Abstract
Background
The viability and virulence of COVID-19 are complex in nature. Although the relationship between environmental parameters and COVID-19 is well studied across the globe, in India, such studies are limited. This research aims to explore long-term exposure to weather conditions and the role of air pollution on the infection spread and mortality due to COVID-19 in India.
Method
District-level COVID-19 data from April 26, 2020 to July 10, 2021 was used for the study. Environmental determinants such as land surface temperature, relative humidity (RH), Sulphur dioxide (SO2), Nitrogen dioxide (NO2), Ozone (O3), and Aerosol Optical Depth (AOD) were considered for analysis. The bivariate spatial association was used to explore the spatial relationship between Case Fatality Rate (CFR) and these environmental factors. Further, the Bayesian multivariate linear regression model was applied to observe the association between environmental factors and the CFR of COVID-19.
Results
Spatial shifting of COVID-19 cases from Western to Southern and then Eastern parts of India were well observed. The infection rate was highly concentrated in most of the Western and Southern regions of India, while the CFR shows more concentration in Northern India along with Maharashtra. Four main spatial clusters of infection were recognized during the study period. The time-series analysis indicates significantly more CFR with higher AOD, O3, and NO2 in India.
Conclusions
COVID-19 is highly associated with environmental parameters and air pollution in India. The study provides evidence to warrant consideration of environmental parameters in health models to mediate potential solutions. Cleaner air is a must to mitigate COVID-19.
Keywords: COVID-19, Pandemic, Environmental parameters, Time series, Spatial association
1. Introduction
Air pollution is a pressing challenge for India. In 2015, it was estimated that nearly 1 million people died in India as a result of air pollution (Guo et al., 2017). World Health Organization (WHO) has recognized that 99% of the world population is living in places where the WHO air quality specified levels are not met (WHO, 2022). It is evident that air pollution is a key contributor to the world's 12.4 million deaths (Balakrishnan et al., 2019, Vulichi et al., 2021) as pollution affects various organs in the human body, especially the respiratory system (Manisalidis et al., 2020b, Patankar and Trivedi, 2011, Rajak et al., 2022). Ambient air pollution was responsible for 17% of ischaemic heart disease, 14% of cerebrovascular disease, 16% of lung cancer, 25% of lower respiratory infections, and 27% of chronic obstructive pulmonary disease deaths in 2015 (Cohen et al., 2017). At the same time, indoor air pollution was responsible for 4 million deaths annually (WHO, 2022). India accounted for 1.24 million deaths attributable to air pollution in 2017, which increased to 1.67 million deaths in 2019 (Pandey et al., 2021).
The COVID-19 infection has affected billions of people globally, killing more than 6 million individuals (WHO, 2022). Caused by the SARS-CoV-2 virus belonging to the Coronaviridae family, the COVID-19 disease has increasingly been deemed as an occupational disease (Abdelzaher et al., 2020). Manifestations of symptoms in the varying background of genetic landscapes of populations are still not well understood. Genetic predispositions may alter not only the susceptibility to infection but also the immune response mounted by our body to the virus as well as the severity of the symptoms. Polymorphisms in the ACE2 cellular receptor (to which SARS-CoV-2 binds) or cellular proteases facilitating viral entry into cells have been evidenced to affect the aforementioned parameters of the infection (Hoffmann et al., 2020, Hussain et al., 2020, Walls et al., 2020). Genetic sequencing of highly-sensitive and highly-resistant (asymptomatic) individuals, albeit challenging, could help in deciphering mechanisms explaining the diverse spectrum of COVID-19 infections across populations. Amidst the changing dynamics of the pandemic spread, specific routes of transmission have received much attention in causing rapid outbreaks and waves. These rely heavily on environmental factors and may cause temporal and spatial heterogeneity observed in the pandemic. Polluted air, for example, can amplify existing respiratory or other comorbidities and regulate aerosol-mediated transport of the virus (Weaver et al., 2022). Though there is a lack of robust evidence for other environmental factors such as chemicals or climatic conditions, there are plausible mechanisms by which these can affect the immune responses to the infection or aggravate other comorbidities (Weaver et al., 2022).
Several pathological and environmental conditions are linked with the etiology of COVID-19 (Manisalidis et al., 2020a). People who have been exposed to long-term air pollution are more vulnerable to the disease because their respiratory system is more susceptible to the effects of air pollution serving as a convenient entry point for a variety of dispersed pollutants (Gerretsen, 2020). Thus, air pollution acts as a vehicle for viral transmission and aids in compromising a person's physiological defensive mechanisms to ambient pollutants; hence, long-term air pollution exposure leads to the collapse of respiratory system inflammation, coughing, bronchitis, asthma attacks, and other health issues (Conticini et al., 2020a, World Health Organization, 2000). Some recently published researches have established the connection between air pollution and the risk of COVID-19 in India (Chattopadhyay and Shaw, 2021a; Chauhan and Singh, 2020; Otmani et al., 2020).
COVID-19 lockdowns resulted in 43% reduction in PM2.5 levels compared to the pre-lockdown time (Sharma et al., 2020). A handful of studies have shown a reduction in PM2.5 concentrations and an improvement of air quality across different cities in India (Kumar et al., 2020, Mahato et al., 2020, Ranjan et al., 2020, Srivastava et al., 2020). However, exposure to air pollution on COVID-19 has been observed in many cities in China, the USA, the UK, India, Bangladesh, and in many other countries (Albayati et al., 2021; Ming et al., 2020; Pal et al., 2021; Rahman et al., 2020; Ropkins and Tate, 2021; Zangari et al., 2020; Bashir et al., 2020; Fattorini and Regoli, 2020; Frontera et al., 2020b). Studies revealed that cities with the worst air pollution suffered the heaviest from the pandemic (Mendy et al., 2021; Naqvi et al., 2021; Shehzad et al., 2020; Berman and Ebisu, 2020; Karuppasamy et al., 2020; Peng et al., 2020;Gupta et al., 2021). Country-specific studies in the USA (Adams, 2020; Bashir et al., 2020; Chen et al., 2020), Italy (Bontempi, 2020a; Conticini et al., 2020b; Fattorini and Regoli, 2020), China (Cui et al., 2020; Liu et al., 2020; Zhu et al., 2020), and India (Chattopadhyay and Shaw, 2021b; Dutta and Dutta, 2021), have shown a significant association between pollutant exposure and susceptibility to COVID-19 infection or fatality. In the ongoing saga of COVID-19, many studies have reported the fast spreading of the virus with higher levels of air pollution (Bontempi, 2020b; Setti et al., 2020; Fattorini and Regoli, 2020; Wu et al., 2020; Zhu et al., 2020; Gupta et al., 2021).
The viability and virulence of COVID-19 are very uncertain and complex in nature. Preliminary studies have shown that the primary mode of infection is via droplets or aerosols and contaminated environmental surfaces transmitted from an infected person (Chaudhuri et al., 2020; Song et al., 2021). Some studies have suggested that atmospheric conditions and the local environment play a major role in transmitting the virus (Ahmadi et al., 2020; Basray et al., 2021; Liu et al., 2020). Most respiratory viral infections show seasonal fluctuations, with peaks in specific winter months due to various meteorological controls like temperature, humidity, dew point and others (Price et al., 2019). Transmission of COVID-19 is high at low temperatures and humidity (Bashir et al., 2020; Sajadi et al., 2020). Recent studies indicate that low relative humidity (RH) affects the viability of the virus as it stabilizes the droplet and enhances the propagation in the nasal mucosa (Sajadi et al., 2020; Wang et al., 2021). Nonetheless, low humidity levels in the atmosphere prompt the virus to remain airborne for a longer period, and cold and dry weather weakens the host's immunity, creating an easy route of entry for the pathogen (Kudo et al., 2019; Lowen and Steel, 2014). Another important viricidal agent for viral exposure is ultraviolet (UV) radiation. Diffey (1991) suggested that UV radiation has the potential to deactivate viruses, implying that the virus loses the ability to proliferate. More shreds of evidence suggest a negative correlation between UV radiations and COVID-19 (Ahmadi et al., 2020; Heβling et al., 2020; Sagripanti and Lytle, 2020; Tang et al., 2021).
However, the relation of environmental factors with the novel infection is country specific and has spatial variations. Currently, we lack evidence on the role of environment in COVID-19 spread, considering the huge spatial heterogeneity of India. This paper, first of its kind, aims to quantify the influence of selected environmental factors on COVID-19 infection and mortality at national level. No study has yet been published on spatial analysis of India considering 640 districts to reveal the association of environmental factors on this infection. Specifically, our research is the first of its kind in India to understand the spread of infection based on the spatio-temporal distribution of cumulative infected cases and its linkage with pollution levels. Thus, this study has considerable potential for informing policymakers to consider environmental cleanliness to avert such a pandemic in the near future.
2. Data and methods
2.1. COVID-19 data
The analysis in this paper was based on data accumulated up to July 10, 2021, when India was getting a certain peak of the second wave of COVID-19. Data was obtained from the crowd sourced database http://covid19india.org/ (Dibyachintan et al., 2020). A total of 640 districts of India were chosen for the spatial analysis. Recently created (after 2011) districts were merged with their parent district following Census 2011 (Census, 2011). For the time series analysis, the district level cumulative cases and mortality data of COVID-19 were collated for a span of 62 weeks (From April 26, 2020 to July 10, 2021). WorldPop data was used to measure the 2020-21 district wise total population of India. The data set provides the raster data with 1 km spatial resolution of the world's population, adjusted and matched with the corresponding official data of the United Nations Population Division (UNPD) of the Department of Economic and Social Affairs (WorldPop, 2021). However, the district-wise population was calculated by applying the zonal statistics using the GIS technique. The CFR was calculated by dividing the total number of deaths in the district at any given time by the total number of confirmed cases in the district at that time (WHO, 2020b).
2.2. Environmental data
Various satellite images were used to understand the association between environmental factors and CFR of COVID-19. Daily temperature and precipitation were considered for the analysis. The climatic data was obtained from ERA5-L. The ERA5-Land data is produced by re-applying the land component of the ERA5 climate re-analysis and covers the time period, January 1950 to near real-time (NRT) with a spatial resolution of ∼10 km. The single simulation technique without coupling to the atmospheric module of the ECMWF's IFS were used to produce the data. The core of ERA5-L is the Tiled ECMWF Scheme for surface exchanges over land incorporating land surface hydrology (H-TESSEL). Further information can be obtained from the Climate Data Store (CDS) Climate Copernicus website (https://cds.climate.copernicus.eu/cdsapp#!/dataset/reanalysis-era5-%20land?tab%20=%20overview).
SO2, NO2, O3 and AOD were considered as the determinants of air pollution and, obtained from Sentinel-5 Precursor (Sentinel-5 P). In 2017, the Sentinel-5 P was launched by Copernicus mission to monitor Erath's atmosphere (Veefkind et al., 2020). The sentinel-5 P is being operated by the European Commission under the Copernicus program, which follows the sun-synchronous orbital cycle of 16 days. The TROPOspheric Monitoring Instrument (TROPOMI) is installed in the satellite, which provides global coverage of air pollutants with ∼5.5 km of spatial resolution (Veefkind et al., 2020). For the present study, the near-real-time (NRTI) datasets, were collected from April 26, 2020 to July 10, 2021. Further, as a proxy of particulate matters, the level-3 (L3) daily AOD data at 550 nm (MOD08_D3) from Moderate Resolution Imaging Spectroradiometer (MODIS) onboard Terra was used in the study. MODIS satellite images provide worldwide coverage of AOD, which is derived from the dark target (DT) and deep blue (DB) algorithms. The DT algorithm covers the ocean and dark surface, whereas the DB algorithm is applied to the land areas of the dark and bright surfaces (Levy et al., 2013). All the district-level data of environmental parameters were extracted using the zonal statistics for the study period.
2.3. Statistical analysis
The bivariate spatial association was used to explore the spatial relationship between CFR and environmental factors. The spatial data was analyzed using the Earth Engine Code Editor, R and ArcMap software. We applied the Bayesian approach that includes explaining the data by meaningful mathematical models, and allocating credibility to parameter values that are consistent with the data and with prior knowledge. When the data grows rapidly with rare events and increased expectation of the number of observed rare events, then the best results are obtained. The final estimates were improved by this method of analysis to reduce the uncertainty related to the situation and efficiently manage rare events (Fudenberg et al., 2017).
The Bayesian model used in our analysis is a multivariate linear regression model that uses a relevant prior distribution. In a regression model, a p-dimensional normal prior distribution is denoted by Np with prior mean vector μ0 and prior covariance matrix ∑0. Now, for j = 1(1)p, the regression coefficients βj has a normal distribution with mean μj and variance σ2 j. According to Bayes' rule, the posterior distribution (Bayes and Hume, 1763) considered in this model is given below-
A linear probability model with normal priors was created as it is more appropriate in this context as all the variables are continuous. A large class of algorithms for generating a representative random sample from a distribution is called Markov Chain Monte Carlo (MCMC) methods. Regardless of which particular sampler from the class is used, in the long run they all converge to an accurate representation of the posterior distribution. The bigger the MCMC sample, the finer-resolution picture we have of the posterior distribution (Andrieu et al., 2003).
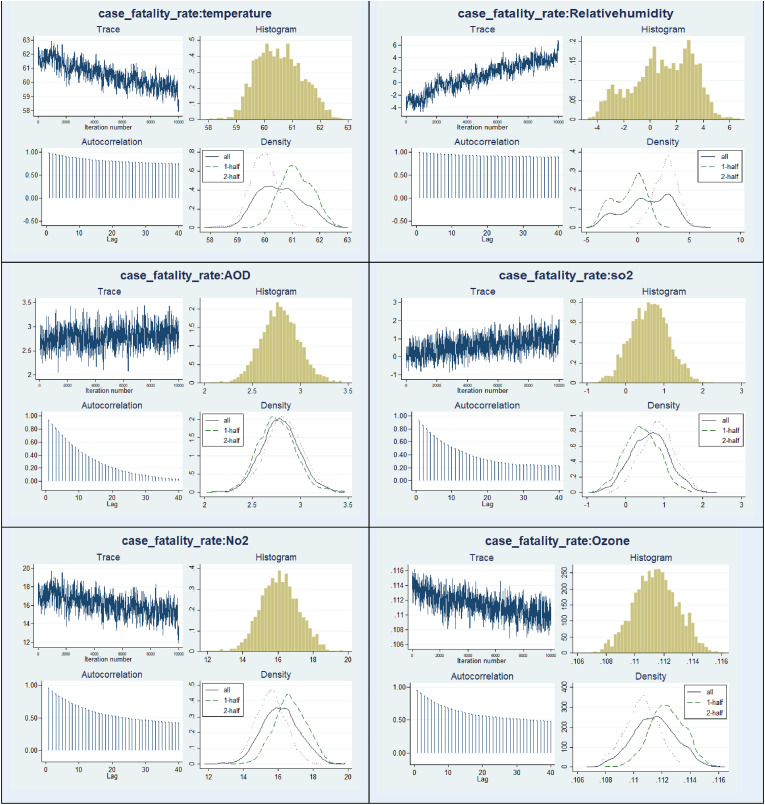
Convergence Diagnostics: There are four diagnostic plots for the convergence which include-times series plots, trace plots, density plots and auto-correlation plots (Fig. 1). The times series plots indicate good convergence over time. The trace plots have the parameter values plotted at each iteration. There are no visible drifts in the plots, indicating convergence. The kernel density plots do not depict multi-modality and are roughly Gaussian, although not exact. The density plots of all the variables satisfy convergence criteria except for RH. The autocorrelation plots also evidently show convergence with increasing lag values.
Fig. 1.
Markov Chain Monte Carlo (MCMC) convergence diagnostic plots of CFR and other covariates.
3. Results
3.1. Spatio-temporal distribution of the pollutants
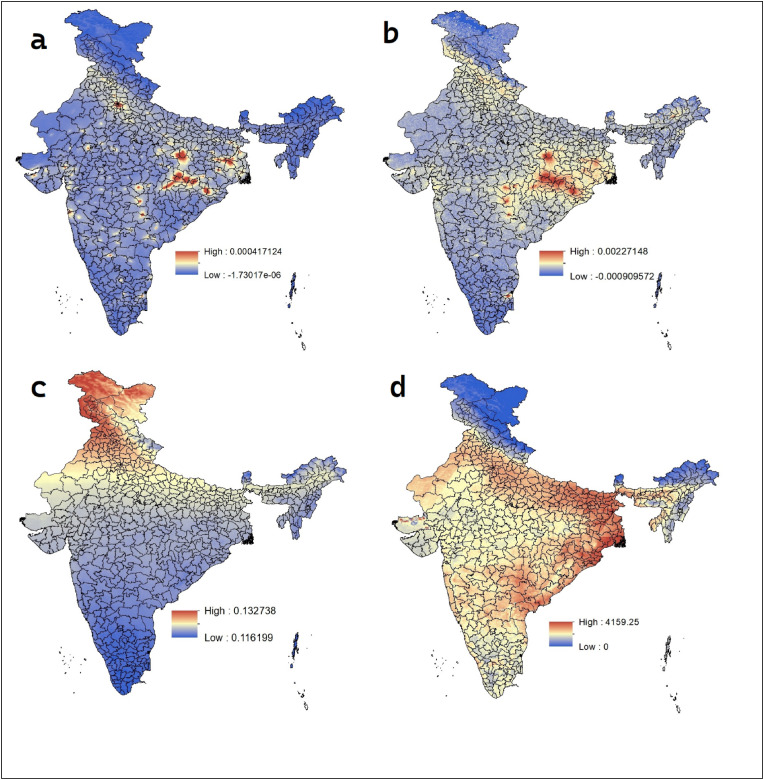
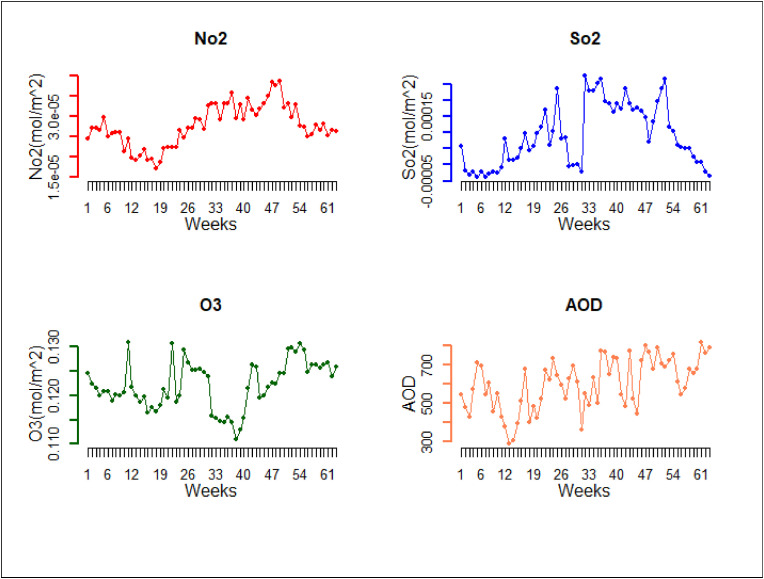
The spatial distribution of different air pollutants during the study period is presented in Fig. 2 . Both SO2 and NO2 are highly concentrated over the Eastern region of India. A higher concentration of NO2 can be observed in the capital of India, Delhi. However, a reduction of the column density of the O3 layer was seen towards the Southern part of India, whereas the density was highest in Northern India. The Gangetic region and some parts of the Eastern region showed a higher concentration of AOD during the study period. A complete lockdown was implemented in India from March to May 2020 in India. The effects of the lockdown on air pollution were reflected in the temporal distribution of the pollutants (Fig. 3 ). As our study was carried out from April 2020, a sudden fall in the concentration of pollutants was observed in the first twelve weeks. A steady upward trend in AOD after the lockdown period clearly illustrates the contribution of human activities to air pollution.
Fig. 2.
Spatial distribution of the pollutants during the study period (April 26, 2020 to July 10, 2021) over India; (a) NO2, (b) SO2, (c) O3 and (d) AOD.
Fig. 3.
Temporal distribution of the pollutants during the study period (April 26, 2020–July 10, 2021) over India.
3.2. Spatio-temporal shift of COVID-19
This section covers the spatial pattern of confirmed cases, infection, and CFR over time. Further, it shows a spatial association between environmental parameters and cCFR. The estimation of air pollution factors affecting the CFR of COVID-19 is presented at the end.
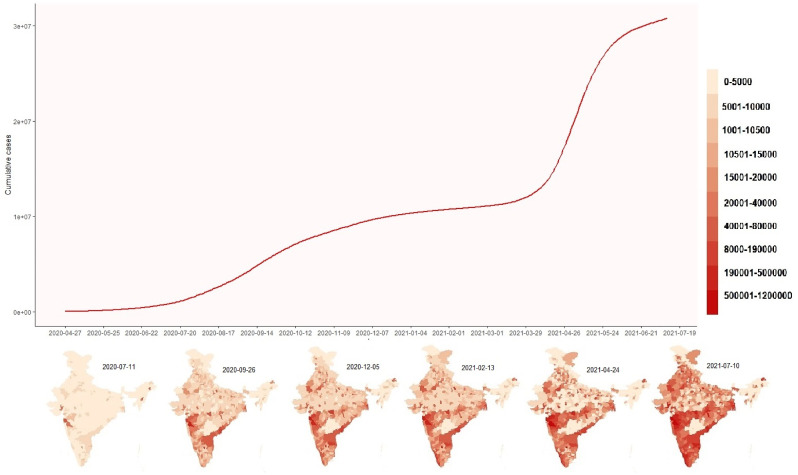
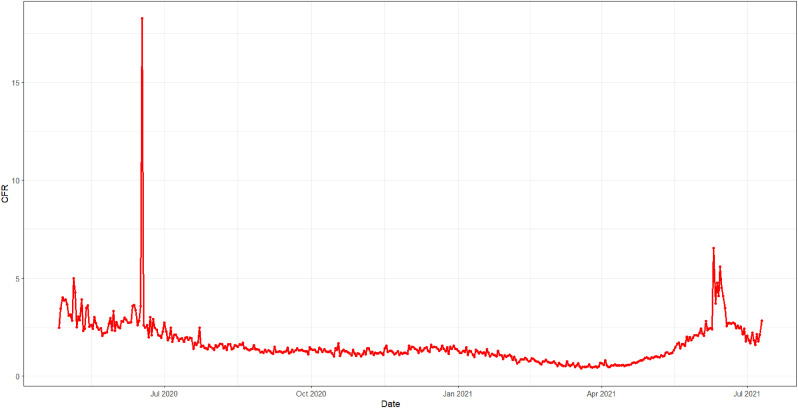
The timeline of cumulative confirmed cases and their spatial distribution has been shown in Fig. 4 . A rapidly rising graph of cumulative cases can be observed from July 2020, and during that time, Western India had the highest number of cases. However, the study observed a spatial concentration of cases in Western and some parts of Southern India during the peak of the first wave of COVID-19 in September 2020. Again, the second wave in India was observed from March 2021, and a rapidly rising number of reported cases can be seen in Fig 4. In contrast, Western, Southern, and some parts of Eastern India contributed significantly. A seasonal pattern of CFR can be observed in Fig. 5 . The figure shows two peaks in June, which had declined until October. The trend line of CFR increased slowly to January, then shrunk until April, from where a rapidly growing trend of CFR was identified in the study.
Fig. 4.
Spatio-temporal distribution of cumulative infected cases of COVID-19 during the study period (April 26, 2020 to July 10, 2021) in India.
Fig. 5.
Time series plot of CFR in India during the study period, April 26, 2020 to July 10, 2021 in India.
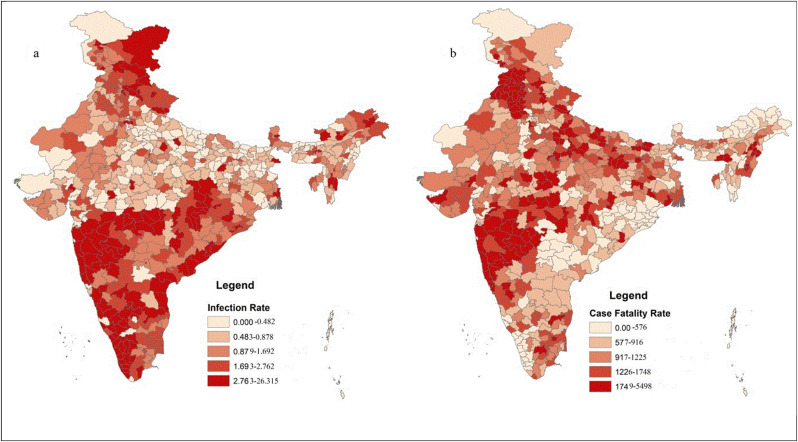
Fig. 6 depicts the spatial pattern of infection rate and CFR across 640 districts of India. It is worth noting that the regional heterogeneity existing in terms of the infection rate of COVID-19 is distinct in India. The occurrence of infection rate was concentrated in most of the Western and Southern regions of India. Interestingly, the lowest level of infection rate was observed in the Central region. The spatial pattern of CFR shows a higher concentration in Northern and parts of Western India. Although the infection rate of Sothern India was greater, the CFR was lower in that region.
Fig. 6.
Spatial distribution of (a) infection rate and (b) CFR of COVID-19 on July 10, 2021 in India.
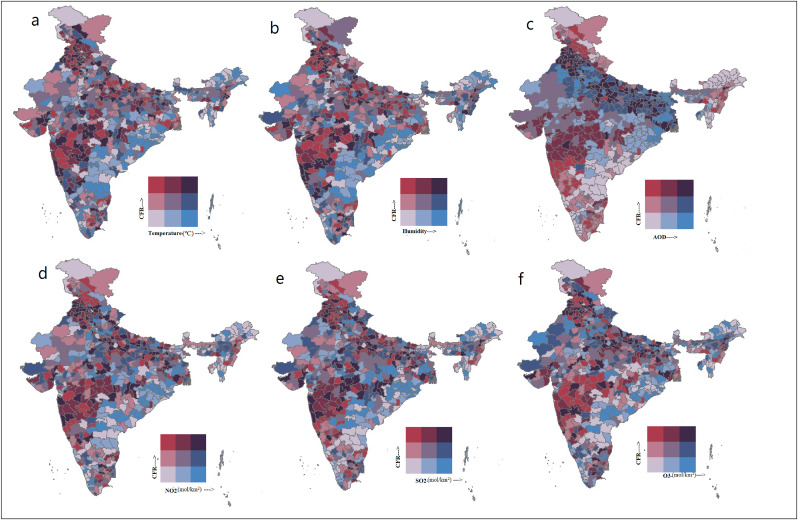
3.3. Spatial association between environmental parameters and COVID-19
The spatial association between environmental parameters and CFR across the districts of India is shown in Fig. 7 . Multiple spatial clusters are simultaneously formed for environmental determinants and CFR, indicating an unequal and varied distribution of CFR across India. However, four main spatial clusters can be recognized during the entire study period. The first cluster was developed over Western India for all the environmental factors, where maximal contribution was from the state of Maharashtra. The second cluster was observed in Northern India, especially the Upper Indo-Gangetic region, which covers the states of Punjab, Haryana, Delhi, Uttar Pradesh, and Bihar. Although a significant spatial association between CFR and all the pollutants such as NO2, SO2, and O3 was identified in the Upper Gangetic region, the association was highest for AOD. The last cluster was located in the Southern part of Tamil Nadu (see Fig. 7) (see Table 1).
Fig. 7.
Bivariate spatial association between CFR and (a) Temperature, (b) RH, (c) AOD, (d) NO2, (e) SO2 and (f) O3 during the study period, April 26, 2020 to July 10, 2021 in India.
Table 1.
Study area-wise literature review showing environmental pollution impact on COVID-19.
| Authors | Pollutants | Country | Study period | Health Effect |
|---|---|---|---|---|
| Rahman et al. (2020) | Temperature, CO2 | 149 countries | January 1, 2020–May 10, 2020 | COVID-19 lethality was negatively associated with temperature. |
| Bashir et al. (2020) | Temperature, Relative humidity, Wind Speed, Air Quality, Rainfall | USA | March 1, 2020–April 12, 2020 | Mean temperature, minimum temperature, and air quality were significantly associated with the COVID-19 pandemic |
| Fattorini & Regoli (2020) | NO2, O3, PM10, PM2.5 | Italy | 2016–2019 | Long-term air-quality data was significantly correlated with COVID-19 cases across 71 Italian provinces |
| Mendy et al. (2021) | PM2.5 | USA | 2009–2018 | 1μg/m3increase in annual PM2.5 was associated with 18% higher hospitalization rates. |
| Chattopadhyay and Shaw, 2021b | SO2, NO2, PM10 | India | 2017–2019 | Spatial auto regressive models suggest that COVID-19 death in Mumbai is associated with higher ambient NO2. |
| Liu et al. (2020) | Temperature, Relative humidity | China | January 5, 2020–March 2, 2020 | Various meteorological factors were associated with increasing COVID-19 cases with accumulated time duration up to 14 days. |
| Zhu et al. (2020) | daily mean temperature, relative humidity, air pressure, and wind speed | China | January 23, 2020–February 29, 2020 | 1°C rise in the mean temperature was associated with a 4.8% increase in the daily COVID-19 cases in China. |
| Gupta et al. (2021) | PM10, PM2.5 | India, Pakistan, Indonesia, China | 2020 | Exposures to PM2.5 over a long period, was significantly correlate with COVID-19 mortality per unit reported cases compared to PM10 (p < 0.05). |
| Setti et al. (2020) | PM10 | Italy | February 24, 2020–March 13, 2020 | PM10 appeared to be a significant predictor of COVID-19 infection across 110 Italian provinces (p < 0.001). |
| Sajadi et al. (2020) | Temperature, Relative humidity, | Multi-Country | January 1, 2020–March 10, 2020 | 50 cities across the globe, along the 30° N to 50° N latitudes cities have shown transmission of COVID-19 with 5–11 °C temperature combined with low specific and absolute humidity. |
| Wang et al. (2021) | Temperature, Relative humidity | China, USA | 2020 | Negative correlations are found between temperature/relative humidity and the reproductive number (R value) in both China and the USA. |
| Adhikari and Yin (2020) | Ozone, PM2.5 | USA | 2019 | Daily average temperature, daily maximum 8-h ozone concentration, average relative humidity, and cloud percentages were significantly and positively associated with daily COVID-19 infection. |
| Comunian et al. (2020) | PM | Italy | 2020 | PM played a significant influence in the transmission of COVID-19 across different Italian cities where the daily PM concentrations were found to be greater than the permissible limit in the months prior to the pandemic. |
| Kolluru et al. (2021) | PM2.5, PM10, CO, O3, AQI | India | 2020 | Temperature was strongly correlated with the COVID-19 cases and deaths during the lockdown (r = 0.54; 0.25) and unlock period (r = 0.66; 0.25). While, O3 and temperature explained variability, up to 34% and 30% of COVID-19 confirmed cases and deaths respectively. |
3.4. Time-series analysis
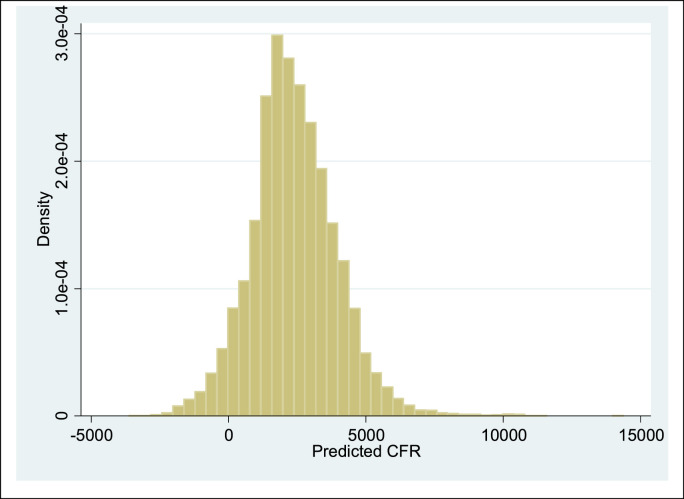
The Bayesian linear regression analysis showing the estimation of environmental factors affecting the CFR has been presented in Table 2 . The analysis controlled all possible confounders. From the graphical summaries as already explained in the method section (see Fig. 1) it can be seen that the MCMC convergence of relevant factors were satisfied. The regression results show that theCFR increases 40.89 units with one unit increase in temperature (MCSE: 0.01, p < 0.001). The CFR also increases significantly by 20.79 units with a unit increase in RH (MCSE: 0.02; p < 0.001). The CFR shows positive relation with AOD, thus indicating that with a unit increase in AOD there is around a 0.99 unit increase in CFR (MCSE: 0.01, p < 0.001). With a unit change in NO2 in the atmosphere, there is a 16.54 unit increase in CFR (MCSE: 0.02; p <0.001). The level of ozone too had a significant positive association with CFR (MCSE: 0.13, p <0.001). Availability of beds in the hospitals, state-level burden of cardiovascular and respiratory diseases, the percentage contribution to Gross State Domestic Product (GSDP), urban growth, population density, and dependency ratio were considered in the model as confounding factors. The predicted case fatality has been plotted in Fig. 8 after model fitting indicating a good normal fit.
Table 2.
Bayesian multivariate linear regression model estimation of environmental factors with CFR of COVID-19.
| Covariates | Case fatality rate |
|
|---|---|---|
| Mean Coefficient (CI) | MCSE | |
| Temperature (°C) | 40.890***(40.782,41.002) | 0.0087 |
| RH | 20.790***(20.454,21.157) | 0.0217 |
| AOD | 0.997***(0.865,1.132) | 0.0108 |
| SO2 (mol/km2) | −1.170***(-1.276, −1.076) | 0.0135 |
| NO2 (mol/km2) | 16.540***(16.392,16.674) | 0.0183 |
| O3 (mol/km2) | 0.126***(0.121,0.131) | 0.0003 |
Note: ***-p<0.001; **- p < 0.01; *-p<0.05; MCSE: Monte Carlo Standard error; RH: Relativehumidity, AOD: Aerosol Optical Depth, SO2: Sulphurdioxide, NO2: Nitrogendioxide, O3: Ozone,Controlled for hospital beds, cardiovascular disease, respiratory disease,Gross State Domestic Product, urban , population density, dependency ratio.
Fig. 8.
Predicted case fatality rate (CFR) after model fitting.
4. Discussion
In this study, we have explored the spatial shift of the COVID-19 pandemic over time across Indian districts. We visualize how the clustering pattern of active COVID-19 infected cases changed from the first phase to the peak of the second phase of the pandemic across India, i.e., from April 26, 2020, to July 10, 2021. The spatial distribution of the infection rate and CFR of COVID-19 can help depict the pandemic situation quantitatively. Finally, the time series analysis shows the association between environmental factors and the CFR for COVID-19 to bridge the huge gap in Indian literature in this arena of research.
4.1. Indian perspective on air pollution
Air pollution is attributed as one of the most potent environmental risks to health, especially in low and middle-income countries. The significant role of air pollution in cardiovascular health and disease is reflected in the recent WHO estimates of the burden of premature deaths occurring due to outdoor ambient air pollutants with the highest numbers reported in South-East Asia and Western Pacific countries (WHO, 2022). In India, the mandate under the Air (Prevention and Control of Pollution) Act has aimed to set standards for the quality of air to meet internationally prescribed requirements. However, as per Central Pollution Control Board (CPCB) data from 2009, levels of Particulate Matters in India far exceed the international recommendations with annual time-weighted average PM2.5 levels being 4 times higher and PM10 levels being 3 times higher than WHO guidelines (WHO, 2020a). This calls for a dire need to address measures to cut down PM levels, among other factors contributing to air pollution as this could significantly reduce pollution-related deaths in the country. Our study reveals a reduction of varying pollutants after imposition of lockdown in India. While the lockdowns implemented during the course of the pandemic had an impressive influence on reducing PM levels , policies supporting cleaner industry, transport, energy-efficiency, and better municipal waste management are crucial to diminish key sources of outdoor air pollution and with it bring an expected decline in spread of communicable diseases like COVID-19 (Kumari et al., 2014).
4.2. Spread of the disease
The first case of COVID-19 was detected in the Southern region of India. A national lockdown was announced on 24th March 2020 to decelerate the spread of the virus (Arunachalam and Halwai, 2020). Our study establishes a clustering of COVID-19 cases in Western India followed by Southern India. Such spatial spread can be explained through the flow of migration. In the first wave of the pandemic, a huge number of people were affected in the Western region, where Maharashtra, and especially its metropolis of Mumbai, contributed to the highest number of infections (Ramasamy and Sundararajan, 2020). The Census 2011 states that Maharashtra and Delhi support the highest number of in-migrants in India (IRG, 2011). A large number of in-migrants reside in Mumbai and adjoining cities for economic opportunities (Bhagat and Keshri, 2020). Post-lockdown, most of the migrants tried to return to their place of origin by road transportation or even by foot (John and Kuruvilla, 2021). Thus, there was a greater possibility of spreading the virus over space. India announced phased unlocking from June 2020 onwards (Arunachalam and Halwai, 2020) considering the economic needs of the nation. Therefore, the movement of people returning to their permanent residences from different states and countries was further aggravated. India, especially Southern India is one of the major origin countries of migrant workers to the Middle East (Kodoth, 2020; Rajan and Saxena, 2019). Along with rapid testing and return migration, the virus started spreading across the Southern region of India (Jesline et al., 2021; Sarkar, 2021).
After the second week of June, the recovery cases started to exceed the active cases. A reduction in the rate of infection was observed in the month of September (Murhekar et al., 2021). Post-mid-January, people gradually started to normalize the situation and tackled the social and economic burden faced during the lockdown. The government announced the ‘endgame’ of COVID-19 at the beginning of 2021 (Lancet, 2021). People started gathering for social and political events. Although the vaccination program against the pandemic commenced in January, initially it was slow-paced, as the first priority was for the frontline workers followed by older persons with comorbidities and lastly, the general population (Kumar et al., 2021).
Our study depicts a laggard spread of the infection in North and East India. Such lag is due to the resurgence of the infection in the second wave in mid-2021 in India. The second wave of COVID-19 began in March 2021 and this wave was more dangerous as compared to the first wave (Lancet, 2021). This wave surged with a national emergency due to the relaxation of lockdown for several humanitarian and realistic reasons leading to uncontrolled public gatherings. Such free movement led to a crisis in Northern and Eastern India (Chakraborty et al., 2021; Quadri, 2020). The delta variant in the second wave was found to be 60% more transmissible than the alpha variant. The strain was also more deadly and common among the young and affluent population (Shiehzadegan et al., 2021). A national emergency was observed due to the huge number of hospitalizations (Lancet, 2021). A large number of deaths was seen in the second wave with the death rate reaching 1.4 from 1.0 in the first wave. However, previous studies found spatial disparities in infection and death rate of COVID-19 (Salvatore et al., 2021). The COVID-19 infected patients with comorbidities such as lung diseases, heart diseases, hypertension, and obesity were more prone to severe infection and death (Asirvatham et al., 2021).
4.3. Environment and infection
Our study observed a significant association of environmental parameters with the CFR of COVID-19 in India. Air temperature, AOD, SO2, and O3 were found to be significantly associated with CFR of COVID-19 in the study. Past environmental studies explored that respiratory diseases are closely influenced by environmental factors (Campbell-Lendrum and Prüss-Ustün, 2019; Santana et al., 2020; Schraufnagel et al., 2019). However, in India, this is the first pan-nation research that reveals a strong relation between COVID-19 and environmental condition, especially the air quality.
Past studies explored a negative association between temperature and mortality due to COVID-19 and these studies are from developed countries (Adhikari and Yin, 2020, Malki et al., 2020; Li et al., 2020). On the contrary, Rahman et al. (2020) stated that temperature is positively associated with COVID-19 mortality in low and middle-income countries. Our study also found a positive association of CFR with temperature, consistent with the previous study conducted in India and the subcontinent. A time-series analysis further stated that rising levels of temperature increase the COVID-19 mortality rate (Ma et al., 2020). High temperature is not only responsible for chronic diseases among older people but also among those who possess a weak immune system, leading to deaths with comorbidities among COVID-19 infected persons (Lin et al., 2009). The mean age of the deceased person in India is 62 and 85% of them were suffering from one or multiple comorbidities (Asirvatham et al., 2021). In addition, India is the leading country in the world in premature deaths and disability-adjusted life years (DALY) attributable to high temperatures (Song et al., 2021). One study from Pakistan, the neighbouring country of India, also found a similar association (Basray et al., 2021). Thus, the study found a potent role of temperature with mortality due to COVID-19. Further, a seasonal pattern of CFR was observed in the study. The peak of CFR was observed in the month of June which corroborates the previous studies conducted in India (Jha et al., 2022, Laxminarayan et al., 2021). However, a virological investigation is required to understand the mechanisms behind it.
In the study, a significant association was also observed between CFR for COVID-19 and air pollutants such as AOD (PM2.5 and PM10), SO2, and O3. PM2.5 is the leading health risk factor as it can penetrate deep into the human body (Xing et al., 2016). Air pollution and exposure to SARS CoV-2 lead to “double-hit” and severe lung injury (Frontera et al., 2020a). PM2.5 enters peripheral airspace and may facilitate viral infections by interacting with the renin-angiotensin system (RAS) of the lungs. SARS-CoV-2 binding to ACE-2 can lead to deficient anti-inflammatory action in severe lung injury (Bourdrel et al., 2021; Xing et al., 2016). Moreover, long exposure to PM2.5 is associated with cardiovascular and respiratory dysfunctions, which increases the risk of death among COVID-19 infected patients (Semczuk-Kaczmarek et al., 2021).
India ranks 168 out of 180 countries worldwide in terms of PM2.5 concentration (Wendling et al., 2020). Moreover, 14 most polluted cities among the top 15 are contributed by India (Environmental Performance Index, 2020). India loses 1.36% of GDP due to premature deaths and morbidity attributable to air pollution (Balakrishnan et al., 2019). Interestingly, we found a spatial association of CFR with PM2.5 in the Upper-Gangetic region, where AOD is at its highest level in India (Das et al., 2021). Long term exposure to air pollutants can increase the susceptibility to the infection (Semczuk-Kaczmarek et al., 2021). This virus can be transmitted through particulate matters, especially PM2.5 (Comunian et al., 2020; Nor et al., 2021).
The air pollutants decreased during the lockdown periods of the pandemic. However, an increasing level of surface ozone was observed in India during that period (Allu et al., 2021; Das et al., 2021). Ozone, one of the primary greenhouse gases, is extremely harmful to human health. Long exposure to ozone is not only responsible for premature deaths but also comorbidities such as cardiovascular and respiratory diseases (Adhikari and Yin, 2020; Allu et al., 2021; Xu, 2021). In addition, pre-exposure to O3 increases cellular protease activity, which helps the virus to enter the host cells. This proteolysis has a major role in spreading respiratory viruses, including SARS CoV-2 (Bourdrel et al., 2021; Kesic et al., 2012). In line with our findings, previous studies also found a positive association between mortality for COVID-19 and exposure to O3 (Adhikari and Yin, 2020; Kolluru et al., 2021).
Our study indicates that a high level of SO2 is significantly associated with death due to COVID-19. Previous epidemiological studies found that long exposure to SO2 is a risk factor for respiratory inflammation and a series of respiratory complications (Marquès and Domingo, 2022; Reno et al., 2015; Santana et al., 2020). Moreover, short-term exposure to SO2 has been considered by past evidence as a risk factor for ischemic heart disease, leading to comorbidities for COVID-19 death (Orellano et al., 2021).
4.4. Issues related to data and possible explanations
One of the major limitations of the study includes the lack of socioeconomic and demographic profile of the expired cases, where the analysis could have controlled those factors for more robustness. Future studies, including more in-depth inclusion of factors catering to social, economic, medical and other climatic factors, are recommended for a more comprehensive understanding. We were not able to include the most recent scenario of the disease due to limited information that is not deemed fit for spatial analysis. We could not deny the reporting error related to infection and death. However, the argument in favor of our findings is that, in the case of reporting error of death, fatality would have also been higher in the South and other better urbanized/developed states of India for better reporting of such deaths, and that is not the case. The study reveals that the infection was higher in South India, Maharashtra, and Punjab which could be due to more testing. Had there been reporting bias in fatality, it would have shown higher concentration in states where health surveillance, testing and reporting, etc were better. However, the North has more fatality and one of the strong reasons for higher CFR is air pollution as shown in our study. The state-wise overall excess mortality during this critical period of pandemic is given in the recently published paper of Jha et al. (2022). States that experienced excess mortality can easily be linked to COVID-19 deaths and again it is supporting our findings of more mortality concentration in North India.
India's notably higher COVID-19 death rate in 2021, compared to the lower-than-expected death rate in 2020, requires further research due to the fact that the nature of the virus changed between these two waves. Similarly, tracking infection and death rates, and release of detail data are essential to understand the effects of future viral variants.
5. Conclusions
This study provides evidence to support the role of environmental factors in the spread of COVID-19 in India. The study suggests that air quality is a significant element associated with COVID-19 related morbidity and mortality, which demands concentrated attention for air quality management and disease control. Policies should be designed to tackle this as one of the risk factors, which has the potential to exacerbate the infection, especially in highly susceptible population groups.
A spatial shifting of the COVID-19 clustering from Western to Southern India followed by the Northern and the Eastern parts of India were observed in the research. We established a significant association between COVID-19 and pollution (AOD, O3, and NO2). Long-term exposure to poor air qualityleads to living with multi-morbidities and dysregulated immune systems, which increases the possibility of dying due to COVID-19. Clean air should be part of the approach to protecting human health. Since a significant relation of environmental factors on CFR is observed in India, it is important to develop an effective mitigation policy and a public attitude towards precautionary measures to overcome this epidemic in India.
Credit author statement
Arup Jana: conceptualization, methodology, software, data curation, formal analysis and writing – original draft; Sampurna Kundu: conceptualization, methodology, formal analysis, writing – original draft; Subhojit Shaw: conceptualization, methodology, data curation, writing – original draft; Sukanya Chakraborty: writing original draft & editing; Aparajita Chattopadhyay: conceptualization, methodology, validation, writing and editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Data availability
Data will be made available on request.
References
- Abdelzaher H., Saleh B.M., Ismail H.A., Hafiz M., Gabal M.A., Mahmoud M., Hashish S., Gawad R.M.A., Gharieb R.Y., Abdelnaser A. COVID-19 genetic and environmental risk factors: a look at the evidence. Front. Pharmacol. 2020;11 doi: 10.3389/fphar.2020.579415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams M.D. Air pollution in Ontario, Canada during the COVID-19 state of emergency. Sci. Total Environ. 2020;742 doi: 10.1016/j.scitotenv.2020.140516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adhikari A., Yin J. Short-term effects of ambient ozone, PM2.5, and meteorological factors on COVID-19 confirmed cases and deaths in Queens, New York. Int. J. Environ. Res. Publ. Health. 2020;17:4047. doi: 10.3390/ijerph17114047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmadi M., Sharifi A., Dorosti S., Jafarzadeh Ghoushchi S., Ghanbari N. Investigation of effective climatology parameters on COVID-19 outbreak in Iran. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albayati N., Waisi B., Al-Furaiji M., Kadhom M., Alalwan H. Effect of COVID-19 on air quality and pollution in different countries. J. Transport Health. 2021;21 doi: 10.1016/j.jth.2021.101061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allu S.K., Reddy A., Srinivasan S., Maddala R.K., Anupoju G.R. Surface ozone and its precursor gases concentrations during COVID-19 lockdown and pre-lockdown periods in Hyderabad city, India. Environ. Process. 2021;8:959–972. doi: 10.1007/s40710-020-00490-z. [DOI] [Google Scholar]
- Andrieu C., de Freitas N., Doucet A., Jordan M.I. An introduction to MCMC for machine learning. Mach. Learn. 2003;50:5–43. doi: 10.1023/A:1020281327116. [DOI] [Google Scholar]
- Arunachalam M.A., Halwai A. An analysis of the ethics of lockdown in India. ABR. 2020;12:481–489. doi: 10.1007/s41649-020-00133-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asirvatham E.S., Sarman C.J., Saravanamurthy S.P., Mahalingam P., Maduraipandian S., Lakshmanan J. Who is dying from COVID-19 and when? An Analysis of fatalities in Tamil Nadu, India. Clinical Epidemiology and Global Health. 2021;9:275–279. doi: 10.1016/j.cegh.2020.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balakrishnan K., Dey S., Gupta T., Dhaliwal R.S. The impact of air pollution on deaths, disease burden, and life expectancy across the states of India: the Global Burden of Disease Study 2017. Lancet Planet. Health. 2019;3:e26–e39. doi: 10.1016/S2542-5196(18)30261-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balakrishnan Kalpana, Dey S., Gupta T., Dhaliwal R.S., Brauer M., Cohen A.J., Stanaway J.D., Beig G., Joshi T.K., Aggarwal A.N., Sabde Y., Sadhu H., Frostad J., Causey K., Godwin W., Shukla D.K., Kumar G.A., Varghese C.M., Muraleedharan P., Agrawal A., Anjana R.M., Bhansali A., Bhardwaj D., Burkart K., Cercy K., Chakma J.K., Chowdhury S., Christopher D.J., Dutta E., Furtado M., Ghosh S., Ghoshal A.G., Glenn S.D., Guleria R., Gupta R., Jeemon P., Kant R., Kant S., Kaur T., Koul P.A., Krish V., Krishna B., Larson S.L., Madhipatla K., Mahesh P.A., Mohan V., Mukhopadhyay S., Mutreja P., Naik N., Nair S., Nguyen G., Odell C.M., Pandian J.D., Prabhakaran D., Prabhakaran P., Roy A., Salvi S., Sambandam S., Saraf D., Sharma M., Shrivastava A., Singh V., Tandon N., Thomas N.J., Torre A., Xavier D., Yadav G., Singh S., Shekhar C., Vos T., Dandona R., Reddy K.S., Lim S.S., Murray C.J.L., Venkatesh S., Dandona L. The impact of air pollution on deaths, disease burden, and life expectancy across the states of India: the Global Burden of Disease Study 2017. Lancet Planet. Health. 2019;3:e26–e39. doi: 10.1016/S2542-5196(18)30261-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bashir M.F., Ma B., Bilal null, Komal B., Bashir M.A., Tan D., Bashir M. Correlation between climate indicators and COVID-19 pandemic in New York, USA. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basray R., Malik A., Waqar W., Chaudhry A., Wasif Malik M., Ali Khan M., Ansari J.A., Ikram A. Impact of environmental factors on COVID-19 cases and mortalities in major cities of Pakistan. Journal of Biosafety and Biosecurity. 2021;3:10–16. doi: 10.1016/j.jobb.2021.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bayes T., Hume D. Proceedings Ofthe British Academy. 1763. BAYES’S theorem. [Google Scholar]
- Berman J.D., Ebisu K. Changes in U.S. air pollution during the COVID-19 pandemic. Sci. Total Environ. 2020;739 doi: 10.1016/j.scitotenv.2020.139864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhagat R.B., Keshri K. In: Internal Migration in the Countries of Asia: A Cross-National Comparison. Bell M., Bernard A., Charles-Edwards E., Zhu Y., editors. Springer International Publishing; Cham: 2020. Internal migration in India; pp. 207–228. [DOI] [Google Scholar]
- Bontempi E. First data analysis about possible COVID-19 virus airborne diffusion due to air particulate matter (PM): the case of Lombardy (Italy) Environ. Res. 2020;186 doi: 10.1016/j.envres.2020.109639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bontempi E. First data analysis about possible COVID-19 virus airborne diffusion due to air particulate matter (PM): the case of Lombardy (Italy) Environ. Res. 2020;186 doi: 10.1016/j.envres.2020.109639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourdrel T., Annesi-Maesano I., Alahmad B., Maesano C.N., Bind M.-A. The impact of outdoor air pollution on COVID-19: a review of evidence from in vitro, animal, and human studies. Eur. Respir. Rev. 2021;30 doi: 10.1183/16000617.0242-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell-Lendrum D., Prüss-Ustün A. Climate change, air pollution and noncommunicable diseases. Bull. World Health Organ. 2019;97:160–161. doi: 10.2471/BLT.18.224295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Census, 2011. Census of India. New Delhi: Office of the Registrar General and Census Commissioner, India.
- Chakraborty C., Sharma A.R., Bhattacharya M., Agoramoorthy G., Lee S.-S. The current second wave and COVID-19 vaccination status in India. Brain Behav. Immun. 2021;96:1–4. doi: 10.1016/j.bbi.2021.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chattopadhyay A., Shaw S. Association between air pollution and COVID-19 pandemic: an investigation in Mumbai, India. Geohealth. 2021;5 doi: 10.1029/2021GH000383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chattopadhyay A., Shaw S. Association between air pollution and COVID-19 pandemic: an investigation in Mumbai, India. Geohealth. 2021;5 doi: 10.1029/2021GH000383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudhuri S., Basu S., Kabi P., Unni V.R., Saha A. Modeling the role of respiratory droplets in Covid-19 type pandemics. Phys. Fluids. 2020;32 doi: 10.1063/5.0015984. 1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chauhan A., Singh R.P. Decline in PM2.5 concentrations over major cities around the world associated with COVID-19. Environ. Res. 2020;187 doi: 10.1016/j.envres.2020.109634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L.-W.A., Chien L.-C., Li Y., Lin G. Nonuniform impacts of COVID-19 lockdown on air quality over the United States. Sci. Total Environ. 2020;745 doi: 10.1016/j.scitotenv.2020.141105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen A.J., Brauer M., Burnett R., Anderson H.R., Frostad J., Estep K., Balakrishnan K., Brunekreef B., Dandona L., Dandona R., Feigin V., Freedman G., Hubbell B., Jobling A., Kan H., Knibbs L., Liu Y., Martin R., Morawska L., Pope C.A., Shin H., Straif K., Shaddick G., Thomas M., van Dingenen R., van Donkelaar A., Vos T., Murray C.J.L., Forouzanfar M.H. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet. 2017;389:1907. doi: 10.1016/S0140-6736(17)30505-6. –1918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comunian S., Dongo D., Milani C., Palestini P. Air pollution and COVID-19: the role of particulate matter in the spread and increase of COVID-19's morbidity and mortality. Int. J. Environ. Res. Publ. Health. 2020;17:4487. doi: 10.3390/ijerph17124487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conticini E., Frediani B., Caro D. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? Environ. Pollut. 2020;261 doi: 10.1016/j.envpol.2020.114465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conticini E., Frediani B., Caro D. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? Environ. Pollut. 2020;261 doi: 10.1016/j.envpol.2020.114465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui Y., Ji D., Maenhaut W., Gao W., Zhang R., Wang Y. Levels and sources of hourly PM2.5-related elements during the control period of the COVID-19 pandemic at a rural site between Beijing and Tianjin. Sci. Total Environ. 2020;744 doi: 10.1016/j.scitotenv.2020.140840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das M., Das A., Ghosh S., Sarkar R., Saha S. Spatio-temporal concentration of atmospheric particulate matter (PM2.5) during pandemic: a study on most polluted cities of indo-gangetic plain. Urban Clim. 2021;35 doi: 10.1016/j.uclim.2020.100758. [DOI] [Google Scholar]
- Dibyachintan S., Nandy P., Das K., Vinjanampathy S., Mitra M.K. 2020. Unequal Lives: A Sociodemographic Analysis of Covid19 Transmission and Mortality in India. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diffey B.L. Solar ultraviolet radiation effects on biological systems. Phys. Med. Biol. 1991;36:299–328. doi: 10.1088/0031-9155/36/3/001. [DOI] [PubMed] [Google Scholar]
- Dutta A., Dutta G. Association of air pollution and meteorological variables with the two waves of COVID-19 pandemic in Delhi: a critical analysis. Heliyon. 2021;7 doi: 10.1016/j.heliyon.2021.e08468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Environmental Performance Index | Environmental Performance Index [WWW Document], n.d. URL https://epi.yale.edu/epi-results/2020/component/epi (accessed 2.8.22).
- Fattorini D., Regoli F. Role of the chronic air pollution levels in the Covid-19 outbreak risk in Italy. Environ. Pollut. 2020;264 doi: 10.1016/j.envpol.2020.114732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frontera A., Cianfanelli L., Vlachos K., Landoni G., Cremona G. Severe air pollution links to higher mortality in COVID-19 patients: the “double-hit” hypothesis. J. Infect. 2020;81:255–259. doi: 10.1016/j.jinf.2020.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frontera A., Martin C., Vlachos K., Sgubin G. Regional air pollution persistence links to COVID-19 infection zoning. J. Infect. 2020;81:318–356. doi: 10.1016/j.jinf.2020.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fudenberg D., He K., Imhof L.A. Bayesian posteriors for arbitrarily rare events. Proc. Natl. Acad. Sci. USA. 2017;114:4925–4929. doi: 10.1073/pnas.1618780114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerretsen, I., 2020. How Air Pollution Exacerbates Covid-19 [WWW Document]. URL https://www.bbc.com/future/article/20200427-how-air-pollution-exacerbates-covid-19 (accessed 12.6.22).
- Guo H., Kota S.H., Sahu S.K., Hu J., Ying Q., Gao A., Zhang H. Source apportionment of PM2.5 in North India using source-oriented air quality models. Environ. Pollut. 2017;231:426–436. doi: 10.1016/j.envpol.2017.08.016. [DOI] [PubMed] [Google Scholar]
- Gupta A., Bherwani H., Gautam S., Anjum S., Musugu K., Kumar N., Anshul A., Kumar R. Air pollution aggravating COVID-19 lethality? Exploration in Asian cities using statistical models. Environ. Dev. Sustain. 2021;23:6408–6417. doi: 10.1007/s10668-020-00878-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heßling M., Hönes K., Vatter P., Lingenfelder C. Ultraviolet irradiation doses for coronavirus inactivation – review and analysis of coronavirus photoinactivation studies. GMS Hyg Infect Control. 2020;15:Doc08. doi: 10.3205/dgkh000343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann M., Kleine-Weber H., Schroeder S., Krüger N., Herrler T., Erichsen S., Schiergens T.S., Herrler G., Wu N.-H., Nitsche A., Müller M.A., Drosten C., Pöhlmann S. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280.e8. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussain M., Jabeen N., Raza F., Shabbir S., Baig A.A., Amanullah A., Aziz B. Structural variations in human ACE2 may influence its binding with SARS-CoV-2 spike protein. J. Med. Virol. 2020;92:1580–1586. doi: 10.1002/jmv.25832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IRG . 2011. Population Tables 2011, Census of India. [Google Scholar]
- Jesline J., Romate J., Rajkumar E., George A.J. The plight of migrants during COVID-19 and the impact of circular migration in India: a systematic review. Humanit Soc Sci Commun. 2021;8:1–12. doi: 10.1057/s41599-021-00915-6. [DOI] [Google Scholar]
- Jha P., Deshmukh Y., Tumbe C., Suraweera W., Bhowmick A., Sharma S., Novosad P., Fu S.H., Newcombe L., Gelband H., Brown P. COVID mortality in India: national survey data and health facility deaths. Science. 2022;375:667–671. doi: 10.1126/science.abm5154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- John Y.V., Kuruvilla M. In: Gendered Experiences of COVID-19 in India. George I., Kuruvilla M., editors. Springer International Publishing; Cham: 2021. The plight of migrant women workers of India during COVID-19: looking at ‘ghar wapsi’ through a gender lens; pp. 117–143. [DOI] [Google Scholar]
- Karuppasamy M.B., Seshachalam S., Natesan U., Ayyamperumal R., Karuppannan S., Gopalakrishnan G., Nazir N. Air pollution improvement and mortality rate during COVID-19 pandemic in India: global intersectional study. Air Qual Atmos Health. 2020;13:1375–1384. doi: 10.1007/s11869-020-00892-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kesic M.J., Meyer M., Bauer R., Jaspers I. Exposure to ozone modulates human airway protease/antiprotease balance contributing to increased influenza A infection. PLoS One. 2012;7 doi: 10.1371/journal.pone.0035108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kodoth P. 2020. In the Shadow of the State: Recruitment and Migration of South Indian Women as Domestic Workers to the Middle East. [Google Scholar]
- Kolluru S.S.R., Patra A.K., Nazneen Shiva Nagendra S.M. Association of air pollution and meteorological variables with COVID-19 incidence: evidence from five megacities in India. Environ. Res. 2021;195 doi: 10.1016/j.envres.2021.110854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kudo E., Song E., Yockey L.J., Rakib T., Wong P.W., Homer R.J., Iwasaki A. Low ambient humidity impairs barrier function and innate resistance against influenza infection. Proc. Natl. Acad. Sci. U. S. A. 2019;116:10905–10910. doi: 10.1073/pnas.1902840116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar P., Hama S., Omidvarborna H., Sharma A., Sahani J., Abhijith K.V., Debele S.E., Zavala-Reyes J.C., Barwise Y., Tiwari A. Temporary reduction in fine particulate matter due to ‘anthropogenic emissions switch-off’ during COVID-19 lockdown in Indian cities. Sustain. Cities Soc. 2020;62 doi: 10.1016/j.scs.2020.102382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar V.M., Pandi-Perumal S.R., Trakht I., Thyagarajan S.P. Strategy for COVID-19 vaccination in India: the country with the second highest population and number of cases. npj Vaccines. 2021;6:1–7. doi: 10.1038/s41541-021-00327-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumari K., Singh S.R., Sinha R.C. Role of pollution control boards in municipal solid waste management. International journal of environmental technology and management. 2014;17(2–4):100–112. [Google Scholar]
- Lancet T. India's COVID-19 emergency. Lancet. 2021;397:1683. doi: 10.1016/S0140-6736(21)01052-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laxminarayan R., Vinay T.G., Kumar K.A., Wahl B., Lewnard J.A. SARS-CoV-2 infection and mortality during the first epidemic wave in Madurai, south India: a prospective, active surveillance study. The Lancet Infectious Diseases. 2021;21(12):1665–1676. doi: 10.1016/S1473-3099(21)00393-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy R.C., Mattoo S., Munchak L.A., Remer L.A., Sayer A.M., Patadia F., Hsu N.C. The Collection 6 MODIS aerosol products over land and ocean. Atmos. Meas. Tech. 2013;6:2989–3034. doi: 10.5194/amt-6-2989-2013. [DOI] [Google Scholar]
- Li H., Xu X.-L., Dai D.-W., Huang Z.-Y., Ma Z., Guan Y.-J. Air pollution and temperature are associated with increased COVID-19 incidence: a time series study. Int. J. Infect. Dis. 2020;97:278–282. doi: 10.1016/j.ijid.2020.05.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin S., Luo M., Walker R.J., Liu X., Hwang S.-A., Chinery R. Extreme high temperatures and hospital admissions for respiratory and cardiovascular diseases. Epidemiology. 2009;20:738–746. doi: 10.1097/EDE.0b013e3181ad5522. [DOI] [PubMed] [Google Scholar]
- Liu J., Zhou J., Yao J., Zhang X., Li L., Xu X., He X., Wang B., Fu S., Niu T., Yan J., Shi Y., Ren X., Niu J., Zhu W., Li S., Luo B., Zhang K. Impact of meteorological factors on the COVID-19 transmission: a multi-city study in China. Sci. Total Environ. 2020;726 doi: 10.1016/j.scitotenv.2020.138513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowen A.C., Steel J. Roles of humidity and temperature in shaping influenza seasonality. J. Virol. 2014;88:7692–7695. doi: 10.1128/JVI.03544-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Y., Zhao Y., Liu J., He X., Wang B., Fu S., Yan J., Niu J., Zhou J., Luo B. Effects of temperature variation and humidity on the death of COVID-19 in Wuhan, China. Sci. Total Environ. 2020;724 doi: 10.1016/j.scitotenv.2020.138226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahato S., Pal S., Ghosh K.G. Effect of lockdown amid COVID-19 pandemic on air quality of the megacity Delhi, India. Sci. Total Environ. 2020;730 doi: 10.1016/j.scitotenv.2020.139086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malki Z., Atlam E.-S., Hassanien A.E., Dagnew G., Elhosseini M.A., Gad I. Association between weather data and COVID-19 pandemic predicting mortality rate: machine learning approaches. Chaos, Solit. Fractals. 2020;138 doi: 10.1016/j.chaos.2020.110137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manisalidis I., Stavropoulou E., Stavropoulos A., Bezirtzoglou E. Environmental and health impacts of air pollution: a review. Front. Public Health. 2020;8 doi: 10.3389/fpubh.2020.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manisalidis I., Stavropoulou E., Stavropoulos A., Bezirtzoglou E. Environmental and health impacts of air pollution: a review. Front. Public Health. 2020;8 doi: 10.3389/fpubh.2020.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marquès M., Domingo J.L. Positive association between outdoor air pollution and the incidence and severity of COVID-19. A review of the recent scientific evidences. Environ. Res. 2022;203 doi: 10.1016/j.envres.2021.111930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendy A., Wu X., Keller J.L., Fassler C.S., Apewokin S., Mersha T.B., Xie C., Pinney S.M. Air pollution and the pandemic: long-term PM2.5 exposure and disease severity in COVID-19 patients. Respirology. 2021;26:1181–1187. doi: 10.1111/resp.14140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ming W., Zhou Z., Ai H., Bi H., Zhong Y. COVID-19 and air quality: evidence from China. Emerg. Mark. Finance Trade. 2020;56:2422–2442. doi: 10.1080/1540496X.2020.1790353. [DOI] [Google Scholar]
- Murhekar M.V., Bhatnagar T., Selvaraju S., Saravanakumar V., Thangaraj J.W.V., Shah N., Kumar Muthusamy Santhosh, Rade K., Sabarinathan R., Asthana S., Balachandar R., Bangar S.D., Bansal A.K., Bhat J., Chopra V., Das D., Deb A.K., Devi K.R., Dwivedi G.R., Khan S.M.S., Kumar C.P.G., Kumar M. Sunil, Laxmaiah A., Madhukar M., Mahapatra A., Mohanty S.S., Rangaraju C., Turuk A., Baradwaj D.K., Chahal A.S., Debnath F., Haq I., Kalliath A., Kanungo S., Kshatri J.S., Lakshmi G.G.J.N., Mitra A., Nirmala A.R., Prasad G.V., Qurieshi M.A., Sahay S., Sangwan R.K., Sekar K., Shukla V.K., Singh P.K., Singh P., Singh R., Varma D.S., Viramgami A., Panda S., Reddy D.C.S., Bhargava B., Andhalkar R., Chaudhury A., Deval H., Dhatrak S., Gupta R.R., Ilayaperumal E., Jagjeevan B., Jha R.C., Kiran K., Krishnan N.N., Kumar A., Kumar V.V., Nagbhushanam K., Nimmathota A., Pandey A.K., Pawar H.S., Rathore K.S., Robinson A., Singh H.B., Wilson V.C., Yadav A., Yadav R., Karunakaran T., Pradhan J., Sivakumar T., Jose A., Kalaiyarasi K., Dasgupta S., Anusha R., Anand T., Babu G.R., Chauhan H., Dikid T., Gangakhedkar R.R., Kant S., Kulkarni S., Muliyil J.P., Pandey R.M., Sarkar S., Shrivastava A., Singh S.K., Zodpey S., Das A., Das P., Dutta S., Kant R., Narain K., Narasimhaiah S., Pati S., Patil S., Rajkumar H., Ramarao T., Sarkar K., Singh S., Toteja G.S., Zaman K. SARS-CoV-2 antibody seroprevalence in India, August–September, 2020: findings from the second nationwide household serosurvey. Lancet Global Health. 2021;9:e257–e266. doi: 10.1016/S2214-109X(20)30544-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naqvi H.R., Datta M., Mutreja G., Siddiqui M.A., Naqvi D.F., Naqvi A.R. Improved air quality and associated mortalities in India under COVID-19 lockdown. Environ. Pollut. 2021;268 doi: 10.1016/j.envpol.2020.115691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nor N.S.M., Yip C.W., Ibrahim N., Jaafar M.H., Rashid Z.Z., Mustafa N., Hamid H.H.A., Chandru K., Latif M.T., Saw P.E., Lin C.Y., Alhasa K.M., Hashim J.H., Nadzir M.S.M. Particulate matter (PM2.5) as a potential SARS-CoV-2 carrier. Sci. Rep. 2021;11:2508. doi: 10.1038/s41598-021-81935-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orellano P., Reynoso J., Quaranta N. Short-term exposure to sulphur dioxide (SO2) and all-cause and respiratory mortality: a systematic review and meta-analysis. Environ. Int. 2021;150 doi: 10.1016/j.envint.2021.106434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otmani A., Benchrif A., Tahri M., Bounakhla M., Chakir E.M., El Bouch M., Krombi M. Impact of covid-19 lockdown on PM10, SO2 and NO2 concentrations in salé city (Morocco) Sci. Total Environ. 2020;735 doi: 10.1016/j.scitotenv.2020.139541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pal S.C., Chowdhuri I., Saha A., Chakrabortty R., Roy P., Ghosh M., Shit M. Improvement in ambient-air-quality reduced temperature during the COVID-19 lockdown period in India. Environ. Dev. Sustain. 2021;23:9581–9608. doi: 10.1007/s10668-020-01034-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandey A., Brauer M., Cropper M.L., Balakrishnan K., Mathur P., Dey Sagnik, Turkgulu B., Kumar G.A., Khare M., Beig G., Gupta T., Krishnankutty R.P., Causey K., Cohen A.J., Bhargava S., Aggarwal A.N., Agrawal A., Awasthi S., Bennitt F., Bhagwat S., Bhanumati P., Burkart K., Chakma J.K., Chiles T.C., Chowdhury S., Christopher D.J., Dey Subhojit, Fisher S., Fraumeni B., Fuller R., Ghoshal A.G., Golechha M.J., Gupta P.C., Gupta Rachita, Gupta Rajeev, Gupta S., Guttikunda S., Hanrahan D., Harikrishnan S., Jeemon P., Joshi T.K., Kant R., Kant S., Kaur T., Koul P.A., Kumar Praveen, Kumar R., Larson S.L., Lodha R., Madhipatla K.K., Mahesh P.A., Malhotra R., Managi S., Martin K., Mathai M., Mathew J.L., Mehrotra R., Mohan B.V.M., Mohan V., Mukhopadhyay S., Mutreja P., Naik N., Nair S., Pandian J.D., Pant P., Perianayagam A., Prabhakaran D., Prabhakaran P., Rath G.K., Ravi S., Roy A., Sabde Y.D., Salvi S., Sambandam S., Sharma B., Sharma M., Sharma S., Sharma R.S., Shrivastava A., Singh S., Singh V., Smith R., Stanaway J.D., Taghian G., Tandon N., Thakur J.S., Thomas N.J., Toteja G.S., Varghese C.M., Venkataraman C., Venugopal K.N., Walker K.D., Watson A.Y., Wozniak S., Xavier D., Yadama G.N., Yadav G., Shukla D.K., Bekedam H.J., Reddy K.S., Guleria R., Vos T., Lim S.S., Dandona R., Kumar S., Kumar Pushpam, Landrigan P.J., Dandona L. Health and economic impact of air pollution in the states of India: the Global Burden of Disease Study 2019. Lancet Planet. Health. 2021;5:e25–e38. doi: 10.1016/S2542-5196(20)30298-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patankar A.M., Trivedi P.L. Monetary burden of health impacts of air pollution in Mumbai, India: implications for public health policy. Publ. Health. 2011;125:157–164. doi: 10.1016/j.puhe.2010.11.009. [DOI] [PubMed] [Google Scholar]
- Peng L., Zhao X., Tao Y., Mi S., Huang J., Zhang Q. The effects of air pollution and meteorological factors on measles cases in Lanzhou, China. Environ. Sci. Pollut. Res. Int. 2020;27:13524–13533. doi: 10.1007/s11356-020-07903-4. [DOI] [PubMed] [Google Scholar]
- Price R.H.M., Graham C., Ramalingam S. Association between viral seasonality and meteorological factors. Sci. Rep. 2019;9:929. doi: 10.1038/s41598-018-37481-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quadri S.A. COVID-19 and religious congregations: implications for spread of novel pathogens. Int. J. Infect. Dis. 2020;96:219–221. doi: 10.1016/j.ijid.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman M., Islam M., Shimanto M.H., Ferdous J., Rahman A.A.-N.S., Sagor P.S., Chowdhury T. A global analysis on the effect of temperature, socio-economic and environmental factors on the spread and mortality rate of the COVID-19 pandemic. Environ. Dev. Sustain. 2020:1–15. doi: 10.1007/s10668-020-01028-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajak R., Mahto R.K., Prasad J., Chattopadhyay A. Assessment of bio-medical waste before and during the emergency of novel Coronavirus disease pandemic in India: a gap analysis. Waste Manag. Res. 2022;40:470–481. doi: 10.1177/0734242X211021473. [DOI] [PubMed] [Google Scholar]
- Rajan S.I., Saxena P. Springer; 2019. India's Low-Skilled Migration to the Middle East. [Google Scholar]
- Ramasamy D.K., Sundararajan J. Social Science Research Network; Rochester, NY: 2020. COVID-19 Outbreak at Mumbai City: Disaster Management Analysis (SSRN Scholarly Paper No. ID 3648272) [Google Scholar]
- Ranjan A.K., Patra A.K., Gorai A.K. Effect of lockdown due to SARS COVID-19 on aerosol optical depth (AOD) over urban and mining regions in India. Sci. Total Environ. 2020;745 doi: 10.1016/j.scitotenv.2020.141024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reno A.L., Brooks E.G., Ameredes B.T. Mechanisms of heightened airway sensitivity and responses to inhaled SO2 in asthmatics. Environ. Health Insights. 2015;9:13–25. doi: 10.4137/EHI.S15671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ropkins K., Tate J.E. Early observations on the impact of the COVID-19 lockdown on air quality trends across the UK. Sci. Total Environ. 2021;754 doi: 10.1016/j.scitotenv.2020.142374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sagripanti J.-L., Lytle C.D. Estimated inactivation of coronaviruses by solar radiation with special reference to COVID-19. Photochem. Photobiol. 2020;96:731–737. doi: 10.1111/php.13293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sajadi M.M., Habibzadeh P., Vintzileos A., Shokouhi S., Miralles-Wilhelm F., Amoroso A. Temperature, humidity, and latitude analysis to estimate potential spread and seasonality of coronavirus disease 2019 (COVID-19) JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.11834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salvatore M., Bhattacharyya R., Purkayastha S., Zimmermann L., Ray D., Hazra A., Kleinsasser M., Mellan T., Whittaker C., Flaxman S., Bhatt S., Mishra S., Mukherjee B. Resurgence of SARS-CoV-2 in India: Potential Role of the B.1.617.2 (Delta) Variant and Delayed Interventions (Preprint) 2021. Infectious Diseases (Except HIV/AIDS) [DOI] [Google Scholar]
- Santana J.C.C., Miranda A.C., Yamamura C.L.K., Silva Filho S.C. da, Tambourgi E.B., Lee Ho L., Berssaneti F.T. Effects of air pollution on human health and costs: current situation in são paulo, Brazil. Sustainability. 2020;12:4875. doi: 10.3390/su12124875. [DOI] [Google Scholar]
- Sarkar S. Breaking the chain: governmental frugal innovation in Kerala to combat the COVID-19 pandemic. Govern. Inf. Q. 2021;38 doi: 10.1016/j.giq.2020.101549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schraufnagel D.E., Balmes J.R., Cowl C.T., De Matteis S., Jung S.-H., Mortimer K., Perez-Padilla R., Rice M.B., Riojas-Rodriguez H., Sood A., Thurston G.D., To T., Vanker A., Wuebbles D.J. Air pollution and noncommunicable diseases: a review by the forum of international respiratory societies' environmental committee, Part 2: air pollution and organ systems. Chest. 2019;155:417–426. doi: 10.1016/j.chest.2018.10.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semczuk-Kaczmarek K., Rys-Czaporowska A., Sierdzinski J., Kaczmarek L.D., Szymanski F.M., Platek A.E. Association between air pollution and COVID-19 mortality and morbidity. Intern Emerg Med. 2021 doi: 10.1007/s11739-021-02834-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Setti L., Passarini F., Gennaro G.D., Barbieri P., Perrone M.G., Piazzalunga A., Borelli M., Palmisani J., Gilio A.D., Piscitelli P., Miani A. 2020. The Potential Role of Particulate Matter in the Spreading of COVID-19 in Northern Italy: First Evidence-Based Research Hypotheses. [DOI] [Google Scholar]
- Sharma S., Zhang M., Gao J., Zhang H., Kota S.H. Effect of restricted emissions during COVID-19 on air quality in India. Science of the total environment. 2020;728:138878. doi: 10.1016/j.scitotenv.2020.138878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shehzad K., Sarfraz M., Shah S.G.M. The impact of COVID-19 as a necessary evil on air pollution in India during the lockdown. Environ. Pollut. 2020;266 doi: 10.1016/j.envpol.2020.115080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiehzadegan S., Alaghemand N., Fox M., Venketaraman V. Analysis of the delta variant B.1.617.2 COVID-19. Clin. Pract. 2021;11:778–784. doi: 10.3390/clinpract11040093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song J., Pan R., Yi W., Wei Q., Qin W., Song S., Tang C., He Y., Liu X., Cheng J., Su H. Ambient high temperature exposure and global disease burden during 1990–2019: an analysis of the Global Burden of Disease Study 2019. Sci. Total Environ. 2021;787 doi: 10.1016/j.scitotenv.2021.147540. [DOI] [PubMed] [Google Scholar]
- Srivastava S., Kumar A., Bauddh K., Gautam A.S., Kumar S. 21-Day lockdown in India dramatically reduced air pollution indices in Lucknow and New Delhi, India. Bull. Environ. Contam. Toxicol. 2020;105:9–17. doi: 10.1007/s00128-020-02895-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang L., Liu M., Ren B., Wu Z., Yu X., Peng C., Tian J. Sunlight ultraviolet radiation dose is negatively correlated with the percent positive of SARS-CoV-2 and four other common human coronaviruses in the U.S. Sci. Total Environ. 2021;751 doi: 10.1016/j.scitotenv.2020.141816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veefkind P., Aben I., Dehn A., Kleipool Q., Loyola D., Richter A., van Roozendael M., Siddans R., Wagner T., Zehner C., Level P. 2020. Sentinel 5 Precursor: Status of TROPOMI and the Operational Data Products 6895. [DOI] [Google Scholar]
- Vulichi S.R., Kabra A., Khalid M., Kumar R., Cruz-Martins N. Interlink between pollution and COVID-19 in India: compelling view and key attributes. Environ. Sci. Pollut. Res. Int. 2021;28:19539–19542. doi: 10.1007/s11356-021-13451-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walls A.C., Park Y.-J., Tortorici M.A., Wall A., McGuire A.T., Veesler D. Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell. 2020;181:281–292. doi: 10.1016/j.cell.2020.02.058. e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Tang K., Feng K., Li X., Lv W., Chen K., Wang F. Impact of temperature and relative humidity on the transmission of COVID-19: a modeling study in China and the United States. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2020-043863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weaver A.K., Head J.R., Gould C.F., Carlton E.J., Remais J.V. Environmental factors influencing COVID-19 incidence and severity. Annu. Rev. Publ. Health. 2022;43:271–291. doi: 10.1146/annurev-publhealth-052120-101420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wendling Z.A., Emerson J.W., de Sherbinin A., Esty D.C., Hoving K., Ospina C.D.…Schreck M. Environmental performance index. Yale Center for Environmental Law And Policy. epi. yale. edu; New Haven, CT: 2020. [Google Scholar]
- WHO . 2020. WHO Coronavirus Disease (COVID-19) Dashboard. [Google Scholar]
- WHO . 2020. Estimating Mortality from COVID-19. [Google Scholar]
- WHO . 2022. Ambient (Outdoor) Air Pollution. [Google Scholar]
- World Health Organization . World Health Organization; 2000. Occupational and Environmental Health Team. Guidelines for air quality (No. WHO/SDE/OEH/00.02) [Google Scholar]
- WorldPop . 2021. Global 1km Population Total Adjusted to Match the Corresponding UNPD Estimate. ([Data set]) [Google Scholar]
- Wu X., Nethery R.C., Sabath B.M., Braun D., Dominici F. medRxiv. 2020. Exposure to Air Pollution and COVID-19 Mortality in the United States: A Nationwide Cross-Sectional Study. 2020.04.05.20054502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xing Y.-F., Xu Y.-H., Shi M.-H., Lian Y.-X. The impact of PM2.5 on the human respiratory system. J. Thorac. Dis. 2016;8:E69–E74. doi: 10.3978/j.issn.2072-1439.2016.01.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu X. Recent advances in studies of ozone pollution and impacts in China: a short review. Current Opinion in Environmental Science & Health. 2021;19 doi: 10.1016/j.coesh.2020.100225. [DOI] [Google Scholar]
- Zangari S., Hill D.T., Charette A.T., Mirowsky J.E. Air quality changes in New York City during the COVID-19 pandemic. Sci. Total Environ. 2020;742 doi: 10.1016/j.scitotenv.2020.140496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y., Xie J., Huang F., Cao L. Association between short-term exposure to air pollution and COVID-19 infection: evidence from China. Sci. Total Environ. 2020;727 doi: 10.1016/j.scitotenv.2020.138704. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.