Abstract
Introduction
The profunda artery perforator (PAP) flap represents a valuable alternative to the deep inferior epigastric artery perforator flap which, nowadays, is considered the golden standard for autologous breast reconstruction. The goal of this study was to evaluate the long-term satisfaction, functional outcomes of the donor site following PAP flap-based breast reconstruction and to present our personal learning experience along with suggestions for technique refinements.
Methods
In this prospective single-center appraisal, 18 patients who underwent PAP flap-based breast reconstruction between January 2016 and November 2019 were enrolled. The Patient and Observer Scar Assessment Scale (POSAS) and the Breast-Q questionnaire were employed to evaluate the results 12 months postoperative. Data were analyzed with the Q-Score program. Complications were recorded in the medical database and classified with the Clavien-Dindo classification.
Results
In the questionable time frame, 164 female patients underwent free flap breast reconstruction. Of those, 18 patients that received PAP flaps (9 bilateral) were included in this study. We recorded one flap loss because of venous failure. Most complications concerned the donor site, including hematoma, seroma, and wound healing problems. Patients' satisfaction was high at 12 months post-surgery, despite critical evaluation of the donor site scar.
Conclusion
The PAP flap serves as an excellent option for breast reconstruction in patients who do not have abundant abdominal tissue. The overall clinical outcome was good and patients' evaluation showed high satisfaction after 12 months despite high complication rates. Modifications in planning and flap harvesting might improve the donor site outcome and the overall complication rate.
Keywords: Breast, Breast cancer, Breast reconstruction, Breast-Q, Free flap, Flap surgery, Long-term outcome, PAP flap, POSAS, Profunda artery perforator flap, Vertical PAP flap
Introduction
The major goals in autologous breast reconstruction include symmetry, sufficient volume, anatomical shape, and a skin paddle matching the locoregional skin if necessary. All these criteria are easily obtained with the use of the deep inferior epigastric artery perforator (DIEP) flap in most patients. If the DIEP is not an option, such as in very lean patients or after extended abdominal surgery [1], the profunda artery perforator (PAP) flap from the thigh [2], first described by Allen et al. [3], can be considered as a secondary option. While the skin paddle is limited, this flap profits from an inconspicuous donor site and the availability of a long vascular pedicle [2]. Also, the average diameter of the vessels, in general, one artery and two veins, are an ideal match for anastomosis with the internal mammary artery. Technical considerations as well as the versatility of this flap have been extensively described in literature [4, 5]. Many refinements have been made concerning the harvesting technique [6, 7] and surgeons try to minimize donor site complications [8] by analyzing the postoperative results and complications [9]. Despite all efforts, detailed information about long-term outcomes, donor site morbidity after a postoperative period greater than 12 months, and overall patient satisfaction are still limited compared to other flaps used for breast reconstruction [10, 11].
In this work, we present our experience and the long-term results of 18 consecutive breast reconstructions with PAP flaps. Herein, we are applying the validated Breast-Q questionnaire [12] along with questions concerning the thigh donor site outcome by Stocco et al. [13] adapted by our group (Table 1). Moreover, the Patient and Observer Scar Assessment Scale (POSAS) [14] was used to evaluate the donor site scar quality. Along with the results, we share the pearls and pitfalls that we learned from our series. We suggest novel refinements for the harvesting technique in order to ease access to the dominant perforators without putting the donor site healing process at risk.
Table 1.
Adapted questions for the postoperative Breast-Q-questionnaire regarding PAP flap-based breast reconstruction
| The following questions are about the satisfaction with your thighs. In the past week, thinking of your thighs, how satisfied have you been with: | Dissatisfied | Somewhat dissatisfied | Somewhat satisfied | Very satisfied |
|---|---|---|---|---|
| How do your thighs look when unclothed? | 1 | 2 | 3 | 4 |
| The position of your gluteal crease (buttocks crease)? | 1 | 2 | 3 | 4 |
| How the thigh scars look? | 1 | 2 | 3 | 4 |
Materials and Methods
This prospective single-center appraisal was approved by the local Ethics Committee (EK Nr: 1058/2021). All patients provided informed consent for standardized photo documentation (Fig. 1), the operative procedure, and assessment of their data. Data were anonymized for analysis. Inclusion criteria were unilateral or bilateral PAP flap-based breast reconstruction due to breast cancer diagnosis, BRCA gene carrier status, recurrent mastitis, or after the failure of implant-based reconstruction, female gender, and age over 18 years. Furthermore, a postoperative follow-up of more than 12 months at the time of inclusion was required. Exclusion criteria were metastatic disease, Poland's syndrome, age younger than 18 years, psychiatric disorders, autologous reconstruction for massive breast asymmetry, and postoperative follow-up less than 12 months. PAP flaps are offered in our clinic as a first-line second choice for patients with low BMI (<25 kg/m2) or prior abdominal surgery resulting in a contraindication for a DIEP flap.
Fig. 1.
Preoperative (a, b) and postoperative (c, d) pictures of a 29-year-old patient requiring bilateral skin sparing mastectomy. Subsequent autologous breast reconstruction was done with profundal artery perforator flaps. The resected areolae were reconstructed using the flap skin paddles and NAC reconstruction was completed after 6 months with local C-V-flaps.
Patient Data
Between January 2016 and December 2019, 164 female patients underwent autologous breast reconstruction in at our dDepartment. Of those, only the patients that received PAP flaps were considered. Of the 29 patients eligible, 6 patients had to be excluded due to the exclusion criteria (psychiatric disorder n = 2, metastatic disease n = 4); 5 patients dropped out during the study course because of completed postoperative follow-up less than 12 months (declined further participance n = 2, moved out of catchment area of the clinic n = 3); and 18 patients completed the follow-up (62.1%).
Complications were recorded in the medical database and classified according to the Clavien-Dindo classification [15]. However, Clavien-Dindo class 1 includes every deviation from the standard postoperative course such as the administration of antiemetics, analgetics, or physiotherapy. In patients after free flap surgery, such applications do not necessarily indicate a complication but are rather mandatory in standard postoperative care. Thus, we considered the patients meeting the criteria for Clavien-Dindo class 1 as complication free. The distance of the dominant profundal artery perforator from the tuber ischiadicum was measured in a routinely performed computed tomography angiography beforehand as well as intraoperatively after choosing the most reliable perforators.
Questionnaires
The study follow-up included two validated questionnaires. The POSAS (German version) [14] was completed by patients and three independent surgeons who evaluated the scar, whereas the Breast-Q [12] was completed by all patients 12 months postoperatively, including a modification regarding the donor site, namely questions regarding the thigh as suggested by Stocco et al. [13]. Ratings were converted by the raw scale summed score into a score from 0 (worst) to 100 (best), herein higher scores reflect a better outcome. Outcomes were interpreted using normative data [16].
Results
Patients and Characteristics
Between January 2016 and December 2019, 29 patients underwent autologous breast reconstruction with PAP flaps in at our dDepartment. After applying the exclusion criteria, 18 patients were included in the long-term survey. Of those, 50% (n = 9) had bilateral reconstruction (as seen in Fig. 1) and the rest 50% had unilateral reconstruction (Fig. 2). Mean patients' age was 43.6 years (range 29–59 years) at the time of flap surgery. One patient was an active smoker. Mean patients' BMI was 21.6 kg/m2 (range 17.9–27.5 kg/m2). Most patients were very lean, only 1 patient had a BMI higher than 25. Indications for reconstruction were breast cancer (n = 17), recurrent infects (n = 1), and prophylactic mastectomies (n = 9). Most of the reconstructions were performed immediately (n = 23), in 4 cases the reconstruction was delayed in a second procedure. Detailed patients' characteristics are listed in Table 2.
Fig. 2.
Preoperative (a, b) and postoperative (c, d) pictures of a 51-year-old patient requiring unilateral autologous breast reconstruction of the right breast with profundal artery perforator flap after nipple-sparing mastectomy due to recurrent mastitis. The donor site is found in the left thigh. Vertical breast reduction following Lejour's technique was performed on the left side.
Table 2.
Patient characteristics
| N (%) | |
|---|---|
| Patients, n (%) | 18 (100) |
| Primary reconstruction, n (%) | 23 (85.2) |
| Secondary reconstruction, n (%) | 4 (14.8) |
| Unilateral reconstruction, n (%) | 9 (50) |
| Bilateral reconstruction, n (%) | 9 (50) |
| Flaps | 27 |
| Flap weight, g | |
| Median | 300 |
| Range | 170–550 |
| Mean ± SD | 327.7±108.2 |
| Age, years | |
| Median | 44.5 |
| Range | 29–59 |
| Mean±SD | 43.6±7.4 |
| Age group, n (%) | |
| <18 years | 0 |
| 18–24 years | 0 |
| 25–34 years | 3 (16.7) |
| 35–44 years | 6 (33.3) |
| 45–54 years | 8 (44.4) |
| 55–64 years | 1 (5.6) |
| >65 years | 0 |
| BMI, kg/m2 | |
| Median | 21.6 |
| Range | 17.9–27.5 |
| Mean ± SD | 21.6±2.3 |
| Smoking status, n (%) | |
| Nonsmoker | 16 (88.9) |
| Active smoker | 1 (5.6) |
| Quit | 1 (5.6) |
| Oncologic therapy, n (%) | |
| Neoadjuvant chemotherapy | 5 (27.8) |
| Adjuvant chemotherapy | 4 (22.2) |
| Adjuvant radiation therapy | 7 (38.9) |
Surgery and Complications
In total, 18 patients received 27 PAP flaps. The mean flap weight was 327.7 g (range 170–550 g). Postoperative complications were documented in 10 patients (for detail see Table 3). Interestingly, patients with bilateral flaps were affected more often from a complicated course (6 patients) than patients with unilateral reconstruction (4 patients). Using the Clavien-Dindo classification [15], we identified 1 case with a type 2 complication (seroma at the recipient site conveniently accessible for puncture). Clavien-Dindo class 3A was assigned to 1 patient (small wound healing problem). Nine patients, 5 of them with bilateral flaps, with type 3B complications had to be taken back to the theatre for surgery in general anesthesia. However, there was only one single flap loss because of venous failure in a patient after bilateral reconstruction. The other cases of revision surgery were donor site complications concerning the thigh area, where we had a total of 9 complications in 8 patients. Of those patients, 7 had to be taken back to the theatre in general anesthesia. Herein, the vast majority were wound healing complications, however, the scars in the upper thigh most often profit from a favorable outcome as they are well concealed by the natural crease (Fig. 3). Of course, the burden of prolonged wound management remains problematic for the patient. In the later course, three-of-our patients had autologous fat grafting to enhance the breast volume (all three were bilateral cases). Only 1 patient desired scar correction of the donor site.
Table 3.
Complications
| Complications | N (%) |
|---|---|
| Flap loss | 1 (5.6) |
|
| |
| Breast | |
| Delayed wound healing (<4 weeks) | 0 |
| Surgical-site infection | 1 (5.6) |
| Unsatisfactory scar | 0 |
| Hematoma | 3 (16.7) |
| Seroma | 3 (16.7) |
| Necrosis of skin envelope | 1 (5.6) |
|
| |
| Donor site | |
| Delayed wound healing (<4 weeks) | 5 (27.8) |
| Surgical-site infection | 2 (11.1) |
| Unsatisfactory scar | 1 (5.6) |
| Hematoma | 3 (16.7) |
| Seroma | 1 (5.5) |
| Movement impairment | 0 |
|
| |
| Clavien-Dindo, breast | |
| Class 2 | 1 (5.6) |
| Class 3a | 0 |
| Class 3b | 5 (27.8) |
| Class 4 | 0 |
| Class 5 | 0 |
|
| |
| Clavien-Dindo, thigh | |
| Class 2 | 0 |
| Class 3a | 1 (5.6) |
| Class 3b | 7 (38.9) |
| Class 4 | 0 |
| Class 5 | 0 |
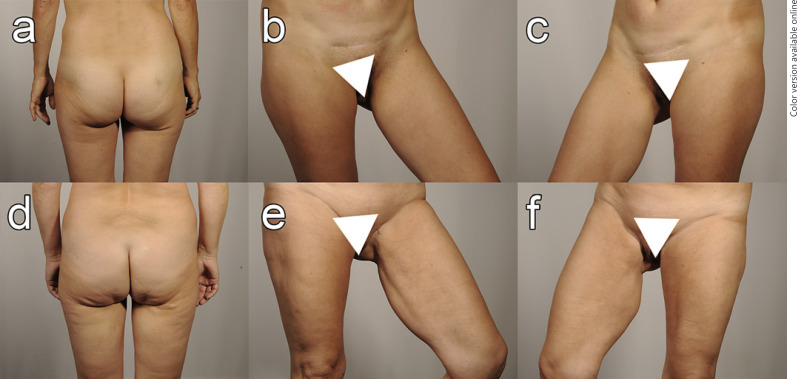
Fig. 3.
The postoperative photographs show a patient after unilateral reconstruction with a primary healed donor site in the right thigh (a–c) and a patient after bilateral PAP flap-based breast reconstruction (d–f) that encountered donor site wound healing disturbance in both thighs. The complications were managed conservatively and resulted in well-concealed scars without a requirement for correction.
Perforator Vessels
The mean number of PAPs identified in the preoperative CT angiographic scans were mean 2.5 (range 1–3) perforators on the right tight and 2.6 (range 1–4) perforators on the left side. However, intraoperatively only the most reliable perforators were chosen and thus, this number decreased. The number of intraoperatively chosen vessels was mean 1.75 (range 1–3) on the right and mean 1.72 (range 1–2) on the left side. The distance from the tuber ischiadicum to the chosen perforator vessel was mean 9.6 ± 3.2 cm on the right side while it was measured mean 9.5 ± 1.9 cm on the left thigh.
Breast-Q Questionnaire
All included patients completed the Breast-Q questionnaire postoperatively, in bilateral cases for each reconstructed breast, rating the results from 0 (worst outcome) to 100 (best outcome). Results are listed in detail in Table 4. Regarding psychosocial well-being, the mean Q-Score in this category was 73.4 (range 45–93). Sexual well-being showed a mean Q-Score of 62, while patients' satisfaction with the breast appearance was 63.8 (range 38–100). The Q-Score regarding the physical well-being of the chest was 82.5 (range 50–100), while the physical well-being regarding the donor site thigh was 77.7 (range 47–100). Concerning the question about a swelling or lymphedema on the ipsilateral site of the mastectomy, 16 patients answered that they never had a swollen arm. However, 1 patient answered that she sometimes had swollen arms, while one other patient suffered from lymphedema of the arm all the time. In the last category, there were three questions based on the details of the donor site, namely general appearance of the unvested thigh, position of gluteal fold, and scar appearance. Answers were ranked from 1 − very unsatisfied to 4 − very satisfied. Answering the question of how the thigh looks unvested, the mean answer value was 2.9 (range 1–4). Regarding the position of the gluteal fold the mean value was 3.2 (range 1–4). Patients' satisfaction with the scar on their thigh was mean 2.8 (range 1–4).
Table 4.
Postoperative Breast-Q items and results
| Breast-Q | Median | Range | Mean ± SD |
|---|---|---|---|
| Psychosocial well-being | 74 | 45–93 | 73.4±12.2 |
| Sexual well-being | 62 | 41–91 | 62.0±11.7 |
| Satisfaction with breast | 59 | 38–100 | 63.8±17.7 |
| Well-being breast | 85 | 64–100 | 82.5±13.8 |
| Swelling ipsilateral arm | 1 | 1–3 | 1.2±0.6 |
| Well-being donor site thighs | 72 | 47–100 | 77.7±16.8 |
| Appearance of thighs | 3 | 1–4 | 2.9±0.9 |
| Position of gluteal fold | 3 | 1–4 | 3.2±0.7 |
| Scar thigh | 3 | 1–4 | 2.8±1.0 |
POSAS Questionnaire
As part of our survey, we evaluated satisfaction with the donor site scar using the standardized POSAS questionnaire. This included 7 questions for each patient and observer rated from 1 (normal skin) to 10 (worst scar imaginable). The average total score for overall patient satisfaction with the scar was mean 4.7 points whereas the observers scored 3.2 points for this question. All detailed results are listed in Table 5.
Table 5.
POSAS questionnaire and results
| Median | Mean ± SD | |
|---|---|---|
| POSAS, patient | ||
| Has the scar been painful in the past few weeks? | 1 | 1.9±1.9 |
| Has the scar been itching in the past few weeks? | 1 | 1.3±0.8 |
| Is the scar color different from the color of your normal skin at present? | 5 | 4.5±2.4 |
| Is the stiffness of the scar different from your normal skin at present? | 4 | 4.5±2.6 |
| Is the thickness of the scar different from your normal skin at present? | 4 | 4.2±2.4 |
| Is the scar more irregular than your normal skin at present? | 4 | 4.4±2.7 |
| What is your overall opinion of the scar compared to normal skin? | 5 | 4.7±2.4 |
|
| ||
| POSAS, observer | ||
| Vascularity | 2 | 2.4±1.1 |
| Pigmentation | 4 | 3.8±1.7 |
| Thickness | 3 | 3.1±1.1 |
| Relief | 3 | 3.4±1.4 |
| Pliability | 2 | 2.4±0.8 |
| Surface area | 3 | 3.1±1.4 |
| Overall opinion | 3 | 3.2±1.3 |
Discussion
The PAP flap represents a valuable alternative to the DIEP flap which nowadays is considered the golden standard for autologous breast reconstruction [2]. It clearly profits from a long pedicle, reliability of the blood supply and also a favorable − because easy to hide − donor site scar [2]. Possible drawbacks are limited flap volume and potential sagging of the scar. The primary goal of this work was to evaluate the long-term satisfaction and functional outcomes of the donor site following PAP flap-based breast reconstruction and to present our personal learning experience, pearls, and pitfalls.
The long-term outcome has been reviewed in literature [9, 17]; however, the standardized and validated instrument for the evaluation of breast reconstruction, namely the Breast-Q questionnaire [12], is not of routine use for PAP flap-based breast reconstruction so far [9]. As suggested by other groups [13], some questions have been adapted to assess the donor site on the upper thigh (see Tables 1, 4) and we asked the patients to evaluate their outcome 12 months postoperatively. Using the previously published normative scores to aid interpretation [16], the patients in our study scored favorable results in comparison to normative data within all relevant Breast-Q items. However, one data point in our patient series was lower than normative data, namely the item “physical well-being of the breast” (Table 4). As for asymmetry of the donor site, either patients with bilateral (Fig. 1) and patients with unilateral reconstruction (Fig. 2) rated the overall appearance of the thighs in the postoperative setting with mean 3 points “somewhat satisfied” (range 2.9 ± 0.9) as mentioned in Table 4 which compares to the results of unilateral TUG flap reconstruction found in literature [10]. In our opinion, the overall results strongly support the use of the PAP flap-based autologous breast reconstruction, despite higher complication rates.
In the POSAS questionnaire (Table 5), patients were satisfied but rated the scar overall less favorable than the observers, indicating the impact of the professional view as a quite important factor. To overcome this, most careful and profound information beforehand the procedure, including example pictures and photographs (as seen in Fig. 1), is used in our clinic as a helpful tool to create realistic expectations in patients.
Complication rates in bilateral reconstruction were higher than in unilateral cases in our cohort. Unfortunately, there is a paucity on high-quality studies on the outcome of the PAP flap for breast reconstruction so far. It is known from a large meta-analysis that bilateral autologous breast reconstruction yields a higher risk for flap loss than unilateral procedures [10], but interestingly a recent meta-analysis on bilateral DIEP-based breast reconstruction found that the unilateral reconstruction yields an overall higher complication risk for flap complications than cases, including both sides [18]. This fact goes against our findings; however, the authors did also find a higher complication rate concerning the donor site in bilateral cases, which is corresponding to our data [18]. Factors that will have an impact here are not only longer operative time, but also the bigger wound area and higher blood loss, aside from patient factors that have to be considered as well [19]. While being a reliable flap, the complication rate of the PAP flap donor site is high compared to the other flaps of choice [20, 21], this is also mirrored by our data. The most common complications in our series were seroma, wound dehiscence of the thigh, and hematoma. In our opinion, this can be explained at least in parts by the characteristics of the harvesting technique. The PAP perforator vessels are located quite distal in the upper thigh, frequently posterior and distal to the gracilis pedicle, as mirrored by our data. The perforators of choice were found frequently more than 9-cm distal to the tuber ischiadicum in our patient group. Thus, a large area of undermined skin is created by placing the scar in the thigh crease, favoring the mentioned complications. In order to gain more volume, alterations of flap geometry have been suggested [22], alternatively extended [23], or even stacked and chimeric [24, 25] flaps could be used. However, the easiest and most straightforward method to gain flap volume seems to be harvesting a skin paddle as wide as possible and to include adjacent fat tissue, thus, even thinning the undermined soft tissues in the donor region. This strategy seems to be successful in terms of flap weight when comparing our data to the literature [9] but on the other hand, it is suspected to add to the considerable amount of wound healing problems. This is especially true in our patient group, as the most patients had a BMI lower than 22, which is lower than in the most comparable studies published in literature [9, 22]. In our opinion, this problem could be overcome by using a vertical skin paddle similar to the vertical inner thigh plasty. Herein, the distal, usually stronger perforators are accessible easily and safely [21]. This technique is similar to the extended PAP flap proposed in literature for the reconstruction of a larger breast; however, in order to further minimize complications we propose a strict vertical design in contrast to the fleur-de-lys design which still yields a complications rate higher than 20% [21].
Conclusion
The PAP flap is considered a valuable alternative to the DIEP flap in microsurgical breast reconstruction in lean patients and patients are satisfied with the long-term outcome after 12 months. As the advantages of the donor site might be outweighed by the complication rate, careful technique, and modifications in harvesting will add to the donor site outcome and morbidity.
Statement of Ethics
This prospective single-center appraisal was reviewed and approved by the Ethics Committee of Innsbruck (approval number EK Nr: 1058/2021). All patients provided written informed consent for photo documentation, the operative procedure, and assessment of their data. The authors declare that the ethical guidelines of the 1975 Declaration of Helsinki as amended in 2013 were followed at all times when conducting this work. All patients gave their oral and written informed consent for the study, the surgical procedure, photo documentation of preoperative, intraoperative and postoperative findings, and the use of their data and photographs in scientific publications.
Conflict of Interest Statement
The authors have no conflict of interest to declare.
Funding Sources
No funding was received for this work.
Author Contributions
All authors were involved in planning and execution of the study, as well as manuscript and figure preparation. E.M.M. and S.W. wrote the manuscript. E.M.M. and S.W. prepared the figures in equal parts. A.A. and P.P. performed data acquisition, T.B. and D.E. interpreted the data and corrected the manuscript, D.W. designed and supervised the study, and moreover critically reviewed the manuscript.
Data Availability Statement
All data generated or analyzed during this study are included in this article. Further inquiries can be directed to the corresponding author.
Acknowledgment
The authors wish to thank Dr. M. Ritter who was involved in the treatment of the patients.
Funding Statement
No funding was received for this work.
References
- 1.Granzow JW, Levine JL, Chiu ES, Allen RJ. Breast reconstruction using perforator flaps. J Surg Oncol. 2006;94((6)):441–454. doi: 10.1002/jso.20481. [DOI] [PubMed] [Google Scholar]
- 2.Allen RJ, Haddock NT, Ahn CY, Sadeghi A. Breast reconstruction with the profunda artery perforator flap. Plast Reconstr Surg. 2012;129((1)):16e–23e. doi: 10.1097/PRS.0b013e3182363d9f. [DOI] [PubMed] [Google Scholar]
- 3.Haddock NT, Greaney P, Otterburn D, Levine S, Allen RJ. Predicting perforator location on preoperative imaging for the profunda artery perforator flap. Microsurgery. 2012;32((7)):507–511. doi: 10.1002/micr.21980. [DOI] [PubMed] [Google Scholar]
- 4.Haddock NT, Cho MJ, Teotia SS. Comparative analysis of single versus stacked free flap breast reconstruction: a single-center experience. Plast Reconstr Surg. 2019;144((3)):369e–77e. doi: 10.1097/PRS.0000000000005906. [DOI] [PubMed] [Google Scholar]
- 5.Dayan JH, Allen RJ. Jr Neurotized diagonal profunda artery perforator flaps for breast reconstruction. Plast Reconstr Surg Glob Open. 2019;7((10)):e2463. doi: 10.1097/GOX.0000000000002463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iida T, Yoshimatsu H, Karakawa R, Kanayama K, Harima M, Okazaki M. Additional venous anastomosis in free profunda artery perforator flap transfer using the posterior accessory saphenous vein. J Plast Reconstr Aesthet Surg. 2019;72((12)):1936–1941. doi: 10.1016/j.bjps.2019.09.013. [DOI] [PubMed] [Google Scholar]
- 7.Karakawa R, Yoshimatsu H, Tanakura K, Miyashita H, Shibata T, Kuramoto Y, et al. An anatomical study of the lymph-collecting vessels of the medial thigh and clinical applications of lymphatic vessels preserving profunda femoris artery perforator (LpPAP) flap using pre- and intraoperative indocyanine green (ICG) lymphography. J Plast Reconstr Aesthet Surg. 2020;73((9)):1768–1774. doi: 10.1016/j.bjps.2020.03.023. [DOI] [PubMed] [Google Scholar]
- 8.Cho MJ, Teotia SS, Haddock NT. Classification and management of donor-site wound complications in the profunda artery perforator flap for breast reconstruction. J Reconstr Microsurg. 2020;36((2)):110–115. doi: 10.1055/s-0039-1697903. [DOI] [PubMed] [Google Scholar]
- 9.Haddock NT, Teotia SS. Consecutive 265 profunda artery perforator flaps: refinements, satisfaction, and functional outcomes. Plast Reconstr Surg Glob Open. 2020;8((4)):e2682. doi: 10.1097/GOX.0000000000002682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pulzl P, Schoeller T, Kleewein K, Wechselberger G. Donor-site morbidity of the transverse musculocutaneous gracilis flap in autologous breast reconstruction: short-term and long-term results. Plast Reconstr Surg. 2011;128((4)):233e–42e. doi: 10.1097/PRS.0b013e3182268a99. [DOI] [PubMed] [Google Scholar]
- 11.Hunsinger V, Hivelin M, Derder M, Klein D, Velten M, Lantieri L. Long-term follow-up of quality of life following DIEP flap breast reconstruction. Plast Reconstr Surg. 2016;137((5)):1361–1371. doi: 10.1097/PRS.0000000000002047. [DOI] [PubMed] [Google Scholar]
- 12.Pusic AL, Klassen AF, Scott AM, Klok JA, Cordeiro PG, Cano SJ. Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg. 2009;124((2)):345–353. doi: 10.1097/PRS.0b013e3181aee807. [DOI] [PubMed] [Google Scholar]
- 13.Stocco C, Figus A, Razzano S. Upgrading the BREAST-Q questionnaire with donor site evaluation after PAP flap breast reconstruction. J Plast Reconstr Aesthet Surg. 2018;71((6)):928–929. doi: 10.1016/j.bjps.2018.01.025. [DOI] [PubMed] [Google Scholar]
- 14.Truong PT, Lee JC, Soer B, Gaul CA, Olivotto IA. Reliability and validity testing of the Patient and Observer Scar Assessment Scale in evaluating linear scars after breast cancer surgery. Plast Reconstr Surg. 2007;119((2)):487–494. doi: 10.1097/01.prs.0000252949.77525.bc. [DOI] [PubMed] [Google Scholar]
- 15.Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250((2)):187–196. doi: 10.1097/SLA.0b013e3181b13ca2. [DOI] [PubMed] [Google Scholar]
- 16.Mundy LR, Homa K, Klassen AF, Pusic AL, Kerrigan CL. Breast cancer and reconstruction: normative data for interpreting the BREAST-Q. Plast Reconstr Surg. 2017;139((5)):1046e–55e. doi: 10.1097/PRS.0000000000003241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Murphy DC, Figus A, Stocco C, Razzano S. A comparison of patient reported outcome measures in patients who received both DIEP flap and PAP flap breast reconstructions. J Plast Reconstr Aesthet Surg. 2019;72((4)):685–710. doi: 10.1016/j.bjps.2019.01.006. [DOI] [PubMed] [Google Scholar]
- 18.Cao Z, Cao J, Pang X, Du W, Wu P. A comparative study for the rate of adverse outcomes in unilateral and bilateral abdominal flap breast reconstruction: a meta-analysis. Medicine. 2020;99((37)):e22096. doi: 10.1097/MD.0000000000022096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Magno-Pardon DA, Luo J, Carter GC, Agarwal JP, Kwok AC. An analysis of the modified five-item frailty index for predicting complications following free flap breast reconstruction. Plast Reconstr Surg. 2022;149((1)):41–7. doi: 10.1097/PRS.0000000000008634. [DOI] [PubMed] [Google Scholar]
- 20.Fosseprez P, Gerdom A, Servaes M, Deconinck C, Pirson G, Berners A. [Profunda artery perforator flap: reliable secondary option for breast reconstruction?] Ann Chir Plast Esthet. 2017;62((6)):637–645. doi: 10.1016/j.anplas.2017.05.002. [DOI] [PubMed] [Google Scholar]
- 21.Qian B, Xiong L, Li J, Sun Y, Sun J, Guo N, et al. A systematic review and meta-analysis on microsurgical safety and efficacy of profunda artery perforator flap in breast reconstruction. J Oncol. 2019;2019:9506720. doi: 10.1155/2019/9506720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hupkens P, Hameeteman M, Westland PB, Slater NJ, Vasilic D, Ulrich DJ. Breast reconstruction using the geometrically modified profunda artery perforator flap from the posteromedial thigh region: combining the benefits of its predecessors. Ann Plast Surg. 2016;77((4)):438–444. doi: 10.1097/SAP.0000000000000619. [DOI] [PubMed] [Google Scholar]
- 23.Tielemans HJP, van Kuppenveld PIP, Winters H, Hupkens P, Ulrich DJO, Hummelink S. Breast reconstruction with the extended profunda artery perforator flap. J Plast Reconstr Aesthet Surg. 2021;74((2)):300–306. doi: 10.1016/j.bjps.2020.08.109. [DOI] [PubMed] [Google Scholar]
- 24.Jo T, Jeon DN, Han HH. The PAP flap breast reconstruction: a practical option for slim patients. J Reconstr Microsurg. 2022 Jan;38((1)):27–33. doi: 10.1055/s-0041-1727200. [DOI] [PubMed] [Google Scholar]
- 25.Heredero S, Falguera-Uceda MI, Sanjuan-Sanjuan A, Dean A, Solivera J. Chimeric profunda artery perforator − gracilis flap: a computed tomographic angiography study and case report. Microsurgery. 2021;41((3)):250–257. doi: 10.1002/micr.30694. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this article. Further inquiries can be directed to the corresponding author.