Abstract
The induction of immune responses to rectally administered recombinant cholera toxin B subunit (CTB) in humans was studied. Three immunizations induced high levels of CTB-specific antibody-secreting cells, particular of the immunoglobulin A isotype, in both rectum and peripheral blood. Antitoxin antibody responses in rectal secretions and serum were also found.
Sexually transmitted diseases (STDs) are a major health problem in both industrialized and developing countries. Induction of a local mucosal immune response including the development of specific secretory immunoglobulin A (IgA) antibodies is important for protection against microorganisms that invade via mucosal surfaces (9, 19). One of the portals of entry for sexually transmitted pathogens such as the human immunodeficiency virus and herpes simplex virus is the mucus surface of the rectum. To provide specific protection against such pathogens, it is of great interest to develop immunization schemes that can induce specific immune responses including a strong IgA antibody response in the rectum (6, 10).
The aim of the present study was to assess the rectal immunization route for its ability to induce specific antibody-secreting cell (ASC) responses in suspensions of mononuclear cells (MNCs) from rectal tissues as well as from peripheral blood of healthy volunteers after rectal administration of cholera vaccine containing cholera toxin B subunit (CTB). CTB-specific antibodies in rectal secretions were also collected and analyzed along with antitoxin antibodies in serum.
Subjects and immunization.
The study was performed with due informed consent and ethical committee approval on eight healthy volunteers (three women), aged 20 to 44 years, who received three rectal immunizations with an inactivated B subunit-whole cell cholera vaccine, which is normally administered orally. The immunizations were given 2 weeks apart. The vaccine, containing 1.0 mg of recombinantly produced CTB and 1011 heat- and formalin-killed vibrios per 3-ml dose (SBL Vaccin, Stockholm, Sweden) (12), was administered by means of a rubber tube, 3 mm in diameter, inserted approximately 5 cm beyond the anus. After administration of the vaccine, the volunteers remained in horizontal position for 30 min.
Collection of specimens.
Rectal biopsies (eight persons), rectal secretions (five persons), and blood specimens (eight persons) were collected before the first immunization (day 0) and 7 days after the third vaccine dose. The rectal biopsies were obtained using a rigid sigmoidoscope and a standard flexible endoscope biopsy forceps (Olympus, Solna, Sweden). On each occasion, four to eight pinched biopsy samples 2 mm in diameter, were collected from rectum approximately 8 to 10 cm from the anus. Rectal secretions were collected before pinch biopsies. After insertion of the sigmoidoscope, each of four polywick tampons (2 by 25 mm; Polyfiltronics Inc., Rockland, Mass.), composed of a mixture of synthetic fibers and cellulose, was grasped with the forceps and carefully placed onto a relatively clean mucosal surface in the rectum approximately 12 to 15 cm from the anus. After 5 min, the tampons were collected with the forceps, and each tampon was placed in an Eppendorf tube. To extract proteins from the tampon, 200 μl of a buffer solution, containing enzyme inhibitors supplemented in 0.1% bovine serum albumin at concentrations previously specified (13), was added. Thereafter, the tubes were centrifuged at 10,000 × g for 2 min at 4°C in order to drive the fluid from the tampon. Supernatants were collected, pooled, and stored at −20°C until analyzed. For determination of circulating vaccine-specific ASC responses, 20 ml of heparinized venous blood was collected from all volunteers immediately before the first immunization and then 7 days after the last immunization. Serum specimens were obtained on the same occasions.
Detection of total and specific Ig-secreting cells.
Intestinal MNCs were isolated from the rectal biopsies using an enzymatic dispersion technique as previously described (20). A pool of four to eight biopsy samples from each individual yielded a mean of 2.7 × 105 viable MNCs (range, 0.9 × 105 to 5.9 × 105). MNCs from heparinized venous blood were isolated by standard gradient centrifugation on Ficoll-Isopaque (Pharmacia, Uppsala, Sweden). Rectal and peripheral blood MNC suspensions were assayed for numbers of total IgA- and IgG-secreting cells and CTB-specific IgA and IgG ASCs by a two-color micromodification (4) of the original enzyme-linked immunospot method (3, 22). Total Ig and CTB-specific Ig ASCs were expressed per 105 MNCs in the rectum and per 106 MNCs in peripheral blood. Vaccinees who had ≥5 CTB-specific ASCs per 105 MNCs in their rectal biopsy samples after vaccination were considered responders when no ASCs, i.e., <2.5 CTB-specific ASCs per 105 MNCs, could be detected prior to immunization. When the preimmune specimens (one case) contained >2.5 CTB-specific ASCs per 105 MNCs, a more than twofold increase in CTB-specific ASCs between pre- and postvaccination samples was considered a vaccine response. The corresponding figure for a response in peripheral blood was set at a postvaccination value of ≥5 CTB-specific Ig ASCs per 106 MNCs (5).
Antibody determinations.
The content of total IgA1 in rectal secretions was determined with an enzyme-linked immunosorbent assay (ELISA) method as previously described (24). Specific IgA (IgA1) antibody responses to cholera toxin in rectal secretions were measured by a GM1 ELISA method (23). The antibody titer was determined as the interpolated dilution of the specimen giving an absorbance value at 405 nm of 0.4 above background. The specific IgA antitoxin activities in rectal secretions were determined by dividing the IgA ELISA antibody titer by the total IgA concentration (micrograms per milliliter) of the sample to adjust for variations in the IgA content in specimens collected from different persons and on various days. A greater than twofold increase in the mean IgA antibody titer/total IgA between pre- and postimmunization specimens was regarded as a response (1). When preimmune specimens were missing (two cases), volunteers were considered responders if their postvaccination IgA antitoxin titer/total IgA exceeded by 2 standard deviations the geometric mean IgA antitoxin titer/total IgA in rectal secretions from seven other nonimmunized individuals.
Serum antibody responses of IgA and IgG classes to cholera toxin were measured by the GM1 ELISA method (23). A twofold or greater increase in endpoint titer between pre- and postvaccination specimens was used to signify seroconversion at a P value of <0.05 (11, 12).
Local immune responses in the rectum.
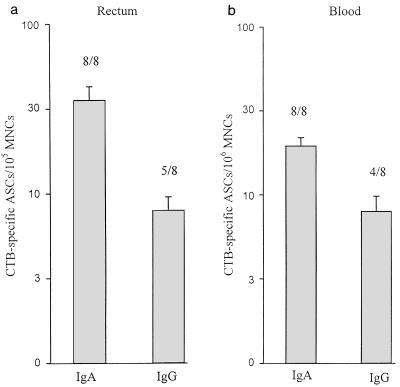
The frequencies of total IgA and IgG secreting cells were similar in rectal biopsy samples obtained before and after three rectal administrations of CTB (Table 1). Prior to immunization, no CTB-specific IgA or IgG ASCs were found in the rectum, except for one individual who had 5 IgG ASCs per 105 MNCs. The vaccination induced substantial increases in CTB-specific IgA ASCs in the rectum in each of the eight volunteers, with a geometric mean fold increase in ASCs of more than 14-fold (Table 1; Fig. 1a). Increases in CTB-specific IgG ASCs were also seen in five (63%) of the volunteers after vaccination, and the geometric mean fold rise in ASCs for these responders was more than fivefold (Table 1; Fig. 1a).
TABLE 1.
CTB-specific ASCs and total Ig-secreting cells in rectal biopsy samples from healthy volunteers before and 7 days after three rectal immunizations with recombinant CTBa
| Volunteer | No. of CTB-specific ASCs and total Ig-secreting cells/105 MNCs in the rectum
|
|||||||
|---|---|---|---|---|---|---|---|---|
| IgA
|
IgG
|
|||||||
| CTB specific
|
Total Ig
|
CTB specific
|
Total Ig
|
|||||
| Pre | Post | Pre | Post | Pre | Post | Pre | Post | |
| 1 | <2.5 | 30 | 11,000 | 12,800 | <2.5 | 15 | 4,000 | 4,800 |
| 2 | <2.5 | 32.5 | 18,000 | 20,000 | <2.5 | <2.5 | 120 | 40 |
| 3 | <2.5 | 10 | 16,000 | 9,000 | <2.5 | 20 | 1,000 | 1,000 |
| 4 | <2.5 | 22.5 | 5,600 | 5,000 | <2.5 | <2.5 | 1,000 | 800 |
| 5 | <2.5 | 50 | 9,000 | 8,000 | <2.5 | <2.5 | 200 | 100 |
| 6 | <2.5 | 250 | 5,000 | 4,000 | 5 | 25 | 1,500 | 1,000 |
| 7 | <2.5 | 37.5 | 10,000 | 12,000 | <2.5 | 25 | 3,000 | 5,000 |
| 8 | <2.5 | 25 | 12,000 | 15,000 | <2.5 | 5 | 3,500 | 4,000 |
Pre and post, pre- and postimmunization.
FIG. 1.
Levels of CTB-specific IgA and IgG ASCs in the rectum (a) and peripheral blood (b) of healthy volunteers 7 days after three rectal administrations of recombinant CTB. The geometric mean numbers of vaccine-specific ASCs + 1 standard error of the mean are shown.
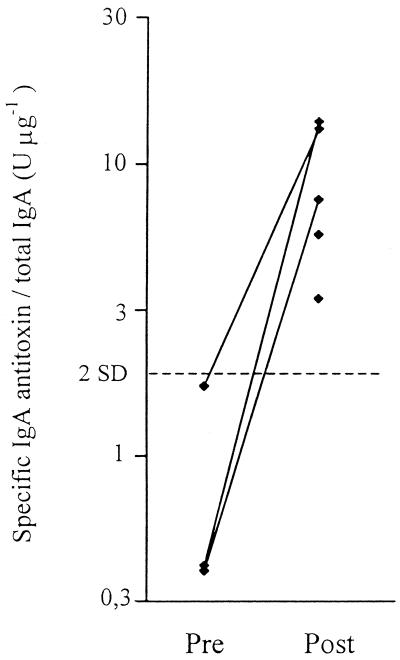
The local immune response in the rectum was also measured as CTB-specific IgA (IgA1) antibodies in secretions from the rectal surface collected by using a tampon method (16). This method was shown to give a yield of IgA antibodies high enough to allow detection of vaccine-specific IgA antibodies in sample eluates. A total of eight secretions collected from five volunteers (preimmune specimens were missing in two cases) contained as a mean 200 μg of total IgA ml−1 (range, 18 to 501 μg ml−1). All of the five volunteers responded to the rectal immunization with increases in CTB-specific IgA antibody titer/total IgA in rectal secretions (Fig. 2).
FIG. 2.
Intestinal IgA (IgA1) antitoxin levels in rectal secretions collected from five volunteers before (Pre) and 7 days after (Post) three rectal administrations of recombinant CTB. The dotted line denotes the geometric mean IgA antitoxin titer/total IgA in rectal secretions from seven nonimmunized individuals. Preimmune specimens were missing for two vaccinees.
Immune responses in blood.
Monitoring of different homing receptors on circulating ASCs indicates that especially ASCs of the IgA isotype, assayed approximately 7 days after oral or rectal vaccination, almost exclusively represent cells of the intestinal immune system (15). Prior to immunization, the number of circulating CTB-specific IgA and IgG ASCs were negligible (≤1 ASC × 106 MNCs). All of the eight volunteers responded with increased numbers of CTB-specific IgA ASCs in blood after three rectal administrations of CTB (Table 2), with a geometric mean fold increase of more than 19-fold (Fig. 1b). Increased levels of circulating IgG ASCs against CTB were also found in four (50%) of the volunteers after vaccination (Table 2; Fig. 2), and the mean fold increase in ASCs for these responders was more than 27-fold. There were also significant increases in serum IgA antitoxin titers in six (75%) of eight volunteers after three rectal doses of CTB, and seven (88%) of the vaccinees developed IgG antitoxin responses too (Table 2). Among responders, these increases in antitoxin were 7.6-fold for IgA and 4.4-fold for IgG.
TABLE 2.
CTB-specific ASCs and total Ig-secreting cells in peripheral blood and antitoxin antibodies in serum in healthy volunteers before and 7 days after three rectal immunizations with recombinant CTBa
| Volunteer | No. of CTB-specific ASCs and total Ig-secreting cells/106 MNCs in blood
|
Antitoxin antibodies in serum
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| IgA
|
IgG
|
IgA
|
IgG
|
|||||||||
| CTB-specific
|
Total Ig
|
CTB-specific
|
Total Ig
|
Pre | Post | Pre | Post | |||||
| Pre | Post | Pre | Post | Pre | Post | Pre | Post | |||||
| 1 | <1 | 23 | 220 | 400 | <1 | 15 | 300 | 400 | 5 | 69 | 14 | 195 |
| 2 | <1 | 30 | 350 | 500 | <1 | <1 | 280 | 350 | 5 | 11 | 58 | 148 |
| 3 | <1 | 15 | 180 | 350 | <1 | 50 | 400 | 700 | 3 | 135 | 40 | 339 |
| 4 | <1 | 14 | 500 | 700 | <1 | 4 | 500 | 500 | 4 | 32 | 47 | 112 |
| 5 | 1 | 20 | 750 | 480 | <1 | 2 | 150 | 200 | 35 | 93 | 52 | 112 |
| 6 | <1 | 10 | 300 | 180 | 1 | 4 | 280 | 360 | 7 | 56 | 49 | 347 |
| 7 | <1 | 40 | 200 | 260 | <1 | 28 | 650 | 800 | 22 | 33 | 68 | 91 |
| 8 | <1 | 18 | 150 | 200 | <1 | 24 | 480 | 730 | 589 | 603 | 85 | 269 |
Pre and post, pre- and postimmunization.
The individual ASC responses to CTB in peripheral blood were compared with corresponding ASC responses in the rectum. A significant correlation between the magnitudes of CTB-specific ASCs in the rectum and in blood was found for IgG (r = 0.71; P < 0.01), whereas no such correlation was observed for IgA ASCs.
In conclusion, the results presented show that the human rectal mucosa can serve as an efficient site for both the induction and expression of local mucosal IgA and IgG antibody responses. The substantial increases in specific IgA antibodies in rectal secretions were consistent with results obtained after repeated rectal immunizations with inactivated cholera vaccine (16) or live Salmonella enterica serovar Typhi Ty21a vaccine (15). The magnitudes of the CTB-specific IgA and IgG responses, in terms of both specific ASCs in rectal biopsies and antibodies in rectal secretions, were similar to those to CTB in the small intestine reported after oral cholera vaccination (13, 18, 21). The appearance of specific IgA and IgG ASCs in blood after rectal immunization with CTB was also in accordance with results obtained in humans after oral or rectal immunization with S. enterica serovar Typhi Ty21a vaccine (8, 15).
CTB was chosen as the immunogen in our studies for several reasons: (i) CTB is a well-defined potent mucosal immunogen, which has been used in several previous studies of mucosal immune responses, especially within the gastrointestinal tract (13, 16, 18, 21); (ii) CTB can be safely administered to humans in the form of a registered oral cholera vaccine (12, 13); and (iii) CTB has in animals been shown to serve as an effective carrier molecule for enhancing the mucosal immunogenicity of various antigens linked chemically or genetically to CTB (2, 7, 14, 17). The latter finding together with the present results suggests that rectal immunization with CTB, and probably also with other antigens linked to CTB, could work well to elicit local mucosal IgA and IgG immune responses and thus allow for effective mucosal immunization of the rectal portal of entry for specific STD pathogens. These findings should be relevant for the development of vaccines against human immunodeficiency virus infection as well as other STDs.
REFERENCES
- 1.Åhrén C, Wennerås C, Holmgren J, Svennerholm A-M. Intestinal antibody response after oral immunization with a prototype cholera B subunit-colonization factor antigen enterotoxigenic Escherichia coli vaccine. Vaccine. 1993;11:929–934. doi: 10.1016/0264-410x(93)90380-g. [DOI] [PubMed] [Google Scholar]
- 2.Bergquist C, Lagergård T, Lindblad M, Holmgren J. Local and systemic antibody responses to dextran-cholera toxin B subunit conjugates. Infect Immun. 1995;63:2021–2025. doi: 10.1128/iai.63.5.2021-2025.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Czerkinsky C, Nilsson L-, Nygren H, Ouchterlony Ö, Tarkowski A A. Solid-phase enzyme-linked immunospot (ELISPOT) assay for enumeration of specific antibody-secreting cells. J Immunol Methods. 1983;65:109–121. doi: 10.1016/0022-1759(83)90308-3. [DOI] [PubMed] [Google Scholar]
- 4.Czerkinsky C, Moldoveanu Z, Mestecky J, Nilsson L-, Ouchterlony Ö. A novel two colour ELISPOT assay. Simultaneous detection of distinct types of antibody-secreting cells. J Immunol Methods. 1988;115:31–37. doi: 10.1016/0022-1759(88)90306-7. [DOI] [PubMed] [Google Scholar]
- 5.Czerkinsky C, Svennerholm A-M, Quiding M, Jonsson R, Holmgren J. Antibody-producing cells in peripheral blood and salivary glands after oral cholera vaccination of humans. Infect Immun. 1991;59:996–1001. doi: 10.1128/iai.59.3.996-1001.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Czerkinsky C, Anjuere F, McGhee J R, George-Chandy A, Holmgren J, Kieny M P, Fujiyashi K, Mestecky J F, Pierrefite-Carle V, Rask C, Sun J B. Mucosal immunity and tolerance: relevance to vaccine development. Immunol Rev. 1999;170:197–222. doi: 10.1111/j.1600-065X.1999.tb01339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Drew M D, Estrada-Correa A, Underdown B J, McDermott M R. Vaccination by cholera toxin conjugated to a herpes simplex virus type 2 glycoprotein D peptide. J Gen Virol. 1992;73:2357–2366. doi: 10.1099/0022-1317-73-9-2357. [DOI] [PubMed] [Google Scholar]
- 8.Forrest B D, Shearman D J C, LaBrooy J T. Specific immune response in humans following rectal delivery of live typhoid vaccine. Vaccine. 1990;8:209–212. doi: 10.1016/0264-410x(90)90047-p. [DOI] [PubMed] [Google Scholar]
- 9.Holmgren J, Rudin A. Mucosal immunity and bacteria. In: Ogra P L, Mestecky J, Lamm M E, Strober W, Bienenstock J, McGhee J R, editors. Mucosal immunology. 2nd ed. San Diego, Calif: Academic Press; 1999. pp. 685–693. [Google Scholar]
- 10.Hook E W, III, Pate M S, Hedges S R, Russell M W, Mestecky J. Mucosal immunology of sexually transmitted diseases. In: Ogra P L, Mestecky J, Lamm M E, Strober W, Bienenstock J, McGhee J R, editors. Mucosal immunology. 2nd ed. San Diego, Calif: Academic Press; 1999. pp. 1463–1481. [Google Scholar]
- 11.Jertborn M, Svennerholm A-M, Holmgren J. Saliva, breast milk, and serum antibody responses as indirect measures of intestinal immunity after oral cholera vaccination or natural disease. J Clin Microbiol. 1986;24:203–209. doi: 10.1128/jcm.24.2.203-209.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jertborn M, Svennerholm A-M, Holmgren J. Safety and immunogenicity of an oral recombinant cholera B subunit-whole cell vaccine in Swedish volunteers. Vaccine. 1992;2:130–132. doi: 10.1016/0264-410x(92)90030-n. [DOI] [PubMed] [Google Scholar]
- 13.Jertborn M, Svennerholm A-M, Holmgren J. Intestinal and systemic immune responses in humans after oral immunization with a bivalent B subunit-01/0139 whole cell cholera vaccine. Vaccine. 1996;14:1459–1465. doi: 10.1016/s0264-410x(96)00071-0. [DOI] [PubMed] [Google Scholar]
- 14.Johansson E-L, Rask C, Fredriksson M, Eriksson K, Czerkinsky C, Holmgren J. Antibodies and antibody-secreting cells in the female genital tract after vaginal or intranasal immunization with cholera toxin B subunit or conjugates. Infect Immun. 1998;66:514–520. doi: 10.1128/iai.66.2.514-520.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kantele A, Häkkinen M, Moldoveanu Z, Lu A, Savilahti E, Alvarez R D, Michalek S, Mestecky J. Differences in immune responses induced by oral and rectal immunizations with Salmonella typhi Ty21a: evidence for compartmentalization within the common mucosal immune system in humans. Infect Immun. 1998;66:5630–5635. doi: 10.1128/iai.66.12.5630-5635.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kozlowski P A, Cu-Uvin S, Neutra M R, Flanigan T P. Comparison of the oral, rectal, and vaginal immunization routes for induction of antibodies in rectal and genital tract secretions of women. Infect Immun. 1997;65:1387–1394. doi: 10.1128/iai.65.4.1387-1394.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lehner T, Bergmeier L A, Panagiotidi C, Tao L, Brookes R, Klavinskis L S, Walker P, Ward J, Ward R D, Hussain L, et al. Induction of mucosal and systemic immunity to a recombinant simian immunodeficiency viral protein. Science. 1992;258:1365–1369. doi: 10.1126/science.1360702. [DOI] [PubMed] [Google Scholar]
- 18.Mattsson A, Lönroth H, Quiding-Järbrink M, Svennerholm A-M. Induction of B-cell responses in the stomach of Helicobacter pylori-infected subjects after oral cholera vaccination. J Clin Investig. 1998;102:51–56. doi: 10.1172/JCI22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Murphy B R. Mucosal immunity to viruses. In: Ogra P L, Mestecky J, Lamm M E, Strober W, Bienenstock J, McGhee J R, editors. Mucosal immunology. 2nd ed. San Diego, Calif: Academic Press; 1999. pp. 695–707. [Google Scholar]
- 20.Nordström I, Quiding M, Kjellson B, Kilander A, Ahlfors E, Holmgren J, Czerkinsky C. Thermolysin treatment: an improved dispersion technique for isolating functional lymphoid cells from human intestinal tissues. In: McDonalds T T, Challacombe S J, Bland P W, Stokes C R, Heatley R V, Mowoat A M, editors. Advances in mucosal immunology. Dordrecht, The Netherlands: Kluwer Academic Publishers; 1990. pp. 103–104. [Google Scholar]
- 21.Quiding M, Nordström I, Kilander A, Andersson G, Hanson L Å, Holmgren J, Czerkinsky C. Oral cholera vaccination induces strong intestinal antibody responses and interferon-γ production and evokes local immunological memory. J Clin Investig. 1991;88:143–148. doi: 10.1172/JCI115270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sedgwick J D, Holt P G. A solid-phase immunoenzymatic technique for the enumeration of specific antibody-secreting cells. J Immunol Methods. 1983;57:301–309. doi: 10.1016/0022-1759(83)90091-1. [DOI] [PubMed] [Google Scholar]
- 23.Svennerholm A-M, Holmgren J, Black R, Levine M, Merson M. Serologic differentiation between antitoxin responses to infection with Vibrio cholerae and enterotoxin-producing Escherichia coli. J Infect Dis. 1983;147:514–522. doi: 10.1093/infdis/147.3.514. [DOI] [PubMed] [Google Scholar]
- 24.Vincent C, Cozon G, Zittoun M, Mellquist M, Kazatchkine M D, Czerkinsky C, Revillard J-P. Secretory immunoglobulins in serum from human immunodeficiency virus (HIV)-infected patients. J Clin Immunol. 1992;12:381–388. doi: 10.1007/BF00920796. [DOI] [PubMed] [Google Scholar]