ABSTRACT
Background
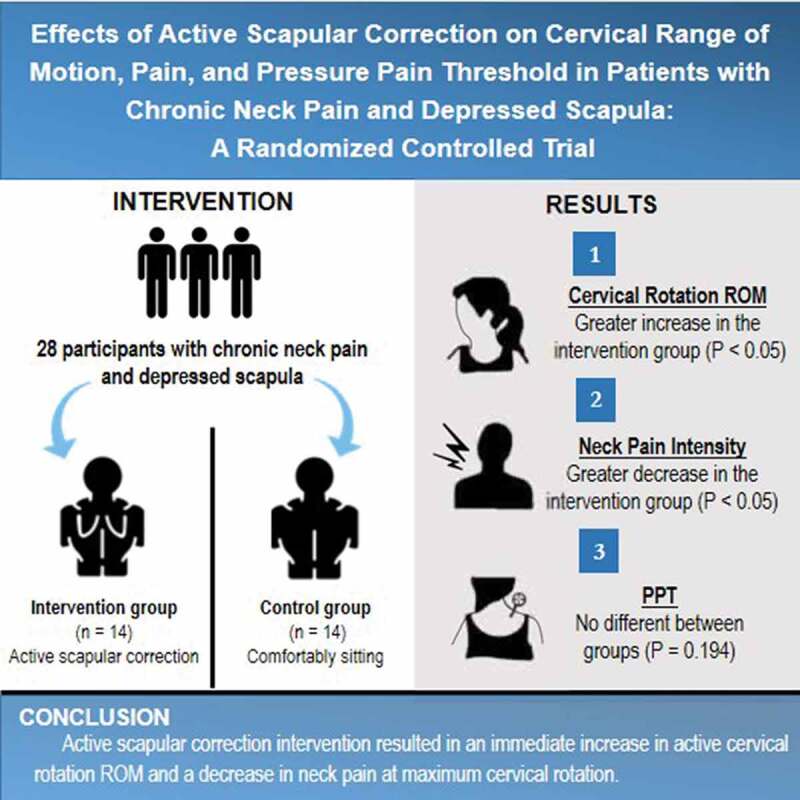
Correction of scapular alignment is advocated as a component for alleviating symptoms for patients with neck pain.
Objective
The study aimed to examine the effect of active scapular correction on cervical range of motion (ROM), pain, and pressure pain threshold (PPT) in patients with chronic neck pain with depressed scapula.
Methods
A randomized control trial research design was conducted. Twenty-eight participants with chronic neck pain and depressed scapula were randomly assigned to either the intervention (n = 14) or control (n = 14) group. Active cervical rotation ROM, pain at maximum cervical rotation, and PPT over the upper trapezius muscle region were measured at baseline and post active scapular correction.
Results
The participants in the intervention group showed significantly greater active cervical rotation ROM and less pain at maximum cervical rotation than the control group, both on the ipsilateral (p < 0.01) and contralateral (p < 0.05) sides of the depressed scapula. No significant difference in PPT between the groups was demonstrated (p = 0.194).
Conclusion
Active scapular correction intervention resulted in an immediate increase in active cervical rotation ROM and a decrease in neck pain at maximum cervical rotation.
KEYWORDS: Exercise, neck pain, scapula
Graphical Abstract
Introduction
Neck pain is one of the most common musculoskeletal problems with a 1-year prevalence that varies from 15.3% to 37.0% in the general population [1–3]. The chronic rate is high, with an estimated 30% of neck pain patients suffering from chronic symptoms [4]. Neck pain and its complications also have a significant impact on public health expenditure both directly and indirectly [4].
The relationships between impairment in scapular alignment and cervical disorders have been described [5]. The impaired alignment can be classified as depressed, elevated, downwardly rotated, abducted, adducted, tilted, and winged scapular position [6]. The prevalence of each type of scapular position remains unknown, but a recent study of individuals with nonspecific neck pain has found that about 60% of participants has downwardly rotated scapula and all participants have at least one type of impaired scapular position [7]. To date, depressed scapula position has received attention from several studies [8–12].
Depressed scapular position is defined as having the acromion process and the superior angle of the scapula located below the spinous process of the second thoracic vertebra10. Tension of the cervicoscapular muscles that connect the scapula to the cervical region (upper trapezius and levator scapulae) in a lengthened position might put load on the cervical spine, which can adversely affect mechanical stresses on pain sensitive cervical structures13. Upper limb neural tissue mechanosensitivity is significantly greater in healthy subjects who display depressed scapula compared with those with normal scapular orientation [8]. Significantly lower pressure pain threshold (PPT) over the upper trapezius [8,10] and middle trapezius muscles11 as well as over the C2/C3 and C5/C6 zygapophyseal joints [8] is reported in healthy subjects with depressed scapula position. Correction of scapular alignment is therefore advocated as a component of intervention for patients with neck pain who also exhibit depressed scapular alignment [9,12].
Correction of the scapular position can be performed passively and actively. Passive intervention uses a manual technique or a mechanical device, while active intervention asks an individual to move the scapula into a neutral position and hold the position steadily for a short period. The passive intervention technique is commonly performed and results in an immediate decrease in neck pain intensity associated with cervical rotation and an increase in active cervical rotation range of motion (ROM) [7,13,14], as well as a reduction in joint position error14,15. An active intervention technique was investigated in two studies. One study examined healthy subjects with depressed scapula. It showed a significant increase in PPT over the upper trapezius muscle after intervention [12]. The other study investigated patients with neck pain and abnormal scapular posture, which demonstrated changes in electromyographic activity in the middle trapezius and the lower trapezius muscle toward normal while performing scapular correction15. However, active scapular correction showed greater reduction in pain and greater increase in PPT at the most painful cervical segment in patients with chronic neck pain16. These results suggest a plausible benefit of active scapular correction, which may be used as a self-exercise in the management of neck pain, although no data on neck pain with cervical movement, cervical ROM, and PPT over the upper trapezius muscle in individuals with neck pain have been reported.
The purposes of this study were twofold. First, to compare cervical rotation ROM, neck pain with cervical rotation, and PPT over the upper trapezius muscle region between the groups that performed active scapular correction exercise and the control group. Second, to assess the immediate effects of active scapular correction on cervical rotation ROM, neck pain with cervical rotation, and PPT over the upper trapezius muscle region in participants with chronic neck pain and depressed scapular alignment.
Methods
Study design
A randomized control trial with blinded outcome assessment was conducted. The study was registered with the Thai Clinical Trial Registry (TCTR 20210123003) and was approved by the Ethics and Research Committee of Chulalongkorn University (COA No. 115.1/63). The full trial protocol can be accessed at http://www.thaiclinicaltrials.org/. The flow chart in Figure 1 gives an overview of the participant flow of the study according to the CONSORT standard (http://www.consort-statement.org/). Participants were recruited from the faculty clinic patients, as well as those using flyers posted at the university and on social networks. Recruitment started in September 2020 and the last participant was recruited in November 2020. Informed consent was obtained from all participants prior to enrollment in the study. Data collection was performed at the laboratory of the Faculty of Allied Health Sciences, Chulalongkorn University.
Figure 1.
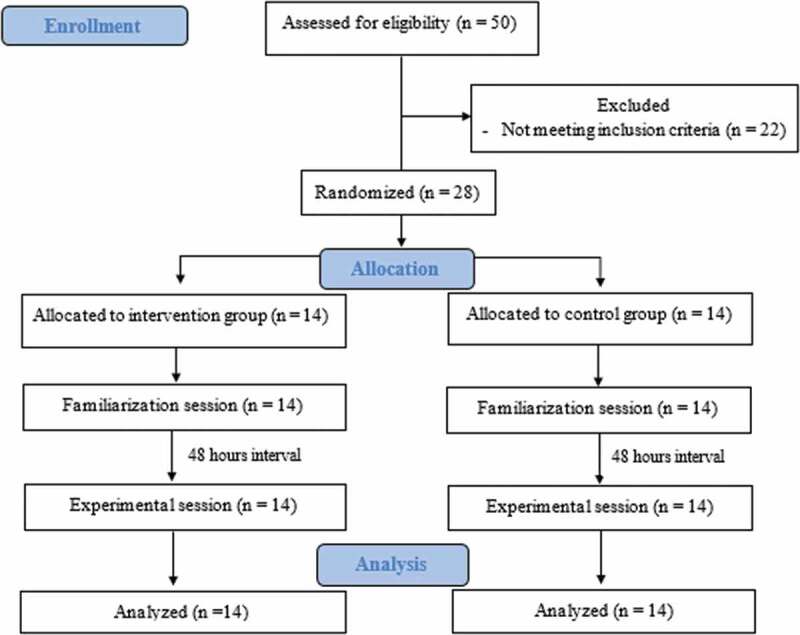
CONSORT flow diagram of the participants.
Participants
Twenty-eight participants (18 females and 10 males) with a history of chronic neck pain and depressed scapula participated in the study. Neck pain was defined as pain in the area between the superior nuchal line and the tip of the first thoracic spinous process that had persisted longer than three months in duration. A depressed scapula could be either unilateral or bilateral. Participants with unilateral neck pain had to have depressed scapula on the same side of the neck pain symptom. Each participant had his or her scapulae assessed by a researcher while standing with both arms relaxed by their sides. A depressed scapula is commonly defined as having the acromion process and the superior angle of the scapula below the second thoracic spinous process10. In the present study, a scapula was classified as depressed when the acromion process and the superior angle of scapula were at or below the third thoracic spinous process. Surface palpation of the scapula and the thoracic spine has been reported to be a valid method for determining the scapular position17 with good intrarater (ICC = 0.96) and interrater reliability (ICCs ranged from 0.96 to 0.97) [18,19].
Inclusion criteria were as follows: age between 18 and 50 years to minimize the effect of degenerative changes to the cervical spine on the cervical ROM20, score of at least 5/50 on the Neck Disability Index (NDI)21, active cervical rotation ROM equal to or less than 70 degrees, and the Numeric Pain Rating Scale (NPRS) of at least 2/10 score with active cervical rotation in both directions. The participants were excluded if they had a history of cervical radiculopathy, congenital scapular abnormalities, cerebrovascular diseases, peripheral nerve injury, inflammation signs in the neck and shoulder areas, fibromyalgia, neoplasm, pathological fractures, infectious disease, systemic inflammatory diseases, cervical myelopathy, and previous surgery in the cervical region.
Sample size was calculated based on previous studies in order to identify a mean difference between groups of 10 degrees of cervical ROM [14], two scores of pain intensity on the NPRS [22] , and 12 N/cm2 of PPT23. With a statistical power of 0.80 (1 − β error probability) and α error-level probability of 0.05, a total sample size of at least 14 patients per group was necessary with an anticipated dropout rate of 20%.
Randomization
The eligible participants were randomly allocated into either an intervention group (n = 14) or a control group (n = 14) using a block randomization table generated by a computerized sequence with a 1:1 allocation ratio that was sequentially numbered. The allocation was concealed in opaque and sealed envelopes for the purpose of blinding the outcome assessor and only revealed immediately before intervention was provided.
Outcome measures
Active cervical rotation ROM. Active cervical rotation ROM was measured using a Cervical Range of Motion (CROM) device (Performance Attainment Associates, St Paul, MN). It consisted of a magnetic neck brace and three inclinometers to measure each anatomical plane of movement. The participants were measured in a sitting position with their feet rested on the ground, their hips and knees positioned at right angles, and both hands placed upon their laps. The CROM device was strapped on the participants’ head by having all three inclinometers read zeroes. The device was found to be a valid and reliable instrument for measuring cervical ROM in both asymptomatic and neck pain patients [24,25]. Participants were asked to move their necks as far as possible in the right and left rotations. Two measurements were taken for each movement, and the mean was calculated25. Data were recorded as ipsilateral and contralateral ROM in relation to the side of the depressed scapula. For participants with bilateral depressed scapulae, the data were recorded in relation to the side of the greater depressed scapula.
Neck pain intensity. An 11-point NPRS26 was used to assess neck pain intensity at the end range of maximum active cervical rotation. On the scale, 0 represented no pain and 10 represented the worst pain imaginable. The mean value of the two trials of cervical rotation in each direction was calculated. Data were recorded as ipsilateral and contralateral pain intensity on the side of the depressed scapula, similar to the active cervical rotation ROM.
PPT. PPT over the upper trapezius muscle region was assessed by an electronic pressure algometer (Commander, J Tech Medical Industries – Heber city, UT, USA). The device was found to be valid and reliable in testing tissue sensitivity to pressure in both asymptomatic and neck pain patients [23,27] . The participants sat in a chair with both hands placed over their laps. Skin over the midpoint between the superior angle and the acromion process of the scapula was marked. An increasing perpendicular pressure was applied over the marked point through the end of the electronic pressure algometer at a controlling rate of 3 N/sec. The measurement was taken on the side of a greater depressed scapula. The participants were instructed to report when the sensation of pressure changed to pain. Two repeated measurements were performed with a 30-second rest between trials [11,28] and the mean was used for data analysis.
Procedure
Each participant attended two sessions (familiarization and experimental). The two sessions were separated by 48–72 hours interval. The familiarization session was to accustom participants (both the intervention and the control groups) with the measurement protocols and the testing environment. The participants were asked to remove their eyeglasses and/or accessories from the head and neck areas. Female participants were requested to wear a camisole, while male participants were requested to take off their upper body clothing. They were then instructed to sit on an adjustable height seat in the standard sitting position, with both hands placed over their laps (feet flat on the floor with hips, knees, and ankles flexed at 90 degrees). Five bony landmarks, including two on the superior angle of both scapulae, two on the lateral border of acromion processes, and one on the second thoracic spinous process were palpated, and 15-millimeter diameter color-tape markers were attached to each one. The CROM device was attached to the participants’ head. Posteriorly, a digital camera with a water-based horizontal level was focused at the second thoracic spinous process, located 50 centimeters away from the participants. Anteriorly, a computer screen connected to a camera was set up to provide real-time visual feedback for self-monitoring of scapular alignment (Figure 2).
Figure 2.

(a) Participants’ position during the intervention and (b) color-tape markers at superior angle of the scapulae (SA), lateral border of the acromion processes (AC), and the second thoracic spinous process (T2).
At the familiarization session, the participants in the intervention group learned to perform active scapular correction by actively moving their scapula to the neutral position. The superior angle of the scapula and the lateral border of the acromion had to be aligned with or just above the second thoracic spinous process [9,10,13]. A participant’s training was completed when they could hold the neutral position for 10 seconds. Each participant was strongly advised to avoid practice after training. In addition, participants were instructed to avoid heavy exercise, neck pain treatment, and consumption of analgesic drugs or other stimulants, such as caffeine and nicotine products, for at least eight hours prior to the experimental session29.
The experimental session consisted of collecting measurements before and after intervention. Baseline measurements were recorded in the following order: active cervical rotation ROM, neck pain intensity at maximum cervical rotation, and PPT over the upper trapezius region. The intervention group performed active scapular correction by lifting the depressed scapula or scapulae up to the correct vertical position. They were asked to hold the position for 10 seconds and repeated the task 10 times with a 10-second rest between repetitions (total contraction time was 100 seconds and total resting time was 100 seconds). This regime was based on a previous study that achieved immediate pain reduction and increased PPT at the most painful cervical segment16. Additional verbal cues and minimal manual assistance were provided if the participants lost the corrected scapular alignment during correction until they completed the intervention. The control group was asked to sit comfortably in the standard sitting position for 200 seconds with their scapulae in natural position. Immediately following intervention, all the baseline measurements were recorded in the same order.
Two researchers with 4 years of clinical experience in orthopedic physical therapy participated in the study. The first researcher, who enrolled and assigned the participants to either group, was responsible for assessing scapula depression and instructing participants on how to perform active scapular correction. The second researcher, who was blinded to group allocation, collected the variables at baseline and post intervention.
Statistical analysis
All statistics were performed using the IBM SPSS Statistics versions 22.0 (IBM Corp. Released 2013, Armonk, NY, USA). Statistical significance was set at p < .05. Based on a combination of qualitative (Q-Q plots and box plots) and quantitative analysis (Shapiro–Wilk test), the majority of variables were found to be not normally distributed, therefore nonparametric statistical analyses were used. Within-group differences between baseline and post intervention were evaluated for each group using a Wilcoxon signed-rank test. Between-group differences between intervention and control groups were compared using a Mann–Whitney U-test. The effect size (r) was analyzed to determine the magnitude of the difference between groups, which was interpreted as small at r = 0.1–0.3, moderate at r greater than0.3 to 0.5 and large at r ˃ 0.5 according to Cohen’s criteria30.
Results
A total of 50 potential participants were screened. Twenty-eight participants met the inclusion criteria and were randomly allocated to the two groups, intervention and control. While none of the participants reported neck pain at rest, the majority (96%) reported pain in their neck movements, particularly in lateral flexion ipsilateral to the symptomatic cervical rotation. There were no significant differences between the groups at baseline (p > 0.05) in demographic characteristics and outcome measures (Table 1). None reported any adverse effects due to the intervention. No participant was lost from the trial after randomization. Post intervention, the participants in the intervention group showed significantly greater active cervical rotation ROM compared to the control group, both on the ipsilateral (p = 0.006, r = 0.52) and contralateral (p = 0.016, r = 0.45) sides of the depressed scapula (Table 2). Neck pain intensity at maximum cervical rotation was also significantly lower in the intervention group than in the control group, both on the ipsilateral (p < 0.001, r = 0.84) and contralateral (p = 0.001, r = 0.64) sides of the depressed scapula. No significant difference in PPT over the upper trapezius region between the groups was demonstrated (p = 0.194, r = 0.25). Due to the statistically nonsignificant difference in PPT over the upper trapezius region, retrospective statistical power analysis was conducted. This aimed to determine the degree of power achieved by the sample size of this study. The magnitude of the minimum clinically significant difference between group means was set at 12 N/cm2. A power of greater than 90% was found for the comparison. This suggests that the statistically nonsignificant difference found in this study can be confidently accepted.
Table 1.
Median (interquartile range) of participants’ demographics and baseline data.
| Variables | Control group (n = 14) | Intervention group (n = 14) | p value |
|---|---|---|---|
| Gender (male/female) | 4/10 | 6/8 | - |
| Unilateral/bilateral depressed scapula | 7/7 | 6/8 | - |
| BMI (kg/m2) | 21.9 (18.3, 24.1) | 22.1 (21.5, 25.0) | 0.603 |
| Age (years) | 31.0 (25.8, 34.3) | 31.0 (20.8, 38.3) | 0.482 |
| NDI (scores) | 10.0 (8.3, 18.5) | 10.5 (6.8, 14.3) | 0.492 |
| Duration of neck pain (months) | 12.0 (6.0, 24.0) | 12.0 (6.0, 24.0) | 0.635 |
| Active cervical rotation ROM (degrees) | |||
| – Ipsilateral side of depressed scapula | 52.0 (47.5, 62.5) | 59.5 (51.5, 62.3) | 0.454 |
| – Contralateral side of depressed scapula | 52.0 (50.0, 60.8) | 53.5 (49.8, 61.8) | 0.804 |
| Neck pain intensity at maximum cervical rotation (0–10) | |||
| – Ipsilateral side of depressed scapula | 4.0 (3.0, 4.5) | 3.0 (3.0, 4.3) | 0.194 |
| – Contralateral side of depressed scapula | 3.0 (2.0, 4.0) | 3.0 (3.0, 4.0) | 0.769 |
| PPT (N/cm2) | 17.8 (12.8, 26.0) | 19.6 (13.6, 23.6) | 0.804 |
NDI = Neck Disability Index, PPT = pressure pain threshold, ROM = range of motion
Table 2.
Median (interquartile range) of active cervical rotation ROM, neck pain intensity with cervical rotation, and PPT over the upper trapezius muscle at baseline and post intervention in the intervention and the control groups.
| Variables | Baseline | Post intervention |
p-value (within group) |
p -value (between group) |
Effect size (r) |
|---|---|---|---|---|---|
| Active cervical rotation ROM (degrees) | |||||
| – Ipsilateral side of depressed scapula | |||||
| – Control | 52.0 (47.5, 62.5) | 52.0 (47.8, 61.3) | 0.952 | 0.006 | 0.52 |
| – Intervention | 59.5 (51.5, 62.3) | 70.0 (57.8, 71.0) | 0.001 | ||
| – Contralateral side of depressed scapula | |||||
| – Control | 52.0 (50.0, 60.8) | 55.5 (50.0, 60.3) | 0.858 | 0.016 | 0.45 |
| – Intervention | 53.5 (49.8, 61.8) | 64.5 (59.0, 73.0) | 0.001 | ||
| Neck pain intensity at maximum cervical rotation (0–10) | |||||
| – Ipsilateral side of depressed scapula | |||||
| – Control | 4.0 (3.0, 4.5) | 3.5 (3.0, 4.3) | 0.046 | <0.001 | − 0.84 |
| – Intervention | 3.0 (3.0, 4.3) | 0.5 (0.0, 2.0) | 0.001 | ||
| – Contralateral side of depressed scapula | |||||
| – Control | 3.0 (2.0, 4.0) | 3.0 (2.0, 4.0) | 0.317 | 0.001 | − 0.64 |
| – Intervention | 3.0 (3.0, 4.0) | 1.0 (0.0, 2.0) | 0.002 | ||
| PPT (N/cm2) | |||||
| – Control | 17.8 (12.8, 26.0) | 16.4 (13.1, 26.8) | 0.116 | 0.194 | 0.25 |
| – Intervention | 19.6 (13.6, 23.6) | 21.6 (15.5, 30.3) | 0.002 | ||
PPT = pressure pain threshold, ROM = range of motion
Changes from baseline to post intervention within the groups revealed a significant improvement in all outcome measures in the intervention group (p < 0.01). No significant changes were found in the control group except for neck pain intensity at the end range on the ipsilateral side of the depressed scapula (p = 0.046) with a difference of 0.5 points on the NPRS. However, this result did not meet the accepted minimum clinically significant difference of two points for this scale [31].
Discussion
To the best of the authors’ knowledge, this is the first study investigating the effects of active scapular correction intervention on individuals with neck pain, who have unilateral or bilateral depressed scapula. Within a minute after completion of intervention, there was an increase in active cervical rotation ROM, a decrease in neck pain with active cervical rotation, and an increase in PPT over the upper trapezius region. The results support recent studies that found integrated scapular training along with other interventions were beneficial for individuals with neck pain [32,33].
In this study, active cervical rotation ROM increased approximately 10 degrees both on the ipsilateral and contralateral sides of the depressed scapula post active scapular correction. Comparison of these results with other research findings is difficult as previous studies on the effect of active scapular correction did not examine active cervical rotation ROM. However, this change is in line with previous studies that assessed passive scapular correction. They found an increase of 13 to 14 degrees in neck pain patients with bilateral downwardly rotated scapulae14 and 5 to 15 degrees in neck pain patients with unknown scapular position13. Simultaneously, participants also experienced a reduction of approximately 65% to 75% in neck pain at maximum cervical rotation after active scapular correction. The reduction ranged from 2.0 to 2.5 points on the NPRS, which is considered to be clinically significant31.
The mechanisms of pain reduction and increase in active cervical rotation ROM following the active scapular correction remain unclear. It might be attributed to the neurophysiological effects of the isometric contraction component of the intervention. Activating the muscle afferent A delta fiber within the contracted muscle could generate an efferent inhibition of pain perception from the opioid analgesics system36,37. The increase in active cervical rotation ROM could be due to the elevated blood flow to the muscle associated with muscle contraction resulting in tissue temperature rise and increased tissue extensibility34,35.
Although the reduction in pain and the increase in active cervical rotation ROM found in this study were explained by different pathways, these two variables tend to be related. This is supported by previous studies in patients with chronic neck pain, which also showed an inverse correlation between pain and active cervical ROM (r = −0.12 to −0.37) as well as between neck pain and cervical muscle force production (r = −0.24 to −0.46). Thus, it may be assumed that neck pain reduction in the present study could improve cervicoscapular muscle function and produce greater maximum cervical rotation ROM.
The PPT values found at baseline in this study (17.8 to 19.6 N/cm2) were in the range of 19.0 ± 9.0 N/cm2 which was reported in healthy young subjects with a depressed scapular position10. An increased PPT of approximately 4 N/cm2 after the intervention are in accordance with previous studies that also required their participants to isometrically contract muscles repeatedly for the same total contraction time of 100 seconds. The PPT immediately increased approximately 10 N/cm2 at the most symptomatic cervical motion segment after active isometric scapular correction exercise16 and approximately 2 N/cm2 after a gentle cranio-cervical flexion exercise29. A larger change might be postulated if the intervention is applied repeatedly or for a longer period. Future studies are required to test this notion.
For clinicians treating patients with neck pain with cervical rotation, assessment of scapular position should be considered. The findings of this study support the use of active scapular correction intervention as a therapeutic exercise for immediate pain relief. The incorporation of a camera and visual display to provide real-time feedback during active scapular correction intervention also suggests the possibility for the use of this protocol as a self-exercise should similar feedback be available.
Limitations
This study was subject to some limitations. First, this study investigated the immediate effects of active scapular correction. Its longer duration effects are not known. Second, this study investigated participants with scapular depression. The results cannot be applied to other types of scapular malalignment. Third, only active cervical rotation was evaluated in this study. The results cannot be generalized to other cervical movements. Fourth, this study did not monitor muscle activity of the cervicoscapular muscles so the changes in these muscle activities during and after intervention could not be established. Fifth, other postural malalignments that alter the position of the scapula were not evaluated. The forward head posture or thoracic hyperkyphosis should be considered in future research. Sixth, the order of dependent variables measured was not randomized, which might affect the performance of subsequent dependent variables. Finally, some participants might practice the active scapular correction intervention during the interval between the familiarization session and the experimental session. The results might therefore be due to a larger dose than the 10 repetitions of 10-second hold.
Conclusion
The active scapular correction intervention resulted in an immediate increase in active cervical rotation ROM and a decrease in neck pain at maximum cervical rotation. The findings offer some support for using this intervention as self-exercise for patients in the management of neck pain.
Supplementary Material
Biographies
Siwaluk Srikrajang, PT, M.Sc., currently works with the attention of musculoskeletal physical therapy. She has a Master’s Degree in Physical Therapy from Chulalongkorn University, Thailand. Her research interests include movement science and musculoskeletal physical therapy.
Rotsalai Kanlayanaphotporn, PT, Ph.D., currently works as an Associate Professor in the Physical Therapy Department at Chulalongkorn University, Thailand. She has done PhD in Health Science from University of South Australia, Australia. Her research lines include human movement science and musculoskeletal rehabilitation.
Funding Statement
This study was supported by the Graduate School Thesis Grant, Chulalongkorn University (number GCUGR1225641075M; Graduate School, Chulalongkorn University).
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplemental Material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/10669817.2022.2077515
References
- [1].Bikbov MM, Kazakbaeva GM, Zainullin RM, et al. Prevalence of and factors associated with low back pain, thoracic spine pain and neck pain in Bashkortostan, Russia: the ural eye and medical study. BMC Musculoskelet Disord. 2020;21(1):64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Fandim JV, Nitzsche R, Michaleff ZA, et al. The contemporary management of neck pain in adults. Pain Manag. 2021;11(1):75–87. [DOI] [PubMed] [Google Scholar]
- [3].Noormohammadpour P, Mansournia MA, Koohpayehzadeh J, et al. Prevalence of chronic neck pain, low back pain, and knee pain and their related factors in community-dwelling adults in Iran: a population-based national study. Clin J Pain. 2017;33(2):181–187. [DOI] [PubMed] [Google Scholar]
- [4].Blanpied PR, Gross AR, Elliott JM, et al. Neck Pain: revision 2017. J Orthop Sports Phys Ther. 2017;47(7):A1–A83. [DOI] [PubMed] [Google Scholar]
- [5].Cagnie B, Struyf F, Cools A, et al. The relevance of scapular dysfunction in neck pain: a brief commentary. J Orthop Sports Phys Ther. 2014;44(6):435–439. [DOI] [PubMed] [Google Scholar]
- [6].Kendall FP, Provance PG, Rodgers MM, et al. Muscles: testing and function with posture and pain. Baltimore: Williams & Wilkins; 2005. [Google Scholar]
- [7].Wannaprom N, Treleaven J, Jull G, et al. Response rate and comparison of clinical features associated with positive or negative responses to a scapular positioning test in patients with neck pain and altered scapular alignment: a cross-sectional study. BMJ Open. 2021;11(12):(e057459). [Google Scholar]
- [8].Martínez-Merinero P, Lluch E, Gallezo-Izquierdo T, et al. The influence of a depressed scapular alignment on upper limb neural tissue mechanosensitivity and local pressure pain sensitivity. Musculoskelet Sci Pract. 2017;29:60–65. [DOI] [PubMed] [Google Scholar]
- [9].Andrade GT, Azevedo DC, De Assis Lorentz I, et al. Influence of scapular position on cervical rotation range of motion. J Orthop Sports Phy Ther. 2008;38(11):668–673. [DOI] [PubMed] [Google Scholar]
- [10].Azevedo DC, de Lima Pires T, de Souza Andrade F, et al. Influence of scapular position on the pressure pain threshold of the upper trapezius muscle region. Eur J Pain. 2008;12(2):226–232. [DOI] [PubMed] [Google Scholar]
- [11].Lee KT, Chuang CC, Lai CH, et al. Study of the trapezius muscle region pressure pain threshold and latency time in young people with and without depressed scapula. Man Ther. 2015;20(1):124–129. [DOI] [PubMed] [Google Scholar]
- [12].Seok J, Kim T.. The effects of scapular alignment exercise and nerve mobilization on pain and muscle activity in subjects with scapular depression alignment. J Musculoskelet Sci Technol. 2020;4(2):58–65 [Google Scholar]
- [13].Van Dillen LR, McDonnell MK, Susco TM, et al. The immediate effect of passive scapular elevation on symptoms with active neck rotation in patients with neck pain. Clin J Pain. 2007;23(8):641–647. [DOI] [PubMed] [Google Scholar]
- [14].Ha SM, Kwon OY, Yi CH, et al. Effects of passive correction of scapular position on pain, proprioception, and range of motion in neck-pain patients with bilateral scapular downward-rotation syndrome. Man Ther. 2011;16(6):585–589. [DOI] [PubMed] [Google Scholar]
- [15].Wegner S, Jull G, O’Leary S, et al. The effect of a scapular postural correction strategy on trapezius activity in patients with neck pain. Man Ther. 2010;15(6):562–566. [DOI] [PubMed] [Google Scholar]
- [16].Lluch E, Arguisuelas MD, Calvente Quesada O, et al. Immediate effects of active versus passive scapular correction on pain and pressure pain threshold in patients with chronic neck pain. J Manipulative Physiol Ther. 2014;37(9):660–666. [DOI] [PubMed] [Google Scholar]
- [17].Lewis J, Green A, Reichard Z, et al. Scapular position: the validity of skin surface palpation. Man Ther. 2002;7(1):26–30. [DOI] [PubMed] [Google Scholar]
- [18].DiVeta J, Walker ML, Skibinski B. Relationship between performance of selected scapular muscles and scapular abduction in standing subjects. Phys Ther. 1990;70(8):470–476. [DOI] [PubMed] [Google Scholar]
- [19].Greenfield B, Catlin PA, Coats PW, et al. Posture in patients with shoulder overuse injuries and healthy individuals. J Orthop Sports Phys Ther. 1995;21(5):287–295. [DOI] [PubMed] [Google Scholar]
- [20].Salo PK, Hakkinen AH, Kautiainen H, et al. Quantifying the effect of age on passive range of motion of the cervical spine in healthy working-age women. J Orthop Sports Phys Ther. 2009;39(6):478–483. [DOI] [PubMed] [Google Scholar]
- [21].Vernon H. The neck disability index: state-of-the-art, 1991-2008. J Manipulative Physiol Ther. 2008;31(7):491–502. [DOI] [PubMed] [Google Scholar]
- [22].Young I, Dunning J, Butts R, et al. Reliability, construct validity, and responsiveness of the neck disability index and numeric pain rating scale in patients with mechanical neck pain without upper extremity symptoms. Physiother Theory Pract. 2019;35(12):1328–1335. [DOI] [PubMed] [Google Scholar]
- [23].Walton DM, Macdermid JC, Nielson W, et al. Reliability, standard error, and minimum detectable change of clinical pressure pain threshold testing in people with and without acute neck pain. J Orthop Sports Phys Ther. 2011;41(9):644–650. [DOI] [PubMed] [Google Scholar]
- [24].Williams MA, Williamson E, Gates S, et al. Reproducibility of the cervical range of motion (CROM) device for individuals with sub-acute whiplash associated disorders. Eur Spine J. 2012;21(5):872–878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Fletcher JP, Bandy WD. Intrarater reliability of CROM measurement of cervical spine active range of motion in persons with and without neck pain. J Orthop Sports Phys Ther. 2008;38(10):640–645. [DOI] [PubMed] [Google Scholar]
- [26].Hawker GA, Mian S, Kendzerska T, et al. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken). 2011;63(11):S240–52. [DOI] [PubMed] [Google Scholar]
- [27].Chesterton LS, Sim J, Wright CC, et al. Interrater reliability of algometry in measuring pressure pain thresholds in healthy humans, using multiple raters. Clin J Pain. 2007;23(9):760–766. [DOI] [PubMed] [Google Scholar]
- [28].Romero-Morales C, Jaén-Crespo G, Rodríguez-Sanz D, et al. Comparison of pressure pain thresholds in upper trapezius and temporalis muscles trigger points between tension type headache and healthy participants: a case–control study. J Manipulative Physiol Ther. 2017;40(8):609–614. [DOI] [PubMed] [Google Scholar]
- [29].O’Leary S, Falla D, Hodges PW, et al. Specific therapeutic exercise of the neck induces immediate local hypoalgesia. J Pain. 2007;8(11):832–839. [DOI] [PubMed] [Google Scholar]
- [30].Pallant J. SPSS survival manual. A step by step guide to data analysis using SPSS for windows. 3rd Berkshire: McGraw Hill: Open University Press; 2007. [Google Scholar]
- [31].Farrar JT, LaMoreaux L, Werth JL, et al. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–158. [DOI] [PubMed] [Google Scholar]
- [32].Javdaneh N, Ambrozy T, Barati AH, et al. Focus on the scapular region in the rehabilitation of chronic neck pain is effective in improving the symptoms: a randomized controlled trial. J Clin Med. 2021;10(16):3495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Yildiz TI, Turgut E, Duzgun I. Neck and scapula-focused exercise training on patients with nonspecific neck pain: a randomized controlled trial. J Sport Rehabil. 2018;27(5):403–412. [DOI] [PubMed] [Google Scholar]
- [34].Knight CA, Rutledge CR, Cox ME, et al. Effect of superficial heat, deep heat, and active exercise warm-up on the extensibility of the plantar flexors. Phys Ther. 2001;81(6):1206–1214. [PubMed] [Google Scholar]
- [35].Chiu TT, Lam TH, Hedley AJ. Correlation among physical impairments, pain, disability, and patient satisfaction in patients with chronic neck pain. Arch Phys Med Rehabil. 2005;86(3):534–540. [DOI] [PubMed] [Google Scholar]
- [36].Holden S, Lyng K, Graven-Nielsen T, et al. Isometric exercise and pain in patellar tendinopathy: a randomized crossover trial. J Sci Med Sport. 2020;23(3):208–214. [DOI] [PubMed] [Google Scholar]
- [37].Ylinen J, Takala EP, Kautiainen H, et al. Association of neck pain, disability and neck pain during maximal effort with neck muscle strength and range of movement in women with chronic non-specific neck pain. Eur J Pain. 2004;8(5):473–478. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


