Abstract
Klippel–Feil syndrome (KFS) is a congenital skeletal disorder with classic clinical triad consisting of short neck, low hairline, and limitation of neck movement. In addition to skeletal deformities, diagnosed cases of KFS may have other anomalies such as cardiac, neurologic, and genitourinary disorder. We report a case of KFS with associated anomalies such as short neck, limitation of neck movement, scoliosis of cervical spine, and dextrocardia who received successful cadaveric kidney transplantation. This article aims to present kidney transplantation as option of treatment in KFS patient with ESRD and emphasize on the difficulty in airway management of this patient.
Keywords: difficult airway, ESRD, kidney transplant, Klippel–Feil syndrome, limited neck movement
Short abstract
Klippel–Feil syndrome is a skeletal disease with fusion of cervical vertebrae. During surgery, attention should be paid to the difficulty in airway management and the importance of being prepared for it using video laryngoscopy. Because anatomy of vessel and bladder were normal, technique of kidney transplant surgery was routine.
1. INTRODUCTION
Klippel–Feil syndrome (KFS) is a congenital skeletal disorder characterized by fusion of at least two adjacent cervical vertebrae. Its estimated prevalence is 0.58%. 1 The syndrome has classic clinical triad consisting in short neck, low hairline, and limitation of neck movements, although less than 50% of patients shows such triad. 2 The vast majority of KFS patients present a single vertebral fusion, and those who are symptomatic more likely have multiple fusions. 1 In this article, we report a patient with KFS, who developed chronic renal failure that was treated by cadaveric kidney transplantation. Airway management is a challenging part of patients treatment, due to both the increasing use of surgery for cadaveric renal transplantation and to limited neck movements.
2. CASE REPORT
A 27‐year‐old patient was admitted to the transplant ward of the urology department for renal transplantation. His past medical history was marked by hypertension. Family history was negative for congenital renal abnormalities, and his parents were nonconsanguineous. He had serum creatinine of 10 mg/dl and eGFR of 14 ml/min/1.73 m2. Indeed, he had been on regular hemodialysis three times a week until then. Short neck, limitation of neck movements, and scoliosis of cervical spine were observed. Ptosis of the right eye was also noted (Figure 1). Eye movements and visual acuity were normal. Evaluation of ear, nose, and throat revealed normal findings.
FIGURE 1.

Short neck is seen.
Chest and cervical spine X‐ray showed fusion of cervical bodies C3‐5, left cervical rib, loss of cervical lordosis, as well as dextrocardia (Figure 2). Transthoracic echocardiography confirmed dextrocardia, and showed as well coarctation of the aorta, moderate left ventricular hypertrophy (LVH), in addition to aortic insufficiency (AI). Abdominopelvic computed tomography (CT) scan showed empty bilateral renal fossa with ectopic pelvic kidney in the right side (Figure 3). Our patient received a cadaveric renal allograft, from a donor died of brain trauma due to car accident. General anesthesia was performed using regular medications including propofol, fentanyl, and atracurium.
FIGURE 2.
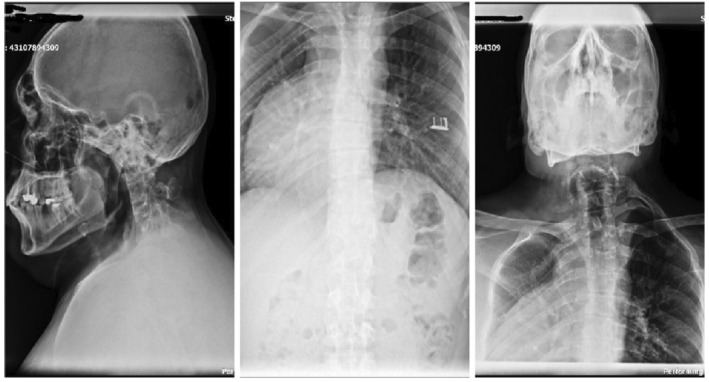
Fusion of cervical bodies C3‐5, dextrocardia, and loss of cervical lordosis
FIGURE 3.

Ectopic pelvic kidney in the right side
Intubation was first tried with direct laryngoscopy. We faced Cormack–Lehane score of four in laryngoscopic view. However, due to difficult airway management, we failed to intubate patient at the first try. Then, video laryngoscope was used through which an acceptable glottis view was taken and trachea was intubated using a 7.5 ID armored tube. General anesthesia was maintained using volatile isoflurane, in addition to intermittent continuous infusion of atracurium, and remifentanyl, respectively. No hemodynamic alterations occurred throughout anesthesia and hemorrhage was minimal, requiring no blood transfusion. Fifty milliliters of sodium bicarbonate (9%) and 100 ml of mannitol (20%) were infused to the kidney before declamp of arterial graft to enhance perfusion of the transplanted kidney. Droplets of urine were seen after declamp of arterial graft of the patient on surgical table.
2.1. Surgical technique
Gibson incision was made in the left side, and external oblique, fascia, internal oblique, and transverse muscles were divided into the line of the incision, respectively. Donated kidney was placed in the retroperitoneal iliac fossa. Renal graft vein and artery were anastomosed end to side to the external iliac vein and artery, respectively. Ureter was reconstructed with modified Lich technique. Immunosuppression regime based on methylprednisolone and thymoglobuline was begun after operation, and the patient was discharged on 35th postoperative day with a creatinine value of 2 mg/dl.
3. DISCUSSION
Klippel–Feil syndrome (KFS) is a congenital skeletal disorder with diagnostic classical clinical triad consisting of short neck, low hairline, and limitation of neck movement. The etiology of the syndrome is not well known. In some cases, mutations in GDF6, GDF3, and MEOX1 genes are the main factors which are related to this syndrome. GDF6 and GDF3 are involved in bone development. MEOX1 encodes for the MOX1 protein, which regulates the separation of vertebrae. 3 KFS is classified into three types: Type I—single congenitally fused cervical segment; Type II—multiple noncontiguous, congenitally fused segments; and Type III—multiple contiguous, congenitally fused cervical segments. 4 Genitourinary anomalies are one of the associated anomalies, with incidence of 35%. 5 The embryological development of the skeletal and genitourinary systems occurs at the same time, and differentiation is comprised between the third and the eighth week of gestation. 6 It is reasonable that any fault of fetal development at this time can produce both genitourinary anomalies and bone defects (including the cervical vertebrae). Such injuries or disruptions may have genetic causes or risk factors. The exact pathogenic mechanisms are however still unknown, and genomic, epigenetic, and environmental factors may concur. 7 Unilateral or bilateral renal agenesis, crossed renal ectopia, and duplication of the collecting system are renal anomalies associated with KFS. They may cause ESRD in these patients. 8 This report aims to emphasize on the difficulty in airway management of these subjects and the importance of being prepared for it, also through the use of indirect video laryngoscopy device. In addition, we want to highlight how the routine surgical technique of kidney transplantation maybe successfully applied to these patients, similar to other clinical conditions. Therefore, this surgical option is an acceptable procedure in case of KFS with ESRD.
AUTHOR CONTRIBUTIONS
Hossein Dialameh: Conceptualization; data curation; project administration; supervision. Farshad Namdari: Data curation; resources. Farhad Etezadi: Conceptualization; writing – review and editing. Seyed Hassan Inanloo: Investigation; visualization. Seyed Hamid Mousavi: Formal analysis. Hormat Rahimzadeh: Resources. Mohammad Javad Nazarpour: Validation; visualization.
FUNDING INFORMATION
None.
CONFLICT OF INTEREST
The authors declare that they have no competing interests.
CONSENT
Informed consent was obtained from the patient for publication of this case report.
ACKNOWLEDGMENTS
The authors acknowledge all the members of transplant ward of urology department.
Dialameh H, Namdari F, Etezadi F, et al. Cadaveric kidney transplantation in an ESRD patient with Klippel–Feil syndrome—A case report. Clin Case Rep. 2023;11:e06850. doi: 10.1002/ccr3.6850
DATA AVAILABILITY STATEMENT
Not applicable.
REFERENCES
- 1. Nouri A, Patel K, Evans H, et al. Demographics, presentation and symptoms of patients with Klippel‐Feil syndrome: analysis of a global patient‐reported registry. Eur Spine J. 2019;28(10):2257‐2265. [DOI] [PubMed] [Google Scholar]
- 2. Gruber J, Saleh A, Bakhsh W, Rubery PT, Mesfin A. The prevalence of Klippel‐Feil syndrome: a computed tomography–based analysis of 2,917 patients. Spine Deformity. 2018;6(4):448‐453. [DOI] [PubMed] [Google Scholar]
- 3. Stelzer JW, Flores MA, Mohammad W, Esplin N, Mayl JJ, Wasyliw C. Klippel‐Feil syndrome with Sprengel deformity and extensive upper extremity deformity: a case report and literature review. Case Rep Orthop. 2018;2018:5796730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Samartzis DD, Herman J, Lubicky JP, Shen FH. Classification of congenitally fused cervical patterns in Klippel‐Feil patients: epidemiology and role in the development of cervical spine‐related symptoms. Spine (Phila Pa 1976). 2006;31(21):E798‐E804. [DOI] [PubMed] [Google Scholar]
- 5. Grise P, Lefort J, Dewald M, Mitrofanoff P, Borde J. Urinary malformations in synostoses of the cervical vertebrae (Klippel‐Feil syndrome). Apropos of 35 Cases. Annales d'urologie; 1984. [PubMed] [Google Scholar]
- 6. Gunderson CH, Greenspan RH, Glaser GH, Lubs HA. The Klippel‐Feil syndrome: genetic and clinical reevaluation of cervical fusion. Medicine. 1967;46(6):491‐512. [DOI] [PubMed] [Google Scholar]
- 7. Moore WB, Matthews TJ, Rabinowitz R. Genitourinary anomalies associated with Klippel‐Feil syndrome. J Bone Joint Surg Am. 1975;57(3):355‐357. [PubMed] [Google Scholar]
- 8. Parmentier‐de León C, Cruz‐Martínez R, Quintero‐Quintero MJ, Alberú J, Contreras AG, Vilatobá M. Trasplante renal de donador vivo en paciente con síndrome de Klippel‐Feil. Diálisis y Trasplante. 2019;40(2):38‐40. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


