Highlights
-
•
The ABCD Substance Use Workgroup describes substance use patterns within the cohort.
-
•
The ABCD cohort is entering adolescence and initiating substance use.
-
•
By ages 12–13, nearly 40% report lifetime substance experimentation and/or use.
-
•
Nearly 7.5% also reported lifetime substance use (>experimentation).
-
•
Sociodemographic and parental substance problems remain as predictors of initiation.
Keywords: Substance use, Adolescence, Substance initiation, Alcohol sipping, ABCD study, Children
Abstract
Background
Though largely substance-naïve at enrollment, a proportion of the youth in the Adolescent Brain Cognitive Development (ABCD) Study are expected to initiate substance use (SU) as they transition into later adolescence. With annual data from youth 9–13 years-old, this study aims to describe their SU patterns over time. Here, prevalence rates of use are reported, along with predicted odds of use while analyzing common risk-factors associated with youth SU.
Methods
The ABCD StudyⓇ enrolled 11,876 participants at Baseline (ages 9-10) and has followed them annually. Data through half of the third follow-up visit are available (ages 12-13; n = 6,251). SU descriptives for all psychoactive substances over time are outlined. General estimating equations (GEEs) assessed whether sociodemographic factors, internalizing and externalizing symptoms, and parental SU problems were associated with SU between Baseline and Y2 follow-up.
Results
Across time, alcohol and nicotine remain the most used substances. Yearly rates of any SU increased (past-year use: 13.9% in Y1; 14% Y2, 18.4% Y3). Cumulatively, by Y3, 39.7% of the cohort reported experimenting (e.g., sipping alcohol) with SU within their lifetime, while 7.4% reported a “full use” (a full alcohol drink, nicotine use, cannabis use, or any other SU) in their lifetime (past-year: 1.9% alcohol, 2.1% nicotine, 1.1% cannabis, 1.2% other substances). GEEs revealed ongoing longitudinal associations between sociodemographic factors, greater externalizing symptoms, and parental drug problems with increased odds of initiating SU.
Conclusions
As ABCD participants transition into their teenage years, the cohort is initiating SU at increasing (though still low) rates.
1. Introduction
The Adolescent Brain Cognitive DevelopmentSM Study (ABCD StudyⓇ) is a landmark study designed to prospectively follow nearly 12,000 youth from early childhood through adolescence to examine factors that influence neurodevelopment broadly, including the impact of substance use (Jernigan et al., 2018; Lisdahl et al., 2018; Volkow et al., 2018). Consistent with study aims to delineate developmental trajectories following the onset of substance use (SU), the ABCD Study successfully recruited a national, diverse cohort of 9–10 year-old youths who were almost exclusively substance naïve at study enrollment (2016–2018; <1% reporting SU beyond sipping alcohol) (Garavan et al., 2018; Lisdahl et al., 2021). These youth have since been followed with annual in-person assessments, including detailed SU patterns interviews (Lisdahl et al., 2018; Lisdahl et al., 2021) with data for the full cohort available through the second follow-up visit and half the cohort through the third follow-up visit (ages 12-13). Data are released yearly to the scientific community through an open-science model (Jernigan et al., 2018; Volkow et al., 2018).
As the ABCD Study cohort transitions into their teenage years, it is important to continue to document SU patterns and potential sociodemographic differences in early onset use; particularly as scientific teams accessing the data examine more nuanced predictors of SU trajectories. Participants within the ABCD study are beginning to reach the age that corresponds to other national datasets of substance use prevalence in adolescents (e.g., the National Survey on Drug Use and Health), which begins at age 12 (SAMHSA, 2021), or the Monitoring the Future (MTF) study, which begins at age 13 (Johnston et al., 2021). Estimates of lifetime prevalence of drug use in 2021 as measured in MTF indicate that, in 8th graders (often ages 13-14), 21.7% have ever used alcohol, 10.2% used cannabis, 7.0% used cigarettes, and 16.6% used electronic nicotine delivery systems (ENDS or vaping). The ABCD Study cohort was younger than the MTF Study surveys at Baseline and had minimal (<1%) use of full doses of any substance, though 22.5% of the cohort reported alcohol sipping at Baseline (Lisdahl et al., 2021). This substance experimentation (e.g., alcohol sipping; nicotine or cannabis puffing) may be an important predecessor to later substance use (Jackson et al., 2015a), thus continued tracking of low-level use is important during the early and middle adolescent years.
In addition to monitoring prevalence rates of early substance initiation, it is also important to identify early sociodemographic differences or risk factors associated with this onset and which may moderate later substance-related outcomes (Squeglia and Cservenka, 2017; Tapert and Eberson-Shumate, 2022). Prior studies suggest sociodemographic characteristics [e.g., high SES, male sex, unmarried parents; (Pelham et al., 2021; Squeglia et al., 2017)] are significant predictors of substance use onset. Family history of alcohol and drug dependence, especially in parents, are linked to earlier substance initiation and increased problems and dependence in offspring (Chassin et al., 2002; Cox et al., 2021; Grant and Dawson, 1997; Henry, 2017; Schuckit and Smith, 1996; Tapert and Eberson-Shumate, 2022). Early signs of psychopathology are also considered an early risk-factor. Externalizing symptoms are most commonly linked to substance use, including early initiation (Cox et al., 2021; Edwards et al., 2016; Ning et al., 2020; Squeglia et al., 2017), while internalizing symptoms are less frequently associated (Ning et al., 2020). Consistent with these results, Baseline data from the ABCD Study revealed being male, being older, having a familial history of substance problems, and greater externalizing symptoms were associated with early alcohol sipping behaviors (Lisdahl et al., 2021).
As the scientific community plans to engage in future data analytic studies around SU, the ABCD Study Substance Use Workgroup aims to describe the patterns of SU reported by youth at the ABCD Study Year 1 (ages 10-11), Year 2 (ages 11-12), and Year 3 (ages 12-13) follow-up sessions (for the whole-cohort and by sex at birth). In addition, in order to highlight important factors to consider longitudinally, this study seeks to identify the associations between previously identified common risk factors (e.g., sociodemographic, parental history of SU problems, mental health symptoms) and early substance use experimentation and initiation from Baseline to Year 2 follow-up sessions. It was hypothesized that previously identified predictors of use (i.e., males, older age, familial history of substance problems, and greater reported externalizing symptoms) will be robust predictors of odds of substance use (SU) initiation during the early adolescent years (Lisdahl et al., 2021).
2. Materials and methods
2.1. Participants and procedures
Participants in the current study included 11,876 youth who enrolled in the ABCD Study at Baseline (Y0), with all available yearly follow-up (Y1, Y2, Y3) and Mid-Year (i.e., six-month) interval phone follow-up (follow-up months: M6, M18, M30) data included for analyses. Participants and their parents/guardians were recruited from 21 U.S. research sites between 2016–2018 using a stratified probability sample of eligible schools to match the sociodemographic profile of the American Community Survey (ACS) [for details: Garavan et al. (2018)]. All study procedures were approved by a centralized institutional review board (IRB) at the University of California, San Diego. Exclusion criteria for the ABCD Study at Baseline enrollment are detailed in the Supplement. Informed consent was obtained from parents/guardians and assent from youth at each session.
At each yearly visit, youth and one parent/guardian participated in 1-2 sessions, which comprised of a comprehensive battery of biological and behavioral assessment modules, including: substance use (Lisdahl et al., 2018), mental and physical health (Barch et al., 2018), peer, family, culture, and environment (Zucker et al., 2018), biological markers (Uban et al., 2018), genetics (Iacono et al., 2018), neurocognitive (Luciana et al., 2018), and magnetic resonance brain imaging (Casey et al., 2018). All annual interviews were conducted in person up until the beginning of the COVID-19 pandemic; participants then completed interviews via private video calls or telephone calls, with only a select number completing in-person visits between March 2020 and February 2021. Questionnaires were primarily administered via iPad through REDCap (Harris et al., 2009), which was harmonized across sites (Auchter et al., 2018). Youth were interviewed separately from parents in private spaces (both during in-person and virtual visits). Mid-Year interval phone follow-up consisted of an abbreviated battery and contained past six-month substance use modules (Lisdahl et al., 2018). The current study utilized data from ABCD Data Release 4.0 (DOI: 10.15154/1523041, October 2021; data collected through February 15, 2021), which includes the full cohort for Y0-Y2 and half the Y3 cohort.
Importantly, confidentiality was reiterated to the youth prior to administration of the substance use module. Youth were asked if they had “heard of” a list of substances (in Y0-Y2 only; see details in Supplement) and, if so, tried/experimented with any substances (see below for comprehensive list); follow-up questionnaires were given only if the youth endorsed experimental use.
2.2. Measures
2.2.1. Sociodemographic factors
Identity and household sociodemographic factors were included in the statistical analyses as covariates: age at Y0 (in months), ageΔ at each follow-up (i.e., change in age relative to Y0), sex assigned at birth (herein referred to as “sex”), 4-levels of self-identified race (Asian, Black, White, Mixed/Other), ethnicity (Hispanic/Latinx, non-Hispanic/Latinx), parent/guardian educational attainment (<HS Diploma, HS Diploma, Some College, Bachelor Degree, Post Graduate Degree), parent/guardian marital status (married, not married), and household income (<$50,000, $50,000-$100,000, >$100,000) (Barch et al., 2018).
2.2.2. Alcohol, nicotine, and cannabis experimentation/low-level use measures
Youth annually completed the iSay Sipping Inventory (Jackson et al., 2013; Jackson et al., 2015b), an 8-item measure of recent alcohol sipping that characterized their first alcohol sipping experience (Lisdahl et al., 2018). First experimentation of nicotine or cannabis product was also assessed (Lisdahl et al., 2018). Follow-up questions about the circumstances around their first use (e.g., age of first use, type of product, from whom they received the substance) were only given at one time-point (i.e., their first use).
2.2.3. Lifetime & past 6-month (Y0)/yearly (Y1-Y3) SU patterns
At Baseline (Y0), youth were asked if they used each major drug category in their lifetime; multiple formal and informal names (including popular names) of each substance were provided (Lisdahl et al., 2018). If youth endorsed using a full standard unit of the substance in the past six months (Y0) or since last study session (Y1-Y3), a web-based Timeline Follow-Back (TLFB) interview was administered for that timeframe (Lisdahl et al., 2018; Sobell and Sobell, 1992). Lifetime SU and TLFB interviews assessed for all substances, including: alcohol, nicotine products [i.e., cigarettes, ENDS/vaping (tobacco), smokeless tobacco, cigars, hookah, pipe, and nicotine replacement products], cannabis products [smoked flower, vaped flower, smoked blunts, edibles, smoked concentrates, vaped concentrates, oral tinctures, cannabis-infused alcohol drinks, and non-medical cannabidiol (CBD)], synthetic cannabinoids, cocaine, cathinones, methamphetamine, ecstasy/MDMA, ketamine, gamma-hydroxybutyrate (GHB), heroin, psilocybin, salvia, other hallucinogens [lysergic acid diethylamide (LSD), phencyclidine (PCP), synthetic hallucinogens], anabolic steroids, inhalants, and prescription misuse of stimulants, sedatives, opioid pain relievers, and over-the-counter (OTC) cough/cold medicine (Lisdahl et al., 2018). Further, at Mid-Year phone follow-up, youth are asked past 6-month substance use, which is integrated into following yearly visit (e.g., M6 + Y1) to create a more comprehensive “past-year” substance use for each yearly follow-up.
For current analyses, SU variables were defined in the following ways:
-
•
SU “Experimentation” – low-level substance use (i.e., alcohol sipping, nicotine or cannabis puffing or trying).
-
•
SU “Initiation” – reported ≥1 standard alcohol drink, >puff/taste cannabis or nicotine or any other occasion of other substance use.
-
•
“Any” SU – either “experimentation” and/or “initiating” a substance (i.e., combines the two definitions above)
-
•
SU “Onset” – the year at which substance use was reported.
2.2.4. Parental history of problematic alcohol or drug use
Parents/Guardians were administered a Family History Assessment Module Screener (FHAM-S) (Rice et al., 1995) at Y0 which obtained biological family history of mental health, alcohol, and drug problems. For analyses, variables for biological parent history of problematic alcohol or drug use were utilized (yes, no).
2.2.5. Internalizing and externalizing scale
Parents rated their child's internalizing (includes withdrawn, somatic complaints, and anxiety/depressed problems) and externalizing behaviors (includes delinquent and aggressive behaviors) on the Child Behavior Checklist (CBCL) (Achenbach, 2009; Barch et al., 2018), which was administered at all yearly visits (Y0-Y3; See Supplementary Table 4). For analyses, raw scores for each scale were used.
2.3. Statistical analysis
Analyses were conducted in R (R Core Team, 2022) (v4.1.1) utilizing ABCD Data Release 4.0 (DOI: 10.15154/1523041, October 2021). First, descriptive statistics were computed for all variables described above (frequency and proportion of yes/no or means and standard deviations, where appropriate). Next, sex differences in “any” SU, SU “experimentation”, and SU “initiation” were investigated due to preestablished sex differences in use in this age range (Johnston et al., 2022); this was achieved through descriptive reporting, chi-square tests for dichotomous outcomes (Yate's correction was employed if a cell is <5), and t-test analyses for continuous outcomes. Lastly, in order to describe relationships between sociodemographic factors, parental history of problematic alcohol or substance use, or internalizing and externalizing behaviors, two Generalized Estimating Equations (GEEs) models [using geepack (Halekoh et al., 2006)] examined whether Y0 age, ageΔ (i.e., time), sex at birth, race, ethnicity, parent/guardian education, parent/guardian marital status, household income, parental history of problematic alcohol use, parental history of problematic drug use, CBCL internalizing scores, or CBCL externalizing scores were associated with dichotomized (1) “Any” SU or (2) SU “Initiation” outcomes (Y0-Y2). Y3 visit was removed from all GEEs due to only half the cohort's data being available; of note, this was decided because the first wave of the ABCD cohort is not fully representative of the entire cohort (e.g., sociodemographic variables). GEEs were fit with a binomial logistic regression, first-order autoregression correlational structure, and observations were clustered on participant to account for the repeated measures design. In the SU “Initiation” GEE, Asian-identifying youth were removed to improve model fit due to minimal SU initiation within this group. Results were considered significant if the Wald statistic (Wχ2) was at the p < .05 level. In addition, standardized odds ratio (OR), and 95% confidence intervals (CI) were derived and included for interpretation with rescaling applied to continuous predictors (Gelman, 2008).
2.3.1. Missing data
Participants with study visit information had minimal missing data; however, some participants (n = 1,229) had missing sociodemographic information which prevented their inclusion in GEE models. SU Prevalence information was included for all participants, including those who were not able to be included in GEEs.
3. Results
3.1. Sociodemographic variables
For sample sociodemographic information of the ABCD participants at Y0, see Table 1; 11,876 youth completed Y0 (ages 9-10), 11,225 completed Y1 (ages 10-11), 10,414 completed Y2 (ages 11-12), and 6,251 completed Y3 (ages 12-13) (data collection still ongoing).
Table 1.
Sociodemographic characteristics of the ABCD cohort at baseline (Y0).
| Mean (SD) [Range] or N (%) | ABCD Participants (N = 11,876) |
|---|---|
| Age (months) | 118.98 (7.5) [107,133] |
| Age (years) | 9.47 (0.54) [8,11] |
| Sex assigned at birth (M/F) | 6196/5680 (52.17%/47.83%) |
| Race | |
| White | 7524 (63%) |
| Black | 1869 (16%) |
| Asian | 275 (2%) |
| Other and >1 category | 2037 (17%) |
| Not reported | 171 (1%) |
| Ethnicity | |
| Non-Hispanic/Latinx | 9312 (78%) |
| Hispanic/Latinx | 2411 (20%) |
| Not reported | 153 (1%) |
| Parental Annual Household Income | |
| <$50,000 | 3223 (27%) |
| $50,000-$100,000 | 3071 (26%) |
| >$100,000 | 4564 (38%) |
| Not reported | 1018 (9%) |
| Parental Highest Education | |
| <High School Diploma | 593 (5%) |
| High School Diploma/GED | 1132 (10%) |
| Some College | 3079 (26%) |
| Bachelor's Degree | 3015 (25%) |
| Post Graduate Degree | 4043 (34%) |
| Not reported | 14 (0.1%) |
| Parental Marital Status | |
| Married Families | 7990 (67%) |
| Not Married Families | 3790 (32%) |
| Not reported | 96 (1%) |
| Twin/Singleton Status | |
| Singleton | 7898 (67%) |
| Siblings | 1810 (15%) |
| Twin | 2138 (18%) |
| Triplet | 30 (0.3%) |
| Parental History of Alcohol Problems1 | |
| No Parent | 9696 (82%) |
| ≥1 Parent | 1732 (15%) |
| Not reported | 448 (4%) |
| Parental History of Drug Problems1 | |
| No Parent | 10166 (86%) |
| ≥1 Parent | 1271 (11%) |
| Not reported | 439 (4%) |
Notes:1 from FHAM-S; CBCL= Child Behavior Checklist. Parent sociodemographic variables include either parent or guardian.
3.2. “Heard Of” descriptives
By Y2, most youth endorsed hearing of alcohol (99.5%), nicotine (99.0%), cannabis (91.67%), prescription or over-the-counter drug misuse (70.8%), and inhalants (67.2%). Fewer youth heard of other drugs (Supplementary Table 3). At Y3, the study discontinued asking youth if they heard of substances.
3.3. Low-level substance use “experimentation”
The most commonly “experimented” (i.e., low-level) substance used across visits was alcohol sipping (Y3: 16.2% past-year, 36.9% lifetime) (Tables 2 and 3). Puffing nicotine products was the second most common (Y3: 2.8% past-year). Lastly, puffing or trying cannabis products remained uncommon from Y0-Y3 (Y3: 0.9% past-year) (Table 2). There were no sex differences in experimentation for each substance by Y3.
Table 2.
Lifetime (Y0) or past-year (Y1–3) substance use patterns (includes all substances, alcohol, nicotine, and cannabis).
| All | Males | Females | χ2 | p-value | |
|---|---|---|---|---|---|
| “Experimentation” | |||||
| Sipped Alcohol | |||||
| Y0 | 22.51% | 24.24% | 20.62% | 22.12 | <.001 |
| Y1 | 12.66% | 14.48% | 10.67% | 36.39 | <.001 |
| Y2 | 12.62% | 13.96% | 11.14% | 18.4 | <.001 |
| Y3 | 16.22% | 16.17% | 16.28% | 0.01 | 0.937 |
| Puffed Nicotine | |||||
| Y0 | 0.68% | 0.89% | 0.46% | 7.46 | 0.006 |
| Y1 | 0.56% | 0.82% | 0.28% | 13.53 | <.001 |
| Y2 | 0.97% | 1.16% | 0.77% | 3.71 | 0.054 |
| Y3 | 2.78% | 2.88% | 2.67% | 0.18 | 0.672 |
| Puffed/Tasted Cannabis | |||||
| Y0 | <0.1% | <0.1% | 0% | 1.17 | 0.28 |
| Y1 | 0.11% | 0.15% | <0.1% | 1.65 | 0.199 |
| Y2 | 0.29% | 0.39% | 0.18% | 3.08 | 0.079 |
| Y3 | 0.93% | 0.91% | 0.95% | 0 | 0.983 |
| Substance Use “Initiation” (i.e., reported ≥1 standard drink, > puff/taste | |||||
| cannabis or nicotine or any other substance use) | |||||
| All Substances | |||||
| Y0 | 1.06% | 1.34% | 0.76% | 9.03 | 0.003 |
| Y1 | 1.55% | 2.03% | 1.03% | 17.67 | <.001 |
| Y2 | 1.98% | 2.24% | 1.69% | 3.7 | 0.054 |
| Y3 | 4.06% | 4.40% | 3.69% | 1.84 | 0.175 |
| Alcohol Use | |||||
| Y0 | 0.38% | 0.48% | 0.26% | 0.87 | 0.352 |
| Y1 | 0.33% | 0.43% | 0.22% | 2.88 | 0.09 |
| Y2 | 0.65% | 0.66% | 0.64% | 0 | 1 |
| Y3 | 1.89% | 1.94% | 1.83% | 0.06 | 0.812 |
| Nicotine Use | |||||
| Y0 | 0.59% | 0.66% | 0.51% | 0.09 | 0.764 |
| Y1 | 0.39% | 0.54% | 0.22% | 6.58 | 0.01 |
| Y2 | 0.71% | 0.70% | 0.73% | 0 | 0.955 |
| Y3 | 2.08% | 2.12% | 2.03% | 0.03 | 0.866 |
| Cannabis Use | |||||
| Y0 | 0.13% | 0.19% | <0.1% | 0 | 0.983 |
| Y1 | 0.45% | 0.63% | 0.26% | 7.62 | 0.006 |
| Y2 | 0.64% | 0.84% | 0.42% | 6.54 | 0.011 |
| Y3 | 1.10% | 1.15% | 1.05% | 0 | 0.983 |
| “Any” Use (i.e., reported “experimentation” OR “initiation”) | |||||
| All Substances | |||||
| Y0 | 23.13% | 25% | 21.09% | 25.24 | <.001 |
| Y1 | 13.90% | 16.13% | 11.45% | 50.77 | <.001 |
| Y2 | 14.02% | 15.54% | 12.35% | 21.55 | <.001 |
| Y3 | 18.43% | 18.90% | 17.90% | 0.97 | 0.325 |
| Alcohol | |||||
| Y0 | 22.58% | 24.31% | 20.70% | 21.78 | <.001 |
| Y1 | 12.78% | 14.63% | 10.74% | 37.62 | <.001 |
| Y2 | 12.77% | 14.07% | 11.35% | 17.03 | <.001 |
| Y3 | 16.69% | 16.81% | 16.55% | 0.06 | 0.809 |
| Nicotine | |||||
| Y0 | 1.12% | 1.32% | 0.90% | 4.47 | 0.035 |
| Y1 | 0.77% | 1.09% | 0.41% | 16.1 | <.001 |
| Y2 | 1.18% | 1.32% | 1.03% | 1.67 | 0.197 |
| Y3 | 2.96% | 3.09% | 2.81% | 0.35 | 0.555 |
| Cannabis | |||||
| Y0 | 0.14% | 0.23% | <0.1% | 5.06 | 0.024 |
| Y1 | 0.46% | 0.65% | 0.26% | 8.21 | 0.004 |
| Y2 | 0.70% | 0.94% | 0.44% | 8.34 | 0.004 |
| Y3 | 1.15% | 1.21% | 1.08% | 0.13 | 0.715 |
Notes: Chi-square and p-values represent comparisons between male and female use. Y0 represents lifetime use as of Baseline assessment, while Y1–3 represents past-year use at 1-, 2-, and 3-year follow-up assessments.
Table 3.
Onset of substance use across annual ABCD study follow-up visits.
| N (%) | Y01 | Y1 | Y2 | Y3 |
|---|---|---|---|---|
| “Any” Substance Use (i.e., reported “experimentation” OR “initiation”) | ||||
| Total Lifetime Onset | 23.13% | 28.54% | 32.43% | 39.67% |
| First onset identified at visit2 | 23.13% | 5.18% | 4.07% | 5.20% |
| Cumulative Onset | NA | 23.36% | 28.36% | 34.47% |
| No Onset at this visit | 76.87% | 71.46% | 67.57% | 60.33% |
| Substance Use “Initiation” (i.e., reported ≥1 standard drink, > puff/taste | ||||
| cannabis or nicotine or any other substance use) | ||||
| Total Lifetime Onset | 1.06% | 2.49% | 4.06% | 7.41% |
| First onset identified at visit2 | 1.06% | 1.42% | 1.59% | 3.17% |
| Cumulative Onset | NA | 1.08% | 2.47% | 4.24% |
| No Onset at this visit | 98.94% | 97.51% | 95.94% | 92.59% |
| First Alcohol Sip | ||||
| Total Lifetime Onset | 22.51% | 27.18% | 30.47% | 36.92% |
| First onset identified at visit2 | 22.51% | 4.45% | 3.48% | 4.24% |
| Cumulative Onset | NA | 22.73% | 26.99% | 32.68% |
| No Onset at this visit | 77.49% | 72.82% | 69.53% | 63.08% |
| First Alcohol Drink | ||||
| Total Lifetime Onset | 0.38% | 0.71% | 1.30% | 2.98% |
| First onset identified at visit2 | 0.38% | 0.32% | 0.60% | 1.49% |
| Cumulative Onset | NA | 0.39% | 0.70% | 1.49% |
| No Onset at this visit | 99.62% | 99.29% | 98.70% | 97.02% |
Notes: NA, not applicable.
Baseline visit (Y0) captured any use throughout lifetime with higher rates of alcohol sipping identified.
No previous report of use.
3.4. Substance use “initiation”
3.4.1. Substance use initiation
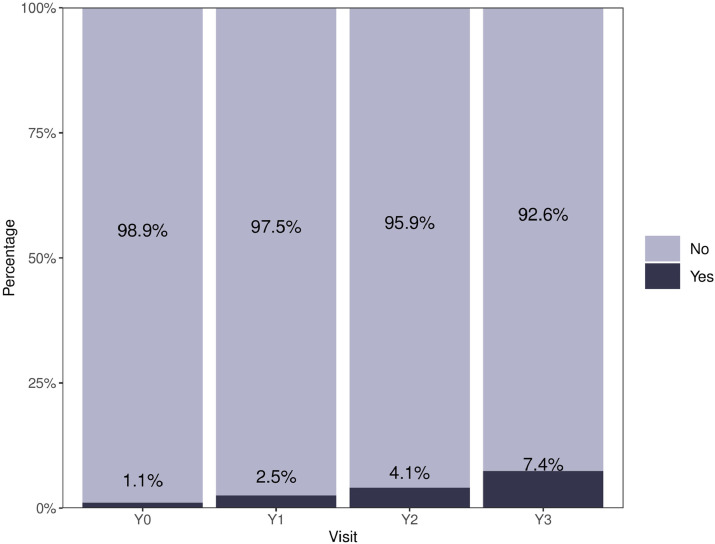
At Y0, 1.1% of youth reported lifetime use of a substance beyond sipping/experimenting (i.e., full standard alcohol drink, beyond singular puff or taste for nicotine, or cannabis, use of any other psychoactive substances). Rates of reported use at each follow-up are in Table 2, Supplementary Fig. 1b. At Y3, 7.4% of youth reported lifetime substance initiation (Fig. 1b), with 3.2% endorsed their first onset at Y3 (Table 3). More males reported SU initiation than females at Y0 and Y1, with no significant sex differences observed at Y2 or Y3.
Fig. 1b.
Cumulative lifetime rates of substance use “initiation” (i.e., reported ≥1 standard drink, > puff/taste cannabis or nicotine or any other substance use) for all substances. If a participant previously endorsed substance use “initiation”, their onset was carried forward regardless of subsequent reports of substance use “initiation”. Notably, Y3 contains half of the ABCD cohort and thus may not be generalizable to the full cohort.
3.4.2. Alcohol use
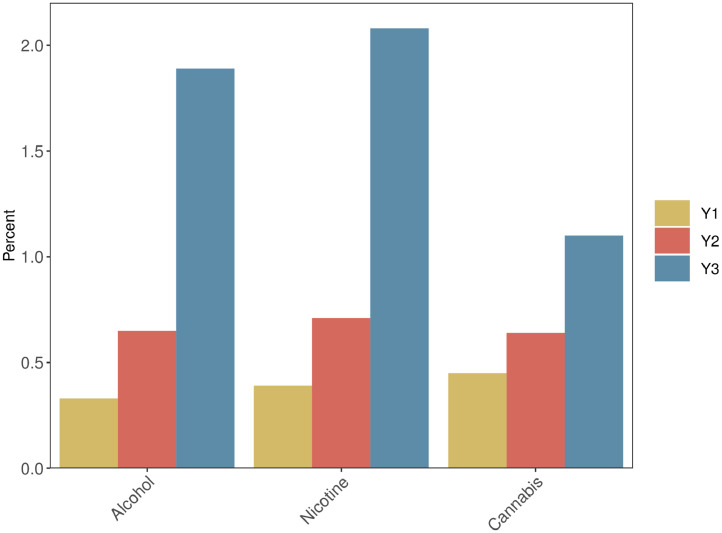
Full drinks of alcohol were the second most used substance (Y3 past-year: 1.9%) (Table 2 and Fig. 3), with lifetime rates increasing each year (1.3% by Y2 and 3.0% by Y3; Table 3). No sex differences were evident.
Fig. 3.
Proportion of participants reporting past-year substance use “initiation” (i.e., reported ≥1 standard drink, > puff/taste cannabis or nicotine) for each alcohol, nicotine or cannabis at Y1-Y3 follow-up visits. Y0 was removed due to capturing lifetime substance use “initiation” rather than past-year use. Notably, Y3 contains half of the ABCD cohort and thus may not be generalizable to the full cohort.
3.4.3. Nicotine use
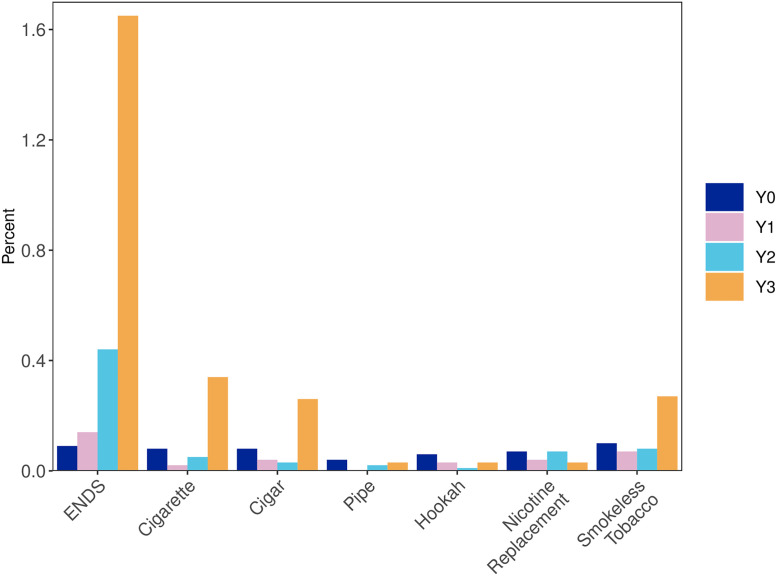
Nicotine was the most reported substance used (Y3 past-year: 2.1%, Table 2 and Fig. 3). ENDS remained the most common nicotine product (Y3 past-year: 1.7%; Table 4), and cigarettes were the second (Y3 past-year: 0.3%) (Fig. 4a). Males used more nicotine than females at Y1.
Table 4.
Lifetime (Y0) or past-year (Y1–3) nicotine and cannabis product-specific patterns according to full cohort and sex.
| N (%) | All | Males | Females |
|---|---|---|---|
| Nicotine Products | |||
| ENDS Use | |||
| Y0 | <0.1% | 0.13% | <0.1% |
| Y1 | 0.14% | 0.20% | <0.1% |
| Y2 | 0.44% | 0.44% | 0.44% |
| Y3 | 1.65% | 1.55% | 1.76% |
| Cigarette Use | |||
| Y0 | <0.1% | 0.10% | <0.1% |
| Y1 | <0.1% | <0.1% | 0% |
| Y2 | <0.1% | <0.1% | <0.1% |
| Y3 | 0.34% | 0.27% | 0.41% |
| Cigar Use | |||
| Y0 | <0.1% | 0.10% | <0.1% |
| Y1 | <0.1% | <0.1% | <0.1% |
| Y2 | <0.1% | <0.1% | <0.1% |
| Y3 | 0.26% | 0.27% | 0.24% |
| Pipe Use | |||
| Y0 | <0.1% | <0.1% | <0.1% |
| Y1 | 0% | 0% | 0% |
| Y2 | <0.1% | <0.1% | 0% |
| Y3 | <0.1% | 0% | <0.1% |
| Hookah Use | |||
| Y0 | <0.1% | <0.1% | <0.1% |
| Y1 | <0.1% | <0.1% | <0.1% |
| Y2 | <0.1% | <0.1% | 0% |
| Y3 | <0.1% | <0.1% | <0.1% |
| Nicotine Replacement | |||
| Y0 | <0.1% | <0.1% | <0.1% |
| Y1 | <0.1% | <0.1% | <0.1% |
| Y2 | <0.1% | <0.1% | <0.1% |
| Y3 | <0.1% | <0.1% | <0.1% |
| Smokeless Tobacco (Chew) | |||
| Y0 | 0.10% | 0.16% | <0.1% |
| Y1 | <0.1% | <0.1% | <0.1% |
| Y2 | <0.1% | 0.11% | <0.1% |
| Y3 | 0.27% | 0.39% | 0.14% |
| Vape Flower (No Nicotine) | |||
| Y0 | NA | NA | NA |
| Y1 | NA | NA | NA |
| Y2 | NA | NA | NA |
| Y3 | 0.63% | 0.97% | 0.24% |
| Cannabis Products | |||
| Smoked Flower Use | |||
| Y0 | <0.1% | <0.1% | 0% |
| Y1 | 0.17% | 0.24% | <0.1% |
| Y2 | 0.27% | 0.35% | 0.18% |
| Y3 | 0.75% | 0.73% | 0.78% |
| Edible Use | |||
| Y0 | <0.1% | <0.1% | 0% |
| Y1 | 0.20% | 0.26% | 0.13% |
| Y2 | 0.23% | 0.31% | 0.14% |
| Y3 | 0.51% | 0.49% | 0.54% |
| Infused Drink Use | |||
| Y0 | <0.1% | <0.1% | 0% |
| Y1 | <0.1% | 0.10% | <0.1% |
| Y2 | <0.1% | <0.1% | 0% |
| Y3 | <0.1% | <0.1% | <0.1% |
| Smoked Concentrate Use | |||
| Y0 | <0.1% | <0.1% | 0% |
| Y1 | <0.1% | 0.14% | <0.1% |
| Y2 | 0.12% | 0.15% | 0.10% |
| Y3 | 0.30% | 0.33% | 0.27% |
| Tincture Use | |||
| Y0 | <0.1% | <0.1% | 0% |
| Y1 | <0.1% | 0.12% | <0.1% |
| Y2 | <0.1% | <0.1% | 0% |
| Y3 | <0.1% | <0.1% | 0% |
| Blunt Use | |||
| Y0 | <0.1% | <0.1% | 0% |
| Y1 | <0.1% | <0.1% | 0% |
| Y2 | <0.1% | <0.1% | <0.1% |
| Y3 | 0.27% | 0.18% | 0.37% |
| Vaped Flower Use | |||
| Y0 | NA | NA | NA |
| Y1 | 0% | 0% | 0% |
| Y2 | <0.1% | <0.1% | 0% |
| Y3 | 0.19% | 0.21% | 0.17% |
| Vaped Oil Use | |||
| Y0 | NA | NA | NA |
| Y1 | 0% | 0% | 0% |
| Y2 | <0.1% | <0.1% | 0% |
| Y3 | 0.13% | 0.18% | <0.1% |
| CBD (Non-Medical) Use | |||
| Y0 | NA | NA | NA |
| Y1 | NA | NA | NA |
| Y2 | 0.18% | 0.19% | 0.18% |
| Y3 | 0.16% | 0.18% | 0.14% |
Notes: ENDS = electronic nicotine delivery system, CBD = cannabidiol, NA = Not assessed. Rates reflect youth who reported use beyond experimental use (i.e., beyond “taste or puff.”) Chi-square and p-values represent comparisons between male and female use. Y0 represents lifetime use as of Baseline assessment, while Y1–3 represents past-year use at Year 1, Year 2, and Year 3 follow-up assessments.
Fig. 4a.
Proportion of participants reporting > puff/taste of specific nicotine products within study visits. Notably, Y3 contains half of the ABCD cohort and thus may not be generalizable to the full cohort, and Y0 is indicative of lifetime use rather than past-year use.
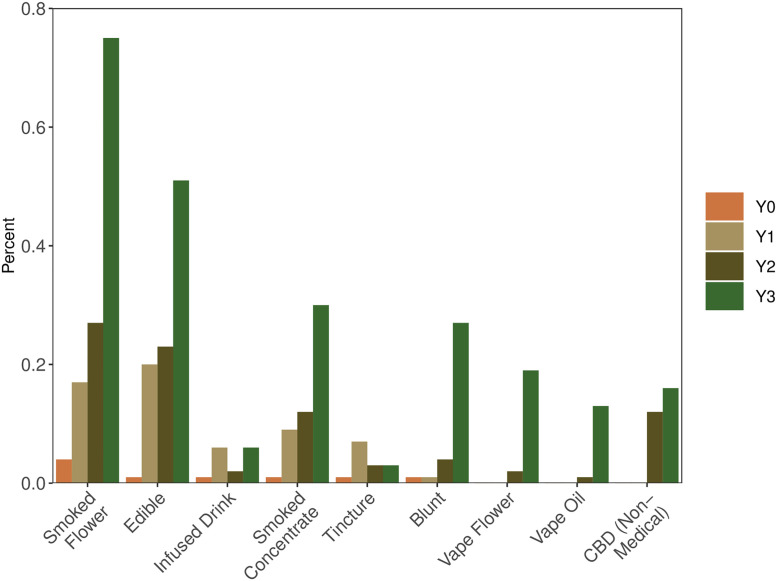
3.4.4. Cannabis use
At Y3, 1.1% reported past-year cannabis use (Table 2); smoked cannabis flower was the most common route of administration (Y3: 0.8%), see Table 4 and Figs. 3 and 4b. Males used more cannabis than females at Y1 and Y2.
3.4.5. Other substance use
Reports of other SU remains low through Y3 (1.2%) (Supplementary Table 2). Males reported more “other” SU than females at Y3 only. No youth reported using a “fake” drug.
3.5. “Any” substance use
3.5.1. Any substance use
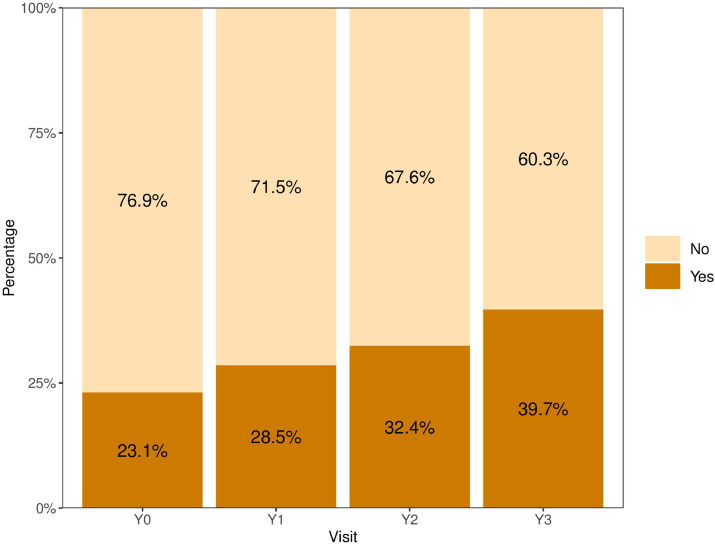
At Y0, 23.1% of youth reported any substance use; follow-up rates were Y1: 13.9%, Y2: 14.0%, Y3: 18.4% (Table 2, Supplementary Fig. 1a). Cumulative: By Y3, 39.7% of the cohort reported “experimentation” with at least one substance within their lifetime (Table 3, Fig. 1a). More males reported more SU than females at Y0, Y1, and Y2, but not Y3.
Fig. 1a.
Cumulative lifetime rates of “any” substance use (i.e., reported “experimentation” OR “initiation”) for all substances. If a participant previously endorsed “any” substance use, their onset was carried forward regardless of subsequent reports of “any” substance use. Notably, Y3 contains half of the ABCD cohort and thus may not be generalizable to the full cohort.
3.5.2. Alcohol use
By Y3, 16.7% of youth reported any past-year alcohol use. Males used more alcohol than females at Y0, Y1, and Y2.
3.5.3. Nicotine use
By Y3, 3.0% reported any past-year nicotine use. Males used more nicotine than females at Y0 and Y1.
3.5.4. Cannabis use
1.2% of youth reported any cannabis use by Y3. Males used more cannabis than females at Y0, Y1, and Y2.
Fig. 4b.
Proportion of participants reporting > puff/taste of specific cannabis product within study visits. Notably, Y3 contains half of the ABCD cohort and thus may not be generalizable to the full cohort and Y0 is indicative of lifetime use rather than past-year use.
3.6. Multivariable predictors of substance use experimentation and substance use initiation
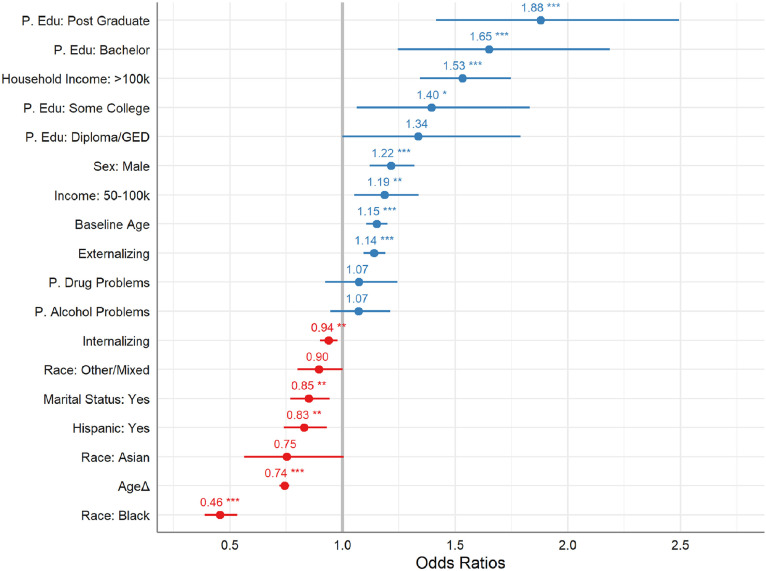
3.6.1. “Any” substance use (i.e., “experimentation” or “initiation”) GEE (Fig. 2a)
Fig. 2a.
Odds ratio (OR) of “any” substance use (i.e., “experimentation” or “initiation”) GEE output. Blue represents positive ORs and red represents negative ORs. OR of the predictor is presented above 95% confidence interval bracket with asterisk denoting statistical significance. Notably, GEEs only analyzed Y0-Y2 data. “P.” = parental, “Edu” = education.
Significant sociodemographic predictors of higher odds of any SU included: age at Y0 [Wχ2=48.4, OR=1.15 (CI: 1.11–1.20), p < 0.001], males [Wχ2=30.9, OR=1.22 (CI: 1.12–1.32), p < 0.001], White youth [Wχ2=183, p < 0.001, vs. Black youth, OR=0.46 (CI: 0.39–0.53)], non-Hispanic youth [Wχ2=10.3, p = 0.001 vs. Hispanic youth, OR=0.83 (CI: 0.74–0.93)], higher household income [Wχ2=85.2, p < 0.001; <50k vs 50–100k, OR=1.19 (CI: 1.05–1.34); vs >100k, OR=1.53 (CI: 1.34–1.75)], more parental education [Wχ2=25.4, p < 0.001; <HS vs some College, OR=1.4 (CI: 1.06–1.83); vs Bachelor, OR=1.65 (CI: 1.24–2.19); vs post-graduate degree, OR=1.88 (CI: 1.42–2.49)], and non-married family status [Wχ2=9.6, OR=0.85 (CI: 0.77–0.94), p = 0.002]. Lower odds of any SU were significantly related to ageΔ (i.e., time) [Wχ2=362.6, OR=0.74 (CI: 0.72–0.76), p < 0.001]; higher rates of any SU are evident at Y0, likely due to lifetime measurement, particularly of sipping alcohol (see Table 2). Parental history of alcohol [Wχ2=1.2, p = 0.28] or drug [Wχ2=0.8, p = 0.36] problems were not significantly associated with odds of any SU. Higher internalizing scores [Wχ2=8.6, OR=0.94 (CI: 0.90–0.98), p = 0.003] were predictive of lower SU odds while higher externalizing scores [Wχ2=37.6, OR=1.14 (CI: 1.09–1.19), p < 0.001] were predictive of higher SU odds. See Supplementary Table 1a for model output.
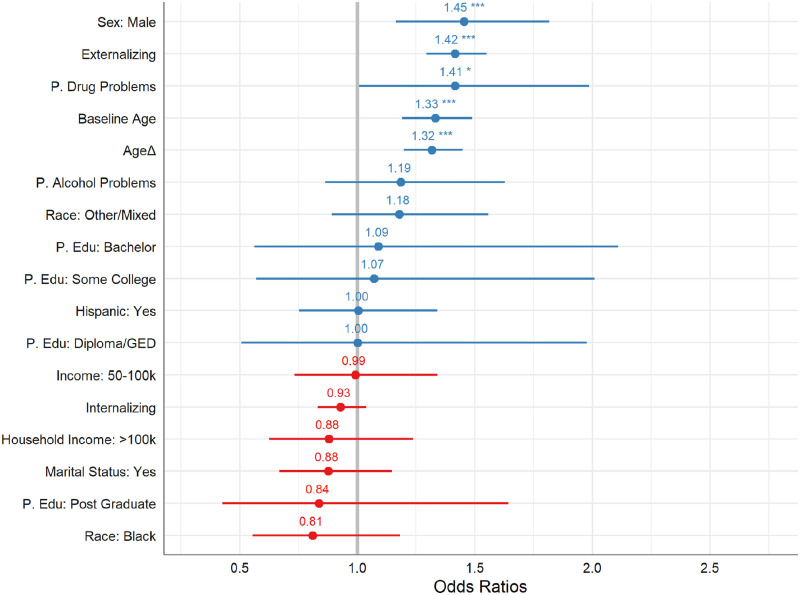
3.6.2. Substance Use “Initiation” GEE (Fig. 2b)
Fig. 2b.
Odds ratio (OR) of substance use “initiation” GEE output. Blue represents positive ORs and red represents negative ORs. OR of the predictor is presented above 95% confidence interval bracket with asterisk denoting statistical significance. Notably, GEEs only analyzed Y0-Y2 data. “P.” = parental, “Edu” = education.
Significant sociodemographic predictors of higher odds of SU “initiation” included: higher age at Y0 [Wχ2=25.1, OR=1.33 (CI: 1.19–1.49), p < 0.001], ageΔ (i.e., time) [Wχ2=32.4, OR=1.32 (CI: 1.20–1.45)], males [Wχ2=10.9, OR=1.45 (CI: 1.16–1.82), p = 0.001], and lower household income [Wχ2=15.1, p < 0.001]. Parental history of drug problems [Wχ2=4.0, OR=1.4 (CI: 1.01–1.99), p = 0.045] and higher externalizing scores [Wχ2=57.7, OR=1.42 (CI: 1.29–1.55), p < 0.001] were predictive of higher SU “initiation” odds. See Supplementary Table 1b for model output.
4. Discussion
Given a primary aim of the ABCD Study is to examine the influence of substance use onset on biological, psychosocial, psychiatric, and neurodevelopment outcomes, it is important to document and describe substance use as this cohort ages. In the present analyses, we reported patterns that emerged from when these youth were 9-10 (Baseline) to 12-13 (Year 3 Follow-Up). Past-year experimental substance use (sipping, puffing/tasting) was stable at each time point for alcohol and cannabis, with increases in nicotine puffing over time. By the third follow-up visit, nearly 40% of the cohort had at least experimented with a substance in their lifetime, while past-year rates for any use were 18% (17% alcohol, 3% nicotine, 1% cannabis). Despite hypothesized differences, prevalence rates by Year 3 follow-up did not generally vary by sex.
As expected, reported substance use is increasing as ABCD participants out of early adolescence (i.e., ages 12-13). While only 1% of youth had ever used a full unit of any substance at Baseline, 7% had by Year 3. An increase in the rate of initiation of use beyond “experimentation” was also observed at each annual visit (Y1=1.4%, Y2=1.6%, Y3=3.2%). Alcohol remains the most used substance overall, with 37% of youth reported sipping alcohol and 3% reported having their first full alcohol drink by Y3. While recent MTF findings suggest 21.7% of 8th graders have used any alcohol (defined as more than just a sip) in their lifetime (NIDA, 2021); variance in rates may be due to the present study's delineation of alcohol sips v. full standard drink, with MTF rates falling between the ABCD reporting levels, and the fact that many ABCD participants are still below the minimum age of MTF participants. As preclinical and clinical research shows risky alcohol use during adolescence is associated with a range of neural and cognitive deficits (Lees et al., 2020), continued documentation and investigation into adolescent alcohol use will be important for informing future prevention and intervention efforts.
Also consistent with Baseline ABCD findings, nicotine remains the next most reported substance used in the ABCD Study cohort. Prevalence increased from 1.1% of youth reported using a nicotine product in their lifetime at Baseline to 3% using nicotine within the past year at Year 3. Vaping nicotine products remained the most popular mode of use across time-points. This is notable as evidence suggests nicotine can be particularly neurotoxic in the developing brain (Yuan et al., 2015) and that early vaping (the most common method of nicotine use in this sample) is correlated with later combustible cigarette and other substance use (McCabe et al., 2018; Staff et al., 2020; Yoong et al., 2021). Notably, these rates were lower than those reported in the most recent MTF study, which reported 12.1% of 8th graders used ENDS in 2021 (Johnston et al., 2022). This is likely due to different recruitment strategies and methodologies that are employed; MTF uses an anonymous, national school-based survey, whereas the ABCD Study recruited in school communities and uses an interviewer-administered TLFB calendar approach combined with numerous other surveys assessing mental and physical health, culture and environment, and includes bioassay collection and MRI brain scans (Garavan et al., 2018; Jernigan et al., 2018; Volkow et al., 2018). Further, during the years reported here, the ABCD Study cohort is still mostly younger than the MTF Study participants; thus, prevalence rates between the two may become more comparable over time. Additionally, timing of the data collection during the pandemic may influence differential cohort SU rates, as pandemic surveys have generally reported lower SU rates in teens (NIDA, 2021). Rates of use reported and timing of the ABCD data collection were also impacted by the pandemic. During the COVID-19 pandemic (spring/summer 2020), all ABCD Study participants were invited to complete online surveys every 4–11 weeks and report past-month substance use (Pelham et al., 2021). These surveys found that past-month alcohol use decreased in the early pandemic months (May-June 2020), while nicotine use increased during this period, with the cumulative nicotine use rate reaching 3.6%. It is challenging to compare findings, as fewer participants opted in to the COVID-19 surveys and non-random factors and methodological differences may explain differences in prevalence rates. Future ABCD Study analyses will monitor the potential influence of data collection methodologies and pandemic-related effects on substance use reporting.
Several risk factors were associated with early substance use in the ABCD Study cohort. Experimentation and initiating any substance use were associated with multiple sociodemographic variables and externalizing symptoms. Analyses revealed relationships between being older at Baseline, male at birth, having a parental history of drug use problems, and parental report of increased externalizing symptoms increasing odds of a “full use” (one full dose of standard drink, nicotine/cannabis use beyond puffing or other occasions of substance use). These results are consistent with previously reported ABCD Cohort Baseline findings of increased early alcohol sipping significantly related to being older, White, male, and parental reports of higher externalizing symptoms (Lisdahl et al., 2021), suggesting consistency of very early risk factors for substance use initiation in this cohort over time. The largest increase in odds of SU initiation was in males (OR=1.45) and externalizing symptoms (OR=1.42), followed by youth with parent drug use problems (OR=1.4). Results are thus consistent with prior research (e.g., externalizing symptoms have been linked to substance use onset; Cox et al., 2021; Edwards et al., 2016; Loeber et al., 2018; Ning et al., 2020). Notably, there were fewer sex differences as the ABCD Study participants aged, which is consistent with the MTF survey finding fewer sex differences in 8th graders (Miech et al., 2020). Here, we found parental history of drug problems, but not alcohol problems, predicted increased odds of substance use. Mixed results are noted from prior analyses in the ABCD Study, suggesting parental history of alcohol or drug problems were not associated with curiosity about substance use at Baseline (Martz et al., 2022), but parental history of alcohol problems contributed to a latent factor which was significantly associated with alcohol curiosity at Year 1 (Wade et al., 2021) and was previously linked with early alcohol sipping (Lisdahl et al., 2021). Overall, these findings once again suggest that sociodemographic factors, externalizing symptoms, and parental history of substance use problems need to be considered when others are utilizing the ABCD data to examine predictors of adolescent substance use trajectories.
Results should be considered within the context of their limitations. As noted, estimates of self-reported substance use prevalence varies (Pelham et al., 2021) and hair toxicology data collected on a subset of youth enrolled in the ABCD Study indicate potential underreporting of substance use, especially in high-risk youth (Wade et al., 2022). In addition, while the ABCD Study withdrawal rate is minimal (1.1%), missed study visits may contribute to the relatively lower prevalence of SU reported here than in other national studies. Though beyond the scope of this paper to fully analyze factors influencing missing visits, the ABCD Retention Workgroup found race, parental education, and parental employment predicted missed visits (Feldstein Ewing et al., 2022). GEEs were limited to Baseline through Year 2 data (NDA 4.0) as only half of Year 3 data is released; continued monitoring of risk factors for substance use onset is needed. The current analysis aimed to report the pattern of substance use in the initial waves of the ABCD Study and examine basic sociodemographic, parental history of substance use problems, and internalizing/externalizing symptoms to inform the scientific community. Numerous other factors were not examined and will be considered by multiple investigators in future analyses [e.g., culture and environmental factors (Zucker et al., 2018), more detailed psychopathology (Barch et al., 2018), physical health (Palmer et al., 2021), SU attitudes (Lisdahl et al., 2018), biological functioning (Uban et al., 2018), genetics (Iacono et al., 2018), and neurocognitive (Casey et al., 2018; Luciana et al., 2018) factors]. The COVID-19 pandemic impacted data collection in that almost all data was collected remotely or in hybrid-fashion for an extended period of time. Given there was limited in-person data collection after Mach 2020 in this data release, it is not possible here to investigate remote v. in-person reporting differences in SU reporting, though this will be important to consider in future investigations.
5. Conclusions
Early substance initiation is associated with quicker transition to, and increased prevalence of, substance use disorders (Volkow et al., 2021). Thus, monitoring early substance use onset patterns and identifying associated risk factors are key to preventing long-term consequences of substance use onset (Tapert and Eberson-Shumate, 2022). The ABCD Study cohort has reported increased use of substances as they transition to teenage years (ages 12-13), though rates are generally lower than seen in other national samples (i.e., MTF). Across Baseline and through Year 3 follow-up, alcohol use is the most used substance, followed by nicotine use (specifically, ENDS) in the ABCD Study cohort. Externalizing symptoms and parental history of drug problems predicted increased odds of substance experimentation and initiation, while sex differences in prevalence rates were less apparent at later follow-up points. Continuing to follow this large, diverse cohort through adolescence will provide a unique and extraordinary opportunity to investigate these and other multifaceted risk and resiliency factors associated with SU onset and consequences in teens.
CRediT authorship contribution statement
Ryan M. Sullivan: Conceptualization, Data curation, Formal analysis, Validation, Visualization, Writing – original draft, Writing – review & editing. Natasha E. Wade: Conceptualization, Data curation, Formal analysis, Validation, Visualization, Writing – original draft, Writing – review & editing. Alexander L. Wallace: Data curation, Formal analysis, Validation, Visualization, Writing – original draft, Writing – review & editing. Susan F. Tapert: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Software, Writing – review & editing. William E. Pelham: Project administration, Validation, Writing – review & editing. Sandra A. Brown: Funding acquisition, Investigation, Methodology, Project administration, Writing – review & editing. Christine C Cloak: Investigation, Project administration, Supervision, Writing – review & editing. Sarah W. Feldstein Ewing: Project administration, Resources, Supervision, Visualization, Writing – review & editing. Pamela A.F. Madden: Funding acquisition, Investigation, Project administration, Supervision, Writing – review & editing. Meghan E. Martz: Writing – review & editing. J. Megan Ross: Writing – review & editing. Christine M. Kaiver: Writing – original draft, Writing – review & editing. Hailey G. Wirtz: Writing – original draft, Writing – review & editing. Mary M. Heitzeg: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing. Krista M. Lisdahl: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing.
Declaration of Competing Interest
The authors have no conflict of interest or competing interests to declare.
Acknowledgments
Data used in the preparation of this article were obtained from the Adolescent Brain Cognitive DevelopmentSM (ABCD) Study (https://abcdstudy.org), held in the NIMH Data Archive (NDA). This is a multisite, longitudinal study designed to recruit more than 10,000 children age 9-10 and follow them over 10 years into early adulthood. The ABCD Study® is supported by the National Institutes of Health and additional federal partners under award numbers U01DA041048, U01DA050989, U01DA051016, U01DA041022, U01DA051018, U01DA051037, U01DA050987, U01DA041174, U01DA041106, U01DA041117, U01DA041028, U01DA041134, U01DA050988, U01DA051039, U01DA041156, U01DA041025, U01DA041120, U01DA051038, U01DA041148, U01DA041093, U01DA041089, U24DA041123, U24DA041147. A full list of supporters is available at https://abcdstudy.org/federal-partners.html. A listing of participating sites and a complete listing of the study investigators can be found at https://abcdstudy.org/consortium_members/. ABCD consortium investigators designed and implemented the study and/or provided data but did not necessarily participate in analysis or writing of this report. All other Federal representatives contributed to the interpretation of the data and participated in the preparation, review and approval of the manuscript, consistent with their roles on the ABCD Federal Partners Group. The views and opinions expressed in this manuscript are those of the authors only and do not necessarily represent the views, official policy or position of ABCD consortium investigators, the U.S. Department of Health and Human Services or any of its affiliated institutions or agencies. The ABCD data repository grows and changes over time. The ABCD data used in this report came from the ABCD Data Release 4.0 (DOI: 10.15154/1523041, October 2021). This work was also supported by F31 DA054761 (PI: Sullivan), K08 DA050779 (PI: Wade), DA055935 and AA030197 (PI: Pelham).
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.dadr.2022.100120.
Appendix. Supplementary materials
References
- Achenbach T.M. University of Vermont Research Center for Children; Burlington, VT: 2009. The Achenbach System of Empirically Based Assessemnt (ASEBA): Development, Findings, Theory, and Applications. Y., & Families (Ed.) [Google Scholar]
- Auchter A.M., Hernandez Mejia M., Heyser C.J., Shilling P.D., Jernigan T.L., Brown S.A., Tapert S.F., Dowling G.J. A description of the ABCD organizational structure and communication framework. Dev. Cogn. Neurosci. 2018;32:8–15. doi: 10.1016/j.dcn.2018.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barch D.M., Albaugh M.D., Avenevoli S., Chang L., Clark D.B., Glantz M.D., Hudziak J.J., Jernigan T.L., Tapert S.F., Yurgelun-Todd D., Alia-Klein N., Potter A.S., Paulus M.P., Prouty D., Zucker R.A., Sher K.J. Demographic, physical and mental health assessments in the adolescent brain and cognitive development study: Rationale and description. Dev. Cogn. Neurosci. 2018;32:55–66. doi: 10.1016/j.dcn.2017.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey B.J., Cannonier T., Conley M.I., Cohen A.O., Barch D.M., Heitzeg M.M., Soules M.E., Teslovich T., Dellarco D.V., Garavan H., Orr C.A., Wager T.D., Banich M.T., Speer N.K., Sutherland M.T., Riedel M.C., Dick A.S., Bjork J.M., Thomas K.M., Chaarani B., Mejia M.H., Hagler D.J., Jr., Daniela Cornejo M., Sicat C.S., Harms M.P., Dosenbach N.U.F., Rosenberg M., Earl E., Bartsch H., Watts R., Polimeni J.R., Kuperman J.M., Fair D.A., Dale A.M., Workgroup A.I.A. The Adolescent Brain Cognitive Development (ABCD) study: Imaging acquisition across 21 sites. Dev. Cogn. Neurosci. 2018;32:43–54. doi: 10.1016/j.dcn.2018.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chassin L., Pitts S.C., Prost J. Binge drinking trajectories from adolescence to emerging adulthood in a high-risk sample: Predictors and substance abuse outcomes. J. Consult. Clin. Psychol. 2002;70(1):67–78. [PubMed] [Google Scholar]
- Cox S.M.L., Castellanos-Ryan N., Parent S., Benkelfat C., Vitaro F., Pihl R.O., Boivin M., Tremblay R.E., Leyton M., Seguin J.R. Externalizing risk pathways for adolescent substance use and its developmental onset: a canadian birth cohort study: trajectoires de comportements exteriorises et le risque pour l'initiation et l'usage de substances des adolescents: une etude de cohorte de naissance canadienne. Can. J. Psychiatry. 2021;66(10):887–896. doi: 10.1177/0706743720982429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards A.C., Gardner C.O., Hickman M., Kendler K.S. A prospective longitudinal model predicting early adult alcohol problems: evidence for a robust externalizing pathway. Psychol. Med. 2016;46(5):957–968. doi: 10.1017/S0033291715002457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldstein Ewing S.W., Dash G.F., Thompson W.K., Reuter C., Diaz V.G., Anokhin A., Chang L., Cottler L.B., Dowling G.J., LeBlanc K., Zucker R.A., Tapert S.F., Brown S.A., Garavan H. Measuring retention within the adolescent brain cognitive development (ABCD)(SM) study. Dev. Cogn. Neurosci. 2022;54 doi: 10.1016/j.dcn.2022.101081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garavan H., Bartsch H., Conway K., Decastro A., Goldstein R.Z., Heeringa S., Jernigan T., Potter A., Thompson W., Zahs D. Recruiting the ABCD sample: Design considerations and procedures. Dev. Cogn. Neurosci. 2018;32:16–22. doi: 10.1016/j.dcn.2018.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelman A. Scaling regression inputs by dividing by two standard deviations. Stat. Med. 2008;27(15):2865–2873. doi: 10.1002/sim.3107. [DOI] [PubMed] [Google Scholar]
- Grant B.F., Dawson D.A. Age at onset of alcohol use and its association with DSM-IV alcohol abuse and dependence: results from the national longitudinal alcohol epidemiologic survey. J. Subst. Abuse Treat. 1997;9:103–110. doi: 10.1016/s0899-3289(97)90009-2. [DOI] [PubMed] [Google Scholar]
- Halekoh U., Højsgaard S., Yan J. The R package geepack for generalized estimating equations. J. Stat. Softw. 2006;15(2):1–11. [Google Scholar]
- Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap)-a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry K.L. Fathers'alcohol and cannabis use disorder and early onset of drug use by their children. J. Stud. Alcohol Drugs. 2017;78:458–462. doi: 10.15288/jsad.2017.78.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iacono W.G., Heath A.C., Hewitt J.K., Neale M.C., Banich M.T., Luciana M.M., Madden P.A., Barch D.M., Bjork J.M. The utility of twins in developmental cognitive neuroscience research: how twins strengthen the ABCD research design. Dev. Cogn. Neurosci. 2018;32:30–42. doi: 10.1016/j.dcn.2017.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson C., Ennett S.T., Dickinson D.M., Bowling J.M. Attributes that differentiate children who sip alcohol from abstinent peers. J Youth Adolesc. 2013;42(11):1687–1695. doi: 10.1007/s10964-012-9870-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson K.M., Barnett N.P., Colby S.M., Rogers M.L. The prospective association between sipping alcohol by the sixth grade and later substance use. J. Stud. Alcohol Drugs. 2015;76:212–221. doi: 10.15288/jsad.2015.76.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson K.M., Colby S.M., Barnett N.P., Abar C.C. Prevalence and correlates of sipping alcohol in a prospective middle school sample. Psychol. Addict. Behav. 2015;29(3):766–778. doi: 10.1037/adb0000072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jernigan T.L., Brown S.A., Coordinators A.C. Introduction. Dev. Cogn. Neurosci. 2018;32:1–3. doi: 10.1016/j.dcn.2018.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston L.D., Miech R.A., O'Malley P.M., Bachman J.G., Schulenberg J.E., Patrick M.E. Institute for Social Research, University of Michigan; Ann Arbor: 2021. Monitoring the Future National Survey Results on Drug Use 1975-2020: Overview, Key Findings on Adolescent Drug Use. [Google Scholar]
- Johnston L.D., Miech R.A., O'Malley P.M., Bachman J.G., Schulenberg J.E., Patrick M.E. Institute for Social Research; Ann Arbor: 2022. Monitoring the Future national Survey Results on Drug Use 1975-2021: Overview, Key Findings on Adolescent Drug Use. U.o.M. (Ed.) [Google Scholar]
- Lees B., Aguinaldo L., Squeglia L.M., Infante M.A., Wade N.E., Hernandez Mejia M., Jacobus J. Parental family history of alcohol use disorder and neural correlates of response inhibition in Children From the Adolescent Brain Cognitive Development (ABCD) study. Alcohol Clin. Exp. Res. 2020;44(6):1234–1244. doi: 10.1111/acer.14343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lisdahl K.M., Sher K.J., Conway K.P., Gonzalez R., Feldstein Ewing S.W., Nixon S.J., Tapert S., Bartsch H., Goldstein R.Z., Heitzeg M. Adolescent brain cognitive development (ABCD) study: overview of substance use assessment methods. Dev. Cogn. Neurosci. 2018;32:80–96. doi: 10.1016/j.dcn.2018.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lisdahl K.M., Tapert S., Sher K.J., Gonzalez R., Nixon S.J., Feldstein Ewing S.W., Conway K.P., Wallace A., Sullivan R., Hatcher K., Kaiver C., Thompson W., Reuter C., Bartsch H., Wade N.E., Jacobus J., Albaugh M.D., Allgaier N., Anokhin A.P., Bagot K., Baker F.C., Banich M.T., Barch D.M., Baskin-Sommers A., Breslin F.J., Brown S.A., Calhoun V., Casey B.J., Chaarani B., Chang L., Clark D.B., Cloak C., Constable R.T., Cottler L.B., Dagher R.K., Dapretto M., Dick A., Do E.K., Dosenbach N.U.F., Dowling G.J., Fair D.A., Florsheim P., Foxe J.J., Freedman E.G., Friedman N.P., Garavan H.P., Gee D.G., Glantz M.D., Glaser P., Gonzalez M.R., Gray K.M., Grant S., Haist F., Hawes S., Heeringa S.G., Hermosillo R., Herting M.M., Hettema J.M., Hewitt J.K., Heyser C., Hoffman E.A., Howlett K.D., Huber R.S., Huestis M.A., Hyde L.W., Iacono W.G., Isaiah A., Ivanova M.Y., James R.S., Jernigan T.L., Karcher N.R., Kuperman J.M., Laird A.R., Larson C.L., LeBlanc K.H., Lopez M.F., Luciana M., Luna B., Maes H.H., Marshall A.T., Mason M.J., McGlade E., Morris A.S., Mulford C., Nagel B.J., Neigh G., Palmer C.E., Paulus M.P., Pecheva D., Prouty D., Potter A., Puttler L.I., Rajapakse N., Ross J.M., Sanchez M., Schirda C., Schulenberg J., Sheth C., Shilling P.D., Sowell E.R., Speer N., Squeglia L., Sripada C., Steinberg J., Sutherland M.T., Tomko R., Uban K., Vrieze S., Weiss S.R.B., Wing D., Yurgelun-Todd D.A., Zucker R.A., Heitzeg M.M., Consortium A. Substance use patterns in 9-10 year olds: Baseline findings from the adolescent brain cognitive development (ABCD) study. Drug Alcohol Depend. 2021;227 doi: 10.1016/j.drugalcdep.2021.108946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeber R., Clark D.B., Ahonen L., FitzGerald D., Trucco E.M., Zucker R.A. A brief validated screen to identify boys and girls at risk for early marijuana use. Dev. Cogn. Neurosci. 2018;32:23–29. doi: 10.1016/j.dcn.2018.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luciana M., Bjork J.M., Nagel B.J., Barch D.M., Gonzalez R., Nixon S.J., Banich M.T. Adolescent neurocognitive development and impacts of substance use: Overview of the adolescent brain cognitive development (ABCD) baseline neurocognition battery. Dev. Cogn. Neurosci. 2018;32:67–79. doi: 10.1016/j.dcn.2018.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martz M.E., Heitzeg M.M., Lisdahl K.M., Cloak C.C., Ewing S.W.F., Gonzalez R., Haist F., LeBlanc K.H., Madden P.A., Ross J.M., Sher K.J., Tapert S.F., Thompson W.K., Wade N.E. Individual-, peer-, and parent-level substance use-related factors among 9- and 10-year-olds from the ABCD Study: prevalence rates and sociodemographic differences. Drug Alcohol Depend. Rep. 2022;3 doi: 10.1016/j.dadr.2022.100037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe S.E., West B.T., McCabe V.V. Associations between early onset of E-cigarette use and cigarette smoking and other substance use among US adolescents: a national study. Nicotine Tob. Res. 2018;20(8):923–930. doi: 10.1093/ntr/ntx231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miech R.A., Johnston L.D., O'Malley P.M., Bachman J.G., Schulenberg J.E., Patrick M.E. Secondary School Students. Institute for Social Research, The University of Michigan; Ann Arbor: 2020. Monitoring the Future National Survey Results on Drug Use, 1975-2019: Volume I. [Google Scholar]
- NIDA . 2021. Percentage of Adolescents Reporting Drug Use Decreased Significantly in 2021 as the COVID-19 Pandemic Endured. [Google Scholar]
- Ning K., Gondek D., Patalay P., Ploubidis G.B. The association between early life mental health and alcohol use behaviours in adulthood: a systematic review. PLoS One. 2020;15(2) doi: 10.1371/journal.pone.0228667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer C.E., Sheth C., Marshall A.T., Adise S., Baker F.C., Chang L., Clark D.B., Coronado C., Dagher R.K., Diaz V., Dowling G.J., Gonzalez M.R., Haist F., Herting M.M., Huber R.S., Jernigan T.L., LeBlanc K., Lee K., Lisdahl K.M., Neigh G., Patterson M.W., Renshaw P., Rhee K.E., Tapert S., Thompson W.K., Uban K., Sowell E.R., Yurgelun-Todd D. A Comprehensive overview of the physical health of the adolescent brain Cognitive Development Study Cohort at Baseline. Front. Pediatr. 2021;9 doi: 10.3389/fped.2021.734184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelham W.E., 3rd, Tapert S.F., Gonzalez M.R., McCabe C.J., Lisdahl K.M., Alzueta E., Baker F.C., Breslin F.J., Dick A.S., Dowling G.J., Guillaume M., Hoffman E.A., Marshall A.T., McCandliss B.D., Sheth C.S., Sowell E.R., Thompson W.K., Van Rinsveld A.M., Wade N.E., Brown S.A. Early adolescent substance use before and during the COVID-19 pandemic: a longitudinal survey in the ABCD Study cohort. J. Adolesc. Health. 2021;69(3):390–397. doi: 10.1016/j.jadohealth.2021.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team (2022). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL: https://www.R-project.org/.
- Rice J.P., Reich T., Bucholz A.K., Neuman R.J., Fishman R., Rochberg N., Begleiter H. Comparison of direct interview and family history diagnoses of alcohol dependence. Alcohol Clin. Exp. Res. 1995;19:1018–1023. doi: 10.1111/j.1530-0277.1995.tb00983.x. [DOI] [PubMed] [Google Scholar]
- SAMHSA . Substance Abuse and Mental Health Services Administration; Rockville, MD: 2021. Key Substance Use and Mental Health Indicators in the United States: Results from the 2020 National Survey on Drug Use and Health Center for Behavioral Health Statistics and Quality. [Google Scholar]
- Schuckit M.A., Smith T.L. An 8-Year Follow-up of 450 Sons of Alcoholic and Control Subjects. Arch. Gen. Psychiatry. 1996;53:202–210. doi: 10.1001/archpsyc.1996.01830030020005. [DOI] [PubMed] [Google Scholar]
- Sobell, L.C., & Sobell, M.B. (1992). Timeline follow-back. In Measuring alcohol consumption (pp. 41-72). Humana Press, Totowa, NJ.
- Squeglia L.M., Ball T.M., Jacobus J., Brumback T., McKenna B.S., Nguyen-Louie T.T., Sorg S.F., Paulus M.P., Tapert S.F. Neural predictors of initiating alcohol use during adolescence. Am. J. Psychiatry. 2017;174(2):172–185. doi: 10.1176/appi.ajp.2016.15121587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Squeglia L.M., Cservenka A. Adolescence and drug use vulnerability: findings from neuroimaging. Curr. Opin. Behav. Sci. 2017;13:164–170. doi: 10.1016/j.cobeha.2016.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staff J., Maggs J.L., Seto C., Dillavou J., Vuolo M. Electronic and combustible cigarette use in adolescence: links with adjustment, delinquency, and other substance use. J. Adolesc. Health. 2020;66(1):39–47. doi: 10.1016/j.jadohealth.2019.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tapert S.F., Eberson-Shumate S. Alcohol and the adolescent brain: what we've learned and where the data are taking us. Alcohol. Res. 2022;42(1):07. doi: 10.35946/arcr.v42.1.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uban K.A., Horton M.K., Jacobus J., Heyser C., Thompson W.K., Tapert S.F., Madden P.A.F., Sowell E.R., Adolescent Brain Cognitive Development S. Biospecimens and the ABCD study: rationale, methods of collection, measurement and early data. Dev. Cogn. Neurosci. 2018;32:97–106. doi: 10.1016/j.dcn.2018.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow N.D., Han B., Einstein E.B., Compton W.M. Prevalence of substance use disorders by time since first substance use among young people in the US. JAMA Pediatr. 2021;175(6):640–643. doi: 10.1001/jamapediatrics.2020.6981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow N.D., Koob G.F., Croyle R.T., Bianchi D.W., Gordon J.A., Koroshetz W.J., Perez-Stable E.J., Riley W.T., Bloch M.H., Conway K., Deeds B.G., Dowling G.J., Grant S., Howlett K.D., Matochik J.A., Morgan G.D., Murray M.M., Noronha A., Spong C.Y., Wargo E.M., Warren K.R., Weiss S.R.B. The conception of the ABCD study: from substance use to a broad NIH collaboration. Dev. Cogn. Neurosci. 2018;32:4–7. doi: 10.1016/j.dcn.2017.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade N.E., Palmer C.E., Gonzalez M.R., Wallace A.L., Infante M.A., Tapert S.F., Jacobus J., Bagot K.S. Risk factors associated with curiosity about alcohol use in the ABCD cohort. Alcohol. 2021;92:11–19. doi: 10.1016/j.alcohol.2021.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade N.E., Tapert S.F., Lisdahl K.M., Huestis M.A., Haist F. Substance use onset in high-risk 9-13 year-olds in the ABCD Study. Neurotoxicol. Teratol. 2022 doi: 10.1016/j.ntt.2022.107090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoong S.L., Hall A., Turon H., Stockings E., Leonard A., Grady A., Tzelepis F., Wiggers J., Gouda H., Fayokun R., Commar A., Prasad V.M., Wolfenden L. Association between electronic nicotine delivery systems and electronic non-nicotine delivery systems with initiation of tobacco use in individuals aged < 20 years. A systematic review and meta-analysis. PLoS ONE. 2021;16(9) doi: 10.1371/journal.pone.0256044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan M., Cross S.J., Loughlin S.E., Leslie F.M. Nicotine and the adolescent brain. J. Physiol. 2015;593(16):3397–3412. doi: 10.1113/JP270492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zucker R.A., Gonzalez R., Feldstein Ewing S.W., Paulus M.P., Arroyo J., Fuligni A., Morris A.S., Sanchez M., Wills T. Assessment of culture and environment in the Adolescent Brain and Cognitive Development Study: rationale, description of measures, and early data. Dev. Cogn. Neurosci. 2018;32:107–120. doi: 10.1016/j.dcn.2018.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.