Abstract
Background
Tumor proliferation is frequently accompanied by aberrant enzyme production. We aim to investigate the potential predictive value of both plasma alkaline phosphatase (ALP) and lactate dehydrogenase (LDH) in patients with HCC and to develop a nomogram to assess the prognosis of HCC.
Methods
The trial involved 2327 patients between May 2015 and March 2022. Within 7 days of enrollment, the levels of ALP and LDH were measured, and their association with survival was assessed. And we had developed and validated a new nomogram based on ALD and ALP.
Results
Using X-tile software, the optimal cut-off values were determined to be ALP = 172 U/L and LDH = 241 U/L. The high ALP (≥ 172), LDH (≥ 241), and ALP/LDH (≥ 0.91) groups had lower median overall survival (mOS) than low ALP (< 172), LDH (< 241), and ALP/LDH (< 0.91) groups (all p < 0.001). In addition, elevated ALP and LDH levels are independent negative prognostic indicators. Moreover, we established that the area under the curve (AUC) values of the predicted 1-, 2-, and 3-year survival rates of receiver operating characteristic curve (ROC) based on the nomogram were 0.79, 0.77, and 0.74, respectively. In addition, the calibration curves and decision curve analyses (DCA) demonstrated that this model possessed strong predictive capability.
Conclusion
ALP, LDH and ALP/LDH can be employed as biomarkers for predicting the prognosis of HCC. Furthermore, the nomograph based on ALH and ALP demonstrates good HCC prediction performance. For HCC patients with high ALH or ALP or ALP/LDH, close surveillance program and adjuvant therapy should be considered.
Keywords: lactate dehydrogenase, alkaline phosphatase, hepatocellular carcinoma, overall survival, nomogram
Introduction
Hepatocellular carcinoma (HCC) is a prevalent malignant tumor that is anticipated to impact over 1 million people annually by 2025.1,2 The majority of HCC patients are in an advanced state at the time of diagnosis. Advanced HCC currently faces the challenge of a median overall survival (mOS) of 5.5 months.3
Therapeutic options for advanced HCC are limited. Surgery still remains frequently curative therapy for HCC, however, the long-term prognosis after resection remains unsatisfactory, due to the high disease relapse rate. Recently approved systemic agents do offer more options for the treatment of advanced HCC patients. Still, the lack of head-to-head comparative studies between first- and second-line treatments leads to confusion when making clinical decisions.
Currently, the US Food and Drug Administration has approved atezolizumab plus bevacizumab as the treatment of choice for unresectable HCC.4 In addition, a large Phase II/III study revealed that sintilimab + bevacizumab biosimilar was superior to sorafenib monotherapy in patients with unresectable HCC.5 With a 5-year OS of 52.0 and a 5-year disease free survival (DFS) of 41.4, radiofrequency ablation (RFA) + transarterial chemoembolization (TACE) for the same aim shown good efficacy in early-stage HCC.6 Although the problem of HCC patients’ low life expectancy has been alleviated, the challenge of gauging the treatment’s effectiveness remains.
Alpha-fetoprotein (AFP), a tumor-associated protein found in serum, is frequently employed in the clinical diagnosis of HCC.7,8 However, AFP is negative in about 30 to 40 of HCC patients with a pathological diagnosis.9 In diagnosing HCC, AFP has a low sensitivity (54), as well as a low prognostic value.10 As a result, we must identify additional relevant biomarkers to improve HCC management.
Tumor proliferation is frequently accompanied by aberrant enzyme production.11 As a result, standard tests are performed on serum liver enzymes lactate dehydrogenase (LDH) and plasma alkaline phosphatase (ALP) before treatment. A hydrolase known as ALP has been found to be broadly distributed throughout the liver.12 Cell cycle control, tumor metastasis, and proliferation were revealed to be strongly related with ALP by Zhang and Zeng et al13–15 Furthermore, LDH, a metabolic enzyme involved in anaerobic glycolysis, is necessary for tumor maintenance.16 The primary metabolic mechanism for energy production in tumors is anaerobic glycolysis. As a result, LDH may possibly be related to tumor progression. A number of studies have demonstrated that ALP and LDH can predict the prognosis of HCC.17–19 A large number of clinical studies are still required to determine the relationship between ALP and LDH levels and the prognosis of HCC due to their small sample size.
This multicenter study was initiated to determine whether LDH and ALP can be used as prognostic markers and to develop a nomogram to assess the prognosis of HCC.
Materials and Methods
Patients
From May 2015 to March 2022, this study included 2327 patients from three Chinese tertiary hospitals. The criteria for inclusion included the following: a) patients were diagnosed with HCC pathologically or clinically; b) patients had not received any anti-tumor treatment; c) plasma ALP and LDH levels were measured within 7 days prior to enrollment; and d) complete clinical data were. We excluded patients with other malignant tumor types. This research was approved by the Hospital Affiliated with Southwest Medical University’s Ethics Committee (KY2020254). The Ethics Committee abandoned the informed consent form because it was a retrospective study. And the data were analyzed anonymously.
Data Collection
Patient baselines that were collected include the following: 1) liver function: albumin–bilirubin (ALBI) and Child–Pugh score; 2) laboratory indicators: alanine aminotransferase (ALT), ALP, leukocyte, LDH, AFP, and platelet count; 3) tumor burden: portal vein tumor thrombus (PVTT), extrahepatic metastasis, tumor number, tumor diameter, and lymph node metastasis; 4) tumor stage: Barcelona Clinic Liver Cancer (BCLC); 5) treatment date: all HCC treatments the patients received; and 7) other data: sex, age, hepatitis B virus (HBV), diabetes mellitus, hepatitis C virus (HCV), alcohol, and hypertension. OS was defined as the period between the start of treatment and the death or last follow-up.
Statistical Analysis
All data were analyzed using SPSS 26.0 (SPSS, Chicago, IL, United States) and R 3.3.2 software. Bilateral P < 0.05 was considered statistically significant. The categorical variables (χ2 test and McNemar analysis) and continuous variables (Mann–Whitney U and Wilcoxon paired signed-rank test) were further processed using SPSS. Optimal cut-off values for serum ALP and LDH were determined based on OS using X-tile software. Propensity score matching (PSM) was next used to identify high/low ALP groups and high/low LDH groups that had similar baseline traits. Following that, we estimated the mOS using Kaplan–Meier statistics and compared the results using the Log rank test. Multivariate Cox analysis was employed to identify independent factors that influence OS. Furthermore, risk factors affecting serum ALP and LDH were identified by logistic regression analysis.
We randomly divided all patients (7:3 ratio) into the training set (n = 1629) and the validation set (n = 698). Independent influencing factors established by multivariate cox analysis in the training set were used to generate a nomogram. The receiver operating characteristic curve (ROC), decision curve analyses (DCA), and calibration curves were utilized to evaluate the prognostic performance of the nomogram. Then, we calculated the risk scores of all patients and stratified them (high, moderate, and low risks) using x-tile software (Yale University, New Haven, CT).
Result
Patient Characteristics
The median ALP plasma concentration was 133.0 U/L and the median LDH concentration was 216.0 U/L. The male, ALBI-2, AFP < 200 ng/mL, Child A, BCLC-C, and multiple tumors represented 81.0, 61.6, 55.4, 62.5, 69.9, and 67.6, respectively. Table 1 outlines the baseline characteristics of all patients recruited.
Table 1.
Baseline Characteristics Before Propensity Score Matching
| Variable | Total | ALP < 172 ng/mL | ALP ≥ 172 ng/mL | p | LDH < 241 ng/mL | LDH ≥ 241 ng/mL | p |
|---|---|---|---|---|---|---|---|
| Patients | 2327 | 1509 | 818 | 1419 | 908 | ||
| Male sex | 1886 (81.0) | 1213 (80.4) | 673 (82.3) | 0.267 | 1150 (81.0) | 736 (81.1) | 0.993 |
| Age ≥ 60 years | 972 (41.8) | 648 (42.9) | 324 (39.6) | 0.12 | 615 (43.3) | 357 (39.3) | 0.055 |
| HBV | 1254 (53.9) | 849 (56.3) | 405 (49.5) | 0.002 | 754 (53.1) | 500 (55.1) | 0.362 |
| HCV | 39 (1.7) | 38 (2.5) | 1 (0.1) | <0.001 | 28 (2.0) | 11 (1.2) | 0.163 |
| Alcohol | 867 (37.3) | 549 (36.4) | 318 (38.9) | 0.235 | 533 (37.6) | 334 (36.8) | 0.705 |
| Diabetes mellitus | 242 (10.4) | 165 (10.9) | 77 (9.4) | 0.251 | 149 (10.5) | 93 (10.2) | 0.842 |
| Hypertension | 384 (16.5) | 260 (17.2) | 124 (15.2) | 0.199 | 232 (16.3) | 152 (16.7) | 0.804 |
| Child–Pugh class | <0.001 | <0.001 | |||||
| A | 1627 (69.9) | 1228 (81.4) | 399 (48.8) | 1100 (77.5) | 527 (58.0) | ||
| B | 635 (27.3) | 258 (17.1) | 377 (46.1) | 294 (20.7) | 341 (37.6) | ||
| C | 65 (2.8) | 23 (1.5) | 42 (5.1) | 25 (1.8) | 40 (4.4) | ||
| ALBI grade | <0.001 | <0.001 | |||||
| 1 | 670 (28.8) | 566 (37.5) | 104 (12.7) | 496 (35.0) | 174 (19.2) | ||
| 2 | 1433 (61.6) | 877 (58.1) | 556 (68.0) | 821 (57.9) | 612 (67.4) | ||
| 3 | 224 (9.6) | 66 (4.4) | 158 (19.3) | 102 (7.2) | 122 (13.4) | ||
| ALP, median, U/L | 133.0 (91.0–220.0) | 102.0 (80.1–130.0) | 287.0 (213.1–426.3) | <0.001 | 114.2 (84.0–175.0) | 172.0 (119.0–300.0) | <0.001 |
| LDH, median, U/L | 216.0 (175.0–295.0) | 199.0 (165.2–260.0) | 260.0 (203.0–371.0) | <0.001 | 184.0 (158.0–208.2) | 330.0 (277.0–453.0) | <0.001 |
| Serum AFP, ng/mL | <0.001 | <0.001 | |||||
| < 200 | 1289 (55.4) | 881 (58.4) | 408 (49.9) | 879 (61.9) | 410 (45.2) | ||
| ≥ 200, < 400 | 127 (5.5) | 80 (5.3) | 47 (5.7) | 80 (5.6) | 47 (5.2) | ||
| ≥ 400 | 911 (39.1) | 548 (36.3) | 363 (44.4) | 460 (32.4) | 451 (49.7) | ||
| Platelet count ≥ 100 × 109/L | 1661 (71.4) | 1028 (68.1) | 633 (77.4) | <0.001 | 984 (69.3) | 677 (74.6) | 0.007 |
| ALT levels ≥ 40 U/L | 1205 (51.8) | 616 (40.8) | 589 (72.0) | <0.001 | 611 (43.1) | 594 (65.4) | <0.001 |
| Leukocyte ≥ 4 × 109/L | 1924 (82.7) | 1210 (80.2) | 714 (87.3) | <0.001 | 1120 (78.9) | 804 (88.5) | <0.001 |
| BCLC stage | <0.001 | <0.001 | |||||
| 0/A | 462 (19.9) | 389 (25.8) | 73 (8.9) | 345 (24.3) | 117 (12.9) | ||
| B | 346 (14.9) | 277 (18.4) | 69 (8.4) | 250 (17.6) | 96 (10.6) | ||
| C | 1454 (62.5) | 820 (54.3) | 634 (77.5) | 799 (56.3) | 655 (72.1) | ||
| D | 65 (2.8) | 23 (1.5) | 42 (5.1) | 25 (1.8) | 40 (4.4) | ||
| Number of tumors ≥ 2 | 1573 (67.6) | 940 (62.3) | 633 (77.4) | <0.001 | 897 (63.2) | 676 (74.4) | <0.001 |
| Tumor diameter, cm | <0.001 | <0.001 | |||||
| < 3 | 408 (17.5) | 319 (21.1) | 89 (10.9) | 315 (22.2) | 93 (10.2) | ||
| ≥ 3, < 5 | 538 (23.1) | 400 (26.5) | 138 (16.9) | 389 (27.4) | 149 (16.4) | ||
| ≥ 5, < 10 | 850 (36.5) | 555 (36.8) | 295 (36.1) | 510 (35.9) | 340 (37.4) | ||
| ≥ 10 | 531 (22.8) | 235 (15.6) | 296 (36.2) | 205 (14.4) | 326 (35.9) | ||
| PVTT | 853 (36.7) | 410 (27.2) | 443 (54.2) | <0.001 | 409 (28.8) | 444 (48.9) | < 0.001 |
| Lymph node metastasis | 1022 (43.9) | 560 (37.1) | 462 (56.5) | <0.001 | 554 (39.0) | 468 (51.5) | < 0.001 |
| Extrahepatic metastases | 537 (23.1) | 264 (17.5) | 273 (33.4) | <0.001 | 281 (19.8) | 256 (28.2) | < 0.001 |
| Lung | 311 (13.4) | 137 (9.1) | 174 (21.3) | 146 (10.3) | 165 (18.2) | ||
| Bone | 149 (6.4) | 74 (4.9) | 75 (9.2) | 79 (5.6) | 70 (7.7) | ||
| Other | 198 (8.5) | 109 (7.2) | 89 (10.9) | 112 (7.9) | 86 (9.5) | ||
| Treatments | <0.001 | < 0.001 | |||||
| Supportive care | 575 (24.7) | 277 (18.4) | 298 (36.4) | 311 (21.9) | 264 (29.1) | ||
| Liver resection | 330 (14.2) | 272 (18.0) | 58 (7.1) | 227 (16.0) | 103 (11.3) | ||
| RFA | 90 (3.9) | 84 (5.6) | 6 (0.7) | 66 (4.7) | 24 (2.6) | ||
| TACE | 702 (30.2) | 448 (29.7) | 254 (31.1) | 406 (28.6) | 296 (32.6) | ||
| Targeted therapy + ICI | 84 (3.6) | 47 (3.1) | 37 (4.5) | 54 (3.8) | 30 (3.3) | ||
| Adjuvant TACE | 90 (3.9) | 85 (5.6) | 5 (0.6) | 73 (5.1) | 17 (1.9) | ||
| Other | 456 (19.6) | 296 (19.6) | 160 (19.6) | 282 (19.9) | 174 (19.2) |
Abbreviations: HBV, hepatitis B virus; HCV, hepatitis C virus; ALBI, albumin–bilirubin; ALP, alkaline phosphatase; LDH, lactate dehydrogenase; AFP, alpha-fetoprotein; ALT, alanine aminotransferase; BCLC, Barcelona Clinic Liver Cancer; PVTT, portal vein tumor thrombus; RFA, radiofrequency ablation; TACE, transcatheter arterial chemoembolization; ICI, immune checkpoint inhibitor.
ALP and LDH Levels and Overall Survival Before and After PSM
The optimal cut-off value for ALP was 172 U/L and for LDH was 241 U/L, as shown using X-Tile software. As a result, all 2327 patients were separated into two groups: low ALP (< 172 U/L, n = 1509) and high ALP (≥ 172 U/L, n = 818) or low LDH (<241 U/L, n = 1419) and high LDH (≥ 241 U/L, n = 908). Prior to PSM, the high ALP and high LDH groups showed inferior liver function and a larger tumor burden compared to the low ALP and low LDH groups (p < 0.05, Table 1). In our investigation, the median duration of follow-up for all patients, those in the high ALP group, those in the low ALP group, those in the high LDH group, and those in the low LDH group was 27.9, 25.9, 28.4, 27.1, and 28.2 months, respectively.
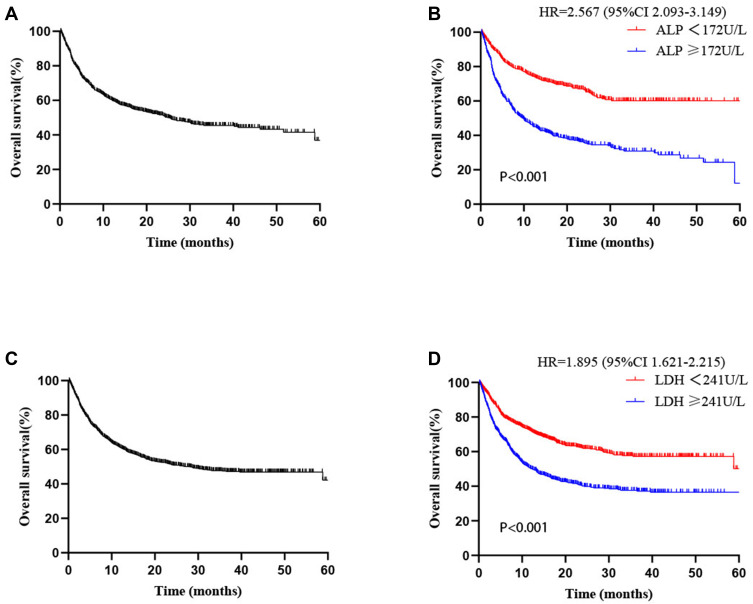
The mOS for each cohort was 25.2 months (95 CI 21.3–29.1, Figure 1A). The mOS in the high ALP group was significantly shorter than in the low ALP group, with a statistically significant difference [7.7 vs 55.4 months, HR=1.594 (95 CI 1.377–1.820), P<0.001, Figure 1B]. Furthermore, the high LDH group had a shorter mOS than the low LDH group [10.7 vs 38.6 months, HR=1.367 (95 CI 1.205–1.554), P < 0.001, Figure 1C].
Figure 1.
Survival graph for every patient (A). Survival curve stratified by alkaline phosphatase concentration (B) and lactate dehydrogenase concentration (C).
Following PSM, there was no statistically significant difference between the various group covariates with ALP and LDH as the corresponding groups (Supplementary Tables 1 and 2). The mOS for HCC patients in the ALP cohort was 25.1 months (Figure 2A). In comparison to the low-ALP group, the mOS in the high-ALP group remained substantially shorter [9.8 vs 75.7 months, HR=2.567, 95 CI (2.093–3.149), P<0.001, Figure 2B]. All HCC patients in the LDH cohort had mOS of 28.1 months (Figure 2C). Furthermore, the mOS for high LDH was 12.3 months and 64.6 months for low LDH, with statistically significant differences [HR=1.895, (95 CI 1.621–2.215), P<0.001, Figure 2D].
Figure 2.
Survival curve for patients after PSM with ALP (A) and LDH (C). Survival curve stratified based on ALP (B) and LDH (D) levels.
Abbreviations: ALP, alkaline phosphatase; LDH, lactate dehydrogenase.
Determination of Prognostic Factors for OS
In the univariate and multivariate analyses, alcohol (p = 0.048), child B/C (p = 0.001), ALP ≥172 U/L (p < 0.001), LDH ≥241 U/L (p < 0.001), more advanced BCLC stage (p < 0.001), number of tumors ≥2 (p = 0.005), tumor diameter ≥ 5 cm (p = 0.002), distant metastasis (p <0.001), and no anti-tumor treatment (p < 0.001) were independent influencing factors of OS (Table 2). After PSM, ALP ≥ 172U/L and LDH ≥ 241U/L remained independent factors affecting OS (Supplementary Tables 3 and 4).4
Table 2.
Univariate and Multivariate Cox Regression Analyses of Overall Survival Before Propensity Score Matching
| Variable | Univariable Cox Regression | Multivariable Cox Regression | ||||
|---|---|---|---|---|---|---|
| HR | 95CI | p | HR | 95CI | p | |
| Sex (male/female) | 1.085 | 0.934–1.259 | 0.286 | |||
| Age (≥ 60/< 60 years) | 0.975 | 0.867–1.096 | 0.668 | |||
| HBV (positive/negative) | 0.976 | 0.869–1.095 | 0.678 | |||
| HCV (positive/negative) | 0.551 | 0.319–0.952 | 0.033 | 1.049 | 0.521–1.577 | 0.729 |
| Alcoholism (positive/negative) | 1.129 | 1.003–1.270 | 0.044 | 1.124 | 1.001–1.27 | 0.048 |
| Diabetes mellitus (positive/negative) | 0.999 | 0.824–1.211 | 0.988 | |||
| Hypertension (positive/negative) | 0.823 | 0.698–0.971 | 0.021 | 0.858 | 0.724–1.009 | 0.065 |
| Child–Pugh class (B + C/A) | 2.067 | 1.835–2.327 | < 0.001 | 1.271 | 1.101–1.463 | 0.001 |
| ALBI grade (2+3/1) | 1.573 | 1.374–1.802 | < 0.001 | 0.969 | 0.833–1.132 | 0.708 |
| ALP (≥ 172/< 172 U/L) | 2.673 | 2.380–3.002 | < 0.001 | 1.594 | 1.377–1.820 | < 0.001 |
| LDH (≥ 241/241 U/L) | 1.918 | 1.709–2.153 | < 0.001 | 1.367 | 1.205–1.554 | < 0.001 |
| AFP (≥ 400/< 400 ng/mL) | 1.199 | 1.067–1.347 | 0.002 | 0.925 | 0.819–1.048 | 0.224 |
| Platelet (< 100,000/≥ 100,000/μL) | 1.010 | 0.890–1.147 | 0.873 | |||
| ALT (≥ 40/< 40 U/L) | 1.361 | 1.211–1.529 | < 0.001 | 0.968 | 0.856–1.102 | 0.649 |
| Leukocyte (< 4000/≥ 4000/μL) | 0.885 | 0.759–1.032 | 0.118 | |||
| BCLC stage | <0.001 | <0.001 | ||||
| 0/A | 1.000 | 1.000 | ||||
| B | 1.351 | 1.053–1.732 | 0.018 | 0.982 | 0.740–1.302 | 0.897 |
| C | 2.940 | 2.436–3.547 | < 0.001 | 1.575 | 1.216–2.045 | 0.001 |
| D | 5.643 | 4.062–7.838 | < 0.001 | 1.836 | 1.257–2.675 | 0.002 |
| Number of tumor (≥ 2/< 2) | 1.825 | 1.594–2.090 | < 0.001 | 1.255 | 1.069–1.472 | 0.005 |
| Tumor diameter (≥ 5/< 5 cm) | 1.849 | 1.633–2.094 | < 0.001 | 1.243 | 1.086–1.425 | 0.002 |
| PVTT (positive/negative) | 2.079 | 1.852–2.335 | < 0.001 | 1.140 | 0.990–1.324 | 0.069 |
| Lymph node metastasis (yes/no) | 1.696 | 1.511–1.904 | < 0.001 | 0.912 | 0.787–1.053 | 0.206 |
| Extrahepatic metastases (yes/no) | 1.958 | 1.728–2.219 | < 0.001 | 1.224 | 1.063–1.401 | 0.005 |
| Antitumor therapy | <0.001 | <0.001 | ||||
| Supportive care | 1.000 | 1.000 | ||||
| Liver resection | 0.288 | 0.231–0.359 | <0.001 | 0.463 | 0.368–0.587 | <0.001 |
| RFA | 0.126 | 0.072–0.218 | <0.001 | 0.225 | 0.129–0.397 | <0.001 |
| TACE | 0.580 | 0.502–0.670 | <0.001 | 0.611 | 0.528–0.716 | <0.001 |
| Targeted therapy+ ICI | 0.819 | 0.610–1.101 | 0.186 | 0.794 | 0.593–1.078 | 0.142 |
| Adjuvant TACE | 0.257 | 0.171–0.385 | <0.001 | 0.437 | 0.292–0.666 | <0.001 |
| Other | 0.548 | 0.464–0.647 | <0.001 | 0.610 | 0.518–0.728 | <0.001 |
Abbreviations: HBV, hepatitis B virus; HCV, hepatitis C virus; ALBI, albumin–bilirubin; ALP, alkaline phosphatase; LDH, lactate dehydrogenase; AFP, alpha-fetoprotein; ALT, alanine aminotransferase; BCLC, Barcelona Clinic Liver Cancer; PVTT, portal vein tumor thrombus; RFA, radiofrequency ablation; TACE, transcatheter arterial chemoembolization; ICI, immune checkpoint inhibitor.
Correlation Between Baseline Characteristics and Preoperative ALP or LDH
Using logistic regression, HBV, HCV, ALBI, ALT, hypertension, Child–Pugh class, LDH, tumor number, platelet, tumor diameter, PVTT, and extrahepatic metastasis were identified as independent factors of ALP expression (Supplementary Table 5). Using logistic regression, tumor diameter, Child–Pugh class, tumor number, AFP, sex, age, HCV, alcoholic, leukocyte, hypertension, ALBI, ALP, ALT, and PVTT were identified as independent factors of LDH expression (Supplementary Table 6).
Subgroup Analysis
Patients were divided into seven subgroups based on treatment modality: supportive care (n = 575), surgery (n = 330), RFA (n = 90), TACE (n = 702), targeted therapy plus immune checkpoint inhibitor (ICI, n = 84), adjuvant TACE (n = 90), and other treatment modalities (n = 456).
In the supportive care, surgery, TACE, adjuvant TACE, and other treatment modality groups, low ALP levels demonstrated significantly improved OS compared to high ALP levels (p < 0.001, p < 0.001, p < 0.001, p = 0.016, p < 0.001, respectively). Notably, low ALP levels did not improve significantly in the RFA and targeted therapy plus ICI groups (Supplementary Figure 1). Low LDH levels were associated with significant OS improvement in the following subgroups: supportive care group, TACE group, targeted therapy plus ICI group, and other treatment groups (p < 0.001, p < 0.001, p = 0.005, p < 0.001, respectively), whereas in the surgery, RFA, and adjuvant TACE groups, low LDH levels were not associated with an improvement in OS (Supplementary Figure 2).
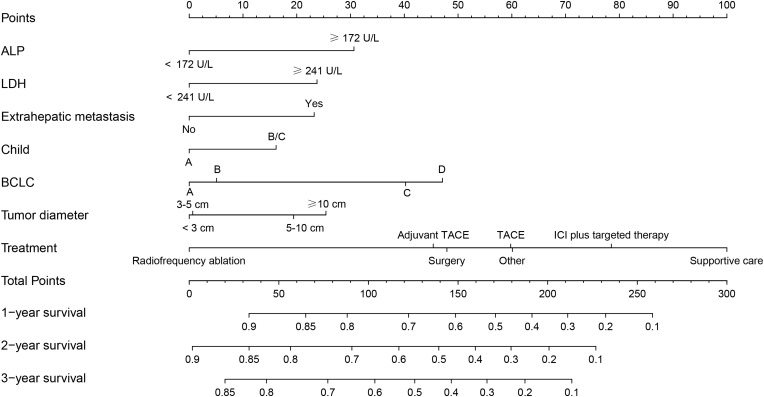
Nomogram Construction and Validation
The baseline characteristics of the training set and validation set are shown in Supplementary Table 7. In the training set, we found that ALP, LDH, extrahepatic metastasis, child grade, BCLC stage, tumor diameter, and treatment methods were independent prognostic factors affecting OS (Table 3). We constructed the nomogram based on these significant factors (Figure 3). In the validation set, we determined that the area under the curve (AUC) values of predicted 1-, 2-, and 3-year survival rates of ROC based on the nomogram were 0.798, 0.776, and 0.748, respectively, which were superior to other significant factors (Supplementary Figure 3). In addition, in the calibration curves (Supplementary Figure 4A) and DCA (Supplementary Figure 4B), this model also shows good prediction potential.
Table 3.
Univariate and Multivariate Cox Regression Analyses of Overall Survival in the Training Set
| Variable | Univariable Cox Regression | Multivariable Cox Regression | ||||
|---|---|---|---|---|---|---|
| HR | 95CI | p | HR | 95CI | p | |
| Sex (male/female) | 1.059 | 0.89–1.261 | 0.516 | |||
| Age (≥60/<60 years) | 0.982 | 0.854–1.128 | 0.793 | |||
| HBV (positive/negative) | 1.003 | 0.874–1.151 | 0.961 | |||
| HCV (positive/negative) | 0.555 | 0.288–1.07 | 0.079 | |||
| Alcoholism (positive/negative) | 1.147 | 0.998–1.318 | 0.054 | |||
| Diabetes mellitus (positive/negative) | 0.969 | 0.775–1.212 | 0.785 | |||
| Hypertension (positive/negative) | 0.879 | 0.724–1.066 | 0.190 | |||
| Child–Pugh class (B + C/A) | 2.045 | 1.775–2.355 | <0.001 | 1.264 | 1.066–1.498 | 0.007 |
| ALBI grade (2 + 3/1) | 1.499 | 1.275–1.761 | <0.001 | 0.976 | 0.815–1.169 | 0.792 |
| ALP (≥ 172/< 172 U/L) | 2.551 | 2.223–2.929 | <0.001 | 1.506 | 1.276–1.777 | <0.001 |
| LDH (≥ 241/ 241 U/L) | 1.917 | 1.671–2.2 | <0.001 | 1.379 | 1.187–1.603 | <0.001 |
| AFP (≥ 400/< 400 ng/mL) | 1.160 | 1.01–1.334 | 0.036 | 0.914 | 0.79–1.058 | 0.227 |
| Platelet (< 100,000/≥ 100,000/μL) | 1.054 | 0.906–1.227 | 0.495 | |||
| ALT (≥ 40/< 40 U/L) | 1.320 | 1.15–1.516 | <0.001 | 0.999 | 0.86–1.16 | 0.987 |
| Leukocyte (< 4000/≥ 4000/μL) | 1.270 | 1.054–1.529 | 0.012 | 1.059 | 0.873–1.283 | 0.563 |
| BCLC stage | <0.001 | 0.001 | ||||
| 0/A | 1.000 | – | 1.000 | |||
| B | 1.212 | 0.901–1.632 | 0.204 | 0.963 | 0.686–1.353 | 0.830 |
| C | 2.839 | 2.288–3.521 | <0.001 | 1.608 | 1.189–2.175 | 0.002 |
| D | 4.893 | 3.245–7.378 | <0.001 | 1.748 | 1.093–2.796 | 0.020 |
| Number of tumor (≥ 2/< 2) | 1.730 | 1.476–2.028 | <0.001 | 1.146 | 0.946–1.387 | 0.163 |
| Tumor diameter (≥ 5/< 5 cm) | 1.916 | 1.653–2.221 | <0.001 | 1.323 | 1.125–1.555 | 0.001 |
| PVTT (positive/negative) | 2.032 | 1.77–2.332 | <0.001 | 1.105 | 0.93–1.312 | 0.256 |
| Lymph node metastasis (yes/no) | 1.693 | 1.476–1.942 | <0.001 | 0.943 | 0.793–1.122 | 0.508 |
| Extrahepatic metastases (yes/no) | 2.203 | 1.902–2.551 | <0.001 | 1.379 | 1.171–1.623 | <0.001 |
| Antitumor therapy | <0.001 | <0.001 | ||||
| Supportive care | 1.000 | |||||
| Liver resection | 0.325 | 0.252–0.418 | <0.001 | 0.500 | 0.383–0.652 | <0.001 |
| RFA | 0.143 | 0.08–0.255 | <0.001 | 0.260 | 0.144–0.469 | <0.001 |
| TACE | 0.591 | 0.497–0.702 | <0.001 | 0.598 | 0.498–0.717 | <0.001 |
| Targeted therapy+ ICI | 0.806 | 0.568–1.143 | 0.226 | 0.748 | 0.525–1.065 | 0.107 |
| Adjuvant TACE | 0.274 | 0.168–0.448 | <0.001 | 0.486 | 0.294–0.803 | 0.005 |
| Other | 0.568 | 0.466–0.692 | <0.001 | 0.598 | 0.488–0.733 | <0.001 |
Abbreviations: HBV, hepatitis B virus; HCV, hepatitis C virus; ALBI, albumin–bilirubin; ALP, alkaline phosphatase; LDH, lactate dehydrogenase; AFP, alpha-fetoprotein; ALT, alanine aminotransferase; BCLC, Barcelona Clinic Liver Cancer; PVTT, portal vein tumor thrombus.
Figure 3.
Nomograph is constructed based on independent risk factors determined by multifactor Cox analysis.
Abbreviations: ALP, alkaline phosphatase; LDH, lactate dehydrogenase; BCLC, Barcelona Clinic Liver Cancer.
Risk Stratification
We calculated the risk scores of all patients based on the nomogram, and then, x-tile software was used to find the best cut-off point for risk stratification (low risk, < 140.8; moderate risk, 140.8–207.4; high risk, > 207.4). In all patients (4.7 vs 15.3 vs 59.4 months, p < 0.001, Supplementary Figure 5A), training sets (6.5 vs 15.1 vs 59.4 months, p < 0.001, Supplementary Figure 5B), and validation sets (4.2 vs 15.6 vs 64.6 months, p < 0.001, Supplementary Figure 5C), the high-risk group had lower mOS than the other groups.
Relationship Between ALP/LDH and Baseline Characteristics or Prognosis
An optimal cut-off value of 0.91 for ALP/LDH based on OS was determined using X-tile software. Patients were grouped into high ALP/LDH (ALP/LDH ≥ 0.91) and low ALP/LDH (ALP/LDH < 0.91) groups. The high ALP/LDH group showed inferior liver function and a larger tumor burden compared to the low ALP/LDH group (p < 0.05, Supplementary Table 8). In addition, the low ALP/LDH group had longer mOS (34.5 vs 10.1 months, p < 0.001, Supplementary Figure 6) than the high ALP/LDH group. Through logistic regression analyses, we confirmed that the HBV, HCV, Child-Pugh class, ALBI grade, platelet, ALT, and PVTT were independent influencing factors for ALP/LDH (Supplementary Table 9).
Discussion
Prognostic markers for HCC, gastric cancer, esophageal cancer, pancreatic cancer, and other cancers include ALP and LDH.18,20–22 Although prior studies suggested that ALP and LDH might be used to predict HCC prognosis, the research samples were generally small, and most patients were only involved in a single treatment.17,23 As a result, we initiated a multicenter study with bigger samples to confirm and further develop a nomogram to assess the prognostic value of ALP and LDH on HCC prognosis. In this study, we found that whether it is ALP ≥ 172U/L or LDH ≥ 241U/L or ALP/LDH ≥ 0.91, it has a shorter mOS (P <0.001) than ALP<172U/L or LDH <241U/L or ALP/LDH < 0.91. Furthermore, Cox analysis revealed that both ALP and LDH are independent influencing factors of OS.
Although AFP is the most extensively used biomarker in clinical practice, around one-third of HCC cases cannot be detected by AFP, and prior studies have also revealed limitations of AFP.9,24 Because the prediction constraint could lead to incorrect clinical decisions, more biomarkers were required to compensate. ALP is a hydrolase present in tissues throughout the body, particularly in the nucleolus of cancer cells.25 Furthermore, ALP is linked to the epithelial–mesenchymal transformation (EMT) cell phenotype, which is thought to be the initial stage in HCC microvascular invasion.26,27 In addition, LDH is a glycolytic enzyme that catalyzes the conversion of pyruvate to lactic acid under anaerobic conditions.28 It causes HIP-1 to become aberrant and is controlled by the P13k/Akt/mTOR pathway, which might result in tumor growth and progression.29,30 According to one study, knocking down the LDH-A gene, which codes for LDH-5, may inhibit tumor development and invasion.16 In conclusion, ALP and LDH are associated with the progression and infiltration of HCC. Wu et al reported that HCC patients with low ALP and low LDH had better OS than those with high ALP and high LDH,23 and our conclusions also support this view. However, the investigators did not control for baseline differences with PSM, nor did they investigate the link between ALP and LDH levels and baseline features, and they only included patients who received surgery as a therapy modality. In this investigation, we addressed the shortcomings of prior studies and developed a nomogram that included ALP and LDH to assess the prognosis of HCC.
In recent years, many studies have further expanded the treatment options for HCC. A promising combined treatment approach that significantly increases the survival of HCC patients is ICI plus targeted drugs, such as lenvatinib + pembrolizumab, sintilimab + bevacizumab, and atezolizumab + bevacizumab.4,5,31 Furthermore, our previous research discovered that programmed death 1 (PD-1) inhibitors combined with anti-angiogenic therapy and intensity-modulated radiotherapy can extend the OS of advanced HCC patients to 20.1 months.32 Moreover, selective internal radiotherapy (SIRT) extended the OS of advanced HCC patients to 8.8 months.33 Zhang et al found that the mOS of inoperable HCC patients receiving TACE-lenvatinib was 30.5 months.34 In addition, Su et al confirmed that gamma knife radiosurgery has a superior OS compared to TACE in the treatment of PVTT-HCC.35 Predicting the prognosis of HCC patients remains a formidable obstacle, despite the widespread use of numerous treatment methods in clinical practice. In our subgroup analysis based on various treatment modes, the ALP and LDH groups with low expression and the ALP and LDH groups with high expression exhibited superior OS. This confirms ALP and LDH’s good prediction performance. In addition, unlike organization biopsy, this is a liquid biopsy technology that can evaluate the patient’s condition rather than a single lesion or time, which is both convenient and inexpensive. This also demonstrates the benefits of using these two indicators in clinical settings.
We used logistic analysis to investigate the relationship between baseline characteristics and ALP, LDH, and ALP/LDH. It is worth noting that ALP, LDH, and ALP/LDH are related to Child grade, AIBI, tumor diameter, and multiple tumors. These indicators have been confirmed to be related to the prognosis of HCC.36–38 This also suggests that ALP and LDH are important prognostic factors for HCC. The large sample characteristics of this study also increase the reliability of our results to some extent. In addition, we wanted to see how ALP and LDH, two commonly used and easily accessible indicators in clinical practice, affected the prognosis of HCC patients. We discussed the differences in OS between groups and discovered the importance of low ALP and LDH in predicting prognosis. Following that, we confirmed that these critical values can be used as prognostic indicators for specific treatment groups. These findings suggest that when assessing the efficacy of HCC patients, they can use ALP or LDH depending on the treatment method. Furthermore, we expanded the nomogram further to include LDH and ALP and confirmed that the model has good prediction performance in the validation set. This adds to the practical clinical application of ALP and LDH in HCC. For HCC patients with high ALH or ALP or ALP/LDH, close surveillance program and adjuvant therapy should be considered.
Our study has some limitations. To begin with, because our research is retrospective, selection bias is unavoidable. Second, while the research findings suggest that LDH can predict the survival of targeted therapy plus ICI, the findings could be influenced by different ICI and targeted drugs. We hope that more prospective clinical research with specific ICI and targeted drugs will be conducted in the future to confirm our conclusions and hypotheses.
Conclusion
Finally, our findings show that ALP, LDH, and ALP/LDH can be employed as predictive biomarkers in the prognosis of HCC. Furthermore, the nomograph based on ALH and ALP performs well in predicting HCC.
Acknowledgment
The authors would like to thank all the reviewers who participated in the review and MJEditor (www.mjeditor.com) for its linguistic assistance during the preparation of this manuscript.
Funding Statement
This work was supported by Project of Science and Technology Department of Sichuan Province (2020JDTD0036).
Abbreviations
HCC, hepatocellular carcinoma; mOS, median overall survival; DFS, disease free survival; RFA, radiofrequency ablation; TACE, transarterial chemoembolization; AFP, alpha-fetoprotein; LDH, dehydrogenase; ALP, alkaline phosphatase; ALBI, albumin–bilirubin; ALT, alanine aminotransferase; PVTT, portal vein tumor thrombus; BCLC, Barcelona Clinic Liver Cancer; HBV, hepatitis B virus; HCV, hepatitis C virus; PSM, propensity score matching; ROC, operating characteristic curve; DCA, decision curve analyses; ICI, immune checkpoint inhibitor; AUC, the area under the curve; EMT, epithelial–mesenchymal transformation; PD-1, programmed death 1; SIRT, selective internal radiotherapy.
Data Sharing Statement
All data generated or analyzed during this study are included in this article and its Supplementary Material Files. Further enquiries can be directed to the corresponding author (hanyunwei@swmu.edu.cn).
Statement of Ethics
This retrospective study was approved by the Ethics Committee of The Affiliated Hospital of Southwest Medical University (approval number KY2020254) and complied with the standards of the Declaration of Helsinki. The Ethics Committee abandoned the informed consent form because it was a retrospective study. And the data were analyzed anonymously.
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi: 10.3322/caac.21660 [DOI] [PubMed] [Google Scholar]
- 2.Hepatocellular carcinoma. % J nature reviews. Dis Primers. 2021;7(1):7. doi: 10.1038/s41572-021-00245-6 [DOI] [PubMed] [Google Scholar]
- 3.Yeo W, Mo FK, Koh J, et al. Quality of life is predictive of survival in patients with unresectable hepatocellular carcinoma. Ann Oncol. 2006;17(7):1083–1089. doi: 10.1093/annonc/mdl065 [DOI] [PubMed] [Google Scholar]
- 4.Finn RS, Qin S, Ikeda M, et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N Engl J Med. 2020;382(20):1894–1905. doi: 10.1056/NEJMoa1915745 [DOI] [PubMed] [Google Scholar]
- 5.Ren Z, Xu J, Bai Y, et al. Sintilimab plus a bevacizumab biosimilar (IBI305) versus sorafenib in unresectable hepatocellular carcinoma (ORIENT-32): a randomised, open-label, Phase 2-3 study. Lancet Oncol. 2021;22(7):977–990. doi: 10.1016/S1470-2045(21)00252-7 [DOI] [PubMed] [Google Scholar]
- 6.Zhang YJ, Chen MS, Chen Y, Lau WY, Peng Z. Long-term outcomes of transcatheter arterial chemoembolization combined with radiofrequency ablation as an initial treatment for early-stage hepatocellular carcinoma. JAMA Netw Open. 2021;4(9):e2126992. doi: 10.1001/jamanetworkopen.2021.26992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Terentiev AA, Moldogazieva NT. Alpha-fetoprotein: a renaissance. Tumour Biol. 2013;34(4):2075–2091. doi: 10.1007/s13277-013-0904-y [DOI] [PubMed] [Google Scholar]
- 8.Tsuchiya N, Sawada Y, Endo I, Saito K, Uemura Y, Nakatsura T. Biomarkers for the early diagnosis of hepatocellular carcinoma. World J Gastroenterol. 2015;21(37):10573–10583. doi: 10.3748/wjg.v21.i37.10573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Agopian VG, Harlander-Locke MP, Markovic D, et al. Evaluation of patients with hepatocellular carcinomas that do not produce α-fetoprotein. JAMA Surg. 2017;152(1):55–64. doi: 10.1001/jamasurg.2016.3310 [DOI] [PubMed] [Google Scholar]
- 10.Farinati F, Marino D, De Giorgio M, et al. Diagnostic and prognostic role of alpha-fetoprotein in hepatocellular carcinoma: both or neither? Am J Gastroenterol. 2006;101(3):524–532. doi: 10.1111/j.1572-0241.2006.00443.x [DOI] [PubMed] [Google Scholar]
- 11.Ferreira LM, Hebrant A, Dumont JE. Metabolic reprogramming of the tumor. Oncogene. 2012;31(36):3999–4011. doi: 10.1038/onc.2011.576 [DOI] [PubMed] [Google Scholar]
- 12.Weiss MJ, Ray K, Henthorn PS, Lamb B, Kadesch T, Harris H. Structure of the human liver/bone/kidney alkaline phosphatase gene. J Biol Chem. 1988;263(24):12002–12010. doi: 10.1016/S0021-9258(18)37885-2 [DOI] [PubMed] [Google Scholar]
- 13.Zhang K, Xie SS, Li WC, Ye ZX, Shen ZW, Shen W. Prediction of microvascular invasion in HCC by a scoring model combining Gd-EOB-DTPA MRI and biochemical indicators. Eur Radiol. 2022;32(6):4186–4197. doi: 10.1007/s00330-021-08502-8 [DOI] [PubMed] [Google Scholar]
- 14.Zeng J, Zeng J, Liu J, Zeng J. Development of pre and post-operative nomograms to predict individual survival for ideal liver resection candidates with hepatocellular carcinoma. Liver Int. 2021;41(12):2974–2985. doi: 10.1111/liv.15042 [DOI] [PubMed] [Google Scholar]
- 15.Hashem S, ElHefnawi M, Habashy S, et al. Machine learning prediction models for diagnosing hepatocellular carcinoma with HCV-related chronic liver disease. Comput Methods Programs Biomed. 2020;196:105551. doi: 10.1016/j.cmpb.2020.105551 [DOI] [PubMed] [Google Scholar]
- 16.Fantin VR, St-Pierre J, Leder P. Attenuation of LDH-A expression uncovers a link between glycolysis, mitochondrial physiology, and tumor maintenance. Cancer Cell. 2006;9(6):425–434. doi: 10.1016/j.ccr.2006.04.023 [DOI] [PubMed] [Google Scholar]
- 17.Kong W, Zuo X, Liang H, et al. Prognostic value of lactate dehydrogenase in patients with hepatocellular carcinoma: a meta-analysis. Biomed Res Int. 2018;2018:1723184. doi: 10.1155/2018/1723184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jiang Y, Chen S, Wu Y, et al. Establishment and validation of a novel prognostic model for non-virus-related hepatocellular carcinoma. Cancer Cell Int. 2022;22(1):300. doi: 10.1186/s12935-022-02725-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lei Y, Han P, Chen Y, et al. Protein arginine methyltransferase 3 promotes glycolysis and hepatocellular carcinoma growth by enhancing arginine methylation of lactate dehydrogenase A. Clin Transl Med. 2022;12(1):e686. doi: 10.1002/ctm2.686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Namikawa T, Ishida N, Tsuda S, et al. Prognostic significance of serum alkaline phosphatase and lactate dehydrogenase levels in patients with unresectable advanced gastric cancer. Gastric Cancer. 2019;22(4):684–691. doi: 10.1007/s10120-018-0897-8 [DOI] [PubMed] [Google Scholar]
- 21.Wei XL, Zhang DS, He MM, et al. The predictive value of alkaline phosphatase and lactate dehydrogenase for overall survival in patients with esophageal squamous cell carcinoma. Tumour Biol. 2016;37(2):1879–1887. doi: 10.1007/s13277-015-3851-y [DOI] [PubMed] [Google Scholar]
- 22.Karimzadeh A, Heck M, Tauber R, et al. 177 Lu-PSMA-I&T for treatment of metastatic castration resistant prostate cancer: prognostic value of scintigraphic and clinical biomarkers. J Nucl Med. 2022:jnumed.122.264402. doi: 10.2967/jnumed.122.264402 [DOI] [PubMed] [Google Scholar]
- 23.Wu SJ, Lin YX, Ye H, Xiong XZ, Li FY, Cheng NS. Prognostic value of alkaline phosphatase, gamma-glutamyl transpeptidase and lactate dehydrogenase in hepatocellular carcinoma patients treated with liver resection. Int J Surg. 2016;36(Pt A):143–151. doi: 10.1016/j.ijsu.2016.10.033 [DOI] [PubMed] [Google Scholar]
- 24.Luo P, Wu S, Yu Y, et al. Current status and perspective biomarkers in AFP negative HCC: towards screening for and diagnosing hepatocellular carcinoma at an earlier stage. Pathol Oncol Res. 2020;26(2):599–603. doi: 10.1007/s12253-019-00585-5 [DOI] [PubMed] [Google Scholar]
- 25.Yamamoto K, Awogi T, Okuyama K, Takahashi N. Nuclear localization of alkaline phosphatase in cultured human cancer cells. Med Electron Microsc. 2003;36(1):47–51. doi: 10.1007/s007950300006 [DOI] [PubMed] [Google Scholar]
- 26.Nitta H, Allard MA, Sebagh M, et al. Prognostic value and prediction of extratumoral microvascular invasion for hepatocellular carcinoma. Ann Surg Oncol. 2019;26(8):2568–2576. doi: 10.1245/s10434-019-07365-0 [DOI] [PubMed] [Google Scholar]
- 27.Chung KY, Cheng IK, Ching AK, Chu JH, Lai PB, Wong N. Block of proliferation 1 (BOP1) plays an oncogenic role in hepatocellular carcinoma by promoting epithelial-to-mesenchymal transition. Hepatology. 2011;54(1):307–318. doi: 10.1002/hep.24372 [DOI] [PubMed] [Google Scholar]
- 28.Faloppi L, Scartozzi M, Bianconi M, et al. The role of LDH serum levels in predicting global outcome in HCC patients treated with sorafenib: implications for clinical management. BMC Cancer. 2014;14:110. doi: 10.1186/1471-2407-14-110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Koukourakis MI, Giatromanolaki A, Sivridis E, et al. Lactate dehydrogenase-5 (LDH-5) overexpression in non-small-cell lung cancer tissues is linked to tumour hypoxia, angiogenic factor production and poor prognosis. Br J Cancer. 2003;89(5):877–885. doi: 10.1038/sj.bjc.6601205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zha X, Wang F, Wang Y, et al. Lactate dehydrogenase B is critical for hyperactive mTOR-mediated tumorigenesis. Cancer Res. 2011;71(1):13–18. doi: 10.1158/0008-5472.CAN-10-1668 [DOI] [PubMed] [Google Scholar]
- 31.Finn RS, Ikeda M, Zhu AX, et al. Phase Ib study of lenvatinib plus pembrolizumab in patients with unresectable hepatocellular carcinoma. J Clin Oncol. 2020;38(26):2960–2970. doi: 10.1200/JCO.20.00808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Su K, Guo L, Ma W, et al. PD-1 inhibitors plus anti-angiogenic therapy with or without intensity-modulated radiotherapy for advanced hepatocellular carcinoma: a propensity score matching study. Front Immunol. 2022;13:972503. doi: 10.3389/fimmu.2022.972503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chow PKH, Gandhi M, Tan SB, et al. SIRveNIB: selective internal radiation therapy versus sorafenib in Asia-Pacific patients with hepatocellular carcinoma. J Clin Oncol. 2018;36(19):1913–1921. doi: 10.1200/JCO.2017.76.0892 [DOI] [PubMed] [Google Scholar]
- 34.Zhang JX, Chen YX, Zhou CG, et al. Transarterial chemoembolization combined with lenvatinib versus transarterial chemoembolization combined with sorafenib for unresectable hepatocellular carcinoma: a comparative retrospective study. Hepatol Res. 2022;52(9):794–803. doi: 10.1111/hepr.13801 [DOI] [PubMed] [Google Scholar]
- 35.Su K, Gu T, Xu K, et al. Gamma knife radiosurgery versus transcatheter arterial chemoembolization for hepatocellular carcinoma with portal vein tumor thrombus: a propensity score matching study. Hepatol Int. 2022;16(4):858–867. doi: 10.1007/s12072-022-10339-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fulgenzi CAM, Cheon J, D’Alessio A, et al. Reproducible safety and efficacy of atezolizumab plus bevacizumab for HCC in clinical practice: results of the AB-real study. Eur J Cancer. 2022;175:204–213. doi: 10.1016/j.ejca.2022.08.024 [DOI] [PubMed] [Google Scholar]
- 37.Hwang SH, Hong HS, Kim D, et al. Total lesion glycolysis on 18F-FDG PET/CT is a better prognostic factor than tumor dose on 90Y PET/CT in patients with hepatocellular carcinoma treated with 90Y transarterial radioembolization. Clin Nucl Med. 2022;47(6):e437–e443. doi: 10.1097/RLU.0000000000004128 [DOI] [PubMed] [Google Scholar]
- 38.Su K, Liu Y, Wang P, et al. Heat-shock protein 90α is a potential prognostic and predictive biomarker in hepatocellular carcinoma: a large-scale and multicenter study. Hepatol Int. 2022;16(5):1208–1219. doi: 10.1007/s12072-022-10391-y [DOI] [PMC free article] [PubMed] [Google Scholar]