Abstract
Screening for adult Attention-Deficit/Hyperactivity Disorder (ADHD) and differentiating ADHD from comorbid mental health disorders remains to be clinically challenging. A screening tool for ADHD and comorbid mental health disorders is essential, as most adult ADHD is comorbid with several mental health disorders. The current pilot study enrolled 955 consecutive patients attending a tertiary mental health center in Canada and who completed EarlyDetect assessment, with 45.2% of patients diagnosed with ADHD. The best ADHD classification model using composite scoring achieved a balanced accuracy of 0.788, showing a 2.1% increase compared to standalone ADHD screening, detecting four more patients with ADHD per 100 patients. The classification model including ADHD with comorbidity was also successful (balanced accuracy = 0.712). The results suggest the novel screening method can improve ADHD detection accuracy and inform the risk of ADHD with comorbidity, and may further inform specific comorbidity including MDD and BD.
Keywords: ADHD screening, ADHD comorbidity, adult ADHD, machine-learning, mental health
Attention-Deficit/Hyperactivity Disorder (ADHD) is a neuro-developmental disorder characterized by inattentive or hyperactive/impulsive behavior with a variety of functionally impairing symptoms (American Psychiatric Association, 2013). ADHD is one of the most common disorders in children with a worldwide prevalence of 5% to 12% (Polanczyk et al., 2007), and remains highly prevalent in adults at 4.4% (Kessler et al., 2006), costing $74 billion in the United States, and $6 to $11 billion annually in Canada (Centre for ADHD Awareness Canada, 2017).
Although a significant portion of childhood ADHD persists into adulthood (Simon et al., 2009; Thomas et al., 2015), clinicians do not routinely screen for adult ADHD. Furthermore, complicating the diagnosis of adult ADHD, are symptom overlap with many other mental disorders, and the common phenotype of adult ADHD and comorbid mental health disorders (Adler et al., 2017; Klassen et al., 2010), such as major depressive disorder (MDD), bipolar disorder (BD), personality disorder, and substance abuse (Watters et al., 2018; Wilens & Biederman, 2006). Lack of appropriate screening for adult ADHD leads to missed, inappropriate, and delayed diagnosis of ADHD and comorbid mental health disorders (De Graaf et al., 2013; Ginsberg et al., 2014; Hankey et al., 2020; Hoyle et al., 2015). Since ADHD with comorbidity also confers poor functional outcomes (Hankey et al., 2020), it is crucial to confirm ADHD and comorbid disorders as soon as possible to choose the appropriate treatments to improve functional outcomes. In addition, adult ADHD symptoms may present differently from childhood ADHD symptoms (Adler et al., 2017; Agnew-Blais et al., 2016; Moffitt et al., 2015; Thomas et al., 2015) further contributing to missed and delayed diagnoses in adult patients. The detrimental outcomes are similar between adult and childhood ADHD (Ginsberg et al., 2014), including negative physical health consequences such as obesity, smoking, asthma, migraines, emergency room visits, and injury-related insurance claims and accidental deaths (Agnew-Blais et al., 2016; Catalá-López et al., 2022; Dalsgaard et al., 2015; Lundervold et al., 2019; Sadeghi-Bazargani et al., 2019); and poor socio-economical outcomes such as higher chance to drop out of school (Fleming & McMahon, 2012), financial problems from ADHD-associated impulsivity at work (Asherson et al., 2012; Pinna et al., 2019) and increased chance to involve in criminal activities or live in detention centers (Baggio et al., 2018). Despite the diagnostic challenges, accurate early diagnoses and appropriate treatment of ADHD could be effective to curb the negative outcomes (Oliva et al., 2021).
Currently, ADHD screening involves multiple aspects such as the DSM-5 criteria, self-report questionnaires, neurocognitive computerized tests, and clinical histories (Gualtieri & Johnson, 2005), where no single test is completely indicative of ADHD, and physicians’ judgment remains the gold standard. The World Health Organization Adult ADHD Self-Report Scale (ASRS) (Kessler et al., 2005) is a short self-report screener with six questions derived from the DSM-IV ADHD to screen for adult ADHD. ASRS has been widely used by physicians and validated in a variety of health care settings (Gray et al., 2014; Silverstein et al., 2018). However, the interpretation of ASRS results offers little insight on the presence of comorbid diagnoses. Thus, we developed EarlyDetect, a digital screening system incorporating the ASRS as a primary screening tool for ADHD, while simultaneously screening for the more common comorbid mental health disorders including Major Depression Disorder (MDD), Bipolar Disorder (BD), Generalized Anxiety Disorder (GAD), and Alcohol Use Disorder (AUD) (Y. Liu et al., 2021; Y. S. Liu et al., 2021). The EarlyDetect screening tool has been shown to improve screening of MDD and BD when compared to existing screening instruments such as PHQ-9 and MDQ respectively (Y. Liu et al., 2021; Y. S. Liu et al., 2021). Compared with a single-disease-focused screening approach, the EarlyDetect has been shown to reap benefits from machine-learning algorithms, including enhanced screening performance (Y. Liu et al., 2021; Y. S. Liu et al., 2021). and insights on reducing screening times (Y. S. Liu et al., 2021).
In this study, we aim to develop a machine learning model to screen and identify ADHD based on EarlyDetect, by utilizing individual questions from the ASRS in conjunction with questions from other clinical questionnaires. We also aim to examine whether EarlyDetect could offer additional insight on determining comorbid diagnoses of ADHD, specifically MDD and BD.
Methods
Sample and Study Population
This single-center, retrospective, naturalistic study, approved by the University of Alberta Health Research Ethics Board, included 955 participants (56.4% female, 1% other; mean age = 35.35, SD = 12.83); 45.2% subsequently diagnosed with ADHD, see Table 1 for subsample summary). Between June 2016 and October 2018, patients who agreed to participate provided written consent upon arrival at their first visit to an interdisciplinary, referral-based tertiary mental health center in western Canada. Participants were not pre-selected based on inclusion or exclusion criteria. Participation was voluntary, with no monetary incentives. Participants were asked to complete the EarlyDetect questionnaire, after which they were seen by one of the center’s certified psychiatrists, who was blinded to the results of the screening questionnaires, for face-to-face assessment, diagnosis, and treatment as usual. Physician diagnosis of ADHD was based on DSM-5 criteria (American Psychiatric Association, 2013).
Table 1.
Study Sample Summary.
| Age | Non-ADHD patients (n = 523) | ADHD patients (n = 432) | |||
|---|---|---|---|---|---|
| Mean (std) | Range | Mean (std) | Range | p Value | |
| 38.70 (13.51) | 17–76 | 31.31 (10.66) | 17–66 | <.001 | |
| n | % | n | % | ||
| Gender = Female | 331 | 63.3 | 208 | 48.2 | <.001 |
| Gender = Male | 189 | 36.1 | 217 | 50.2 | <.001 |
| Gender = Other | 3 | 0.6 | 7 | 1.6 | .114 |
| MDD | 235 | 44.9 | 95 | 22.0 | <.001 |
| GAD | 196 | 37.5 | 136 | 31.5 | .053 |
| BD | 72 | 13.8 | 107 | 24.8 | <.001 |
| AUD | 25 | 4.8 | 25 | 5.8 | .487 |
| ADHD only | 0 | 0.0 | 163 | 37.7 | na |
Note. Due to some patients having multiple comorbidities, the total proportion will not equal 100%. The p values were based on paired sample t-test on age, and two by two χ2 tests for all frequency-based variables.
EarlyDetect Questionnaires
The EarlyDetect is a set of self-report clinical questionnaires distilled to approximate the clinical interview process. The current version of EarlyDetect (Y. Liu et al., 2021; Y. S. Liu et al., 2021) consists of a proprietary Life History Questionnaire (LHQ) probing a patient’s mental health history, two proprietary ADHD screening questions for initial ADHD screening, and ASRS-v1.1—Part A for ADHD-specific symptom screening, and the Sheehan Disability Scale (SDS) (Sheehan et al., 1996) as a proxy indicator of self-reported functional impairments. In addition to ADHD-specific screening, EarlyDetect also screens for MDD, BD, GAD, and AUD (Y. Liu et al., 2021; Y. S. Liu et al., 2021).
Statistical Analysis
For evaluation and comparison of screening performance, we adapted a machine learning approach from earlier studies (Y. Liu et al., 2021; Y. S. Liu et al., 2021). Machine learning analyses were conducted using Python 3.6 with Scikit-Learn 0.22.1. The individual questions for each clinical questionnaire, including yes/no answers to MINI Screening questions, were used as model features. Missing values in continuous variables were imputed using the mean of the non-missing cases. Missing values in categorical variables were coded as a new category. Questions using Likert-scales or representing numerical values (e.g., age) were treated as continuous variables and rescaled using the StandardScaler function, questions with a binary yes/no answer or representing categories were dummy encoded, resulting in a total of 134 features. For all analyses, selected features were used to predict the diagnosis of ADHD using Elastic Net (Zou & Hastie, 2005) with a five-fold internal cross-validation for hyperparameter tuning and a fixed L1 ratio of 0.5. The models were optimized for balanced accuracy (Brodersen et al., 2010), defined as an average of sensitivity and specificity. We used a leave-one-out cross-validation procedure (LOOCV) for external cross-validation, where data from each patient was reserved to test a learned model’s performance trained with the remaining sample, iterating through all patients. Thus, classification performances of the LOOCV were literally a collection of individual-level model predictions. The use of cross-validation for hyperparameter tuning combined with external cross-validation to evaluate model performances is also known as nested-cross-validation, a technique widely used in machine-learning studies to evaluate a model’s generalizability (Kassraian-Fard et al., 2016; Wong, 2015). We present the cross-validation results by evaluating the model predicted label against the actual diagnosis label of ADHD. As baseline comparisons, we fitted two additional models using the same LOOCV procedure: Baseline A is using only the original ASRS scores (Kessler et al., 2005). Baseline B is using all six individual questions from the ASRS as features. Because cross-validation results are representing the model’s performance on data withheld from the computer during model building, it represents the model’s ability to generalize to new data, where the numerical difference in cross-validation performance alone is commonly used to select the best model. To further evaluate the numerical difference statistically, McNamar’s test (Dietterich, 1998) was conducted to evaluate the LOOCV performance of the best model versus other models.
Predictive features were selected if the feature’s coefficients were consistently non-zero across the LOOCV iterations. Then the selected features were ranked based on the magnitude of the averaged coefficient value of the Elastic Net models across all LOOCV iterations.
To explore model performance on differentiating ADHD and ADHD with comorbid conditions. We further conducted a 3-way classification, dividing the ADHD label into a group with only ADHD diagnosis (ADHD_pure, n = 163) and a group with ADHD and one or more comorbid diagnoses of MDD, BP, GAD, or AUD into separate classes (ADHD_comorbid, n = 269), in addition to the class of patients without an ADHD diagnosis (no ADHD, n = 523).
Results
Classification Performance
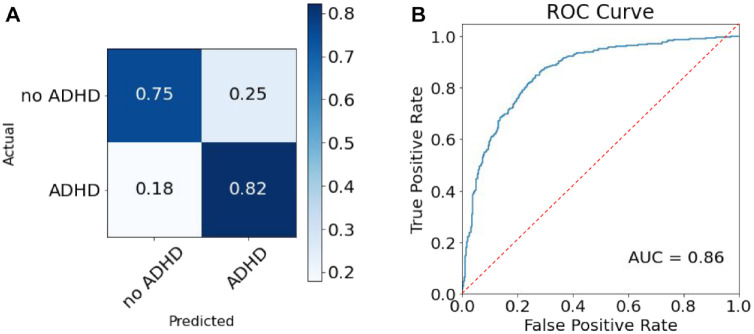
The LOOCV performance of the Elastic Net model using answers to individual questions as features reached a balanced accuracy of 0.788 for classifying ADHD, with a sensitivity of 0.822 and a specificity of 0.753, with positive predictive value and negative predictive value for ADHD at 0.733 and 0.837 respectively (see Figure 1). Thus, 82.2% of patients with ADHD can be identified by the model, whereas 75.3% of patients with no ADHD can be identified by the model. If a patient is screened positive, there is a 73.3% chance the patient has ADHD, and if a patient is screened negative, there is an 83.7% chance the patient does not have ADHD. All baseline models had lower balanced accuracy than the model based on all individual questions, 0.767 for model A, 0.780 for model B (Table 2) with the model using all individual questions outperforming baseline models when considering both sensitivity and specificity, by 2.1% to the model based on ASRS original score (χ2 = 12.4, p < .001), and 0.8% to the model based on individual questions of ASRS (χ2 = 4.4, p < .05).
Figure 1.
Model performance on ADHD classification.
Note. Panel A presents the confusion matrix of the LOOCV performance for the best-performing model. Panel B presents the Receiver Operating Characteristic Curve. AUC stands for the area under the curve.
Table 2.
Model Comparisons.
| Balanced accuracy | Sensitivity | Specificity | PPV | NPV | |
|---|---|---|---|---|---|
| All individual questions | 0.788 | 0.822 | 0.753 | 0.733 | 0.837 |
| Baseline A: ASRS original score | 0.767 | 0.724 | 0.807 | 0.757 | 0.781 |
| Baseline B: Individual questions from ASRS | 0.780 | 0.847 | 0.713 | 0.709 | 0.849 |
Note. PPV denotes positive predictive value, and NPV denotes negative predictive value. The model with the highest balanced accuracy is in bold.
Predictive Features
Our machine-learning algorithm selected 30 predictive features. Among the top 10 ranked predictive features, the most predictive features are the first and second stem ADHD screening questions probing ADHD symptoms of childhood and whether symptoms continue as an adult, where experiencing ADHD symptoms and continued experience of the symptoms in adulthood are positively associated with an ADHD diagnosis. Other top predictive features where an increase in score is associated with an increased chance of ADHD diagnoses are Mini International Neuropsychiatric Interview-(Hypo)Manic Episode (MINI-HME) (Sheehan et al., 1998), question 6 on ASRS probing for hyperactivity (Kessler et al., 2005). The higher age of the patient, higher age of first feeling unwell, higher SDS score on experiencing disability of social life and leisure activities (Sheehan et al., 1996), children not having diagnosed mental health issues, being female, experienced other (not listed) stressful life events are associated with lower risk of ADHD diagnoses (Figure 2).
Figure 2.
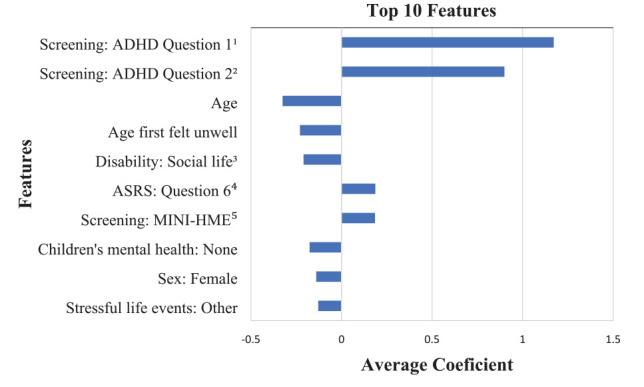
Top 10 features on ADHD classification.
Note. The average coefficient values were calculated from all individual Elastic Net models in LOOCV.
1“As a child, were you often fidgety, restless, unable to concentrate or remember things, disorganized, or impulsive and did these symptoms make it difficult to complete tasks such as homework or get along with others?”
2“Do you still experience some of these symptoms as an adult?”
3“The symptoms have disrupted your social life/leisure activities.”
4“How often do you feel overly active and compelled to do things, like you were driven by a motor?”
5“Have you ever had a period of time when you were feeling ‘up’ or ‘high’ or ‘hyper’ or so full of energy or full of yourself that you got into trouble, or that other people thought you were not your usual self? (Do not consider times when you were intoxicated on drugs or alcohol.).”
Comorbidity
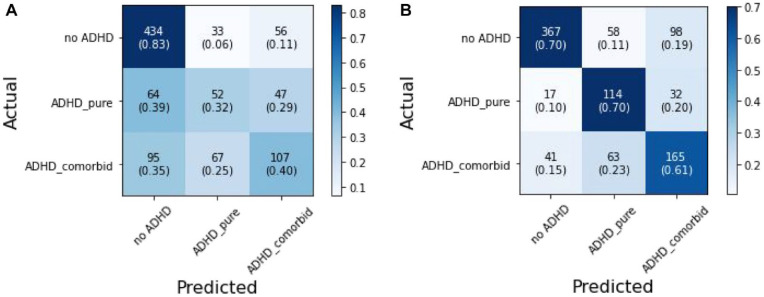
In the 3-way classification task, the model based only on ASRS questions failed to differentiate between comorbid ADHD and pure ADHD patients, the cell prediction is performing close to the chance level (Figure 3a). The model based on individual questions from EarlyDetect performed adequately on the 3-way classification to differentiate the pure ADHD, comorbid ADHD, and no ADHD cases (Figure 3b). Overall, the kappa coefficient (Landis & Koch, 1977), representing a chance adjusted agreement between predicted and actual label, is higher for the individual-question-based model than the ASRS-only model, with a fair agreement (κ = .336) and moderate agreement (κ = .484) respectively. For identifying pure ADHD in the 3-way classification model, the classification performance is comparable to the binary classification models, at a balanced accuracy of 77.3%, with a sensitivity of 69.9% and a specificity of 84.7%. The classification of comorbid ADHD cases is at a balanced accuracy of 71.2%, with a sensitivity of 61.3% and a specificity of 81.0%.
Figure 3.
LOOCV results on the classification of ADHD with comorbidity table.
Note. Panel A presents the confusion matrix of the LOOCV performance for the model using individual questions from ASRS. Panel B presents the confusion matrix of the LOOCV performance for the model using all individual questions. Individual cell presents frequency counts followed by row-wise proportions.
Discussions
Adult ADHD is most often associated with comorbid mental health disorders, such as major depressive disorder and bipolar disorder. Missed diagnosis of comorbid mental health disorders associated with ADHD confers significant functional impairment. Thus, it is of paramount importance to screen for ADHD and comorbid disorders from the onset of a clinical evaluation.
This study presents preliminary evidence that a machine learning approach integrating multiple sources of mental health assessment scales may offer superior performance in screening for adult ADHD and comorbid disorders such as MDD and BD, in line with similar approaches in screening for MDD (Y. Liu et al., 2021) and BD (Y. S. Liu et al., 2021). To the best of our knowledge, this machine learning approach using EarlyDetect is the first screening instrument that has a high predictive value screening for ADHD and comorbid MDD and BD. A set of top predictive features underly the machine-learning model’s performance were identified, consistent with known ADHD risk factors. The study also demonstrates that harvesting multiple sources of patients’ self-report data can offer additional benefits in identifying ADHD patients with comorbid conditions, which may facilitate diagnostic clarification. This current study demonstrates the successful identification of ADHD and ADHD with comorbidity. Although the current model was not built to facilitate screening of specific comorbidity, it should prompt clinicians to probe for comorbidity.
Reassuringly, EarlyDetect has been validated on screening for MDD and BD, and thus provides confidence to screen for these disorders in patients with comorbid ADHD (Y. Liu et al., 2021; Y. S. Liu et al., 2021). When an ADHD patient was flagged for potential comorbidity, clinicians can use the MDD and BD screening module to rule in and rule out MDD and BD, the most common and functional impairing comorbid disorders of ADHD.
The best-performing model using all questions collected from EarlyDetect as features achieved a 2.1% increase in balanced accuracy compared to the threshold-cut-off-based scoring of ASRS. Albeit a smaller numerical lead in balanced accuracy at 0.8%, the best-fitting model performs significantly better than a model based on individual questions from ASRS. The improved performance may be explained by the model’s access to more features from other screening tests. Because balanced accuracy is an average of sensitivity and specificity, a 2.1% increase in balanced accuracy may translate to a sensitivity increase of 4.2% if specificity can be held as a constant, detecting four more patients with ADHD per 100 patients.
The top 10 features underly ADHD classification echo known factors associated with ADHD. The ADHD screening questions probing for patients’ ADHD symptoms from childhood (question 1) to adulthood (question 2) were the top two contributing features respectively for ADHD classification. Other risk factors associated with an increased chance of ADHD are ASRS’s question 6 probing for hyperactivity symptoms, and the MINI-HME screening for mania symptoms with can also be present in ADHD (Klassen et al., 2010). Demographics information including higher age, higher age when first felt mentally unwell, and being female are utilized by the model contributing to reduced risk of ADHD, this may be attributed to ADHD’s earlier onset than other common mental health disorders screened by EarlyDetect and its disproportionally higher diagnosed rates in male than female (Hankey et al., 2020; Kessler et al., 2006). The best-fitting model also associates lower social life disability compared to other common mental health disorders with ADHD patients, as well as reporting no mental health conditions for children and experiencing non-typical stressful life events. Those results need to be interpreted with caution. Lower social life disability in ADHD patients needs to be interpreted in the context that other psychiatric diagnoses such as MDD and BD may be associated with more severe disabilities, this does not suggest ADHD patients have no impairment in social function; further, ADHD is a developmental disorder, thus maybe less associated with stressful life events, yet we cannot interpret the results with confidence as the “other” option of stressful life events were not logged. Also due to the chronic and developmental nature of ADHD, unlike MDD and BD that are episodic in nature where patients are more aware of the contrasts between well and unwell periods, ADHD patients may not realize their social functioning has been affected because they have no experience of a normal or well social function as a comparison reference. Moreover, the lack of report on children’s mental health history may be arbitrarily associated with the younger age of ADHD patients in our sample, they may either not have children or has a smaller time window to identify children’s mental health history.
Comorbidity
Up to 70% of adult ADHD is associated with comorbidities (Kessler et al., 2006). Our sample echoes Kessler et al.’s (2006) results, finding that 63.3% (N = 269) of patients diagnosed with ADHD had at least one comorbidity amongst MDD, GAD, BD, and AUD. When each comorbid diagnosis was considered individually, we found that 22.0% of ADHD patients have comorbid MDD, 31.5% have comorbid GAD, and 24.8% have comorbid BD (Table 1). The function to detect risk of comorbid mental health conditions with ADHD is an important property for a screening tool and may have a significant impact on treatment options selection and positively impact treatment outcomes. Our analysis demonstrates that a single-purpose screening tool such as the ASRS lacks the ability to detect comorbidity risks, where comorbidity risks could be evaluated by using multiple screening tools. ADHD patients with comorbid psychiatric diagnoses are generally suffering from more functional disabilities than ADHD patients without comorbidities (Hankey et al., 2020). Thus, early identification of the comorbidity risk of ADHD may enable appropriate intervention to prevent severe disability. For example, for ADHD patients with comorbid bipolar disorder, if the bipolar disorder is undiagnosed, prescribing psychostimulant medication may trigger manic episodes and worsen the patient’s mental health condition (Viktorin et al., 2017). For ADHD patients with a comorbid MDD, treatment options may include medications that may benefit both MDD and ADHD symptoms such as Bupropion (Bond et al., 2012).
Limitations
The study results need to be interpreted with caution, as data were collected under a naturalistic setting, where the diagnoses and self-report assessments both contain an element of bias (Y. Liu et al., 2021). The study also did not look at identifying specific comorbidities with ADHD, for example, ADHD comorbid with GAD. Another limitation is the use of a single-blinded rater. However, this is a pilot project needing replication of the EarlyDetect screening tool with large a sample size, multiple raters, and centers.
Conclusion
The high comorbidity rates of adult ADHD drive the demand for an ADHD screening tool to inform comorbidity risks to facilitate more accurate clinical diagnosis and may lead to better downstream treatment outcomes. The current pilot study implemented a machine-learning-based screening of ADHD, and ADHD with comorbidity by utilizing multiple clinical questionnaires in addition to ASRS. The results showed preliminary evidence this novel screening method can improve ADHD detection accuracy and inform the risk of ADHD with comorbidity at a tertiary mental health center, warranting future validation studies.
Acknowledgments
We acknowledge the Chokka center for Integrative Health and MITACS Accelerate Scholarship for funding support, and The Chokka Center for Integrative Health for research site provision and onsite support. We thank Kevin Zhan for his contribution on background literature search.
Author Biographies
Dr. Yang S. Liu is a postdoctoral researcher at the department of psychiatry, University of Alberta. Dr. Liu is interested in computational psychiatry and personalized medicine, and leveraging cross-linked administrative health records, electronic medical records, multimodal patient data, and machine-learning to improve patient experience and clinical outcome.
Dr. Bo Cao is an associate professor at the department of psychiatry, University of Alberta, and Canada Research Chair in computational psychiatry. Dr. Cao’s is interested in computational psychiatry and precision medicine in mental health.
Dr. Pratap Chokka is a clinical professor at the department of psychiatry, University of Alberta, founder and CEO of Chokka Center for Integrative Health, and a consultant psychiatrist at the Grey Nuns Hospital in Edmonton, Alberta, Canada.
Footnotes
Author Contributions: Yang S. Liu designed the study, processed, quality-controlled and analyzed the data, drafted the manuscript, and critically edited the manuscript. Bo Cao and Pratap Chokka designed the study, supervised the data processing, provided instrumental support, and critically edited the manuscript draft.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: P. Chokka reports grants from Pfizer, Janssen, Lundbeck, Purdue, Shire, and Allergan. These are all unrelated to the submitted work.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by a MITACS Accelerate Industrial Postdoc Scholarship (IT13648). MITACS had no role in study design, data collection, analysis, or interpretation, report writing, or the decision to submit the article for publication. MITACS provided salary support for Y. S. Liu.
ORCID iD: Yang S. Liu  https://orcid.org/0000-0003-0406-8056
https://orcid.org/0000-0003-0406-8056
References
- Adler L. A., Faraone S. V., Spencer T. J., Berglund P., Alperin S., Kessler R. C. (2017). The structure of adult ADHD. International Journal of Methods in Psychiatric Research, 26(1), e1555. 10.1002/mpr.1555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agnew-Blais J. C., Polanczyk G. V., Danese A., Wertz J., Moffitt T. E., Arseneault L. (2016). Evaluation of the persistence, remission, and emergence of attention-deficit/hyperactivity disorder in young adulthood. JAMA Psychiatry, 73(7), 713–720. 10.1001/jamapsychiatry.2016.0465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Author. [Google Scholar]
- Asherson P., Akehurst R., Kooij J. J., Huss M., Beusterien K., Sasané R., Gholizadeh S., Hodgkins P. (2012). Under diagnosis of adult ADHD: Cultural influences and societal burden. Journal of Attention Disorders, 16(5 Suppl), 20S–38S. 10.1177/1087054711435360 [DOI] [PubMed] [Google Scholar]
- Baggio S., Fructuoso A., Guimaraes M., Fois E., Golay D., Heller P., Perroud N., Aubry C., Young S., Delessert D., Gétaz L., Tran N. T., Wolff H. (2018). Prevalence of attention deficit hyperactivity disorder in detention settings: A systematic review and meta-analysis. Frontiers in Psychiatry, 9, 331. 10.3389/fpsyt.2018.00331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bond D. J., Hadjipavlou G., Lam R. W., McIntyre R. S., Beaulieu S., Schaffer A., Weiss M. (2012). The Canadian network for mood and anxiety treatments (CANMAT) task force recommendations for the management of patients with mood disorders and comorbid attention-deficit/hyperactivity disorder. Annals of Clinical Psychiatry, 24(1), 23–37. [PubMed] [Google Scholar]
- Brodersen K. H., Ong C. S., Stephan K. E., Buhmann J. M. (2010, August 23–26). The balanced accuracy and its posterior distribution [Conference session]. International Conference on Pattern Recognition, Istanbul, Turkey. 10.1109/ICPR.2010.764 [DOI] [Google Scholar]
- Catalá-López F., Hutton B., Page M. J., Driver J. A., Ridao M., Alonso-Arroyo A., Valencia A., Macías Saint-Gerons D., Tabarés-Seisdedos R. (2022). Mortality in persons with autism spectrum disorder or attention-deficit/hyperactivity disorder: A systematic review and meta-analysis. JAMA Pediatrics, 176(4), e216401. 10.1001/jamapediatrics.2021.6401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centre for ADHD Awareness Canada. (2017). Paying attention to the cost of ADHD. . . The price paid by Canadian families, governments and society. https://bcadhd.com/wp-content/uploads/2013/09/Paying-Attention-Paying-Attention-to-the-Cost-of-ADHD.-The-Price-Paid-by-Canadian-Families-Government-s-and-Society-caddac-for-Canadian-ADHD-Awareness-week-.pdf
- Dalsgaard S., Østergaard S. D., Leckman J. F., Mortensen P. B., Pedersen M. G. (2015). Mortality in children, adolescents, and adults with attention deficit hyperactivity disorder: A nationwide cohort study. Lancet, 385(9983), 2190–2196. 10.1016/s0140-6736(14)61684-6 [DOI] [PubMed] [Google Scholar]
- De Graaf R., Ten Have M., Tuithof M., Van Dorsselaer S. (2013). First-incidence of DSM-IV mood, anxiety and substance use disorders and its determinants: Results from the Netherlands Mental Health Survey and Incidence Study-2. Journal of Affective Disorders, 149(1–3), 100–107. [DOI] [PubMed] [Google Scholar]
- Dietterich T. G. (1998). Approximate statistical tests for comparing supervised classification learning algorithms. Neural Computation, 10(7), 1895–1923. 10.1162/089976698300017197 [DOI] [PubMed] [Google Scholar]
- Fleming A. P., McMahon R. J. (2012). Developmental context and treatment principles for ADHD among college students. Clinical Child and Family Psychology Review, 15(4), 303–329. 10.1007/s10567-012-0121-z [DOI] [PubMed] [Google Scholar]
- Ginsberg Y., Quintero J., Anand E., Casillas M., Upadhyaya H. P. (2014). Underdiagnosis of attention-deficit/hyperactivity disorder in adult patients: A review of the literature. The Primary Care Companion for CNS Disorders, 16(3), PCC.13r01600. 10.4088/PCC.13r01600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray S., Woltering S., Mawjee K., Tannock R. (2014). The adult ADHD self-report scale (ASRS): Utility in college students with attention-deficit/hyperactivity disorder. PeerJ, 2(1), e324. 10.7717/peerj.324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gualtieri C. T., Johnson L. G. (2005). ADHD: Is objective diagnosis possible? Psychiatry, 2(11), 44–53. [PMC free article] [PubMed] [Google Scholar]
- Hankey J., Liu Y., Chokka P. (2020). Adult ADHD: Prevalence, comorbidities, and patient-reported dysfunction in a tertiary mental health clinic. Psychiatry and Clinical Psychopharmacology, 30, 3–9. 10.5455/pcp.20200212045154 [DOI] [Google Scholar]
- Hoyle S., Elliott L., Comer L. (2015). Available screening tools for adults suffering from bipolar affective disorder in primary care: An integrative literature review. Journal of the American Association of Nurse Practitioners, 27(5), 280–289. 10.1002/2327-6924.12214 [DOI] [PubMed] [Google Scholar]
- Kassraian-Fard P., Matthis C., Balsters J. H., Maathuis M. H., Wenderoth N. (2016). Promises, pitfalls, and basic guidelines for applying machine learning classifiers to psychiatric imaging data, with autism as an example. Frontiers in Psychiatry, 7, 177. 10.3389/fpsyt.2016.00177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R. C., Adler L., Ames M., Demler O., Faraone S., Hiripi E., Howes M. J., Jin R., Secnik K., Spencer T., Ustun T. B., Walters E. E. (2005). The World Health Organization Adult ADHD self-report scale (ASRS): A short screening scale for use in the general population. Psychological Medicine, 35(2), 245–256. 10.1017/s0033291704002892 [DOI] [PubMed] [Google Scholar]
- Kessler R. C., Adler L., Barkley R., Biederman J., Conners C. K., Demler O., Faraone S. V., Greenhill L. L., Howes M. J., Secnik K., Spencer T., Ustun T. B., Walters E. E., Zaslavsky A. M. (2006). The prevalence and correlates of adult ADHD in the United States: Results from the National Comorbidity Survey Replication. American Journal of Psychiatry, 163(4), 716–723. 10.1176/ajp.2006.163.4.716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klassen L. J., Katzman M. A., Chokka P. (2010). Adult ADHD and its comorbidities, with a focus on bipolar disorder. Journal of Affective Disorders, 124(1–2), 1–8. 10.1016/j.jad.2009.06.036 [DOI] [PubMed] [Google Scholar]
- Landis J. R., Koch G. G. (1977). The measurement of observer agreement for categorical data. Biometrics, 33(1), 159–174. 10.2307/2529310 [DOI] [PubMed] [Google Scholar]
- Liu Y., Hankey J., Cao B., Chokka P. (2021). Screening for major depressive disorder in a tertiary mental health centre using EarlyDetect: A machine learning-based pilot study. Journal of Affective Disorders Reports, 3, 100062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y. S., Chokka S., Cao B., Chokka P. R. (2021). Screening for bipolar disorder in a tertiary mental health centre using EarlyDetect: A machine learning-based pilot study. Journal of Affective Disorders Reports, 6, 100215. [Google Scholar]
- Lundervold A. J., Halleland H. B., Brevik E. J., Haavik J., Sørensen L. (2019). Verbal memory function in intellectually well-functioning adults with ADHD: Relations to working memory and response inhibition. Journal of Attention Disorders, 23(10), 1188–1198. 10.1177/1087054715580842 [DOI] [PubMed] [Google Scholar]
- Moffitt T. E., Houts R., Asherson P., Belsky D. W., Corcoran D. L., Hammerle M., Harrington H., Hogan S., Meier M. H., Polanczyk G. V., Poulton R., Ramrakha S., Sugden K., Williams B., Rohde L. A., Caspi A. (2015). Is adult ADHD a childhood-onset neurodevelopmental disorder? Evidence from a four-decade longitudinal cohort study. American Journal of Psychiatry, 172(10), 967–977. 10.1176/appi.ajp.2015.14101266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliva F., Malandrone F., Mirabella S., Ferreri P., Girolamo G., Maina G. (2021). Diagnostic delay in ADHD: Duration of untreated illness and its socio-demographic and clinical predictors in a sample of adult outpatients. Early Intervention in Psychiatry, 15, 957–965. 10.1111/eip.13041 [DOI] [PubMed] [Google Scholar]
- Pinna M., Visioli C., Rago C. M., Manchia M., Tondo L., Baldessarini R. J. (2019). Attention deficit-hyperactivity disorder in adult bipolar disorder patients. Journal of Affective Disorders, 243, 391–396. 10.1016/j.jad.2018.09.038 [DOI] [PubMed] [Google Scholar]
- Polanczyk G., de Lima M. S., Horta B. L., Biederman J., Rohde L. A. (2007). The worldwide prevalence of ADHD: A systematic review and metaregression analysis. American Journal of Psychiatry, 164(6), 942–948. 10.1176/AJP.2007.164.6.942/ASSET/IMAGES/LARGE/R820F2.JPEG [DOI] [PubMed] [Google Scholar]
- Sadeghi-Bazargani H., Hasanzadeh K., Salarilak S., Amiri S., Golestani M., Shahedifar N. (2019). Evaluating the relationship between adult attention-deficit/hyperactivity disorder and riding behavior of motorcyclists. Journal of Injury and Violence Research, 11(1), 45–52. 10.5249/jivr.v11i1.1098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan D. V., Harnett-Sheehan K., Raj B. A. (1996). The measurement of disability. International Clinical Psychopharmacology, 11, 89–96. 10.1097/00004850-199606000-00015 [DOI] [PubMed] [Google Scholar]
- Sheehan D. V., Lecrubier Y., Sheehan K. H., Amorim P., Janavs J., Weiller E., Hergueta T., Baker R., Dunbar G. C. (1998). The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry, 59 Suppl 20, 22–33. [PubMed] [Google Scholar]
- Silverstein M. J., Alperin S., Faraone S. V., Kessler R. C., Adler L. A. (2018). Test-retest reliability of the adult ADHD Self-Report Scale (ASRS) v1.1 Screener in non-ADHD controls from a primary care physician practice. Family Practice, 35(3), 336–341. 10.1093/fampra/cmx115 [DOI] [PubMed] [Google Scholar]
- Simon V., Czobor P., Bálint S., Mészáros A., Bitter I. (2009). Prevalence and correlates of adult attention-deficit hyperactivity disorder: Meta-analysis. The British Journal of Psychiatry, 194(3), 204–211. 10.1192/bjp.bp.107.048827 [DOI] [PubMed] [Google Scholar]
- Thomas R., Sanders S., Doust J., Beller E., Glasziou P. (2015). Prevalence of attention-deficit/hyperactivity disorder: A systematic review and meta-analysis. Pediatrics, 135(4), e994–e1001. 10.1542/peds.2014-3482 [DOI] [PubMed] [Google Scholar]
- Viktorin A., Rydén E., Thase M. E., Chang Z., Lundholm C., D’Onofrio B. M., Almqvist C., Magnusson P. K., Lichtenstein P., Larsson H., Landén M. (2017). The risk of treatment-emergent mania with methylphenidate in bipolar disorder. American Journal of Psychiatry, 174(4), 341–348. 10.1176/appi.ajp.2016.16040467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watters C., Adamis D., McNicholas F., Gavin B. (2018). The impact of attention deficit hyperactivity disorder (ADHD) in adulthood: A qualitative study. Irish Journal of Psychological Medicine, 35(3), 173–179. 10.1017/ipm.2017.21 [DOI] [PubMed] [Google Scholar]
- Wilens T. E., Biederman J. (2006). Alcohol, drugs, and attention-deficit/hyperactivity disorder: A model for the study of addictions in youth. Journal of Psychopharmacology, 20(4), 580–588. 10.1177/0269881105058776 [DOI] [PubMed] [Google Scholar]
- Wong T. T. (2015). Performance evaluation of classification algorithms by k-fold and leave-one-out cross validation. Pattern Recognition, 48(9), 2839–2846. 10.1016/j.patcog.2015.03.009 [DOI] [Google Scholar]
- Zou H., Hastie T. (2005). Regularization and variable selection via the elastic net. Journal of the Royal Statistical Society: Series B (Statistical Methodology), 67(2), 301-320. [Google Scholar]