Abstract
IMPORTANCE
The ongoing overdose crisis continues to adversely affect adolescents and young adults (AYAs) and has led to numerous preventable deaths. Medications for opioid use disorder (MOUD), such as methadone, buprenorphine, and naltrexone, have the potential to reduce opioid use and associated harms; however, there are concerns that AYAs lack access to these potentially life-saving medications.
OBJECTIVE
To systematically review peer-reviewed literature on MOUD access and associated factors to synthesize strategies that can improve MOUD access for AYAs who use opioids.
EVIDENCE REVIEW
The MEDLINE, Embase, PsycINFO, CINAHL, Sociological Abstracts, Web of Science, and Global Dissertations & Theses databases were searched from database inception until May 3, 2021. English, French, Russian, or Spanish peer-reviewed studies that evaluated the availability, prescription receipt, or initiation of MOUD were eligible for inclusion.
FINDINGS
This systematic review identified 37 cohort (n = 17), cross-sectional (n = 15), and qualitative (n = 5) studies that accounted for 179 785 AYAs (mean [SD] age, 24.4 [3.9] years; 148 779 [85%] were female; 67 771 [84%] were White) and examined access to methadone (30 studies), buprenorphine (26 studies), and naltrexone (10 studies). Findings reinforce concerns that AYAs were less likely to access MOUD and suggest that adolescents were more likely to receive naltrexone or buprenorphine-naloxone, which have a lower potential for abuse, in comparison with young adults. This review also identified other factors that were associated with MOUD access, including criminal justice involvement, residing in the US South, living in a limited-income area, Black race, and Hispanic or Latino ethnicity, suggesting ways in which treatment services may be improved to increase MOUD access and meet the treatment goals of AYAs.
CONCLUSION AND RELEVANCE
This systematic review found gaps in MOUD access between AYAs and non-AYA populations in addition to differences in MOUD access between adolescents and young adults. Considering that existing clinical guidelines recommend the use of MOUD among AYAs, and in light of the increasing number of opioid toxicity deaths, there is a need to improve MOUD access among AYAs by reducing barriers to MOUD and providing AYAs with a continuum of health and social supports alongside MOUD. Future research into ways to encourage MOUD uptake among AYAs may improve the treatment and health outcomes for this population.
In North America, opioid-related overdose is the leading cause of unintentional death.1,2 One tool that has proved to reduce opioid toxicity deaths and has the ability to mitigate the ongoing public health emergency are medications for opioid use disorder (MOUD).3,4 Medications for opioid use disorder include opioid agonist treatments (OATs), such as methadone and buprenorphine, which bind to mu opioid receptors and prevent cravings without precipitating withdrawal symptoms. Also included among MOUD are antagonist treatments such as naltrexone, which have a higher affinity for mu receptors than opioids and prevent the euphoric effects of opioids if taken concurrently.5 Although OATs prevent withdrawal symptoms, opioid antagonists precipitate withdrawal and require abstinence from opioids before induction.5
Existing reviews examining MOUD among adolescents and young adults (AYAs) have shown positive outcomes associated with their use.6,7 Nevertheless, researchers and public health experts have raised concerns about the lack of access to MOUD among AYAs,8,9 emphasizing the need to better understand MOUD access among this population. Given this research gap, the purpose of this systematic review was to summarize existing evidence on MOUD access and associated factors to improve MOUD access for AYAs who may benefit from these treatments.
Methods
This review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline10 (eTable 1 in the Supplement). A comprehensive search strategy was designed and adapted to CINAHL, Embase, Global Dissertations & Theses, MEDLINE, PsycINFO, Sociological Abstracts, and Web of Science from database inception until May 3, 2021. Peer-reviewed studies that evaluated the availability, prescription receipt, and/or initiation of MOUD and were published in either English, French, Russian, or Spanish languages were eligible for inclusion, based on the co-authors’ language capacity. The finalized strategy is included in eTable 2 in the Supplement, and the study protocol is registered in the Open Science Framework (https://osf.io/d7hvb). The population, exposures, comparisons, and outcomes for this review are detailed in the Table. We collected race and ethnicity data to identify differences in MOUD access among AYAs. Those included were Asian (pan-Asian, Chinese), Black, Hispanic, Indigenous (Alaska Native, First Nations, Hawaiian, Inuit, Métis, Native American, Pacific Islander), Latino, White, and Other (multiracial, unknown) and were deduced using public and private databases, electronic health records, and self-reporting. In addition, the screening inclusion and exclusion criteria, race- and ethnicity-based data collection, gray literature search strategy, and quality assessment approach are described in the eMethods in the Supplement, whereas risk of bias scores are presented in eTables 3, 4, and 5 in the Supplement.
Table.
Population, Exposures, Comparisons, Outcomes, and Study Design
| Criteria | Definition |
|---|---|
| Population | Adolescents and young adults with a mean or median sample age between 10 y and 30 y and who report opioid use |
| Exposures | MOUD, including opioid agonist, partial agonist, and antagonist treatments |
| Comparisons | None stipulated but could include placebo, nonexposed, or no interventions |
| Outcomes | Access to MOUD and associated factors; access includes any assessment of the availability, prescription receipt, or initiation of MOUD |
| Study designs | All empirical study designs, excluding case series/studies and reviews |
Abbreviation: MOUD, medications for opioid use disorder.
References retrieved from bibliographic databases were imported to Endnote X9 (Clarivate Analytics) for deduplication and subsequently exported to Covidence software (Veritas Health Innovation). Title and abstract screening were completed by one of us (A.P.), and approximately 20% of all retrieved records were randomly checked by another one of us (D.J.B.). Identified studies proceeded to full-text review and independent assessment for eligibility performed by 2 of us (A.P. and M.K.), followed by a quality assessment of the included studies. All disagreements were resolved through consensus. Because of the heterogeneity among included studies, a narrative approach was used to summarize findings.
Results
Of the 11 278 unique records identified, 37 studies were included in this review and are presented in the PRISMA flowchart (Figure). In summary, studies were conducted between May 1, 1992,11 and April 18, 2021,12 representing 179 785 AYAs (mean [SD] age, 24.4 [3.9] years; 148 779 [85%] were female; 67 771 [84%] were White; the included studies had a mean of 4859 participants, median of 404 participants, and range of 5–82 992 participants) and 3243 adolescent treatment facilities.13–15 Among the 37 studies, 17 were cohort studies, 15 were cross-sectional studies, and 5 were qualitative studies. Twenty-four studies were conducted in the US,13–36 4 in Canada,12,37–39 3 in Australia,11,40,41 2 in England,42,43 2 in Ireland,44,45 and 1 in Italy,46 whereas 1 study derived data from Austria, Canada, and the US.47 Details on study design, setting, sample characteristics, inclusion and exclusion criteria, and study quality are presented in eTable 6 in the Supplement.
Figure.
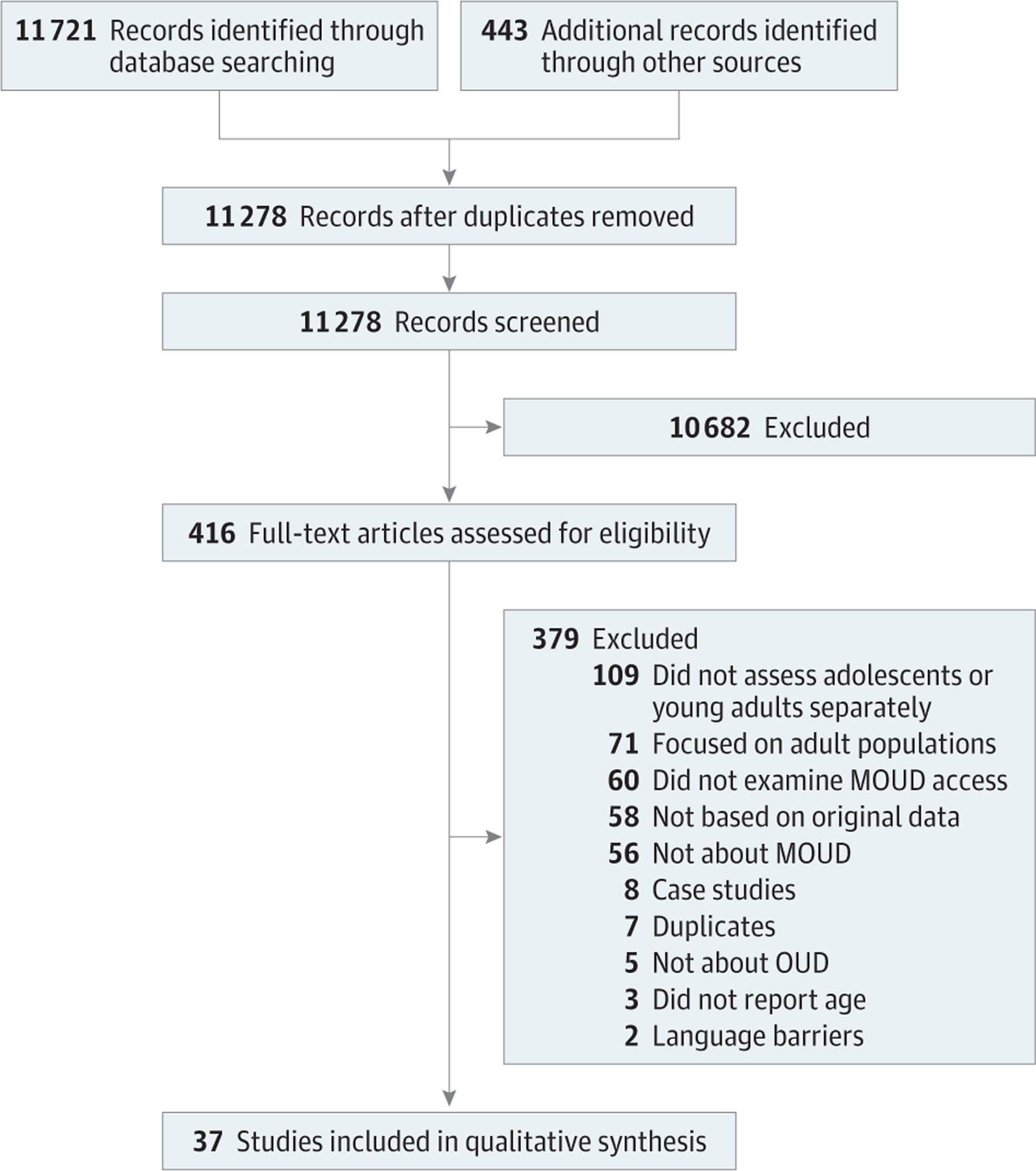
The Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) Flow Diagram
MOUD indicates medications for opioid use disorder.
Fourteen studies included participants with an opioid use disorder (OUD) diagnosis,12,19,21–23,25,26,28,31–35,47 9 examined heroin and other opioid use,16,18,29,36,38,41,42,45,46 and 7 examined any opioid use.11,20,30,39,40,43,44 In addition, 2 studies examined primary opioid use,17,24 1 evaluated nonmedical prescription opioid use,27 and 1 reviewed any injection drug use.37 Sixteen studies included any opioid use during the study period,12,19–23,25,26,31–33,35,37,42,43,48 9 examined current opioid use,17,18,24,28,29,36,44,45,47 3 examined past 30-day opioid use,27,41,46 2 examined past year opioid use,30,38 and 1 examined past 6-month opioid use.39 The remaining studies included opioid use in the 3 months before and 1 month after an opioid-related overdose,13 upon imprisonment,32,40 and in the 3 days and 8 or more years before treatment admission.11
Access to MOUD and Associated Factors
Thirty studies examined access to methadone,11–14, 16–18, 20, 22–26,28–30, 32–35, 37–45, 47 26 examined access to buprenorphine,13–19,21–26,29–36,40,41,43,45,47 and 10 examined access to naltrexone,13–16,19,21–23,30,31 whereas 2 studies did not specify the type of MOUD being investigated.27,46 In addition, 2 studies reviewed access to buprenorphine-naloxone,12,31 1 reviewed access to lofexidine,43 1 reviewed access to disulfiram and acamprosate,15 and 1 reviewed access to slow-release oral morphine and injectable OAT,12 while 3 studies examined MOUD-based detoxification.32,36,43 The proportion of AYAs who accessed MOUD ranged from 0.4%29 to 80.7%,11 including between 1.2%22 and 80.7%11 for methadone, 3%31 and 30%43 for buprenorphine, and 0.8%19 and 37%31 for naltrexone. Additional study findings are summarized in eTable 7 in the Supplement.
Age and Time
Eighteen studies11–14, 19, 21–23, 25, 26, 29–31, 35, 36, 39, 41, 45 reported a significant association between age and MOUD access, which suggests that AYAs were less likely than non-AYA populations to access MOUD. Adding to this, evidence suggests that adolescents were more likely than young adults to receive opioid antagonists (ie, naltrexone) or partial opioid agonists (ie, buprenorphine-naloxone). For example, 1 study reported that a higher proportion of adolescents received buprenorphine-naloxone at their last treatment episode vs methadone (60.1% vs 38.0%), whereas young adults reported similar proportions of buprenorphine-naloxone vs methadone access (49.5% vs 48.3%).12 Similarly, 3 studies22,23,30 reported that AYAs were more likely to access naltrexone compared with non-AYA populations. In addition, 1 study13 of treatment facilities found that MOUD was less likely to be provided when a greater proportion of clients were adolescents, whereas another study14 found that county population characteristics were associated with MOUD receipt. Specifically, the study found that MOUD was more likely to be provided in youth-tailored treatment facilities located in counties with a greater proportion of residents aged 45 to 64 years than 0 to 19 years, whereas counties with a greater proportion of residents aged 25 to 44 years vs those aged 0 to 19 years were less likely to provide MOUD.14
Seven studies examined MOUD access over time.16,21,25,26,35,36,41 The first examined trends in buprenorphine and naltrexone use in the US and found that the proportion of AYAs with MOUD access increased from 2% in 2002 to 31.8% in 200921; however, the proportion of AYAs with MOUD access subsequently decreased to 27.5% in 2014, which coincided with increased odds of receiving naltrexone from 2009 to 2014.21 Similarly, studies among pregnant women found an increase in buprenorphine access but a decrease in methadone access between 2009 and 201526 and an increase in buprenorphine access from 10.1% in 2009 to 33.2% in 2012 with little change in methadone access over the same period.25 Another study reported an increase in MOUD receipt through individual and other referral sources from 1992 to 2017.35 Last, 1 study found that young adults reported a shorter time between heroin initiation and treatment access,41 whereas another study found that receiving MOUD within 30 days of a nonfatal overdose was positively associated with prior MOUD use and having an OUD diagnosis.16
Criminal Justice or Legal System
Five studies17,25,27,32,35 reported on criminal justice or legal system–related factors associated with MOUD access. Two studies17,35 found that referral from the criminal justice system was negatively associated with MOUD access among pregnant women, although pre-incarceration MOUD32 and receiving a criminal justice referral for MOUD in US Medicaid expansion states35 were positively associated with MOUD receipt in prison settings. In addition, residing in a state where child abuse charges are permitted against pregnant women who use drugs was negatively associated with MOUD access,17 as was not having custodial rights over one’s children.25
Geography and Urbanity
Geographic factors associated with MOUD access were reported in 6 studies.13,14,17,21,24,46 Four studies13,17,21,24 identified a negative association between residing in the US South and MOUD access vs residing in the US Northeast, Midwest, and West, whereas 1 additional study14 found that adolescent treatment facilities in the Mid-Atlantic and Mountain US census regions were more likely to provide MOUD vs the New England census region. A study conducted in Italy46 showed that those accessing MOUD in northern Italy were significantly younger than those in southern Italy, suggesting geographic gaps in MOUD access in that country. Last, a study from the US21 found that living in a nonmetropolitan area was positively associated with accessing buprenorphine vs naltrexone, whereas another study14 found that adolescent treatment facilities in medium and small metropolitan, micropolitan, and noncore areas were more likely to provide MOUD vs facilities in large metropolitan areas.
Health and Social Systems
Fourteen studies13,15–17,20,25,27,32,33,37,38,42,46,47 reported an association between health and social system–related factors and MOUD access. Studies reported a positive association between previous treatment attempts and MOUD access,16,20,25,46 although current MOUD enrollment was found to be negatively associated with accessing other MOUD.47 In addition, participants who accessed MOUD were more likely to report experiencing drug-related discrimination in the health care system, which was attributed to their increased contact with the health care system.27 Another study20 found that providing treatment information was positively associated with MOUD access, whereas another study37 found that methadone dispensation fees impeded MOUD access. Two studies32,33 investigated the association between MOUD access and pregnancy and insurance status, with 1 study32 finding that women in the second and third trimester were more likely to receive MOUD vs women in their first trimester. The other study33 reported that pregnant women were less likely to access MOUD vs nonpregnant women and that nonpregnant women with Medicaid insurance were less likely to receive MOUD vs women with private insurance.
Two studies17,42 examined the role of the health care professional and referral source in MOUD access. One qualitative study42 found that long treatment wait times, the delayed prescription of MOUD, and experiencing difficulty when searching for a prescriber were negatively associated with MOUD access. In a study among pregnant women,17 being referred to treatment by an addiction specialist or a health care professional, through the criminal justice system, from the community, or from an unknown referral source was negatively associated with MOUD being included in the patient care plans.
Three studies13–15 assessed facility characteristics to be positively associated with MOUD access, 1 study14 of which found that private vs nonprofit, accredited, and larger facilities with a greater proportion of counselors with graduate degrees were more likely to offer MOUD, whereas facilities that admitted patients were less likely to offer MOUD.15 Another study13 found that nonprofit facilities that accepted insurance, offered inpatient services, and were licensed by a national authority were more likely to offer MOUD. The positive association between insurance acceptance and MOUD access was similarly reported in a study among pregnant women18; however, other studies17,33,36 found that having Medicaid or other insurance was negatively associated with MOUD access.
Personal Health and Social Networks
Nine studies20,22,25,28,37–40,42 identified personal health or social network–related factors associated with MOUD access. Four of these studies20,37,40,42 qualitatively explored motivations for treatment entry, which included feeling unwell and wanting stabilization,20,42 wanting to cease injection drug use,37 and being afraid of contracting hepatitis C in prison.40 In addition, 1 quantitative study39 found that having hepatitis C was positively associated with methadone access, whereas another28 found that a majority of pregnant women accessed MOUD because of concerns for their babies’ health. One study22 found that being diagnosed with depression was negatively associated with MOUD access. Relationship status was also associated with MOUD access, such as in 1 quantitative study25 in which having a partner with a substance use disorder was negatively associated with buprenorphine vs methadone access among pregnant women. In addition, 1 study20 described the influence of coercion on treatment engagement, suggesting that external pressure to enter treatment was associated with deterred treatment engagement.
Race or Ethnicity
Five studies21,22,27,34,36 reported on an association between race or ethnicity and MOUD access, whereas 1 study39 was specific to Indigenous AYAs. Although 1 study27 found a positive association between Latino ethnicity and MOUD access, 3 studies reported a negative association between Black race,21,22,34 Latino ethnicity,21,34 and non-White race27 and MOUD access. This includes 1 study34 that found that pregnant non-Hispanic Black and Hispanic women with depression and anxiety were less likely to receive buprenorphine vs no MOUD compared with pregnant White women with depression or anxiety. Last, 1 study found that White AYAs were more likely to report accessing buprenorphine detoxification vs maintenance treatment.
Sex
Five studies21,22,38,39,41 found an association between sex and MOUD access: women were more likely to access MOUD in 4 studies,22,38,39,41 whereas men were more likely to access MOUD in 1 study.21 In addition, 3 studies38,44,45 compared MOUD access between women and men. One study44 found that women were more likely to report having a history of attempting suicide by overdose and being in a relationship, and men were more likely to report having a sibling with alcohol use disorder, having a past criminal conviction, and being a younger age at school dropout when entering a methadone program. The second study45 reported that women entering a methadone program were more likely to be in a relationship or report self-harm, whereas men were younger, reported sibling opiate use, had previous criminal convictions, had previous incarceration, and were discharged from prison. Last, women entering a methadone program were more likely to report being housed or living in a group home, using a greater number of substances, and encountering program restrictions and stigma as barriers to treatment, whereas men were more likely to report an older age of first heroin use, homelessness, and peer influence.38
Socioeconomic
Six studies14,21,25,27,36,44 examined educational level, income, or employment-related factors associated with MOUD access. Two21,44 found an association between education and MOUD access, one of which showed that AYAs in low- and low-middle educational level neighborhoods were more likely to report MOUD access vs AYAs from high educational level neighborhoods.21
Four additional studies21,25,27,36 reported an association between income or employment and MOUD access. Although 1 study21 found that AYAs from high-middle–income neighborhoods were less likely to access MOUD compared with AYAs from higher-income neighborhoods, it also found that, in comparison with AYAs from high-income neighborhoods, AYAs from low-, low-middle–, and middle-high–income neighborhoods were more likely to access buprenorphine vs naltrexone. Similarly, a study of adolescent treatment facilities14 found that MOUD was more likely to be provided in low-income vs high-income neighborhoods.
A study among young adults27 also found that having a monthly income of $501 to $1500 (US dollars) per month was negatively associated with attempting MOUD and positively associated with unsuccessfully attempting MOUD compared with young adults with a monthly income less than or equal to $500. In terms of employment-related factors, 1 study25 among pregnant women found that those who were employed were more likely to access buprenorphine than methadone, whereas another study36 reported that AYAs accessing buprenorphine detoxification were significantly less likely to report being employed.
Substance Use Type and Behaviors
Six studies11,22,25,36,39,46 reported an association between substance use–related factors and MOUD access. One study46 found that illicit heroin use, use of heroin combined with nonmedical prescription opioids, and codeine, methadone, oxycodone, and tramadol use were positively associated with MOUD access among AYAs. Although this study46 also found that young people accessing buprenorphine detoxification were more likely to report any injection drug use, another study39 showed a positive association between daily injection drug use and methadone access. Two studies found that alcohol use22,39 and other substance use disorders22 were negatively associated with MOUD access, whereas another study among pregnant women found that participants who reported benzodiazepine use were significantly less likely to access buprenorphine vs methadone.25 In addition, 1 study from Australia11 found that methadone program rejection was positively associated with daily opioid use, having a positive urine drug screen for opioids, and having 10 or more criminal convictions compared with those who were admitted to a methadone program, whereas a longer duration of substance use was negatively associated with rejection.
Discussion
Consistent with existing literature examining MOUD access in the general population,29,49–51 this systematic review found younger age to be negatively associated with MOUD access. In addition, the findings suggest that younger age was positively associated with accessing opioid antagonists and partial opioid agonists, such as naltrexone and buprenorphine-naloxone, respectively. One potential explanation for this is the reluctance of clinicians to provide MOUD to AYAs,52–54 which may be due to concerns of diversion53,54 or beliefs that OAT enables substance use and should be used as a last resort.52 More specifically, prescribers may be using value-based decision-making whereby their discriminatory views toward AYAs who use drugs, or their personal perspectives on treatment approaches, may result in the prescription of MOUD that they deem to have a lower potential for abuse. Despite this hesitancy, the toxicity of the illicit drug supply and associated overdose risk is far greater than the risk of prescribing MOUD,6 and efforts should be made to address prescribers’ misconceptions around OUD and biases toward prescribing MOUD to AYAs.
Some evidence from this review points to racial differences in MOUD access. Given the known discrimination and structural racism that many Black, Hispanic, or Latino AYAs experience in the health care system,55 these findings suggest the importance of improving the treatment experiences of Black, Hispanic, or Latino AYAs, which may include improving access to culturally safe treatment services.56,57 Previous qualitative research among Indigenous AYAs have indicated their preference and desire for culturally safe treatment services, which are important to addressing the ongoing legacy of colonization.58
Furthermore, findings suggest that increased access to MOUD was associated with residing in neighborhoods with more residents who have lower income and educational level rather than in neighborhoods with residents who have higher income and higher educational level, which may be explained by the concentration of substance use treatment programs in low-income settings. Despite this, other findings suggest that treatment facilities in high-income neighborhoods were more likely to offer MOUD to AYAs. This emphasizes the importance of ensuring that AYAs have access to a continuum of supports—including health care, housing, income assistance, and education, among others59—alongside MOUD regardless of their socioeconomic background.
Similarly, the substantial geographic differences in MOUD access between the US South and other regions are problematic, especially given recommendations by the American Academy of Pediatrics urging the prescription of MOUD to AYAs.60 These findings suggest the importance of understanding the discrepancies in MOUD access and identifying ways to improve MOUD access for AYAs in this and other regions. Potential solutions to this are communicating the benefits of MOUD to policymakers and clinicians and to AYAs who use drugs, as well as establishing channels for AYAs to access MOUD in underserved, rural, or remote regions.
In addition, the sex-based differences in MOUD suggest that men were less likely to access MOUD. This may be reflective of findings that men are more likely to be influenced by their peer networks, which has been demonstrated in previous qualitative research among AYAs.38 Nevertheless, research61 has shown the positive outcome of peer networks on disseminating pertinent harm reduction and public health information, which may be another solution to addressing sex-based gaps in MOUD access.
Findings pertaining to the association between criminal justice system involvement and MOUD access require further attention. As MOUD remains illegal or out of reach in prison settings around the world,62 existing evidence suggests that many incarcerated patients with OUD who discontinue opioid use in the absence of OAT relapse on release,63 especially within the first 2 weeks of their release.64 Therefore, it is important that access to MOUD be improved for incarcerated or treatment-mandated AYAs to reduce the harms experienced by this population. Similarly, the criminalization of parents who use drugs, especially women who are pregnant or have children, and the negative association with MOUD access is concerning. One intervention that has proved successful is the implementation of a continuum of prenatal and postnatal supports for women who use opioids. This includes community- and hospital-based “rooming in” interventions, where mothers are able to keep their newborn babies at their bedside, that provide MOUD and improve maternal and neonatal health outcomes.65
The negative associations between other types of substance use and MOUD access provide insight into additional areas where treatment access can be improved. As evidence indicates that AYAs have different substance use patterns and treatment needs vs non-AYA populations,66–68 it is important to better understand and offer treatment services that meet the needs of AYAs who report polysubstance use. One promising approach is the provision of prescription stimulants alongside MOUD, which—when adequately dosed—have been found to reduce both illicit opioid and stimulant use.69–71
Gaps in Research
Despite age-related differences in MOUD access, there is limited research examining the mechanisms underlying this relationship. Future research examining both demand- and supply-related barriers and motivators to MOUD may help improve access. Second, only 1 identified study27 examined the association between sexual orientation and MOUD access. Given the heightened risk for substance use disorder among people who identify as lesbian, gay, bisexual, transgender, queer (or questioning), asexual (or allied), intersex, or two-spirit (LGBTQIA2S+),72,73 research seeking to understand MOUD experiences and ways to improve access within this population is needed. Third, research into how to provide MOUD in a culturally safe way, or the health and social services AYAs want, may improve MOUD uptake. Fourth, additional research examining the association between MOUD access, criminal justice involvement, and health system–related factors may help identify ways to reduce barriers to MOUD.
Limitations
This study has several limitations. Although relevant academic databases were searched, records may have been missed in the search and screening process. Second, the heterogeneity between the included studies made it difficult to calculate pooled effect measures; therefore, a narrative synthesis approach was used. In addition, the different approaches to assessing age-related associations made it difficult to compare MOUD access between AYAs. Third, identified studies were all derived from high-income countries; therefore, findings were not generalizable to low- and middle-income settings. Despite these limitations, the quality of included studies was mostly moderate to high, and the identified studies point to ways to improve MOUD access among AYAs.
Conclusions
This systematic review found that a majority of AYAs who report OUD have limited access to MOUD, which is problematic given recommendations for their use.60 Findings suggest there is an urgent need to address barriers to MOUD access, including prescriber reluctance, which may be accomplished by providing AYAs with access to a continuum of health and social supports alongside MOUD. Similarly, determining ways to both encourage and reduce barriers to the prescription of MOUD may be helpful in improving MOUD access among this hard-to-reach population.
Supplementary Material
Key Points.
Question
What factors are associated with access to medications for opioid use disorder (MOUD) among adolescents and young adults (AYAs)?
Findings
In this systematic review of 37 studies including 179 785 AYAs, adolescents were significantly less likely to access opioid agonist treatments and significantly more likely to access MOUD with a lower potential for abuse than were young adults. Differences in MOUD access among AYAs were found to be associated with living in the US South, residing in limited-income areas, Black race, and Hispanic or Latino ethnicity, among other observed factors.
Meaning
Results of this review suggest that there is a need to address barriers to MOUD access among AYAs, especially adolescents; providing AYAs with a continuum of health and social supports, including MOUD, may improve the well-being of AYAs.
Role of the Funder/Sponsor:
The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Funding/Support:
Mr Pilarinos is supported by a 4-year fellowship from the University of British Columbia. Dr Karamouzian is supported in part by a Pierre Elliot Trudeau Foundation doctoral scholarship. This study was also supported in part by grant T32 MH020031 from the National Institute for Mental Health (Mr Bromberg), grant D43 TW010540 from the Fogarty International Center (Mr Bromberg), and grant F31 DA054861 from the National Institute on Drug Abuse (Mr Bromberg).
Footnotes
Conflict of Interest Disclosures: None reported.
Contributor Information
Andreas Pilarinos, British Columbia Centre on Substance Use, Vancouver, British Columbia, Canada, Interdisciplinary Studies Graduate Program, University of British Columbia, Vancouver, Canada.
Daniel J. Bromberg, Yale School of Public Health, Yale University, Laboratory of Epidemiology and Public Health, New Haven, Connecticut, Centre for Interdisciplinary Research on AIDS, New Haven, Connecticut.
Mohammad Karamouzian, British Columbia Centre on Substance Use, Vancouver, British Columbia, Canada, School of Population and Public Health, University of British Columbia, Vancouver, Canada.
REFERENCES
- 1.Donroe JH, Socias ME, Marshall BD. The deepening opioid crisis in North America: historical context and current solutions. Curr Addict Rep 2018;5:454–463. doi: 10.1007/s40429-018-0228-5 [DOI] [Google Scholar]
- 2.Lee LK, Mannix R. Increasing fatality rates from preventable deaths in teenagers and young adults. JAMA 2018;320(6):543–544. doi: 10.1001/jama.2018.6566 [DOI] [PubMed] [Google Scholar]
- 3.Irvine MA, Kuo M, Buxton JA, et al. Modelling the combined impact of interventions in averting deaths during a synthetic-opioid overdose epidemic. Addiction 2019;114(9):1602–1613. doi: 10.1111/add.14664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jones CW, Christman Z, Smith CM, et al. Comparison between buprenorphine provider availability and opioid deaths among US counties. J Subst Abuse Treat 2018;93:19–25. doi: 10.1016/j.jsat.2018.07.008 [DOI] [PubMed] [Google Scholar]
- 5.Carney BL, Hadland SE, Bagley SM. Medication treatment of adolescent opioid use disorder in primary care. Pediatr Rev 2018;39(1):43–45. doi: 10.1542/pir.2017-0153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Camenga DR, Colon-Rivera HA, Muvvala SB. Medications for maintenance treatment of opioid use disorder in adolescents: a narrative review and assessment of clinical benefits and potential risks. J Stud Alcohol Drugs 2019;80(4):393–402. doi: 10.15288/jsad.2019.80.393 [DOI] [PubMed] [Google Scholar]
- 7.Viera A, Bromberg DJ, Whittaker S, et al. Adherence to and retention in medications for opioid use disorder among adolescents and young adults. Epidemiol Rev 2020;42(1):41–56. doi: 10.1093/epirev/mxaa001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saloner B, Feder KA, Krawczyk N. Closing the medication-assisted treatment gap for youth with opioid use disorder. JAMA Pediatr 2017;171(8):729–731. doi: 10.1001/jamapediatrics.2017.1269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chang DC, Klimas J, Wood E, Fairbairn N. Medication-assisted treatment for youth with opioid use disorder: current dilemmas and remaining questions. Am J Drug Alcohol Abuse 2018;44(2):143–146. doi: 10.1080/00952990.2017.1399403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009;151(4):264–269, W64. doi: 10.7326/0003-4819-151-4-200908180-00135 [DOI] [PubMed] [Google Scholar]
- 11.Bell J, Digiusto E, Byth K . Who should receive methadone maintenance? Br J Addict 1992;87(5): 689–694. doi: 10.1111/j.1360-0443.1992.tb02714.x [DOI] [PubMed] [Google Scholar]
- 12.Krebs E, Min JE, Zhou H, Davison C, McGowan G, Nosyk B. The cascade of care for opioid use disorder among youth in British Columbia, 2018. J Subst Abuse Treat 2021;130:108404. doi: 10.1016/j.jsat.2021.108404 [DOI] [PubMed] [Google Scholar]
- 13.Alinsky RH, Hadland SE, Matson PA, Cerda M, Saloner B. Adolescent-serving addiction treatment facilities in the United States and the availability of medications for opioid use disorders. J Adolesc Health 2020;67(4):542–549. doi: 10.1016/j.jadohealth.2020.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hadland SE, Jent VA, Alinsky RH, Marshall BDL, Mauro PM, Cerdá M. Opioid use disorder treatment facilities with programs for special populations. Am J Prev Med 2020;59(3):e125–e133. doi: 10.1016/j.amepre.2020.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paino M, Aletraris L, Roman PM. Organizational predictors and use of evidence-based practices in adolescent substance abuse treatment. Subst Abus 2015;36(4):462–469. doi: 10.1080/08897077.2014.960959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alinsky RH, Zima BT, Rodean J, et al. Receipt of addiction treatment after opioid overdose among Medicaid-enrolled adolescents and young adults. JAMA Pediatr 2020;174(3):e195183. doi: 10.1001/jamapediatrics.2019.5183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Angelotta C, Weiss CJ, Angelotta JW, Friedman RA. A moral or medical problem? the relationship between legal penalties and treatment practices for opioid use disorders in pregnant women. Womens Health Issues 2016;26(6):595–601. doi: 10.1016/j.whi.2016.09.002 [DOI] [PubMed] [Google Scholar]
- 18.Bachhuber MA, Mehta PK, Faherty LJ, Saloner B. Medicaid coverage of methadone maintenance and the use of opioid agonist therapy among pregnant women in specialty treatment. Med Care 2017;55(12):985–990. doi: 10.1097/MLR.0000000000000803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chavez LJ, Bonny AE, Bradley KA, et al. Medication treatment and health care use among adolescents with opioid use disorder in Ohio. J Adolesc Health 2020;67(1):33–39. doi: 10.1016/j.jadohealth.2020.01.016 [DOI] [PubMed] [Google Scholar]
- 20.Guarino HM, Marsch LA, Campbell WS III, Gargano SP, Haller DL, Solhkhah R. Methadone maintenance treatment for youth: experiences of clients, staff, and parents. Subst Use Misuse 2009; 44(14):1979–1989. doi: 10.3109/10826080802494800 [DOI] [PubMed] [Google Scholar]
- 21.Hadland SE, Wharam JF, Schuster MA, Zhang F, Samet JH, Larochelle MR. Trends in receipt of buprenorphine and naltrexone for opioid use disorder among adolescents and young adults, 2001–2014. JAMA Pediatr 2017;171(8):747–755. doi: 10.1001/jamapediatrics.2017.0745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hadland SE, Bagley SM, Rodean J, Levy S, Zima BT. Use of evidence-based medication treatment among Medicaid-enrolled youth with opioid use disorder, 2014–2015. J Adolesc Health 2018;62(2): S16. doi: 10.1016/j.jadohealth.2017.11.033 [DOI] [Google Scholar]
- 23.Hadland SE, Bagley SM, Rodean J, et al. Receipt of timely addiction treatment and association of early medication treatment with retention in care among youths with opioid use disorder. JAMA Pediatr 2018;172(11):1029–1037. doi: 10.1001/jamapediatrics.2018.2143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hand DJ, Short VL, Abatemarco DJ. Substance use, treatment, and demographic characteristics of pregnant women entering treatment for opioid use disorder differ by United States census region. J Subst Abuse Treat 2017;76:58–63. doi: 10.1016/j.jsat.2017.01.011 [DOI] [PubMed] [Google Scholar]
- 25.Krans EE, Bogen D, Richardson G, Park SY, Dunn SL, Day N. Factors associated with buprenorphine versus methadone use in pregnancy. Subst Abus 2016;37(4):550–557. doi: 10.1080/08897077.2016.1146649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krans EE, Kim JY, James AE III, Kelley D, Jarlenski MP. Medication-assisted treatment use among pregnant women with opioid use disorder. Obstet Gynecol 2019;133(5):943–951. doi: 10.1097/AOG.0000000000003231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liebling EJ, Yedinak JL, Green TC, Hadland SE, Clark MA, Marshall BD. Access to substance use treatment among young adults who use prescription opioids non-medically. Subst Abuse Treat Prev Policy 2016;11(1):38. doi: 10.1186/s13011-016-0082-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Quigley JM, Knudsen HK, Lofwall MR. Substance use characteristics and treatment perceptions among opioid dependent pregnant women initiating methadone treatment. Am J Addict 2012;21(4):394–395. doi: 10.1111/j.1521-0391.2012.00241.x [DOI] [Google Scholar]
- 29.Feder KA, Krawczyk N, Saloner B. Medication-assisted treatment for adolescents in specialty treatment for opioid use disorder. J Adolesc Health 2017;60(6):747–750. doi: 10.1016/j.jadohealth.2016.12.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bagley SM, Larochelle MR, Xuan Z, et al. Characteristics and receipt of medication treatment among young adults who experience a nonfatal opioid-related overdose. Ann Emerg Med 2020;75 (1):29–38. doi: 10.1016/j.annemergmed.2019.07.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bell LA, Dir AL, Tu W, Aalsma MC. Characteristics of youth receiving medication treatment for opioid use disorder. J Adolesc Health 2021;68(2 Suppl):S46. doi: 10.1016/j.jadohealth.2020.12.095 [DOI] [Google Scholar]
- 32.Knittel AK, Zarnick S, Thorp JM Jr, Amos E, Jones HE. Medications for opioid use disorder in pregnancy in a state women’s prison facility. Drug Alcohol Depend 2020;214:108159. doi: 10.1016/j.drugalcdep.2020.108159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Patrick SW, Richards MR, Dupont WD, et al. Association of pregnancy and insurance status with treatment access for opioid use disorder. JAMA Netw Open 2020;3(8):e2013456–e2013456. doi: 10.1001/jamanetworkopen.2020.13456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schiff DM, Nielsen T, Hoeppner BB, et al. Assessment of racial and ethnic disparities in the use of medication to treat opioid use disorder among pregnant women in Massachusetts. JAMA Netw Open 2020;3(5):e205734. doi: 10.1001/jamanetworkopen.2020.5734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Winkelman TNA, Ford BR, Shlafer RJ, McWilliams A, Admon LK, Patrick SW. Medications for opioid use disorder among pregnant women referred by criminal justice agencies before and after Medicaid expansion: a retrospective study of admissions to treatment centers in the United States. PLoS Med 2020;17(5):e1003119. doi: 10.1371/journal.pmed.1003119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stancliff S, Joseph H, Fong C, Furst T, Comer SD, Roux P. Opioid maintenance treatment as a harm reduction tool for opioid-dependent individuals in New York City: the need to expand access to buprenorphine/naloxone in marginalized populations. J Addict Dis 2012;31(3):278–287. doi: 10.1080/10550887.2012.694603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Boyd J, Fast D, Hobbins M, McNeil R, Small W. Social-structural factors influencing periods of injection cessation among marginalized youth who inject drugs in Vancouver, Canada: an ethno-epidemiological study. Harm Reduct J 2017; 14(1):31. doi: 10.1186/s12954-017-0159-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brands B, Leslie K, Catz-Biro L, Li S. Heroin use and barriers to treatment in street-involved youth. Addict Res Theory 2005;13(5):477–487. doi: 10.1080/16066350500150624 [DOI] [Google Scholar]
- 39.Yang J, Oviedo-Joekes E, Christian KW, et al. The Cedar Project: methadone maintenance treatment among young Aboriginal people who use opioids in two Canadian cities. Drug Alcohol Rev 2011;30(6):645–651. doi: 10.1111/j.1465-3362.2010.00258.x [DOI] [PubMed] [Google Scholar]
- 40.Larney S, Zador D, Sindicich N, Dolan K. A qualitative study of reasons for seeking and ceasing opioid substitution treatment in prisons in New South Wales, Australia. Drug Alcohol Rev 2017; 36(3):305–310. doi: 10.1111/dar.12442 [DOI] [PubMed] [Google Scholar]
- 41.Mills KL, Teesson M, Darke S, Ross J, Lynskey M. Young people with heroin dependence: findings from the Australian Treatment Outcome Study (ATOS). J Subst Abuse Treat 2004;27(1):67–73. doi: 10.1016/j.jsat.2004.05.001 [DOI] [PubMed] [Google Scholar]
- 42.Ayres R, Ingram J, Rees A, Neale J, Beattie A, Telfer M. Enhancing motivation within a rapid opioid substitution treatment feasibility RCT: a nested qualitative study. Subst Abuse Treat Prev Policy 2014;9:44. doi: 10.1186/1747-597X-9-44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bateman J, Gilvarry E, Tziggili M, Crome IB, Mirza K, McArdle P. Psychopharmacological treatment of young people with substance dependence: a survey of prescribing practices in England. Child Adolesc Ment Health 2014;19(2): 102–109. doi: 10.1111/camh.12013 [DOI] [PubMed] [Google Scholar]
- 44.Fagan J, Naughton L, Smyth B. Opiate-dependent adolescents in Ireland: a descriptive study at treatment entry. Ir J Psychol Med 2008;25(2):46–51. doi: 10.1017/S0790966700010934 [DOI] [PubMed] [Google Scholar]
- 45.Smyth BP, Fagan J, Kernan K. Outcome of heroin-dependent adolescents presenting for opiate substitution treatment. J Subst Abuse Treat 2012;42(1):35–44. doi: 10.1016/j.jsat.2011.07.007 [DOI] [PubMed] [Google Scholar]
- 46.Maremmani I, Guareschi M, Deruvo G, et al. Prescription opioids (substitution medications and pain medications) in patients looking for opioid agonist treatment in northern and southern Italy, using a 18-month survey methodology. Heroin Addict Relat Clin Probl 2015;17(1):33–41. Accessed November 1, 2021. https://www.heroinaddictionrelatedclinicalproblems.org/harcparchives.php?year=2015 [Google Scholar]
- 47.Stine SM, Heil SH, Kaltenbach K, et al. Characteristics of opioid-using pregnant women who accept or refuse participation in a clinical trial: screening results from the MOTHER study. Am J Drug Alcohol Abuse 2009;35(6):429–433. doi: 10.3109/00952990903374080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Adelson M, Linzy S, Ray B, Kreek MJ, Schiffman P, Peles E. Effects of non-scheduled urine drug tests among all students at a private high school in the USA. Heroin Addict Relat Clin Probl 2017;19(5):45–54. [Google Scholar]
- 49.Choi S, Yerneni R, Healy S, Goyal M, Neighbors CJ. Predictors of medication utilization for opioid use disorder among Medicaid-insured HIV patients in New York. Am J Addict 2020;29(2):151–154. doi: 10.1111/ajad.12998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stein BD, Gordon AJ, Sorbero M, Dick AW, Schuster J, Farmer C. The impact of buprenorphine on treatment of opioid dependence in a Medicaid population: recent service utilization trends in the use of buprenorphine and methadone. Drug Alcohol Depend 2012;123(1–3):72–78. doi: 10.1016/j.drugalcdep.2011.10.016 [DOI] [PubMed] [Google Scholar]
- 51.Yang JC, Roman-Urrestarazu A, Brayne C. Differences in receipt of opioid agonist treatment and time to enter treatment for opioid use disorder among specialty addiction programs in the United States, 2014–17. PLoS One 2019;14(12):e0226349. doi: 10.1371/journal.pone.0226349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Upadhyaya H, Deas D. Pharmacological interventions for adolescent substance use disorders. In: Adolescent Substance Abuse: Psychiatric Comorbidity and High-Risk Behaviors Routledge; 2008:145–162. [Google Scholar]
- 53.Huhn AS, Dunn KE. Why aren’t physicians prescribing more buprenorphine? J Subst Abuse Treat 2017;78:1–7. doi: 10.1016/j.jsat.2017.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Netherland J, Botsko M, Egan JE, et al. ; BHIVES Collaborative. Factors affecting willingness to provide buprenorphine treatment. J Subst Abuse Treat 2009;36(3):244–251. doi: 10.1016/j.jsat.2008.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dreyer BP. Racial/ethnic bias in pediatric care and the criminalization of poverty and race/ethnicity—seek and ye shall find. JAMA Pediatr 2020;174(8):751–752. doi: 10.1001/jamapediatrics.2020.1033 [DOI] [PubMed] [Google Scholar]
- 56.Rowan M, Poole N, Shea B, et al. Cultural interventions to treat addictions in Indigenous populations: findings from a scoping study. Subst Abuse Treat Prev Policy 2014;9(1):34. doi: 10.1186/1747-597X-9-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Guerrero EG, Song A, Henwood B, Kong Y, Kim T. Response to culturally competent drug treatment among homeless persons with different living arrangements. Eval Program Plann 2018;66:63–69. doi: 10.1016/j.evalprogplan.2017.10.005 [DOI] [PubMed] [Google Scholar]
- 58.Russell C, Neufeld M, Sabioni P, et al. Assessing service and treatment needs and barriers of youth who use illicit and non-medical prescription drugs in northern Ontario, Canada. PLoS One 2019;14(12): e0225548. doi: 10.1371/journal.pone.0225548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.McKay JR. Making the hard work of recovery more attractive for those with substance use disorders. Addiction 2017;112(5):751–757. doi: 10.1111/add.13502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Committee on Substance Use and Prevention. Medication-assisted treatment of adolescents with opioid use disorders. Pediatrics 2016;138(3): e20161893. doi: 10.1542/peds.2016-1893 [DOI] [PubMed] [Google Scholar]
- 61.Mackesy-Amiti ME, Finnegan L, Ouellet LJ, et al. Peer-education intervention to reduce injection risk behaviors benefits high-risk young injection drug users: a latent transition analysis of the CIDUS 3/DUIT study. AIDS Behav 2013;17(6):2075–2083. doi: 10.1007/s10461-012-0373-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Harm Reduction International. Global State of Harm Reduction Harm Reduction International; 2020.
- 63.Leach D, Oliver P. Drug-related death following release from prison: a brief review of the literature with recommendations for practice. Curr Drug Abuse Rev 2011;4(4):292–297. doi: 10.2174/1874473711104040292 [DOI] [PubMed] [Google Scholar]
- 64.Binswanger IA, Stern MF, Deyo RA, et al. Release from prison—a high risk of death for former inmates. N Engl J Med 2007;356(2):157–165. doi: 10.1056/NEJMsa064115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Abrahams RR, MacKay-Dunn MH, Nevmerjitskaia V, MacRae GS, Payne SP, Hodgson ZG. An evaluation of rooming-in among substance-exposed newborns in British Columbia. J Obstet Gynaecol Can 2010;32(9):866–871. doi: 10.1016/S1701-2163(16)34659-X [DOI] [PubMed] [Google Scholar]
- 66.Unger JB, Simon TR, Newman TL, Montgomery SB, Kipke MD, Albomoz M. Early adolescent street youth: an overlooked population with unique problems and service needs. J Early Adolesc 1998;18(4):325–348. doi: 10.1177/0272431698018004001 [DOI] [Google Scholar]
- 67.Corace K, Willows M, Schubert N, Overington L, Howell G. Youth require tailored treatment for opioid use and mental health problems: a comparison with adults. Can J Addict 2018;9(4): 15–24. doi: 10.1097/CXA.0000000000000032 [DOI] [Google Scholar]
- 68.Calvo M, MacFarlane J, Zaccaro H, et al. Young people who use drugs engaged in harm reduction programs in New York City: overdose and other risks. Drug Alcohol Depend 2017;178:106–114. doi: 10.1016/j.drugalcdep.2017.04.032 [DOI] [PubMed] [Google Scholar]
- 69.Siefried KJ, Acheson LS, Lintzeris N, Ezard N. Pharmacological treatment of methamphetamine/amphetamine dependence: a systematic review. CNS Drugs 2020;34(4):337–365. doi: 10.1007/s40263-020-00711-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Palis H, Harrison S, MacDonald S, Marsh DC, Schechter MT, Oviedo-Joekes E. Self-managing illicit stimulant use: a qualitative study with patients receiving injectable opioid agonist treatment. Drug Alcohol Rev 2020;39(7):914–923. doi: 10.1111/dar.13117 [DOI] [PubMed] [Google Scholar]
- 71.Nuijten M, Blanken P, van de Wetering B, Nuijen B, van den Brink W, Hendriks VM. Sustained-release dexamfetamine in the treatment of chronic cocaine-dependent patients on heroin-assisted treatment: a randomised, double-blind, placebo-controlled trial. Lancet 2016;387(10034): 2226–2234. doi: 10.1016/S0140-6736(16)00205-1 [DOI] [PubMed] [Google Scholar]
- 72.Hughto JMW, Quinn EK, Dunbar MS, Rose AJ, Shireman TI, Jasuja GK. Prevalence and co-occurrence of alcohol, nicotine, and other substance use disorder diagnoses among US transgender and cisgender adults. JAMA Netw Open 2021;4(2):e2036512–e2036512. doi: 10.1001/jamanetworkopen.2020.36512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Marshal MP, Friedman MS, Stall R, et al. Sexual orientation and adolescent substance use: a meta-analysis and methodological review. Addiction 2008;103(4):546–556. doi: 10.1111/j.1360-0443.2008.02149.x [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


