Abstract
Objective
Describe participants’ perspectives about the feasibility of a virtual, physiotherapist-guided knee health program for people at risk of post-traumatic osteoarthritis after a sport-related knee injury.
Design
Qualitative description study nested within a quasi-experimental study evaluating the feasibility of the Stop OsteoARthritis (SOAR) with persons with sport-related knee injuries. SOAR includes: 1) one-time Knee Camp (group education, 1:1 exercise/activity goal-setting); 2) weekly home-based exercise/activity program with tracking, and; 3) weekly 1:1 physiotherapy-guided action-planning. Upon program completion, semi-structured 1:1 interviews were conducted with participants identified by convenience and maximum variation sampling (age, gender, program satisfaction). Open-ended questions elicited participants’ experiences with the program. Content analysis was conducted.
Results
12 women and 4 men [median (min-max) age; 30 (19–46) years] were interviewed. Four categories depicted participants' experiences: 1) ‘SOAR satisfies an unmet need’ portrayed the perceived relevance and need for a program that promotes knowledge about knee health and self-efficacy for independent exercise behaviour, 2) ‘Regaining control of knee health’ described how SOAR empowered participants and fostered a sense of ‘leading the charge’ to their own knee health, 3) ‘Social support encourages exercise participation’ highlighted that weekly physiotherapy interactions provided accountability for achieving exercise goals, and that relating to other participants was inspirational, 4) ‘Program refinements and barriers’ suggested enhancements to meet the needs of future participants.
Conclusions
Participants report the SOAR program to be acceptable, relevant, and empowering. Improved knowledge about one's knee health, self-efficacy, autonomy, and social support may encourage exercise adherence and self-management of future knee OA risk.
Keywords: Knee injuries, Qualitative research, Social support, Self-management, Rehabilitation, Osteoarthritis
1. Introduction
Knee injuries are an important risk factor for osteoarthritis (OA) [1] and are most common in adolescents and young adults participating in sport and recreational activities [2]. Although exercise therapy (activities prescribed to address specific therapeutic goals) [3] and physical activity are safe and effective solutions for promoting knee health after injury [4,5], there is no direct evidence that they prevent (delay or halt) post-traumatic OA.
Emerging consensus recommendations to prevent post-traumatic knee OA advocate for informational support (i.e., education) and exercise-based interventions that target potential risk factors and promote self-care through person-centered goals [6]. This guidance is consistent with previous work that identified autonomy, and timely informational and emotional support about short- and long-term knee health as important for recovery after anterior cruciate ligament (ACL) injuries [7,8]. As exercise is a behaviour, it may be helpful to leverage behavioural change techniques (BCTs) to promote participation in exercise-based interventions. Goal-setting, social support, and feedback on exercise behaviour are the most effective BCTs for promoting exercise in persons with MSK pain, and may be important for promoting behaviours to support life-long knee health [9]. It is unclear if an education and exercise-based intervention that incorporates BCTs can improve knee health in young persons at risk for OA.
SOAR (Stop OsteoARthritis) is a virtual, physiotherapist (PT)-guided knee health program that targets people discharged from formal care after a sport-related knee injury [10]. SOAR aims to increase knee muscle function and physical activity participation while improving one's capacity to self-manage their knee health and OA risk. We have recently demonstrated the feasibility (i.e., acceptability, practicality, implementation) of an abridged (i.e., 4-week) version of the SOAR program including preliminary efficacy for promoting self-reported physical activity, perceived self-management, and function [10]. The current study aimed to provide additional insight into participant's experiences of the program's feasibility and explore needs to refine the program in preparation for further evaluation.
2. Methods
2.1. Study design
A qualitative description study nested within a quasi-experimental study evaluating the feasibility of an abridged SOAR program. A qualitative description design was selected to provide a description of participants’ perspectives of the feasibility of the program and suggestions for refining [11]. Reporting followed the Standard of Reporting Qualitative Research [12]. The research was conducted between Oct-2020-April-2021 during the COVID-19 pandemic. The study was approved by the University of British Columbia Clinical Research Ethics Board (REB #H20-00158) and all participants provided informed consent.
2.2. Paradigm and theory
A pragmatist worldview was adopted to address a practical problem in the real world [13]. The theoretical underpinnings this study were Bowen et al.‘s (2009) approach to feasibility, which addresses acceptability, demand, implementation (i.e., facilitators and barriers), and limited efficacy of a program (Table 1) [14].
Table 1.
Components of Feasibility as per Bowen et al. [14].
| Feasibility Component | Definition |
|---|---|
| Acceptability | The degree of suitability, satisfaction, and attractiveness of the program to those delivering and participating in the program. |
| Demand | The perceived need for the program. |
| Implementation | The extent to which the program can be successfully delivered to intended participants, including identification of perceived barriers and facilitators for intended users. |
| Limited Efficacy | Signs indicating the new or novel idea, program, or process, shows promise of being successful with the intended population. |
2.3. Research context
The intervention was a 4-week abridged version of the SOAR program. SOAR aims to increase the capacity of persons with sport-related knee injuries to self-manage their knee health and OA risk and was developed based on previous research [7,8,15,16] and behaviour change theory [17]. SOAR has 3 components: 1) one-time virtual Knee Camp (group interactive education, 1:1 knee exam and exercise-therapy and physical activity goal-setting); 2) individualized weekly home-based exercise-therapy and physical activity with tracking, and; 3) weekly 1:1 PT-guided virtual exercise-therapy and activity action-planning with optional group exercise class. The program was delivered by four PTs (2 men, 2 women with 3–10 years of clinical musculoskeletal rehabilitation experience) who were certified in Brief Action Planning (BAP) 3 months prior. Table 2 summarizes the components of the program, including embedded BCTs. A full description of the program is published elsewhere [10,18].
Table 2.
Summary of SOAR interventiond.
| SOAR Component | Description | Behavioural Change Domaina | Behavioural Change Constructb | Behaviour Change Technique and Rationalec |
|---|---|---|---|---|
| Knee Camp | Interactive group education session (∼1 h) followed by 1:1 functional knee assessment and 1:1 exercise-therapy and physical activity goal-setting with a PT (∼50 min) |
|
|
Knowledge of condition/scientific rationale: provides information about topics related to knee health to improve awareness and self-management of current and future knee health. Skill assessment: allows for the program to be tailored to participants' needs, builds participants' confidence (i.e., self-efficacy) about their functional capabilities are. Individualized goal setting and action planning: BAP is used to co-develop personalized and meaningful SMART (specific, measurable, attainable, relevant, and time-bound) exercise therapy and physical activity goals for week one of the program. BAP aims to build participants' self-efficacy for behaviour change. Social support: provides an occasion for participants and PTs to establish a therapeutic relationship and forum for meeting other participants. |
| Individualized weekly exercise therapy and physical activity goal setting with tracking | Individualized exercise-therapy and physical activity program based on SMART goals. Physical activity was tracked using a Fitbit®. Exercise completion, pain and rating of perceived exertion was tracked using an online exercise platform called TeleHab®. |
|
|
Individualized exercise and physical activity program: promotes selection of exercises and activities that participants see as relevant, and consistent with their functional capabilities and goals, which facilitates exercise adherence. Self-monitoring and feedback on behaviour: provides feedback about physical activity participation and exercise completion to promote motivation and adherence. |
| 1:1 PT weekly counselling | Weekly 1:1 PT counselling sessions (∼15 min) where participants co-develop SMART exercise therapy and physical activity goals for the upcoming week using a BAP approach. |
|
|
Knowledge: provides information about knee health and exercises as requested. Individualized goal setting and action planning: PTs provide guidance on continued action planning using BAP for exercise and physical activity goal-setting and identification of barriers and problem-solving for exercising when necessary. Social support: forum for social connections with PT to foster a therapeutic relationship. |
| Weekly optional group exercise class | PT-guided group exercise class that targets trunk and lower body function (∼1 h). |
|
|
Knowledge: provides additional education about knee health (e.g., the rationale for exercises). Observations/monitoring with feedback: improve confidence and competence with exercises. Social support: forum for social connections between PT and other injured participants to build relationships. |
BAP=Brief Action Planning; SMART=Specific, Measurable, Attainable, Relevant, Time-bound; SOAR=Stop OsteoARthritis; PT = physical therapist.
Behavioural Change Domain are based on the Theoretical Domains Framework of behaviour change which identifies cognitive, affective, social and environmental influences on behaviour [17].
Behavioural Change Construct are theoretical factors relevant for behaviour change. Similar constructs/factors are grouped together to make up a behaviour change domain.
Behavioural Change Technique are tangible strategies applied to target a behaviour change construct.
Further details of the SOAR intervention can be found at Whittaker et al. (2022) [10].
2.4. Participant recruitment and sampling
Participants in the quasi-experimental study were recruited in two blocks (Block 1: Oct–Dec 2020, Block 2: Jan–April 2021) and included a convenience sample of persons (16–55 years) who had been discharged from regular healthcare after a sport-related knee injury (clinical diagnosis of knee ligament, meniscal, intra-articular tibio- or patellofemoral injury that required both medical consultation and disrupted sport participation) [19]. Exclusion criteria included: residency outside of the study region; no activity-related time-loss knee injury requiring medical attention; inability to communicate in English; pregnancy; inflammatory arthritis or systemic condition; lower limb injury, surgery, or intra-articular injection in the past six-months; no email address or daily access to a computer/internet; or refusal to wear an activity tracker.
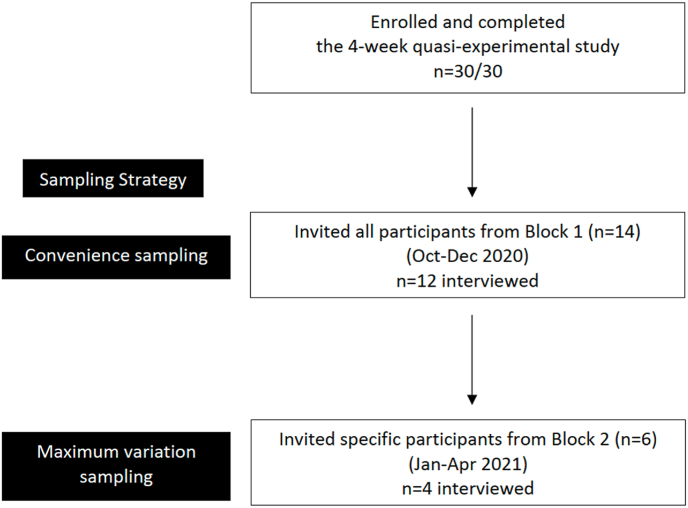
A multi-pronged approach was used to sample participants from the quasi-experimental study for this study (Fig. 1). First, all block 1 participants were invited to participate in 1:1 interviews. Then, maximum variation sampling [20] was used to select participants from block 2 who had different characteristics (i.e., age, sex/gender, SOAR program satisfaction, study PT) to those who participated from block 1. A heterogenous sample was sought as experiences may differ by program satisfaction, program PTs, and recovery from knee trauma differs by age and sex [16,21].
Fig. 1.
Flow chart of sampling from quasi-experimental study.
2.5. Data collection
After completing the SOAR program, participants were asked questions about their experience during semi-structured 1:1 interviews facilitated by an interview guide (Appendix). Questions focused on participants’: 1) knee injury journey (to build participant-interviewer rapport), 2) experience with the SOAR program, and 3) perceptions of their knee health management before and after the SOAR program.
Interviews were conducted by the first author through a videoconferencing platform (Zoom®), audio-recorded and transcribed. Sampling ceased once enough data was collected to provide a meaningful and comprehensive reflection of participants’ experiences.
2.6. Analysis
Transcripts were verified and de-identified by the first author. Data analysis was led by the first author in regular consultations with the research team. A conventional content analysis that followed an abductive approach was adopted [22]. First, data immersion (preliminary transcript reading and re-reading) provided an opportunity to become familiar with the data. This was followed by initial coding of responses into area of focuses for feasibility and SOAR components (see Table 1) using a customized excel form. Initial categorization in this format was a strategy to help organize the data and gain a sense of the repeated counts of a particular type of response (e.g., how many participants reported barriers with the tracking tools). This structure was too rigid to capture the scope of the data and limited the analysis and author's ability to provide a nuanced and rich description of participants‘ experiences. Therefore, an inductive approach was employed to identify any new categories, with all transcripts recoded and managed with NVivo v12.4.0. First, codes were identified by reading each transcript. Second, categories were formed by grouping similar codes together. Categories and sub-categories were refined iteratively, allowing for more latent themes or relationships to be explored and identified. Despite initially using a deductive approach to organize the data, the final categories were derived inductively from the data. Given that gender may play a role in how individuals perceive exercise and strength training [23], and that social support needs may differ by sex and gender after knee injuries [24,25], categories were also reviewed with a gender lens throughout the analysis.
2.7. Rigor
The first author had an insider-researcher lens as a PT within the SOAR program (i.e., primary PT for 7/16 participants interviewed and weekly group class instructor). This unique perspective provided in-depth knowledge about the nuances of the program which was beneficial when interviewing participants and analyzing the data (e.g., understanding the context allowed for deeper exploration of interview responses and during data analysis). Reflexive journaling [26] was employed to understand how the first author may have influenced the generation and interpretation of the data. Two senior qualitative researchers also met regularly with the first author to discuss any tensions being an insider-researcher. Memoing [27], field notes [28], an audit trail of analytic decisions, and regular meetings with team members and patient-partners were used to aid in flushing out interpretations (e.g., challenging old and new categories) and to promote trustworthiness and transparency of the findings [29].
2.8. Patient-partner involvement
Three patient-partners and co-authors, assisted in co-developing the interview guide, reviewed the categories/preliminary findings to help identify/clarify relationships, and were involved in the manuscript preparation. This included a young woman with lived experience of a sport-related ACL reconstruction (AP), a middle-aged woman with lived experience of a sport-related ACL reconstruction and recent knee OA diagnosis (MM), and a middle-aged woman with lived experience of a sport-related ACL reconstruction, knee OA, and knee arthroplasty (TSL).
3. Results
20 participants (14 from block 1, 6 from block 2) were invited for interviews and 16 (12 from block 1, and 4 from block 2) agreed to participate. Of those, 12 identified as cis-gendered women and 4 as cis-gendered men, with a median age of 30 (minimum-maximum: 19–46). Participants’ characteristics are summarized in Table 3. Interviews ranged from 41 to 73 min and took place a median of 8 (minimum-maximum, 3–31) days after completing the SOAR program.
Table 3.
Participants’ characteristics.
| Participant | Gender | Age | Injury Age | Injury Experiencea | Injury Type | Primary Pre-injury Sport | SOAR Satisfactionb | Online Delivery Satisfactionb |
|---|---|---|---|---|---|---|---|---|
| 1 | Women | 31 | 14 | Chronic | ACL tear | Soccer | 10 | 10 |
| 2 | Women | 45 | 44 | Recent | ACL tear | Running | 10 | 10 |
| 3 | Women | 25 | 22 | Recent | ACL tear | Volleyball | 9 | 9 |
| 4 | Women | 36 | 32 | Recent | Dislocated kneec | Basketball | 10 | 10 |
| 5 | Men | 46 | 32 | Chronic | ACL tear | Ultimate frisbee | 10 | 10 |
| 6 | Women | 30 | 29 | Recent | ACL tear | Volleyball | 9 | 10 |
| 7 | Men | 19 | 18 | Recent | Diagnosis unknown | Volleyball | 9 | 9 |
| 8 | Women | 46 | 36 | Chronic | Patella dislocation | Rugby | 10 | 10 |
| 9 | Men | 32 | 27 | Chronic | ACL tear | Soccer | 8 | 10 |
| 10 | Women | 34 | 32 | Recent | ACL tear | Volleyball | 10 | 10 |
| 11 | Women | 30 | 22 | Chronic | Meniscus tear | Ultimate frisbee | 10 | 10 |
| 12 | Women | 31 | 23 | Chronic | ACL tear | Soccer | 10 | 10 |
| 13 | Women | 25 | 21 | Recent | Dislocated kneec | Wakeboard | 8 | 10 |
| 14 | Women | 23 | 17 | Chronic | Dislocated kneec | Skiing | 8 | 9 |
| 15 | Men | 23 | 18 | Recent | ACL tear | Rugby | 10 | 10 |
| 16 | Women | 23 | 21 | Recent | Patella dislocation | Rugby | 10 | 10 |
| Median (min-max) | 30 (19–46) | 22.5 (14–44) | 10 (8–10) | 10 (9–10) |
ACL = anterior cruciate ligament.
Chronic = injury 5 years or greater, Recent = injury less than 5 years.
Satisfaction scores were captured with an online exit survey [10] where participants rated their satisfaction of the SOAR program on a 0–10 point Likert scale, with higher scores indicating greater satisfaction.
Dislocated knee injuries all included ACL tears.
3.1. Findings
Key findings are presented in a narrative form with sub-categories italicized. Four main categories were generated from the data analysis: 1) SOAR satisfies an unmet need; 2) Regaining control of knee health; 3) Social support encourages exercise participation; and 4) Program refinements and barriers. Table 4 provides a breakdown of the categories with additional supporting quotes.
Table 4.
Breakdown of how categories and sub-categories were operationalized and organized with supporting quotes.
| Category | Sub-Category | Supporting Quotes |
|---|---|---|
|
1. SOAR satisfies an unmet need This category depicts the perceived value, demand, and acceptability of the program. It supports that the structure of SOAR (i.e., program components) does facilitate self-care by promoting knowledge about knee health and self-efficacy for independent exercise behaviour. |
Design met needs of participants -supports the structure/components of SOAR are acceptable |
“Overall, it's a ten out of ten. [laughs] It was great. Going in I wasn't sure how it was going to be, but I feel it was a very, like supportive role in terms of, you know, holding me accountable to doing my exercises. Also educating me about my knee more. Especially that first session, that was great cause I learned a lot from that.” (P15) “The ability to meet up with a physio without having to drive somewhere was really, really helpful. The knee camp totally fine online and getting to meet each other in breakout rooms and then coming back, I think that actually works better than being in-person. I think people are a little more confident with talking through Zoom than if we were all in-person in a big group setting.” (P12) |
| Motivation to join SOAR -identifies pre-program motivations and the type of participants who enrolled in the SOAR program |
“You know I have nothing else to do at the moment [due to COVID], [SOAR was an] opportunity to work on my knee, which was great; free physio – you know that was really cool. Fitbit, I still wear it.” (P06). “I genuinely am concerned about getting arthritis, especially like early onset sort of osteoarthritis … So that was kind of one of the things I was just hoping that [SOAR] could give me something to put in the back of my head for the next whatever 10, 20 years; to make sure that I implement certain things into my lifestyle to ensure that I don't have that sort of early onset arthritis.” (P04) |
|
|
2. Regaining control of knee health This category expresses participants' experience of feeling empowered to manage their knee health. This involved changing perceptions towards their knee health and promoting autonomy and self-efficacy. |
Education helps change perceptions on knee health -highlights the importance of informational support in the program |
“It was very informative in terms of like explaining, you know, what is important in making sure your knee is healthy. And just like long term goals that you're supposed to assign for yourself and how to do that.” (P15) “So the knowledge piece was a huge one for me, and then like I said too, I feel I have the tools and what I need to do in the future.” (P02) “I really enjoyed [Knee Camp]. I thought it was incredibly informative, and as I previously mentioned, it gave me so much motivation to invest in the SOAR program, and invest in my knee health knowing, you know facts about OA and what it really was.” (P16) |
| Gradual building of autonomy -describes participants experience with the BAP technique, goal-setting |
“[Goal-setting] was good. It was, the study PT didn't leave it all up to me, but didn't just tell me what I had to do. So it was, it was a nice, nice mix of ‘okay so what do you want to get out of this? Okay so what do you want to do?‘ … So I just found it really, really helpful.” (P08) “I was definitely surprised that it was more me picking exercises I wanted to do. I was expecting more to be like told … I think it was definitely beneficial to do it yourself because it kind of teaches you how to [pick exercises], once you're done [the] study.” (P14) “I'm also looking to the study PT, as much as I want flexibility. I'm also looking to the physio as a guide. So maybe a little bit more guiding in terms of the solutions, and here's what I think would be good for your knee … And I get that the study PT wanted me to be part of the process, but every once in a while, I just felt it was just me. I feel like I was the one giving the exercises, right? So I would like some, some more leadership I guess, in that sense … I don't know just ask, in terms of like ‘oh do you – do you want my advice?’ … But yeah just ask, ‘do you mind if I butt in or do you mind if I give you another idea, or my opinion of that or how you can improve that?’ Just more simple things like that I guess.” (P09) |
|
| Changes experienced from the program -reports participants noticing meaningful change in physical (e.g., symptom relief), and/or psychological domains (e.g., improved confidence and changes in perceptions toward exercising) |
“I can run, it didn't hurt, and I could [now] do the [PT] exercises … By the end of the four weeks, there was no pain behind the kneecap anymore … there was less crunching … It was really cool, in four weeks, I mean [4 weeks]'s nothing, and what, 45 min a week basically.” (P08) “I'm less afraid to kind of do stuff, and I'm less likely to just sit on my ass for the week and do nothing, because I know that it’s actually – now that I know scientifically that its actually good for me to continue to move. I think that's been probably the thing I've taken from this program.” (P04) “I am continuing being more diligent with my exercises than I ever was before the study. [laughs] And I feel like I'm more empowered to do things for this left leg. And I have a plan so that's what I'm doing to boost confidence, just using it more, but using it in a way that I know I can do.” (P10) “There definitely is a way that I'll differ in the way that I manage my knee injury. Cause earlier when I got injured there was just a lot of uncertainty about what to do. But now it's like, ‘okay I have to keep moving, for osteoarthritis.” (P07) |
|
| Feeling hopeful towards the future -outlines the mindset/optimism participants felt when speaking of their general experience of the program |
“I'm really grateful to have been a part of [SOAR] and to have received the information I have; and gotten the tools that I have from it. I think it would be extremely valuable for anybody else going [through this with] their knee. I wish that I had, had something like this ten years ago when I was still going through so much, and [the knee injury] was still so new and scary, and discouraging. I think something like this would have been really beneficial.” (P01) “They made it very easy for us, you know, force us to think about our knee health and make it a priority. So that's a good thing that I participated in this study, because without it, I don't think I would be where I'm at right now.” (P15) “Yeah I think definitely made me feel in charge of my knee health again, and that I kind of know what to do and I feel I also just have resources available to me, if something goes wrong or if I don't know what I'm doing, which was a big thing. And I just again, feel I'm not just doing it on my own, I just have more resources available now, and kind have some clearer guidelines of how to get to my goals.” (P03) |
|
|
Social support encourages exercise participation This category outlines how the support received from the study PTs, research team, or other program participants impacted participants' exercise adherence. This involved creating a supportive environment, providing accountability, and having a shared injury experience to help promote exercise adherence. |
Creating a shared injury experience -describes the importance of meeting and connecting with participants and other research members |
“I think it just the social aspect of it, makes people more inclined to do the work, as well, and realizing they're not the only one doing it. So I think that's true with most exercise and that's why people like going to the gym because there's other people there and they're like, ‘I'm not the only one that has to work out all the time to keep fit, these other people are doing it too,’ so yeah.” (P11) “We all went around and we talked about how we hurt ourselves, or what is our best winter sports and all that; get to know people. That was nice, I liked that. But yeah it [was] nice to hear how other people hurt themselves, not in a sadistic way, but just you know share, feel some comradery.” (P09) “I really like the weekly classes, I liked that you come together as a group and you're going through it all together, and you're learning a little bit about people's stories along the way. And I'm definitely more motivated in a group setting than when I'm just doing them on my own. I liked variety of workouts, I liked the vibe. I really liked them.” (P01) |
| Accountability promotes exercise engagement -reports on the value of weekly PT counselling |
“I think for me its motivation and accountability [with the weekly PT visits]. And it's just having someone being like ‘hey you're doing a great job, what you're experiencing is normal, you know. Here are some tips to keep improving in the following week, and like keep going.’” (P01) “Felt like [the weekly PTs visits] are needed; they definitely were helpful. ‘Cause seeing people, someone on a weekly basis, like if you do lose track, cause I feel like if I didn't see the study PT on a weekly basis, I would have in the second week, the compliance would go down a lot in terms of doing the physio exercises and doing physical activity.” (P07) |
|
| Creating a supportive environment -details the interactions across the SOAR program that extended beyond just exercising |
“And obviously my study PT and I have had, like made this great relationship, which I've really, really enjoyed, and I feel that like I would say my physio experiences before haven't been so personal. And like it's always been about rugby and my knee, opposed to this more holistic approach where it's like all these things involved; and we've talked very openly about that which I've enjoyed.” (P16) “I think that was extremely important to have that one-on-one time and to know that you could ask any questions about [anything], and it was just focused on your health, and yeah that was really important I think. And I'm assuming all the physiotherapists are like this, but my physiotherapist was very much like ‘you're doing a great job, or this is great, or I'm so proud that you're doing this thing’ or whatever. And I think that positive reinforcement for people, it just goes a really long way.” (P11) |
|
|
Program refinements and barriers This category describes suggested refinements to help meet the needs of future participants. The most common suggestion was a hybrid program to allow for more social connection with PTs and/or program participants and use of self-tracking tools (refer to Table 5 for more details). |
Suggestions and improvements -outlines ideas to improve the program |
“I just have basically nothing but good things to say about it, and I loved it, and yeah the only complaint is that it should have been longer.” (P11) |
| Tracking only helped some with motivation and accountability -describes participants' experiences with self-tracking tools in the program |
“I felt like [the Fitbit] also just kind of kept me accountable, like it kind of it – it shows like how many minutes you're active and so it was almost like a challenge for me to be like I'm going to like complete it all today. Or like I'm going to get all my steps in, and so yeah I felt like it was kind of like a good motivator.” (P03) “I mean mostly I find the accuracy of it is just like the steps, so that's like mostly what I used it for … I guess I would prefer to use a Fitbit with [a] heartrate or something on it, cause then it would [pick up] you actually working out at this time.’” (P10) “[TeleHab] was fine, I wouldn't say it was great, I wouldn't say it was terrible. It was just whatever, it was good. I'm glad there was an app. I liked that there was an app, it was nice to – you know refer [to it] in the gym … So I enjoyed that aspect, but I wouldn't, not giving it a gold star.” (P06) “[I felt] it wasn't necessarily … It was just kind of like I remembered what [my exercises were], and I kind of almost forgot about [the app], that it was there, that I could record what I'm doing if I wanted the study PT to see.” (P07) “I didn't really like the App and I didn't want to have to go into the app to record that I was doing the exercises.” (P04) |
|
| Barriers to the program -identifies any barriers to consider going forward |
“I mean, I guess its maybe a question to you of how effective [the knee assessment] actually is, like just seeing me do movement as opposed to like actually manually like being there and getting to touch my knee.” (P03) “I really liked the – the group session, it just didn't always work well for me, from a timing front.” (P02) |
3.2. Category 1: SOAR satisfies an unmet need
Participants highlighted that the program satisfied unmet needs for understanding their knee health despite receiving prior healthcare for their knee injury. When asked why they enrolled in the study, participants expressed three motivations: 1) recover fully from their knee injury (most common amongst those recently injured); 2) get back on track with an exercise program as the COVID-19 pandemic derailed their exercise behaviours (most common amongst those with chronic knee injuries); or 3) gain knowledge about their knee health and how to reduce their risk for OA. Pre-program motivations were closely tied to participants feeling that no support existed after they were discharged from care for their acute knee injury, “… knowing there's a long-term program, I didn't even think that was an option” (P16).
Participants identified the Knee Camp and weekly PT counselling sessions as the most important components as they shifted the focus beyond exercise: “the counselling is just as much important as the exercise [given]” (P10). Although there was initial hesitancy with participating in a virtual program, all participants reported no issues with a virtual program. Some participants felt “[the program] works better than being in-person,” (P12) as it was more accessible, convenient, and manageable; however, others felt some in-person element would increase connectedness with their PT and other participants.
3.3. Category 2: Regaining control of knee health
A key concept underlying why participants value the program was how it helped them to “regain control,” which was strongly driven by education helping to change their perceptions towards their knee health. All participants found Knee Camp to be informative as many felt “in the dark about [OA]” (P04). The knowledge gained during Knee Camp, and reinforced throughout the program, gave participants a new perspective of OA that either empowered them: “it's made [OA] less scary and made me feel empowered that I have control over the situation and how my knee [is] long-term” (P14) or, more confident to exercise: “that confidence of [knowing] putting weight on your knee [is ok], is a huge thing for a lot of people,” (P09).
BAP, a study feature that allowed PTs to counsel participants to co-develop individualized SMART goals, helped participants gradually build autonomy over their knee health. While participants acknowledged the importance of making autonomous decisions, they valued their PTs expertise. This perceived value about expert guidance was more commonly reported amongst recently injured and younger participants. Despite a desire to balance autonomy and guidance, most participants stated that having options and choices on exercises led to greater exercise adherence.
I really liked the fact that the study PT gave me an option to say ‘what kind of things do you enjoy doing?’ It wasn’t just ‘here’s what I’m going to give you’ … So I had the opportunity to choose things that I would be more motivated to complete. (P01)
Participants also highlighted the changes experienced from the program reinforced their sense of control with their knee health. These changes included: reduced knee pain, more knee confidence during exercise, or generally feeling empowered to engage in ongoing care of their knee. When asked if they would change the way they approach managing their knee in the long-term, many stated they felt hopeful towards the future: “I felt so helpless before, as far as developing [OA]; and now I feel I have more control over it, which gives me more motivation to be doing these [exercises]. So hopefully in the long-term, I'll be much better off” (P16).
3.4. Category 3: social support encourages exercise participation
Participants valued the support provided by their study PT, the research team, and other participants during the program. The weekly PT sessions were essential because accountability promoted exercise engagement: “I think having someone you meet with on a regular basis, visually and having that commitment, again keeps that engagement and that accountability” (P02). Although the program was delivered virtually, most participants commented on the therapeutic relationship when describing the weekly PT sessions: “I felt I really connected with my PT, it was [the] perfect pairing,” (P08). Some participants even went as far to state: “I found it more personal than previous physio experiences,” (P16). Consistent, weekly PT interactions fostered this connectivity alongside creating a supportive environment, which was achieved by providing positive reinforcement, creating a non-judgmental and open environment, helping to build self-efficacy, and personalizing the program:
Getting to interact with the study PT every week, they didn't look at me like I’m damaged or anything. It was just getting to talk to someone who knows my story but is there to help, and so I felt that was really supportive. (P03)
Social support influences were also reported when meeting other participants either through Knee Camp or group exercise class. Meeting other participants and the research team (many with relatable knee injuries) created a shared injury experience by providing opportunity to express various perspectives on experiencing a knee injury, which was motivating and inspirational:
I think definitely [meeting others] helps you; 1) [not] feel so alone and not the only one going through this; 2) it can also be inspirational when you can see people that have gone through the experience and they’ve come out on top, or they’ve been able to get back to their sport. I think that’s nice cause you see, ‘oh it is possible.’ (P11)
3.5. Category 4: program refinements and barriers
Participants reported mixed feelings about the tools used to self-monitor exercise and physical activity (i.e., Fitbit® and TeleHab®). Some participants indicated the tools encouraged them to exercise, while some felt, “the Fitbit® was not accurate at all” (P05) and a Fitbit® with a heartrate monitor would be more helpful. Other barriers are summarized in Table 5. The most suggested refinements for the program were to consider a hybrid program (online and in-person), longer program duration, and ongoing education (e.g., further resources about knee health/OA). Additional suggestions can be found in the Appendix 2.
Table 5.
Experience and barriers to SOAR components.
| SOAR Component | Overall Experience | Reported Barriers |
|---|---|---|
|
Online Delivery |
Participants reported minor concerns about a virtual program (e.g., lack of in-person interaction). They had no issues with the online delivery, with some preferring this approach. Most participants indicated a hybrid delivery would be ideal but enjoyed the convenience and accessibility of the online delivery. Knee Camp and group exercise classes were the components that most reported could have benefited from being in-person. |
Some participants reported a perceived inability to socially connect with other participants and PT because SOAR is delivered online. |
|
SOAR Component |
Experience |
Barriers |
| Knee Camp | Participants reported this was a valued and essential component of the program (see category 1 above). | No barriers reported. |
| 1:1 Knee Assessment | Participants were generally satisfied with the virtual 1:1 assessment and appreciated how it helped to tailor the program to their individual need. | Some participants questioned the validity of an online exam due to the lack of ‘hands on’ or perception that PTs could not observe movements effective. |
| 1:1 Weekly PT Counselling | Participants reported the weekly counselling as an integral component of the program (see category 2 above). | No barriers reported. |
| Weekly Exercise and Physical Activity Goal-setting and Tracking | Participants reported that the weekly goal-setting assisted to address barriers to exercises and kept them accountable. Half of the participants found the tools to track exercise and physical activity (i.e., Fitbit® Inspire and TeleHab®) helped promote accountability and exercise engagement, while others felt the tools were not helpful or necessary to the study. |
Participants reported the main barriers to completing weekly exercise goals was time, lack of motivation and space or equipment availability (particularly for participants with more advanced exercises incorporating jumping or running). Some participants reported these tools were not important to the study. Barriers to using Fitbit® use included: perceptions of accuracy, lack of automatic synchronization for some activities (e.g., cycling) and a lack of awareness of the Fitbit® features. Barriers to TeleHab® use included: relevance, time, technical issues (unable to easily access the app on an Android device, initial set up), and lack of clear instructions. |
| Optional Weekly Group Exercise Class | Women participants were more likely to attend group classes. However, several men that did not attend reported that they were interested but it conflicted with their schedule. Of the men that did attend, all reported the class was fun, encouraging, and challenging (see category 2 above). | Some participants reported they were not able to attend due to scheduling issues and some indicated issues balancing the demands of their individualized program and the classes (e.g., too sore from physical activity or exercise program to attend class) |
4. Discussion
Our findings suggest that the unique design of the SOAR program is acceptable, relevant, and empowering for persons with sport-related knee injuries at risk of post-traumatic OA. Participants expressed a high demand for the program as it satisfied unmet knee health needs and knowledge around OA. Positive experiences of the program were centralized around regaining control over one's knee health which stimulated a sense of empowerment and hope for their future. Social support from the program PT and other participants were perceived as valuable facilitators for exercise engagement, as were informational support, autonomy, self-efficacy, accountability, and the individualized nature of the program. The most valued components of the program were Knee Camp and the weekly PT counselling, while tools for self-monitoring exercise and physical activity were less valued. Although refinements were suggested, all participants felt the program improved their ability to manage their knee health.
4.1. “I'll differ in the way that I manage my knee injury”
Participants reported informational support and 1:1 PT counselling were the main drivers of exercise. These elements reportedly fostered a sense of independence and confidence to exercise, which was one reason participants felt the program was valuable. Early knowledge about OA risk management was desired and reportedly lacking for many participants. This was consistent with previous work demonstrating youth with knee injuries feel there is a need to balance their activity priorities and future knee health [8]. Taken together, this suggests that interventions for OA prevention may be needed early after injury, despite contrary belief that young persons with knee injuries either don't care about OA, or simply accept their future risk.
Participants stressed the value of regular PT guidance about exercise, including how to pace (i.e., using symptoms and rating of perceived effort to adjust dose). This finding is consistent with evidence 20–30 years following an ACL tear [30] and knee OA [31] demonstrating the need for PT guidance may not resolve over time. This is not surprising given that exercise and physical activity are behaviours, suggesting that interventions that aim to change and maintain behaviour need to move beyond simply exercising. In fact, a similar approach utilizing BCTs alongside PT interventions has been shown to be effective in improving physical activity adherence in older adults with lower limb OA [32].
A unique aspect of the SOAR program is the integration of a motivational interviewing technique (BAP) to guide weekly exercise and physical activity goal-setting. This approach was adopted to gradually build participants' autonomy and knee self-efficacy for exercising. BAP encourages a partnership between PT and participant to promote health behaviour change [33]. Participants reported the BAP technique took some adjustment based on the degree of autonomy they desired. For example, some participants wanted to be ‘told what to do.’ Traditionally, PT care often reflects a hierarchical medical model where patients are meant to be passive recipients of care provided by healthcare practitioners [34]. The SOAR program deviates from this hierarchical model and encourages participants to actively engage in the decision-making process and is likely to be experienced as different from previous PT encounters. In time, participants reported the BAP approach was more collaborative and patient-centered than past healthcare encounters, leaving them to feel more confident to manage their knee after the program was over. This suggests that SOAR's novel approach may improve one's self-efficacy to independently manage their knee health and future OA risk, however, further testing is needed.
While suggestions and refinements were provided, participants indicated the structure of the program (i.e., Knee Camp, 1:1: PT counselling with goal-setting, optional group class) should remain unchanged. Self-monitoring or tracking was the program component most discussed as needing to be refined. Despite the effectiveness of apps and activity trackers for increasing physical activity in adults [35]; only half of the participants felt the self-monitoring tools were helpful, suggesting the utility of these tools may vary individually. One explanation for this is the lack of feedback provided to participants regarding how this data can be used in subsequent weeks of the study. In a systematic review investigating BCTs to promote physical activity in persons with physical disabilities, self-monitoring behaviour (e.g., using an activity tracker) with feedback was found to be the most effective to promote physical activity [36]. Therefore, the inclusion of any tool to promote exercise adherence needs to be accompanied by meaningful feedback or it may be perceived as not helpful.
The online delivery of the program was considered both a barrier and facilitator. Online delivery made the program accessible, convenient, and reduced participant burden related to travel. Conversely, the online 1:1 virtual assessment was perceived as less effective compared to in-person assessments because there was no ‘hands-on’ or ability to observe movement up close. These negative perceptions of online delivery is contrary to findings of a systematic review of RCTs which reported telerehabilitation as being just as effective as other PT interventions [37]. Providing patients with information about the effectiveness of virtual care and acknowledging how access and comfort to internet and digital interventions may impact patient experiences [38,39] should be considered in future online interventions. However, respecting that some patients may value in-person over online (or vice versa) is important to ensure care remains individualized. A solution may be to consider a hybrid program.
4.2. “The social aspect of it, makes people more inclined to do the work”
Our findings highlight the role social relationships could play in promoting exercise behaviour. This is not surprising given that social support has been consistently identified as a facilitator of exercise across various populations [9,32,40]. In our study, social support appeared to influence exercise engagement in three ways. First, informational support was tied to changing perceptions of OA and exercising. Second, continuous emotional and esteem support from the PT promoted accountability to exercise. Lastly, emotional support was received by connecting with other participants and the research team, helping to validate participants own experiences leading them to be more motivated and inspired to exercise. The supportive environment and strong connection with the PT were key features of the program, despite being online. In fact, we were surprised that some participants reported that they felt a stronger relationship with their program PT over previous in-person encounters. This was reassuring as a strong therapeutic relationship has been shown to influence patient outcomes [41,42], and it was evident we were able to recreate an environment to foster a connection between the PT and participant with an online program. These findings reiterate the impact of contextual factors (e.g., relationship between the PT and patient) on shaping how interventions will be taken up by participants in research or clinical settings. While the need for social support following knee injuries has been reported [7], future research is needed to understand how we can build and leverage these social networks during rehabilitation and long-term management of persons with knee injuries to promote recovery.
We attempted to look at the experiences of participants from a gender lens but no differences were identified. Attendance at the optional group exercise classes was largely by women. While pacing was the most evident reason reported for not attending the classes, women in our study often discussed the importance of connecting with other participants. This is consistent with past research which identified gender difference to how patients respond to social loss as they age after ACL injuries, with women (unlike men) discussing difficulties with friends they exercised with [30].
4.3. Research and clinical implications
Prevention of post-traumatic knee OA is complex and requires interventions that address real-world complexity and consider multiple factors that promote self-care of OA risk through exercise and physical activity. Our findings suggest that exercise-based interventions that incorporate BCTs are relevant and empowering for young persons with sport-related knee injuries, and that the SOAR program demonstrates early promise. Although participants in our study report the novel approach of SOAR is acceptable and has limited efficacy, this does not serve as evidence of the efficacy or effectiveness of the program and that separate appropriately designed studies, which are currently under way [18], are needed.
As exercise and physical activity are behaviours, clinicians need to move beyond only providing exercise to foster behaviour change. Promoting autonomy and self-efficacy through techniques like BAP and individualized goal-setting, providing social support and accountability through regular check-ins may be strategies clinicians can use to facilitate long-term exercise adherence.
4.4. Strengths & limitations
Although the participants in this study were heterogenous across various characteristics, no participant reported low satisfaction or poor-quality PT encounters due to the lack of variability of these features in the recruitment pool. Therefore, our findings may be more reflective of participants with positive experiences of the program. The first author's prior relationships with participants may have influenced participants' responses or willingness to participate in the interviews. To mitigate this, we used purposive sampling to ensure equal representation of participants across all PTs. The richness and diverse responses suggest participants shared their own experiences and likely did not respond to appease the interviewer. Finally, our study involved various patient-partners throughout the study, enriching the interpretation and trustworthiness of the data.
4.5. Conclusion
Participants report an abridged version of the SOAR program satisfied an unmet need, was acceptable, relevant, empowering, and promising for promoting exercise adherence and self-management of OA risk after a knee injury. Future studies aimed at determining the efficacy of the SOAR program are warranted.
Ethical approval
University of British Columbia Clinical Research Ethics Board (REB #H20-00158).
Studies involving humans or animals
Clinical trials or other experimentation on humans must be in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Randomized controlled trials should follow the Consolidated Standards of Reporting Trials (CONSORT) guidelines and be registered in a public trials registry.
Studies involving experiments with animals were in accordance with institution guidelines Please sign below to certify your manuscript complies with the above requirements and then upload this form at https://www.editorialmanager.com/oac/
Author's contribution statement
LKT and JLW conceived the study. LKT and JLW were responsible for participant recruitment, and JLW secured funding. LKT conducted and transcribed all interviews. All authors contributed to the interpretation of the data. LKT drafted the first versions of the manuscript. All authors contributed to and approved the final manuscript.
Role of funding source
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Funding
Funding to conduct this study came from the BC SUPPORT Unit, Canadian MSK Rehab Research Network (CIHR FRN: CFI-148081) and Arthritis Society. JLW is supported by the Michael Smith Foundation for Health Research and the Arthritis Society. LKT is supported by a Canadian Institutes of Health Research Fellowship. LCL is funded by a Tier 2 Canada Research Chair in Patient-oriented Knowledge Translation and holds the Harold Robinson/Arthritis Society Chair in Arthritic Diseases.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors would like to acknowledge the administrative support of Shireen Divecha, Kiran Dhiman, and Hussein Mamdani as well as contributions from Christina Le, Justin Losciale, and Declan Norris who participated as physiotherapists in the study.
Handling Editor: Professor H Madry
Appendix 1.
Interview Guide
Interview Guide Goal: To elicit information about participants experiences and perspectives of the SOAR program, to inform future modifications.
| Primary Question | Prompts and Probes |
|---|---|
|
General background questions (build rapport and context) To start, I like to hear a little about your knee injury and experience in sport and exercise. | |
| Tell me a little bit about the sports or exercise you enjoy? |
|
| Can you briefly tell me about your prior knee injuries? |
|
| Prior to the SOAR program, what did you do to take care of your knee? |
|
| What is the role of others in your rehabilitation or recovery of your knee injury? |
|
| What role do you see yourself playing when it comes to managing your knee injury? |
|
|
SOAR program questions (assess experiences with the program) I would like to hear about your experiences with and perspectives on the SOAR program. | |
| Why did you decide to participate in the SOAR program? |
|
| What was your experience with the SOAR program? |
|
| Tell me about your experience of having this program delivered online? |
|
| Tell me about your experience of the ‘Knee Camp’. |
|
| What was your experience with the breakout session during knee camp? |
|
| Exercise and goal component of SOAR program (assess experiences with the program) | |
| Tell me about your experience with the exercises you were prescribed. |
|
| Tell me about your experience working with the physiotherapist to set goals for your home exercises and physical activity. |
|
| Tell me about your experience with the weekly physiotherapy follow up and activity counselling? |
|
| What was your experience weekly group-based physiotherapy exercise class? |
|
| Self-monitoring components of SOAR program | |
| What was your experience using TeleHab? |
|
| Tell me about your thoughts on using the Fitbit to track your physical activity? |
|
| What was your experience using the Zoom platform? |
|
| Closing questions (provide opportunity to share) | |
| Now that you had a chance to reflect and share your experience about the SOAR program, tell me a little if this program changed the way you approach how you will care for your knee? |
|
| Is there anything you would like to share or add to the interview about your experience with SOAR program? |
|
APPENDIX 2.
Improvements and suggestions to improve the SOAR program
Table 1.
Overview of suggestions for improving SOAR reported by 2 or more participants
| SOAR Program or Component | Suggestions |
|---|---|
| Overall |
|
| Knee Camp (Education) |
|
| Knee Camp (1v1 PT Assessment) |
|
| Exercise Goal Setting and 1:1 weekly counselling |
|
| Technology for Exercise and Physical Activity Tracking |
|
| Optional Group Weekly Classes |
|
References
- 1.Snoeker B., Turkiewicz A., Magnusson K., Frobell R., Yu D., Peat G., et al. Risk of knee osteoarthritis after different types of knee injuries in young adults: a population-based cohort study. Br. J. Sports Med. 2019;54:725–730. doi: 10.1136/bjsports-2019-100959. [DOI] [PubMed] [Google Scholar]
- 2.Gianotti S.M., Marshall S.W., Hume P.A., Bunt L. Incidence of anterior cruciate ligament injury and other knee ligament injuries: a national population-based study. J. Sci. Med. Sport. 2009;12:622–627. doi: 10.1016/j.jsams.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 3.National Center for Biotechnology Information. Exercise therapy. Published Accessed: April 24, https://www.ncbi.nlm.nih.gov/mesh/68005081.
- 4.Whittaker J.L., Roos E.M. A pragmatic approach to prevent post-traumatic osteoarthritis after sport or exercise-related joint injury. Best Pract. Res. Clin. Rheumatol. 2019;33:158–171. doi: 10.1016/j.berh.2019.02.008. [DOI] [PubMed] [Google Scholar]
- 5.Fransen M., McConnell S., Harmer A.R., Van der Esch M., Simic M., Bennell K.L. Exercise for osteoarthritis of the knee. Cochrane Database Syst. Rev. 2015:1465–1858. doi: 10.1002/14651858.CD004376.pub3. 10.1002/14651858.CD004376.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Whittaker J.L., Culvenor A.G., Juhl C.B., Berg B., Bricca A., Filbay S.R., et al. OPTIKNEE: 2022 consensus recommendations to optimise knee health after traumatic knee injury to prevent osteoarthritis. Br. J. Sports Med. 2022;56:1393–1405. doi: 10.1136/bjsports-2022-106299. [DOI] [PubMed] [Google Scholar]
- 7.Truong L.K., Mosewich A.D., Holt C.J., Le C.Y., Miciak M., Whittaker J.L. Psychological, social and contextual factors across recovery stages following a sport-related knee injury: a scoping review. Br. J. Sports Med. 2020;54:1149–1156. doi: 10.1136/bjsports-2019-101206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Truong L.K., Mosewich A.D., Miciak M., Pajkic A., Le C.Y., Li L.C., et al. Balance, reframe, and overcome: the attitudes, priorities, and perceptions of exercise-based activities in youth 12–24 months after a sport-related ACL injury. J. Orthop. Res. 2021;40:170–181. doi: 10.1002/jor.25064. [DOI] [PubMed] [Google Scholar]
- 9.Meade L.B., Bearne L.M., Sweeney L.H., Alageel S.H., Godfrey E.L. Behaviour change techniques associated with adherence to prescribed exercise in patients with persistent musculoskeletal pain: systematic review. Br. J. Health Psychol. 2019;24:10–30. doi: 10.1111/bjhp.12324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Whittaker J.L., Truong L.K., Silvester-Lee T., Losciale J.M., Miciak M., Pajkic A., et al. Feasibility of the SOAR (Stop OsteoARthritis) program. Osteoarthritis and Cartilage Open. 2022;4 doi: 10.1016/j.ocarto.2022.100239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sandelowski M. What's in a name? Qualitative description revisited. Res. Nurs. Health. 2010;33:77–84. doi: 10.1002/nur.20362. [DOI] [PubMed] [Google Scholar]
- 12.O'Brien Bridget C., Harris Iiene B., Beckman Thomas J., Reed Darcy A., Cd A. Standards for reporting qualitative research. A Synthesis of Recommendations Academic Medicine. 2014;89:1245–1251. doi: 10.1097/ACM.0000000000000388. [DOI] [PubMed] [Google Scholar]
- 13.Kaushik V., Walsh C.A. Pragmatism as a research paradigm and its implications for social work research. Soc. Sci. 2019;8 doi: 10.3390/socsci8090255. [DOI] [Google Scholar]
- 14.Bowen D.J., Kreuter M., Spring B., Cofta-Woerpel L., Linnan L., Weiner D., et al. How we design feasibility studies. Am. J. Prev. Med. 2009;36:452–457. doi: 10.1016/j.amepre.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Holt C.J., McKay C.D., Truong L.K., Le C.Y., Gross D.P., Whittaker J.L. Sticking to it: a scoping review of adherence to exercise therapy interventions in children and adolescents with musculoskeletal conditions. J. Orthop. Sports Phys. Ther. 2020;50:503–515. doi: 10.2519/jospt.2020.9715. [DOI] [PubMed] [Google Scholar]
- 16.Whittaker J.L., Toomey C.M., Nettel-Aguirre A., Jaremko J.L., Doyle-Baker P.K., Woodhouse L.J., et al. Health-related outcomes after a youth sport–related knee injury. Med. Sci. Sports Exerc. 2019;51:255–263. doi: 10.1249/mss.0000000000001787. [DOI] [PubMed] [Google Scholar]
- 17.Atkins L., Francis J., Islam R., O'Connor D., Patey A., Ivers N., et al. A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implement. Sci. 2017;12:77. doi: 10.1186/s13012-017-0605-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Whittaker J.L., Truong L.K., Losciale J.M., Silvester-Lee T., Miciak M., Pajkic A., et al. Efficacy of the SOAR knee health program: protocol for a two-arm stepped-wedge randomized delayed-controlled trial. BMC Muscoskel. Disord. 2022;23 doi: 10.1186/s12891-022-05019-z. 85-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Whittaker J.L., Toomey C.M., Woodhouse L.J., Jaremko J.L., Nettel-Aguirre A., Emery C.A. Association between MRI-defined osteoarthritis, pain, function and strength 3-10 years following knee joint injury in youth sport. Br. J. Sports Med. 2017 doi: 10.1136/bjsports-2017-097576. [DOI] [PubMed] [Google Scholar]
- 20.Coyne I.T. Sampling in qualitative research. Purposeful and theoretical sampling; merging or clear boundaries? J. Adv. Nurs. 1997;26:623–630. doi: 10.1046/j.1365-2648.1997.t01-25-00999.x. [DOI] [PubMed] [Google Scholar]
- 21.Ardern C.L., Taylor N.F., Feller J.A., Webster K.E. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br. J. Sports Med. 2014;48:1543–1552. doi: 10.1136/bjsports-2013-093398. [DOI] [PubMed] [Google Scholar]
- 22.Hsieh H.-F., Shannon S.E. Three approaches to qualitative content analysis. Qual. Health Res. 2005;15:1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 23.Parsons J.L., Coen S.E., Bekker S. Anterior cruciate ligament injury: towards a gendered environmental approach. Br. J. Sports Med. 2021:984–990. doi: 10.1136/bjsports-2020-103173. [DOI] [PubMed] [Google Scholar]
- 24.Yang J., Peek-Asa C., Lowe J.B., Heiden E., Foster D.T. Social support patterns of collegiate athletes before and after injury. J. Athl. Train. 2010;45:372–379. doi: 10.4085/1062-6050-45.4.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bianco T. Social support and recovery from sport injury: elite skiers share their experiences. Res. Q. Exerc. Sport. 2001;72:376–388. doi: 10.1080/02701367.2001.10608974. [DOI] [PubMed] [Google Scholar]
- 26.Finlay L. Outing” the researcher: the provenance, process, and practice of reflexivity. Qual. Health Res. 2002;12:531–545. doi: 10.1177/104973202129120052. [DOI] [PubMed] [Google Scholar]
- 27.Birks M., Chapman Y., Francis K. Memoing in qualitative research: probing data and processes. J. Res. Nurs. 2008;13:68–75. doi: 10.1177/1744987107081254. [DOI] [Google Scholar]
- 28.Mayan M. first ed. Edition. Routledge; New York: 2009. Essentials of Qualitative Inquiry. [DOI] [Google Scholar]
- 29.Smith B., McGannon K. Developing rigor in qualitative research: problems and opportunities within sport and exercise psychology. Int. Rev. Sport Exerc. Psychol. 2017;11:101–121. doi: 10.1080/1750984X.2017.1317357. [DOI] [Google Scholar]
- 30.Fjellman-Wiklund A., Söderman K., Lundqvist M., Häger C.K. Retrospective experiences of individuals two decades after anterior cruciate ligament injury – a process of re-orientation towards acceptance. Disabil. Rehabil. 2021:1–10. doi: 10.1080/09638288.2021.1962415. [DOI] [PubMed] [Google Scholar]
- 31.Darlow B., Brown M., Thompson B., Hudson B., Grainger R., McKinlay E., et al. Living with osteoarthritis is a balancing act: an exploration of patients' beliefs about knee pain. BMC Rheumatology. 2018;2:15. doi: 10.1186/s41927-018-0023-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Willett M., Duda J., Fenton S., Gautrey C., Greig C., Rushton A. Effectiveness of behaviour change techniques in physiotherapy interventions to promote physical activity adherence in lower limb osteoarthritis patients: a systematic review. PLoS One. 2019;14 doi: 10.1371/journal.pone.0219482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gutnick D., Reims K., Davis C., Gainforth H., Jay M., Cole S. Brief action planning to facilitate behavior change and support patient self-management. J. Clin. Outcome Manag. 2014;21:17–29. [Google Scholar]
- 34.Daluiso-King G., Hebron C. Is the biopsychosocial model in musculoskeletal physiotherapy adequate? An evolutionary concept analysis. Physiother. Theory Pract. 2020:1–17. doi: 10.1080/09593985.2020.1765440. [DOI] [PubMed] [Google Scholar]
- 35.Laranjo L., Ding D., Heleno B., Kocaballi B., Quiroz J.C., Tong H.L., et al. Do smartphone applications and activity trackers increase physical activity in adults? Systematic review, meta-analysis and metaregression. Br. J. Sports Med. 2021;55:422. doi: 10.1136/bjsports-2020-102892. http://bjsm.bmj.com/content/55/8/422.abstract [DOI] [PubMed] [Google Scholar]
- 36.Ma J.K., Martin Ginis K.A. A meta-analysis of physical activity interventions in people with physical disabilities: content, characteristics, and effects on behaviour. Psychol. Sport Exerc. 2018;37:262–273. doi: 10.1016/j.psychsport.2018.01.006. [DOI] [Google Scholar]
- 37.Dias J.F., Oliveira V.C., Borges P.R.T., Dutra F.C.M.S., Mancini M.C., Kirkwood R.N., et al. Effectiveness of exercises by telerehabilitation on pain, physical function and quality of life in people with physical disabilities: a systematic review of randomised controlled trials with GRADE recommendations. Br. J. Sports Med. 2021;55:155. doi: 10.1136/bjsports-2019-101375. http://bjsm.bmj.com/content/55/3/155.abstract [DOI] [PubMed] [Google Scholar]
- 38.Statistics Canada. Use of Internet services and technologies by age group and household income quartile. Published 2019-10-29. Accessed: October 19, 2022, https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=2210011301.
- 39.Alkire L., O'Connor G.E., Myrden S., Köcher S. Patient experience in the digital age: an investigation into the effect of generational cohorts. J. Retailing Consum. Serv. 2020;57 doi: 10.1016/j.jretconser.2020.102221. [DOI] [Google Scholar]
- 40.Sheridan D., Coffee P., Lavallee D. A systematic review of social support in youth sport. Int. Rev. Sport Exerc. Psychol. 2014;7:198–228. doi: 10.1080/1750984X.2014.931999. [DOI] [Google Scholar]
- 41.Kinney M., Seider J., Beaty A.F., Coughlin K., Dyal M., Clewley D. The impact of therapeutic alliance in physical therapy for chronic musculoskeletal pain: a systematic review of the literature. Physiother. Theory Pract. 2018:1–13. doi: 10.1080/09593985.2018.1516015. [DOI] [PubMed] [Google Scholar]
- 42.Hall A.M., Ferreira P.H., Maher C.G., Latimer J., Ferreira M.L. The influence of the therapist-patient relationship on treatment outcome in physical rehabilitation: a systematic review. Phys. Ther. 2010;90:1099–1110. doi: 10.2522/ptj.20090245. [DOI] [PubMed] [Google Scholar]