Highlights
-
•
Naloxone distribution efforts often miss young adults who use opioids.
-
•
Convenience, privacy, and knowledge were key themes contributing to naloxone uptake.
-
•
Naloxone vending machines were considered an acceptable venue by young adults.
-
•
Vending machine location features, access strategies, and safety will impact uptake.
Keywords: Young adults, Opioid overdose, Vending machine, Harm reduction, Naloxone
Abstract
Background
Take home naloxone (THN) programs have been shown to effectively reverse opioid overdose events with limited adverse events, yet often miss young adults who use opioids. To identify opportunities for naloxone expansion, we conducted interviews with young adults who had used opioids. We explored young adults’ experience with current THN programs, and perspectives on ideal THN programs and emerging naloxone public health vending machine (PHVM) programs shown to increase access to sterile syringes in young adults.
Methods
We interviewed 16 young adults receiving substance treatment services within an integrated safety net healthcare system. Participants were 18–30 years of age with a history of nonmedical prescription opioid use. Interviews obtained the patient perspective of current THN, ideal THN and PHVM programs. Interviews were transcribed and coded by team-based methods. Themes were developed using an inductive-deductive iterative approach and defined through consensus.
Results
Treatment was often the first exposure to naloxone. Participants recommended easy to access programs for ideal naloxone distribution and had overall positive feedback on PHVMs. Three key themes were identified to improve naloxone uptake: knowledge, convenience, and privacy. Participants identified safety, lack of police presence, and low costs as important vending machine features.
Conclusions
Our results identified implementation opportunities to increase naloxone uptake including convenient location and hours, privacy, and using trusted sources of information to improve program awareness. PHVMs present an opportunity to maximize these opportunities and increase access to naloxone in young adults.
1. Introduction
The opioid epidemic is a global health challenge that has been further exacerbated by the COVID-19 pandemic (Degenhardt et al., 2019; Slavova et al., 2020). In the United States (U.S.) there was a sharp increase in opioid overdose deaths reaching 76,002 deaths in the year ending June 2021 (Ahmed et al., 2021). Naloxone, an opioid antagonist medication, can effectively reverse overdose events with limited adverse events (Wermeling, 2015). As such, formulations of the medication have been made available to the public to facilitate bystander use (Wermeling, 2013). Take home naloxone (THN) programs most often occur in community based organizations (often harm reduction agencies), pharmacies (standing orders), and health systems (emergency department, substance use treatment, provider prescriptions, and co-dispensing with opioids) (Weiner et al., 2019). In multiple reviews, take home naloxone (THN) programs providing naloxone and opioid overdose education to persons who use opioids have been shown to reduce opioid overdose events with a lack of adverse events (Dwyer et al., 2018; McAuley et al., 2015; McDonald and Strang, 2016). Additionally, naloxone has no addictive potential and possession has not been shown to increase opioid risk behavior (Binswanger et al., 2022; Strang et al., 1996)
However, THN efforts are leading to unequal access to naloxone in young adults, the age group with the historically highest rate of opioid overdose events (Wilson et al., 2020). Young adults are less likely than adults to use the healthcare system and treatment services, limiting exposure to health system naloxone distribution programs (Bernstein, 2004; Hadland et al., 2018; Stockings et al., 2016). Additionally, young adults have the highest estimated rates of nonmedical use of prescription opioids (NMUPO), a population reporting lack of naloxone knowledge and engagement with harm reduction programs (Frank et al., 2015; Substance Abuse and Mental Health Services Administration, 2020). Even with access to services, naloxone distribution is limited as demonstrated by less than 2% of the commercially insured population at high risk of opioid overdose dispensed naloxone (Follman et al., 2019). Patients report knowledge, stigma and costs as barriers to naloxone uptake (Bessen et al., 2019; Ko et al., 2021).
New strategies are emerging to increase access to naloxone by maximizing accessibility and privacy. In Europe and Australia, vending machines have been used for decades to supplement sterile syringe programs. Sterile syringe inventory is obtained through coins or syringe exchange limiting interaction requirements and increasing temporal service availability (Islam et al., 2008b). Evidence suggests public health vending machines (PHVMs) reach young injection drug using adults who are less engaged with other treatment services and have a shorter duration of drug use (Islam and Conigrave, 2007; Otiashvili et al., 2022) Additionally, program evaluations have found no adverse events associated with machine use (McDonald, 2009), a lack of association with syringe litter, and increased inquiries in Hep C services (Islam et al., 2008a, 2008b).
Public health vending machine (PHVM) programs began in the U.S. in 2017 (United, 2020). A limited number of U.S. programs have begun distributing naloxone along with other harm reduction supplies. However, program implementation varies across the U.S. in inventory, registration (none, online by phone, in person), and access strategies (none, card, or code) and may not always provide the same low threshold access to inventory demonstrated in sterile syringe vending machine programs in other countries. Program implementation heterogeneity and a lack of information on populations reached makes it unclear if naloxone PHVMs address the current barriers to naloxone uptake in young adults. Thus, the goal of this work is to identify opportunities to adapt current THN programs to reach young adults who use opioids by exploring perceived factors contributing to obtaining naloxone under current THN, ideal THN programs and naloxone PHVM programs.
2. Materials and methods
We used a directed content analysis, as this strategy aligns with the goal of this work to expand our understanding of the contextual factors contributing to uptake of naloxone and modifiable features of THN programs (Hsieh and Shannon, 2005). The directed content analysis method informed all aspects of the study including question conceptualization, methods, and data analysis. In this manuscript we adhere to the consolidated criteria for reporting qualitative research (COREQ) (see supplement B) (Tong et al., 2007).
2.1. Study sample and recruitment
We conducted one-hour, semi-structured interviews with young adults, 18–30 years of age, from May-June 2021. We chose the broad definition of young adults to capture the transition from adolescence (18) into full adulthood (age 30), and to include those who may be losing dependent medical coverage at age 26 (DiNardi, 2021; Olfson et al., 2018; Stroud et al., 2015). Participants were eligible if they had witnessed or experienced an opioid overdose. Participants with no opioid overdose experience (personal or witnessing) were eligible if they had nonmedical opioid use in the last 4 months. All participants had a history of opioid use.
We conducted purposeful sampling through in-person recruitment in a safety net health system substance use treatment service clinic in Denver, Colorado. Colorado naloxone laws include third party naloxone administration without criminal prosecution, standing orders, and Good Samaritan Laws (Colorado Department of Public Health & Environment, 2022). Services provided in the clinic included counseling and medication for opioid use disorder. Staff conducting interviews recruited participants in the clinic lobby.
2.2. Framework and interviews
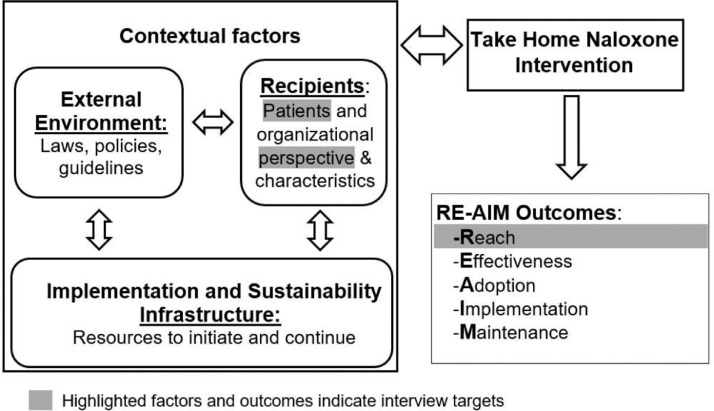
Interview guides were informed by the Practical Robust Implementation and Sustainability Model (PRISM). PRISM is an extension of the Reach, Effectiveness, Adoption, Implementation and Sustainability (RE-AIM) framework, one of the most widely used planning and evaluation frameworks (Glasgow et al., 2019). PRISM incorporates contextual factors contributing to the public health value of an intervention. The interview guide was designed to explore the PRISM contextual factors contributing to engagement with current THN programs (reach) and to identify opportunities for adaptation of the intervention's features to reach a cohort of young adults who have used opioids (Fig. 1). We sought to understand uptake under current THN programs through participants’ perspectives and experiences with naloxone distribution approaches. We asked participants to reflect on experiences obtaining naloxone prior to treatment to inform perspectives of those who have not engaged with substance use services.
Fig. 1.
Practical Robust Implementation and Sustainability Model (PRISM) Contextual Factors Contributing to Take Home Naloxone (THN) Program Outcomes.
An emphasis of the interviews was to identify opportunities for adaptation of current THN programs. We first asked participants to describe an ideal naloxone distribution program and second, impressions of a naloxone PHVM program. Vending machines were described to participants as “like a soda machine containing naloxone” to obtain general impressions. We then described current program features and probed to examine preferred implementation (registration, access strategies, and inventory). While not the focus of these interviews, other features of the PRISM framework are its emphasis on organizational characteristics and perspective, external environment, and the implementation and sustainability infrastructure. These PRISM features informed interview probes to identify opportunities for adaptation such as police presence (external environment), location of services (organizational characteristics), and participant's willingness to pay for naloxone (infrastructure and sustainability). Interviews were conducted by a qualitatively trained female researcher (NW) and continued until preliminary analysis indicated that we reached data saturation (Saunders et al., 2018). Dr. Wagner had no prior relationship with participants and explained the aims of the project at consent.
2.3. Analysis
Interviews were audio recorded and transcribed by a professional translation company. Using a mixed inductive and deductive coding strategy, two qualitatively trained researchers (NW and JB) coded the transcripts within ATLAS.ti 9 software. Deductive codes were derived using operational definitions from the PRISM framework. Next, the team double coded 25% of the transcripts (independently coding the same transcripts) using the predetermined codes and inductively coded new categories or subcategories to establish shared understanding of the concepts in the data and consistency in application of codes amongst the coding team (Hsieh and Shannon, 2005). Codes were reviewed, discrepancies resolved, and definitions refined until consensus was reached. The remaining coding was iteratively reviewed with team-based discussion further refining definitions, resolving discrepancies through consensus, and determining data saturation (see supplement A for codebook). Final coded transcripts were analyzed for recurrent themes and salient quotes were extracted. Study procedures were approved by the Colorado Multiple Institutional Review Board (CoMIRB).
3. Results
3.1. Study population characteristics
Seventeen participants expressed a willingness to be interviewed. One participant was excluded due to an inability to consent. We completed 16 interviews. A young child accompanied a participant in 4 interviews. The median age of participants was 27 years, with a range of 18–30. All participants reported NMUPO in their lifetime, and many participants (n = 11) reported using heroin. Fourteen participants (87.5%) reported opioid overdose experience (witnessing or experiencing), of which eight (57%) both witnessed and experienced an opioid overdose. The remaining two participants with no opioid overdose experience used opioids in the last 4 months. Half of the population identified with a race other than white. Just under half (n = 6) of the cohort were female and had less than a high school education (n = 6). There were a variety of living situations (Table 1) and of those aware of their household income (n = 11), all but one participant were below 200% of the federal poverty level.
Table 1.
Characteristics of the Interview Participants.
| Characteristic | N = 16 |
|---|---|
| Age, median (range) | 27 (18–30) |
| Male, n (%) | 10 (62.5) |
| Witness an opioid overdose, n (%) | 12 (75.0) |
| Experienced an opioid overdose, n (%) | 9 (56.4) |
| Race/Ethnicity, n (%) | |
| Hispanic | 2 (12.5) |
| Race, n (%) | |
| White | 8 (50.0) |
| Black | 3 (18.8) |
| Othera | 5 (31.0) |
| Education, n (%) | |
| <High school graduate | 6 (37.5) |
| High school graduate or GED | 3 (18.8) |
| Some college or technical school | 6 (37.5 |
| College graduate | 1 (6.3) |
| Living arrangements, n (%) | |
| Own House or apartment | 5 (31.3) |
| On the streets | 1 (6.3) |
| Hotel or motel | 1 (6.3) |
| Rooming boarding house/shelter | 2 (12.5) |
| Parent or guardian's house | 4 (25.0) |
| Other's house or apartment | 3 (18.8) |
| Household annual income, n (%) | |
| <$5000 | 3 (18.8) |
| $5000-$15,000 | 5 (31.3) |
| $15,000-$39,999 | 3 (18.8) |
| Unknown | 5 (31.3) |
GED=General Education Development;.
Other races included American Indian or Alaska Native, Asian, other races as defined by the participant, and participants identifying as more than one race.
3.2. Key themes overview
All participants had obtained naloxone and knew it could reverse an opioid overdose. While recognizing the benefits of naloxone for oneself, participants also reported a desire to have naloxone to protect peers. A participant expressed the benefits of having naloxone available, “Like if there's a kid in the house or something and they just happen to get ahold of my frickin’ medications or something. It's good to have Narcan [naloxone] just in case…” He went on to report frequently carrying naloxone “Got it on me right now.”
Overall, participants had a positive impression of naloxone PHVMs, as shared by a participant, “Yeah, that'd be cool just if you ever need Narcan, just go to the vending machine and go get it.” Participants noted a desire to limit child accessibility, “Definitely would have to put some signage up that would deter younger children from approaching said vending machine.”
In discussion of current, ideal, and vending machine naloxone distribution programs, three key themes emerged representing factors contributing to naloxone uptake that present opportunities to adapt current THN programs to increase use by young adults who use opioids: knowledge, convenience, and privacy.
3.2.1. Knowledge
Knowledge was defined as the awareness of naloxone and THN programs. When asked about experiences with current THN programs, many participants reported substance use treatment as their first exposure to naloxone. The lack of naloxone awareness was further emphasized when participants reflected on experiences prior to treatment, “Well, I never knew that there was Narcan ‘til I started here.”
Several participants connected lack of knowledge to living in rural communities, “We were in a small town, and the whole small town did drugs. I never heard of the Narcan.” A participant describing ideal naloxone distribution programs recommended targeting rural communities, “I'm from a little, tiny, little town of about 3000 people. I would reach out to all the little towns ‘cause…where I'm from, I didn't know the world had these kinds of resources.”
Opportunities to increase knowledge were explored through requests for communication recommendations in ideal and vending machine naloxone distribution that could reach young adults and encourage obtaining naloxone. Participants identified multiple modes of communication such as magazines, news, radio stations, billboards, posted signs, and social media. While mode of communication varied, two key features of communication strategies emerged. First, participants said they would consider close friends as trusted sources of naloxone information, “…friends and parents ‘cause they're someone close to you, who's telling you [about naloxone].” Second, participants described advertising in places where you could find people who misuse opioids, “around the places you go, like around this clinic…” and a second person shared, “I would say maybe put flyers up in places where people use the most and maybe where drugs are being sold.”
3.2.2. Convenience
Convenience was defined as having easy to access naloxone. When discussing use of current THN programs, participants primarily reported obtaining naloxone in circumstances in which they were receiving other services and naloxone was handed to them (treatment, syringe exchange program, peer distribution). A participant described an experience obtaining naloxone at a harm reduction program, “They hand it out like candy. Yeah, they're like, ‘Here. You need Narcan?’ Every time you go up there.” While describing his experience obtaining naloxone during treatment services a participant reflected on the benefits of having naloxone included with other needed items, “They provided me with a bag of stuff ’cause I was homeless and— That one [naloxone] was included in there, so it was nice.”
Overall participants described ideal naloxone distribution programs in which naloxone came directly to the participant, such as mail distribution, outreach worker distribution, and mobile delivery units. Expanding on knowledge gaps above, the participant recommending targeting rural communities described the need to address rural access barriers, “I would reach out to all the little towns…the closest suboxone/methadone clinic [location participant obtained naloxone] to where I'm from is 160 miles away.” Participants also identified easy access for family and friends of people who misuse opioids as an ideal strategy for naloxone distribution, “It's not really easy for somebody that doesn't have an opiate addiction to get it [naloxone]…I wish it was available for everybody else ‘cause family members and friends would be—it would be nice to have people around you that is in— a right state of mind, too, that know how to do it.”
When providing overall impressions of naloxone PHVMs, participants had positive reactions emphasizing convenience as a benefit. As one person told us, “I mean it's easier to access.” However, further exploration of implementation features of naloxone PHVMs identified lack of convenience as a potential barrier. When discussing different inventory access strategies (phone, in person, or online), one participant expressed the potential barriers interaction may pose, “if it takes time, and they [people who use drugs] gotta do that [contact harm reduction agency staff for access code], they won't do it.” Many participants were not opposed to strategies to obtain a code if the process was simple.
Similarly, participants emphasized convenient locations and hours of operations as key strategies for naloxone PHVM implementation. When asked where a naloxone PHVM should be located participants emphasized meeting people where they are, “like places where drug addicts are gonna be, like downtown by the shelters and other places, high traffic drug trade areas…” Participants consistently reported a desire for 24-hour access to the naloxone PHVM, because there is “more activity at night.”
3.2.3. Privacy
“When you're on drugs you don't trust anybody really. You believe everyone's setting you up. It's scary and it's crazy to think and say that, but it's true.” This participant was describing the final key theme, privacy. Privacy was defined as a fear of judgment including a desire to obtain substance use services anonymously. Another participant reflected on her partner's desire for privacy about drug use “People keep it a secret and don't wanna say anything to anybody. He did for a while. I was the only one who knew about him using it.”
Participants were currently engaged in treatment services and less concerned with privacy, “I'm not too embarrassed to do it [receive naloxone] ’cause I know that it will help me in the future.” However, when asked to reflect on circumstances prior to obtaining treatment, participants recalled privacy concerns, “I think it's the whole wanting to remain anonymous thing mainly because before I was willing to admit that I had a problem, it's just like nobody could know. It's gotta be a secret”
Ideal THN programs incorporated approaches to protect privacy. A participant described universal naloxone distribution from primary care physicians to increase exposure and protect privacy,
I feel like they should be offering it to everyone at the doctor's office who goes in for a physical…Not everyone is that obvious addict….No one would suspect I used drugs, but if a doctor had offered it to me at the doctor's office, I'd say, ‘yeah, I'll take it. Why not be safe?” I wouldn't necessarily wanna tell the doctor that like, “oh yeah, I'm a drug user,” but I would appreciate having it.
Some participants highlighted privacy as a consideration for how naloxone PHVMs are implemented, “like that kind of setting, something anonymous that's less intrusive and invasive makes the person more willing to approach it.” Another participant incorporated convenience and privacy in location recommendations, “Easily accessible places, maybe put it in a little corner or something where you don't feel judged and you don't be like, ‘Oh, there are people staring at me. I'm not gonna go get some.’” One participant reflected on people who may want to obtain naloxone but would be reticent if required to obtain an access code from a harm reduction agency, “Yeah, they'd be like, ‘Oh, if other people that don't use drugs see me go in there, they might think that I use drugs.’”
Other participants felt the vending machine itself provided the desired privacy, “…obviously no one's gonna judge you ’cause no one's handing them to you, so no one really knows, so it's very private.” Potential solutions to privacy concerns with vending machines were offered including masking inventory, ‘’Be able to cover up the stuff a little bit… make sure that it doesn't look too—they know what it is,” and incorporating a wide variety of inventory, “if you put clothing in there, too, or water, or whatever, they don't [know] whether you're walking up to that vending machine for water or Narcan or needles or whatever.”
3.2.4. Vending machine implementation and maintenance themes
In addition to knowledge, convenience, and privacy, themes emerged reflecting important implementation and maintenance features of vending machines to maximize uptake. First, police presence was consistently reported as a deterrent to use of naloxone PHVMs as reflected by one participant,
Well, I definitely think if there was law enforcement or security-looking people near it, that would deter people ‘cause…—alotta addicts tend to distrust law enforcement, and they might think, oh the police officer sees me buying Narcan. He knows that I have drugs on me. Now he's gonna arrest me once I get out onto the parking lot.
Second, safety concerns were identified in female participants fearing naloxone vending machines could make her a target,
If someone saw you using the vending machine, they figure that either you have drugs on you, and they might try to rob you…Then they might follow you and see you administer it to a person, who is very vulnerable and make that their target like…. Let's raid their pockets,’ yeah…Worse they could assault the person.
When asked what would make her feel safe, she suggested an emergency outreach option, “Maybe to have a ringer or it closed off somewhere where you can push a button and talk to somebody…and having somebody close, at least, like a call person around there.”
Lastly, when exploring the infrastructure to maintain a naloxone PHMV program, participants were asked what cost they would be willing to pay. Many participants reported they would be willing to pay a nominal fee for the convenience and privacy, “I'd pay a couple of bucks for the convenience…Yeah, and not have to frickin' involve my doctor and let them know that ‘Hey, another one of my friends dropped. I had to save 'em.’" However, participants currently receive naloxone at no cost. Thus, some participants were unwilling or unable to pay.
4. Discussion
Multiple THN programs exist yet have challenges reaching young adults (Marshall et al., 2016). As the rate of fatal opioid overdose continues to grow, new strategies to increase availability of naloxone for timely use are needed (Ahmed et al., 2021). Our qualitative interviews with young adults who used opioids identified a desire to have naloxone. Participants reported knowledge, convenience, and privacy, as opportunities to optimize uptake of naloxone, particularly in young adults early in drug use. Results support acceptability of vending machine naloxone distribution programs to increase naloxone uptake in young adults if implemented in convenient locations with 24-hour access, incorporating privacy and safety measures (such as masking materials, including non-drug use items, and limiting police presence), and including advertising strategies through trusted messengers.
Our findings that many participants had not obtained naloxone prior to treatment services and those who had, obtained it from peers and harm reduction services is consistent with the literature (Burton et al., 2021; Follman et al., 2019). As previous studies with young adults have demonstrated a lack of naloxone knowledge (Frank et al., 2015), ensuring awareness of THN programs appears to be the first step in expanding naloxone uptake. Participants identified trusted sources and advertisement in locations they congregate (e.g. parks where drugs are sold) as strategies to increase awareness. Participants also emphasized the benefits of naloxone for peer protection, highlighting an opportunity for messaging focused on protecting others. Recent evidence demonstrates younger and older adults who use fentanyl viewed risk perception messages differently, suggesting a tailored messaging approach for young adults is warranted (Gunn et al., 2021).
Increasing knowledge alone would likely not address the barriers of naloxone uptake. Social and self-stigma have been well established factors negatively contributing to health outcomes in people who use opioids (Cumming et al., 2016). It is common for health care professionals to have negative attitudes towards people who use drugs that can then negatively impact health care delivery (Van Boekel et al., 2013). This is consistent with participant recommendations to ensure privacy and limit staff interaction. Similarly, access is a well-documented barrier to substance use service and naloxone uptake, particularly in populations with co-occurring mental illness and rural communities (Browne et al., 2016; Liebling et al., 2016; Lozo et al., 2019; Priester et al., 2016). Increased hours of operation and availability of services in more convenient locations could address this barrier but may pose significant implementation challenges to current THN programs.
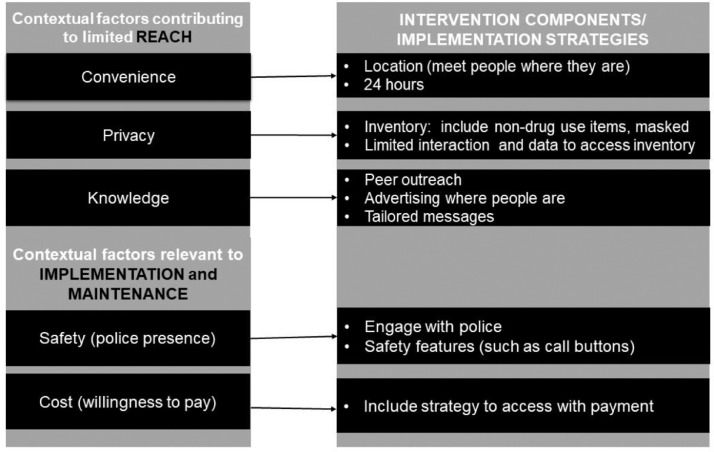
If advertised in a way that reaches young adults, naloxone PHVMs present an opportunity to overcome barriers imposed by service location, hours of operation, and stigma (social and self). The use of PRISM facilitated identification of intervention features and implementation strategies to maximize uptake (Fig. 2) including simple inventory access with limited interaction and data input, masking inventory through many items and covering what is dispensed, locating naloxone PHVMs in places where people use opioids, limiting police presence, and providing a safe environment with features such as call buttons. Participants’ fear of police presence near naloxone PHVMs is consistent with the literature demonstrating police interactions pose a barrier to use of harm reduction services (Cooper et al., 2005; Koester et al., 2017). Thus, naloxone PHVM programs may also require engagement with local police to ensure alignment of goals and safety of program users. Participants also encouraged naloxone PHVMs in rural areas to reach underserved communities, presenting an opportunity to supplement current programs for expansion in hard-to-reach locations with limited substance use resources.
Fig. 2.
Contextual Factors informing Features of Naloxone Vending Machine Programs to increase Naloxone Uptake in Young Adults Who Misuse Opioids.
While these recommendations may be feasible implementation strategies in many environments, there may be organizational and location limitations to naloxone PHVM implementation. Naloxone access laws vary, and in some cases may limit how naloxone PHVMs are implemented (Legislative Analysis and Public Analysis Association, 2020). For example, some states in the U.S. require overdose training with naloxone distribution requiring an education component incorporated into obtaining PHVM inventory. This can be overcome with a variety of training modalities (e.g. online), but may poses additional registration requirements. Other logistical features may limit capacity, such as maintaining and filling vending machines in low resource and hard to reach settings. However, participants did report a willingness to pay a nominal fee for naloxone, indicating payment strategies could be considered for long term maintenance of a naloxone PHVM program. Thus, incorporating the perspective of young adults who use opioids with the multilevel organizational perspective is needed to design the optimal program (Concannon et al., 2012).
Opportunities to increase naloxone uptake in young adults who misuse opioids are not limited to vending machines. Our results highlight opportunities existing under current THN programs. For example, participants described ideal programs that currently exist including mail order and mobile outreach (Yang et al., 2021). With improved advertising these programs could expand uptake to this young adult cohort. As recommended by a participant, routine naloxone distribution in primary care is warranted to address health system stigma and reach those who may not be willing to disclose drug use in the primary care system. Additionally, all participants obtained naloxone through treatment services. Expanding availability of treatment service (location and hours) and increasing advertising may pose an opportunity to increase naloxone uptake.
This study is limited by the population sampled and by recall bias. Participants were recruited from one inner-city clinic with participants who were engaged with treatment services, which may not reflect young adults who have not yet engaged with treatment or live in other geographic regions. However, participants reflected on their experiences prior to treatment and when living in other geographic regions, including rural communities, informing the results of this work. Participants also represented a variety of race and ethnicities, education levels, housing arrangements, and opioid use (NMPOU and heroin). Findings were also limited to participants’ perception of naloxone PHVMs and not based on actual experiences with the machines. As the number of available naloxone PHVMs grow, further evaluation is needed to inform the uptake and potential barriers of naloxone PHVM use.
5. Conclusion
Using the PRISM model as a guide, we explored contextual features contributing to uptake of naloxone in young adults who use opioids and opportunities to adapt naloxone distribution programs. We identified implementation opportunities to increase uptake of naloxone including meeting people where they are through convenient locations and hours of service, increasing privacy to address concerns with stigma, and working with trusted sources to improve program awareness. PHVMs provide an opportunity to capitalize on these opportunities and increase access of naloxone in young adults who use opioids. Future research is needed to obtain the organization perspective and assess the uptake of vending machine naloxone distribution in young adults.
Roles of funding source
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung and Blood Institute of the National Institutes of Health. The funding organization had no role in the collection, management, analysis, and interpretation of the data or the decision to submit the manuscript for publication.
Contributors
Dr. Wagner conceptualized and designed the study, collected the data, conducted analysis, interpreted the data, drafted the initial manuscript, and reviewed and revised the manuscript. Drs. Morris and Kempe supported design of the study, interpreted the data, and reviewed and revised the manuscript. Ms. Barnard supported development of the analytic plan, coded the transcripts, conducted analysis, interpreted the data, and reviewed and revised the manuscript. Drs. Havranek and Rinehart supported site coordination and data capture, interpretation of results, and reviewed and revised the manuscript. Drs Glasgow and Blum supported design of the study and reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Funding
This work was supported by the National Heart Lung and Blood Institute [grant number K12HL137862].
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Nicole Wagner reports financial support was provided by National Heart Lung and Blood Institute.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.dadr.2022.100094.
Contributor Information
Nicole M. Wagner, Email: Nicole.Wagner@cuanschutz.edu.
Allison Kempe, Email: Allison.Kempe@childrenscolorado.org.
Juliana G Barnard, Email: Juliana.Barnard@cuanschutz.edu.
Deborah J. Rinehart, Email: Deborah.Rinehart@dhha.org.
Edward P. Havranek, Email: Ed.Havranek@dhha.org.
Russell E. Glasgow, Email: Russell.Glasgow@cuanschutz.edu.
Joshua Blum, Email: Joshua.Blum@dhha.org.
Megan A Morris, Email: Megan.A.Morris@cuanschutz.edu.
Appendix. Supplementary materials
References
- Ahmed F., Rossen L., Sutton P. National Center for Health Statistics; 2021. Provisional Drug Overdose Death Counts. [Google Scholar]
- Bernstein A.B. National Center for Health Statistics; 2004. Health Care in America: Trends in utilization. Center for Disease Control and Prevention. [Google Scholar]
- Bessen S., Metcalf S.A., Saunders E.C., Moore S.K., Meier A., McLeman B., Walsh O., Marsch L.A. Barriers to naloxone use and acceptance among opioid users, first responders, and emergency department providers in New Hampshire, USA. Int. J. Drug Policy. 2019;74:144–151. doi: 10.1016/j.drugpo.2019.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binswanger I.A., Rinehart D., Mueller S.R., Narwaney K.J., Stowell M., Wagner N., Xu S., Hanratty R., Blum J., McVaney K. Naloxone co-dispensing with opioids: a cluster randomized pragmatic trial. J. Gen. Intern. Med. 2022:1–10. doi: 10.1007/s11606-021-07356-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne T., Priester M.A., Clone S., Iachini A., DeHart D., Hock R. Barriers and facilitators to substance use treatment in the rural south: a qualitative study. J. Rural Health. 2016;32(1):92–101. doi: 10.1111/jrh.12129. [DOI] [PubMed] [Google Scholar]
- Burton G., McAuley A., Schofield J., Yeung A., Matheson C., Parkes T. A systematic review and meta-analysis of the prevalence of take-home naloxone (THN) ownership and carriage. Int. J. Drug Policy. 2021 doi: 10.1016/j.drugpo.2021.103298. [DOI] [PubMed] [Google Scholar]
- Concannon T.W., Meissner P., Grunbaum J.A., McElwee N., Guise J.-.M., Santa J., Conway P.H., Daudelin D., Morrato E.H., Leslie L.K. A new taxonomy for stakeholder engagement in patient-centered outcomes research. J. Gen. Intern. Med. 2012;27(8):985–991. doi: 10.1007/s11606-012-2037-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper H., Moore L., Gruskin S., Krieger N. The impact of a police drug crackdown on drug injectors’ ability to practice harm reduction: a qualitative study. Soc. Sci. Med. 2005;61(3):673–684. doi: 10.1016/j.socscimed.2004.12.030. [DOI] [PubMed] [Google Scholar]
- Cumming C., Troeung L., Young J.T., Kelty E., Preen D.B. Barriers to accessing methamphetamine treatment: a systematic review and meta-analysis. Drug. Alcohol Depend. 2016;168:263–273. doi: 10.1016/j.drugalcdep.2016.10.001. [DOI] [PubMed] [Google Scholar]
- Degenhardt L., Grebely J., Stone J., Hickman M., Vickerman P., Marshall B.D., Bruneau J., Altice F.L., Henderson G., Rahimi-Movaghar A. Global patterns of opioid use and dependence: harms to populations, interventions, and future action. Lancet North Am. Ed. 2019;394(10208):1560–1579. doi: 10.1016/S0140-6736(19)32229-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiNardi M. Aging out of the federal dependent coverage mandate and purchases of prescription drugs with high rates of misuse. Econ. Human Biol. 2021;43 doi: 10.1016/j.ehb.2021.101066. [DOI] [PubMed] [Google Scholar]
- Dwyer R., Olsen A., Fowlie C., Gough C., van Beek I., Jauncey M., Lintzeris N., Oh G., Dicka J., Fry C.L., Hayllar J., Lenton S. An overview of take-home naloxone programs in Australia. Drug Alcohol Rev. 2018;37(4):440–449. doi: 10.1111/dar.12812. [DOI] [PubMed] [Google Scholar]
- Follman S., Arora V.M., Lyttle C., Moore P.Q., Pho M.T. Naloxone prescriptions among commercially insured individuals at high risk of opioid overdose. JAMA Netw. Open. 2019;2(5) doi: 10.1001/jamanetworkopen.2019.3209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank D., Mateu-Gelabert P., Guarino H., Bennett A., Wendel T., Jessell L., Teper A. High risk and little knowledge: overdose experiences and knowledge among young adult nonmedical prescription opioid users. Int. J. Drug Policy. 2015;26(1):84–91. doi: 10.1016/j.drugpo.2014.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow R.E., Harden S.M., Gaglio B., Rabin B., Smith M.L., Porter G.C., Ory M.G., Estabrooks P.A. RE-AIM planning and evaluation framework: adapting to new science and practice with a 20-year review. Front. Public Health. 2019;7:64. doi: 10.3389/fpubh.2019.00064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunn C.M., Maschke A., Harris M., Schoenberger S.F., Sampath S., Walley A.Y., Bagley S.M. Age-based preferences for risk communication in the fentanyl era:‘A lot of people keep seeing other people die and that's not enough for them. Addiction. 2021;116(6):1495–1504. doi: 10.1111/add.15305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadland S.E., Bagley S.M., Rodean J., Silverstein M., Levy S., Larochelle M.R., Samet J.H., Zima B.T. Receipt of timely addiction treatment and association of early medication treatment with retention in care among youths with opioid use disorder. JAMA Pediatr. 2018;172(11):1029–1037. doi: 10.1001/jamapediatrics.2018.2143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh H.F., Shannon S.E. Three approaches to qualitative content analysis. Qual. Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- Islam M.M., Conigrave K.M. Assessing the role of syringe dispensing machines and mobile van outlets in reaching hard-to-reach and high-risk groups of injecting drug users (IDUs): a review. Harm. Reduct. J. 2007;4(1):1–9. doi: 10.1186/1477-7517-4-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam M.M., Stern T., Conigrave K.M., Wodak A. Client satisfaction and risk behaviours of the users of syringe dispensing machines: a pilot study. Drug Alcohol Rev. 2008;27(1):13–19. doi: 10.1080/09595230701711199. [DOI] [PubMed] [Google Scholar]
- Islam M.M., Wodak A., Conigrave K.M. The effectiveness and safety of syringe vending machines as a component of needle syringe programmes in community settings. Int. J. Drug Policy. 2008;19(6):436–441. doi: 10.1016/j.drugpo.2007.07.006. [DOI] [PubMed] [Google Scholar]
- Ko J., Chan E., Doroudgar S. Patient perspectives of barriers to naloxone obtainment and use in a primary care, underserved setting: a qualitative study. Subst. Abus. 2021;42(4):1030–1039. doi: 10.1080/08897077.2021.1915915. [DOI] [PubMed] [Google Scholar]
- Koester S., Mueller S.R., Raville L., Langegger S., Binswanger I.A. Why are some people who have received overdose education and naloxone reticent to call Emergency Medical Services in the event of overdose? Int. J. Drug Policy. 2017;48:115–124. doi: 10.1016/j.drugpo.2017.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colorado Department of Public Health & Environment, 2022. Colorado public health harm reduction legislation. https://cdphe.colorado.gov/prevention-and-wellness/colorado-public-health-harm-reduction-legislation. (Accessed 7/7/2022).
- AIDS United, 2020. Breaking Down Barriers to Syringe Access by Meeting People Where They Are: implementing Syringe Vending in Your Community. https://www.youtube.com/watch?v=3KcG89niikQ&t=5s. (Accessed Feburary 11, 2022).
- Legislative Analysis and Public Analysis Association, 2020. Naloxone Access: summary of State Laws. https://legislativeanalysis.org/wp-content/uploads/2020/10/Naloxone-summary-of-state-laws-FINAL-9.25.2020.pdf. (Accessed February 1, 2022).
- Liebling E.J., Yedinak J.L., Green T.C., Hadland S.E., Clark M.A., Marshall B.D. Access to substance use treatment among young adults who use prescription opioids non-medically. Subst. Abuse Treat. Prev. Policy. 2016;11(1):1–12. doi: 10.1186/s13011-016-0082-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lozo K.W., Nelson L.S., Ramdin C., Calello D.P. Naloxone deserts in NJ cities: sociodemographic factors which may impact retail pharmacy naloxone availability. J. Med. Toxicol. 2019;15(2):108–111. doi: 10.1007/s13181-019-00700-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall B.D., Green T.C., Yedinak J.L., Hadland S.E. Harm reduction for young people who use prescription opioids extra-medically: obstacles and opportunities. Int. J. Drug Policy. 2016;31:25–31. doi: 10.1016/j.drugpo.2016.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAuley A., Aucott L., Matheson C. Exploring the life-saving potential of naloxone: a systematic review and descriptive meta-analysis of take home naloxone (THN) programmes for opioid users. Int. J. Drug Policy. 2015;26(12):1183–1188. doi: 10.1016/j.drugpo.2015.09.011. [DOI] [PubMed] [Google Scholar]
- McDonald D. The evaluation of a trial of syringe vending machines in Canberra. Int. J. Drug Policy. 2009;20(4):336–339. doi: 10.1016/j.drugpo.2008.06.004. [DOI] [PubMed] [Google Scholar]
- McDonald R., Strang J. Are take-home naloxone programmes effective? Systematic review utilizing application of the Bradford Hill criteria. Addiction. 2016;111(7):1177–1187. doi: 10.1111/add.13326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olfson M., Wall M., Barry C.L., Mauro C., Mojtabai R. Effects of the Affordable Care Act on private insurance coverage and treatment of behavioral health conditions in young adults. Am. J. Public Health. 2018;108(10):1352–1354. doi: 10.2105/AJPH.2018.304574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otiashvili D., Kirtadze I., Mgebrishvili T., Beselia A., Tabatadze M., Vardanashvili I., Ober A.J. Implementation and evaluation of a syringe vending machine trial in Tbilisi. Int. J. Drug Policy. 2022;103 doi: 10.1016/j.drugpo.2022.103649. [DOI] [PubMed] [Google Scholar]
- Priester M.A., Browne T., Iachini A., Clone S., DeHart D., Seay K.D. Treatment access barriers and disparities among individuals with co-occurring mental health and substance use disorders: an integrative literature review. J. Subst. Abuse. 2016;61:47–59. doi: 10.1016/j.jsat.2015.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders B., Sim J., Kingstone T., Baker S., Waterfield J., Bartlam B., Burroughs H., Jinks C. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual. Quant. 2018;52(4):1893–1907. doi: 10.1007/s11135-017-0574-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavova S., Rock P., Bush H.M., Quesinberry D., Walsh S.L. Signal of increased opioid overdose during COVID-19 from emergency medical services data. Drug. Alcohol Depend. 2020;214 doi: 10.1016/j.drugalcdep.2020.108176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stockings E., Hall W.D., Lynskey M., Morley K.I., Reavley N., Strang J., Patton G., Degenhardt L. Prevention, early intervention, harm reduction, and treatment of substance use in young people. Lancet Psychiatry. 2016;3(3):280–296. doi: 10.1016/S2215-0366(16)00002-X. [DOI] [PubMed] [Google Scholar]
- Strang J., Darke S., Hall W., Farrell M., Ali R. Heroin overdose: the case for take-home naloxone. Br. Med. J. Publish. Gr. 1996:1435–1436. doi: 10.1136/bmj.312.7044.1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroud C., Walker L.R., Davis M., Irwin C.E., Jr Investing in the health and well-being of young adults. J. Adolesc. Health. 2015;56(2):127–129. doi: 10.1016/j.jadohealth.2014.11.012. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration Key Substance Use and Mental Health Indicators in the United States: Results from the 2019 National Survey On Drug Use and Health. 2020 [Google Scholar]
- Tong A., Sainsbury P., Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care. 2007;19(6):349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- Van Boekel L.C., Brouwers E.P., Van Weeghel J., Garretsen H.F. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend. 2013;131(1–2):23–35. doi: 10.1016/j.drugalcdep.2013.02.018. [DOI] [PubMed] [Google Scholar]
- Weiner J., Murphy S.M., Behrends C. Expanding access to naloxone: a review of distribution strategies. Issue Brief. 2019;23:132. [Google Scholar]
- Wermeling D.P. A response to the opioid overdose epidemic: naloxone nasal spray. Drug Deliv Transl Res. 2013;3(1):63–74. doi: 10.1007/s13346-012-0092-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wermeling D.P. Review of naloxone safety for opioid overdose: practical considerations for new technology and expanded public access. Ther. Adv. Drug. Saf. 2015;6(1):20–31. doi: 10.1177/2042098614564776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson N., Kariisa M., Seth P., Smith H.t., Davis N.L. Drug and opioid-involved overdose deaths - United States, 2017-2018. MMWR Morb. Mortal. Wkly. Rep. 2020;69(11):290–297. doi: 10.15585/mmwr.mm6911a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang C., Favaro J., Meacham M.C. NEXT harm reduction: an online, mail-based naloxone distribution and harm-reduction program. Am. J. Public Health. 2021;111(4):667–671. doi: 10.2105/AJPH.2020.306124. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.