Abstract
Introduction:
Healthcare organizations increasingly are screening patients for social needs (e.g., food, housing) and referring them to community resources. This systematic mixed studies review assesses how studies evaluate social needs resource connections and identifies patient- and caregiver-reported factors that may inhibit or facilitate resource connections.
Methods:
Investigators searched PubMed and CINAHL for articles published from October 2015 to December 2020 and used dual review to determine inclusion based on a priori selection criteria. Data related to study design, setting, population of interest, intervention, and outcomes were abstracted. Articles’ quality was assessed using the Mixed Methods Appraisal Tool. Data analysis was conducted in 2021.
Results:
The search identified 34 articles from 32 studies. The authors created a taxonomy of quantitative resource connection measures with 4 categories: whether participants made contact with resources, received resources, had their social needs addressed, or rated some aspect of their experience with resources. Barriers to resource connections were inadequacy, irrelevancy, or restrictiveness; inaccessibility; fears surrounding stigma or discrimination; and factors related to staff training and resource information sharing. Facilitators were referrals’ relevancy, the degree of support and simplicity embedded within the interventions, and interventions being comprehensive and inclusive.
Discussion:
This synthesis of barriers and facilitators indicates areas where healthcare organizations may have agency to improve the efficacy of social needs screening and referral interventions. The authors also recommend that resource connection measures be explicitly defined and focus on whether participants received new resources and whether their social needs were addressed.
INTRODUCTION
Numerous health disciplines, including public health and primary care, have long recognized the interconnections among social justice, social conditions, and health outcomes.1–3 Recently, the healthcare sector revitalized “an explosion of interest”4 in both identifying patients’ social risks (e.g., housing instability and food insecurity) and addressing patients’ social needs (the social risks they wish to have addressed).5 In the U.S., this renewed focus on healthcare-based social interventions corresponds with an ongoing shift toward value-based care, reflecting the intentions of multiple policies and incentives, especially the Affordable Care Act, to foster better care, better health, and lower costs.6–9 The coronavirus disease 2019 (COVID-19) pandemic further accelerated these efforts by highlighting and exacerbating longstanding social injustices that cause health disparities.10–13
Healthcare-based social interventions encompass a wide range of contexts and approaches and may potentially improve patients’ health through a variety of mechanisms, including by connecting patients with resources to decrease their unmet social needs.14,15 In the U.S., prominent organizations—especially the American Academy of Pediatrics and the American Academy of Family Physicians16—and initiatives have been influential in promoting screening and referral strategies to facilitate access to resources. For example, since 2015, the American Academy of Pediatrics has recommended pediatricians implement routine screening and referral interventions for food insecurity.16,17 Likewise, the Centers for Medicare & Medicaid Services is currently testing whether systematically identifying social risks and addressing social needs among Medicare and Medicaid beneficiaries can reduce healthcare costs and utilization through their Accountable Health Communities model.18
A key component of healthcare-based social interventions is facilitating resource connections for patients, yet the idea of what a “resource connection” entails is neither straightforward nor universally understood by healthcare organizations. For example, it may refer to a patient speaking with a staff member at a food bank, enrolling in a program to receive food boxes, or acquiring sufficient food through having received food boxes. Definitions matter because they inform how organizations design interventions and evaluate their impact. As health systems increasingly respond to patients’ social needs, clarifying the range of “resource connection” definitions currently in use (as well as their potential advantages and drawbacks) is critical. Additionally—regardless of the definition(s) an organization selects—it is vital to understand what factors patients say do or do not allow them to connect with needed resources.
Therefore, the authors conducted a systematic mixed studies review (SMSR)19,20 of social needs screening and referral interventions to: (1) assess the ways in which healthcare organizations define—and subsequently measure—resource connections, and (2) identify patient-reported factors that may inhibit or facilitate all types of resource connections. An SMSR follows the same guidelines as a traditional systematic review, but places greater emphasis on synthesizing results across diverse study designs. This type of review may be particularly helpful when synthesizing “complex and highly context-sensitive interventions.”19 An SMSR was salient for this project, as the authors knew a priori that articles would include diverse contexts, study designs, populations of interest, and interventions.21
METHODS
Data Sources and Search Strategy
The review followed PRISMA guidelines and is registered in PROSPERO (CRD42021232123). Working with a health sciences librarian, the authors developed search strategies for MEDLINE and CINAHL databases. They identified a combination of subject terms and keywords for each of 3 concepts: screening, social needs, and referral. These concepts were combined using “AND” to ensure inclusion of all 3 concepts. The search was restricted to English-language studies published from October 2015 (when the American Academy of Pediatrics began recommending pediatricians screen for food insecurity)22 through December 23, 2020. The full search strategy for MEDLINE is available as Appendix Table 1. The authors identified additional articles through the Social Interventions Research & Evaluation Network Evidence & Resource Library.23
Study Selection and Eligibility Criteria
Articles were imported into EndNote, version X9 software and duplicates were removed. Two authors (ASR and KB) independently reviewed titles and abstracts for inclusion or exclusion based on the protocol. The same authors read the full texts of the remaining articles, again using the protocol to make inclusion and exclusion decisions. At both stages, the authors compared their choices and resolved any points of confusion or disagreement. Included articles assessed U.S. healthcare-based social needs screening and referral interventions. Interventions screened patients or caregivers for ≥1 of 5 domains from the Accountable Health Communities Health-Related Social Needs Screening Tool: housing, food, transportation, utilities, and safety.24 Most social needs screening tools include these domains.25 “Referral” meant any attempt to link participants with needed resources, such as by providing a resource sheet or facilitating a handoff to a community-based organization (CBO). Referrals did not need to depend on screening results. Finally, articles had to report quantitative or qualitative outcomes on participants’ ability to access resources or have their social needs addressed. Qualitative outcomes needed to come from patients or caregivers who had participated in an intervention. As the review emphasized material resource connections, studies focusing exclusively on interpersonal safety were excluded.
Data Abstraction, Analysis, and Quality Appraisal
The authors abstracted information on study design, setting, population, intervention, and outcomes into a spreadsheet. The raw data are available from the lead author upon request. The analytic process was inductive, iterative, and applied a parallel-results convergent synthesis design, an optional synthesis approach for SMSRs.20 First, 1 author (ASR) reviewed abstracted data for the outcomes of interest at the level of individual studies (i.e., resource connection measures, barriers, and facilitators) using codes generated directly from the text. In a second pass, ASR identified emerging themes across studies.26 Initial codes and themes were shared with the senior author (MD), practitioners of healthcare-based social interventions, and an expert in the field for further validation. Next, 3 authors (ASR, MD, and KB) used negative case analysis27—a process in which a theory is proposed and then tested and refined based on the data—to categorize resource connection measures into a taxonomy. Regarding barriers and facilitators to resource connections, the same 3 authors collaborated to summarize the breadth and prevalence of themes initially developed by ASR.
Authors used the Mixed Methods Appraisal Tool (MMAT) to assess articles’ quality.28 The MMAT assesses 5 types of designs: quantitative descriptive, non-randomized, RCTs, qualitative, and mixed methods. Reviewers identified the study type and then assessed 5 corresponding methodological criteria, rating each as “yes,” “no,” or “can’t tell.” The MMAT recommends against quality scores, as this can obscure patterns in the types of weaknesses or strengths that exist.28 One author (ASR) completed quality appraisals for all included studies. A second individual (either AT or a research assistant) independently completed second quality appraisals for a subset of the articles. The 2 quality appraisers for each article met to compare their work and draw conclusions through dialogue and consensus.
RESULTS
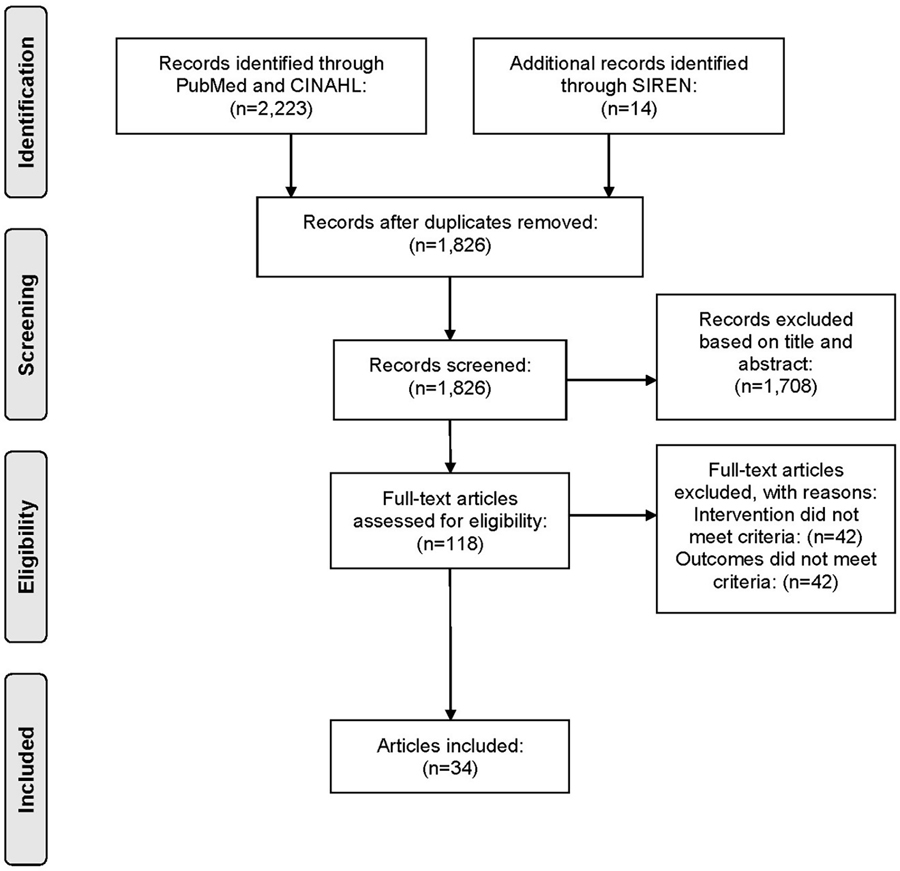
Two authors (ASR and KB) reviewed 1,826 unique abstracts, of which 118 articles underwent full-text review. Eighty-four articles were excluded because of interventions or outcomes being out of scope. Thirty-four articles met inclusion criteria (Figure 1) that report results from 32 studies.
Figure 1.
PRISMA flow diagram.
CINAHL, Cumulative Index to Nursing and Allied Health Literature; SIREN, Social Interventions Research & Evaluation Network.
Mixed Methods Appraisal Tool Results
Included articles encompassed diverse study designs, including descriptive (n=14),29–42 qualitative (n=9),43–51 articles with descriptive and qualitative components (n=2),52,53 explicitly mixed methods (n=4),54–57 RCTs (n=4),58–61 and a non-randomized approach (n=1).62 Appendix Table 2 provides each article’s full MMAT assessment. The majority of articles adhered with all or most of their respective quality criteria on the MMAT, though descriptive studies appeared particularly prone to selection biases.
Study Participants and Settings
As summarized in Appendix Table 3, 16 studies focused on caregivers of pediatric patients,29,31,33,34,38,39,42,43,47,48,51–53,56,58–61 12 focused on adults,30,37,40,44–46,49,50,54,55,57,62 3 appeared to include participants of all ages,35,36,41 and 1 focused on adolescents.32 Some articles further incorporated participants with certain characteristics, including veterans,30,44,55 adults with diabetes,40,46 and children with certain chronic diseases.34,42 Common exclusion criteria were language (e.g., non-English or Spanish speakers) and health status (e.g., severe illness).
The studies represented many healthcare settings (Appendix Table 3), including community health centers, federally qualified health centers, specialty clinics, emergency departments, and others. Twenty-three studies (72%) came from 5 states (California, Massachusetts, Pennsylvania, Minnesota, and New York) and most studies (n=20, 63%) were conducted in urban environments.
Screening and Resource Connection Strategies
As shown in Table 1, a total of 12 studies (38%) concentrated on food insecurity, using either the Hunger Vital Sign™ or U.S. Household Food Security Survey Module screening tools.29,31,36,37,41–43,46–48,52,54,56 Three studies (9%) focused on housing instability, using the Homelessness Screening Clinical Reminder.30,44,55 The remaining 17 studies (53%) identified multiple social needs using 8 screening tools, the most common being modifications of a tool developed by Health Leads (n=7 studies).33,35,39,45,50,57,62 All tools with multiple social needs included food and housing and several included child care, transportation, employment, finances, and utilities.
Table 1.
Screening and Resource Connection Strategies (n=32 studies)
| Screening | Resource connection strategy | ||||||
|---|---|---|---|---|---|---|---|
| Author/year | Screening tool | Screening processa | One-to-one navigation support | Written materials/resource sheets | Community partner facilitates resource connections | Other community partner or resources on-site | Unclear or inconsistent connection strategy |
| Marpadga (2019)46 | Hunger Vital Sign | Healthcare personnela | X | X | X | ||
| Swavely (2019)54 | Hunger Vital Sign | Healthcare personnel | X | X | X | ||
| Cullen (2020)43 | Hunger Vital Sign | Healthcare personnel OR Participantsa | X | X | |||
| Orr (2019)47 | Hunger Vital Sign | Participants | X | X | |||
| Fox (2016)31 | Hunger Vital Sign | Participants | X | ||||
| Fritz (2020)42 | Hunger Vital Sign | Participants | X | ||||
| Martel (2018)41 | Hunger Vital Sign | Healthcare personnel | X | ||||
| Knowles (2018)52 | Hunger Vital Sign | Healthcare personnel OR Participants | X | ||||
| Palakshappa (2017a)56 Palakshappa (2017b)48 |
Hunger Vital Sign | Healthcare personnel | X | ||||
| Smith A (2020)36 | Hunger Vital Sign | Healthcare personnel | X | ||||
| Smith S (2017)37 | U.S. Household Food Security Survey Module | Participants | X | X | |||
| Bottino (2017)29 | U.S. Household Food Security Survey Module (Embedded within Online Advocate, now HelpSteps) | Participants | X | ||||
| Hassan (2015)32 | HelpSteps (Online Advocate) | Participants | X | X | |||
| Cusack (2020)44 | Homelessness Screening Clinical Reminder (HSCR) | Healthcare personnel | X | ||||
| Fargo (2017)30 | HSCR | Healthcare personnel | X | ||||
| Montgomery (2020)55 | HSCR | Healthcare personnel | X | ||||
| Berkowitz (2019)57 | Health Leads | Participants | X | ||||
| Fiori (2020)39 | Health Leads | Participants | X | X | |||
| Hsu (2020)45 | Health Leads | Participants | X | ||||
| Polk (2020)33 | Health Leads | Healthcare personnel OR Participants | X | ||||
| Manian (2020)35 | Health Leads | Healthcare personnel OR Participants | X | ||||
| Schickedanz (2019)62 | Health Leads | Healthcare personnel | X | ||||
| Zhu (2020)50 | Two different tools, both inspired by Health Leads | Healthcare personnel OR Participants | X | ||||
| Garg (2015)b 59 | WE CARE | Participants | X | ||||
| Power-Hays (2019)34 | WE CARE | Participants | X | ||||
| Emengo (2020)51 | Social Health Alliance to Promote Equity (SHAPE) (Formerly “Family Needs”) | Participants | X | X | |||
| Uwemedimo (2018)38 | Social Health Alliance to Promote Equity (SHAPE) (Formerly “Family Needs”) | Participants | X | X | |||
| Gottlieb (2020)b 58 | 18-item social risk screening questionnaire (iScreen) | Healthcare personnel | X | X | |||
| Gottlieb (2018)b
61 Gottlieb (2016)b 60 |
14-item social and mental health needs questionnaire (iScreen) | Healthcare personnel | X | ||||
| Nguyen (2016)40 | 7-item social needs checklist | Healthcare personnel | X | X | |||
| Ray (2020)53 | 59-item survey (7 questions related to social needs) | Participants | X | ||||
| Hamity (2018)49 | Your Current Life Situation (YCLS) tool | Unclear | X | ||||
| Total | 16 | 10 | 8 | 7 | 4 | ||
Screening process = Person who administered the screening; Healthcare personnel = People administering the screening to the participants (i.e., study team members, healthcare personnel, volunteers); Participants = Patients or caregivers completed the screening tool on their own.
For the RCTs, the table reflects what appeared to be done for the intervention groups.
In 14 studies (44%), participants appeared to complete the screening for themselves, either through paper, tablet, or a web-based platform (Table 1).29,31,32,34,37–39,42,45,47,51,53,57,59 In many cases, healthcare staff were available to support completion when challenges arose (e.g., comprehension, literacy, vision). The screening was administered verbally for 12 studies (38%), either in person or by phone.30,36,40,41,44,46,48,54–56,58,60–62 In 5 studies (16%), the screenings were both self- and staff-administered.33,35,43,50,52
The authors identified 4 types of referral/resource connection strategies (Table 1). Approximately 30% of studies applied >1 type of strategy. These strategies included 1-to-1 navigation support, the provision of written materials or resource sheets, a community partner facilitating the resource connections, and other community collaboration or on-site resources. The authors defined 1-to-1 navigation support as personalized assistance to understand and connect with relevant resources; varied types of healthcare staff or trained volunteers provided this help. Sixteen studies (50%) used 1-to-1 navigation support, most of which screened for multiple social needs.32,33,35,37–40,45,46,50,51,54,57,58,60–62 Ten studies (31%) provided written materials or resources sheets.29,32,34,40,43,46,47,53,58,59 Eight studies (25%), all of which focused on food insecurity, worked with a community partner who was responsible for facilitating the resource connections.31,36,41–43,48,52,54,56 Finally, 7 studies (22%) described additional types of community partnerships or offered on-site resources.37–39,46,47,51,54
Resource Connection Outcome Measures
Twenty-five studies included diverse quantitative outcome measures related to participants’ (i.e., patients or caregivers) social needs resource reconnections. The authors created a taxonomy of these measures, classifying them into 4 categories (Table 2).
Table 2.
Taxonomy of Quantitative Resource Connection Outcome Measures (n=25 studies)
| Author/year | Whether made contact with a service / organization | Whether enrolled in or received new services | Whether social needs were addressed | Participants’ ratings of their experiences with resources |
|---|---|---|---|---|
| Fargo (2017)30 | X | |||
| Montgomery (2020)55 | X | |||
| Ray (2020)53 | X | |||
| Schickedanz (2019)62 | X | |||
| Uwemedimo (2018)38 | X | |||
| Swavely (2019)54 | X | |||
| Power-Hays (2019)34 | X | X | ||
| Bottino (2017)29 | X | X | ||
| Fiori (2020)39 | X | X | ||
| Garg (2015)59 | X | X | ||
| Nguyen (2016)40 | X | X | ||
| Fox (2016)31 | X | X | ||
| Knowles (2018)52 | X | X | ||
| Palakshappa (2017a)56 | X | X | ||
| Marpadga (2019)46 | X | X | ||
| Smith S (2017)37 | X | X | ||
| Fritz (2020)42 | X | X | ||
| Martel (2018)41 | X | X | ||
| Smith A (2020)36 | X | X | ||
| Polk (2020)33 | X | X | X | |
| Manian (2020)35 | X | X | X | |
| Hassan (2015)32 | X | X | ||
| Berkowitz (2019)57 | X | |||
| Gottlieb (2020)58 | X | |||
| Gottlieb (2018)61 Gottlieb (2016)60 |
X |
Most studies with quantitative outcomes discussed resource connections as participants having made contact with services or organizations (n=22, 88%).29–42,46,52–56,59,62 This was stated explicitly in most cases. For example, the number of participants who were “successfully contacted by [the community partner]”41 or reported that more intervention than control group participants “had contacted a community resource.”59 At other times, resource connections were indicated despite ambiguous language used by the study authors. For example, the percentage of participants who “received services”55 or “successfully utilized program-provided resources.”38
Fewer studies (n=13, 52%) provided evidence for whether participants enrolled in or received new services.31,33,35–37,39–42,46,52,56,59 This mostly occurred in the food-related studies, which often reported on whether or not participants enrolled in the Supplemental Nutrition Assistance Program (SNAP). Other studies provided specific details around what types of resources participants appeared to access through the intervention. Garg et al.59 reported a higher proportion of participants in the intervention group enrolled in a job training program, enrolled children in child care, and were receiving fuel assistance.
Six studies (24%) included outcomes on whether participants’ social needs resolved, which may or may not have been attributed to the intervention.32,33,35,57,58,60,61 Hassan and colleagues32 provided information regarding the percentage who “reported resolution of their top-priority problem.” Berkowitz et al.57 collected pre- and post-intervention data regarding the types of needs, and reported whether there were significant decreases in the prevalence of each need. Two RCTs by Gottlieb et al. examined changes in the number and types of “social needs”60,61 or “social risk factors.”58 For example, Gottlieb and colleagues60,61 found significant reductions in social needs for intervention versus control groups.
Finally, 2 studies included quantitative outcome measures that seemed to reflect an aspect of participants’ experiences with the resources. Bottino et al.29 asked participants whether they were getting “[none, a little, most, or all] of the help they needed with their referral selection.” And Power-Hays and colleagues34 reported on the percentage who found organizations to be “helpful.”
Participant-Reported Barriers and Facilitators to Resource Connections for Social Needs
Table 3 summarizes participant-reported barriers and facilitators to resource connections across the qualitative components of the studies. Results also include the ways in which additional sources of data from the studies (e.g., quantitative data, clinicians’ perspectives) corroborate and expand upon participants’ perspectives.
Table 3.
Participant-Reporteda Barriers and Facilitators to Resource Connections (n=13)
| Barriers |
|
|
| Inadequate, Irrelevant, Restrictive |
| • Inadequacy or irrelevancy of the resources offered and/or existing resources in the community.44–46,48,50–52,54,57 |
| • Restrictive eligibility criteria.44,45,48,54 |
| Inaccessible |
| • Navigating complex systems.44,45,48,49,51,54 |
| • Physical inaccessibility (e.g., transportation barriers, medical complexity).43,45–47,50,57 |
| • Language and/or literacy barriers.45,50,54,57 |
| • Competing demands (e.g., work, childcare).43,46,47,49,50,54,57 |
| Stigma, Discrimination, Fear |
| • Concerns related to stigma and/or discrimination.43,45,46,52 |
| • Immigration policies causing fear.45,46 |
| Staff Training & Resource Information Sharing |
| • Unsatisfactory experiences with healthcare and/or social services personnel (e.g., impersonal handoffs, staff lack of knowledge about resources) 44,45,49,52 |
| • Losing, forgetting, or not learning about resources.43,44,46,47,49,53,54 |
| • Inaccurate information provided about resources.45,57 |
|
|
| Facilitators |
|
|
| Relevancy |
| • Aligning referrals with participants’ social needs and contexts.46,48,50,51,53,54,57 |
| Support, Simplicity |
| • Help navigating complex systems (e.g., establishing rapport, answering questions, help filling out forms).44–46,48–50,52,54 |
| • Prompt and simple follow-up processes.44,46,51 |
| • Electronic resources easier to access.43,44 |
| Comprehensive, Inclusive |
| • Focusing on multiple social needs.57 |
| • Offering referrals to everyone versus only those who disclose social needs.43,53 |
Refers to patients or caregivers, specifically.
The most frequent participant-reported barrier included the resources being inadequate or irrelevant. Inadequacy related to a lack of resources in the community (e.g., housing)45,50 or the resources offered not being tailored to or adequately addressing participants’ social needs.44–46,48,51,52,54,57 For example, an inability to take advantage of food resources owing to not having a place to cook46 or food resources not being tailored to medical recommendations.54 A related barrier was restrictive eligibility criteria.44,45,48,54 Articles with quantitative outcomes also found participants disclosing food insecurity, but being ineligible for or already enrolled in in SNAP.31,36,41,42,52
Multiple factors related to resource inaccessibility. Broadly, participants discussed challenges of navigating complex systems and applications,44,45,48,49 including delayed or absent resource follow-up.51,54 Inaccessibility also included mobility and transportation. Those with certain diseases or disabilities reported difficulty in accessing services45,57 and resources were sometimes geographically inconvenient.43,46,47,50 Other barriers were language or literacy inaccessibility.45,50,54,57 Zhu et al.50 reported that participants described language barriers when filling out social services forms. In a descriptive study, Spanish speakers had significantly lower odds of successfully acquiring resources compared with English speakers in 3 of 4 examined regions.33 Finally, participants’ competing demands inhibited accessibility (e.g., not having child care).43,46,47,49,50,54,57
Studies discussed participants’ concerns around stigma or discrimination in relation to both disclosure of social needs, as well as pursuing resource referrals.43,45,46,52 In particular, 2 studies (1 from participants’ and 1 from clinicians’ perspectives) pointed out fear due to immigration policies.46,52 In another study, a participant-reported systems barrier was immigration status and policies.45 One descriptive study explicitly examined disparities related to immigration status. It found families with a non-U.S. citizen were most likely to be lost to follow-up, but were also most likely to utilize resources if they did engage.38
Some participants noted unsatisfactory experiences with healthcare or social services personnel. One study described mistreatment,52 but most reported staff not having the necessary knowledge, skills, or time to support with resource connections.44,45,49 A descriptive study found the type of professional conducting the screening was associated with participants receiving services.55 Other barriers were resource information sharing and perceived information quality. Information retention, misplacing resource sheets, and participants inconsistently being told about resources may have inhibited connections.43,44,46,47,49,53,54 Additionally, participants reported low-quality information, such as when resources were out of date or hyperlinks were nonfunctional.45,57
A finding across many studies was participants’ desire for referrals relevant to their needs and contexts.46,48,50,51,53,54,57 This included referrals to resources that existed in the community, that were geographically convenient, for which participants met the eligibility criteria, and that adequately aligned with the needs disclosed. For example, 2 articles indicated the importance of food resources beyond SNAP,48,54 especially given some participants already receiving SNAP remained food insecure. Two similar RCTs compared the effectiveness of resource sheets (control group) versus navigation (intervention group) in decreasing participants’ social needs.58,60 Whereas the first study only found decreases in the intervention group, the second found decreases in both groups. Authors speculated this might have occurred because of improved resource sheets in the second study, with better updated information, listing contact names at the relevant agencies, and highlighting the resources that most aligned with participants’ priorities.58
Patients and caregivers shared the importance of receiving help navigating systems and enrolling in services,44,45,48–50,52,54 including effective communication to establish trust and rapport. Similarly, participants expressed a desire for prompt, simple, and convenient follow-ups.44,46,51 In 2 of the descriptive articles, more follow-ups were associated with “successful referrals”39 and “optimally successful resource connections.”35 In 1 of these studies, outreach occurring within 30 days from the start of the intervention was associated with a higher proportion of “successful referrals.”39 Participants also suggested receiving resource information in one form versus another (e.g., electronic versus printout) could ease connections.43,44
Final facilitating factors addressed the kinds of resources offered and who is helped. A finding by Berkowitz and colleagues57 described “nonlinearity” between which resources addressed which needs. For instance, getting help with medication costs could free up monies for food. This may suggest an advantage of offering resources for multiple needs. In 2 studies, participants suggested resources be advertised to everyone versus only those with positive screening results.43,53 This recommendation is supported by quantitative findings from Bottino et al.29 that 14.7% of participants selected referrals despite not disclosing food insecurity.
DISCUSSION
Although a number of reviews explore various facets of healthcare-based social interventions,21,63–68 this is the first to focus squarely on resource connections across varied social needs. The review makes 3 notable contributions: a taxonomy of resource connection measures, a synthesis of patient- and caregiver-reported barriers and facilitators to resource connections, and the application of an SMSR approach that may be useful for both practitioners and researchers.
Taxonomy of Resource Connection Measures
The findings on resource connection measures indicate most of the included studies had outcomes about whether participants contacted services or organizations, and fewer provided details on participants’ ability to enroll in or receive new services, success with addressing social needs, or experiences with resource connection processes. Additionally, vague language in some of the studies made process measures difficult to interpret or categorize. As others have pointed out, a key aspect of determining whether healthcare-based social interventions improve participants’ health is first establishing whether the interventions perform as intended.15,21 As screening and referral programs are meant to link participants with resources that will address their needs, the authors argue study designs and measures demonstrating enrollment in new services and whether needs are reduced are likely the most meaningful outcomes. By identifying distinct forms of resource connections, the review’s taxonomy may help lay the groundwork for future comparative work, including meta-analyses, on the extent to which screening and referral interventions connect patients with resources.
Synthesis of Participant-Reported Barriers and Facilitators to Resource Connections
The barriers and facilitators synthesis suggests areas where healthcare organizations may have agency to improve the likelihood of success across all components of the resource connection taxonomy: making contact with CBOs, enrolling in services, getting needs resolved, and having a good experience with the process at large. Namely—given the complexity of U.S. healthcare and social services systems, the priorities that patients and caregivers are juggling, and stigma and discrimination concerns—the authors recommend simplicity, accessibility, adequate training for healthcare teams, and more CBO partnerships. Interventions could minimize the number of handoffs and follow up quickly with participants. Healthcare organizations could consider whether programs are inclusive of those with limited English proficiency, low health literacy, disabilities, and other factors that may inhibit accessibility. It is also crucial referrals be tailored to the unique needs and preferences of participants to the extent possible. This includes referrals corresponding with social needs, being geographically convenient, and for which participants are eligible. Adequate training for healthcare personnel, both in terms of communication skills (e.g., empathic inquiry)69 and an understanding of local resources, could also enhance connections. This is particularly salient for easing participants’ legitimate concerns around stigma or discrimination (e.g., fears related to child welfare involvement or immigration policies),70,71 which could impact decisions to pursue referrals. Finally, many studies in this review did not describe CBO partnerships, a critical dimension given these are likely crucial for improving connections.68,72,73 Future research could focus on effective collaboration strategies and how to overcome structures that make health and social services organizations reluctant to collaborate.74
Results around the frequent unavailability and inadequacy of resources also reaffirm the limits of healthcare organizations to address participants’ social needs without major upstream investments in public health initiatives and policies.75,76 As healthcare settings collect more data about resource gaps within their communities, the authors suggest they advocate for population-level investments to improve the conditions in which people live.77 In that regard, it is notable that few studies in the review explicitly included rural areas, which often experience a scarcity of healthcare and social services resources.76,78,79
Though the review focuses on barriers and facilitators at the point when participants had disclosed social risks and consented to receive help with social needs, other researchers have noted the importance to understanding what affects connections along the entire “pathway” of screening and referral interventions; there are other instances in which “drop-offs” in participant engagement occur (A Schweitzer, Senior Fellow, Mossavar-Rahmani Center for Business & Government, Harvard Kennedy School, unpublished work, 2021). For example, many studies report drop-offs in terms of participants declining resource navigation assistance after having disclosed social risks.80 Also, interventions only including certain groups (e.g., those with medical complexity) are prone to bias and may overlook people who would otherwise benefit.81
Systematic Mixed Studies Review Approach
A third contribution is the use of an SMSR approach to highlight the ways in which findings garnered from diverse methodologies coalesced around the topic of interest. To avoid privileging one form of evidence over another, the authors used the MMAT28 to assess the quality of study designs in their own right, keeping in mind that all methodologies operate through distinct epistemologies82 and inform different aspects of theory creation and practice. Although RCTs are frequently identified as the gold standard when it comes to establishing causality, other study designs are also vital for understanding real-world applications of complex interventions across multiple contexts.83–87 Instead of jumping to whether healthcare-based social interventions connect patients and caregivers with needed resources, an SMSR approach prompted and allowed the authors to explore the paradigmatically pragmatic88 questions of how to meaningfully define “resource connections” and why resource connections may or may not be successful across diverse contexts. Owing to the highly complex nature of healthcare-based social interventions, other researchers may find an SMSR approach to be beneficial for their research questions.
Limitations
The review has 2 primary limitations. First, by focusing on interventions with a screening component, studies using alternative strategies to link participants with resources (e.g., “CommunityRx”)89,90 were excluded. All approaches to resource connections merit exploration, but the authors narrowed the scope to screening and referral interventions given their current prominence across various healthcare organizations and initiatives. Second, the search terms and strategy removed certain types of information that are likely salient for better understanding this topic, including evidence from the gray literature, articles published outside the U.S., and those published before October 2015. Regarding the cut-off date, this decision would have been more problematic had the authors intended to perform a meta-analysis. Instead, the goal was to synthesize current evaluation approaches and narratives, beginning at a time when there was a notable momentum shift surrounding these interventions. Lastly, although authors consulted with a health sciences librarian, it is possible that different or additional search terms may have identified more studies.
CONCLUSIONS
As healthcare organizations increasingly develop interventions to connect patients and caregivers with resources for social needs, the review summarizes current efforts and offers specific recommendations regarding design and evaluation. To the extent that is feasible, organizations should be thoughtful about how to create programs that are simple, accessible, and incorporate adequate training for all healthcare personnel involved. Evaluation measures of resource connection should be clearly stated, and ideally focus on whether participants accessed new resources and whether the resources were able to address their needs. Effective partnerships with CBOs may increase the likelihood of both resource connections and the ability to track outcomes. Finally, advocacy for upstream public health policies is critical to the success of healthcare-based social interventions, as a primary challenge for health care is to connect patients when resources are not available in their local communities.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank several individuals who contributed to the development of this manuscript. Laura Zeigen—Health Sciences Education and Research Librarian with Oregon Health & Science University—provided substantial guidance in the development and implementation of the search strategy. The authors also acknowledge the following colleagues who double-checked data abstraction and articles’ quality: Zoe Major-McDowall, Lisa Tanrikulu, Zoe Rothberg, and Claire Londagin.
The content is solely the responsibility of the authors and does not necessarily represent the views of the Agency for Healthcare Research and Quality.
Anna Steeves-Reece received funding support for this research by the Agency for Healthcare Research and Quality grant 1R36HS027707-01. The Agency for Healthcare Research and Quality had no role in study design; collection, analysis, or interpretation of the data; writing the manuscript; or the decision to submit the manuscript for publication. The remaining authors have no conflicts of interest to report.
Footnotes
The authors were accepted to share findings from this systematic mixed studies review in an oral presentation at the American Public Health Association’s Annual Meeting in October 2021.
No financial disclosures were reported by the authors of this paper.
REFERENCES
- 1.Beauchamp DE. Public health as social justice. Inquiry. 1976;13(1):3–14. [PubMed] [Google Scholar]
- 2.Krieger N, Birn AE. A vision of social justice as the foundation of public health: commemorating 150 years of the spirit of 1848. Am J Public Health. 1998;88(11):1603–1606. 10.2105/ajph.88.11.1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lawn JE, Rohde J, Rifkin S, Were M, Paul VK, Chopra M. Alma-Ata 30 years on: revolutionary, relevant, and time to revitalise. Lancet. 2008;372(9642):917–927. 10.1016/s0140-6736(08)61402-6. [DOI] [PubMed] [Google Scholar]
- 4.Kreuter MW, Thompson T, McQueen A, Garg R. Addressing social needs in health care settings: evidence, challenges, and opportunities for public health. Annu Rev Public Health. 2020;42:329–344. 10.1146/annurev-publhealth-090419-102204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alderwick H, Gottlieb LM. Meanings and misunderstandings: a social determinants of health lexicon for health care systems. Milbank Q. 2019;97(2):407–419. 10.1111/1468-0009.12390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fraze T, Lewis VA, Rodriguez HP, Fisher ES. Housing, transportation, and food: how ACOs seek to improve population health by addressing nonmedical needs of patients. Health Aff (Millwood). 2016;35(11):2109–2115. 10.1377/hlthaff.2016.0727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sullivan HR. Hospitals’ obligations to address social determinants of health. AMA J Ethics. 2019;21(3):E248–E258. 10.1001/amajethics.2019.248. [DOI] [PubMed] [Google Scholar]
- 8.Buehler JW, Snyder RL, Freeman SL, Carson SR, Ortega AN. It’s not just insurance: the Affordable Care Act and population health. Public Health Rep. 2018;133(1):34–38. 10.1177/0033354917743499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Onie RD, Lavizzo-Mourey R, Lee TH, Marks JS, Perla RJ. Integrating social needs into health care: a twenty-year case study of adaptation and diffusion. Health Aff (Millwood). 2018;37(2):240–247. 10.1377/hlthaff.2017.1113. [DOI] [PubMed] [Google Scholar]
- 10.Baptiste DL, Commodore-Mensah Y, Alexander KA, et al. COVID-19: shedding light on racial and health inequities in the USA. J Clin Nurs. 2020;29(15–16):2734–2736. 10.1111/jocn.15351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sharma SV, Chuang RJ, Rushing M, et al. Social determinants of health–related needs during COVID-19 among low-income households with children. Prev Chronic Dis. 2020;17:E119. 10.5888/pcd17.200322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bowleg L We’re not all in this together: on COVID-19, intersectionality, and structural inequality. Am J Public Health. 2020;110(7):917. 10.2105/ajph.2020.305766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yearby R Structural racism and health disparities: reconfiguring the social determinants of health framework to include the root cause. J Law Med Ethics. 2020;48(3):518–526. 10.1177/1073110520958876. [DOI] [PubMed] [Google Scholar]
- 14.Fichtenberg CM, Alley DE, Mistry KB. Improving social needs intervention research: key questions for advancing the field. Am J Prev Med. 2019;57(6 suppl 1):S47–S54. 10.1016/j.amepre.2019.07.018. [DOI] [PubMed] [Google Scholar]
- 15.Gurewich D, Garg A, Kressin NR. Addressing social determinants of health within healthcare delivery systems: a framework to ground and inform health outcomes. J Gen Intern Med. 2020;35(5):1571–1575. 10.1007/s11606-020-05720-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gusoff G, Fichtenberg C, Gottlieb LM. Professional medical association policy statements on social health assessments and interventions. Perm J. 2018;22:18–092. 10.7812/tpp/18-092. [DOI] [Google Scholar]
- 17.O’Keefe L Identifying food insecurity: Two-question screening tool has 97% sensitivity. AAP News. October 22, 2015. https://publications.aap.org/aapnews/news/11198. Accessed December 21, 2021. [Google Scholar]
- 18.Alley DE, Asomugha CN, Conway PH, Sanghavi DM. Accountable health communities—addressing social needs through Medicare and Medicaid. N Engl J Med. 2016;374(1):8–11. 10.1056/nejmp1512532. [DOI] [PubMed] [Google Scholar]
- 19.Pluye P, Hong QN. Combining the power of stories and the power of numbers: mixed methods research and mixed studies reviews. Annu Rev Public Health. 2014;35:29–45. 10.1146/annurev-publhealth-032013-182440. [DOI] [PubMed] [Google Scholar]
- 20.Hong QN, Pluye P, Bujold M, Wassef M. Convergent and sequential synthesis designs: implications for conducting and reporting systematic reviews of qualitative and quantitative evidence. Syst Rev. 2017;6(1):61. 10.1186/s13643-017-0454-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gottlieb LM, Wing H, Adler NE. A systematic review of interventions on patients’ social and economic needs. Am J Prev Med. 2017;53(5):719–729. 10.1016/j.amepre.2017.05.011. [DOI] [PubMed] [Google Scholar]
- 22.American Academy of Pediatrics, Council on Community Pediatrics, Committee on Nutrition. Promoting food security for all children. Pediatrics. 2015;136(5):e1431–e1438. 10.1542/peds.2015-3301. [DOI] [PubMed] [Google Scholar]
- 23.Social Interventions Research & Evaluation Network (SIREN). Evidence & Resource Library. https://sirenetwork.ucsf.edu/tools/evidence-library. Accessed December 17, 2021.
- 24.Billioux A, Verlander K, Anthony S, Alley D. Standardized screening for health-related social needs in clinical settings: the accountable health communities screening tool. NAM Perspect. May 30, 2017. 10.31478/201705b. [DOI] [Google Scholar]
- 25.Moen M, Storr C, German D, Friedmann E, Johantgen M. A review of tools to screen for social determinants of health in the United States: a practice brief. Popul Health Manag. 2020;23(6):422–429. 10.1089/pop.2019.0158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Patton MQ. Qualitative Analysis and Interpretation. In: Qualitative research and evaluation methods. 3rd ed. Thousand Oaks, CA: Sage Publications, Inc.; 2002:431–534. [Google Scholar]
- 27.Bernard RH, Wutich A, Ryan GW. Conceptual models. In: Analyzing qualitative data: systematic approaches. 2nd ed. Thousand Oaks, CA: Sage Publications, Inc.; 2017:175–198. [Google Scholar]
- 28.Hong QN, Fàbregues S, Bartlett G, et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Education for Information. 2018;34(4):285–291. 10.3233/efi-180221. [DOI] [Google Scholar]
- 29.Bottino CJ, Rhodes ET, Kreatsoulas C, Cox JE, Fleegler EW. Food insecurity screening in pediatric primary care: can offering referrals help identify families in need? Acad Pediatr. 2017;17(5):497–503. 10.1016/j.acap.2016.10.006. [DOI] [PubMed] [Google Scholar]
- 30.Fargo JD, Montgomery AE, Byrne T, Brignone E, Cusack M, Gundlapalli AV. Needles in a haystack: screening and healthcare system evidence for homelessness. Stud Health Technol Inform. 2017;235:574–578. 10.3233/978-1-61499-753-5-574. [DOI] [PubMed] [Google Scholar]
- 31.Fox CK, Cairns N, Sunni M, Turnberg GL, Gross AC. Addressing food insecurity in a pediatric weight management clinic: a pilot intervention. J Pediatr Health Care. 2016;30(5):e11–e15. 10.1016/j.pedhc.2016.05.003. [DOI] [PubMed] [Google Scholar]
- 32.Hassan A, Scherer EA, Pikcilingis A, et al. Improving social determinants of health: effectiveness of a web-based intervention. Am J Prev Med. 2015;49(6):822–831. 10.1016/j.amepre.2015.04.023. [DOI] [PubMed] [Google Scholar]
- 33.Polk S, Leifheit KM, Thornton R, Solomon BS, DeCamp LR. Addressing the social needs of Spanish-and English-speaking families in pediatric primary care. Acad Pediatr. 2020;20(8):1170–1176. 10.1016/j.acap.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Power-Hays A, Li S, Mensah A, Sobota A. Universal screening for social determinants of health in pediatric sickle cell disease: a quality-improvement initiative. Pediatr Blood Cancer. 2020;67(1):e28006. 10.1002/pbc.28006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Manian N, Wagner CA, Placzek H, Darby BA, Kaiser TJ, Rog DJ. Relationship between intervention dosage and success of resource connections in a social needs intervention. Public Health. 2020;185:324–331. 10.1016/j.puhe.2020.05.058. [DOI] [PubMed] [Google Scholar]
- 36.Smith AM, Zallman L, Betts K, et al. Implementing an electronic system to screen and actively refer to community based agencies for food insecurity in primary care. Healthc (Amst). 2020;8(1):100385. 10.1016/j.hjdsi.2019.100385. [DOI] [PubMed] [Google Scholar]
- 37.Smith S, Malinak D, Chang J, et al. Implementation of a food insecurity screening and referral program in student-run free clinics in San Diego, California. Prev Med Rep. 2017;5:134–139. 10.1016/j.pmedr.2016.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Uwemedimo OT, May H. Disparities in utilization of social determinants of health referrals among children in immigrant families. Front Pediatr. 2018;6:207. 10.3389/fped.2018.00207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fiori KP, Rehm CD, Sanderson D, et al. Integrating social needs screening and community health workers in primary care: the community linkage to care program. Clin Pediatr (Phila). 2020;59(6):547–556. 10.1177/0009922820908589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nguyen AL, Angulo M, Haghi LL, et al. A clinic-based pilot intervention to enhance diabetes management for elderly Hispanic patients. J Health Environ Educ. 2016;8:1–6. 10.18455/08001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Martel ML, Klein LR, Hager KA, Cutts DB. Emergency department experience with novel electronic medical record order for referral to food resources. West J Emerg Med. 2018;19(2):232–237. 10.5811/westjem.2017.12.35211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fritz CQ, Thomas J, Brittan MS, Mazzio E, Pitkin J, Suh C. Referral and resource utilization among food insecure families identified in a pediatric medical setting. Acad Pediatr. 2021;21(3):446–454. 10.1016/j.acap.2020.11.019. [DOI] [PubMed] [Google Scholar]
- 43.Cullen D, Attridge M, Fein JA. Food for thought: a qualitative evaluation of caregiver preferences for food insecurity ccreening and resource referral. Acad Pediatr. 2020;20(8):1157–1162. 10.1016/j.acap.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cusack M, Montgomery AE, Sorrentino AE, Dichter ME, Chhabra M, True G. Journey to home: development of a conceptual model to describe veterans’ experiences with resolving housing instability. Hous Stud. 2020;35(2):310–332. 10.1080/02673037.2019.1598551. [DOI] [Google Scholar]
- 45.Hsu C, Cruz S, Placzek H, et al. Patient perspectives on addressing social needs in primary care using a screening and resource referral intervention. J Gen Intern Med. 2020;35(2):481–489. 10.1007/s11606-019-05397-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Marpadga S, Fernandez A, Leung J, Tang A, Seligman H, Murphy EJ. Challenges and successes with food resource referrals for food-insecure patients with diabetes. Perm J. 2019;23:18–097. 10.7812/tpp/18-097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Orr CJ, Chauvenet C, Ozgun H, Pamanes-Duran C, Flower KB. Caregivers’ experiences with food insecurity screening and impact of food insecurity resources. Clin Pediatr (Phila). 2019;58(14):1484–1492. 10.1177/0009922819850483. [DOI] [PubMed] [Google Scholar]
- 48.Palakshappa D, Doupnik S, Vasan A, et al. Suburban families’ experience with food insecurity screening in primary care practices. Pediatrics. 2017(b);140(1):e20170320. 10.1542/peds.2017-0320. [DOI] [PubMed] [Google Scholar]
- 49.Hamity C, Jackson A, Peralta L, Bellows J. Perceptions and experience of patients, staff, and clinicians with social needs assessment. Perm J. 2018;22:18–105. 10.7812/tpp/18-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhu E, Ahluwalia S. An evaluation of connect for health: a social referral program in RI. R I Med J (2013). 2020;103(5):65–69. [PubMed] [Google Scholar]
- 51.Emengo VN, Williams MS, Odusanya R, et al. Qualitative program evaluation of social determinants of health screening and referral program. PLoS One. 2020;15(12):e0242964. 10.1371/journal.pone.0242964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Knowles M, Khan S, Palakshappa D, et al. Successes, challenges, and considerations for integrating referral into food insecurity screening in pediatric settings. J Health Care Poor Underserved. 2018;29(1):181–191. 10.1353/hpu.2018.0012. [DOI] [PubMed] [Google Scholar]
- 53.Ray KN, Gitz KM, Hu A, Davis AA, Miller E. Nonresponse to health-related social needs screening questions. Pediatrics. 2020;146(3):e20200174. 10.1542/peds.2020-0174. [DOI] [PubMed] [Google Scholar]
- 54.Swavely D, Whyte V, Steiner JF, Freeman SL. Complexities of addressing food insecurity in an urban population. Popul Health Manag. 2019;22(4):300–307. 10.1089/pop.2018.0126. [DOI] [PubMed] [Google Scholar]
- 55.Montgomery AE, Rahman AF, Chhabra M, Cusack MC, True JG. The importance of context: linking veteran outpatients screening positive for housing instability with responsive interventions. Adm Policy Ment Health. 2021;48:23–35. 10.1007/s10488-020-01028-z. [DOI] [PubMed] [Google Scholar]
- 56.Palakshappa D, Vasan A, Khan S, Seifu L, Feudtner C, Fiks AG. Clinicians’ perceptions of screening for food insecurity in suburban pediatric practice. Pediatrics. 2017;140(1):e20170319. 10.1542/peds.2017-0319. [DOI] [PubMed] [Google Scholar]
- 57.Berkowitz SA, Hulberg AC, Placzek H, et al. Mechanisms associated with clinical improvement in interventions that address health-related social needs: a mixed-methods analysis. Popul Health Manag. 2019;22(5):399–405. 10.1089/pop.2018.0162.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gottlieb LM, Adler NE, Wing H, et al. Effects of in-person assistance vs personalized written resources about social services on household social risks and child and caregiver health: a randomized clinical trial. JAMA Netw Open. 2020;3(3):e200701. 10.1001/jamanetworkopen.2020.0701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Garg A, Toy S, Tripodis Y, Silverstein M, Freeman E. Addressing social determinants of health at well child care visits: a cluster RCT. Pediatrics. 2015;135(2):e296–e304. 10.1542/peds.2014-2888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gottlieb LM, Hessler D, Long D, et al. Effects of social needs screening and in-person service navigation on child health: a randomized clinical trial. JAMA Pediatr. 2016;170(11):e162521. 10.1001/jamapediatrics.2016.2521. [DOI] [PubMed] [Google Scholar]
- 61.Gottlieb L, Hessler D, Long D, et al. Are acute care settings amenable to addressing patient social needs: a sub-group analysis. Am J Emerg Med. 2018;36(11):2108–2109. 10.1016/j.ajem.2018.03.034. [DOI] [PubMed] [Google Scholar]
- 62.Schickedanz A, Sharp A, Hu YR, et al. Impact of social needs navigation on utilization among high utilizers in a large integrated health system: a quasi-experimental study. J Gen Intern Med. 2019;34(11):2382–2389. 10.1007/s11606-019-05123-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.De Marchis EH, Torres JM, Benesch T, et al. Interventions addressing food insecurity in health care settings: a systematic review. Ann Fam Med. 2019;17(5):436–447. 10.1370/afm.2412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sokol R, Austin A, Chandler C, et al. Screening children for social determinants of health: a systematic review. Pediatrics. 2019;144(4):e20191622. 10.1542/peds.2019-1622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sandhu S, Xu J, Eisenson H, Prvu Bettger J. Workforce models to screen for and address patients’ unmet social needs in the clinic setting: a scoping review. J Prim Care Community Health. 2021;12:1–12. 10.1177/21501327211021021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Pinto AD, Hassen N, Craig-Neil A. Employment interventions in health settings: a systematic review and synthesis. Ann Fam Med. 2018;16(5):447–460. 10.1370/afm.2286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bickerdike L, Booth A, Wilson PM, Farley K, Wright K. Social prescribing: less rhetoric and more reality. a systematic review of the evidence. BMJ Open. 2017;7:e013384. 10.1136/bmjopen-2016-013384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Escobar ER, Pathak S, Blanchard CM. Screening and referral care delivery services and unmet health-related social needs: a systematic review. Prev Chronic Dis. 2021;18:e78. 10.5888/pcd18.200569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Oregon Primary Care Association. Empathic Inquiry. https://www.orpca.org/initiatives/empathic-inquiry. Accessed December 17, 2021.
- 70.Schleifer D, Diep A, Grisham K. It’s About Trust: Low-Income Parents’ Perspectives on How Pediatricians Can Screen for Social Determinants of Health. Public Agenda; 2019. https://www.publicagenda.org/wp-content/uploads/2019/08/itsAboutTrust_UHF_Final.pdf. Accessed December 17, 2021. [Google Scholar]
- 71.Rodriguez LS. Intersectionality framework for children with special healthcare needs: a scoping review. International Health Trends and Perspectives. 2021;1(3):315–327. [Google Scholar]
- 72.O’Gurek DT, Henke C. A practical approach to screening for social determinants of health. Fam Pract Manag. 2018;25(3):7–12. [PubMed] [Google Scholar]
- 73.Berry C, Paul M, Massar R, Marcello RK, Krauskopf M. Social needs screening and referral program at a large US public hospital system, 2017. Am J Public Health. 2020;110(S2):S211–S214. 10.2105/ajph.2020.305642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Petchel S, Gelmon S, Goldberg B. The organizational risks of cross-sector partnerships: a comparison of health and human services perspectives. Health Aff (Millwood). 2020;39(4):574–581. 10.1377/hlthaff.2019.01553. [DOI] [PubMed] [Google Scholar]
- 75.Castrucci B, Auerbach J. Meeting individual social needs falls short of addressing social determinants of health. Health Affairs Blog. January 16, 2019. https://www.healthaffairs.org/do/10.1377/hblog20190115.234942/full. Accessed December 17, 2021.
- 76.Kreuter M, Garg R, Thompson T, et al. Assessing the capacity of local social services agencies to respond to referrals from health care providers. Health Aff (Millwood). 2020;39(4):679–688. 10.1377/hlthaff.2019.01256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wojcik O, Miller CE, Plough AL. Aligning health and social systems to promote population health, well-being, and equity. Am J Public Health. 2020;110(S2):S176–S177. 10.2105/ajph.2020.305831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lutfiyya MN, McCullough JE, Haller IV, Waring SC, Bianco JA, Lipsky MS. Rurality as a root or fundamental social determinant of health. Dis Mon. 2012;58(11):620–628. 10.1016/j.disamonth.2012.08.005. [DOI] [PubMed] [Google Scholar]
- 79.Leider JP, Meit M, McCullough JM, et al. The state of rural public health: enduring needs in a new decade. Am J Public Health. 2020;110(9):1283–1290. 10.2105/ajph.2020.305728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.De Marchis EH, Alderwick H, Gottlieb LM. Do patients want help addressing social risks? J Am Board Fam Med. 2020;33(2):170–175. 10.3122/jabfm.2020.02.190309.. [DOI] [PubMed] [Google Scholar]
- 81.Sundar KR. Universal screening for social needs in a primary care clinic: a quality improvement approach using the your current life situation survey. Perm J. 2018;22:18–089. 10.7812/tpp/18-089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Moon K, Blackman D. A guide to understanding social science research for natural scientists. Conserv Biol. 2014;28(5):1167–1177. 10.1111/cobi.12326. [DOI] [PubMed] [Google Scholar]
- 83.Bero LA. Improving the quality of systematic reviews in public health: introduction to the series. Am J Public Health. 2020;110(11):1601–1602. 10.2105/ajph.2020.305914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Noyes J, Booth A, Moore G, Flemming K, Tunçalp Ö, Shakibazadeh E. Synthesising quantitative and qualitative evidence to inform guidelines on complex interventions: clarifying the purposes, designs and outlining some methods. BMJ Glob Health. 2019;4:e000893. 10.1136/bmjgh-2018-000893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Cerigo H, Quesnel-Vallée A. Systematic mixed studies reviews: leveraging the literature to answer complex questions through the integration of quantitative and qualitative evidence. Int J Public Health. 2020;65:699–703. 10.1007/s00038-020-01386-3. [DOI] [PubMed] [Google Scholar]
- 86.Rhodes T, Lancaster K. Evidence-making interventions in health: a conceptual framing. Soc Sci Med. 2019;238:112488. 10.1016/j.socscimed.2019.112488. [DOI] [PubMed] [Google Scholar]
- 87.Victora CG, Habicht J-P, Bryce J. Evidence-based public health: moving beyond randomized trials. Am J Public Health. 2004;94(3):400–405. 10.2105/ajph.94.3.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Shannon-Baker P Making paradigms meaningful in mixed methods research. J Mix Methods Res. 2016;10(4):319–334. 10.1177/1558689815575861. [DOI] [Google Scholar]
- 89.Lindau ST, Makelarski JA, Abramsohn EM, et al. CommunityRx: a real-world controlled clinical trial of a scalable, low-intensity community resource referral intervention. Am J Public Health. 2019;109(4):600–606. 10.2105/ajph.2018.304905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Tung EL, Abramsohn EM, Boyd K, et al. Impact of a low-intensity resource referral intervention on patients’ knowledge, beliefs, and use of community resources: results from the CommunityRx Trial. J Gen Intern Med. 2020;35(3):815–823. 10.1007/s11606-019-05530-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.