Abstract
Background
Emergency medicine (EM) residencies offer a wide variety of scheduling models for pediatric patient experience, including blocked weeks in pediatric emergency departments and longitudinal models with pediatric emergency pod/department shifts integrated within other clinical experiences. Concerns with autonomy, attending entrustment, and resident comfort imply that these different scheduling models may impact EM residents' pediatric procedure volumes. The purpose of this study is to quantitatively compare EM residents' pediatric procedure experience and volumes between block versus longitudinal scheduling models. We hypothesize noninferiority between the scheduling models.
Methods
A retrospective review characterized the numbers and types of procedures performed by The Ohio State Emergency Medicine residents at the tertiary care pediatric hospital where residents' receive their pediatric emergency medicine clinical experience. Procedure numbers and variety were compared across six academic years: four with a block model, one reorganization year, and one integrated longitudinal year.
Results
2552 procedures were performed by 266 resident academic years over the 6‐year period. Overall, no statistically significant differences in the number of procedures performed per year or the variety of types of procedures performed per year were found when comparing the block and longitudinal models. Differences were seen in experience of PGY1 versus PGY3 residents between scheduling models and the overall experience and volumes of the PGY2 residents during the reorganization year.
Conclusions
Our study quantitatively concluded that the longitudinal scheduling model is noninferior to the more traditional block scheduling model for emergency medicine residents' pediatric emergency medicine clinical experience when reviewing volumes and types of procedures performed in a pediatric emergency department. This suggests that procedural opportunities do not need to dictate scheduling models.
BACKGROUND
Emergency medicine (EM) residency programs are tasked with training residents to care for patients of all ages and acuity. Pediatric patients aged 0–14 make up 19.7% of national annual emergency department (ED) visits, with 80% of pediatric visits occurring under the care of general EM physicians without specialized pediatric emergency medicine (PEM) training. 1 , 2 While the Accreditation Council for Graduate Medical Education (ACGME) requires that 20% of patient encounters during EM residency are with pediatric patients, EM residents' patient experiences are limited due to access to pediatric care facilities and duty hour restrictions. 3 EM educators and residency program leaders have raised concerns regarding the impact these limitations have on residents' educational experience including fewer patient encounters, more hand‐offs, and less flexibility to provide extra‐clinical educational opportunities. 3 , 4
While some residency programs have a high number of pediatric patients at their primary training site, other programs must send their residents to affiliated pediatric hospitals, and many programs supplement pediatric education with pediatric intensive care or pediatric surgery rotations. Many EM residency programs send their residents to affiliated tertiary care pediatric children's hospitals to increase encounters with critically ill pediatric patients, traumas, and procedures. 5 , 6 , 7 However, despite specific pediatric ED experiences, even upon graduation EM residents continue to have deficits in pediatric critical care procedures and resuscitations. 6 , 8 , 9 , 10 At the conclusion of their training, many EM physicians cite pediatrics and pediatric procedures as an area of weakness. 11 , 12 , 13 Additionally, there are trends towards fewer procedures in pediatric EDs, such as fewer intubations in favor of noninvasive ventilation or less frequent lumbar punctures in febrile neonates, 14 , 15 which further limits EM residents opportunities to hone their pediatric procedure skills. 9 , 16
The likelihood of performing pediatric specific procedures is not limited to rotations at affiliated tertiary care pediatric hospitals but extends to the residency program's scheduling model itself. Traditional block scheduling models utilize separate PEM months over the course of training, where residents rotate in a pediatric emergency department (PED) and only see pediatric patients during these pediatric blocks. Alternative models provide a longitudinal experience by integrating pediatric specific shifts into general EM months year round. There is no literature to support which model is more commonly used in EM residencies nationwide or the factors that lead programs to select a block vs. longitudinal pediatric rotation model. Perceived benefits to the integrated longitudinal pediatric shift model include exposure to seasonal variation, a well‐reported phenomenon in the PED, and the ability to transition from adult to pediatric patients more seamlessly as is done in most community EDs. 17 , 18 However, other studies have shown that resident entrustment is highly influenced by scheduling and the familiarity attending physicians have with residents. 19 , 20 , 21 An integrated longitudinal scheduling model has the potential to decrease attending familiarity with residents, with studies suggesting that lack of familiarity with residents may limit entrustment of residents to perform procedures in a PED. 19 , 22
The purpose of this study is to quantitatively compare two common models of EM pediatric education and determine which model is superior to the other with regard to providing more opportunities to learn pediatric procedures. We hypothesize noninferiority between block vs. longitudinal schedules for EM residents' pediatric procedure experience.
METHODS
Study setting
Pediatric encounters were based out of the PED at Nationwide Children's Hospital (NCH), an urban children's hospital in Columbus, Ohio that has an annual ED census of ~90,000 visits. The PED has between 14–18 residency programs rotating in each academic year (AY), with variation in the number of programs and residents annually. The typical make‐up includes the NCH pediatric residency programs, 3–5 emergency medicine residencies from the central Ohio area, and 7–10 family medicine residencies from Columbus and the central Ohio area. Additionally, NCH is home to one of the largest pediatric emergency medicine fellowships in the nation and all residents staff a portion of their patient encounters with fellows.
As a tertiary care referral hospital, NCH has extensive resources available in the PED including consultants and procedure technicians, which may limit residents' procedure experience. For example, multiple orthopedic residency programs rotate at NCH and are largely responsible for performing fracture reductions, thereby limiting fracture reduction and/or splint/cast placement opportunities. NCH also has a robust suture/orthopedic technician program made up of Licensed Practical Nurses with specialized training in wound and orthopedic injury management, whose primary responsibilities include laceration repairs, incision and drainage, digital blocks, and splint/cast placement. Residents are able to perform these procedures but given the overall volume of patients and scheduling of residents to the higher acuity sections within the PED, there may be fewer opportunities to perform these procedures than at similar pediatric hospitals without suture/orthopedic technicians. 23
Study population
This study specifically examines the procedures performed by The Ohio State University (OSU) emergency medicine residents at NCH as they changed from a block to a longitudinal schedule. The residency's primary training site has a negligible volume of pediatric encounters, so their PEM clinical experience has always occurred via dedicated pediatric shifts at NCH. Given the significant schedule differences between a 3‐year vs. a 5‐year residency, combined OSU EM/Internal Medicine residents were excluded.
In the baseline period of academic years (AY) July 2013–June 2017 (AY1‐AY4), the categorical EM residents rotated in the PED for five 4‐week blocks, one as Post‐Graduate Year (PGY) 1 s, two as PGY2s, and two as PGY3s. Beginning in July 2017 (AY5), based on feedback from residents and interviewees, the OSU EM residency switched to a longitudinal shift model. PGY1s continued have pediatric shifts at NCH during an isolated 4‐week block. PGY2s and PGY3s moved to an integrated longitudinal scheduling model where pediatric shifts were integrated into each ED block, resulting in 12–14 adult shifts and 3–4 pediatric shifts during each 4‐week block. The total NCH pediatric shifts numbers for PGY2s and PGY3s did not change between scheduling models.
A total of six academic years (AY) were included in the study from July 1, 2013 through June 30, 2019. During the first four academic years (AY1‐AY4) all residents were on the traditional block schedule, and these “Block” years combined to provide our baseline averages. Academic Year 5 represents a “Reorganization” year, as this was the first year PGY2s and PGY3s were on a longitudinal schedule. Although all residents had the same scheduling model in the “Reorganization” Year (AY5) and the “Longitudinal” year (AY6), these years were separated for statistical analysis. In the Reorganization Year (AY5) PGY3 residents had experienced their pediatric shifts under both the traditional block and new longitudinal schedule, block schedule as PGY2s in AY4, and longitudinal schedule as PGY3s in AY5. Given the possible entrustment that had been built during the residents' block schedule as PGY2s, the authors felt AY5 and AY6 should be reviewed separately. Additional Longitudinal Years were not included in this study, because of the impactful drop in patient encounters related to the Covid‐19 pandemic.
Study design and analysis
A retrospective review of PED encounters from July 2013–June 2019 was performed. The institutional review board of Nationwide Children's Hospital approved the study. In collaboration with the OSU Emergency Medicine residency leadership a list of residents for each academic year was provided. The electronic medical record was queried for all procedure notes written by OSU EM residents within the study time frame. The procedures were then coded into one of the 16 core procedure categories noted in Figure 1. Individual patient charts were reviewed as needed to provide clarity of the procedure performed. Procedure notes that described procedures other than core procedures were removed. Each procedure entry was coded to include Academic Year 1–6 of the study period and resident PGY at the time of the procedure.
FIGURE 1.
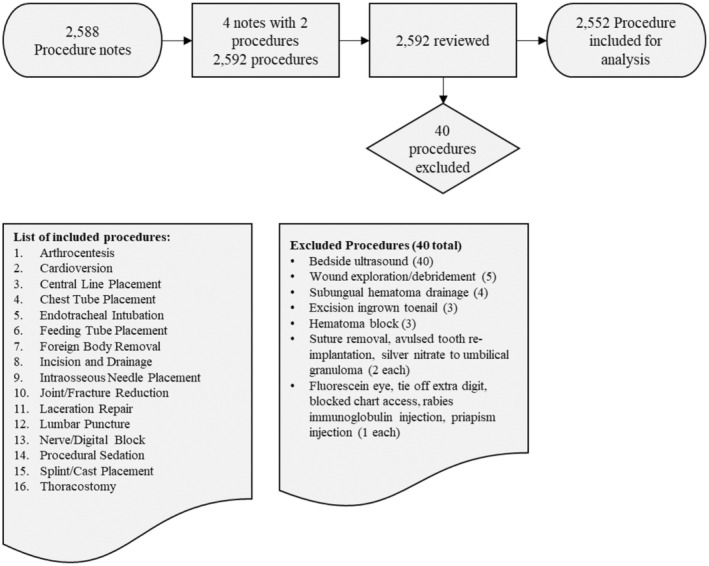
Procedure designation and review.
Data analyses were conducted with SAS Enterprise Guide version 8.1. Descriptive statistics were used to summarize the data (the mean and standard deviation for numerical variables, and frequency and percentage for categorical variables). Fisher's Exact test was used to compare the number of procedures between groups on procedure level. The mean number procedures were compared by Analysis of Variance (ANOVA). p values less than 0.05 were considered statistically significant.
RESULTS
The initial data query resulted in 2588 procedure notes. Four notes included two separate procedures in the same note. During review and coding, 40 procedures that were not representative of tracked procedures (e.g., Fluorescein stain of eye, bedside ultrasound) were excluded (Figure 1). A total of 2552 procedures comprised the analytic sample. Over the 6‐year study period, the average annual number of patients seen in the PED remained stable and 266 resident academic years were analyzed. There was an increase in the number of residents in the EM residency program during study period from 12 residents in the graduating class of 2014 to 16 residents in the graduating classes of 2018 and 2019 (Table 1). The proportion of female residents fluctuated between classes though was similar across academic years. While the total procedures performed by OSU EM residents (range 401–475) did not change (Table 1), the average number of procedures performed by each resident did decline over the course of study (11.88 in AY1 vs. 8.79 in AY6). Similarly, over the 6‐year study period, the number of different types of procedures performed by each resident (range 11–15) did not change; however, the average number of different types of procedures performed by each resident declined (4.8 in AY1 vs. 3.5 in AY6).
TABLE 1.
Description of residents and procedures
| Scheduling model | |||||||
|---|---|---|---|---|---|---|---|
| Block | Reorganization | Longitudinal | |||||
| Academic years (AY) | AY1 (2013–2014) | AY2 (2014–2015) | AY3 (2015–2016) | AY4 (2016–2017) | Block cumulative | AY5 (2017–2018) | AY6 (2018–2019) |
| Residents | |||||||
| % Female | 15 (37.5%) | 13 (31%) | 17 (40%) | 22 (48%) | ‐ | 26 (55%) | 28 (58%) |
| Total number of residents a | 40 | 42 | 43 | 46 | 171 | 47 | 48 |
| Post graduate year 1 (PGY1) | 14 | 14 | 15 | 16 | 59 | 15 | 16 |
| Post graduate year 2 (PGY2) | 14 | 14 | 14 | 16 | 58 | 16 | 15 |
| Post graduate year 3 (PGY3) | 12 | 14 | 14 | 14 | 54 | 16 | 17 |
| Procedures | |||||||
| Total number of procedures | 475 | 407 | 433 | 401 | 1716 | 420 | 416 |
| Mean (SD) number of procedures | 11.9 (4.5) | 9.7 (7.0) | 10.1 (7.2) | 8.7 (4.8) | 10.04 (6.06) | 8.9 (5.7) | 8.7 (5.4) |
| Total number types of procedures | 13 | 15 | 11 | 14 | ‐ | 13 | 12 |
| Mean (SD) number of types of procedures | 4.8 (1.6) | 4.1 (1.8) | 3.6 (1.5) | 3.6 (1.7) | ‐ | 3.4 (1.8) | 3.5 (1.4) |
Note: The gray shade indicates the combination of the four columns (AY1, AY2, AY3, and AY4).
Fluctuations in the number of residents per graduating class each Academic Year due to residents leaving or joining the program, Family and Medical Leave Act extensions, and remediation.
The most common procedures performed by residents were procedural sedation (n = 1002) and lumbar puncture (n = 763). There were differences in the numbers of each type of procedure performed between the Block, Reorganization, and Longitudinal academic years (Table 2). Overall, there was no significant difference in the number of each procedure performed by residents between the Block and Longitudinal groups. Some common procedures such as laceration repair, foreign body removal, digital block, and incision and drainage had limited numbers performed by residents in this cohort, as many of these procedures were performed by suture techs. A few specific procedures, such as cardioversion, central line placement, and thoracotomy were too infrequent for statistical comparisons between scheduling models.
TABLE 2.
Types of procedures by scheduling model
| Overall Total | Block a | Reorganization a | Longitudinal a | Block vs. Reorg. | Block vs. Longitudinal | Reorg. vs. Longitudinal | |
|---|---|---|---|---|---|---|---|
| Mean/Year | p value | p value | p value | ||||
| Procedural sedation | 1002 | 158.25 | 222 | 147 | <0.0001 | 0.5709 | <0.0001 |
| Lumbar puncture | 763 | 132 | 88 | 147 | <0.0001 | 0.078 | <0.0001 |
| Endotracheal intubation | 208 | 33.75 | 33 | 40 | 1 | 0.2332 | 0.3924 |
| Joint reduction | 172 | 33.25 | 18 | 21 | 0.0141 | 0.0576 | 0.6263 |
| Incision and drainage | 114 | 22.75 | 10 | 13 | 0.0099 | 0.0748 | 0.5339 |
| Laceration repair | 101 | 16.75 | 17 | 17 | 0.8888 | 0.8882 | 1 |
| Foreign body removal | 74 | 14.25 | 6 | 11 | 0.0370 | 0.5377 | 0.2311 |
| Splint/cast placement | 43 | 7.75 | 6 | 6 | 0.8343 | 0.8339 | 1 |
| Intraosseous needle placement | 27 | 3.25 | 8 | 6 | 0.0484 | 0.2381 | 0.7888 |
| Nerve/digital block | 17 | ‐ | 3 | 2 | 1 | 1 | 1 |
| Feeding tube placement | 18 | 1.75 | 7 | 4 | 0.0103 | 0.2409 | 0.5462 |
| Central line placement b | 4 | ‐ | 1 | 0 | |||
| Chest tube placement b | 4 | ‐ | 0 | 2 | |||
| Arthrocentesis b | 3 | ‐ | 1 | 0 | |||
| Cardioversion b | 1 | ‐ | 0 | 0 | |||
| Thoracostomy b | 1 | ‐ | 0 | 0 | |||
| Total | 2552 | 429 | 420 | 416 |
Note: Bolded values are to highlight statistically significant (p < 0.05) value given the large number of comparisons.
Block includes Academic Years 2013–2017 (AY1‐4), Reorganization is Academic Year 2017–2018 (AY5), and Longitudinal is Academic Year 2018–2019 (AY6).
Cell sizes too small for statistical comparisons.
A one‐way ANOVA was performed to compare the three different scheduling models (Table 3). There was no significant difference in the average numbers of procedures performed when all resident years (PGY1 to PGY3) were included and specifically no significant difference was noted between Block model and Longitudinal year (AY6) (p = 0.20). The averages for each PGY year by AY and scheduling model are presented in Figure 2.
TABLE 3.
Number of procedures by post graduate year (PGY) and scheduling model
| Block | Reorganization | Longitudinal | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Total sum | Mean | SD | df | F a | Overall p value | N | Total sum | Mean | SD | df | F | Block vs. Reorg. p value | N | Total sum | Mean | SD | df | F | Block vs. Long. p value | |
| PGY 1 | 59 | 362 | 6.14 | 4.79 | 2 | 2.81 | 0.0654 | 15 | 86 | 5.73 | 2.74 | 1 | 0.10 | 0.7563 | 16 | 54 | 3.38 | 1.89 | 1 | 5.06 | 0.0275 |
| PGY 2 | 58 | 719 | 12.4 | 6.16 | 2 | 4.90 | 0.0097 | 16 | 126 | 7.88 | 4.00 | 1 | 7.69 | 0.0071 | 15 | 143 | 9.53 | 4.14 | 1 | 2.89 | 0.0936 |
| PGY 3 | 54 | 635 | 11.76 | 5.09 | 2 | 0.89 | 0.4164 | 15 | 202 | 13.47 | 7.00 | 1 | 1.11 | 0.2949 | 17 | 225 | 13.24 | 4.52 | 1 | 1.14 | 0.2885 |
| TOTAL | 171 | 1716 | 10.04 | 6.06 | 2 | 1.14 | 0.321 | 46 | 414 | 9.00 | 5.79 | 1 | 1.08 | 0.3006 | 48 | 422 | 8.79 | 5.52 | 1 | 1.64 | 0.2021 |
Note: Bolded values are to highlight statistically significant (p < 0.05) value given the large number of comparisons.
F test from the ANOVA compared means across the three groups: Block, Reorganization, and Longitudinal years.
FIGURE 2.
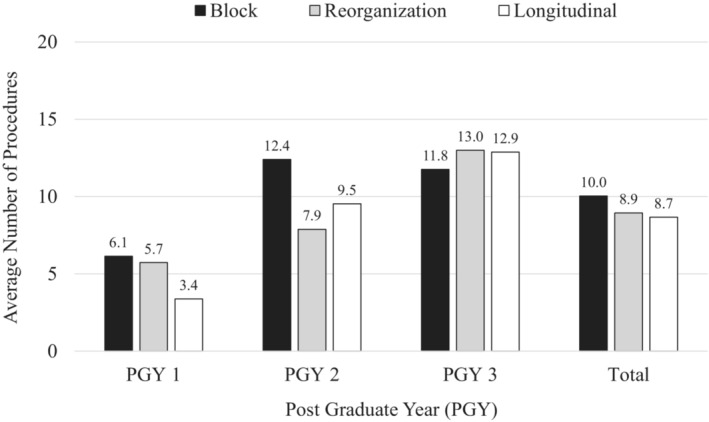
Average number of procedures conducted by residents per academic year.
Interns (PGY1) on average performed fewer procedures in the Longitudinal year vs. Block years (Block 6.14 vs. Longitudinal 3.38, F(1,1) = [5.06], p = 0.03). Overall the PGY2s performed more procedures when comparing all three scheduling variations (F(2,1) = [4.90], p = 0.01). Specifically, during the Reorganization year, the PGY2s performed a significantly lower number of procedures (Block 12.40 vs. Reorganization 7.88, F(1,1) = [7.69], p = 0.01). Despite this, no significant difference was observed for the PGY2s in comparison of the Block vs. Longitudinal schedules (Block 12.4 vs. Longitudinal 9.52; p = 0.09). The PGY3 residents had no statistically significant difference in average number of procedures with one‐way ANOVA testing comparing all scheduling variations (F(2,1) = [0.89], p = 0.4160) and specifically no difference was noted between the Block and Longitudinal schedule (Block 11.76 vs. Longitudinal 13.24; p = 0.29).
The average number of types of procedures each resident performed between scheduling models was not significantly different (Table 4). Across all PGY years there was no difference between Block and Longitudinal scheduling (p = 0.13). However, PGY3s performed more types of procedures than PGY1s, and there was a difference between schedules for the intern PGY1 year (Block 3.1 vs. Longitudinal 2.06; p = 0.02). In comparing Block vs. Longitudinal, there was no statistically significant difference in the variety of procedures performed in the PGY2 year (p = 0.24) or the PGY3 year (p = 0.68). In looking at the Reorganization year, there was a difference in the number of types of procedures performed both for all PGY years combined (Block 3.98 vs. Reorganization 3.39; p = 0.43) and specifically for the PGY2 residents (Block 4.36 vs. Reorganization 3.19; p = 0.01).
TABLE 4.
Types of procedures by post graduate year (PGY) and scheduling model
| Block | Reorganization | Longitudinal | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Types sum | Mean | SD | Overall a p value | N | Types sum | Mean | SD | Block v. Reorg. p value | N | Types sum | Mean | SD | Block v. Long. p value | |
| PGY 1 | 59 | 183 | 3.10 | 1.74 | 0.0469 | 15 | 39 | 2.60 | 1.24 | 0.2977 | 16 | 33 | 2.06 | 0.44 | 0.0210 |
| PGY 2 | 58 | 253 | 4.36 | 1.55 | 0.0251 | 16 | 51 | 3.19 | 1.87 | 0.0125 | 15 | 58 | 3.87 | 0.92 | 0.2419 |
| PGY 3 | 54 | 245 | 4.54 | 1.53 | 0.8536 | 15 | 66 | 4.40 | 1.88 | 0.7711 | 17 | 80 | 4.71 | 1.26 | 0.6807 |
| TOTAL | 171 | 681 | 3.98 | 1.73 | 0.0634 | 46 | 156 | 3.39 | 1.82 | 0.0428 | 48 | 171 | 3.56 | 1.46 | 0.1256 |
Note: Bolded values are to highlight statistically significant (p < 0.05) value given the large number of comparisons.
Overall ANOVA compared means across the three groups: Block, Reorganization, and Longitudinal years.
DISCUSSION
Longitudinal scheduling demonstrated noninferiority in procedural experience for emergency medicine residents training at a large tertiary children's hospital. The average number of procedures performed by this large cohort of trainees at one of the busiest children's hospitals in the country was stable through a 6‐year study period during which they reorganized from a traditional block schedule to a longitudinal model for PGY2 and PGY3 residents. We analyzed over 2500 procedures during the 6‐year period. While slight differences appeared during the Reorganization year, this resolved when comparing the Block vs. Longitudinal years. Overall, we conclude that longitudinal scheduling is noninferior to traditional block scheduling for EM residents' quantitative pediatric procedure experience.
There was an overall decrease in the average number of procedures performed per OSU resident across the years, without notable difference in the overall number of procedures each academic year by the cohort. This suggests a finite number of procedures performed in an ED, and as training program sizes increase it dilutes individual residents’ clinical experiences with bedside procedures.
While there was no appreciable difference in procedure experience between the longitudinal and block scheduling models, the trends and timing of when residents did the most procedures is concerning. Given that the average procedure numbers were stable, there was a general trend each year of fewer procedures per resident. Since there is a finite number of pediatric procedures in the clinical setting and procedure proficiency needs to be gained, programs may need to consider alternate learning environments such as anesthesia rotations or simulation. Additionally, there was a limited number of nerve blocks, laceration repairs, incision and drainage, joint reductions, and splint placement, likely due to other GME learners and suture/orthopedic techs. Residency program directors and ED directors must continue to weigh the impact outside learners and flow/efficiency initiatives have on residents and long‐term skill competency. When comparing the Block vs. Longitudinal schedule, there was a significant decrease in the number of procedures and variety of procedures performed during the intern year (Tables 3 and 4). Given that career planning decisions, including pursuit of fellowship, academic, or community practice, are often made during PGY2 year, care must be taken that procedural experience in the first 2 years is sufficient for trainees to make these choices with confidence.
It is unclear if entrustment plays a role in this change, but it was noted in previous studies 19 , 21 , 22 that attending familiarity with residents, which is limited with the longitudinal schedule, could have negative impact on attendings' entrustment of residents to perform pediatric procedures. Additionally, the notable decline in procedures performed by PGY2 residents during the reorganization year may have been due to entrustment concerns. Programs must monitor residents’ procedure experiences especially during time of programmatic change (i.e., Reorganization year, AY5) to ensure the best training environment for those residents. Additionally, less clinical procedural experience impacts competence with the mechanics and “muscle memory” of a procedure prior to independent practice and limits learning opportunities from experienced educators and attending staff on tips, tricks, and ways to avoid complications. While we conclude the scheduling models are noninferior, program directors and residents must weigh how the different scheduling models may impact their individual group of learners.
Overall, the ACGME tracks only a small subset of general procedures in EM, and care should be taken throughout the curriculum to utilize a variety of learning modalities, only one of which is the clinical setting, to ensure adequate experience for trainees. While this study shows that scheduling models appear equivocal, other factors such as which staff/residents are performing procedures at the training institution, fellowship interest, and resident future career locations (academic vs. community, rural vs. urban) may impact scheduling decisions of residency programs. This analysis alleviates concern about the quantitative impact of longitudinal scheduling on procedural training. Institutions and training programs should feel free to utilize other factors in determining which scheduling model is optimal for their learner group.
LIMITATIONS
General trends were seen that may have benefited from an additional academic year of review. However, due to the Covid‐19 pandemic in the subsequent academic year (July 2019–June 2020) and associated rapid decline in patient volumes seen at NCH and children's hospitals across the country, the additional year of data would not have allowed for accurate comparison between that academic year and the preceding years. The impact Covid‐19 may have on the workforce now entering into independent practice, in terms of procedural experience, is an opportunity for future study.
Procedures were queried utilizing the author of the procedure note. If a procedure note was filed by an attending or fellow documenting the resident's performance of a procedure this would not have been captured by our data query. This may have missed some procedure involvement such as unsuccessful LP or intubation attempts by residents, although in general at our institution, residents log the procedure regardless of the number of attempts or by whom. Additionally, should a resident have documented the procedure within their ED Provider Note rather than a separate procedure note, this would not have been captured in the data query. Reviewing all resident ED encounters for possible procedure notes embedded with provider notes was not within the scope of this project. Some note templates embed the procedure note within the provider note, such as a nursemaid's elbow reduction procedure note contained within the template nursemaid elbow provider note, so some of these procedures were likely uncaptured in the data query.
Finally, this was a single residency program study with pediatric experience based at an affiliated tertiary care pediatric hospital. Residency programs without separate pediatric hospitals or with high volumes of pediatric patients at their primary training site within general emergency department months may have procedure opportunities that may not be generalizable to this type of residency model. Additionally, programs without separate Pediatric EM faculty at the tertiary pediatric hospital outside of the EM residency may not have procedure entrustment concerns possibly contributing to resident procedure volumes. However, given the large number of programs who rely on a tertiary care PED for training, this is likely generalizable to many emergency medicine residency programs, though admittedly not all.
CONCLUSION
Utilizing a large data set comprising 6 years of procedures in one of the largest PEDs in the country, this single emergency medicine residency program retrospective chart review quantitatively concluded that longitudinal scheduling is a noninferior scheduling method compared to traditional block scheduling for emergency medicine resident pediatric procedure experience. Trends such as overall decline in number of procedures performed annually and decrease number and variety of procedures in the PGY2 class may affect a resident's career choice and long‐term proficiency. Several factors should be considered by a program prior to implementing a new scheduling model. Residency program directors can choose a scheduling model without concern that schedule type will have a negative impact on their residents’ pediatric procedure experience.
AUTHOR CONTRIBUTIONS
MR, CL, and JM conceptualized and designed the study, performed the interpretation of the data, drafted the initial manuscript, and reviewed and revised the manuscript. JS conducted the data analysis. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FUNDING INFORMATION
The project was supported through internal funding from the Division of Emergency Medicine at Nationwide Children's Hospital, Columbus, Ohio.
CONFLICT OF INTEREST
MR, CL, JS, and JM report no conflicts of interest.
Reynolds MS, Lo C, Shi J, Mitzman J. Scheduling doesn't matter! A noninferiority study of block versus longitudinal scheduling for emergency medicine resident pediatric procedural training experience. AEM Educ Train. 2023;7:e10838. doi: 10.1002/aet2.10838
REFERENCES
- 1. Hudgins JD, Monuteaux MC, Bourgeois FT, et al. Complexity and severity of pediatric patients treated at United States emergency departments. J Pediatr. 2017;186:145‐149. e1. [DOI] [PubMed] [Google Scholar]
- 2. CDC . National Hospital Ambulatory Medical Care Survey, 2018 Emergency Department Summary Tables. 2018.
- 3. ACGME . ACGME program requirements for graduate medical education in emergency medicine. 2021.
- 4. Hoelle RM, Vega T, Atanelov Z, Toklu H. Emergency medicine residency programs: the changing face of graduate medical education. Int J Med Educ. 2018;9:9‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Burns R, Auerbach M, Mitzman J. Pediatric emergency medicine curricula for emergency medicine residents. AEM Educ Train. 2021;5:147‐148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cloutier RL, Walthall JD, Mull CC, Nypaver MM, Baren JM. Best educational practices in pediatric emergency medicine during emergency medicine residency training: guiding principles and expert recommendations. Acad Emerg Med. 2010;17(Suppl 2):S104‐S113. [DOI] [PubMed] [Google Scholar]
- 7. Mitzman J, King AM, Fastle RK, et al. A modified Delphi study for development of a pediatric curriculum for emergency medicine residents. AEM Educ Train. 2017;1:140‐150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chen EH, Cho CS, Shofer FS, Mills AM, Baren JM. Resident exposure to critical patients in a pediatric emergency department. Pediatr Emerg Care. 2007;23:774‐778. [DOI] [PubMed] [Google Scholar]
- 9. Chen EH, Shofer FS, Baren JM. Emergency medicine resident rotation in pediatric emergency medicine: what kind of experience are we providing? Acad Emerg Med. 2004;11:771‐773. [DOI] [PubMed] [Google Scholar]
- 10. Douglass A, Yip K, Lumanauw D, Fleischman RJ, Jordan J, Tanen DA. Resident clinical experience in the emergency department: patient encounters by postgraduate year. AEM Educ Train. 2019;3:243‐250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Loftus KV, Schumacher DJ, Mittiga MR, McDonough E, Sobolewski B. A descriptive analysis of the cumulative experiences of emergency medicine residents in the pediatric emergency department. AEM Educ Train. 2021;5:e10462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Simon HK, Sullivan F. Confidence in performance of pediatric emergency medicine procedures by community emergency practitioners. Pediatr Emerg Care. 1996;12:336‐339. [DOI] [PubMed] [Google Scholar]
- 13. Chen W‐C, Chaou C‐H, Ng C‐J, Liu Y‐P, Chang Y‐C. Assessing the effectiveness of pediatric emergency medicine education in emergency medicine residency training: a national survey. Hong Kong J Emerg Med. 2022;29(6):349‐357. [Google Scholar]
- 14. Pantell RH, Roberts KB, Adams WG, et al. Evaluation and Management of Well‐Appearing Febrile Infants 8 to 60 days old. Pediatrics. 2021;148(2):e2021052228. [DOI] [PubMed] [Google Scholar]
- 15. Wolfler A, Raimondi G, Pagan de Paganis C, Zoia E. The infant with severe bronchiolitis: from high flow nasal cannula to continuous positive airway pressure and mechanical ventilation. Minerva Pediatr. 2018;70:612‐622. [DOI] [PubMed] [Google Scholar]
- 16. Iyer MS, Way DP, Schumacher DJ, Lo CB, Leslie LK. What procedures are important to general pediatricians and why? Acad Pediatr. 2021;21:1281‐1287. [DOI] [PubMed] [Google Scholar]
- 17. Cohen HA, Blau H, Hoshen M, Batat E, Balicer RD. Seasonality of asthma: a retrospective population study. Pediatrics. 2014;133:e923‐e932. [DOI] [PubMed] [Google Scholar]
- 18. Lipsett SC, Monuteaux MC, Fine AM. Seasonality of common pediatric infectious diseases. Pediatr Emerg Care. 2021;37:82‐85. [DOI] [PubMed] [Google Scholar]
- 19. Tiyyagura G, Balmer D, Chaudoin L, et al. The greater good: how supervising physicians make entrustment decisions in the pediatric emergency department. Acad Pediatr. 2014;14:597‐602. [DOI] [PubMed] [Google Scholar]
- 20. Sterkenburg A, Barach P, Kalkman C, Gielen M, ten Cate O. When do supervising physicians decide to entrust residents with unsupervised tasks? Acad Med. 2010;85:1408‐1417. [DOI] [PubMed] [Google Scholar]
- 21. Choo KJ, Arora VM, Barach P, Johnson JK, Farnan JM. How do supervising physicians decide to entrust residents with unsupervised tasks? A Qualitative Analysis. J Hosp Med. 2014;9:169‐175. [DOI] [PubMed] [Google Scholar]
- 22. Mitzman J, Way DP. Block versus longitudinal scheduling of emergency medicine Residents' rotation in an independent Children's hospital: pediatric emergency medicine attending Faculty's perspective. Cureus. 2019;11:e6476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wagner TL, Dunn MW, Iyer MS, Buckingham D, Spencer SP. A quality improvement initiative to increase the number of pediatric resident laceration repairs. J Grad Med Educ. 2020;12:51‐57. [DOI] [PMC free article] [PubMed] [Google Scholar]


