to community transmission stage of COVID-19, CECC announces four major medical response strategies to maintain medical capacities. Available at https://www.cdc.gov.tw/En/Bulletin/Detail/LXxH1ewYLBwoAF5D2GWE0A?typeid=158. Accessed December 13, 2021.
- 16.Central Epidemic Command Center. CECC to lower epidemic alert level to Level 2 from July 27 to August 9; CECC urges public to continue following epidemic prevention and control measures to protect health of people in Taiwan. Available at https://www.cdc.gov.tw/En/Bulletin/Detail/C--9A7siqyLWsca5Qb6npkA?typeid=158. Accessed December 13, 2021.
- 17.Calderwood AH, Calderwood MS, Williams JL, Dominitz JA. Impact of the COVID-19 pandemic on utilization of EGD and colonoscopy in the United States: an analysis of the GIQuIC registry. Tech Innov Gastrointest Endosc 2021;23:313–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Esmaily S, Yau CC, Dwarakanath D, Hancock J, Mitra V. Impact of COVID-19 pandemic on key performance indicators in pancreatobiliary endoscopy: prioritise, minimise risk, keep scoping and training. Frontline Gastroenterol 2020;12:288–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thaker AM, Mosko JD, Berzin TM. Post-endoscopic retrograde cholangiopancreatography pancreatitis. Gastroenterol Rep (Oxf) 2015;3:32–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bhatt H. Post-endoscopic retrograde cholangiopancreatography pancreatitis: an updated review of current preventive strategies. Clin Exp Gastroenterol 2021;14:27–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gondran H, Musquer N, Perez-Cuadrado-Robles E, Deprez PH, Buisson F, Berger A, et al. Efficacy and safety of endoscopic papillectomy: a multicenter, retrospective, cohort study on 227 patients. Therap Adv Gastroenterol 2022;15:17562848221090820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jang DK, Kim J, Paik CN, Kim JW, Lee TH, Jang JY, et al. Endoscopic retrograde cholangiopancreatography-related adverse events in Korea: a nationwide assessment. United European Gastroenterol J 2022;10:73–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Langerth A, Isaksson B, Karlson BM, Urdzik J, Linder S. ERCP-related perforations: a population-based study of incidence, mortality, and risk factors. Surg Endosc 2020;34:1939–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sheppard DP, Craddock SJ, Warner BD, Wilkinson ML. ERCP cannulation success benchmarking: implications for certification and validation. Frontline Gastroenterol 2015;6:141–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Peng C, Nietert PJ, Cotton PB, Lackland DT, Romagnuolo J. Predicting native papilla biliary cannulation success using a multinational endoscopic retrograde cholangiopancreatography (ERCP) quality network. BMC Gastroenterol 2013;13:147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liao WC, Angsuwatcharakon P, Isayama H, Dhir V, Devereaux B, Khor CJ, et al. International consensus recommendations for difficult biliary access. Gastrointest Endosc 2017;85:295–304. [DOI] [PubMed] [Google Scholar]
- 27.Vasilieva L, Alexopoulou A, Papadhimitriou SI, Romanos A, Xynopoulos D, Dourakis SP. Total bilirubin is a good discriminator between benign and malignant biliary strictures. HPB (Oxford) 2012;14:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Silina EV, Stupin VA, Abramov IS, Bolevich SB, Deshpande G, Achar RR, et al. Oxidative stress and free radical processes in tumor and non-tumor obstructive jaundice: influence of disease duration, severity, and surgical treatment on outcomes. Pathophysiology 2022;29:32–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Castro Filho EC, Castro R, Fernandes FF, Pereira G, Perazzo H. Gastrointestinal endoscopy during the COVID-19 pandemic: an updated review of guidelines and statements from international and national societies. Gastrointest Endosc 2020;92:440–5.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Repici A, Maselli R, Colombo M, Gabbiadini R, Spadaccini M, Anderloni A, et al. Coronavirus (COVID-19) outbreak: what the department of endoscopy should know. Gastrointest Endosc 2020;92:192–7. [DOI] [PMC free article] [PubMed] [Google Scholar]