Abstract
Play is a pleasurable physical or mental activity that enhances the child’s skills involving negotiation abilities, problem-solving, manual dexterity, sharing, decision-making, and working in a group. Play affects all the brain's areas, structures, and functions. Children with autism have adaptive behavior, adaptive response, and social interaction limitations. This review explores the different applications of play therapy in helping children with autism disorder. Play is usually significantly impaired in children with autism. Play therapy is mainly intended to help children to honor their unique mental abilities and developmental levels. The main aim of play therapy is to prevent or solve psychosocial difficulties and achieve optimal child-healthy growth and development. Play therapy helps children with autism to engage in play activities of their interest and choice to express themselves in the most comfortable ways. It changes their way of self-expression from unwanted behaviors to more non-injurious expressive behavior using toys or activities of their choice as their words. Play therapy also helps those children to experience feeling out various interaction styles. Every child with autism is unique and responds differently. Therefore, different types of intervention, like play therapy, could fit the differences in children with autism. Proper evaluation of the child is mandatory to evaluate which type fits the child more than the others. This narrative review revised the different types of play therapy that could fit children with autism in an evidence-based way. Despite weak evidence, play therapy still has potential benefits for patients and their families.
Keywords: Autism, Play therapy, Children, Autism spectrum disorder, Sensory integration therapy, Art-play therapy, Equine-partnered play therapy, Child-centered play therapy, Synergistic play therapy
Core Tip: Play is a pivotal activity for humans, especially children. It plays an essential role in children’s physical and mental development. Play therapy has been used for a long time to manage various diseases. Play therapy helps children with autism to engage in play activities of their interest, express themselves in comfortable ways, and change their self-expression from unwanted behavior to more non-injurious expressive behavior. There are different forms of play therapy. Proper evaluation of the child is mandatory to evaluate which fits the child more. Play therapy has a lot of potential benefits for patients and their families.
INTRODUCTION
Play is pleasurable, intrinsically motivating, process-oriented, freely chosen physical or mental activities in which the child actively engages spontaneously, mainly in a safe environment. Children must have fun, or it is not considered a play[1]. Children from the neonatal period to adolescence spend 3%-20% of the day playing. Play is a fundamental daily activity that allows children to learn and master various skills involving negotiation abilities, problem-solving, emotional intelligence, improving their manual dexterity, sharing, decision-making, and working within a group. Play helps children to discover their interests. Play promotes the integration of mental development with social life.
Furthermore, unstructured play allows children to exercise more, spend more calories, avoid sedentary life effects, and remain healthy. Children do not need to learn how to play; they acquire it naturally. Play is developmentally relevant to childhood[2,3].
Consequently, play becomes the child's language, and the toys become the child's words. Play and toys become a medium to prevent or resolve social and/or psychological difficulties that the child may become exposed to. Adults usually underestimate children's capabilities, especially when it comes to playing. Adults usually lead the children during playing with an agenda that seems vital to them without allowing them to play according to what they want or need. There is less opportunity for children to play without directiveness, rules, conditions, and/or agenda. Adults usually change or ruin the child's structure and flow of play[4]. The play could be advocated in educational, medical, mental health systems, and/or community settings. Play became an option when all seriousness occurred. It became a reward despite being crucial and is integrated into healthy child development. Play helps us to communicate with the child's language so that we can enter their world, which is often left silent. Play is the child's language when we start to listen to him[5].
Autism prevalence has been increasing over the last decades. Autism is a spectrum characterized by a wide range of persistent shortages in social interaction, impaired communication skills, restricted-repetitive forms of behavior, and the loss of social interests or activities. These social communication and interaction impairments may be due to impaired social signaling interpretation and failure to guide proper behaviors[6]. The exact mechanisms for these behavioral abnormalities are not yet defined. However, autism results from genetic defects and neuroinflammation of the immature brain. Neuroinflammation could result from a malfunctioning placenta, an immature blood-brain barrier, aberrant maternal immune activation by infection and maternal dysbiosis during pregnancy, a premature delivery, and antenatal exposure to nutritional and toxic metals through mid-fatal development, early postnatal encephalitis, or a toxic environment[7,8]. There are more mitochondrial disorders and dysfunction incidences in children with autism than in the general population, which commonly occur secondary to environmental factors[9]. In addition, discrepancies in the glutathione redox system are a crucial factor in autism pathophysiology, causing proteotoxic stress and other defects in sulfhydryl-containing enzymes in the blood and brain[10]. This review aims to explore the effects of play in modulating the symptoms of autism and aims to investigate the different applications of play therapy in helping children with autism disorder.
LITERATURE SEARCH
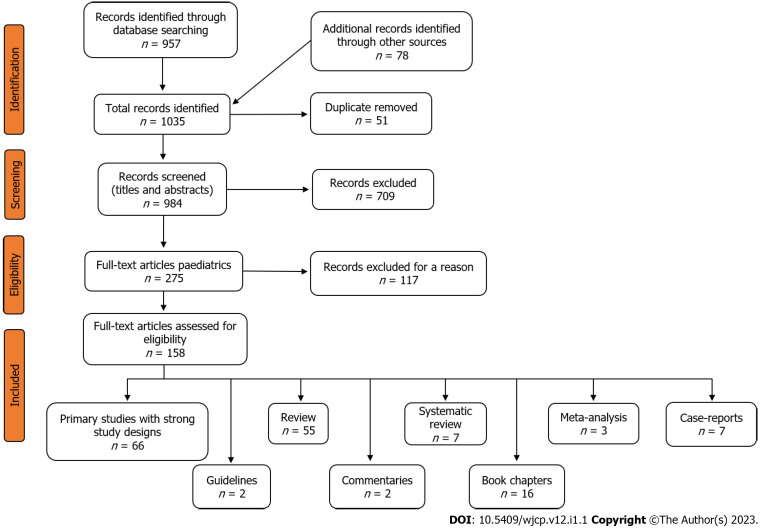
To build an evidence-based view of this aim, we conducted a comprehensive literature review by searching electronic databases, including PubMed, Embase, Cochrane Library, Cumulative Index to Nursing and Allied Health Literature, Web of Science, Scopus, Library, and Information Science Abstracts, and the National Library of Medicine catalog up until June 30, 2022, using the keywords: play, play therapy, autism, autism spectrum disorder. We included full-text research (66 articles), reviews (55 articles), systematic reviews (7 articles), metanalysis (3 articles), Case reports (7 articles), guidelines (two articles), commentaries (two articles), and book chapters (16), written in English and concerned with using play therapy in the management of children with autism (Figure 1). Reference lists were inspected, and citation searches were performed on the included studies. We also reviewed many review articles concerned with the same topic. We also reviewed the articles that are available as abstracts only. We excluded articles that could have a commercial background.
Figure 1.
The flow chart of the study, according to PRISMA 2009 guidelines.
PLAY IN DIFFERENT STAGES OF CHILDHOOD
Intrauterine fetal play
The fetus develops a unique type of sensory play at a very early stage of gestation and begins to develop its tactile system due to the surrounding amniotic fluid. The fetus swims smoothly in a way that activates the vestibular system and sense of direction, which helps to develop a sense of proprioception when kicking and pushing the inner sides of the womb[11]. The fetus starts to hear the mother's body sounds, such as heartbeats or stomach rumbling, by the 18th week of gestation and starts to react to these sounds by the 26th week. After the 32nd week of gestation, the fetus can recognize certain vowel sounds from the mother language, suggesting very early language development even before birth. The fetus can memorize his mother's voice and more complex auditory external sounds with considerable discrimination capacity[12]. Fetuses may startle or even cry when exposed to sudden loud sounds. The mother can start playing with her fetus by touching or rubbing her abdomen in response to fetal movement. The father can massage the fetus's bump if the mother is happy with that. Both can talk, sing and read, so the fetus can get used to sounds[13]. These maneuvers help to strengthen feto-maternal bonding and enhance fetal development. The auditory and olfactory systems also develop in unique ways. A previous study has shown that the baby feels comfortable if his pillow is sprayed with the smell of food that the mother used to eat while she was pregnant with that baby. Babies who ate cereals with carrot flavor showed better facial expressions if the mother consumed carrots during gestation. Moreover, if the baby listens to music that the mother used to hear while she was pregnant with him, he will sleep deeper and more comfortably[14].
Neonatal play
Playing with newborns helps them learn about the new world and how to interact with it. Play permits their brains to grow and develop, build muscles, and develop gross and fine motor skills. The mother's play with the baby helps her understand her baby and helps the baby feel love and build trust with the mother. Play strengthens the bonding between the mother and the newborn. Playing with the newborn needs simple actions such as singing, chatting, tickling, counting toes, blowing raspberries, smiling, laughing, rolling the eyes, or poking the tongue out. Even during the nappy change, the mother could have an excellent chance for face-to-face play[15]. In other words, the mother needs to use what is called “serve and return,” in which the child gives action, and the mother or the father must respond right away to keep the child engaged[16]. The mother can use rattles, soft toys, or cloth books with painted pages and different textures. This tactile play helps the neonates to feel different things and learn about the external world. Reading can start soon after birth. The mother should hold books close to the baby's eyes within the visual range of 20 to 30 centimeters. Early reading helps infants get used to sounds and words to build language and enjoyment with books[17,18].
Childhood play
Play is a central component in typical child development and learning and is a fundamental right of every child. Play is the main occupation of children. Play is critical in maintaining children's physical and mental health. The main intention of the child’s play is to have fun; however, play enhances psychosocial development and helps children to discover the surrounding world. It helps children enface reality and adapt it to their wishes[19]. Play enriches the children's physical, social, cognitive, and emotional abilities and sense of well-being. In the meantime, play promotes the children's skills and abilities to study and work. In addition, it hones their relationships with their peers and community and helps them gain independence, confidence, self-esteem, interaction, resilience, curiosity, and coping with challenging situations[20]. The degree of playful behaviors during play varies between 0-100% depending on the presence of purpose, pleasure, and enjoyment degree, and how much the child is process-oriented[21].
Children are affected by day-to-day changes in the world around them. Consequently, the degree of playful activities depends on the child's age, the local culture that impacts the parents' concepts of playing, and the type of the child's play. It is also affected by social class and urban or rurality[22]. Playtime is also affected by the media, local culture and tradition, fashion, books, sex, and ethnicity. Unfortunately, children currently spend less time in actual playing due to the stress of study and school testing, even though play establishes the foundation for effective lifetime learning. Therefore, pediatricians must promote the importance of playful learning to young children by supplying children with rich play practices and assisting the parents to understand better the significance of playful learning in children's lives. Parents playing with their children establish the base for children's ability to play with their peers effectively[23,24].
Play could help to build motivated, happy, and healthy children to be the future of a productive society. There are different types of social play the children can do. In the solitary play, every child plays alone, while in parallel play, the children are engaged in similar activities, but each child plays separately. In associative play, children play individually, but they may share, pay joint attention, and occasionally communicate with each other. Meanwhile, in cooperative play, children are involved in play with a shared goal, and they play together to achieve this goal. Consequently, play helps to increase social interaction, which usually increases over time[25,26].
Object play
In object play, children actively playfully manipulate objects. This active manipulative play is used to either explore or construct objects. With time, manipulating and visualizing objects and toys improves visual-motor integration skills necessary for reading, writing, and many other daily-life activities[16]. It starts as early as the fifth postnatal month when the infant starts exploratory playing by putting everything in his mouth. By age two, the child starts constructive playing as he can combine objects when playing, such as building a tower from some blocks or lining small cars beside each other[27]. Over the next few years, constructive play increases to be combined with imaginative and pretended play, where children start to construct more complex creative models blending constructive and pretended play together, representing the world around them. Constructive play is established when the child develops a constructional praxis ability[28]. By year four, children spend about half of their free-play time in constructive play, extending to preschool and elementary years. Object Play significantly impacts the children's physical, cognitive, and social development by enhancing fine and gross motor skills and manual dexterity. Interactive, cooperative object playing with adults or peers significantly impacts the child's social development more than solitary, parallel, or associative play[29].
Pretend play
Pretend play is characteristic of early childhood, in which the child creates an imaginary reality alternative to the real world. The child assumes other people's roles or imagines other places, things, or other times. The child can also use objects as a symbol for what is imagined. For example, the child uses the banana as a telephone. Pretend play can occur in a group, where a group of children cooperate and assume complementary characters, which enhances social interaction[30]. Pretend play may appear by twelve months when the infant pretends to sleep. Later, children direct their pretending towards other people and surrounding objects. They may animate the surrounding objects in their imaginative play. They may use models like dolls or stuffed animals in their acting play. The child also can respond to pretend play as early as two years old; for example, when a person pretends to do something, the child may pretend to do a complementary or opposite action[31]. Overt pretend play usually diminishes by middle childhood when the child acquires more interest in organized games. Pretend play performs a crucial role in the cognitive and social development of the child with a marked impact on a wide range of cognitive, cultural, emotional, social, and competence skills. It also helps to enhance the child's creative and problem-solving abilities and language skills[32]. The earlier the pretend play, the better literacy outcomes, especially for reading and comprehension abilities and communication skills, particularly speech and writing. Pretend play is also a prominent factor in developing the child's self-regulating abilities and different aspects of executive function[33]. These abilities, in turn, impact school readiness, memory development, attention empowerment, intelligence enhancement, morality, and emotion regulation. Pretending also helps children to understand others. When they step into the shoes of a character, they imagine what he would say, do, or feel, which helps them to understand other people. Pretending and fantasy could also allow children to express their feelings, regulate their thoughts, and better cope with their emotions[34].
Physical play (locomotor or exercise play)
Physical play involves any physical activity performed in a playful and joyful context, such as running, climbing, skipping, gambol, hopping, kicking a football, and chasing. It has an inverted U-shaped curve, gradually rising from infancy across the school years and then decreasing during adolescence[35]. Physical play is essential nowadays, especially with increasing obesity and insulin resistance rates among children and adolescents. Physical activity improves insulin sensitivity, helps fight obesity, and promotes healthy lifestyles[36]. Encouraging childhood physical play and gross motor skills is essential to boost physical activity levels with enormous health benefits, including aerobic endurance, strengthening muscle growth, better coordination, enhanced growth stimulation of crucial organs, and augmented bone mineral content[37,38]. In addition, physical play improves cognitive, mental, and academic fields, contributes to self-regulation development and expression, and improves school-age children's executive function, particularly with organized and planned activities like sports. It also enhances academic outcomes through increased attention to educational tasks[39,40]. Physical play promotes the sensory integration, incorporation, and processing mechanism between the central nervous system and the body. Thus, sensory integration enhances cognitive, social, emotional, academic, and communication skills to higher levels[41]. Physical play and sensory integration are evidence-based methods that support the development of children in general and children with ASD. Figure 2 shows the application of sensory play in the Genomics Childhood Sensory Play Center, the first epigenetic play center in the world, based in Manama, Bahrain. Unfortunately, physical play is markedly affected during the COVID-19 pandemic reaching alarming rates. This environmental deprivation affected children’s physical, emotional, communication, social, and academic learning abilities[42].
Figure 2.
The application of sensory play in the Genomics Childhood Sensory Play Center, the first epigenetic play center in the world, based in Manama, Bahrain.
Media play
Technology plays a crucial role in children's lives today, much more than before. Before the COVID-19 era, children younger than three years spent 3-4 h/day on-screen media. This number increased to 7.5 h/d by eight years of age. In the COVID-19 era, the number of hours children spend on media screens has significantly risen[43]. There are contradictory opinions about the effects of media on children's behavior and development. A popular opinion suggests that media and gaming are responsible for increasing obesity rates, reducing social skills development, encouraging violent behavior, and negatively affecting language, social, cognitive, and emotional development[44]. On the other hand, other studies endorse that media and video gaming enhance athletic participation and decrease the rate of obesity. Those studies suggest that video game players are more likely to be open-minded, show more obedience to their parents, have more academically minded friends, and are no more violent or aggressive than non-video game players[45,46]
Technology-based games construct a powerful tool to enhance playful learning, especially when the interest in traditional play starts to wane. In addition to fun, these games allow children to practice high self-control and self-learning with trial and error. These games also varnish their memory, skills, critical thinking, executive function, qualitative thinking, and creativity in problem-solving and advance their knowledge through escalated levels of complexity impregnated into the games. In addition, these games used different tactile, visual, and auditory modalities with increased visuospatial abilities, allowing children to have various learning styles[47,48]. These games teach children to stay on task for longer and be more patient in reaching their goals. For instance, Genomics Childhood Sensory Play Center uses interactive projector games that enable children to use tactile, vestibular, proprioceptive, auditory, and visual systems more effectively.
Moreover, they have specific reaction times to give an adaptive response and functional performance. Thus, they promote self-esteem, self-confidence, mind, brain, and behavior. That being experienced, children achieve higher and innovate throughout their future education, career, family, and life in general. However, the degree of benefit from media and video games is age dependent. For example, television viewing has mostly negative associations for children younger than two years, particularly for executive function and language. Conversely, television viewing has positive and negative outcomes for preschool children[49].
Meanwhile, media play has more positive results in older children. Educational video games targeting middle-school to college students increase learning achievement by 7%-40% more than lecture-based learning[47]. We should also emphasize that technology will never replace traditional play. Children still need outdoor playing, pretending, hard book reading, manual drawing, and other forms of play that enhance manual dexterity. Media and video games should only be considered tools to enhance child play and learning within monitored contexts, age groups, and evidence-based practices. It is critical to mention that the effects of flat-screen media usage on developing brains are detrimental, especially for children below two years old. Children between two to five years old are advised to have no longer than one hour of daily flat-screen use[50].
THE SEXUAL DIFFERENCES IN PLAY
The differences in play between boys and girls are related to many factors, particularly parents and other social influences (e.g., local cultures and media). Physique is also an essential factor in sex differences in play. Tissera et al[51] found that adolescent males outperformed females in all off-court fitness characteristics. Sex differences in play appear as early as 18 mo of age. Caldera et al[52] and Dinella et al[53] showed that these children demonstrated more interest when playing with same-sex-typed or neutral toys than when playing with cross-gender toys. This sex-typed play continues to increase as they get older[52,53].
Boys differ from girls in three aspects of play: preferred play partners, toy choices, and social play. Boys usually prefer dynamic toys such as rocket ships, vehicles, cars, trucks, boats, mechanical sets, and toy weapons such as guns and swords, while girls prefer cosmetics, passive nature—dolls, dress-up costumes, and household toys such as toy stoves and tea sets. Most children (80% and 90%) favor playmates of the same sex. Hence, girls prefer to play with girls, and boys prefer to play with boys. Boys are more physically active than girls, so they also prefer aggressive and rough play, such as chases, fights, wrestling, and other kinds of rough play[54-56]. Lamminmäki et al[57] did an exciting study to explain the difference between boys' and girls' play. They correlated the testosterone levels with the play type. They found that testosterone levels in boys significantly and positively correlated with playing with a train and negatively correlated with doll playing.
EFFECT OF THE PLAY ON THE BRAIN
Cortico-cerebellar system is a neural system involved in complex cognition and creating complex behavior, including play[58]. Play induces epigenetic molecular changes, enhancement of neural cell connectivity, behavioral modifications in executive functioning skills, socioemotional status and learning, and adaptive and prosocial behavior. Play affects all the brain's areas, structures, and functions, including the upper and lower brain and the right and left hemispheres, particularly for sensory integration and processing. The prefrontal cortex is the anterior part of the frontal lobe. It is considered the brain's executive control center, involved in cognitive control, planning complex cognitive behavior, decision-making, personality expression, controlling social behavior, managing attention, prospective memory, impulse inhibition, and cognitive flexibility[5]. The more engaging in free play, the more the brain builds new circuits in the prefrontal area to facilitate the navigation of these intricate social interactions. Play through increasing dopamine and gamma-aminobutyric acid (GABA) causes prefrontal cortex changes and increases its wiring, enhancing the executive control system involved in controlling emotions, problem-solving, plan-making abilities, and whole brain sensory integration and information processing speed[59]. Designing special programs with active and dynamic play elements may be more effective in stimulating executive function development due to the influential early motor learning and the social motive aspects of learning[60].
A healthy brain is a well-integrated brain, where various parts of the brain can co-transmit a message to each other and work in harmony as one unit. Play increases whole brain integration, like sensory integration and processing. Play increases physical movement, enhances creative self-expression, and increases self-regulation practice. Therefore, play helps the integration of the left cerebral hemisphere with its logical, analytical, personal narrative, and emotional language with the right cerebral hemisphere with its creativity, expression, and sensations functions[5]. In addition, play triggers the brain's incentive circuitry but not harmful stress responses, enabling proper attention and action[61]. Not only the prefrontal cortex is modified by play, but the lower brain regions as well. Play affects these regions due to motor regulation, emotional engagement, and the children's trials to build a sense of safety and to create physically 'safe' worlds with continuous repetitive motor, emotional and sensory feedback to and fro involving the neural network with a continuous rewiring process, benefiting from the high brain plasticity during childhood. Kerney et al[58] found a positive association between the relative size of the cortico-cerebellar system's main components and the amount of play in a sample of primate species.
Play refines the medial prefrontal cortex's dendritic length, density, and spine complexity at the cellular level. Play also stimulates the production of the brain-derived neurotrophic factor (BDNF) in the amygdala, hippocampus, dorsolateral frontal cortex, and pons, supporting existing neurons' survival and promoting the new neurons' and synapses' growth and differentiation[62,63]. A 30-min play can modify the expression of approximately one-third of the 1200 genes (especially the BDNF gene) present in the posterior and frontal cortical regions within an hour[64,65]. Two hours of daily play showed significant changes in the weight and efficiency of the experimental animals' brains[66]. Conversely, play deficiency impeded the process of pruning and synaptogenesis with impaired problem-solving and executive functioning skills and less behavioral flexibility[67,68]. Play affects the level of brain neurotransmitters, increasing dopamine levels in substantia nigra and ventral tegmentum neurons, activating norepinephrine which facilitates synaptic learning and improves brain plasticity, and decreases levels of the stress hormone cortisol[5,69].
PLAY THERAPY
Play therapy has been implemented in psychiatry for nearly e century. However, it has been practiced for hundreds or even thousands of years. Play therapy is mainly intended to help children. It is a way in which the children use play to honor their unique mental abilities and developmental levels to window up their feelings, emotions, wishes, wants, desires, joys, fears, anxiety, worries, and communication as a play language. The main aim of play therapy is to prevent or solve psychosocial difficulties and achieve optimal child-healthy growth and development[70]. It enables the child to overcome different obstacles in the pathway to proper development, helps the child to be more responsible in his behavior, and develops successful strategies and creative solutions to problems. It also trains the child to respect and accept himself and others, learn how to express his feelings and emotions, and respect others' thoughts and feelings[71]. Play therapy can be used as a diagnostic and therapeutic tool. Initially, the play therapist observes the child during playing to identify the child's problem; assess his/her problem. Then, the therapist deals with the problem accordingly by scaffolding and supporting the child to learn and execute self-expression and communicate via his/her thoughts of the inner world. The therapist helps overcome unresolved trauma, enables the child to master and execute a new coping mechanism, redirects inappropriate behaviors, and enriches adaptive behavioral responses[59,72].
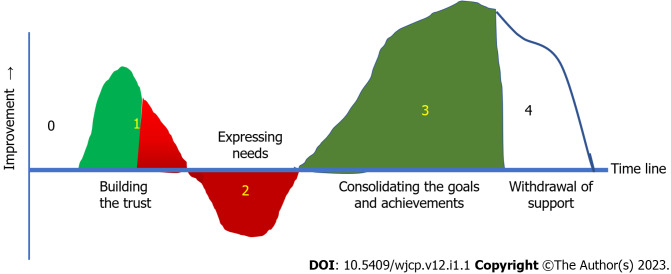
Although play therapy schools differ in their philosophy and techniques, they all incorporate play's therapeutic effects and developmental assets[73]. Each play therapy session lasts about 30 to 60 min, once a week or so. Play therapy has four primary therapy stages after an initial phase of an interview with the family and child with a preliminary treatment assessment (Table 1 and Figure 3). The number of sessions in each phase depends on the child's needs and response to this type of therapy. Therapy can occur individually or in groups.
Table 1.
Stages of play therapy
|
Stage order
|
First
|
Second
|
Third
|
Fouth
|
| Name of stage | Initiation phase or exploratory stage | Resistance phase, negative reaction, aggressive stage | Growing phase, or work phase | Termination phase |
| Duration | Initial 4-6 sessions | Few sessions to a few months | The longest phase | Gradual decrease the number of sessions to every other week or once a month to see if the child can maintain the progress with less support |
| Aim | The child gets to know the room, the therapist, and the toys, learn the roles of each participant and what is expected from him and develops a bond with the therapist | To help the child confront his maladaptive behavior, helps the child to express his emotions and learn how to communicate his feeling in his body in an acceptable way to society, and start accepting the new changes | To start learning, healing, stepping out of the child's comfort zone and making changes with an improvement of self-esteem, behaviors, communication, and overall outlook on life | To gradually withdraw the play therapy when the child reaches behavioral and emotional function stability in different situations |
| Counselor role | Acknowledge the child's presence and let the child be aware of his presence | The counselor confronts the child with his maladaptive habits and pushes him to decide to put in the work or keep fighting because it feels difficult | To help the child better address and understand his difficulties, how to best overcome these difficulties, and how to live happier and playful life by utilizing practical coping skills with little prompting, demonstrate self-regulation, and build resiliency and flexibility with change | To ensure that the child is consistently demonstrating his new skills with ease, and that behavioral and emotional needs have stabilized in multiple environments |
| They are building a trusting relationship and fostering a safe environment for the child to express himself freely | ||||
| To support what the child achieved during the few appointments the child does | ||||
| Parents Role | The parents may attend the first session to support and encourage him till he is used to the therapist | They can support and encourage the child to give the treatment a chance to begin working | They should practice empathy and remain consistent with their expectations. They should support the child emotionally and remind him of his new skill set | They should compensate for the decreasing number of appointments by building a bridge of trust with their child |
| Child status | The child explores the playroom and the toys. He may have a desire to touch and try out everything he sees to gain an awareness of what is available to him. He also could be hesitant and uncertain about his role in the playroom and look to the therapist to take the lead. He needs to know what to do and what not to do | The child shifts from the comfortable to the uncomfortable zone with a loss of familiarity and starts the change. The child may no longer want to attend therapy | The child will achieve significant advances. However, he may have regression into some of their pre-existing problem, behaviors, or symptoms. This regression may frustrate both child and parents | The child feels this stage is difficult as the secure relationship he had developed with his therapist will start to change with fewer appointments. He feels as if he is being punished for making positive changes |
Figure 3.
Stages of play therapy. Stage 0: Pre-therapy family and child interview and assessment; Stage 1: The first part in green is the exploratory or Initiation stage, followed by testing for protection (part in gradient red); Stage 2: Resistance phase, negative reaction, or aggressive stage; Stage 3: The growing or work phase; Stage 4: The termination phase.
The first phase is the initiation phase or exploratory stage, which is the most critical time when the child explores a new atmosphere (the playroom, the play therapist, and the play therapy process) not used to and starts to adapt himself to it. The duration of this phase depends on the child's personality. This phase becomes longer if the child exhibits more shyness and introverted traits. The child usually needs the family's encouragement, so he or she will provide the therapist a chance to begin working. Once the child is comfortable expressing himself, he realizes his role as an active agent and develops a sense of security necessary for advanced therapeutic work; he moves into the next stage of play therapy after being tested for his non-so-socially acceptable behavior. After successful testing, some children may experience the resistant (aggressive) phase when confronted with their maladaptive behavior. In this stage, the child resists change and may actively avoid attending play therapy sessions. Some children may pass this phase rapidly within a few sessions, while others may need months to overcome that[74,75].
After passing the resistant phase, the actual work phase comes, as it is the most crucial and usually the longest part of play therapy. The child is ready in each session to exert the hard work needed for personal growth and recognize his or her problems, how to best solve those problems, and how to survive a much happier and more active life. He improves his self-esteem, communication, behavior, and general attitude toward life[76]. Occasionally, the child may show some regression and step back, but with the parents' and the therapist's support, he overcomes it. When the child shows a consistent demonstration of his new skills easily, achieves the targeted therapeutic goals, and shows emotional and behavioral stability in different situations and environments, we can start the termination phase in which we gradually decrease the frequency of the session to once weekly and then monthly until we discharge the child, provided that the child maintains his progress with less support. Some children may feel frustrated during this phase due to their feeling of being punished for achieving positive outcomes[77].
The play therapist should create and hold a safe space for the child. He should be able to reflect feelings and behaviors with unconditional positive regard. He creates a permissive environment for the child where anything can be expressed. At the same time, he should set boundaries when necessary to ensure an appropriate holding environment. The therapist observes and gains perceptions of the child's problems; then, he can help the child explore his emotions and deal with any unresolved trauma by scaffolding the child and the therapeutic achievement[78]. The therapist uses play to help children redirect unacceptable behaviors, discover and practice new coping mechanisms, and form new functional neuronal circuits and healthier epigenetic mechanisms. Therefore, the therapist should have competent clinical, psychological, and occupational Knowledge, exceptional communication skills, a calm, patient, and friendly manner, with the ability to understand a variety of emotions and behaviors and to adapt to change and handle stressful situations. As play may need physical effort, the therapist should be physically fit to work on the floor or perform various physical activities[72].
Effects of play therapy on the brain
Play is an emotionally pleasing and creative experience that raises oxytocin levels. The Oxytocin hormone boosts feelings of emotional well-being and trust. Thus, Oxytocin facilitates the therapeutic relationship between the play therapist and the child, which helps the child to use his imagination and makes him ready for behavioral change. Play also activates the mirror neurons, which helps the therapist to read and interact with the child's emotional status accurately. Play therapy encourages the formation of new neural circuits and promotes neuroplasticity[79]. Play therapy-induced neuroplasticity through four main pathways: empathic harmony, which provides the ideal chemical environment to develop new neural pathways; emotional provocation, which consolidates and integrates the neural pathways; affect and cognition integration which helps the emergence of complex, elegant neural outlines, and co-constructing nonverbal narratives of self-cognizance and changes[80,81]. Play therapy allows the child to integrate the creative, emotional, and expressive functions of the right brain with the logical, rule-oriented, and analytical functions of the left brain. The brain needs 400 repetitions to develop a new synapse; play helps the brain create a synapse for every 10-20 repetitions.
Indication of play therapy
Although play therapy can help people at any age, it is characteristically used to help children 3-12 years of age. Play therapy may be helpful in various circumstances; some examples are mentioned in Table 2. Play therapy can help three categories of children; healthy kids, children with organic diseases, and children with mental or psychological problems.
Table 2.
Indications of play therapy
|
Children categories
|
Indication
|
| Physically and mentally normal kids | Family issues, like divorce, separation, or death of a close family member |
| Natural disasters or traumatic events | |
| Domestic violence, abuse, or neglect | |
| Grief | |
| Functional gastrointestinal disorders such as eating and toileting disorders | |
| Substance abuse | |
| Before routine childhood vaccination | |
| Physically-ill children | Facing medical procedures, chronic diseases, or palliative care |
| Mentally and psychologically ill children | Post-traumatic stress disorder |
| Developmentaltal delay or learning disabilities | |
| School behavioural problems | |
| Aggressive or angry behavior | |
| Attention deficit hyperactivity disorder | |
| Autism spectrum disorder |
Healthy kids
Play therapy can help the child become more responsible for certain behaviors, develop coping strategies, enhance creative problem-solving skills, learn self-respect, respect others, express feelings, and strengthen family relationships. Play therapy is indicated for children passing through a transition time in their lives, such as a change of place of the house or school environment, parental divorce, a loss of a loved person, or the birth of a new sibling. Play therapy also helps children suffering from bullying phenomena, domestic violence or abuse victims, or suffering social withdrawal[82]. It could also help children with functional disorders such as toileting, eating, or sleep disorders[83]. Play therapy helps to release the child's tension and facilitates the adult's communication with the child's inner world. Play can also help prepare the child for routine vaccination. An exciting study by Pontes et al[84] showed that children prepared with therapeutic play before vaccination are more cooperative and accept more than those without preparation.
Physically-ill children
Children with a chronic medical condition that needs frequent hospitalization, such as cancer, are more liable to stress, anxiety, and fear related to their illness and treatment. In addition, children who are undergoing major surgery usually encounter significant preoperative anxiety and fear. Play therapy can help minimize the worries caused by hospitalization or surgical procedure, assist in the fight against the disease, and modulate the child's immunity. Play allows proper lymphatic system pumping, boosts the immune system, and decreases stress, reducing the over-responsiveness of the hypothalamic-pituitary-adrenal axis system[85].
Mentally and psychologically-ill children
Children with certain illnesses hampering their emotional and social expressions usually benefit significantly from play therapy. For example, play therapy may have moderate to high positive effects on children with post-traumatic stress disorder (PTSD); however, these effects need more studies[86]. Children with mental and developmental retardation have a reduced attention span, poor eye-hand coordination, restricted memory, and weak concentration. Play is more effective, long-lasting, and understandable than traditional teaching activities[87]. Play also reduces the impact on parents after having their child diagnosed as mentally or developmentally disabled. It also helps to build more bonds and interactions between parents and their disabled children[88]. Children with aggressive behavior have reduced expressive or reflective verbalization capacity, reduced dramatic or imaginative play, and tend to feel highly threatened by the therapist's slightest observation or inquiry. However, play therapy helps reach these children when chosen and performed correctly. It is most helpful when used to assist these children in developing mature adaptive social skills and responses through building nonthreatening relationships[89]. Attention deficit/ hyperactivity disorder (ADHD) is prevalent in children and adolescents. Abdollahian et al[90] found that play therapy can significantly decrease the symptoms of ADHD. The significant differences between the experimental and control groups indicate that play therapy could be an effective treatment method for children with ADHD aged 7-9 years[90]. Some children with autism spectrum disorder (ASD) have deficiencies in play. In this article, we will review the efficiency and limitations of play therapy in children with autism.
PLAY DISORDER IN CHILDREN WITH AUTISM
Autism spectrum disorders (ASD) are a spectrum of neurodevelopmental disorders with classic core symptoms of social deficits, language impairment, and repetitive and restricted behaviors. It has an increasing prevalence all over the world (1/1000 population) with wide heterogeneity from one country to another, reaching a very high level in the United States (1/40-60 population)[91]. The exact mechanism of autism is controversial. However, atypical neurobiological mechanisms obviously underlie the disorder with documented defects in the cerebellum, limbic structures, and cortex, especially the frontal lobe[92]. Frontal lobe dysfunction impacts specific cognitive functions of patients with autism, such as memory, learning, face recognition, emotional judgment, and interpreting biological motion cues[93,94]. The social impairments observed in patients with autism may be related to the impairment of social signals interpretation[95-97].
There is difficulty in comprehension and atypical sensory processing in children with autism. They have limitations in their adaptive behavior and impairments in their ability to relate and interact socially with others, with the presence of significant communication challenges and restricted or stereotyped behaviors[98]. As play needs integration of motor, social, language, and communication skills, it is usually significantly impaired and very limited in children with ASD. They prefer to play alone, engage in selected types of repetitive play such as lining up toys, moving objects from a particular place to another one, or playing with the same toys all the time, and they develop rage attacks and/or tantrums when the parents try to remove them[99,100].
Children with autism struggle to share experiences with others, understand the feelings and thoughts of others, pay attention, respond to others, and/or take turns. They may be unaware of the surrounding children. They have challenges learning new play skills via observation or communication. They lack symbolic play and joint attention, representing two critical developmental challenges in young children with autism[101]. They also have a problem understanding the non-verbal cues of body language, such as facial expressions, gestures, and voice tones. They have difficulties copying simple actions or exploring the environment. They also have a problem with imaginative and pretend play. They are critical features for successful interactive play. They are unlikely to share in games that need making decisions, cooperation, or social communication[102,103]. Children with autism usually get "jammed" in the earliest forms of solitary play. They prefer purposeless, meaningless, and repetitive actions that mean something to them without meaning to the typical people around them. Children with autism also show symptoms of restricted and repetitive behavior. Atypical play behavior appears early in life and depends on the severity of the autistic features.
When getting older, some children with autism may improve their playing skills and understand some rules of games. However, their behavior during play is still different from their typically developing peers. They may strictly adhere to the game rules, so they may be unable to cope with any logical changes in the game. They also may become obsessed with particular video games that provide solitary play. They also may show over-concentration on and adherence to a particular game point. For example, they may concentrate on the football player's T-shirt color without actually playing the game. These symptoms may develop into obsessive-compulsive disorder if untreated in the long term[102].
PLAY AND OCCUPATIONAL THERAPY FOR CHILDREN WITH AUTISM
Occupational therapy is a well-known therapy used to support the development of children with autism to use their senses (gustatory, olfactory, tactile, vestibular, proprioceptive, auditory, and visual systems) to make sense of their environment. Ayres Sensory Integration is one of the most renowned evidence-based approaches to promoting children’s play[59,104]. Sensory integration is a specialty area of occupational therapy based on over 50 years of theory and research originated at USC by A. Jean Ayres. Sensory integration is a process that begins with receiving sensory inputs by the senses and interceptors from the environment and within the body. Then these sensory inputs are perceived, processed, and integrated into the brain to give an adaptive response, functional reaction, adequate communication, and typical behavior right on time[105]. Play therapy blended with sensory integration is a structured therapy commonly used by occupational therapists to involve children and develop emotional well-being, functional development, and typical growth[106].
Despite lacking play skills in children with ASD, they still can learn how to play, especially with the help of their parents and sibling. The parent's role is crucial in managing the child's difficulties. Parental denial or ignorance worsens the symptoms and makes the likelihood of successful therapies minimal or nil. In addition, the effects of therapy depend on the time of initiation; the earlier, the better[106].
Play therapy in children with autism aims to engage them in playful activities of their choice and interest. It helps them to express themselves freely and comfortably. Play therapy depends on building partnerships and trustable solid relationships between the therapist and the children through involvement in the joyful activities of playing[107]. Play therapy helps children with autism to change their way of self-expression from unwanted behavior such as aggressive, self-injurious, property destructive, or tantrum behavior to more non-injurious expressive behavior using toys or activities of their choice as their words. Since verbal expression is difficult in children with autism, play therapy offers them different ways to express their suppressed emotions. Children with autism have poor social skills, so play therapy emphasizes the relationship-building trust with the person through interaction and having fun with the play therapist[89]. Play therapy also helps children with autism experience how to feel various interaction styles, whether they realize that or not. It also provides those children with a safe environment to learn self-regulatory behavior, which helps to emphasize appropriate behaviors and decrease unwanted ones, such as aggressive or destructive behaviors. At the same time, the child experiences freedom of choice during playing, like choosing what he likes and desires, controlling the speed and time of activities of the session, and deciding what he wants to do. Thus, play helps him develop independence with time, a valuable developmental stimulant[108].
Autism is a spectrum with heterogenous symptoms; every child with autism is unique and responds differently. Children with autism usually prefer sensory toys such as weighted stuffed animals, fidget toys, and putty, because these toys help calm the children and encourage them to engage their senses during playing positively[109]. Currently, no specific play therapy is standardized for treatment. Because every child responds differently to different things, some traditional play therapy methods have been constantly shown to improve social and emotional skills in children with autism over time. The efficacy of play therapy depends on many factors, as illustrated in Table 3. However, occupational therapy using the sensory integration theory is evidence-based to uses a child-friendly playful method to enhance the neuronal connections of the brains of children with ASD[59].
Table 3.
Factors affecting the success of the therapy
| The child's age at the time of initiation of the therapy |
| The degree of cooperation, awareness, and adherence of the parents and the family |
| The severity of the condition |
| The developmental level |
| The marital status of the family |
| The family education and socioeconomic levels |
| The therapist's competency |
| The type of play therapy |
Child-centered play therapy
Child-centered play therapy is one of the most comprehensively studied types of play therapy in children with autism. This type of therapy is a relationship-based intervention, where the therapist enters the child's world and uses the built relationship to intervene rather than train the child. Schottelkorb et al[110] investigated the intensive child-centered play therapy effectiveness in children diagnosed with ASD. They found that children who received intensive child-centered play therapy significantly reduced ASD core symptoms and behavioral disorders, such as attention problems, externalizing problems, and aggression, than control group children[110]. Novita et al[111] found that child-centered play therapy effectively improved joint attention skills in children with ASD. Joint attention is one of the first types of visible communication that implies the child's ability to coordinate his attention around an object or event with a social partner. It is observed when the child displays evident skills such as alternating gaze between an object and a person, drawing attention to, pointing, or offering to share or show[111].
Carrizales[112] showed that child-centered play therapy showed positive growth in a range of areas in young children with ASD. She studied three children with ASD who showed varying degrees of improvement concerning play skills. Three of them showed more natural play, two of them showed advanced play skills, and one of them showed fewer play skill changes. These findings support the theory that a safe, acceptable environment provides children with ASD with more motivation and capacity to freely and naturally interact intimately with the external environment and improve their self-healing power[112]. This type of therapy is not only child-centered but also therapist-dependent. Goodman et al[113] showed that the child's response to the treatment differs according to the therapist, even though the child remains constant. Child-centered play therapy is part of an integrative treatment approach that includes behavioral techniques and parental training. It improves parent education, training, and the child's social skills to improve the child's functioning and correct maladaptive behavior. Child-centered play therapy is a promising intervention in increasing children's emotional and social behaviors with ASD[114]. However, we still need more research to establish whether child-centered play therapy is effective in children with ASD.
Child-led play
Since it is very challenging to direct children with ASD to do specific actions, especially in severe cases, we need to find a way to attract the children's interests while helping to pull them out of their shells; so they do not stick to their repetitive behaviors. This method is called a non-directive approach in which the therapist follows the child’s choices and adapts the tools and environment to serve the therapeutic goals. Child-led play is an approach that allows the child to choose the activity they like to do, and the therapist joins them. It is usually helpful in severely affected children with autism, but it takes a longer time to see significant gains[115]. Child-led play therapy has improved children's social and communication skills with severe autism. It differs from child-centered play therapy, in which there is a preset specific thing and rules the therapist will do and not to do and a specific way of being in the playroom. Gengoux et al[116] showed the efficacy of a pivotal response treatment package (PRT-P) for children with autism. PRT is play-based therapy initiated by the child. They investigated 48 children with Autism with PRT-P for 24 wk. PRT-P demonstrated more significant improvement in child social communication skills and in teaching parents to implement PRT[116]. de Korte et al[117] also showed a significant improvement in spontaneous initiations during the 14-wk protocol of PRT with a semi-structured therapist-child interaction and widespread increases in overall clinical functioning[117].
Floor time-play therapy is one of the most famous play therapies to treat children with ASD, discovered by Wieder and Greenspan[118] in 1980. It can be done at home and in the therapist's office, in a calm environment for a session between two to five hours. It can be provided by child psychologists, occupational therapists, speech therapists, special education teachers, parents, or caregivers with adequate training[118]. Essentially, the therapist or a caregiver sits on the floor to play with the child according to the child's own terms. In this therapy, the therapist or caregiver starts playing, following the child's way of playing (non-directive; the therapist follows, and the child leads). Then, the therapist introduces new elements, such as new toys, acts, or some words (hidden directive). This way of playing with back-and-forth conversations between the child and the therapist ultimately helps the child focus his thinking, improve his emotional skills, and expand his communication circles[119]. With the child's progress, floor time play can also be practiced with typically developing peers when done in a preschool setting. The main aim of floor time play therapy is to meet the child's developmental level, build on the child's own comforts, interests, and strengths, and create relationships during the play course[119].
Floor time play can help the child to improve different critical developmental milestones. It provides him with two-way communication that may progress to more complex communication. It helps him to develop inspirational ideas and emotional thinking, which enables him to enjoy intimacy and engage in relationships. Ultimately, it helps the child improve his self-regulation, enhance emotional and intellectual growth, and empower his interest in the world[120]. Studies show that children with autism significantly improved overall development with 25 h of floor time play per week for a minimum of two years. Wieder et al[118] showed that spontaneous 'floor time' play sessions for three years helped a young boy improve his attention, engagement in simple and complex gestures, and problem-solving skills to guide the child into the outside world with lots of ideas and improve abstract thinking. Solomon et al[121] studied the effects of 8-12 mo of floor time play therapy in 68 children with ASD. They encouraged the parents to deliver 15 h per week of 1:1 floor time interaction. They found that 45.5% of children achieved good to excellent progress in their functional development with significant increases in child subscale scores[121]. Pajareya and Nopmaneejumruslers found that 14 h/week for one year of floor time parenteral playing with their children showed improvement in the development and decreased signs of autism in 47% of 31 children with autism[122]. In addition, Liao et al[123] found in a pilot study involving 11 children with ASD that the floor time home-based intervention program for ten weeks significantly improved mean scores for the children's communication, emotional functioning, and daily life living skills with positive changes in the parent-child interactions. However, the success of floor time play depends on many factors. Praphatthanakunwong et al[124] showed that being married, with a lower income, and having higher awareness of floor time play theory are associated with higher parent engagement. They also found that the more severe the autism and the longer the treatment continuation, the more parent engagement and child development improvement[124].
Clown therapy or medical clowning
Clown therapy is currently an essential aspect of managing hospitalized children worldwide. Clown doctors help to minimize the child's stress and anxiety related to the hospital atmosphere during surgical procedures or particular devastating therapies[125]. Clown therapy should be differentiated from the clown person that enters the hospital to cheer up kids and alleviate their tension. Clown therapy (or medical clowning) mimics drama therapy, which helps patients to discover their inner clowns and release clown-like behavior in group settings. This therapy helps patients to discover the absurdity and paradoxes in their everyday lives. They also find new o communication methods[126]. There are scarce data about using Clown therapy in treating children with ASD. However, Shefer et al[127] showed that medical clowning sessions enhanced communication in children with ASD during the interventions compared with other interventions. It caused a reduction in stereotypic movement frequency in children with ASD over time[127].
3i play therapy (intensive, individual, and interactive)
The 3i play therapy was induced by Catherine de La Presle in 2004 in France to help her grandson, who had autism. It. It works through play and is conducted at the child's home, with the involvement of many volunteers to provide several hours daily of individual therapeutic relations to the child. It is an educative method with several elements, including the importance of play, with a low-intrusive approach that emphasizes interaction and behavioral dialogue and ensures the child's excellent and long-lasting mental stability. Developing self-consciousness and mental capacities are obtained through developing relations and stimulating the need for communication with others[128]. Tilmont Pittala et al[129] studied 20 children with autism using the 3i method for two years. They showed that children treated with the 3i method for two years had significant behavioral and developmental skills improvement with an evident decrease in autism severity. Their results suggested that the 3i method can be a valuable tool for children with ASD by improving their daily interactions and social environment[129]. Brefort et al[130] did a more extensive controlled study that involved 90 children with ASD receiving 3i therapy (intensive developmental play therapy) for two years. They found that 3i therapy improves ASD severity with observed interaction, communication, and repetitive behavior improvements[130].
Integrated play groups
This model is a play-dependent intervention intended to develop meaningful peer relationships and adequate play and social-communication skills in children with ASD through adult-facilitated peer interactions. It involves neurotypical children, "expert players," and children with autism ("novice players") playing together so that the latter can learn better social skills. A trained adult facilitator serves as a "play guide" to assist and outline interactions between expert and novice players. The facilitator divides the children into mixed groups. Each group has three to five children’s groups. The facilitator sets the tones and rules for the play before they take control[131]. Yang et al[132] investigated the effect of integrated play groups (IPGs) on children with ASD playing with typically developing familiar (siblings at home) and unfamiliar peers (at school in Taiwan. They studied the effect of IPGs on the symbolic and social play of two children with ASD in early elementary school. They noted significant gains in symbolic/pretend play and reciprocal social interaction while participating in IPG[132]. Recently, Wolfberg et al[133] studied the effects of 12 wk of IPG therapy on 48 children with ASD participating in play groups with typical peers. They found significant increases in symbolic and social play using unsupported play with both familiar and unfamiliar peers, which maximizes the developmental potential and social inclusion in children with ASD[133]. A 30-min IPG session twice weekly for 16 wk can improve the child's ability in pretend play and his interaction with his peers. IPG also helps the child with ASD learn how to use the toys more typically.
Joint attention symbolic play engagement and regulation
Joint attention symbolic play engagement and regulation (JASPER) is a well-studied naturalistic intervention to improve developmental behavior. This method aims to improve the attentiveness of the child with autism by training him to focus on a toy and another person simultaneously (joint attention). This method improves the child's language and play, making it more effective and reactive with his peers, increasing pretending abilities, and expanding the range of play with different toy types. The child may need to spend up to 25 h weekly in a one-to-one meeting with his therapist. In addition, some preschools can provide this type of therapy. Most studies showed that children who received JASPER intervention significantly improved as a minimum outcome related to joint child engagement, joint attention, play, and language skills compared to the control groups[134]. Goods et al[135] tested the effects of 30 min of JASPER intervention twice weekly for 12 wk in children 3 to 5 years old. The intervention induced greater play diversity upon standardized assessment. This effect also appeared in the classroom, where participants in the intervention group started showing more signs of engagement and spent less time without than before[135]. Shire et al[136] investigated how toddlers with autism engage with their peers. They found that children who experienced peer intervention (JASPER ) had more engagement with their peers, more receptive language, and better combination and presymbolic play when an adult was present, but not when the children were left unsupported[136]. JASPER can also be conducted online. Shire et al[137] showed that a technology-enabled adaptation of the evidence-based caregiver-mediated JASPER successfully provided the caregivers with online materials that helped them conduct home-based JASPER. The caregivers navigated the content smoothly and gave positive feedback and suggestions to improve the content[137].
However, children may differ in their response to JASPER. Some may show incredible progress, while others may have slow or no progress. Panganiban and Kasari studied 99 preschool-age children with ASD and limited language for their language improvement after JASPER intervention to predict their response to JASPER. They divided the children after the intervention into super responders and slow responders using traditional standardized assessment tools of behavioral and cognition data. They found that children who could play appropriately with a more comprehensive toy diversity before starting the intervention had the best improvements in their expressive language[138]. However, we need more research to verify whether it can also improve a more comprehensive range of symptoms and outcomes in children with ASD.
Synergetic play therapy
This approach identifies the significance of the comprehensive therapeutic experience the child is exposed to, including different factors in the therapy, such as the child himself, the therapist, the parents, and all other factors that could impact the child's progress. So, this approach that Lisa Dion created tries to use all the details of the child's life to work in harmony to create a balanced and all-encircling response to the problem the child enfaces. This approach determines a specific role for everybody in the child's life, such as a sibling, cousin, classmate, friend, grandparents, and every other tie they live into[139]. This approach is not straightforward as it is a system of life and existing that concentrates on a more natural and comprehensive approach to therapeutic interaction. When done correctly, this synergetic play therapy (SPT) approach helps the child to co-regulate his internal experience, overcoming his challenging, uncomfortable memories, thoughts, and body sensations. So SPT is a comprehensive play therapy approach that concentrates on the child and the therapist realistically interacting with each other and themselves in an attempt to become more thoughtful. This approach allows for better child development and maturation[139]. Dion and Gray[140] showed that SPT provoked significant improvement in emotionally tolerant behaviors percentage in response to trustworthy therapist expressions from the first to third sessions of SPT. SPT also had a 100% success rate in inducing emotionally tolerant behaviors by their fifth session[140]. Unfortunately, there is very scarce data about the effects of SPT on children with autism, and there are no well-controlled studies. Simmons[141] studied two children using SPI, one of them was a nine-year-old boy with high-functioning autism suffering from aggressive behaviors and difficulty managing his emotional range. He had a one-hour session weekly for 13 wk. The boy has made noticeable progress across several parameters; he was more able to control his anger, engage in cooperative play, and make eye contact effectively[141].
Equine-partnered play therapy
Equine-partnered play therapy (EPPT) is a distinctive type of play therapy intended for children aged three to nine. It uses the special relationship between animals and children. This model of therapy is a modified child-centered play therapy (CCPT) that blends Equine Assisted Counselling with CCPT. In CCPT, children see, explore the world, and express themselves through play[142]. In EPPT, the child will express his thoughts, feelings, needs, and wants through horse riding rather than the toys used in play. In EPPT, horses serve as group members, allowing the child to enhance his social skills while getting feedback from the horses. Including miniature horses (small ponies), EPPT can support the child to feel safe and accept to be her/himself[143]. Horse riding helps the child to express complicated feelings, receive nurturing from the horse, receive feedback from the horse to ground the session in reality, gain self-control and decision-making abilities, and enhance personal responsibility, self-expression, self-direction, self-respect, and acceptance. The EPPT team consists of an equine specialist and a play therapist. However, safety and ethical considerations should be in mind while conducting EPPT. The environment should be safe and comfortable for both the horse and the child[144].
Bass et al[145], during their controlled study, showed that children with ASD who had horseback riding intervention for 12 wk demonstrated more excellent sensory seeking, sensitivity, and social motivation. They also had less distractibility, inattention, and sedentary behaviors. These results confirmed the therapeutic benefits of horseback riding in treating children with ASD[145]. Harris and Williams[146] showed a significant reduction in the severity of ASD symptoms and hyperactivity and improved social functioning in children with ASD after horse riding sessions of 45 min weekly for seven weeks compared to the control group. Another self-controlled study by Steiner and Kertesz[147] showed significant differences pre- and post-intervention in the length of the gait cycle that became more stable in the sagittal plane in 26 children with ASD who were subjected to horse riding for one month of therapy. A systemic review by McDaniel Peters and Wood showed that four types of equine-assisted therapies were identified from eight studies that reported improvements in motor control and self-care of children and adolescents with ASD[148].
Art-play therapy
Art therapy is a form of expressive and communicative therapy that uses the act of arty interest to decrease anxiety, enhance self-esteem and settle any psychological conflicts. This therapy is entirely different from play therapy. However, child art therapy is sometimes confused with play therapy, as many play therapists include art-based activities during play therapy. Meanwhile, some art therapists use specific play tools such as toys, puppets, or even physical games to enforce and promote the child's artistic expression. While play therapy is more valid for children aged 2-12 who can express themselves through movements, creative media, and play, art therapy is more suitable for 3-12, who can use visual language better than movement. Art therapy can be practiced individually or in groups, with a session usually lasting 30 to 50 min[149-151].
Wypyszyńska et al[152] showed that art therapy has a positive therapeutic effect on speech, social relations, and unusual behavior in children and adolescents with ASD than in the control group. A systematic review by Schweizer et al[153] showed that art therapy might provide a more compliant and relaxed approach that can empower the self-image and improve the learning and communicative skills of children with ASD. Art therapy can help to overcome poor social communication and repetitive and restricted behavior patterns in subjects with ASD. Art therapy, with its sensory experiences such as sight and touch, can increase flexibility and attention abilities and improve the social behavior of children with ASD[153]. Moghaddam et al[154] investigated the effects of family-based art therapy with the enforcement of verbal interaction, imitation, and phonation in children with autism. They showed that these practices helped children with autism to use art to express their connotations and feelings. Family-based art therapy also effectively reduces stereotypical behaviors and increases social interaction in children with ASD[154]. However, there is a strong need for further empirical well-controlled research to confirm the outcome of art therapy in autism.
Tele-play therapy
With the rise of the COVID-19 pandemic, there was a significant increase in the number of children with special needs, including those with autism. Besides the high morbidity and mortality related to COVID-19-, the pandemic negatively impacted the health and educational-related issues of children with autism. The lockdown negatively altered cognitive abilities, sensory-motor development, sleep, morale, and social and behavioral interactions in about 50% of children with special needs[155]. With the need to continue the services provided to children with autism, telemedicine, including teleplay therapy, provides significant help during the pandemic. Despite teleplay therapy being initially created to provide services to those in remote geographical locations, the pandemic experience paved the way for a new virtual platform where therapeutic play can continue regardless of the place and be provided across borders. Therapists can provide their services to another country and continue their services when traveling or when the child in need of the therapy travels. So, teleplay therapy decreases users' barriers to the therapists and the therapy procedure. Through teleplay therapy, children continue interacting with the world, communicating with others, practicing problem-solving, discovering their emotions and empathy, and provoking their brilliant imagination[156]. However, we emphasize that virtual play therapy does not replace face-to-face play therapy. It needs specific considerations to be followed to ensure safety, accessibility, and efficacy while conducting teleplay therapy. Despite many advantages, such as exploring the child's environment and less anxiety when enfacing strange people, teleplay therapy has many disadvantages. Teleplay therapy may enface various problems, including privacy, possible easy distraction, technological problems such as digital ecosystem malfunction, and connectivity problems[157,158].
LIMITATIONS OF THE REVIEW
Despite our effort to review all that was published, the research regarding play therapy in children with autism is minimal, and the number of cases in many studies is very few to make a solid conclusion. Therefore, we still have a long way to go to prove the efficacy of teleplay therapy with more well-designed controlled studies.
CONCLUSION
Play therapy is an effective tool in the management of children with ASD. However, it depends on many factors. Play therapy should be continuous as the effect may wane with discontinuation. It is hard to make a conclusion from the previous studies due to many limitations, including the weak experimental design, which makes the generalization of their results to the larger community difficult. Play therapy is usually conducted as a part of a comprehensive intervention, so it is hard to claim that the improvement in the participant's behavior was related to the play therapy intervention. More well-designed controlled studies are needed to understand and judge play therapy's effects on this particular group of children. Despite the weak evidence, play therapy still has a lot of potential benefits for patients and their families. It helps improve the child's social skills and communication in a relaxed environment, integrates the parents, strengthens the child-parent bond, and decreases the tension over the shoulder of the parents. In addition, play therapy has no significant side effects and is cost-effective. More research is needed to experiment with evidence-based therapeutic models on sensory integration play models, neuroscience, and developmental psychology to support children with ASD, the typical ones, and others during and after the COVID-19 pandemic. It is also worth studying the effects of play therapy on frontal lobe functions and neurobiology in children with autism.
ACKNOWLEDGEMENTS
We thank the editors and the anonymous referees for their valuable suggestions.
Footnotes
Conflict-of-interest statement: The authors declare that they have no conflict of interest.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: July 27, 2022
First decision: September 5, 2022
Article in press: November 23, 2022
Specialty type: Pediatrics
Country/Territory of origin: Egypt
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Liao JX, China; Masaru T, Hungary S-Editor: Gong ZM L-Editor: A P-Editor: Gong ZM
Contributor Information
Reem Elbeltagi, Department of Medicine, Royal College of Surgeons in Ireland - Bahrain, Busaiteen 15503, Bahrain.
Mohammed Al-Beltagi, Department of Pediatrics, Faculty of Medicine, Tanta University, Tanta 31527, Egypt; Department of Pediatrics, University Medical Center, King Abdulla Medical City, Dr. Sulaiman Al-Habib Medical Group, Manama 26671, Bahrainmbelrem@hotmail.com.
Nermin Kamal Saeed, Pathology Department, Salmaniya Medical Complex, Manama 12, Bahrain; Pathology Department, Irish Royal College of Surgeon, Bahrain, Busaiteen 15503, Bahrain.
Rawan Alhawamdeh, Pediatrics Research and Development Department, Genomics Creativity and Play Center, Manama 0000, Bahrain; School of Continuing Education, Masters in Psychology, Harvard University, Cambridge, MA 02138, United States.
References
- 1.Burghardt GM. Defining and recognizing play. In Pellegrinin AD (Ed.), The Oxford handbook of the development of play. Oxford: Oxford University Press, 2011: 9-18. [Google Scholar]
- 2.Campbell SB, Denham SA, Howarth GZ, Jones SM, Whittaker JV, Williford AP, Willoughby MT, Yudron M, Darling-Churchill K. Commentary on the review of measures of early childhood social and emotional development: Conceptualization, critique, and recommendations. J Appl Dev Psychol . 2016;45:19–41. [Google Scholar]
- 3.Milteer RM, Ginsburg KR Council on Communications and Media; Committee on Psychosocial Aspects of Child and Family Health. The importance of play in promoting healthy child development and maintaining strong parent-child bond: focus on children in poverty. Pediatrics. 2012;129:e204–e213. doi: 10.1542/peds.2011-2953. [DOI] [PubMed] [Google Scholar]
- 4.Vedechkina M, Borgonovi F. A Review of Evidence on the Role of Digital Technology in Shaping Attention and Cognitive Control in Children. Front Psychol. 2021;12:611155. doi: 10.3389/fpsyg.2021.611155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yogman M, Garner A, Hutchinson J, Hirsh-Pasek K, Golinkoff RM Committee on Psychosocial Aspects of Child and Family Health; Council on Communications and Media. The Power of Play: A Pediatric Role in Enhancing Development in Young Children. Pediatrics. 2018;142 doi: 10.1542/peds.2018-2058. [DOI] [PubMed] [Google Scholar]
- 6.Tanaka M, Szabó Á, Spekker E, Polyák H, Tóth F, Vécsei L. Mitochondrial Impairment: A Common Motif in Neuropsychiatric Presentation? Cells. 2022;11 doi: 10.3390/cells11162607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee GA, Lin YK, Lai JH, Lo YC, Yang YSH, Ye SY, Lee CJ, Wang CC, Chiang YH, Tseng SH. Maternal Immune Activation Causes Social Behavior Deficits and Hypomyelination in Male Rat Offspring with an Autism-Like Microbiota Profile. Brain Sci. 2021;11 doi: 10.3390/brainsci11081085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ratajczak HV. Theoretical aspects of autism: causes--a review. J Immunotoxicol. 2011;8:68–79. doi: 10.3109/1547691X.2010.545086. [DOI] [PubMed] [Google Scholar]
- 9.Rossignol DA, Frye RE. Mitochondrial dysfunction in autism spectrum disorders: a systematic review and meta-analysis. Mol Psychiatry. 2012;17:290–314. doi: 10.1038/mp.2010.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bjørklund G, Doşa MD, Maes M, Dadar M, Frye RE, Peana M, Chirumbolo S. The impact of glutathione metabolism in autism spectrum disorder. Pharmacol Res. 2021;166:105437. doi: 10.1016/j.phrs.2021.105437. [DOI] [PubMed] [Google Scholar]
- 11.Mennella JA, Jagnow CP, Beauchamp GK. Prenatal and postnatal flavor learning by human infants. Pediatrics. 2001;107:E88. doi: 10.1542/peds.107.6.e88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chelli D, Chanoufi B. [Fetal audition. Myth or reality] J Gynecol Obstet Biol Reprod (Paris) 2008;37:554–558. doi: 10.1016/j.jgyn.2008.06.007. [DOI] [PubMed] [Google Scholar]
- 13.Marx V, Nagy E. Fetal Behavioural Responses to Maternal Voice and Touch. PLoS One. 2015;10:e0129118. doi: 10.1371/journal.pone.0129118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marlier L, Schaal B, Soussignan R. Bottle-fed neonates prefer an odor experienced in utero to an odor experienced postnatally in the feeding context. Dev Psychobiol. 1998;33:133–145. [PubMed] [Google Scholar]
- 15.Aguilar R. Infantile experience and play motivation. Soc Neurosci. 2010;5:422–440. doi: 10.1080/17470919.2010.503618. [DOI] [PubMed] [Google Scholar]
- 16.Committee on the Science of Children Birth to Age 8: Deepening and Broadening the Foundation for Success; Board on Children, Youth, and Families; Institute of Medicine; National Research Council; Allen L, Kelly BB, editors. Transforming the Workforce for Children Birth Through Age 8: A Unifying Foundation. Washington (DC): National Academies Press (US); 2015. [PubMed] [Google Scholar]
- 17.Tobar FL, Lencina MJ. The "Learning Through Play" project. Importance of interdisciplinary work among children born prematurely and their family groups in an area of high socio-environmental risk. Arch Argent Pediatr. 2017;115:588–594. doi: 10.5546/aap.2017.eng.588. [DOI] [PubMed] [Google Scholar]
- 18.Chang MC, Weng CY, Yu JH, Cheng WL, Chu SY. [The Effectiveness of a Shared Reading Program Among Parents of Newborns] Hu Li Za Zhi. 2022;69:73–82. doi: 10.6224/JN.202202_69(1).10. [DOI] [PubMed] [Google Scholar]
- 19.Cooke BM, Shukla D. Double helix: reciprocity between juvenile play and brain development. Dev Cogn Neurosci. 2011;1:459–470. doi: 10.1016/j.dcn.2011.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fisch SM. Cross-platform learning: on the nature of children's learning from multiple media platforms. New Dir Child Adolesc Dev. 2013;2013:59–70. doi: 10.1002/cad.20032. [DOI] [PubMed] [Google Scholar]
- 21.Pellegrini AD. The role of play in human development. New York: Oxford University Press, 2009. [Google Scholar]
- 22.Chawla L. Childhood nature connection and constructive hope: A review of research on connecting with nature and coping with environmental loss. People Nat . 2020;2:619–642. [Google Scholar]
- 23.Marino AJ, Fletcher EN, Whitaker RC, Anderson SE. Amount and environmental predictors of outdoor playtime at home and school: a cross-sectional analysis of a national sample of preschool-aged children attending Head Start. Health Place. 2012;18:1224–1230. doi: 10.1016/j.healthplace.2012.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ridgers ND, Stratton G, Fairclough SJ. Physical activity levels of children during school playtime. Sports Med. 2006;36:359–371. doi: 10.2165/00007256-200636040-00005. [DOI] [PubMed] [Google Scholar]
- 25.Scott HK, Cogburn M. Peer Play. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022. [PubMed] [Google Scholar]
- 26.Broadhead P, Howard J, Wood E (eds) Play and Learning in the Early Years: From Research to Practice. London: SAGE Publications Ltd, 2010. [Google Scholar]
- 27.Orr E. Object play as a mediator of the role of exploration in communication skills development. Infant Behav Dev. 2020;60:101467. doi: 10.1016/j.infbeh.2020.101467. [DOI] [PubMed] [Google Scholar]
- 28.Serrada-Tejeda S, Santos-Del-Riego S, May-Benson TA, Pérez-de-Heredia-Torres M. Influence of Ideational Praxis on the Development of Play and Adaptive Behavior of Children with Autism Spectrum Disorder: A Comparative Analysis. Int J Environ Res Public Health. 2021;18 doi: 10.3390/ijerph18115704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee RLT, Lane S, Brown G, Leung C, Kwok SWH, Chan SWC. Systematic review of the impact of unstructured play interventions to improve young children's physical, social, and emotional wellbeing. Nurs Health Sci. 2020;22:184–196. doi: 10.1111/nhs.12732. [DOI] [PubMed] [Google Scholar]
- 30.Weisberg DS. Pretend play. Wiley Interdiscip Rev Cogn Sci. 2015;6:249–261. doi: 10.1002/wcs.1341. [DOI] [PubMed] [Google Scholar]
- 31.Gelman SA. Learning from others: children's construction of concepts. Annu Rev Psychol. 2009;60:115–140. doi: 10.1146/annurev.psych.59.103006.093659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Richard S, Baud-Bovy G, Clerc-Georgy A, Gentaz E. The effects of a 'pretend play-based training' designed to promote the development of emotion comprehension, emotion regulation, and prosocial behaviour in 5- to 6-year-old Swiss children. Br J Psychol. 2021;112:690–719. doi: 10.1111/bjop.12484. [DOI] [PubMed] [Google Scholar]
- 33.Skibbe LE, Montroy JJ, Bowles RP, Morrison FJ. Self-regulation and the Development of Literacy and Language Achievement from Preschool through Second Grade. Early Child Res Q. 2019;46:240–251. doi: 10.1016/j.ecresq.2018.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Garber J, Frankel SA, Herrington CG. Developmental Demands of Cognitive Behavioral Therapy for Depression in Children and Adolescents: Cognitive, Social, and Emotional Processes. Annu Rev Clin Psychol. 2016;12:181–216. doi: 10.1146/annurev-clinpsy-032814-112836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jago R, Tibbitts B, Willis K, Sanderson E, Kandiyali R, Reid T, MacNeill S, Kipping R, Campbell R, Sebire SJ, Hollingworth W. Peer-led physical activity intervention for girls aged 13 to 14 years: PLAN-A cluster RCT. Southampton (UK): NIHR Journals Library; 2022. [PubMed] [Google Scholar]
- 36.Al-Beltagi M, Bediwy AS, Saeed NK. Insulin-resistance in paediatric age: Its magnitude and implications. World J Diabetes. 2022;13:282–307. doi: 10.4239/wjd.v13.i4.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Committee on Physical Activity and Physical Education in the School Environment; Food and Nutrition Board; Institute of Medicine. Educating the Student Body: Taking Physical Activity and Physical Education to School. Kohl HW III, Cook HD, editors. Washington (DC): National Academies Press (US); 2013. [PubMed] [Google Scholar]
- 38.Gunter K, Baxter-Jones AD, Mirwald RL, Almstedt H, Fuchs RK, Durski S, Snow C. Impact exercise increases BMC during growth: an 8-year longitudinal study. J Bone Miner Res. 2008;23:986–993. doi: 10.1359/JBMR.071201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Best JR. Effects of Physical Activity on Children's Executive Function: Contributions of Experimental Research on Aerobic Exercise. Dev Rev. 2010;30:331–551. doi: 10.1016/j.dr.2010.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tomporowski PD, Lambourne K, Okumura MS. Physical activity interventions and children's mental function: an introduction and overview. Prev Med. 2011;52 Suppl 1:S3–S9. doi: 10.1016/j.ypmed.2011.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pfeiffer BA, Koenig K, Kinnealey M, Sheppard M, Henderson L. Effectiveness of sensory integration interventions in children with autism spectrum disorders: a pilot study. Am J Occup Ther. 2011;65:76–85. doi: 10.5014/ajot.2011.09205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Meherali S, Punjani N, Louie-Poon S, Abdul Rahim K, Das JK, Salam RA, Lassi ZS. Mental Health of Children and Adolescents Amidst COVID-19 and Past Pandemics: A Rapid Systematic Review. Int J Environ Res Public Health. 2021;18 doi: 10.3390/ijerph18073432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kim SJ, Lee S, Han H, Jung J, Yang SJ, Shin Y. Parental Mental Health and Children's Behaviors and Media Usage during COVID-19-Related School Closures. J Korean Med Sci. 2021;36:e184. doi: 10.3346/jkms.2021.36.e184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Robidoux H, Ellington E, Lauerer J. Screen Time: The Impact of Digital Technology on Children and Strategies in Care. J Psychosoc Nurs Ment Health Serv. 2019;57:15–20. doi: 10.3928/02793695-20191016-04. [DOI] [PubMed] [Google Scholar]
- 45.Priyam P, Sil A. Burnout: The Resident Evil - Perspectives from the Horses' Mouth! Indian Dermatol Online J. 2020;11:816–817. doi: 10.4103/idoj.IDOJ_262_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Williams D, Yee N, Caplan SE. Who plays, how much, and why? J Comput Mediat Commun . 2008;13:993–1018. [Google Scholar]
- 47.Mayo MJ. Video games: a route to large-scale STEM education? Science. 2009;323:79–82. doi: 10.1126/science.1166900. [DOI] [PubMed] [Google Scholar]
- 48.Goldstein J. Technology and play. In Pellegrini A (Ed.). The Oxford handbook of the development of play. New York: Oxford University Press, 2011: 323-337. [Google Scholar]
- 49.Anderson DR, Subrahmanyam K Cognitive Impacts of Digital Media Workgroup. Digital Screen Media and Cognitive Development. Pediatrics. 2017;140:S57–S61. doi: 10.1542/peds.2016-1758C. [DOI] [PubMed] [Google Scholar]
- 50.Canadian Paediatric Society, Digital Health Task Force, Ottawa , Ontario Screen time and young children: Promoting health and development in a digital world. Paediatr Child Health. 2017;22:461–477. doi: 10.1093/pch/pxx123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tissera KM, Naughton GA, Gabbett TJ, Krause LM, Moresi MP, Benson AC. Sex Differences in Physical Fitness Characteristics and Match-Play Demands in Adolescent Netball: Should Male and Female Adolescents Co-compete in Netball? J Strength Cond Res. 2019;33:846–856. doi: 10.1519/JSC.0000000000002947. [DOI] [PubMed] [Google Scholar]
- 52.Caldera YM, Huston AC, O'Brien M. Social interactions and play patterns of parents and toddlers with feminine, masculine, and neutral toys. Child Dev. 1989;60:70–76. doi: 10.1111/j.1467-8624.1989.tb02696.x. [DOI] [PubMed] [Google Scholar]
- 53.Dinella LM, Weisgram ES, Fulcher M. Children's Gender-Typed Toy Interests: Does Propulsion Matter? Arch Sex Behav. 2017;46:1295–1305. doi: 10.1007/s10508-016-0901-5. [DOI] [PubMed] [Google Scholar]
- 54.Barbu S, Cabanes G, Le Maner-Idrissi G. Boys and girls on the playground: sex differences in social development are not stable across early childhood. PLoS One. 2011;6:e16407. doi: 10.1371/journal.pone.0016407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Coplan RJ, Gavinski-Molina MH, Lagacé-Séguin DG, Wichmann C. When girls versus boys play alone: nonsocial play and adjustment in kindergarten. Dev Psychol. 2001;37:464–474. doi: 10.1037//0012-1649.37.4.464. [DOI] [PubMed] [Google Scholar]
- 56.Fabes RA, Martin CL, Hanish LD. Young children's play qualities in same-, other-, and mixed-sex peer groups. Child Dev. 2003;74:921–932. doi: 10.1111/1467-8624.00576. [DOI] [PubMed] [Google Scholar]
- 57.Lamminmäki A, Hines M, Kuiri-Hänninen T, Kilpeläinen L, Dunkel L, Sankilampi U. Testosterone measured in infancy predicts subsequent sex-typed behavior in boys and in girls. Horm Behav. 2012;61:611–616. doi: 10.1016/j.yhbeh.2012.02.013. [DOI] [PubMed] [Google Scholar]
- 58.Kerney M, Smaers JB, Schoenemann PT, Dunn JC. The coevolution of play and the cortico-cerebellar system in primates. Primates. 2017;58:485–491. doi: 10.1007/s10329-017-0615-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lane SJ, Mailloux Z, Schoen S, Bundy A, May-Benson TA, Parham LD, Smith Roley S, Schaaf RC. Neural Foundations of Ayres Sensory Integration®. Brain Sci. 2019;9 doi: 10.3390/brainsci9070153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shaheen S. How child's play impacts executive function--related behaviors. Appl Neuropsychol Child. 2014;3:182–187. doi: 10.1080/21622965.2013.839612. [DOI] [PubMed] [Google Scholar]
- 61.Wang S, Aamodt S. Play, stress, and the learning brain. Cerebrum. 2012;2012:12. [PMC free article] [PubMed] [Google Scholar]
- 62.Diamond MC, Krech D, Rosenzweig MR. The effects of an enriched environment on the histology of the rat cerebral cortex. J Comp Neurol. 1964;123:111–120. doi: 10.1002/cne.901230110. [DOI] [PubMed] [Google Scholar]
- 63.Gordon NS, Burke S, Akil H, Watson SJ, Panksepp J. Socially-induced brain 'fertilization': play promotes brain derived neurotrophic factor transcription in the amygdala and dorsolateral frontal cortex in juvenile rats. Neurosci Lett. 2003;341:17–20. doi: 10.1016/s0304-3940(03)00158-7. [DOI] [PubMed] [Google Scholar]
- 64.Burgdorf J, Kroes RA, Beinfeld MC, Panksepp J, Moskal JR. Uncovering the molecular basis of positive affect using rough-and-tumble play in rats: a role for insulin-like growth factor I. Neuroscience. 2010;168:769–777. doi: 10.1016/j.neuroscience.2010.03.045. [DOI] [PubMed] [Google Scholar]
- 65.Gordon NS, Kollack-Walker S, Akil H, Panksepp J. Expression of c-fos gene activation during rough and tumble play in juvenile rats. Brain Res Bull. 2002;57:651–659. doi: 10.1016/s0361-9230(01)00762-6. [DOI] [PubMed] [Google Scholar]
- 66.Bell HC, Pellis SM, Kolb B. Juvenile peer play experience and the development of the orbitofrontal and medial prefrontal cortices. Behav Brain Res. 2010;207:7–13. doi: 10.1016/j.bbr.2009.09.029. [DOI] [PubMed] [Google Scholar]
- 67.Pellis SM, Pellis VC, Himmler BT. How play makes for a more adaptable brain: a comparative and neural perspective. Am J Play . 2014;7:73–98. [Google Scholar]
- 68.Einon DF, Morgan MJ, Kibbler CC. Brief periods of socialization and later behavior in the rat. Dev Psychobiol. 1978;11:213–225. doi: 10.1002/dev.420110305. [DOI] [PubMed] [Google Scholar]
- 69.Vanderschuren LJ, Niesink RJ, Van Ree JM. The neurobiology of social play behavior in rats. Neurosci Biobehav Rev. 1997;21:309–326. doi: 10.1016/s0149-7634(96)00020-6. [DOI] [PubMed] [Google Scholar]
- 70.Johnson JL. The History of Play Therapy. In: O'Connor KJ, Schaefer CE, Braverman LD (eds). Handbook of Play Therapy. John Wiley & Sons, Inc., 2015: 17-34. [Google Scholar]
- 71.Dougherty J, Ray D. Differential impact of play therapy on developmental levels of children. Int J Play Ther . 2007;16:2–19. [Google Scholar]
- 72.Koukourikos K, Tsaloglidou A, Tzeha L, Iliadis C, Frantzana A, Katsimbeli A, Kourkouta L. An Overview of Play Therapy. Mater Sociomed. 2021;33:293–297. doi: 10.5455/msm.2021.33.293-297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Reddy RP, Hirisave U. Child's Play: Therapist's Narrative. Indian J Psychol Med. 2014;36:204–207. doi: 10.4103/0253-7176.130998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Moss L, Hamlet HS. An Introduction To Child-Centered Play Therapy. Ther Person-Centered J . 2020;25:91–103. [Google Scholar]
- 75.Pidgeon K, Parson J, Mora L, Anderson J, Stagnitti K, Mountain V. Play Therapy. In: Noble C, Day E (Editors). Psychotherapy and Counselling: Reflections on Practice. Oxford University Press. 2015: 1-30. [Google Scholar]
- 76.Senko K, Bethany H. PLAY THERAPY: An Illustrative Case. Innov Clin Neurosci. 2019;16:38–40. [PMC free article] [PubMed] [Google Scholar]
- 77.Frick-Helms SB, Drewes AA. Introduction to play therapy research theme issue. Int J Play Ther . :2010, 19: 1–3. [Google Scholar]
- 78.Jayne KM, Purswell KE, Stulmaker HL. Facilitating congruence, empathy, and unconditional positive regard through therapeutic limit-setting: Attitudinal conditions limit-setting model (ACLM) Int J Play Ther . 28:238–249. [Google Scholar]
- 79.Stewart AL, Field TA, Echterling LG. Neuroscience and the Magic of Play Therapy. Int J Play Ther . :2016, 25: 4–13. [Google Scholar]
- 80.Lambert MJ, Barley DE. Research summary on the therapeutic relationship and psychotherapy outcome. Psychotherapy . 2001;38:357–361. [Google Scholar]
- 81.Shirk SR, Karver MS, Brown R. The alliance in child and adolescent psychotherapy. Psychotherapy. 2011;48:17–24. doi: 10.1037/a0022181. [DOI] [PubMed] [Google Scholar]
- 82.Ogundele MO. Behavioural and emotional disorders in childhood: A brief overview for paediatricians. World J Clin Pediatr. 2018;7:9–26. doi: 10.5409/wjcp.v7.i1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sampaio F, Bonnert M, Olén O, Hedman E, Lalouni M, Lenhard F, Ljótsson B, Ssegonja R, Serlachius E, Feldman I. Cost-effectiveness of internet-delivered cognitive-behavioural therapy for adolescents with irritable bowel syndrome. BMJ Open. 2019;9:e023881. doi: 10.1136/bmjopen-2018-023881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Pontes JE, Tabet E, Folkmann MÁ, Cunha ML, Almeida Fde A. Therapeutic play: preparing the child for the vaccine. Einstein (Sao Paulo) 2015;13:238–242. doi: 10.1590/S1679-45082015AO2967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Koukourikos K, Tzeha L, Pantelidou P, Tsaloglidou A. The importance of play during hospitalization of children. Mater Sociomed. 2015;27:438–441. doi: 10.5455/msm.2015.27.438-441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Rusmana N, Hafina A, Suryana D. Group Play Therapy for Preadolescents: Post-Traumatic Stress Disorder of Natural Disaster Victims in Indonesia. Open Psychol J . 2020:13: 213–222. [Google Scholar]
- 87.Rathnakumar D. Play Therapy and Children with Intellectual Disability. Shanlax Int J Educ . 2020;8:35–42. [Google Scholar]
- 88.Paul O. [Parental Resolution of the Child's Disability Diagnosis in the Reaction to Diagnosis Interview (RDI) and Effects on the Play Interaction with the Child] Prax Kinderpsychol Kinderpsychiatr. 2020;69:625–642. doi: 10.13109/prkk.2020.69.7.625. [DOI] [PubMed] [Google Scholar]
- 89.Kennedy-Behr A, Rodger S, Mickan S. Aggressive interactions during free-play at preschool of children with and without developmental coordination disorder. Res Dev Disabil. 2013;34:2831–2837. doi: 10.1016/j.ridd.2013.05.033. [DOI] [PubMed] [Google Scholar]
- 90.Abdollahian E, Mokhber N, Balaghi A, Moharrari F. The effectiveness of cognitive-behavioural play therapy on the symptoms of attention-deficit/hyperactivity disorder in children aged 7-9 years. Atten Defic Hyperact Disord. 2013;5:41–46. doi: 10.1007/s12402-012-0096-0. [DOI] [PubMed] [Google Scholar]
- 91.Al-Beltagi M. Autism medical comorbidities. World J Clin Pediatr. 2021;10:15–28. doi: 10.5409/wjcp.v10.i3.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Lainhart JE, Piven J. Diagnosis, treatment, and neurobiology of autism in children. Curr Opin Pediatr. 1995;7:392–400. doi: 10.1097/00008480-199508000-00009. [DOI] [PubMed] [Google Scholar]
- 93.Golarai G, Grill-Spector K, Reiss AL. Autism and the development of face processing. Clin Neurosci Res. 2006;6:145–160. doi: 10.1016/j.cnr.2006.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Mazzoni N, Ricciardelli P, Actis-Grosso R, Venuti P. Difficulties in Recognising Dynamic but not Static Emotional Body Movements in Autism Spectrum Disorder. J Autism Dev Disord. 2022;52:1092–1105. doi: 10.1007/s10803-021-05015-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Candini M, Battaglia S, Benassi M, di Pellegrino G, Frassinetti F. The physiological correlates of interpersonal space. Sci Rep. 2021;11:2611. doi: 10.1038/s41598-021-82223-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ellena G, Battaglia S, Làdavas E. The spatial effect of fearful faces in the autonomic response. Exp Brain Res. 2020;238:2009–2018. doi: 10.1007/s00221-020-05829-4. [DOI] [PubMed] [Google Scholar]
- 97.Borgomaneri S, Vitale F, Battaglia S, Avenanti A. Early Right Motor Cortex Response to Happy and Fearful Facial Expressions: A TMS Motor-Evoked Potential Study. Brain Sci. 2021;11:1203. doi: 10.3390/brainsci11091203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Woodard CR, Chung J. Feasibility of a play-based intervention set for toddlers with autism. Res Dev Disabil. 2018;80:24–34. doi: 10.1016/j.ridd.2018.05.010. [DOI] [PubMed] [Google Scholar]
- 99.McCleery JP, Elliott NA, Sampanis DS, Stefanidou CA. Motor development and motor resonance difficulties in autism: relevance to early intervention for language and communication skills. Front Integr Neurosci. 2013;7:30. doi: 10.3389/fnint.2013.00030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Lord C, Elsabbagh M, Baird G, Veenstra-Vanderweele J. Autism spectrum disorder. Lancet. 2018;392:508–520. doi: 10.1016/S0140-6736(18)31129-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Kasari C, Freeman S, Paparella T. Joint attention and symbolic play in young children with autism: a randomized controlled intervention study. J Child Psychol Psychiatry. 2006;47:611–620. doi: 10.1111/j.1469-7610.2005.01567.x. [DOI] [PubMed] [Google Scholar]
- 102.Correction and Republication: Prevalence and Characteristics of Autism Spectrum Disorder Among Children Aged 8 Years - Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2012. MMWR Morb Mortal Wkly Rep. 2018;67:1279. doi: 10.15585/mmwr.mm6745a7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Abrams DA, Lynch CJ, Cheng KM, Phillips J, Supekar K, Ryali S, Uddin LQ, Menon V. Underconnectivity between voice-selective cortex and reward circuitry in children with autism. Proc Natl Acad Sci USA. 2013;110:12060–12065. doi: 10.1073/pnas.1302982110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Tomchek S, Koenig KP, Arbesman M, Lieberman D. Occupational Therapy Interventions for Adolescents With Autism Spectrum Disorder. Am J Occup Ther. 2017;71:7101395010p1–7101395010p3. doi: 10.5014/ajot.2017.711003. [DOI] [PubMed] [Google Scholar]
- 105.Kuhaneck H, Spitzer SL, Bodison SC. A Systematic Review of Interventions to Improve the Occupation of Play in Children With Autism. OTJR (Thorofare N J) 2020;40:83–98. doi: 10.1177/1539449219880531. [DOI] [PubMed] [Google Scholar]
- 106.Yahaya A, Mahir IB, Lee GM, Maakip I, Arus BM, Voo P, Kwan SS. Shelter house play therapy for a child with autism. IJASOS . 2018;4:299–307. [Google Scholar]
- 107.Hyman SL, Levy SE, Myers SM Council on Children with Disabilities, Section on Developmental and Behavioral Pediatrics. Identification, Evaluation, and Management of Children With Autism Spectrum Disorder. Pediatrics. 2020;145:e20193447. doi: 10.1542/peds.2019-3447. [DOI] [PubMed] [Google Scholar]
- 108.Donnellan AM, Hill DA, Leary MR. Rethinking autism: implications of sensory and movement differences for understanding and support. Front Integr Neurosci. 2012;6:124. doi: 10.3389/fnint.2012.00124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kashefimehr B, Kayihan H, Huri M. The Effect of Sensory Integration Therapy on Occupational Performance in Children With Autism. OTJR (Thorofare N J) 2018;38:75–83. doi: 10.1177/1539449217743456. [DOI] [PubMed] [Google Scholar]
- 110.Schottelkorb AA, Swan KL, Ogawa Y. Intensive Child-Centered Play Therapy for Children on the Autism Spectrum: A Pilot Study. J Counsell Dev . 2020;98:63–73. [Google Scholar]
- 111.Novita M, Atmodiwirjo ET, Basaria D. The Effectiveness of Child-Centered Play Therapy to Improve Joint Attention Skills in Children with Autism Spectrum Disorder. The Asian Conference on Education 2017. [Accessed Jul 22, 2022] [Google Scholar]
- 112.Carrizales KE. Transcendence Through Play: Child-Centered Play Therapy and Young Children with Autism. Published Doctor of Philosophy dissertation, University of Northern Colorado, 2015. [Google Scholar]
- 113.Goodman G, Chung H, Fischel L, Athey-Lloyd L. Simulation modeling analysis of sequential relations among therapeutic alliance, symptoms, and adherence to child-centered play therapy between a child with autism spectrum disorder and two therapists. Clin Child Psychol Psychiatry. 2017;22:455–466. doi: 10.1177/1359104517691082. [DOI] [PubMed] [Google Scholar]
- 114.Kenny MC, Dinehart LH, Winick CB. Child-centered play therapy for children with autism spectrum disorder. In: Drewes AA, Schaefer CE (Eds.). Play therapy in middle childhood. American Psychological Association. 2016: 257-274. [Google Scholar]
- 115.Baum RA. Learning to Play and Playing to Learn: Enhancing Interactions in Young Children With ASD. Pediatrics. 2019;144 doi: 10.1542/peds.2019-1270. [DOI] [PubMed] [Google Scholar]
- 116.Gengoux GW, Abrams DA, Schuck R, Millan ME, Libove R, Ardel CM, Phillips JM, Fox M, Frazier TW, Hardan AY. A Pivotal Response Treatment Package for Children With Autism Spectrum Disorder: An RCT. Pediatrics. 2019;144 doi: 10.1542/peds.2019-0178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.de Korte MWP, van Dongen-Boomsma M, Oosterling IJ, Buitelaar JK, Staal WG. Pivotal Response Treatment (PRT) parent group training for young children with autism spectrum disorder: a pilot study. Sci Rep. 2022;12:7691. doi: 10.1038/s41598-022-10604-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Wieder S, Greenspan SI. Climbing the symbolic ladder in the DIR model through floor time/interactive play. Autism. 2003;7:425–435. doi: 10.1177/1362361303007004008. [DOI] [PubMed] [Google Scholar]
- 119.Lal R, Chhabria R. Early Intervention of Autism: A Case for Floor Time Approach. In: Fitzgerald M. Recent Advances in Autism Spectrum Disorders. 2013. [Google Scholar]
- 120.Dionne M, Martini R. Floor time play with a child with autism: a single-subject study. Can J Occup Ther. 2011;78:196–203. doi: 10.2182/cjot.2011.78.3.8. [DOI] [PubMed] [Google Scholar]
- 121.Solomon R, Necheles J, Ferch C, Bruckman D. Pilot study of a parent training program for young children with autism: the PLAY Project Home Consultation program. Autism. 2007;11:205–224. doi: 10.1177/1362361307076842. [DOI] [PubMed] [Google Scholar]
- 122.Pajareya K, Nopmaneejumruslers K. A one-year prospective follow-up study of a DIR/Floortime parent training intervention for pre-school children with autistic spectrum disorders. J Med Assoc Thai. 2012;95:1184–1193. [PubMed] [Google Scholar]
- 123.Liao ST, Hwang YS, Chen YJ, Lee P, Chen SJ, Lin LY. Home-based DIR/Floortime intervention program for preschool children with autism spectrum disorders: preliminary findings. Phys Occup Ther Pediatr. 2014;34:356–367. doi: 10.3109/01942638.2014.918074. [DOI] [PubMed] [Google Scholar]
- 124.Praphatthanakunwong N, Kiatrungrit K, Hongsanguansri S, Nopmaneejumruslers K. Factors associated with parent engagement in DIR/Floortime for treatment of children with autism spectrum disorder. Gen Psychiatr. 2018;31:e000009. doi: 10.1136/gpsych-2018-000009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Boscarelli A. Clown therapy: not only a pediatric matter. Transl Pediatr. 2017;6:111–112. doi: 10.21037/tp.2017.03.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Gordon J, Shenar Y, Pendzik S. Clown therapy: A drama therapy approach to addiction and beyond. Arts Psychother . 2018;57:88–94. [Google Scholar]
- 127.Shefer S, Leon Attia O, Rosenan R, Wald OA, Ende H, Gabis LV. Benefits of medical clowning in the treatment of young children with autism spectrum disorder. Eur J Pediatr. 2019;178:1283–1289. doi: 10.1007/s00431-019-03415-7. [DOI] [PubMed] [Google Scholar]
- 128.Gardziel A, Ozaist P, Sitnik E. Method 3i in ASD therapy. Psychoterapia . 2015;172:37–45. [Google Scholar]
- 129.Tilmont Pittala E, Saint-Georges-Chaumet Y, Favrot C, Tanet A, Cohen D, Saint-Georges C. Clinical outcomes of interactive, intensive and individual (3i) play therapy for children with ASD: a two-year follow-up study. BMC Pediatr. 2018;18:165. doi: 10.1186/s12887-018-1126-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Brefort E, Saint-Georges-Chaumet Y, Cohen D, Saint-Georges C. Two-year follow-up of 90 children with autism spectrum disorder receiving intensive developmental play therapy (3i method) BMC Pediatr. 2022;22:373. doi: 10.1186/s12887-022-03431-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Green E. Integrated Play Groups (IPG) Model. In: Volkmar FR (eds). Encyclopedia of Autism Spectrum Disorders. Springer, New York, NY. 2013. [Google Scholar]
- 132.Yang TR, Wolfberg PJ, Wu SC, Hwu PY. Supporting children on the autism spectrum in peer play at home and school: piloting the integrated play groups model in Taiwan. Autism. 2003;7:437–453. doi: 10.1177/1362361303007004009. [DOI] [PubMed] [Google Scholar]
- 133.Wolfberg P, DeWitt M, Young GS, Nguyen T. Integrated play groups: promoting symbolic play and social engagement with typical peers in children with ASD across settings. J Autism Dev Disord. 2015;45:830–845. doi: 10.1007/s10803-014-2245-0. [DOI] [PubMed] [Google Scholar]
- 134.Waddington H, Reynolds JE, Macaskill E, Curtis S, Taylor LJ, Whitehouse AJ. The effects of JASPER intervention for children with autism spectrum disorder: A systematic review. Autism. 2021;25:2370–2385. doi: 10.1177/13623613211019162. [DOI] [PubMed] [Google Scholar]
- 135.Goods KS, Ishijima E, Chang YC, Kasari C. Preschool based JASPER intervention in minimally verbal children with autism: pilot RCT. J Autism Dev Disord. 2013;43:1050–1056. doi: 10.1007/s10803-012-1644-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Shire SY, Shih W, Bracaglia S, Kodjoe M, Kasari C. Peer engagement in toddlers with autism: Community implementation of dyadic and individual Joint Attention, Symbolic Play, Engagement, and Regulation intervention. Autism. 2020;24:2142–2152. doi: 10.1177/1362361320935689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Shire SY, Arbuckle S, Bao W. Development and Usability Testing of a Web-Based Adaptation of the Joint Attention, Symbolic Play, Engagement, and Regulation Social Communication Intervention. Perspectives . 2022;7:310–323. [Google Scholar]
- 138.Panganiban J, Kasari C. Super responders: Predicting language gains from JASPER among limited language children with autism spectrum disorder. Autism Res. 2022;15:1565–1575. doi: 10.1002/aur.2727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Schaad J, Dion L. Synergetic Play Therapy Combined With EMDR Therapy, In: Beckley-Forest A, Monaco A. EMDR with Children in the Play Therapy Room. Springer Publishing Company, New York. 2020: 109-144. [Google Scholar]
- 140.Dion L, Gray K. Impact of therapist authentic expression on emotional tolerance in synergetic play therapy. Int J Play Ther . 2014;23:55–67. [Google Scholar]
- 141.Simmons J. Moving Toward Regulation Using Synergetic Play Therapy. Canadian J Counsell Psychother . 2020;54:242–258. [Google Scholar]
- 142.Sheade H. Equine-Partnered Play Therapy™ for Children with Oppositional Behavior. In: Equine-Assisted Mental Health Interventions, First edition, Routledge, 2018: 1-8. [Google Scholar]
- 143.Chandler CK. Animal-Assisted Therapy in Counseling, 3rd Edition, Routledge Company, 2017. [Google Scholar]
- 144.Roberts F, Bradberry J, Williams C. Equine-facilitated psychotherapy benefits students and children. Holist Nurs Pract. 2004;18:32–35. doi: 10.1097/00004650-200401000-00006. [DOI] [PubMed] [Google Scholar]
- 145.Bass MM, Duchowny CA, Llabre MM. The effect of therapeutic horseback riding on social functioning in children with autism. J Autism Dev Disord. 2009;39:1261–1267. doi: 10.1007/s10803-009-0734-3. [DOI] [PubMed] [Google Scholar]
- 146.Harris A, Williams JM. The Impact of a Horse Riding Intervention on the Social Functioning of Children with Autism Spectrum Disorder. Int J Environ Res Public Health. 2017;14 doi: 10.3390/ijerph14070776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Steiner H, Kertesz Z. Effects of therapeutic horse riding on gait cycle parameters and some aspects of behavior of children with autism. Acta Physiol Hung. 2015;102:324–335. doi: 10.1556/036.102.2015.3.10. [DOI] [PubMed] [Google Scholar]
- 148.McDaniel Peters BC, Wood W. Autism and Equine-Assisted Interventions: A Systematic Mapping Review. J Autism Dev Disord. 2017;47:3220–3242. doi: 10.1007/s10803-017-3219-9. [DOI] [PubMed] [Google Scholar]
- 149.Bosgraaf L, Spreen M, Pattiselanno K, van Hooren S. Art Therapy for Psychosocial Problems in Children and Adolescents: A Systematic Narrative Review on Art Therapeutic Means and Forms of Expression, Therapist Behavior, and Supposed Mechanisms of Change. Front Psychol. 2020;11:584685. doi: 10.3389/fpsyg.2020.584685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Hermann C. Bonsai as a group art therapy intervention among traumatized youth in KwaZulu-Natal. Psych J. 2021;10:177–186. doi: 10.1002/pchj.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.West C. Art therapy. Nurs Older People. 2008;20:18–19. [PubMed] [Google Scholar]
- 152.Wypyszyńska J, Zaboklicka N, Stachura M, Sito Z, Męcik-Kronenberg T. Opinions of parents of children with autism spectrum disorders on art therapy in the improvement of their functioning. Wiad Lek. 2021;74:2452–2459. [PubMed] [Google Scholar]
- 153.Schweizer C, Knorth E J, Spreen M. Art therapy with children with Autism Spectrum Disorders: A review of clinical case descriptions on 'what works'. Arts Psychother . 2014;41:577–593. [Google Scholar]
- 154.Moghaddam K, Zadeh Mohammadi A, Sharifi Daramadi P, Afrooz G. Effect of the Family-based Art Therapy Program on the Social Interactions, Verbal Skills and Stereotypic Behaviors of Children with Autism Spectrum Disorders (ASD) Iran J Public Health. 2016;45:830–832. [PMC free article] [PubMed] [Google Scholar]
- 155.Al-Beltagi M, Saeed NK, Bediwy AS, Alhawamdeh R, Qaraghuli S. The Effects of COVID-19 on children with Autism. World J Virol. 2022:In press. doi: 10.5501/wjv.v11.i6.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Schueller SM, Stiles-Shields C, Yarosh L. Online Treatment and Virtual Therapists in Child and Adolescent Psychiatry. Child Adolesc Psychiatr Clin N Am. 2017;26:1–12. doi: 10.1016/j.chc.2016.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Renshaw KL, Parson JA. Tele-Play Therapy. In: Play Therapy and Expressive Arts in a Complex and Dynamic World. First Edition. Routledge, 2020: 27. [Google Scholar]
- 158.Tuber S, Da Costa R, Eidman J, Feldman H, Hadar O, Kaur N, Zanotti P, Schulder T, Tocatly K. Dialectical Reflections on the Advantages and Disadvantages of Tele-Play Therapy. J Infant, Child, Adol Psychother . 2022;21:19–26. [Google Scholar]