Case description
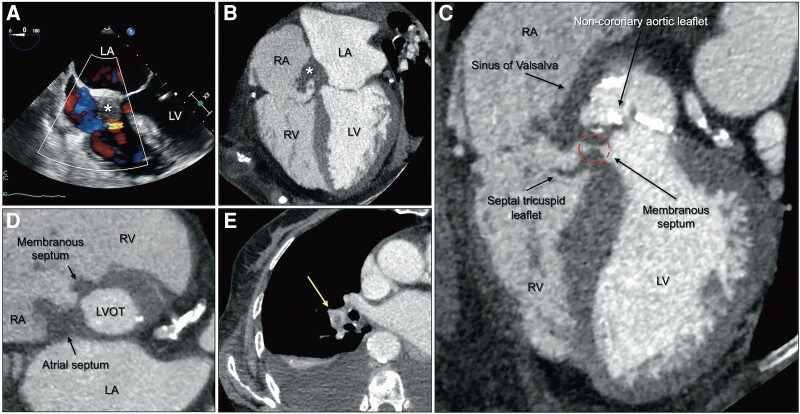
An 87-year-old woman was referred to our institution because of fever and general fatigue. Several separate blood cultures were positive for Streptococcus anginosus. Electrocardiography showed a complete atrioventricular block. Transthoracic echocardiography suspected mass-like thickening in the right atrium (RA) in contact with the atrial septum (see Supplementary material online, Figure S1). Transoesophageal echocardiography showed mass-like thickening in the RA in contact with the atrial septum, similar to transthoracic echocardiography findings. A systolic colour jet towards the RA from the left ventricle (LV) was observed, suggestive of communication. However, it was difficult to identify the shunt site (Figure 1A, Supplementary material online, Video S1). Electrocardiogram-gated contrast-enhanced computed tomography revealed a mass-like thickened wall of the non-coronary aortic sinus of Valsalva, the atrial septum, and the membranous septum. Non-coronary aortic leaflet thickening and communication between the LV outflow tract, below the non-coronary aortic sinus, and the RA, above the septal tricuspid leaflet, were observed, suggesting a Gerbode defect (Figure 1B–D). Moreover, an embolus was observed in the right pulmonary artery (Figure 1E). Unfortunately, the patient did not wish to undergo surgical treatment and suddenly had cardiac arrest from a long pause despite antibiotic therapy.
Figure 1.
Four-chamber images of transoesophageal echocardiography (A) and electrocardiogram-gated contrast-enhanced computed tomography (B) showed mass-like thickening in the right atrium in contact with the atrial septum (*). A colour jet towards the right atrium from the left ventricle was observed, suspecting communication among them. (C) Oblique four-chamber image of electrocardiogram-gated contrast-enhanced computed tomography revealed a mass-like thickened wall of the non-coronary aortic sinus of Valsalva and the membranous septum, thickening of the non-coronary aortic leaflet, and communication between the left ventricular outflow tract below the non-coronary aortic sinus and the right atrium above the septal tricuspid leaflet, which was consistent with a Gerbode defect (dashed circle). (D) Short-axis image of the virtual basal ring plane showed a mass-like thickened wall of the atrial septum and membranous septum. (E) An embolus was observed in the right pulmonary artery (arrow). LA, left atrium; LV, left ventricle; LVOT, left ventricular outflow tract; RA, right atrium; RV, right ventricle.
The Gerbode defect is a rare abnormal communication between the LV and the RA; an unusual type of ventricular septal defect that can be congenital or acquired. Acquired Gerbode defect can be secondary to cardiac surgery, myocardial infarction, trauma, or endocarditis.1 Anatomically, the defect was classified into Types I (below the tricuspid valve, indirect LV–RA defect), II (above the tricuspid valve, direct LV–RA defect), and III (combination of Types I and II).2 Here, the Gerbode defect was considered as Type II (direct LV–RA defect), caused by endocarditis. Inflammation of the membranous septum could have caused the complete atrioventricular block, with extension to the RA through the Gerbode defect, forming vegetations. These may have torn off, causing a pulmonary embolism. Computed tomography could add precise information regarding shunt site detection and identify septic emboli in the pulmonary bed.3
Supplementary Material
Acknowledgement
The authors thank Yuko Yoshigai, Yoshihiro Saito, Hiromi Toki, and Tsuyoshi Osue for helpful discussions.
Contributor Information
Masataka Suzuki, Department of Cardiology, Kobe City Nishi-Kobe Medical Center, 5-7-1 Kojidai, Nishi-ku, Kobe, Hyogo 651-2273, Japan.
Hiromi Hashimura, Department of Radiology, Kobe University Graduate School of Medicine, Kobe, Japan.
Junya Ejiri, Department of Cardiology, Kobe City Nishi-Kobe Medical Center, 5-7-1 Kojidai, Nishi-ku, Kobe, Hyogo 651-2273, Japan.
Hiroshi Eizawa, Department of Cardiology, Kobe City Nishi-Kobe Medical Center, 5-7-1 Kojidai, Nishi-ku, Kobe, Hyogo 651-2273, Japan.
Supplementary material
Supplementary material is available at European Heart Journal – Case Reports.
Consent: The authors confirm that written consent for submission and publication of this case report including images has been obtained from the patient in line with COPE guidance.
Funding: None declared.
References
- 1. Yuan SM. A systematic review of acquired left ventricle to right atrium shunts (Gerbode defects). Hellenic J Cardiol 2015;56:357–372. [PubMed] [Google Scholar]
- 2. Yuan SM. Left ventricular to right atrial shunt (Gerbode defect): congenital versus acquired. Postepy Kardiol Interwencyjnej 2014;10:185–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Habib G, Lancellotti P, Antunes MJ, Bongiorni MG, Casalta JP, Del Zotti F, et al. 2015 ESC guidelines for the management of infective endocarditis. Eur Heart J 2015;36:3075–3123.26320109 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.