Abstract
Background
Severe early childhood caries (SECC) is an inflammatory disease with complex pathology. Although changes in the oral microbiota and metabolic profile of patients with SECC have been identified, the salivary metabolites and the relationship between oral bacteria and biochemical metabolism remains unclear. We aimed to analyse alterations in the salivary microbiome and metabolome of children with SECC as well as their correlations. Accordingly, we aimed to explore potential salivary biomarkers in order to gain further insight into the pathophysiology of dental caries.
Methods
We collected 120 saliva samples from 30 children with SECC and 30 children without caries. The microbial community was identified through 16S ribosomal RNA (rRNA) gene high-throughput sequencing. Additionally, we conducted non-targeted metabolomic analysis through ultra-high-performance liquid chromatography combined with quadrupole time-of-flight mass spectrometry to determine the relative metabolite levels and their correlation with the clinical caries status.
Results
There was a significant between-group difference in 8 phyla and 32 genera in the microbiome. Further, metabolomic and enrichment analyses revealed significantly altered 32 salivary metabolites in children with dental caries, which involved pathways such as amino acid metabolism, pyrimidine metabolism, purine metabolism, ATP-binding cassette transporters, and cyclic adenosine monophosphate signalling pathway. Moreover, four in vivo differential metabolites (2-benzylmalate, epinephrine, 2-formaminobenzoylacetate, and 3-Indoleacrylic acid) might be jointly applied as biomarkers (area under the curve = 0.734). Furthermore, the caries status was correlated with microorganisms and metabolites. Additionally, Spearman's correlation analysis of differential microorganisms and metabolites revealed that Veillonella, Staphylococcus, Neisseria, and Porphyromonas were closely associated with differential metabolites.
Conclusion
This study identified different microbial communities and metabolic profiles in saliva, which may be closely related to caries status. Our findings could inform future strategies for personalized caries prevention, detection, and treatment.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12903-023-02722-8.
Keywords: SECC, Saliva, Microbiome, Metabolome, Biomarkers
Background
Dental caries is among the most common chronic childhood diseases, affecting > 560 million children worldwide [1]. Early childhood caries (ECC) is defined as the presence of caries in children aged < 6 years of age. Further, severe ECC (SECC) is defined as any sign of smooth-surface caries in children < 3 years of age, and from ages 3 through 5, one or more cavitated, missing (due to caries), or filled.
smooth surfaces in primary maxillary anterior teeth or a decayed, missing, or filled score of ≥ 4 (age 3), ≥ 5 (age 4), or ≥ 6 (age 5) surfaces constitute S-ECC [2]. The prevalence of ECC in developed and developing countries is 1–12% and up to 70%, respectively [3]. Additionally, ECC is more prevalent in lower social income groups [4, 5]. A Chinese oral epidemiological survey conducted in 2018 found that the prevalence of dental caries in the milk teeth of 5-year-old children was 71.9%, which indicated a ≈ 6% increase compared with that reported 10 years ago; further, the untreated rate was as high as 95.9% [6].
The severe effects of SECC on masticatory function may cause height and weight deficits in children [7], which results in various adverse physical and psychological effects. Moreover, SECC reduces the overall quality of life and imposes a huge economic burden on families and society [8, 9]. Therefore, there is a need to elucidate the underlying mechanism and develop relevant biomarkers for early personalized prevention, diagnosis, and treatment of caries [10].
The oral microbiota is among the most complex microbiotas in the human body, with > 700 bacterial species present [11]. Due to the limitations of microbiological research, Streptococcus mutans and Lactobacillus have been long considered the specific pathogens for ECC. However, from an ecological perspective, ECC is now considered to arise when environmental disturbances alter the oral microbiota balance. Eventually, caries-causing bacteria predominate, resulting in demineralization and decomposition of dental tissue [12–14].
Variations in oral microbiota among different ecological niches as well as interactions within and outside the host during ECC development remain unclear. Saliva is considered an important medium for reflecting individual oral microbial characteristics and various disease states [15]. There are significant differences in the salivary microbial community between caries hosts and caries-free hosts [16, 17], with several studies exploring possible biomarkers [18–20]. The application of metabolomics techniques has facilitated the identification of small molecule metabolites that partly reflect the metabolic profile of the flora and are used to identify disease-related biomarkers. Metabolomics techniques have recently become increasingly sophisticated and have been used in studies on dental caries [21], periodontitis [22], and oral cancer [23]. However, only a few studies have investigated childhood caries, mainly involving plaque [24] and saliva [25]. A study on the salivary nuclear magnetic resonance (NMR) metabolome of children under different conditions suggested that non-stimulated salivary metabolomics may present the metabolite profile of caries [26]. However, most studies have conducted independent microbiome analyses. Additionally, although several studies have demonstrated differences in flora according to the disease states, the microbial interactions remain unclear.
To our knowledge, no studies have applied a multi-omics approach to explore salivary microbial interactions in the caries state. We aimed to identify microbial communities and metabolic profiles in children with and without SECC by combining high-throughput sequencing of 16S ribosomal RNA (rRNA) genes and untargeted metabolomics through ultra-high performance liquid chromatography combined with quadrupole time-of-flight mass spectrometry (UHPLC-Q/TOF–MS). Additionally, we aimed to explore salivary biomarkers for caries status and the possible mechanisms of microbial interactions in order to inform future strategies for the prevention and diagnosis of caries in children.
Materials and methods
Study population and clinical examination
This study was approved by the Ethics Committee of Hebei Children's Hospital (No. 207). All legal guardians of participating children were provided written informed consent following the Declaration of Helsinki. In June 2020, the Department of Stomatology of Hebei Children's Hospital enrolled 60 children in a kindergarten under the jurisdiction of Shijiazhuang, including 30 children with SECC (SECC group) and 30 children without caries (Group CF). The inclusion criteria were as follows: local kindergarten students in Shijiazhuang, no history of long-term (> 3 months) relocation; no use of antibiotics, antibacterial mouthwash, or toothpaste use within 1 month; no orthodontic devices; no systemic diseases; no oromandibular system abnormalities and salivary gland diseases; and no irritable or restless behaviour during examination or sample collection. A single physician clinically examined the caries status of the children under natural light based on the World Health Organization guidelines and records regarding the child's sex, age, ethnicity, caries status, etc.
Sample collection
The participants and their guardians were instructed not to perform oral care (brushing and flossing) in the morning on the day of sample collection and not to eat or drink for 2 h before sample collection. Sample collection was performed in the morning (9:30 a.m. to 10:00 a.m.) by four paediatric dentists and six kindergarten teachers (for emotional reassurance of young children). Specifically, after mouth rinsing with distilled water, approximately 3 mL of non-irritating saliva was collected in a quiet state using a sterile 50 ml centrifuge tube. Subsequently, samples were stored in two separate 1.5 mL Eppendorf tubes using sterile pipettes, immediately placed in an insulated box filled with dry ice, and transported to the laboratory for storage at -80 °C before further processing. One sample was used for 16SrRNA sequencing and the other for metabolic assessment. The successful sample collection rate was 100%.
Sample preparation and 16S rRNA gene sequencing
Genomic DNA extraction and PCR amplification
The genomic DNA of the samples was first extracted using the CTAB/SDS method, the DNA purity and concentration were checked using agarose gel electrophoresis. DNA was diluted as per the concentration l μg/μL using sterile water.
Using the diluted genomic DNA as template, the 16S V3-V4 sequencing region was selected and PCR was performed using specific primers (341F CCTAYGGGRBGCASCAG and 806R GGACTACNNGGGTATCTAAT). All PCR reactions were carried out with 15µL of Phusion® High-Fidelity PCR Master Mix (New England Biolabs). The PCR reaction procedure was as follows: 98 °C pre-denaturation for 1 min; 30 cycles including (98 °C, 10 s; 50 °C, 30 s; 72 °C, 30 s); 72 °C, 5 min.
Mixing and purification of PCR products
The PCR products were detected by electrophoresis using 2% concentration of agarose gel; the resulting products were purified by magnetic beads, quantified by enzyme labelling, and then mixed in equal amounts according to the concentration of PCR products. Then, they were mixed thoroughly and detected by electrophoresis using a 2% agarose gel. The products were recovered using Qiagen gel recovery kit (Qiagen, Germany) for the target bands.
Library construction and sequencing
Libraries were constructed using TruSeq® DNA PCR-Free Sample Preparation Kit (Illumina, USA) library construction kit, and the constructed libraries were quantified by Qubit® 2.0 Fluorometer (Thermo Fisher, USA) and Q-PCR; subsequently, the libraries were sequenced using NovaSeq6000 (Illumina, USA) and 250 bp paired-end reads were generated. Sequence are processed using the Tags quality control process from QIIME (Version 1.9.1, http://qiime.org/scripts/split_libraries_fastq.html). The UPARSE algorithm was applied to analyze the sequences (UPARSE v7.0.1001, http://www.drive5.com/uparse/). Sequences with ≥ 97% similarity were assigned to the same operational taxonomic units (OTUs). The abundance information of the OTUs was normalized using a standard of sequence number corresponding to the sample with the least number of sequences. The subsequent computation of alpha and beta diversities was performed using QIIME (Version 1.9.1) (Additional file 1).
Metabolome sample preparation and testing conditions
Sample preparation
The samples were sent to the laboratory for centrifugation at 13,500 r/min at 4 °C for 10 min. The supernatant was removed, dispensed and stored at -80 °C. The samples were removed from the -80 °C refrigerator at the beginning of the experiment and thawed; 100 μL of acetonitrile was added to 50 μL of the saliva sample, vortexed for 30 s at 15,000 r/min, and centrifuged at 4 °C for 10 min; this process was performed again. The supernatant was used for analysis. Three different types of samples were used during the sample analysis, including the blank solution, quality control sample, and real sample. The injection order of the samples can have a significant impact on the experimental results. Therefore, the injection sequence in each model was varied. The blank solution and QC sample were sequentially injected five times and six times, respectively. After that, the random sampling method was performed in the real sample analysis process and one blank solution and one QC sample were inserted into every eight real samples. The blank solution was a 95% acetonitrile solution to balance the system. The QC was used to evaluate the precision of the instrument before the analysis process and to evaluate whether the experimental condition was stable from the first real sample to the last one in each analysis model. It was separately prepared, pooled, and separately mixed with the same volume of six randomly selected processed real samples.
Testing conditions
An AB SCIEX Q-TOF 5600 + triple quadrupole-time of flight mass spectrometer with Shimadzu LC-30A ultra performance liquid chromatograph (Kyoto, Japan) and Triple-TOFTM5600 + mass spectrometer (AB SCIEX, USA) was used. Since saliva contains approximately 99% water, many endogenous metabolites were expected to be highly polar. HILIC columns have excellent separation capabilities for the analysis of strongly polar endogenous substances, while HSS T3 columns target substances with low to medium polarity. The liquid phase part was separated using a hydrophilic (HILIC) column and a reversed-phase (HSS T3) column, and the mass spectrometry part was acquired in full scan mode using an ESI source in the positive ion mode. The experiments were divided into two modes HILIC ( +) mode and HSS T3 ( +) mode. The hydrophilic column was ACQUITY UPLC® BEH HILIC (2.1 × 100 mm, 1.7 μm), and the mobile phases included 10 mM aqueous ammonium acetate (A) and acetonitrile (B) with gradient elution. The elution procedure was as follows: 0–2 min, 95–95% B; 2–8 min, 95–75% B; 8–9.5 min, 75–55% B; 9.5–10 min, 55–95% B; 10–15 min, 95–95% B; flow rate: 0.3 mL/min; column temperature: 35.00 °C; injection volume 5 μL; sample chamber temperature: 4 °C. The reversed-phase column was an ACQUITY UPLC® HSS T3 (2.1 × 100 mm, 1.8 μm) with the mobile phases of 1‰ formic acid-5 mM aqueous ammonium acetate (A) and acetonitrile (B), and the gradient elution program was as follows: 0–2 min, 10–50%; 2–9.5 min, 50–95% B; 9.5–10 min, 95–10% B 10–15 min, 10–10% B; flow rate: 0.3 mL/min; column temperature: 35.00 °C; injection volume 5μL; sample chamber temperature: 4 °C.
Mass spectrometry conditions in positive ion mode: ion source, ESI source; full scan mode acquisition. MS1 conditions: acquisition range, 100–1000 Da; nebulizing gas (Gas 1), 55 psi; heating gas (Gas 2), 55 psi; curtain gas (CUR), 35 psi; temperature (TEM), 550 °C; source injection voltage (IVF), 5500 V; declustering Information-dependent acquisition (IDA): MS2 acquisition of the eight most responsive peaks above 50 cps, with dynamic background subtraction (DBS) turned on. MS2 conditions: acquisition range, 50–1000 Da; DP, 50 V; CE, 30 eV; collision energy expansion (CES), 15 eV. The experimental procedure was performed using automatic calibration (CDS).
Statistical analysis
The 16S rRNA sequence data were analysed using the QIIME software package (Version 1.9.1) to calculate the Ace, chao1 and Shannon indices for assessing alpha diversity. Analysis of variance was performed using Student’s t-test. Additionally, cumulative box plots of species were plotted using R software (Version 2.15.3). Additionally, beta-diversity analysis was performed using R software to plot weighted/unweighted UniFrac distance metrics, principal coordinate analysis (PCoA) plots, and nonmetric multidimensional scaling (NMDS) plots based on operational taxonomic unit (OTU) levels. PCoA was performed using the WGCNA, stats, and ggplot2 packages of R software. Further, NMDS analysis was performed using the vegan package of R software. Metastats analysis was conducted using R software at each classification level (Phylum, Class, Order, Family, Genus, Species) through between-group permutation tests to obtain p values, which were visualized as violin plots. We performed analysis of similarity (ANOSIM), multi-response permutation procedure (MRPP), and ADONIS (permutational multivariate analysis of variance) analysis using the R vegan package's anosim function, mrpp function, and adonis function. R software based on the analysis of species abundance can be used to perform a random forest model, Significant species were screened by MeanDecreaseAccuracy and MeanDecreaseGin, after which cross-validation (default tenfold) was done for each model and ROC curves were plotted.
The raw data for the MS downcomers were acquired using Analyst TF 1.6 software (AB SCEIX, USA) and converted to mzML format through ProteoWizard using the XCMS program (http://www.bioconductor.org/packages/release/bioc/html/ xcms.html). We performed peak extraction, alignment, and retention time correction. Peak areas were corrected using the "SVR" method; moreover, peaks with > 50% deletion rate in each sample group were filtered. After calibration and filtering, peaks were identified by querying the laboratory's database, integrating public libraries, and mtDNA method. All statistical analyses, which included univariate and multivariate statistical analyses, were conducted using R software (Version 2.15.3). Univariate statistical analysis included multiplicative analysis of variance while multivariate statistical analysis included principal component analysis (PCA) and orthogonal partial least squares discrimination analysis (OPLS-DA). The quality of the OPLS-DA was evaluated by the values of R2X or R2Y and Q2.We performed differential metabolite enrichment analyses using the KEGG database (KEGG, http://www.genome.jp/kegg) and MetaboAnalyst 3.0 (Montreal, QC, Canada). Values for the area under the curve (AUC) of the ROC were used to assess the diagnostic utility of candidate metabolites for SECC.
We analysed the relationships among microbial communities, metabolites, and clinical indicators through Spearman’s correlation analysis and drew the heat maps. Spearman was performed with R software (R package = psych).
Results
Microbial profiles of saliva samples
The physiological indicators including age and sex of the participants are known to affect experimental results. The Wilcoxon Rank Sum test and Chi-squared test were used to access whether age and sex affected the experimental grouping result. There were no significant between-group differences in age or sex (Table 1).
Table 1.
Demographic and clinical characteristics of the subjects
| Clinical parameters | SECC | Caries-free |
|---|---|---|
| Age (month)a | 58.57 ± 9.58 | 51.63 ± 9.95 |
| Sexb | ||
| Male | 16 | 17 |
| Female | 14 | 13 |
| Caries status | ||
| dmft | 8.83 ± 2.63 | 0 |
| dmfs | 14.83 ± 4.44 | 0 |
aRepresented as mean ± standard deviation, No significance between SECC
group and caries-free group (p > 0.05), by Wilcoxon Rank Sum test
bNo significance between SECC group and caries-free group (p > 0.05), by
Chi-squared test
A total of 120 saliva samples were collected, with 60 being for 16S rRNA gene sequencing. A total of 3,871,616 high-quality sequences were obtained, and the average number for each sample was 62,527. Sequence clustering yielded 2877 OTUs, which involved 42 phyla, 90 classes, 190 orders, 300 families, and 513 genera.
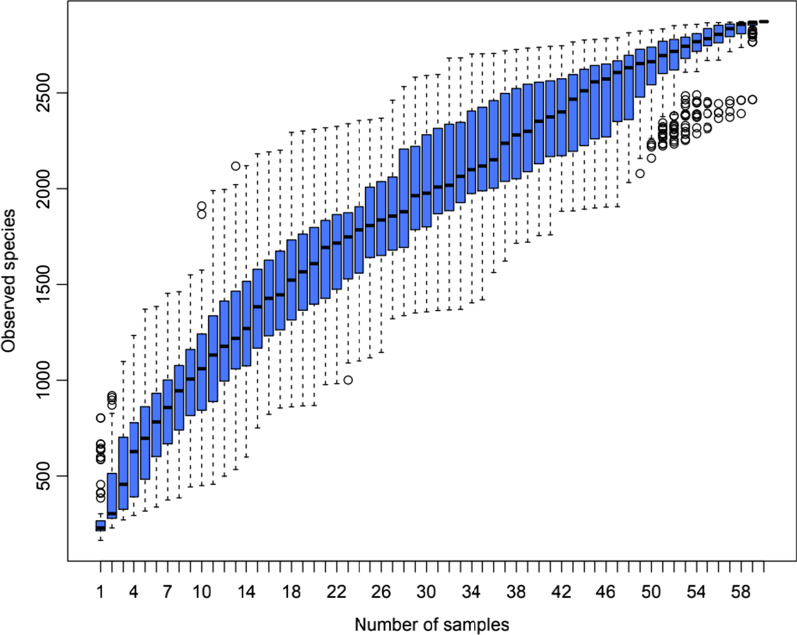
The species accumulation box plot reflects the rate of emergence of new OTUs (new species) with continuous sampling. The box plot position levelled off with increasing sample size, which indicated that the sampling depth could reflect the flora of salivary microorganisms (Fig. 1).
Fig. 1.
Species Accumulation Box Plot for Children with and without SECC
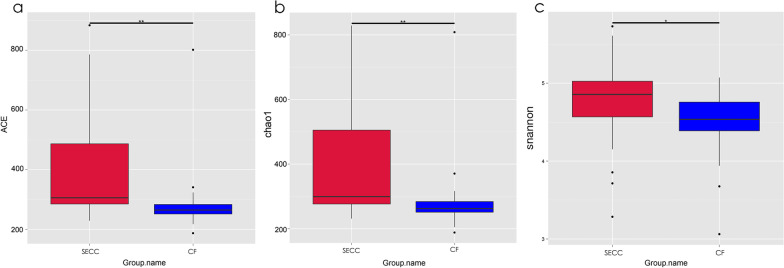
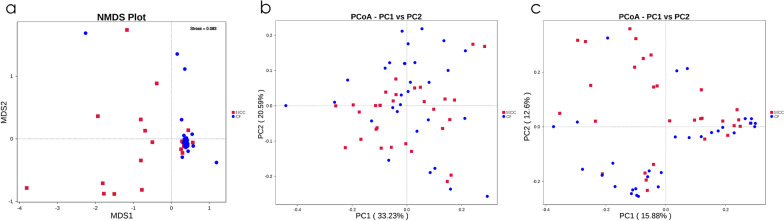
We used the alpha and beta diversity of the microbial community to further analyse its overall compositional richness and structural characteristics. Compared with the CF group, the SECC group showed significantly larger Alpha-diversity indices, including the abundance-based coverage estimator (ACE, p < 0.01), chao1 index (p < 0.01) and Shannon index (p < 0.05), which indicated a higher richness and diversity of salivary microbial communities (Fig. 2a–c). Beta-diversity analysis using OTUs in NMDS analysis, as well as PCoA analysis based on the weighted and unweighted Unifrac distance, revealed between-group differences in microorganisms (Fig. 3a–c). Moreover, the non-parametric statistical methods, including ANOSIM, ADONIS, and MRPP, revealed significant between-group differences in the overall biotope structures (all p < 0.05).
Fig. 2.
Alpha-diversity of bacterial communities of severe early childhood caries (SECC) and caries-free subjects (CF). Microbiota alpha-diversity as calculated by abundance-based coverage estimator (ACE) index (a), chao1 index (b) and shannon index (c) of saliva samples in both groups. *p < 0.05, **p < 0.01
Fig. 3.
Beta-diversity of saliva samples in two groups. Nonmetric multidimensional scaling (NMDS) (a), as well as principal coordinates analysis (PCoA) of the unweighted (b) and weighted UniFrac distance (c), were performed based on the operational taxonomic unit (©) abundances
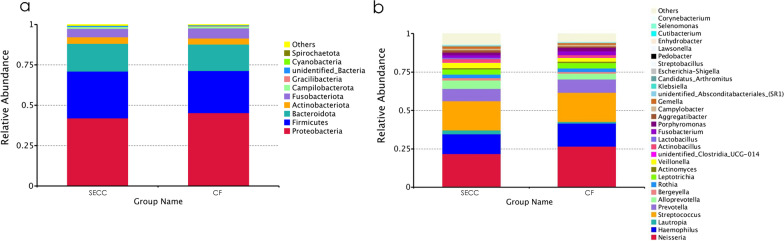
The five most abundant species under both groups at the phylum level were Proteobacteria, Firmicutes, Bacteroidota, Actinobacteriota, and Fusobacteriota, which accounted for > 97% of the total sequences (Fig. 4a).
Fig. 4.
Bacterial compositions in the SECC and CF groups. Relative abundance of bacterial composition at the phylum level (a) and genus level (b) of saliva samples in the SECC and CF groups
The top five most abundant species in both groups at the genus level were Neisseria, Streptococcus, Haemophilus, Prevotella, and Alloprevotella which accounted for > 64% of the total sequences (Fig. 4b).
Regarding Metastats analysis at the phylum and genus levels, there were between-group differences in the abundance of 8 phyla and 32 genera (relative abundance > 0.01%).
At the phylum level, the relative abundance of Firmicutes, Cyanobacteria, Acidobacteriota, Methylomirabilota, Chloroflexi, Gemmatimonadetes, and Myxococcota was significantly higher in the SECC group than in the CF group. Moreover, the relative abundance of Gracilibacteri was significantly higher in the CF group than in the SECC group (Additional file 2: Fig. S1).
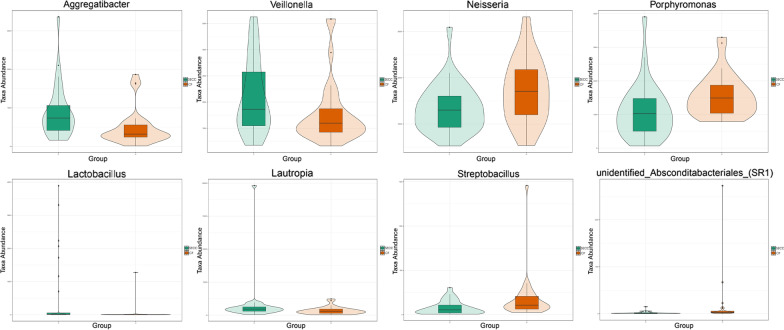
The top eight taxa with the highest between-group differences in abundance at the genus level are presented as violin plots to visualize the distribution characteristics of the data. Lautropia, Veillonella, Lactobacillus, and Aggregatibacter were significantly enriched in the SECC group than in the CF group. Contrastingly, Neisseria, Porphyromonas,unidentified_Absconditabacteriales_(SR1), and Streptobacillus were lower in the SECC group than in the CF group (Fig. 5).
Fig. 5.
Taxon abundances at the genus levels were compared between the SECC and CF groups using Metastats. The violin plots show the top eight genera with significant between-group differences
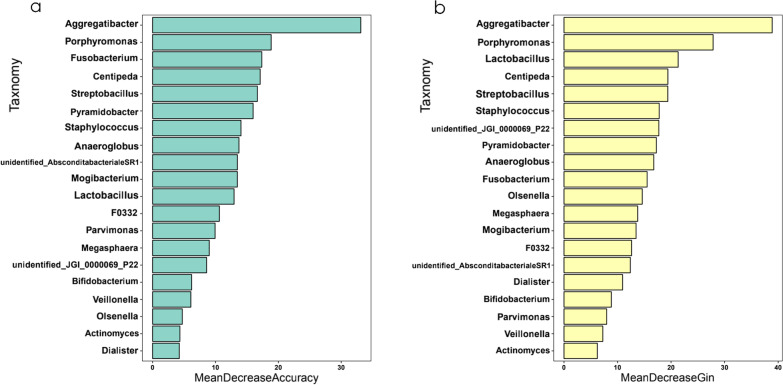
For further sample analysis using a random forest machine learning approach, we constructed a prediction model based on two parameters (MeanDecreaseAccuracy and MeanDecreaseGin20; Fig. 6a, b). The experimental analysis was performed at genus level including 513 genera. MeanDecreaseAccuracy is the degree of reduction in the predictive accuracy of a random forest by taking the value of a variable and turning it into a random number ( larger values indicate a greater importance of the variable.) MeanDecreaseGin calculates the effect of each variable on the heterogeneity of observations at each node of the classification tree, and thus compares the importance of the variables (larger values indicate a greater importance of the variable) to filter out important species. Additionally, we verified that the maximum AUC was 85.71% when 20 microorganisms were selected, which allowed satisfactory between-group distinction (Additional file 3: Fig. S2).
Fig. 6.
The random forest model was constructed for the genus taxonomic level. The important 20 species were screened by MeanDecreaseAccuracy (a) and MeanDecreaseGin (b)
Shifts in the metabolomic profiles of saliva samples
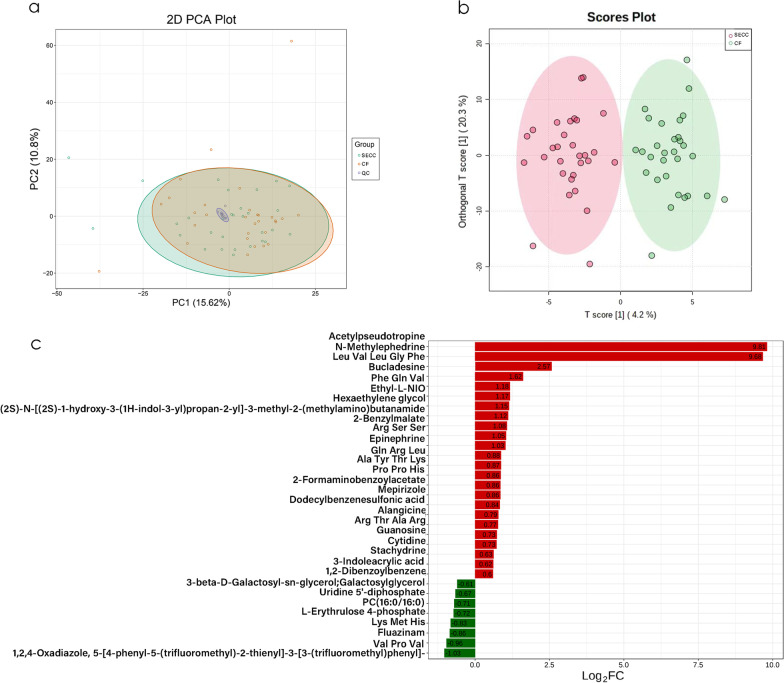
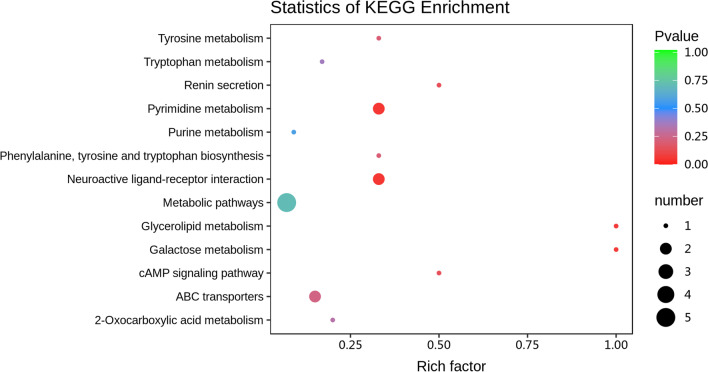
To investigate changes in salivary metabolomics under SECC and their relationship with microbial changes, we performed untargeted metabolomics using 60 saliva samples. A total of 356 qualifiable metabolites were used in the subsequent analysis after removing internal standards and false positive peaks as well as combining peaks of the same metabolites. The experimental, control, and quality control samples in the PCA showed good aggregation. Moreover, the pre-treatment and experimental conditions for each shot were stable, which indicated that the sample data was reliable in this analytical mode (Fig. 7a). There was a clear between-group distinction in the model established using OPLS-DA; moreover, evaluation of the model quality using the 200 permutation test revealed reliable prediction and modelling ability (Additional file 4: Fig. S3), with significant alterations of the metabolic substances in the SECC group (Fig. 7b). A total of 32 differential metabolites were yielded in the HILIC (+) and HSS T3 (+) analysis models based on the criteria of a fold change ≥ 1.5 or ≤ 0.67 and VIP > 1. Among the differential metabolites, 24 and 8 were significantly upregulated and downregulated, respectively (Fig. 7c). Cytidine, 3-indoleacrylic acid, 2-formaminobenzoylacetate, guanosine, stachydrine epinephrine, Ala-Tyr-Thr-Lys, Arg-Ser-Ser, and Pro-Pro-His were significantly increased in the SECC group. Contrastingly, L-erythrulose 4-phosphate, galactosylglycerol, PC(16:0/16:0), Lys-Met-His, fluazinam, uridin’ 5'-diphosphate, Val-Pro-Val, and 1,2,4-oxadiazole were significantly increased in the CF group. These compounds are listed in Fig. 7c and table 2. Next, we used the KEGG database annotation to hierarchically classify the differential metabolites according to their involvement in the KEGG metabolic pathway. Subsequently, we performed an enrichment analysis of the differential metabolites in the KEGG pathways to identify the related metabolic pathways [27]. We identified several metabolic pathways of the differential salivary metabolites associated with dental caries, including tryptophan metabolism, pyrimidine metabolism, purine metabolism, ABC transporters, tyrosine metabolism, cAMP signalling pathway, renin secretion, galactose metabolism, phenylalanine, tyrosine and tryptophan biosynthesis (Fig. 8). Additionally, there was enrichment of intermediate metabolites such as epinephrine (neuroactive ligand-receptor interactions, renin secretion), guanosine (ABC transporters, purine metabolism), and 2-benzylmalate (phenylalanine, tyrosine and tryptophan biosynthesis, and 2-carbonylformate metabolism).
Fig. 7.
Between-group differences in the metabolic profiles. Principal component analysis (PCA) (a) and OPLS-DA analysis (b) of the salivary metabolic profiles. Values of log2 (FC) after between-group comparison (c). Positive and negative Log2 (FC) values indicate a relatively higher concentration in the SECC and CF groups, respectively
Table 2.
Details of the differential metabolites between the SECC and CF groups
| Compounds | Formula | VIP | Log2FC | Type |
|---|---|---|---|---|
| Acetylpseudotropine | C10H17NO2 | 1.35 | 9.81 | Up |
| 3-Indoleacrylic acid | C11H9NO2 | 1.98 | 0.62 | Up |
| 2-Formaminobenzoylacetate | C10H9NO4 | 2.15 | 0.86 | Up |
| Cytidine | C9H13N3O5 | 1.66 | 0.73 | Up |
| Guanosine | C10H13N5O5 | 2.30 | 0.73 | Up |
| Stachydrine | C7H13NO2 | 1.07 | 0.63 | Up |
| Epinephrine | C9H13NO3 | 1.77 | 1.03 | Up |
| Ala Tyr Thr Lys | C22H35N5O7 | 2.12 | 0.87 | Up |
| Arg Ser Ser | C12H24N6O6 | 2.06 | 1.05 | Up |
| Pro Pro His | C16H23N5O4 | 2.03 | 0.86 | Up |
| L-Erythrulose 4-phosphate | C4H9O7P | 1.35 | − 0.72 | Down |
| Phe Gln Val | C19H28N4O5 | 1.87 | 1.18 | Up |
| Mepirizole | C11H14N4O2 | 2.56 | 0.86 | Up |
| 3-beta-D-Galactosyl-sn-glycerol;Galactosylglycerol | C9H18O8 | 1.32 | − 0.61 | Down |
| N-Methylephedrine | C11H17NO | 1.36 | 9.68 | Up |
| Dodecylbenzenesulfonic acid | C18H30O3S | 2.00 | 0.84 | Up |
| Gln Arg Leu | C17H33N7O5 | 1.93 | 0.88 | Up |
| Arg Thr Ala Arg | C19H38N10O6 | 2.02 | 0.77 | Up |
| PC(16:0/16:0) | C40H75NO9 | 1.06 | − 0.71 | Down |
| Lys Met His | C17H30N6O4S1 | 1.51 | − 0.83 | Down |
| Leu Val Leu Gly Phe | C28H45N5O6 | 1.42 | 2.57 | Up |
| Alangicine | C28H36N2O5 | 2.00 | 0.79 | Up |
| 2-Benzylmalate | C11H12O5 | 1.24 | 1.08 | Up |
| Hexaethylene glycol | C12H26O7 | 2.16 | 1.15 | Up |
| Ethyl-L-NIO | C9H19N3O2 | 1.90 | 1.17 | Up |
| (2S)-N-[(2S)-1-hydroxy-3-(1H-indol-3-yl)propan-2-yl]-3-methyl-2-(methylamino)butanamide | C17H25N3O2 | 2.27 | 1.12 | Up |
| Bucladesine | C18H24N5O8P | 2.23 | 1.62 | Up |
| Val Pro Val | C15H27N3O4 | 1.60 | − 0.96 | Down |
| 1,2,4-Oxadiazole, 5-[4-phenyl-5-(trifluoromethyl)-2-thienyl]-3-[3-(trifluoromethyl)phenyl]- | C20H10F6N2OS | 1.43 | − 1.03 | Down |
| Uridine 5'-diphosphate | C9H14N2O12P2 | 1.23 | − 0.67 | Down |
| 1,2-Dibenzoylbenzene | C20H14O2 | 1.93 | 0.60 | Up |
| Fluazinam | C13H4Cl2F6N4O4 | 1.33 | − 0.86 | Down |
Fig. 8.
KEGG enrichment plots of the differential metabolites. The rich factor represents the ratio of the number of differential metabolites in the corresponding pathway to the total number of metabolites annotated in the pathway, with larger values indicating greater enrichment. A smaller p value indicates a more significant enrichment
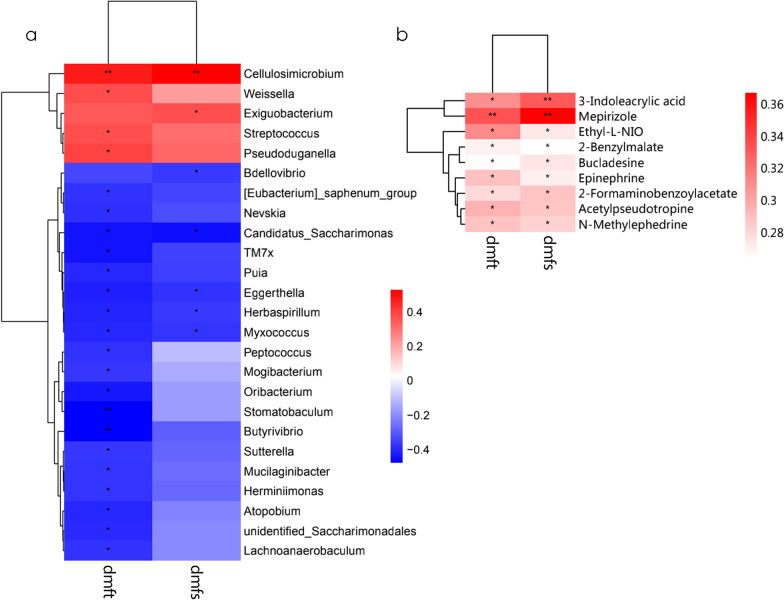
Correlations of the microbiota and metabolites with the clinical indices for caries
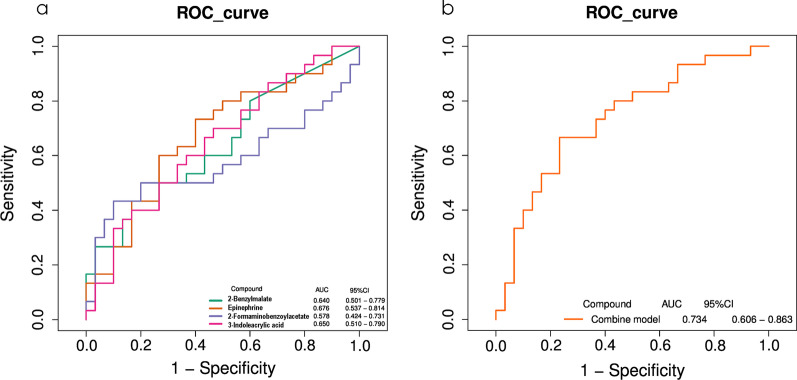
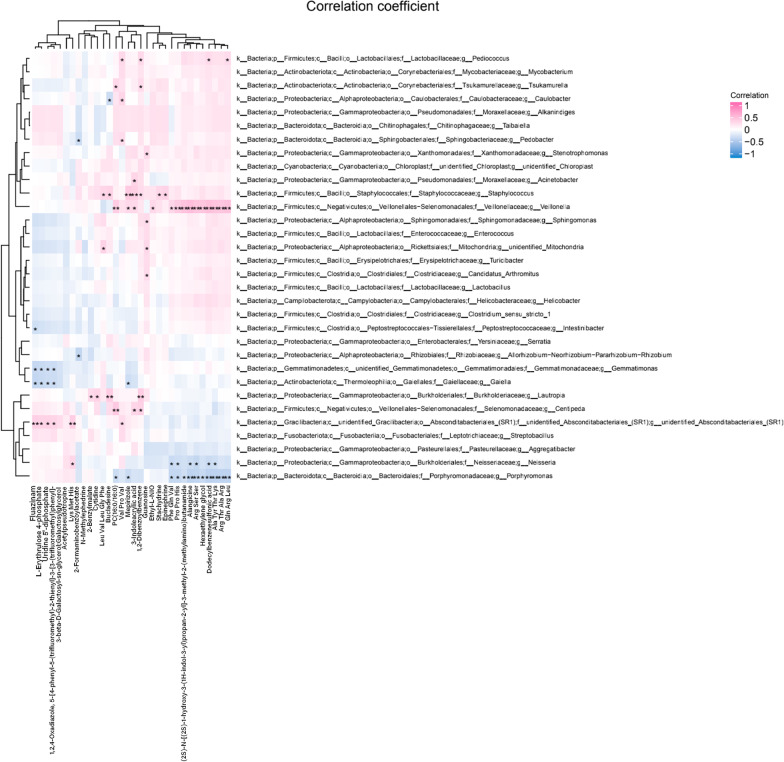
We found that 25 genera were significantly correlated with at least one of the clinical datasets (Fig. 9a). Known caries-related genera, including Streptococcus and Weissella, were positively correlated with caries status, while Eggerthella, Sutterella, Peptococcus, and Atopobium were negatively correlated with clinical indices. These findings suggest that alterations in some salivary flora may be related to clinical indices in children. Regarding the metabolome, nine differential metabolites were positively correlated with clinical data, which suggests a close association between salivary metabolites and dental caries given the abundance and diversity of microorganisms in the SECC group (Fig. 9b). Among the aforementioned metabolites, we included four endogenous metabolites in the ROC analysis, including 2-benzylmalate, epinephrine, 2-formaminobenzoylacetate, and 3-indoleacrylic acid. They demonstrated moderate predictive power (AUC = 0.734), and thus could be potential biomarkers of the inflammatory status (Fig. 10). To further explore the correlation between salivary microbial alterations and metabolite changes, we examined the correlations between phylum and genus with between-group differences and 32 metabolites. The metabolites were correlated with five phyla, including Gracilibacteria, Firmiutes, Acidobacteriota, Methylomirabilota, and Myxococcota (Additional file 5: Fig. S4). Moreover, 20 genera were correlated with metabolites. Among them, Veillonella, Staphylococcus, Neisseria, and Porphyromonas showed the most extensive correlations with metabolic differentials; specifically, they were correlated with 7, 14, 7, and 13 differential metabolites, respectively. Moreover, Veillonella and Staphylococcus showed significant positive correlations with the metabolites, while Neisseria and Porphyromonas showed negative correlations with the metabolites (Fig. 11).
Fig. 9.
A heat map showing the correlations among the microbiota and clinical indices (only genera significantly correlated with at least one clinical index [p < 0.05] are shown). *Significant correlation between the genera and clinical indices (*p < 0.05, **p < 0.01) (a). Heat map of clinical indices correlated with differential metabolites. Spearman’s rank correlation coefficients between two clinical indices and nine differential metabolites. All nine metabolites were upregulated in the SECC group. * indicates a significant correlation between the metabolites and clinical indices (*p < 0.05, **p < 0.01) (b)
Fig. 10.
Receiver operating characteristic (ROC) curve of four differential metabolites (a). 2-Benzylmalate, epinephrine, 2-formaminobenzoylacetate, and 3-indoleacrylic acid were selected and validated as putative biomarkers, with an area under the curve (AUC) of 0.734 (b)
Fig. 11.
Correlations between microbiota (genus level) and metabolites in saliva. Each row and column in the graph represents a metabolite and genus, respectively, while each lattice represents a correlation coefficient between a component and a metabolite. Red and blue represent positive and negative correlations, respectively. *Indicates a significant correlation between the genera and metabolites (*p < 0.05, **p < 0.01)
Discussion
We used 16SrRNA gene sequencing and UHPLC-Q/TOF–MS untargeted metabolomics to assess and compare differential salivary microbiota and their metabolites in children with and without SECC. We screened for potential microbial and metabolite markers for caries in children and investigated the mechanisms underlying changes in the oral microbial ecosystem in SECC.
Microbiome
Dental caries is caused by various microorganisms rather than a specific bacterium. Specifically, it is caused by a complex interaction involving at least tens of bacteria [28, 29]. Differences in the composition of oral microorganisms can distinguish the caries status and can facilitate disease diagnosis and prognosis [30–32] as well as prediction of caries occurrence [33]. However, there remains no consensus regarding cariogenic microorganisms and functional composition.
The composition of the oral microbiota changes throughout the life span from newborns to young adults with mixed and permanent dentition to the elderly [34–36]; further, it differs according to sex [37].
A study on children aged 4–6 years showed that the plaque microbiota showed increased sensitivity to the host than saliva with age progression; moreover, the oral microbiota could distinguish the different age-related changes and identify caries occurrence in these children [38]. In our study, there were no between-group differences in age and sex; moreover, all participants were from a local kindergarten and belonged to the Han ethnicity.
The oral cavity is a highly heterogeneous ecosystem with “a healthy core microbiota" in children [39]. Compared with dental plaque, saliva has more microbial functional markers since microbiota attached to teeth and soft tissue surfaces continuously flow into saliva, which makes saliva a reservoir of the entire oral microbiota [40]. The microbial and metabolic compositions and pathways differ across ecological niches. The salivary microbiota is valuable for predictive modelling and has considerable practical advantages as a sampling site, especially for children with poor compliance.
We further investigated the microbiota data through alpha and beta diversity analysis. Compared with the CF group, the SECC group showed a significantly greater alpha index (ACE, chao1, p < 0.01 and Shannon, p < 0.05) than the CF group. This is indicated that children with SECC had a higher microorganism abundance and diversity than children without SECC, which is consistent with previous reports [38, 41]. Previous studies have demonstrated that only the flora structure, but not the salivary microbial communities, differ between children with and without SECC [42–44].
These findings suggest that the appearance of dental caries may be related to oral flora disorders, which should be further investigated. The observed between-group differences in the indices of community diversity (ANOSIM, MRPP, and ADONIS; p < 0.05) demonstrate that the significant alterations in the structure of the salivary microbial community contributed to caries occurrence. Regarding genus classification, Metastat analysis revealed significant between-group differences in the abundance of Neisseria, Lautropia, Lactobacillus, Porphyromonas, and Aggregatibacter (p < 0.05). A previous study reported that Neisseria was more abundant in CF children and could be a diagnostic biomarker [45], which is consistent with our findings. Additionally, a previous study found that Veillonella was more abundant in childhood caries and that its co-aggregation and adhesion with Streptococcus spp. promotes biofilm formation and metabolic synergistic growth [46]. However, our findings regarding the differential flora are only partially consistent with previous reports [34, 47]. This could be attributed to differences in the study methodology as well as the age, ethnicity, and regions of the participants. There may be similarities in the functional performance of the combinations of different strains, which demonstrates the need for related metabolomic studies. Furthermore, most differential strains were of species with low abundance, which is consistent with previous reports [48]. This suggests the dominant flora routinely defined in the oral cavity do not comprise the microbiome biomarkers or disordered flora related to caries development.
Additional screening of the species using a random forest machine learning algorithm [49] showed that the selection of 20 bacterial species yielded the largest ROC value (85.71%). Among these species, only six had an abundance < 1%, which further demonstrates the importance of low-abundance species in saliva as markers for oral caries.
Metabolome
To our knowledge, this is the first study to apply UHPLC-MS untargeted metabolomics to probe the salivary metabolomic profile of children with SECC and to combine this approach with microbiomics.
Metabolomic studies on caries have mainly applied NMR assays [50, 51], with only a few studies using MS [25]. NMR-based metabolomics techniques are widely used in non-targeted studies given their stability, high discrimination, and excellent reproducibility; however, NMR has an inherent disadvantage of low resolution [52].
Contrastingly, MS-based metabolomics allows highly selective and sensitive quantitative analysis, which facilitates the detection of low-molecular-weight compounds at concentrations below the range of nanogram per millilitre [53]. Additionally, since LC–MS allows optimized detection of each compound in a complex mixture, it facilitates improved separation of complex systems [54]. In our study, salivary metabolites, including amino and organic acids, were positively correlated with the bacterial load; furthermore, the oral microbiota significantly contributed to the salivary metabolome. The salivary metabolome can facilitate the diagnosis of conditions reflecting ecological dysbiosis [55]. In addition, the salivary metabolome composition is influenced by multiple physiological and environmental factors [56]. The inclusion of children as study participants allows circumvention of the effects of smoking, alcohol consumption, and complex organismal and oral environment. A previous NMR study showed that caries status, but not sex and dental stage, significantly affected the salivary metabolic profile [26]. Additionally, the salivary metabolic profile did not significantly differ between stimulated and unstimulated saliva. However, stimulation is expected to affect salivary composition since unstimulated saliva (resting state) is mainly secreted by the submandibular and sublingual glands, while stimulated saliva is mainly secreted by the parotid gland [57].
Previous metabolomic studies on bacterial plaque biofilms [24, 58] have suggested large differences in the two ectopic differential metabolites according to caries status, which is slightly inconsistent with our findings. This could be attributed to between-study differences in the ectopic flora, participants, experimental and statistical methods, saliva collection site in the oral cavity, and host circulating metabolites.
Carbohydrate metabolism
Oral microorganisms in children with caries can metabolize intrinsic carbohydrates through various pathways. Additionally, carbohydrate metabolism is closely related to caries occurrence and development. In our study, we observed metabolite pathway analysis revealed significant enrichment of galactose metabolism. Streptococcus mutans, which is the main pathogen in dental caries, shows highly complex galactose utilization [59, 60]. Galactose metabolism may be used as a marker for children at a high risk of caries risk [61] and is active in the gingival crevicular fluid in patients with periodontitis [62].
During caries development, excess carbohydrate levels can alter the local microenvironment and contribute to caries induction by related bacteria such as Streptococcus mutans [63].
Galactose metabolism by Streptococcus mutans mainly occurs in the plaque. Our findings of decreased galactose metabolite levels in the SECC group are inconsistent with previous reports by NMR metabolomic studies. This could be attributed to the fact that differences in the ingested carbohydrates and/or oral habits among participants may influence the measured carbohydrate levels. Therefore, our findings regarding carbohydrate metabolism should be treated with caution.
Organic acid metabolism
Unexpectedly, 2-benzylmalate was the only differential organic acid metabolite, which appears to be inconsistent with the acidic conditions contributing to surface demineralization of dental tissues, and thus caries production. Short-term salivary secretion may not allow sufficient accumulation of organic acids due to saliva removal as well as the saliva’s strong buffering and dilution capacity. This further demonstrates the large differences in the saliva metabolic changes within the two ecological niches. A study on the metabolic pathways involved in different oral hygiene practices suggested the involvement of 2-oxocarboxylic acid metabolism [64]. Previous studies have reported altered levels of lactate [50] and butyric acid [26], which is inconsistent with our findings. This could be attributed to differences in the experimental techniques or classes of bacteria fermentation.
Amino acid metabolism
We did not identify any differential amino acids, which is consistent with a previous study on salivary metabolomics [65]. However, we observed enrichment of tryptophan metabolism; tyrosine metabolism; and intermediates of phenylalanine, tyrosine, and tryptophan biosynthesis processes. This could be attributed to matrix collagen degradation in the dentin during caries development [66] as well as the hydrolysis of salivary proteins/peptides by protein-hydrolysing oral bacteria [67]. In saliva, there is complex mutual facilitation between the synthesis and metabolism of tryptophan and tyrosine.
Our finding of increased metabolism of tyrosine, which is an amino acid precursor for the synthesis of catecholamines such as epinephrine, norepinephrine, and dopamine, is consistent with previous reports [26]. Moreover, disrupted tyrosine metabolism may be closely related to aggressive periodontitis [68]. Additionally, the observed increased tryptophan synthesis is consistent with previous reports [47]. Disrupted tryptophan metabolism is also related to the development of oral ulcers [69]. Contrastingly, other studies have reported decreased phenylalanine levels in children with dental caries [51]. There are significant changes in aspartic acid, ornithine, arginine, and proline metabolism related to dental caries [25]. Differences in previous reports regarding the types and pathways of amino acids in saliva involved in caries, which have also been demonstrated in studies on periodontal metabolomics [62], suggest the need to focus on changes in the amino acid metabolic pathways rather than single metabolites.
Taken together, functions related to amino acid metabolism may be crucial in the oral microecology under caries conditions, which should be further investigated.
Other metabolic pathways and metabolites
ABC transporters mediate important substances, including carbohydrates, amino acids, proteins, lipids, and inorganic ions, crucially involved in biofilm formation [70]. The formation and maturation of plaque biofilm is a prerequisite for caries formation; accordingly, the salivary microecology undergoes changes that promote caries development.
A previous microbiomic study reported a correlation of SECC and recurrent caries with ABC transporters [71]. Accordingly, it is important to pay attention to further elucidate the role of ABC transporters in biofilm formation and function as a necessary condition for caries development.
Uridine 5'-diphosphate, cytidine, and guanosine were enriched in purine and pyrimidine metabolism, which is consistent with previous reports [26]. Moreover, a study on periodontitis reported increased hypoxanthine levels [72]. This suggests that oxidative stress and inflammation accelerate purine degradation. Pyrimidine metabolism is crucially involved in the synthesis, degradation, and interconversion of DNA, RNA, lipids, and carbohydrates. Pathogenic bacteria can use pyrimidine metabolism to potentially alter the metabolic activity of the hosts and create favourable conditions for themselves [73], and therefore affect the health of dental tissues.
Salivary epinephrine levels are correlated with the severity of periodontitis [74]. Moreover, enrichment analysis has demonstrated the involvement of increased epinephrine levels in the cAMP signalling pathway, which can regulate salivary amylase secretion [75, 76]. Amylase secretion contributes to reduced plaque acid produced by Streptococcus mutans, which dissolves the enamel and may be a biomarker for dental caries [77]. α-amylase is closely associated with dental caries; additionally, low α-amylase levels may promote the development of early childhood caries [78]. We observed upregulated levels of stachydrine, which has anti-inflammatory activity. In many Middle Eastern and African countries, Salvadora persica L. (toothbrush tree, Miswak) is used as a toothbrush, with its root being rich in stachydrine [79].
The remaining metabolic pathways such as glycerolipid metabolism and neuroactive ligand-receptor interaction are crucially involved in the pathogenesis of oral squamous carcinoma [80, 81]. Future studies should investigate their relationship with dental caries in children. We used ROC curves to assess the accuracy of salivary metabolites as biomarkers. In our study, we identified four metabolites that could be jointly used as biomarkers for SECC.
This study demonstrated that non-differential salivary microorganisms were related to caries severity and were mostly in the low-abundance species groups. This could be attributed to the following factors. First, saliva is not the site of caries occurrence; accordingly, caries occurrence is weakly correlated with salivary microorganisms. Second, our microbial sequencing depth may not have been sufficiently deep, and it would be better to draw conclusions at the species or strain level. Third, there is extensive heterogeneity in our ECC classification with respect to caries severity and intraoral distribution [82]. Further clarification of microbial roles should apply a combination of multi-omic approaches, including transcriptomics. The combined application of multi-omics may provide the most powerful diagnostic tool in studies on diseases [83].
Regarding metabolites, some differential metabolites were correlated with clinical data, which suggests the potential utility of salivary metabolites in dental caries research. Combined analysis of microorganisms and metabolites revealed significant correlations of most differential salivary microorganisms with metabolites. Specifically, Veillonella and Staphylococcus enriched in the SECC group as well as Neisseria and Porphyromonas enriched in the CF group were extensively correlated with metabolites. Most genera enriched in the SECC group were positively and negatively correlated with up-regulated and down-regulated metabolites, respectively, in the CF group. Opposite correlations were observed between genera enriched in the CF group and metabolites upregulated in the SECC group. Our findings confirm that host and oral microorganisms are closely connected and interact in the development of dental caries.
Shortcomings and outlook
This study has several limitations. First, this study had a small sample size. Second, the depth of microbiome sequencing was not sufficiently deep; moreover, 16SrRNA technology could not sufficiently reveal the structure of flora composition under the species classification. Third, we did not conduct a longitudinal analysis. Future longitudinal studies combining host genomics, behavioural factors, and environmental factors, as well as screening of precise biomarkers, are warranted.
Using a multi-omics approach can help elucidate the composition and function of the salivary microbial community in the caries condition, as well as inform caries prevention and treatment.
Supplementary Information
Additional file 1. 16S rRNA Gene Sequencing.
Additional file 2: Fig. S1. Taxon abundances at the phylum levels were compared between the SECC and CF groups using Metastats.
Additional file 3: Fig. S2. The random forest model was constructed for the genus taxonomic level (a). Comparison of model performance of random forests with different numbers of species, with the largest ROC values obtained for the 20 species selected (b). The AUC (Area Under Curve) is defined as the area under the ROC curve. Typically, it has a value between 1.0 and 0.5. For AUC > 0.5, the closer the AUC is to 1, the better the classification prediction is.
Additional file 4. Fig. S3. OPLS-DA 200 permutation testing. The R2Y(cum) and Q2(cum) results were (0.292, 0.131). The calculated R2X and R2Y(cum) estimates the goodness of fit of the model; Q2(cum) estimates the ability of prediction. For OPLS-DA, the permutation analysis between one predictive(p1) and three orthogonal (o1, o2, and o3) components produced the observed and cross-validated R2X, R2Y, and Q2 coefficients.
Additional file 5. Fig. S4. Correlations between microbiota (phylum level) and metabolites in saliva. Each row and column in the graph represents a metabolite and phylum, respectively, while each lattice represents a correlation coefficient between a component and a metabolite. Red and blue represent positive and negative correlations, respectively. * indicates a significant correlation between the phyla and metabolites (*p < 0.05, **p < 0.01).
Acknowledgements
The authors would like to express their sincere gratitude to the staff of the Department of Pharmacy, Hebei Medical University, They supported the part of the research.
Author contributions
LXC, LHY and MLQ conceived and reviewed the manuscript. LK participated the survey and wrote draft manuscript. WJM conducted the statistical analysis and prepared all figures. DN and SYJ participated in the sampling process. SQ and YWW revised the manuscript. All authors read and approved the final manuscript.
Funding
The study was supported by “Health Commission of Hebei Province (20211076) and Government Funding for Health Excellence Specialist (2021), 0300000147”.
Availability of data and materials
The datasets presented in this study can be found in SRA (Accession: PRJNA868496). https://www.ncbi.nlm.nih.gov/bioproject.
Declarations
Ethics approval and consent to participation
This study was approved by the Ethics Committee of Hebei Children's Hospital (Approval no. 207). All legal guardians of participating children were provided written informed consent following the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization. Sugars and dental caries. World Health Organization, 2017.
- 2.American Academy of Pediatric Dentistry Policy on early childhood caries (ECC): classifications, consequences, and preventive strategies. Pediatr Dent. 2016;38(6):52–54. [PubMed] [Google Scholar]
- 3.Anil S, Anand PS. Early childhood caries: prevalence, risk factors, and prevention. Front Pediatr. 2017;5:157. doi: 10.3389/fped.2017.00157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ismail AI, Lim S, Sohn W, et al. Determinants of early childhood caries in low-income African American young children. Pediatr Dent. 2008;30(4):289–296. [PubMed] [Google Scholar]
- 5.Ellakany P, Madi M, Fouda SM, et al. The effect of parental education and socioeconomic status on dental caries among Saudi children. Int J Environ Res Public Health. 2021;18(22):11862. doi: 10.3390/ijerph182211862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang X. The fourth national oral health epidemiological survey report. Beijing: People’s Medical Publishing House; 2018. [Google Scholar]
- 7.Vania A, Parisella V, Capasso F, et al. Early childhood caries underweight or overweight, that is the question. Eur J Paediatr Dent. 2011;12(4):231. [PubMed] [Google Scholar]
- 8.Cummins D. Dental caries: a disease which remains a public health concern in the 21st century–the exploration of a breakthrough technology for caries prevention. J Clin Dentistry. 2013;24(Spec Iss A):A1–A14. [PubMed] [Google Scholar]
- 9.Acharya S, Tandon S. The effect of early childhood caries on the quality of life of children and their parents. Contemp Clin Dent. 2011;2(2):98. doi: 10.4103/0976-237X.83069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Selwitz RH, Ismail AI, Pitts NB. Dental caries. Lancet. 2007;369(9555):51–59. doi: 10.1016/S0140-6736(07)60031-2. [DOI] [PubMed] [Google Scholar]
- 11.Kuramitsu HK, He X, Lux R, et al. Interspecies interactions within oral microbial communities. Microbiol Mol Biol Rev. 2007;71(4):653–670. doi: 10.1128/MMBR.00024-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gross EL, Beall CJ, Kutsch SR, et al. Beyond Streptococcus mutans: dental caries onset linked to multiple species by 16S rRNA community analysis. 2012. [DOI] [PMC free article] [PubMed]
- 13.Gross EL, Leys EJ, Gasparovich SR, et al. Bacterial 16S sequence analysis of severe caries in young permanent teeth. J Clin Microbiol. 2010;48(11):4121–4128. doi: 10.1128/JCM.01232-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marsh PD, Zaura E. Dental biofilm: ecological interactions in health and disease. J Clin Periodontol. 2017;44:S12–S22. doi: 10.1111/jcpe.12679. [DOI] [PubMed] [Google Scholar]
- 15.Javaid MA, Ahmed AS, Durand R, et al. Saliva as a diagnostic tool for oral and systemic diseases. J Oral Biol Craniofac Res. 2016;6(1):67–76. doi: 10.1016/j.jobcr.2015.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ling Z, Kong J, Jia P, et al. Analysis of oral microbiota in children with dental caries by PCR-DGGE and barcoded pyrosequencing. Microb Ecol. 2010;60(3):677–690. doi: 10.1007/s00248-010-9712-8. [DOI] [PubMed] [Google Scholar]
- 17.Yang F, Ning K, Chang X, et al. Saliva microbiota carry caries-specific functional gene signatures. PLoS ONE. 2014;9(2):e76458. doi: 10.1371/journal.pone.0076458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Luo AH, Yang DQ, Xin BC, et al. Microbial profiles in saliva from children with and without caries in mixed dentition. Oral Dis. 2012;18(6):595–601. doi: 10.1111/j.1601-0825.2012.01915.x. [DOI] [PubMed] [Google Scholar]
- 19.Chandna P, Srivastava N, Sharma A, et al. Isolation of Scardovia wiggsiae using real-time polymerase chain reaction from the saliva of children with early childhood caries. J Indian Soc Pedodont Prevent Dent. 2018;36(3):290. doi: 10.4103/JISPPD.JISPPD_225_17. [DOI] [PubMed] [Google Scholar]
- 20.Yang F, Zeng X, Ning K, et al. Saliva microbiomes distinguish caries-active from healthy human populations. ISME J. 2012;6(1):1–10. doi: 10.1038/ismej.2011.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Takahashi N, Washio J, Mayanagi G. Metabolomics of supragingival plaque and oral bacteria. J Dent Res. 2010;89(12):1383–1388. doi: 10.1177/0022034510377792. [DOI] [PubMed] [Google Scholar]
- 22.Singh N, Chandel S, Singh H, et al. Effect of scaling & root planing on the activity of ALP in GCF & serum of patients with gingivitis, chronic and aggressive periodontitis: a comparative study. J Oral Biol Craniofac Res. 2017;7(2):123–126. doi: 10.1016/j.jobcr.2017.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sinevici N, Mittermayr S, Davey GP, et al. Salivary N-glycosylation as a biomarker of oral cancer: a pilot study. Glycobiology. 2019;29(10):726–734. doi: 10.1093/glycob/cwz046. [DOI] [PubMed] [Google Scholar]
- 24.Zandona F, Soini HA, Novotny MV, et al. A potential biofilm metabolite signature for caries activity-A pilot clinical study. Metabol Open Access. 2015;5(1):140. doi: 10.4172/2153-0769.1000140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Foxman B, Srinivasan U, Wen A, et al. Exploring the effect of dentition, dental decay and familiality on oral health using metabolomics. Infect Genet Evol. 2014;22:201–207. doi: 10.1016/j.meegid.2013.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pereira JL, Duarte D, Carneiro TJ, et al. Saliva NMR metabolomics: Analytical issues in pediatric oral health research. Oral Dis. 2019;25(6):1545–1554. doi: 10.1111/odi.13117. [DOI] [PubMed] [Google Scholar]
- 27.Kanehisa M, Goto S. KEGG: kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 2000;28(1):27–30. doi: 10.1093/nar/28.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Xu H, Hao W, Zhou Q, et al. Plaque bacterial microbiome diversity in children younger than 30 months with or without caries prior to eruption of second primary molars. PLoS ONE. 2014;9(2):e89269. doi: 10.1371/journal.pone.0089269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Head DA, Marsh PD, Devine DA. Non-lethal control of the cariogenic potential of an agent-based model for dental plaque. PLoS ONE. 2014;9(8):e105012. doi: 10.1371/journal.pone.0105012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li Y, Zou CG, Fu Y, et al. Oral microbial community typing of caries and pigment in primary dentition. BMC Genomics. 2016;17(1):1–11. doi: 10.1186/s12864-016-2891-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xu H, Tian J, Hao W, et al. Oral microbiome shifts from caries-free to caries-affected status in 3-year-old Chinese children: a longitudinal study. Front Microbiol. 2009;2018:9. doi: 10.3389/fmicb.2018.02009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ma C, Chen F, Zhang Y, et al. Comparison of oral microbial profiles between children with severe early childhood caries and caries-free children using the human oral microbe identification microarray. PLoS ONE. 2015;10(3):e0122075. doi: 10.1371/journal.pone.0122075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhu C, Yuan C, Ao S, et al. The predictive potentiality of salivary microbiome for the recurrence of early childhood caries. Front Cell Infect Microbiol. 2018;8:423. doi: 10.3389/fcimb.2018.00423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Crielaard W, Zaura E, Schuller AA, et al. Exploring the oral microbiota of children at various developmental stages of their dentition in the relation to their oral health. BMC Med Genomics. 2011;4(1):1–13. doi: 10.1186/1755-8794-4-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lif Holgerson P, Öhman C, Rönnlund A, et al. Maturation of oral microbiota in children with or without dental caries. PLoS ONE. 2015;10(5):e0128534. doi: 10.1371/journal.pone.0128534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Xu X, He J, Xue J, et al. Oral cavity contains distinct niches with dynamic microbial communities. Environ Microbiol. 2015;17(3):699–710. doi: 10.1111/1462-2920.12502. [DOI] [PubMed] [Google Scholar]
- 37.Ortiz S, Herrman E, Lyashenko C, et al. Sex-specific differences in the salivary microbiome of caries-active children. J Oral Microbiol. 2019;11(1):1653124. doi: 10.1080/20002297.2019.1653124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Teng F, Yang F, Huang S, et al. Prediction of early childhood caries via spatial-temporal variations of oral microbiota. Cell Host Microbe. 2015;18(3):296–306. doi: 10.1016/j.chom.2015.08.005. [DOI] [PubMed] [Google Scholar]
- 39.Xu Y, Jia YH, Chen L, et al. Metagenomic analysis of oral microbiome in young children aged 6–8 years living in a rural isolated Chinese province. Oral Dis. 2018;24(6):1115–1125. doi: 10.1111/odi.12871. [DOI] [PubMed] [Google Scholar]
- 40.Lazarevic V, Whiteson K, Hernandez D, et al. Study of inter-and intra-individual variations in the salivary microbiota. BMC Genomics. 2010;11(1):1–11. doi: 10.1186/1471-2164-11-523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Neves AB, Lobo LA, Pinto KC, et al. Comparison between clinical aspects and salivary microbial profile of children with and without early childhood caries: a preliminary study. J Clin Pediatr Dent. 2015;39(3):209–214. doi: 10.17796/1053-4628-39.3.209. [DOI] [PubMed] [Google Scholar]
- 42.Jiang S, Gao X, Jin L, et al. Salivary microbiome diversity in caries-free and caries-affected children. Int J Mol Sci. 2016;17(12):1978. doi: 10.3390/ijms17121978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gomar-Vercher S, Cabrera-Rubio R, Mira A, et al. Relationship of children’s salivary microbiota with their caries status: a pyrosequencing study. Clin Oral Invest. 2014;18(9):2087–2094. doi: 10.1007/s00784-014-1200-y. [DOI] [PubMed] [Google Scholar]
- 44.Wang Y, Zhang J, Chen X, et al. Profiling of oral microbiota in early childhood caries using single-molecule real-time sequencing. Front Microbiol. 2017;8:2244. doi: 10.3389/fmicb.2017.02244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lee E, Park S, Um S, et al. Microbiome of saliva and plaque in children according to age and dental caries experience. Diagnostics. 2021;11(8):1324. doi: 10.3390/diagnostics11081324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Luo YX, Sun ML, Shi PL, et al. Research progress in the relationship between Veillonella and oral diseases. Hua xi kou qiang yi xue za zhi= Huaxi kouqiang yixue zazhi= West China J Stomatol. 2020, 38(5): 576–582. [DOI] [PMC free article] [PubMed]
- 47.Wang Y, Wang S, Wu C, et al. Oral microbiome alterations associated with early childhood caries highlight the importance of carbohydrate metabolic activities. MSystems. 2019;4(6):e00450–e519. doi: 10.1128/mSystems.00450-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hurley E, Barrett MPJ, Kinirons M, et al. Comparison of the salivary and dentinal microbiome of children with severe-early childhood caries to the salivary microbiome of caries-free children. BMC Oral Health. 2019;19(1):1–14. doi: 10.1186/s12903-018-0693-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Khalilia M, Chakraborty S, Popescu M. Predicting disease risks from highly imbalanced data using random forest. BMC Med Inform Decis Mak. 2011;11(1):1–13. doi: 10.1186/1472-6947-11-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fidalgo TKS, Freitas-Fernandes LB, Angeli R, et al. Salivary metabolite signatures of children with and without dental caries lesions. Metabolomics. 2013;9(3):657–666. [Google Scholar]
- 51.Fidalgo TKS, Freitas-Fernandes LB, Almeida FCL, et al. Longitudinal evaluation of salivary profile from children with dental caries before and after treatment. Metabolomics. 2015;11(3):583–593. [Google Scholar]
- 52.Reo NV. NMR-based metabolomics. Drug Chem Toxicol. 2002;25(4):375–382. doi: 10.1081/dct-120014789. [DOI] [PubMed] [Google Scholar]
- 53.Beltran A, Suarez M, Rodríguez MA, et al. Assessment of compatibility between extraction methods for NMR-and LC/MS-based metabolomics. Anal Chem. 2012;84(14):5838–5844. doi: 10.1021/ac3005567. [DOI] [PubMed] [Google Scholar]
- 54.Pan Z, Raftery D. Comparing and combining NMR spectroscopy and mass spectrometry in metabolomics. Anal Bioanal Chem. 2007;387(2):525–527. doi: 10.1007/s00216-006-0687-8. [DOI] [PubMed] [Google Scholar]
- 55.Gardner A, Parkes HG, So PW, et al. Determining bacterial and host contributions to the human salivary metabolome. J Oral Microbiol. 2019;11(1):1617014. doi: 10.1080/20002297.2019.1617014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sugimoto M, Saruta J, Matsuki C, et al. Physiological and environmental parameters associated with mass spectrometry-based salivary metabolomic profiles. Metabolomics. 2013;9(2):454–463. [Google Scholar]
- 57.Navazesh M, Kumar SKS. Measuring salivary flow: challenges and opportunities. J Am Dent Assoc. 2008;139:35S–40S. doi: 10.14219/jada.archive.2008.0353. [DOI] [PubMed] [Google Scholar]
- 58.Heimisdóttir LH, Lin BM, Cho H, et al. Metabolomics insights in early childhood caries. J Dent Res. 2021;100(6):615–622. doi: 10.1177/0022034520982963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zeng L, Das S, Burne RA. Utilization of lactose and galactose by Streptococcus mutans: transport, toxicity, and carbon catabolite repression. J Bacteriol. 2010;192(9):2434–2444. doi: 10.1128/JB.01624-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Abranches J, Chen YYM, Burne RA. Galactose metabolism by Streptococcus mutans. Appl Environ Microbiol. 2004;70(10):6047–6052. doi: 10.1128/AEM.70.10.6047-6052.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Meng Y, Wu T, Billings R, et al. Human genes influence the interaction between Streptococcus mutans and host caries susceptibility: a genome-wide association study in children with primary dentition. Int J Oral Sci. 2019;11(2):1–8. doi: 10.1038/s41368-019-0051-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shi M, Wei Y, Nie Y, et al. Alterations and correlations in microbial community and metabolome characteristics in generalized aggressive periodontitis. Front Microbiol. 2020;11:573196. doi: 10.3389/fmicb.2020.573196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Moye ZD, Zeng L, Burne RA. Fueling the caries process: carbohydrate metabolism and gene regulation by Streptococcus mutans. J Oral Microbiol. 2014;6(1):24878. doi: 10.3402/jom.v6.24878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hallang S, Esberg A, Haworth S, et al. Healthy oral lifestyle behaviours are associated with favourable composition and function of the oral microbiota. Microorganisms. 2021;9(8):1674. doi: 10.3390/microorganisms9081674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Schulz A, Lang R, Behr J, et al. Targeted metabolomics of pellicle and saliva in children with different caries activity. Sci Rep. 2020;10(1):1–11. doi: 10.1038/s41598-020-57531-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Aimetti M, Cacciatore S, Graziano A, et al. Metabonomic analysis of saliva reveals generalized chronic periodontitis signature. Metabolomics. 2012;8(3):465–474. [Google Scholar]
- 67.Fonteles CSR, Guerra MH, Ribeiro TR, et al. Association of free amino acids with caries experience and mutans streptococci levels in whole saliva of children with early childhood caries. Arch Oral Biol. 2009;54(1):80–85. doi: 10.1016/j.archoralbio.2008.07.011. [DOI] [PubMed] [Google Scholar]
- 68.Chen HW, Zhou W, Liao Y, et al. Analysis of metabolic profiles of generalized aggressive periodontitis. J Periodontal Res. 2018;53(5):894–901. doi: 10.1111/jre.12579. [DOI] [PubMed] [Google Scholar]
- 69.Li Y, Wang D, Zeng C, et al. Salivary metabolomics profile of patients with recurrent aphthous ulcer as revealed by liquid chromatography–tandem mass spectrometry. J Int Med Res. 2018;46(3):1052–1062. doi: 10.1177/0300060517745388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zhu X, Long F, Chen Y, et al. A putative ABC transporter is involved in negative regulation of biofilm formation by Listeria monocytogenes. Appl Environ Microbiol. 2008;74(24):7675–7683. doi: 10.1128/AEM.01229-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kalpana B, Prabhu P, Bhat AH, et al. Bacterial diversity and functional analysis of severe early childhood caries and recurrence in India. Sci Rep. 2020;10(1):1–15. doi: 10.1038/s41598-020-78057-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Barnes VM, Ciancio SG, Shibly O, et al. Metabolomics reveals elevated macromolecular degradation in periodontal disease. J Dent Res. 2011;90(11):1293–1297. doi: 10.1177/0022034511416240. [DOI] [PubMed] [Google Scholar]
- 73.Garavito MF, Narváez-Ortiz HY, Zimmermann BH. Pyrimidine metabolism: dynamic and versatile pathways in pathogens and cellular development. J Genet Genomics. 2015;42(5):195–205. doi: 10.1016/j.jgg.2015.04.004. [DOI] [PubMed] [Google Scholar]
- 74.Ota S. Catecholamines level in saliva from patients with periodontal disease. Nihon Shishubyo Gakkai Kaishi. 1985;27(3):509–517. [Google Scholar]
- 75.Kondo Y, Melvin JE, Catalan MA. Physiological cAMP-elevating secretagogues differentially regulate fluid and protein secretions in mouse submandibular and sublingual glands. Am J Physiol Cell Physiol. 2019;316(5):C690–C697. doi: 10.1152/ajpcell.00421.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Yamada K, Inoue H, Kida S, et al. Involvement of cAMP response element-binding protein activation in salivary secretion. Pathobiology. 2006;73(1):1–7. doi: 10.1159/000093086. [DOI] [PubMed] [Google Scholar]
- 77.Culp DJ, Robinson B, Cash MN. Murine salivary amylase protects against Streptococcus mutans-induced caries. Front Physiol 2021: 919. [DOI] [PMC free article] [PubMed]
- 78.Mojarad F, Fazlollahifar S, Poorolajal J, et al. Effect of alpha amylase on early childhood caries: a matched case-control study. Brazilian Dental Science. 2013;16(1):41–45. [Google Scholar]
- 79.Farag MA, Shakour ZT, Lübken T, et al. Unraveling the metabolome composition and its implication for Salvadora persica L. use as dental brush via a multiplex approach of NMR and LC–MS metabolomics. J Pharmaceut Biomed Anal. 2021;193:113727. doi: 10.1016/j.jpba.2020.113727. [DOI] [PubMed] [Google Scholar]
- 80.Nijakowski K, Gruszczyński D, Kopała D, et al. Salivary metabolomics for oral squamous cell carcinoma diagnosis: a systematic review. Metabolites. 2022;12(4):294. doi: 10.3390/metabo12040294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Zhang G, Bi M, Li S, et al. Determination of core pathways for oral squamous cell carcinoma via the method of attract. J Cancer Res Ther. 2018;14(12):1029. doi: 10.4103/0973-1482.206868. [DOI] [PubMed] [Google Scholar]
- 82.Divaris K. Predicting dental caries outcomes in children: a “risky” concept. J Dent Res. 2016;95(3):248–254. doi: 10.1177/0022034515620779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Mileguir D, Golubnitschaja O. Human saliva as a powerful source of information: multi-omics biomarker panels. EPMA world congress: traditional forum in predictive, preventive and personalised medicine for multi-professional consideration and consolidation. EPMA J. 2017;8(1):1–54. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. 16S rRNA Gene Sequencing.
Additional file 2: Fig. S1. Taxon abundances at the phylum levels were compared between the SECC and CF groups using Metastats.
Additional file 3: Fig. S2. The random forest model was constructed for the genus taxonomic level (a). Comparison of model performance of random forests with different numbers of species, with the largest ROC values obtained for the 20 species selected (b). The AUC (Area Under Curve) is defined as the area under the ROC curve. Typically, it has a value between 1.0 and 0.5. For AUC > 0.5, the closer the AUC is to 1, the better the classification prediction is.
Additional file 4. Fig. S3. OPLS-DA 200 permutation testing. The R2Y(cum) and Q2(cum) results were (0.292, 0.131). The calculated R2X and R2Y(cum) estimates the goodness of fit of the model; Q2(cum) estimates the ability of prediction. For OPLS-DA, the permutation analysis between one predictive(p1) and three orthogonal (o1, o2, and o3) components produced the observed and cross-validated R2X, R2Y, and Q2 coefficients.
Additional file 5. Fig. S4. Correlations between microbiota (phylum level) and metabolites in saliva. Each row and column in the graph represents a metabolite and phylum, respectively, while each lattice represents a correlation coefficient between a component and a metabolite. Red and blue represent positive and negative correlations, respectively. * indicates a significant correlation between the phyla and metabolites (*p < 0.05, **p < 0.01).
Data Availability Statement
The datasets presented in this study can be found in SRA (Accession: PRJNA868496). https://www.ncbi.nlm.nih.gov/bioproject.