Abstract
Study objective
The first 2 years of the COVID-19 pandemic brought substantial and dynamic changes to emergency department volumes and throughput. The objective of this study was to describe changes in ED boarding among US academic EDs across the duration of the COVID-19 pandemic.
Methods
We conducted a retrospective analysis of monthly data collected from a convenience sample of academic departments of emergency medicine. The study period was from January 2019 to December 2021. The primary outcome was total boarding hours, and secondary outcomes included patient volume stratified by ED disposition. We used multivariable linear panel regression models with fixed effects for individual EDs to estimate adjusted means for 3-month quarters.
Results
Of the 73 academic departments of emergency medicine contacted, 34 (46.6%) participated, comprising 43 individual EDs in 25 states. The adjusted mean total boarding hours per month significantly decreased during the second quarter of 2020 (4,449 hours; 95% confidence interval [CI] 3,189 to 5,710) compared to the first quarter of 2019 (8,521 hours; 95% CI 7,845 to 9,197). Beginning in the second quarter of 2021, total boarding hours significantly increased beyond pre-pandemic levels, peaking during the fourth quarter of 2021 (12,127 hours; 95% CI 10,925 to 13,328).
Conclusions
A sustained and considerable increase in boarding observed in selected US academic EDs during later phases of the COVID-19 pandemic may reflect ongoing stresses to the health care system, with potential consequences for patient outcomes as well as clinician well-being.
SEE EDITORIAL,P. XX.
Editor’s Capsule Summary.
What is already known on this topic
Emergency department (ED) boarding is associated with poor patient and health systems outcomes.
What question this study addressed
How did boarding change during the COVID-19 pandemic in select US academic EDs?
What this study adds to our knowledge
In this retrospective study, tracking operational data from a convenience sample of 34 academic EDs between Jan 2019 to Dec 2021, mean total boarding hours per month increased from a low of 4449 hours (Q2 2020) to 12127 hours (Q4 2021), well beyond pre-pandemic levels.
How this is relevant to clinical practice
At these sites, the strain imposed on ED acute care changed and grew as the COVID-19 pandemic evolved. Policymakers must address structural changes to mitigate the harm that can arise from crowded EDs.
Introduction
Background
During the first wave of the COVID-19 pandemic, the number of patients seeking care in US emergency departments fell dramatically.1 This decline coincided with stay-at-home orders and public health measures amidst considerable fear and uncertainty.2 Whereas some patients sought alternative treatment settings, including telemedicine, others delayed seeking necessary care, leading to worse outcomes.3 , 4 ED boarding, or the time that admitted patients spend in the ED awaiting inpatient beds, also fell during the initial phase of the pandemic.5 However, early reports suggest that boarding has resurged, potentially beyond pre-pandemic levels.6 , 7
Importance
Prolonged ED boarding is associated with worse patient outcomes and creates considerable challenges—if not crises—for clinicians and hospitals.8 Boarding and crowding not only represent intractable problems for delivering high-quality emergency care but also serve as key indicators for the functioning of the health care system overall. Sustained increases in boarding during the later phase of the COVID-19 pandemic may reflect ongoing stresses, and potentially lasting structural changes, to the health care system that merit immediate attention by policymakers and leaders.
Goals of this Investigation
In this study, we describe trends in ED boarding over the course of the COVID-19 pandemic among US academic EDs. We also determined whether changes in ED volume have persisted throughout the pandemic, including a comparison of patients requiring hospitalization to those who were discharged.
Methods
Study design and setting
This study was a retrospective cross-sectional analysis of data collected from a convenience sample of US academic EDs to investigate changes in ED boarding and volume from January 2019 and December 2021. The Academy of Administrators in Academic Emergency Medicine (AAAEM) and Association of Academic Chairs of Emergency Medicine (AACEM) conduct an annual benchmarking survey of academic EDs. A detailed description of the annual survey, eligibility criteria, and administration methods has been previously reported.9 To monitor changes in ED clinical operations during the COVID-19 pandemic, the AAAEM/AACEM Benchmark Committee collected supplemental monthly data, which were used for this study. We followed the Strengthening the Reporting of Observational Studies in Epidemiology guidelines for cross-sectional observational studies (Supplement, available at http://www.annemergmed.com.)10 The institutional review board at the University of Pennsylvania determined that this study was exempt from review.
Selection of Participants
In August 2020, we approached 73 academic EDs who participate in the annual survey to voluntarily submit monthly operations data. Departments were asked to report selected operations metrics using standard internal processes utilizing electronic health record systems. The metrics were chosen by the study team to represent key aspects of ED operations, including total boarding hours and patient volumes. The data collection instrument is provided in the Supplement. Previously designated administrators at all eligible departments were contacted twice through an existing email listserv. Sites that did not submit data within one month were considered nonresponders and not contacted again, given the burden of managing ED operations during the early COVID-19 pandemic.
As the pandemic continued, updated data were requested through direct emails to designated administrators from participating sites. Three additional updates occurred in February 2021, July 2021, and January 2022. Participants reported metrics for one or more affiliated EDs, which could include the primary academic hospital as well as affiliated hospitals within the same academic department. We excluded dedicated pediatric EDs. Data were electronically transferred between participants and the survey administrator (CAH) responsible for managing the data. The administrator reviewed individual data points for each hospital and month to check for reporting errors or outliers and compared data to historical levels to ensure consistency within sites.
Outcomes and Measurements
The primary outcome was the total boarding hours per month. Boarding time was defined as the interval between the time of an inpatient admission or observation order and the time when the patient left the ED for an inpatient unit. Given variation between sites, the data collection instrument specified that the first documented time for any of the following might be used as long as the measure remained consistent for each individual facility: 1) admission or inpatient observation order by the emergency clinician, 2) bed request order, or 3) time of acceptance by an admitting clinician.
Secondary outcomes included the total number of ED encounters per month, defined as all patients who registered to receive ED care. The total ED encounters were further stratified by disposition: 1) hospitalization (admission or observation), 2) discharge, and 3) left without being seen (LWBS) or screened and left, which, together, include patients who registered but did not receive full evaluation by a clinician. Finally, we examined the total number of patient arrivals by emergency medical services per month. For all outcomes, we standardized monthly count data to account for variations in the number of days per month.
We obtained baseline characteristics for participating and nonparticipating EDs from the 2020 AAAEM/AACEM annual survey.9 To adjust for differences in the impact of COVID-19 case volumes between participating sites over the study period, we obtained publicly available data from the Centers for Disease Control and Prevention on the number of new cases of COVID-19 for each month and the state in which the ED was located.11 We then determined per capita COVID-19 incidence using the estimated state population for April 2020, available from the US Census Bureau.12
Analysis
We first plotted monthly median values for primary and secondary outcomes using standard box-and-whisker plots. We then aggregated monthly data into quarters (3-month intervals). To compare outcomes across quarters, we estimated adjusted means for primary and secondary outcomes. To do so, we used multivariable linear panel regression models, with fixed effects for individual EDs. This approach allowed us to estimate within-ED changes across the study period, comparing subsequent quarters with the first quarter of 2019 as the pre-pandemic reference period. This approach does not require further adjustment for baseline hospital or ED characteristics, with each ED serving as its own control for any observed or unobserved characteristics. Models were adjusted for per capita COVID-19 cases for each month and the state in which EDs were located. We used cluster-robust standard errors to account for correlated observations within each ED, with standard error estimates, therefore, robust to heteroscedastic and autocorrelated disturbances in the model. Finally, we reviewed any missing data for hospitals by month, although panel regression can incorporate missing outcomes values for individual hospitals.13 For ease of interpretation, we used predictive margins to report adjusted means. As a secondary analysis, we performed interrupted time-series analyses to characterize trends for outcomes over 6-month intervals during the study period.14 Analyses were performed using Stata, version 16.1 (StataCorp LP).
Results
Of the 73 academic EDs approached, 34 (46.6%) participated in the study, comprising 43 individual EDs. These facilities were located in 25 states. Thirty-eight individual EDs provided data for the entire study period, ending in December 2021; 3 provided data through August 2020, 1 provided data through February 2021, and 1 provided data through June 2021. The 39 departments that did not respond to the survey included 64 individual EDs. Characteristics of participating and nonparticipating EDs are shown in Table 1 .
Table 1.
Characteristics of participating and nonparticipating hospitals.
| Hospital Characteristics | Participating Hospitals (N=43) | Nonparticipating Hospitals (N=64) |
|---|---|---|
| US Region, n (%) | ||
| Northeast | 20 (46.5) | 25 (39.1) |
| South | 7 (16.3) | 17 (26.6) |
| Midwest | 12 (27.9) | 9 (14.1) |
| West | 4 (9.3) | 13 (20.3) |
| Hospital type,∗ n (%) | ||
| Primary academic | 33 (76.7) | 39 (60.9) |
| Academic affiliate | 10 (23.2) | 25 (39.1) |
| Licensed hospital beds, no., median (IQR) | 664 (404-895) | 519 (224-717) |
| ED treatment spaces, no., median (IQR) | 57 (43-82) | 56 (34-73) |
| Overflow treatment spaces, no., median (IQR) | 10 (6-20) | 8 (4-15) |
| Annual ED volume, no., median (IQR) | ||
| Total arrivals | 58,562 (46,921-67,048) | 57,747 (35,160-74,730) |
| ED admissions | 14,555 (9,348-18,838) | 11,873 (6,941-15,339) |
| ED discharges | 37,292 (29,072-42,338) | 38,931 (24,290-50,091) |
| EMS arrivals, %, median (IQR) | 25.9 (20.2-32.9) | 22.2 (17.6-31.5) |
| Pediatric visits,∗∗ %, median (IQR) | 1.1 (0.1-10.1) | 2.8 (0.6-13.7) |
| LWBS or SAL, %, median (IQR) | 2.8 (1.5-5.3) | 3.1 (1.6-5.4) |
| ED encounters by billing level, %, median (IQR) | ||
| 99281 and 99282 | 2.5 (1.3-5.4) | 4.2 (1.3-8.2) |
| 99283 | 15.3 (7.2-21.2) | 16.3 (6.7-21.6) |
| 99284 | 35.0 (29.3-40.8) | 39.9 (28.7-52.6) |
| 99285 and 99291 | 44.6 (35.7-56.3) | 35.9 (26.3-47.2) |
| ED total lengthofstay, hours, median (IQR) | ||
| All encounters | 6.4 (4.6-8.7) | 5.6 (4.0-7.3) |
| Hospitalizations | 9.2 (6.9-11.1) | 8.8 (6.4-12.4) |
| Discharges | 4.9 (3.9-5.7) | 4.3 (3.4-5.4) |
| ED boarding time,∗∗∗ hours, median (IQR) | 5.2 (3.3-7.2) | 4.1 (2.0-5.8) |
| Payer, %, median (IQR) | ||
| Commercial | 28.5 (23.5-32.6) | 24.2 (20.0-32.5) |
| Medicare | 30.1 (26.5-33.2) | 27.2 (23.0-32.3) |
| Medicaid | 25.3 (17.7-32.6) | 27.1 (19.8-40) |
| Other | 11.1 (6.7-16.3) | 13.3 (9.5-17.7) |
IQR, interquantile range; EMS, emergency medical services; LWBS, left without being seen; SAL, screened- and left.
Primary academic hospitals are defined as the main teaching hospital within the academic department of emergency medicine; academically affiliated hospitals are other hospitals included, managed, and staffed by the academic department.
Pediatric visits are defined as any visit by patients younger than 18 years of age.
ED boarding time is defined as the interval between the time of an inpatient admission or observation order and when the patient left the ED for an inpatient unit.
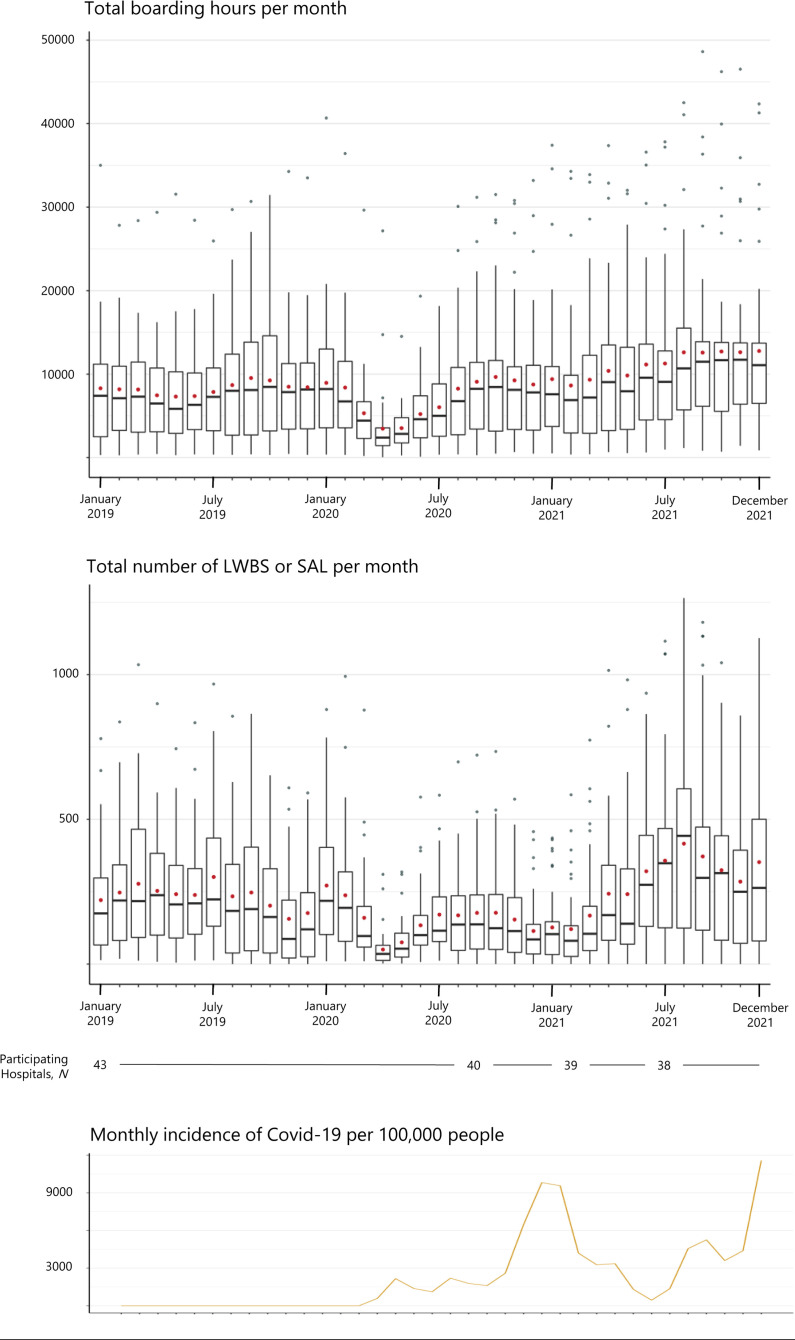
Median total boarding hours by quarter are shown in Table 2 . The Figure shows box-and-whisker plots for total boarding hours by month, presented against the monthly incidence of COVID-19 cases.
Table 2.
Medians and adjusted means for primary and select secondary outcomes by quarter.
| Outcome | 2019 Q1∗ Jan-Mar (reference) |
2020 Q1 Jan-Mar |
2020 Q2 Apr-Jun |
2020 Q3 Jul-Sep |
2020 Q4 Oct-Dec |
2021 Q1 Jan-Mar |
2021 Q2 Apr-Jun |
2021 Q3 Jul-Sep |
2021 Q4 Oct-Dec |
|---|---|---|---|---|---|---|---|---|---|
| Total boarding hours per month | |||||||||
| Median (IQR) | 7,204 (2,968-11,286) | 5,643 (3,042-10,309) | 2,965 (1,824-5,232) | 6,713 (2,660-10,462) | 7,920 (3,280-11,247) | 7,134 (2,995-11,179) | 8,928 (3,730-13,265) | 10,040 (5,635-13,879) | 11,480 (6,370-13,796) |
| Adjusted Mean (95% CI) | 8,521 (7,845-9,197) | 8,033 (7,191-8,875) | 4,449 (3,189-5,710) | 7,844 (7,096-8,592) | 8,812 (8,109-9,514) | 8,827 (8,275-9,379) | 10,383 (9,677-11,088) | 11,838 (10,806-12870) | 12,127 (10,925-13,328) |
| Total LWBS or SAL per month | |||||||||
| Median (IQR) | 201 (77-339) | 159 (78-308) | 57 (21-107) | 133 (55-237) | 101 (41-213) | 98 (34-160) | 189 (84-395) | 348 (115-510) | 262 (66-443) |
| Adjusted Mean (95% CI) | 253 (228-277) | 227 (195-258) | 88 (50-125) | 173 (153-193) | 141 (120-162) | 133 (115-152) | 269 (242-297) | 379 (328-430) | 313 (278-350) |
| Total ED encounters per month | |||||||||
| Median (IQR) | 5,236 (4,127-6,494) | 5,032 (4,150-6,311) | 3,672 (2,965-4,762) | 4,548 (3,738-5,819) | 4,439 (3,603-5,602) | 4,534 (3,597-5,495) | 5,117 (4,215-6,127) | 5,275 (4,262-6,354) | 4,983 (3,957-6,022) |
| Adjusted Mean (95% CI) | 5,449 (5,345-5,554) | 5,254 (5,157-5,351) | 3,733 (3,521-3,946) | 4,744 (4,657-4,831) | 4,726 (4,625-4,828) | 4,675 (4,605-4,745) | 5,283 (5,218-5,348) | 5,493 (5,394-5,592) | 5,300 (5,186-5,415) |
| Total ED hospitalizations per month | |||||||||
| Median (IQR) | 1,506 (1,043-1,936) | 1,439 (1,061-1,799) | 1,237 (904-1,528) | 1,462 (1,041-1,683) | 1,424 (1,047-1,739) | 1,427 (1,035-1,834) | 1,543 (1,104-1,984) | 1,501 (1,059-1,871) | 1,437 (1,034-1,806) |
| Adjusted Mean (95% CI) | 1,508 (1,447-1,569) | 1,447 (1,400-1,494) | 1,262 (1,226-1,297) | 1,431 (1,406-1,456) | 1,429 (1,392-1,466) | 1,436 (1,404-1,469) | 1,518 (1,489-1,546) | 1,495 (1,442-1,548) | 1,438 (1,392-1,484) |
Additional quarters (2019 Q2, Q3, Q4) were omitted from this table for ease of interpretation; no significant differences from the baseline period were observed for these quarters in the adjusted model.
Figure.
Total boarding hours and LWBS or SAL per month, with monthly incidence of COVID-19 per 100,000 people. Box-and-whisker plots show, for each month, median (horizontal bar), IQR (box), 1.5∗IQR (whisker), and outliers (points). Red points indicate unadjusted monthly mean. The number of participating EDs/hospitals varies over time; 43 EDs are included from January 2019 to August 2020, 40 EDs are included from September 2020 to February 2021, 39 EDs are included from March 2021 to June 2021, and 38 EDs are included from July 2021 to December 2021.
In the adjusted analysis, mean total boarding hours per month were significantly decreased during the second quarter of 2020 (4,449 hours; 95% confidence interval [CI] 3,189 to 5,710) compared to the first quarter of 2019 (8,521 hours; 95% CI 7,845 to 9,197). However, mean total boarding hours returned to pre-pandemic levels in the next quarter (Table 2). Beginning in the second quarter of 2021, total boarding hours were significantly increased compared to the pre-pandemic period, peaking during the fourth quarter of 2021 (12,127 hours; 95% CI 10,925 to 13,328).
A similar pattern was observed for the total number of LWBS or screened-and-left encounters per month, with significant decreases that began during the second quarter of 2020 and persisted until the second quarter of 2021, after which LWBS or screened-and-left encounters exceeded pre-pandemic levels (Table 2).
The mean total number of ED encounters were significantly decreased in the second quarter of 2020 (3,733 encounters; 95% CI 3,521 to 3,946) compared to the first quarter of 2019 (5,449 encounters; 95% CI 5,345 to 5,554) and remained significantly lower until the third quarter of 2021. However, mean total ED hospitalizations were only reduced for the second quarter of 2020 compared to the pre-pandemic reference period, with no significant changes for any subsequent quarters (Table 2). Mean total ED discharges remained significantly lower than pre-pandemic levels from the second quarter of 2020 through the end of the study period (Supplement).
In the interrupted time-series analyses, the primary outcome demonstrated a rising trend from July 2020 through the end of the study period (Supplement). Mean total boarding hours rose by 447 hours per month from July 2020 to December 2020 (95% CI, 212 to 681), 367 hours per month from January 2021 to June 2021 (95% CI, 134 to 601), and 220 hours per month (95% CI, 21 to 461) from July 2021 to December 2021. Trends for secondary outcomes are described in the Supplement.
Limitations
This brief report has many limitations. First, EDs included in this study are located in academic medical centers and affiliated hospitals, limiting generalizability. It is possible that changes in boarding and volume were greater in these hospitals, given that many are safety net institutions located in urban centers and care for more complex or severely ill patients. Second, participants comprise a convenience sample of hospitals that responded to requests to report monthly data during the COVID-19 pandemic, introducing possible nonresponse bias. Third, this study does not include patient-level data, including patient characteristics that may influence patterns in utilization or boarding. A related limitation is that we did not account for transient system or practice changes during the pandemic, such as thresholds for hospitalization. Finally, some participants did not report outcomes data for the entire study period; however, our analyses accounted for missing outcomes data by using panel regression with hospital fixed effects.13
Discussion
In this study, we found that boarding transiently decreased in selected academic EDs during the initial phase of the COVID-19 pandemic but subsequently surged beyond 40% of pre-pandemic levels by the end of 2021. We also found that the total number of patients seeking emergency care in this sample of academic EDs returned to baseline levels. Although the number of patients who required hospitalization rapidly recovered after the initial shock of the pandemic, EDs still discharged fewer patients at the end of 2021 compared to before the pandemic. Together, these trends suggest deepening challenges for ED and hospital capacities as the COVID-19 pandemic has evolved.
These findings are consistent with emerging evidence, as well as media reports, that ED boarding has increased over the later phase of the pandemic.6 , 7 This study did not examine potential explanations for the increased boarding. However, previous literature suggests that increased surgical volume, hospital closures, increased hospital length of stay, and decreased hospital staffing all may contribute to worsening ED boarding.8 All of these factors are likely consequences of the COVID-19 pandemic or responses to financial challenges for hospitals during this time. Another potential cause may have been operational changes to inpatient hospital units, with the need to cohort patients with COVID-19 for infection control purposes creating inefficient bed management practices, as well as the need to obtain COVID-19 testing prior to admission. Regardless of the likely multifactorial etiologies for this surge in boarding, the consequences for not only patient experience but also patient outcomes are severe. Furthermore, emergency clinicians may struggle under the burden of increased boarding, exacerbating an ongoing staffing and well-being crisis.15
In summary, the total number of patients seeking emergency care in selected academic medical centers has returned to pre-pandemic levels, although these EDs still discharge fewer patients than before the pandemic. However, patients awaiting hospital admission are boarded in academic EDs for considerably more time than before the pandemic. As the pandemic—and US health care system—continues to evolve, it will be essential to not only monitor these trends but consider structural approaches to alleviating the boarding crisis.
Footnotes
Please see page XX for the Editor’s Capsule Summary of this article.
Supervising editors: Hemal K. Kanzaria, MD; Richelle J. Cooper, MD, MSHS. Specific detailed information about possible conflict of interest for individual editors is available at https://www.annemergmed.com/editors.
Author contributions: ASK, JJS, CAH, and AKA conceived and designed the study. JJS and CAH undertook recruitment of participating centers. CAH managed the data, including quality control. ASK, AM, and AKA provided statistical advice on study design and analyzed the data. ASK, RG, and AKA drafted the manuscript, and all authors contributed substantially to its revision. ASK takes responsibility for the paper as a whole.
Authorship: All authors attest to meeting the four ICMJE.org authorship criteria: (1) Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND (2) Drafting the work or revising it critically for important intellectual content; AND (3) Final approval of the version to be published; AND (4) Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Fundingandsupport: By Annals policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist. Dr. Kilaru is supported by the Agency for Healthcare Research and Quality (5K12HS026372-04).
Trial registration number: Not applicable.
Supplementary Data
References
- 1.Jeffery M.M., D’Onofrio G., Paek H., et al. Trends in emergency department visits and hospital admissions in health care systems in 5 states in the first months of the COVID-19 pandemic in the US. JAMA Intern Med. 2020;180:1328–1333. doi: 10.1001/jamainternmed.2020.3288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sen S., Karaca-Mandic P., Georgiou A. Association of stay-at-home orders with COVID-19 hospitalizations in 4 states. JAMA. 2020;323:2522. doi: 10.1001/jama.2020.9176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel S.Y., Mehrotra A., Huskamp H.A., et al. Variation in telemedicine use and outpatient care during the COVID-19 pandemic in the United States. Health Aff (Millwood) 2021;40:349–358. doi: 10.1377/hlthaff.2020.01786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Findling M.G., Blendon R.J., Benson J.M. Delayed care with harmful health consequences—reported experiences from national surveys during coronavirus disease 2019. JAMA Health Forum. 2020;1 doi: 10.1001/jamahealthforum.2020.1463. [DOI] [PubMed] [Google Scholar]
- 5.Cohen B.A., Wessling E.G., Serina P.T., et al. Emergency department operations in a large health system during COVID-19. Am J Emerg Med. 2021;41:241–243. doi: 10.1016/j.ajem.2020.05.097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Janke A.T., Melnick E.R., Venkatesh A.K. Hospital occupancy and emergency department boarding during the COVID-19 pandemic. JAMA Netw Open. 2022;5 doi: 10.1001/jamanetworkopen.2022.33964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Janke A.T., Melnick E.R., Venkatesh A.K. Monthly rates of patients who left before accessing care in US emergency departments, 2017-2021. JAMA Netw Open. 2022;5 doi: 10.1001/jamanetworkopen.2022.33708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kelen G.D., Wolfe R., D’Onofrio G., et al. Emergency department crowding: the canary in the health care system. NEJM Catalyst. September 28, 2021 https://catalyst.nejm.org/doi/full/10.1056/CAT.21.0217 [Google Scholar]
- 9.Reznek M.A., Scheulen J.J., Harbertson C.A., et al. Contributions of academic emergency medicine programs to U.S. health care: summary of the AAAEM-AACEM benchmarking data. Acad Emerg Med. 2018;25:444–452. doi: 10.1111/acem.13337. [DOI] [PubMed] [Google Scholar]
- 10.von Elm E., Altman D.G., Egger M., et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention COVID data tracker. https://covid.cdc.gov/covid-data-tracker/#trends_dailycases
- 12.United States Census Bureau National population totals and components of change: 2020-2021. https://www.census.gov/data/tables/time-series/demo/popest/2020s-national-total.html
- 13.Young R., Johnson D.R. Handling missing values in longitudinal panel data with multiple imputation. J Marriage Fam. 2015;77:277–294. doi: 10.1111/jomf.12144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Linden A. Conducting interrupted time-series analysis for single- and multiple-group comparisons. Stata J. 2015;15:480–500. [Google Scholar]
- 15.Agarwal A.K., Hahn L., Pelullo A., et al. Capturing real-time emergency department sentiment: a feasibility study using touch-button terminals. Ann Emerg Med. 2020;75:727–732. doi: 10.1016/j.annemergmed.2019.07.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.