PURPOSE
The objective of this study was to test the feasibility of implementing a postoperative monitoring program for women with gynecologic cancers composed of patient-reported outcomes (PROs) and a wearable activity monitor.
METHODS
We prospectively enrolled patients undergoing gynecologic cancer surgery to this single-arm study. Enrolled patients completed PROs (Patient-Reported Outcomes Measurement Information System physical function, sleep disturbance, anxiety, fatigue, and pain intensity) at baseline and one-week intervals for 4 weeks. They also wore a wearable accelerometer device that measured steps, heart rate, and intensity of physical activity. The primary outcome was feasibility. The secondary outcome was prediction of unscheduled contacts with the health care system on a given postoperative day.
RESULTS
We enrolled 34 women. Three patients were unevaluable. The mean age was 58 years. The mean body mass index was 31 kg/m2; 17 patients were White (54.8%), 12 patients were Black (38.7%), and two patients (6.5%) were Asian. The overall wear time was 83.8%, and patients responded to 80.4% of the PRO instruments. Twenty-two patients (71%) had an unscheduled contact with the health care system postoperatively (median 1.5, 0.0-8.0). The day of an unscheduled health care utilization event was predicted with acceptable discrimination (area under the receiver operating characteristic curve 0.75; 95% CI, 0.67 to 0.81). PROs of fatigue and physical function were most predictive followed by wearable device outputs of lightly active minutes and average daily heart rate.
CONCLUSION
Implementation of a postoperative monitoring program of patient-reported outcomes and a wearable device was feasible. The specific day of an unscheduled contact with the health care system was predicted with acceptable discrimination.
INTRODUCTION
Adverse events after cancer surgery are associated with increased morbidity and mortality and decreases in health-related quality of life.1-3 For many patients with cancer, adjuvant treatment is needed after surgery. Postoperative adverse events that delay recovery lead to decreased survival through both direct effects of the adverse event itself and adjuvant treatment delays.4 Prompt identification of postoperative adverse events leads to improvement in perioperative recovery and ultimately to improved long-term outcomes for patients.
CONTEXT
Key Objective
To determine the feasibility of a postoperative monitoring program consisting of patient-reported outcomes and a wearable device among women undergoing gynecologic cancer surgery.
Knowledge Generated
We found that postoperative monitoring using patient-reported outcomes and a wearable device was feasible with good wear time and response rates. The day on which a postoperative adverse event occurred can also be predicted with reasonable discrimination.
Relevance
Patients undergoing surgery can be monitored, and abnormal events can be detected. This may help to identify and assist those with deviations from the expected postoperative recovery trajectory.
Traditional efforts to identify patients at risk of adverse events have focused on preoperative risk factors such as patient age and medical comorbidities. Calculators such as the National Surgical Quality Improvement Program use preoperatively identified patient variables to calculate a patient-specific risk of postoperative complication.5-8 These calculators can help us to identify patients at risk and improve preoperative surgical counseling and surgical decision-making. However, these efforts only allow us to identify patients who are at risk for complications, not identify when during the postoperative period those complications might occur so that we can intervene sooner to help patients with resulting symptoms or alleviate the sequelae from these adverse events.
Patient-reported outcomes (PROs) and a wearable accelerometer device are promising tools to monitor patients in the postoperative period and potentially detect when adverse events are likely to occur. Among patients with gynecologic cancer undergoing surgery, those who experienced postoperative complications had inferior physical and functional well-being at one month as measured by PROs.1 Furthermore, in a large, randomized trial of patients undergoing chemotherapy, PRO monitoring and clinician review were associated with an overall survival benefit, suggesting that observed changes in PROs related to treatment have the potential to improve patient outcomes.9 The postoperative period is a time of rapid change, and therefore, PROs alone may not be sufficiently sensitive. Wearable devices that measure physical activity, such as step counts, heart rate, or minutes spent in different physical activity intensities, require little patient effort, provide continuous information, and have been well tolerated with high adherence rates in diverse populations.10-12 Furthermore, physical activity measurements, such as daily step counts, have been shown to correlate with functional recovery and reduced postoperative complications.10,13,14 Specifically, in pediatric surgery and in women with ovarian cancer undergoing chemotherapy, decreases in step counts have been found in the days before hospital admission for infection and an emergency room (ER) visit for a bowel obstruction.13,15 These findings suggest that declines in physical activity may precede an adverse event.
The objective of this study was to pilot test a postoperative monitoring program consisting of PROs and a wearable accelerometer device and measure the feasibility of implementing such a program. A secondary objective was the ability of PROs and physical activity data from a wearable accelerometer device to predict the occurrence of postoperative adverse events on a daily basis.
METHODS
Study Cohort
We prospectively enrolled women to this single-arm study that examined the use of a novel postoperative monitoring program for women after gynecologic cancer surgery. Eligible women were those undergoing surgery for a gynecologic cancer or a suspected gynecologic cancer at Prentice Women's Hospital. Additional inclusion criteria were age > 18 years, owning and being willing to use a smartphone, and English proficiency. Eligible patients were approached for study participation, and written informed consent was obtained before enrollment. Institutional Review Board approval was obtained from the Northwestern University Institutional Review Board (STU00206617).
Measures
Enrolled patients completed five PRO measures including Patient-Reported Outcomes Measurement Information System (PROMIS) physical function, sleep disturbance, anxiety, fatigue, and pain intensity at baseline (the week before surgery) and then at 1-week intervals for 4 weeks. PROMIS is a comprehensive group of more than 70 measures that are robust and validated to describe various symptom domains. Each questionnaire is scored through the previously studied process, and PROMIS scores are standardized to a T-score metric, with a score of 50 representing the US population mean. Patients received PRO measures through an e-mail link and completed the measures directly into RedCap. If patients did not complete a measure, a 48-hour reminder e-mail was sent. They also wore a Fitbit Alta HR device that contains a triaxial accelerometer preoperatively for at least 72 hours and postoperatively through 28 days. We also collected their sociodemographic and clinic data from Electronic Health Records. Using the wearable accelerometer device, patients' mean daily heart rate, total steps taken, and minutes spent in active, sedentary, or light activity were recorded. All measures were recorded through the study period and then analyzed at study completion.
Outcomes
The primary outcome was the feasibility of patients adhering to the postoperative monitoring program. We defined a feasible monitoring program as the one in which ≥ 80% of patients were adherent to the monitoring program. Adherence for an individual patient was defined as completing ≥ 75% of given PROs, and for Fitbit, wearing the device for ≥ 16 days during the 28-day postoperative period. These definitions were based on previous studies of patients with cancer undergoing PRO monitoring and a small study of women with metastatic ovarian cancer using an accelerometer for symptom detection.15-17 The secondary analysis examined the ability of the collected information (PROs and accelerometer output) to predict unscheduled contacts with the health care system. Unscheduled contacts with the health care system were defined as phone calls or messages through the electronic medical record (EMR) for medical complaints (not including those for scheduling, paperwork, or other nonmedical complaint-driven questions), unscheduled clinic visits, ER visits, and unscheduled hospitalizations.
Statistical Analysis
Sample size for this prospective single-arm study was based on the feasibility of postoperative patients adhering to the weekly PROs and wearing of the Fitbit device. For the monitoring program to be feasible and useful, ≥ 80% of patients would have to be adherent to the monitoring program as defined above. A sample size of n = 28 provides 85% power with a two-sided α = .05 to detect a difference between a 55% adherence rate and an 80% adherence rate. Given that some women may drop out, we enrolled 34 patients with an expected nonparticipation after an enrollment rate of 15%. Fifteen percent was selected on the basis of observed nonparticipation rates among patients with cancer completing PROs during active cancer treatment.17
The feasibility of the postoperative monitoring program was measured with descriptive statistics. Patient and clinical characteristics, PROs, and wearable device outputs were also described with descriptive statistics. Means were used for variables with a normal distribution. Normality was tested using a Shapiro-Wilk test.
The ability of PROs and output from the wearable accelerometer to predict postoperative unscheduled contacts with the health care system was examined using predictive modeling with feature importance. For these models, each day was considered an observation, and the model attempted to discriminate between whether during that day the patient experienced an unscheduled contact with the health care system. We experimented with several machine learning models: logistic regression, random forests, gradient boosting, and XGBoost, and these models were selected a priori.
Model inputs were considered in three main groups: clinical information, PRO responses, and wearable device output. Inputs were tested to determine if their addition improved the discrimination of the model by noting an increase in the area under the receiver operating characteristic curve (AUC). Clinical information, such as age, length of hospital stay, and type of cancer, was relatively useful for predicting the presence of an unscheduled contact with the health care system at any time in the postoperative period (AUC = 0.64), but did not improve the discrimination of the models, which predicted the day that the unscheduled contact would occur and so were not included in the final model. We also experimented with using different model inputs beyond the inputs for the day of variables (eg, using the average of the steps from the three prior days, the steps from three days prior), but we did not find that these improved discrimination and so they were not included in the final model. If model discrimination was similar between two models, the model that most easily explained the data was used. We were also sensitive to overfitting, given the sample size of 868 days, and thus did not experiment with more than 40 features (868/20). In addition, to prevent overfitting, we also performed five-fold cross-validation on the training data (80% of the whole data set) to determine the final model.
We also analyzed feature importance of the final model using permutation-based feature importance.18 The permutation feature importance is defined to be the decrease in a model score when a single feature value is randomly shuffled. By dropping the feature, we break the relationship between the feature and the target, and thus, the drop in the model score is indicative of how much the model depends on that feature. This technique is model-agnostic and can be calculated many times with different permutations of the feature. Then, for a particular model, we ranked all the features on the basis of their feature importance. For the final model, we only included the top 10 features on the basis of their ranking. All the code was written in Python (v3.0), and scikit-learn (v0.24) and pandas (1.2.1) packages were used. Discrimination was measured using the AUC.
RESULTS
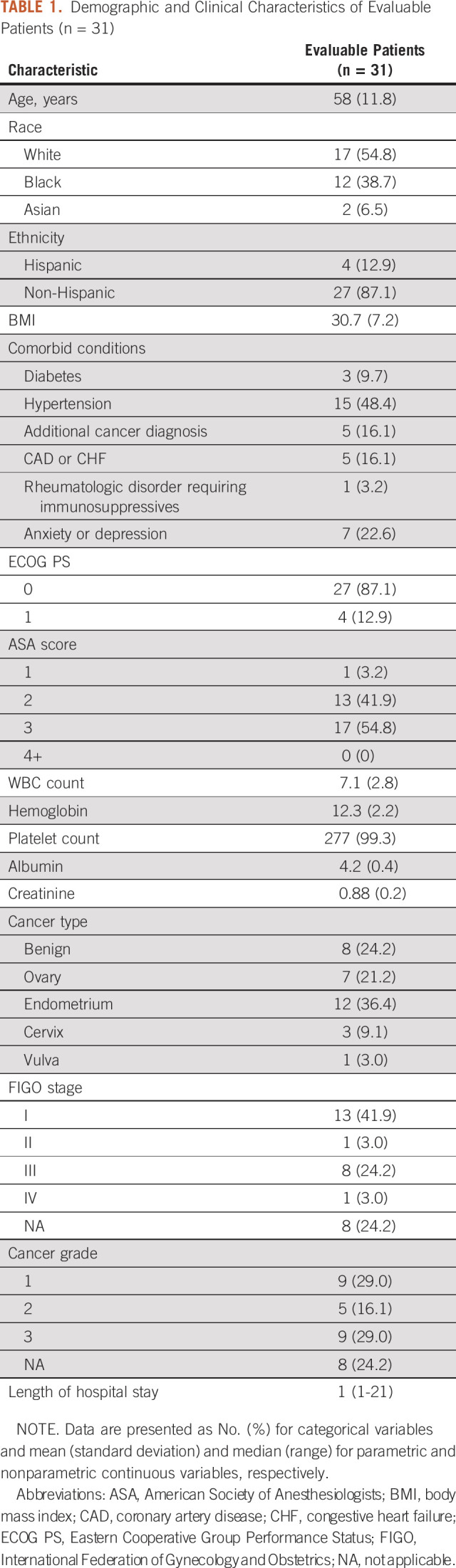
We enrolled 34 women to this study. Three patients were not evaluable and did not complete any postoperative monitoring because of not undergoing planned surgery (2) and loss of smartphone service (1). Therefore, a total of 31 women were evaluable with the clinical and demographic characteristics noted in Table 1. The mean age was 58 years, and the mean body mass index was 31 kg/m2; 17 patients were White (54.8%), 12 patients were Black (38.7%), and two patients (6.5%) were Asian. The overall wear time for the cohort during the 28-day postoperative period was 83.8%, with 90.3% of patients wearing their device for > 16 days of the postoperative period. Patients responded to 80.4% of the PRO instruments, and 83.9% of patients responded to > 75% of the surveys that they received. On the basis of the prespecified feasibility criteria, our postoperative monitoring program was feasible for patients with high wear time and good response to weekly PROs.
TABLE 1.
Demographic and Clinical Characteristics of Evaluable Patients (n = 31)
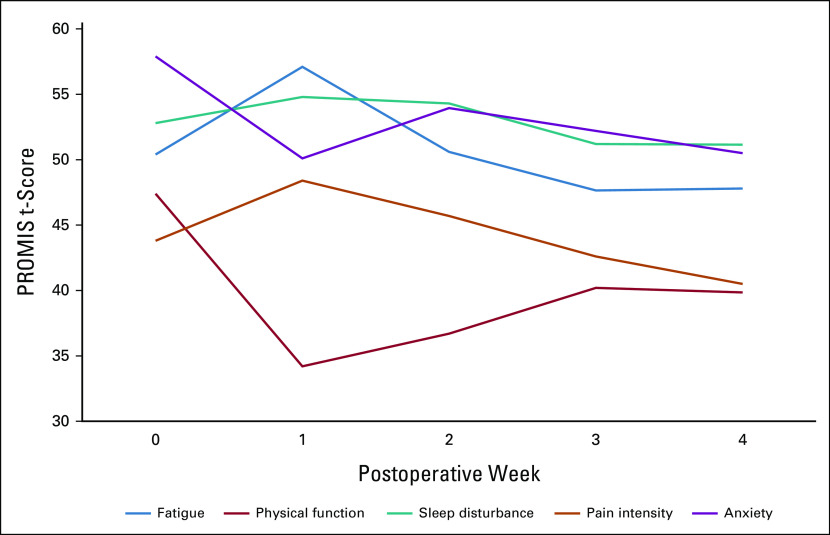
Preoperatively, patients had higher than mean population levels of anxiety (t-score of 50 on the PROMIS measures) and these decreased through the study period (Fig 1). Median scores for sleep disturbance, fatigue, and pain intensity initially worsened over the postoperative period, but were back to baseline by 4 weeks. Physical function worsened postoperatively and had not returned to presurgical levels by week 4.
FIG 1.
PROs during the 4-week postoperative period. Median weekly scores for each patient-reported outcome measure for the population over the study period. Time 0 represents the preoperative period. PRO, patient-reported outcome; PROMIS, Patient-Reported Outcomes Measurement Information System.
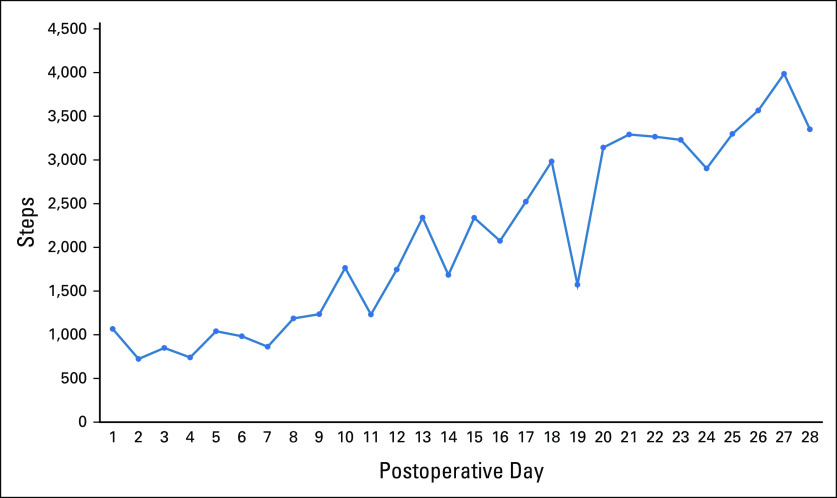
Median baseline daily steps (over the period of 2 weeks before surgery) were 4,296 (interquartile range [IQR] 2,115-6,251), and the mean baseline HR was 76 (±8.5). During the postoperative period, the average number of daily steps decreased drastically to 888 (IQR 474-2,046) in week 1, but improved to 1,399 (761-3,422) in week 2, 2,395 (IQR 1,125-4,426) in week 3, and 3,273 (IQR 1,625-5,651) in week 4 (Fig 2).
FIG 2.
Daily steps during the 28-day postoperative period. Median daily steps for the population over the study period.
Nineteen patients (65.5%) had an unscheduled contact with the health care system during the 4-week postoperative period. Patients had a median of 1.5 of these unscheduled contacts (range 0.0-8.0). These included 16 EMR messages, 20 phone calls, four unscheduled office visits, seven ER visits, and four hospitalizations. Examples of EMR messages and phone calls included topics such as pain, dehydration, constipation, and wound concerns.
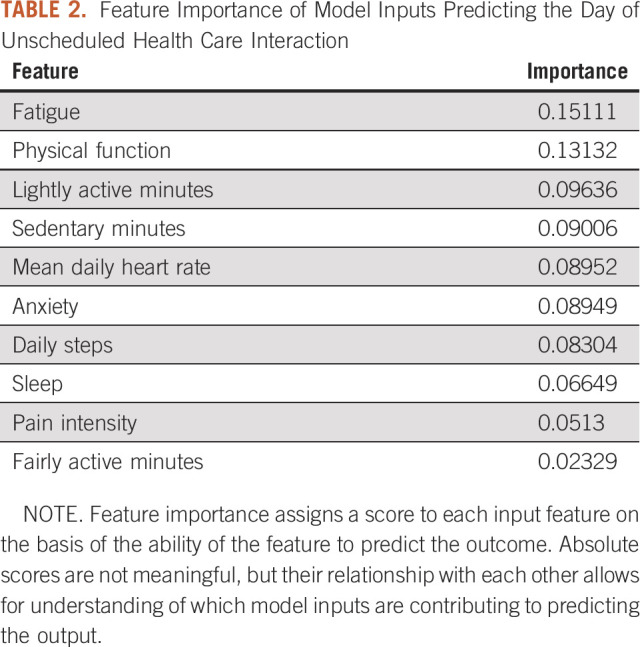
We undertook predictive modeling to identify which patients had a higher likelihood of having an unscheduled contact with the health care system and during which days those contacts were more likely to occur. In the final model, our outcome was an unscheduled contact with the health care system on a given day, and PROs and wearable device output were our predictors. In this model, each day was an observation. There were 10 features in the final model, which are listed in Table 2. We found that this combination of PROs and wearable device output results in the ability to discriminate between the days a patient had an unscheduled health care utilization event and those they did not with good discrimination with an AUC of 0.75 (95% CI, 0.67 to 0.81). The feature importance for which specific predictors were most useful in this discrimination is listed in Table 2. As can be seen, PROs of fatigue and physical function were most useful, followed by lightly active minutes and average daily heart rate. Higher scores for fatigue, lightly active minutes, and heart rate were associated with adverse events, whereas higher scores for sleep and physical function were negatively associated with adverse events. Both PROs and wearable device output contributed to discrimination in the model.
TABLE 2.
Feature Importance of Model Inputs Predicting the Day of Unscheduled Health Care Interaction
DISCUSSION
In this study, we found that implementation of a postoperative monitoring program consisting of PROs and a wearable accelerometer in patients undergoing gynecologic cancer surgery was feasible, with > 80% of patients able to adhere to the prespecified definitions of regular use of PROs and wearing of the accelerometer device. In addition, we found associations between PROs, output from the wearable device, and unscheduled contacts with the health care system. We were able to use predictive modeling to identify the specific days on which these unscheduled health care utilization events were likely to occur.
Strengths of this study include that, to our knowledge, it is the first to use a combination monitoring program of PROs and a wearable device in postoperative gynecologic oncology patients. It demonstrated that completing electronic weekly PROs and wearing a wrist device was feasible. In addition, the strategy of attempting to predict postoperative adverse events on the day on which they occur is novel and showed promise in this study. Limitations include that this was a single-arm pilot study and thus lacks the ability to generalize to other settings. There is also a possibility of overfitting of the algorithm given the small sample size; however, although we only had 31 evaluable patients, we had 868 postoperative days on which to train the algorithm, which helps to ameliorate this concern.
PROs have been used to monitor care of patients for more than a decade. In one of the most impactful articles on the use of PROs to drive clinical care, patients undergoing chemotherapy were randomly assigned to PRO completion versus usual care. Those randomly assigned to PROs had improved overall survival, highlighting the use of changes in PROs to prompt clinical care and improve patient outcomes.9 In gynecologic oncology, changes in postoperative PROs have been associated with postoperative complications, with those patients experiencing a postoperative complication having inferior physical and functional well-being.1,19 In this study, we found that PROs were some of the most predictive model inputs; specifically, patient-reported physical function and fatigue were useful in discriminating between the days that patients had unscheduled health care utilization events and those they did not. Patient-reported anxiety, sleep disturbance, and pain intensity were also predictive of these events, but to a lesser degree.
Wearable accelerometers offer complimentary information to PROs to monitor the postoperative period and in this study, provided clinically meaningful data. These devices have the benefit of not requiring patients to log in and answer questions, as studies have shown that postoperative patients are less likely to respond to PRO surveys, specifically, if they experience postoperative complications or are early in their postoperative period when symptom burden is higher.20,21 In this study, adherence to wearing the accelerometer device was higher than completion of PROs, suggesting that this form of monitoring may be a useful adjunct. Lightly active minutes and mean heart rate were most useful in predicting the days on which a patient would experience an adverse event. These findings corroborate previous studies in patients with ovarian cancer undergoing palliative chemotherapy and in pediatric postoperative patients, which found that changes in physical activity measured by an accelerometer preceded an ER visit for a bowel obstruction and a hospital readmission for a postoperative infection.13,15 Our study takes the next step and applies machine learning algorithms, albeit in a small sample, to predict these events on a daily basis with a quantitative result, extending this work beyond just visual association and pattern recognition.
Traditionally, symptom screening and PROs have been collected from patients during their interaction with the health care system, which may be days or weeks after the occurrence of a symptom or problem. As we increasingly use enhanced recovery pathways and send patients home from the hospital earlier, there is increasing interest in using tools to help us understand and monitor patients when they are no longer under our direct care. Real-time monitoring in which assistance is directed to patients when abnormalities in PROs or physical activity are identified may play a role in future surgical care. The ability of these monitoring tools to be useful depends on their degree of precision in identifying patients who are in need of assistance in a time frame in which such assistance could be offered. Our study differs from previous studies in that we attempted to predict the adverse event on the day it occurs. This level of precision will likely be needed if these tools are to be used to monitor patients in real time and direct resources on the basis of observed abnormalities.
In this study, postoperative monitoring of patients using PROs and a wearable device was feasible and showed moderate ability to discriminate between the days the patients experienced postoperative adverse events and those they did not. The future of surgical care will likely incorporate some form of postoperative monitoring, allowing us to extend care for patients beyond the traditional medical complex. Future applications of this tool require additional research to validate the prediction algorithm and operationalize the intervention to be used if an unscheduled contact with the health care system is predicted.
Emma L. Barber
Consulting or Advisory Role: Merck, Immunogen
Research Funding: Lilly (Inst)
Dario Roque
Honoraria: Intuitive Surgical
Consulting or Advisory Role: Myriad Genetics
Speakers' Bureau: GlaxoSmithKline
Research Funding: Bristol Myers Squibb Foundation
Travel, Accommodations, Expenses: Intuitive Surgical, GlaxoSmithKline
Edward Tanner
Consulting or Advisory Role: Johnson & Johnson/Janssen
Speakers' Bureau: AstraZeneca/Merck, Merck, Eisai
No other potential conflicts of interest were reported.
SUPPORT
Supported by a grant from the Friends of Prentice Foundation. E.L.B. was supported by NICHD (K12 HD050121-12), the NIA (P30AG059988-01A1), and the GOG Foundation.
AUTHOR CONTRIBUTIONS
Conception and design: Emma L. Barber, Ravi Garg
Financial support: Emma L. Barber
Administrative support: Edward Tanner
Provision of study materials or patients: Emma L. Barber, Anna Strohl, Dario Roque, Edward Tanner
Collection and assembly of data: All authors
Data analysis and interpretation: Emma L. Barber, Ravi Garg, Dario Roque, Edward Tanner
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/cci/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Emma L. Barber
Consulting or Advisory Role: Merck, Immunogen
Research Funding: Lilly (Inst)
Dario Roque
Honoraria: Intuitive Surgical
Consulting or Advisory Role: Myriad Genetics
Speakers' Bureau: GlaxoSmithKline
Research Funding: Bristol Myers Squibb Foundation
Travel, Accommodations, Expenses: Intuitive Surgical, GlaxoSmithKline
Edward Tanner
Consulting or Advisory Role: Johnson & Johnson/Janssen
Speakers' Bureau: AstraZeneca/Merck, Merck, Eisai
No other potential conflicts of interest were reported.
REFERENCES
- 1.Doll KM, Barber EL, Bensen JT, et al. : The impact of surgical complications on health-related quality of life in women undergoing gynecologic and gynecologic oncology procedures: A prospective longitudinal cohort study. Am J Obstet Gynecol 215:457.e1-457.e13, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fagotti A, Ferrandina G, Vizzielli G, et al. : Phase III randomised clinical trial comparing primary surgery versus neoadjuvant chemotherapy in advanced epithelial ovarian cancer with high tumour load (SCORPION trial): Final analysis of peri-operative outcome. Eur J Cancer 59:22-33, 2016 [DOI] [PubMed] [Google Scholar]
- 3.Anthony T, Long J, Hynan LS, et al. : Surgical complications exert a lasting effect on disease-specific health-related quality of life for patients with colorectal cancer. Surgery 134:119-125, 2003 [DOI] [PubMed] [Google Scholar]
- 4.Wright JD, Herzog TJ, Neugut AI, et al. : Effect of radical cytoreductive surgery on omission and delay of chemotherapy for advanced-stage ovarian cancer. Obstet Gynecol 120:871-881, 2012 [DOI] [PubMed] [Google Scholar]
- 5.Neumayer L, Hosokawa P, Itani K, et al. : Multivariable predictors of postoperative surgical site infection after general and vascular surgery: Results from the patient safety in surgery study. J Am Coll Surg 204:1178-1187, 2007 [DOI] [PubMed] [Google Scholar]
- 6.Barber EL, Rutstein S, Miller WC, et al. : A preoperative personalized risk assessment calculator for elderly ovarian cancer patients undergoing primary cytoreductive surgery. Gynecol Oncol 139:401-406, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rivard C, Nahum R, Slagle E, et al. : Evaluation of the performance of the ACS NSQIP surgical risk calculator in gynecologic oncology patients undergoing laparotomy. Gynecol Oncol 141:281-286, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cohen ME, Bilimoria KY, Ko CY, et al. : Development of an American College of Surgeons National Surgery Quality Improvement Program: Morbidity and mortality risk calculator for colorectal surgery. J Am Coll Surg 208:1009-1016, 2009 [DOI] [PubMed] [Google Scholar]
- 9.Basch E, Deal AM, Dueck AC, et al. : Overall survival results of a trial assessing patient-reported outcomes for symptom monitoring during routine cancer treatment. JAMA 318:197-198, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van der Meij E, van der Ploeg HP, van den Heuvel B, et al. : Assessing pre- and postoperative activity levels with an accelerometer: A proof of concept study. BMC Surg 17:56, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Appelboom G, Taylor BE, Bruce E, et al. : Mobile phone-connected wearable motion sensors to assess postoperative mobilization. JMIR Mhealth Uhealth 3:e78, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Appelboom G, Yang AH, Christophe BR, et al. : The promise of wearable activity sensors to define patient recovery. J Clin Neurosci 21:1089-1093, 2014 [DOI] [PubMed] [Google Scholar]
- 13.Ghomrawi HM, Baumann LM, Kwon S, et al. : Using accelerometers to characterize recovery after surgery in children. J Pediatr Surg 53:1600-1605, 2018 [DOI] [PubMed] [Google Scholar]
- 14.Sun V, Dumitra S, Ruel N, et al. : Wireless monitoring program of patient-centered outcomes and recovery before and after major abdominal cancer surgery. JAMA Surg 152:852-859, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wright AA, Raman N, Staples P, et al. : The HOPE pilot study: Harnessing patient-reported outcomes and biometric data to enhance cancer care. JCO Clin Cancer Inform 2:1-12, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Basch E, Deal AM, Kris MG, et al. : Symptom monitoring with patient-reported outcomes during routine cancer treatment: A randomized controlled trial. J Clin Oncol 34:557-565, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Basch E, Artz D, Iasonos A, et al. : Evaluation of an online platform for cancer patient self-reporting of chemotherapy toxicities. J Am Med Inform Assoc 14:264-268, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Altmann A, Tolosi L, Sander O, et al. : Permutation importance: A corrected feature importance measure. Bioinformatics 26:1340-1347, 2010 [DOI] [PubMed] [Google Scholar]
- 19.Doll KM, Barber EL, Bensen JT, et al. : The health-related quality of life journey of gynecologic oncology surgical patients: Implications for the incorporation of patient-reported outcomes into surgical quality metrics. Gynecol Oncol 141:329-335, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Meyer LA, Nick AM, Shi Q, et al. : Perioperative trajectory of patient reported symptoms: A pilot study in gynecologic oncology patients. Gynecol Oncol 136:440-445, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Armbruster SD, Sun CC, Westin SN, et al. : Prospective assessment of patient-reported outcomes in gynecologic cancer patients before and after pelvic exenteration. Gynecol Oncol 149:484-490, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]