Abstract
Plaque rupture is the most common cause of acute coronary syndromes and sudden cardiac death. Characteristics and pathobiology of vulnerable plaques prone to plaque rupture have been studied extensively over two decades in humans using optical coherence tomography (OCT), an intravascular imaging technique with micron scale resolution. OCT studies have identified key features of plaque vulnerability and described the in vivo characteristics and spatial distribution of thin cap fibroatheromas as major precursors to plaque rupture. In addition, OCT data supports the evolving understanding of coronary heart disease as a panvascular process associated with inflammation. In the setting of high atherosclerotic burden, plaque ruptures often occur at multiple sites in the coronary arteries and plaque progression and healing are dynamic processes modulated by systemic risk factors. This review details major investigations with intravascular OCT into the biology and clinical implications of plaque vulnerability and plaque rupture.
Condensed Abstract
Characteristics and pathobiology of vulnerable plaques prone to plaque rupture have been studied extensively over two decades in humans using intravascular optical coherence tomography (OCT). OCT provided an opportunity to study the in vivo characteristics and spatial distribution of thin cap fibroatheromas as major precursors to plaque rupture. In addition, OCT data supports the evolving understanding of coronary heart disease as a dynamic, panvascular process associated with inflammation. This review details major investigations with intravascular OCT into the biology and clinical implications of plaque vulnerability and plaque rupture.
Introduction
A tremendous worldwide burden of atherosclerotic coronary artery disease has driven intense efforts over decades to understand the causal chain of events leading to acute myocardial infarction and cardiac death. From pathology studies arose the concept of the vulnerable plaque, which is prone to acute rupture of a thin fibrous cap and release of a necrotic lipid core into the lumen, prompting ignition of coagulation and abrupt narrowing or closure of the vessel with thrombus. Now validated from many viewpoints – pathology, intravascular imaging, and noninvasive imaging - plaque rupture remains the most commonly identified cause of acute coronary syndrome (ACS), and the thin cap fibrous atheroma (TCFA) its most notorious precursor. It is now appreciated that the atherosclerosis that plagues the coronary vascular tree is a highly dynamic process modulated by multiple systemic risk factors, and that individual coronary plaques may progress or regress at different rates in different patients. Furthermore, plaque ruptures are more common than previously thought, and most do not lead to ACS. Intravascular optical coherence tomography (OCT) has made possible the visualization of coronary artery microstructure at unprecedented resolution. This review details investigations of the biology of plaque rupture and plaque vulnerability with OCT over the last 20 years. Investigations with OCT have also contributed significantly to understanding the biology of plaque erosion and calcified culprit plaque in ACS, the development of layered plaques, and the role of endothelial shear stress in plaque progression and destabilization. These topics will be addressed in separate articles.
Invention of Cardiac OCT and Evolution of the Technology
OCT was developed in 1991 by Professor James Fujimoto and colleagues at the Massachusetts Institute of Technology (MIT) (1). The promise for profiling coronary artery pathology with OCT was evident from the beginning and led to early in vitro (2) and animal studies (3). In 1998, two scientists from the Fujimoto group (Brett Bouma and Guillermo Tearney) joined Ik-Kyung Jang at the Massachusetts General Hospital (MGH) to establish the “MGH Cardiac OCT Group.” After 2 years of careful bench work and preclinical experiments, the team produced a clinically viable catheter-based OCT system at the MGH Wellman Center for Photomedicine. In 2000, Jang and colleagues performed the first-in-man (FIM) study using the custom-built MGH OCT console and OCT catheters (Figure 1). The catheters were built at MGH by replacing the core of a commercial intravascular ultrasound (IVUS) catheter with an optical fiber. This prototype OCT console was heavy and bulky, and required adjustment of various parameters after each image acquisition. Nonetheless, all 10 patients completed the procedure without complication, and in 2002 Jang et al. published the experience of the FIM study in the Journal of the American College of Cardiology (Figure 2) (4). In 2005, the first in vivo characterization of culprit plaque in relation to clinical presentation was subsequently reported (5).
Figure 1:
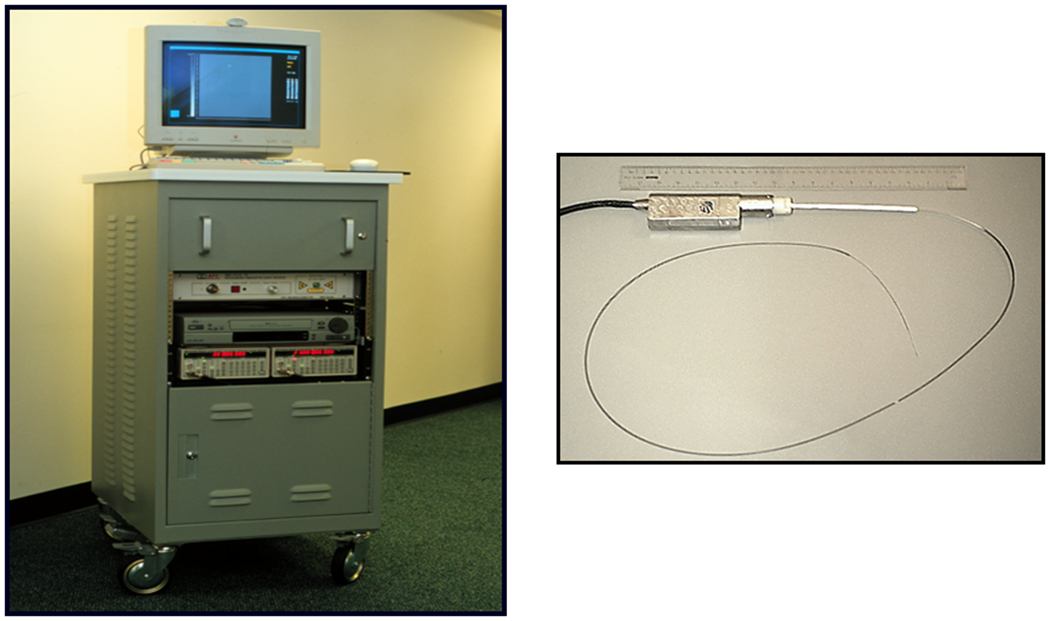
Prototype OCT system and a catheter built at MGH in 2002.
Figure 2:

A. First in vivo comparison of OCT and IVUS (4). An eccentric fibrous plaque is seen at 9 o’clock. B. Post-thrombolysis angiogram and the first OCT demonstration of a ruptured thin fibrous cap (arrows), lipid-rich plaque (L), and residual thrombus (T).
In 2006, high speed frequency domain (FD) OCT was introduced, which revolutionized intracoronary imaging. Unlike the first-generation time-domain OCT, FD-OCT was user friendly, eliminating multiple steps that were required for the first generation TD-OCT. In addition, the image quality was significantly improved. Finally, in 2010, the United States FDA approved this new diagnostic imaging modality for clinical use. In the same year, the MGH OCT Registry, which currently houses approximately 2700 patients’ data, was launched. Data were collected at 21 sites from 6 countries around the world, and Professors James Fujimoto and Valentin Fuster have served as supervisors for the past 20 years. This data set has been a rich source for teaching and research.
OCT can detect features of TCFA, plaque vulnerability, and plaque rupture
In 2002, Yabushita et al. published OCT imaging features from 357 autopsy specimens correlated with histology for three major plaque types: fibrous, fibrocalcific, and lipid-rich (6). The study demonstrated high sensitivity (0.87 – 0.95) and specificity (0.94 – 1.0) for distinguishing between plaque types. Lipid-rich plaques were defined by signal-poor regions with diffuse borders in contrast to the homogeneous signal-rich layers of a fibrous plaque. Subsequent investigations further defined OCT metrics for plaque vulnerability. From prior autopsy studies, a vulnerable plaque was defined as possessing 1) a thin fibrous cap (<65 um), 2) a large lipid pool, and 3) activated macrophages near the fibrous cap (7–10). Tearney et al. demonstrated that high standard deviation of OCT signal (heterogeneous signal) in the fibrous cap correlated with macrophage density, enabling quantification of macrophages (11). Additional plaque characteristics including calcific nodules and presence and type of thrombus (white vs. red) were also defined (6). Jang et al. used these OCT features to characterize culprit plaques in vivo in 57 patients, demonstrating that patients presenting with ST-elevation myocardial infarction (STEMI) compared with non-ST elevation MI / unstable angina (NSTEMI/UA) or stable angina (SAP) had higher prevalence of TCFA (Table) (5). Standard characterization of lipid plaque with OCT now typically includes measurement of lipid core arc, lipid core length, fibrous cap integrity and thickness, as well as presence of macrophages, calcification, thrombus, microvessels, and cholesterol crystals (Central Illustration).
Table.
Comparison of culprit plaque phenotype between AMI, ACS, and SAP (5)
| AMI (n=20) | ACS (n=20) | SAP (n=17) | P value | |
|---|---|---|---|---|
| Lipid-rich plaque | 90% | 75% | 58% | 0.09 |
| FCT, μm | 47 | 53.8 | 102.6 | 0.03 |
| TCFA | 72% | 50% | 20% | 0.01 |
AMI: acute myocardial infarction, ACS: acute coronary syndromes, SAP: stable angina pectoris, FCT: fibrous cap thickness, TCFA: thin cap fibroatheroma
Central Illustration: OCT Imaging of TCFA and Plaque Rupture.

OCT identifies features of plaque vulnerability at high resolution including A) TCFA (yellow arrows) B) Macrophage present in the fibrous cap (red arrows), C) thrombus (yellow *), and D) microchannels indicating neovascularization (green arrows). Plaque rupture (E) is visualized on OCT with a disrupted fibrous cap (red arrow) and plaque cavity (red *). F) Plaque rupture culprit lesions in STEMI have high frequency of lipid plaque and TCFA, microchannels, and positive remodeling. Data reproduced from (19). G) Spatial distribution of TCFA indicates clustering of lesions in the proximal aspects of the LAD and LCx and a two peak distribution in the RCA. Figure modified from (23).
Characteristics of TCFA and Plaque Rupture
Early studies established that OCT can identify TCFA and plaque rupture with superior resolution compared to intravascular ultrasound (IVUS) and other modalities (5,12,13), which fueled new investigations into plaque rupture biology. The role of inflammation in plaque stability has been extensively explored. MacNeill et al. showed that sites of plaque rupture had greater macrophage density compared with non-ruptured sites in patients presenting with coronary disease (14). In a separate study, baseline white blood cell (WBC) count and macrophage density were studied in patients presenting with ACS or stable angina pectoris (15). WBC count correlated with fibrous cap macrophage density, and both WBC and macrophage density correlated inversely with plaque fibrous cap thickness. Intraplaque neovascularization seen as plaque microchannels has also been associated with other features of plaque vulnerability and TCFA (16). In patients with unstable angina, culprit lesions with evidence of neovascularization had higher incidence of TCFA, thinner fibrous cap, and longer lipid core compared to those without neovascularization.
Two studies utilizing multi-modality imaging with OCT and IVUS provide in vivo insight into the association between plaque vulnerability and plaque remodeling. Positive remodeling of a plaque was more commonly associated with lipid-rich plaque, a thin fibrous cap, the presence of TCFA, and a higher fibrous cap macrophage density (17). In a larger study of 3-vessel coronary imaging with OCT, IVUS, and angiography, Tian et al looked at features of plaque vulnerability at different degrees of stenosis and found that the relative prevalence of TCFA was higher in the severe stenosis group (18).
At autopsy, plaque rupture is the most frequent finding in patients with sudden cardiac death, but it has long been recognized that it is not the only culprit mechanism of ACS (9,10) . In 2013, our group determined the relative prevalence of plaque rupture, plaque erosion, and calcified nodule using OCT in patients presenting with ACS. Plaque rupture was the culprit in 43.7% of cases, followed by plaque erosion in 31.0% and calcified nodule in 7.9%. Patients with plaque rupture more frequently presented with STEMI and more severe underlying lesion stenosis and more frequently had TCFA and white thrombus. A follow up study looked at the underlying mechanisms in STEMI with OCT and IVUS (19). In this cohort, plaque rupture was present at the culprit lesion in 64.8% of patients. Lesions with plaque rupture had more TCFA, higher plaque burden, and higher remodeling index compared with erosion or calcified nodule. Two subsequent studies by Niccoli et al. (20) and by Yonetsu et al. (21) have investigated the prognosis of plaque rupture compared to plaque erosion and shown that major adverse cardiac events occur more frequently in patients with plaque rupture.
Prevalence, Frequency and Distribution of TCFA and Plaque Ruptures
Autopsy investigations showed that TCFA and plaque rupture predominantly occur in the proximal portions of the three major epicardial vessels, with the proximal left anterior descending (LAD) coronary artery the most common location (9,22). Araki et al. utilized 3-vessel OCT to perform comprehensive mapping of vulnerable plaque frequency and distributions (23). Plaques were classified into fibrous plaque (FP), fibrocalcific plaque (FCP), thin cap fibroatheromas (TCFA) or thick cap fibroatheromas (ThCFA). Of 534 plaques analyzed, 27% were FPs, 13.3% were FCPs, 40.8% were ThCFAs, and 18.9% were TCFAs. TCFAs made up 20.6% of plaques in the right coronary artery (RCA), 19.2% of plaques in the left circumflex artery (LCx), and 16.8% of plaques in the LAD. Prevalence of TCFA as a function of spatial segments analyzed was 6.7% in the RCA, 7.0% in the LAD, and 5.3% in the LCx. TCFAs showed clustering in the proximal segment of the arteries, particularly in the LAD. Notably, in patients with ACS compared to those without ACS, TCFAs showed stronger proximal clustering in the LAD, two distinct peaks of clustering in the RCA, and one peak of clustering in the proximal-mid LCx (Central Illustration). The presence of rupture was significantly higher in the LAD in the proximal segments as well. Finally, Araki and colleagues compared the degree of stenosis and features of plaque vulnerability. Prevalence of TCFA as well as macrophages, microvessels, cholesterol crystals, and plaque rupture were all significantly highest in the tertile of greatest stenosis (>70.6%).
Nonculprit lesions and pan-vascular vulnerability
The emphasis on detection of individual vulnerable plaques has given way over the past two decades to an understanding of atherosclerosis and risk as a systemic or pan-coronary process (24–26). Early investigations proposing widespread coronary inflammation (27,28) were strengthened by imaging reports demonstrating multiple vulnerable plaques and plaque ruptures in vivo (29,30). Several OCT investigations have further contributed to the concept of pan-vascular vulnerability. The work of MacNeill et al. (14) showed that macrophage densities in plaque fibrous caps correlated significantly between culprit and non-culprit lesions within the same patient. Moreover, there was not a significant difference in macrophage content between remote and culprit sites for each clinical presentation group (STEMI, NSTEMI/UA, or SAP) studied, but there was greater macrophage density in acute compared to stable clinical syndromes. Kato et al. further investigated nonculprit plaques in acute coronary syndromes using 3-vessel OCT (31). Imaging of 248 nonculprit plaques revealed that non-culprit lesions in ACS had a wider lipid arc, longer lipid length, and thinner fibrous cap compared to non-ACS presentations. Additionally, TCFA, macrophage, and thrombus were more frequent in nonculprit plaques in ACS, all of which are consistent with increased vulnerability of remote plaques in acute coronary syndrome presentations. Tian et al. then compared features of ruptured culprit plaques (RCP) with ruptured nonculprit plaques (RNCP) and TCFA lesions in patients with ACS using 3-vessel OCT and IVUS (18). RCP had greater plaque burden and smaller lumen area compared with RNCP and TCFA, and fibrous cap thickness of < 52 um distinguished ruptured plaques from TCFA (AUC 0.857, p<0.001).
The study of Vergallo et al. defined the prevalence and predictors of multiple coronary plaque ruptures (32). Using 3-vessel OCT, the investigators found non-culprit plaque rupture in 20% of all patients, including those with stable symptoms, and multiple plaque ruptures in 20% of these patients. TCFA was more prevalent in patients with nonculprit plaque ruptures and the presence of TCFA, intimal vasculature, and macrophages were independent morphological predictors of multiple plaque ruptures. Compared with culprit plaque ruptures, nonculprit ruptures demonstrated smaller lipid arc, shorter lipid length, and greater minimum fibrous cap thickness. The nonculprit ruptures also had significantly smaller ruptured cavity area, lower frequency of adherent thrombus, and less frequent white thrombus compared to culprit plaque ruptures. Notably nonculprit plaque ruptures had overlying thrombus in most patients with AMI but only a minority of those with UAP or SAP, suggesting a hypercoagulable state. Additionally, patients with nonculprit plaque rupture had a significantly higher prevalence overall of fibroatheromas and TCFA compared to those without nonculprit ruptures.
Evolution and progression of TCFA and plaque rupture
Pathology (22,33), IVUS (29,34), and OCT data (18,32) demonstrate that many plaque ruptures do not lead to clinical events. The PROSPECT trial (35) sought to define the natural history of coronary lesions in patients presenting with ACS using serial angiography and IVUS. The cumulative rate of major adverse cardiovascular events over 3 years was 20.4%, of which 11.6% were due to nonculprit lesions. Arbab-Zadeh and Fuster have pointed out that overall risk of MI or sudden death due to the nonculprit lesions in PROSPECT cohort was low though, and they have suggested that it is not practical to consider the vulnerable plaque as a target for detection and intervention (24,25). Rather a focus should be placed on mitigating risk factors and evaluating atherosclerotic burden as a metric of risk for the patient. Serial imaging studies from Kubo et al. using virtual histology IVUS further highlight a complex and dynamic evolution of individual nonculprit TCFAs, with most TCFAs healing over 12 months and new TCFAs developing (34).
Xing et al. have explored the natural history of lipid-rich plaque using OCT over a 4-year follow up. Nearly 1500 patients from 20 international sites that had target vessel OCT imaging were followed for major adverse cardiac events (36). Nonculprit lipid-rich plaque in the target vessel was present in 33.6% of patients and was independently associated with MACE at nonculprit sites, though the MACE was predominantly driven by revascularization for recurrent ischemia.
Recent OCT insights into plaque progression and healing have helped to further understand the natural history of plaque rupture. Xie et al. showed using one time OCT and serial IVUS out to 12 months that 77% of lesions do not progress while two-thirds of those that do progress have a rapid, phasic pattern compared to a more gradual pattern in the remaining third (37). Fracassi et al. then looked at culprit-vessel OCT in 376 patients with ACS (38). In these patients, healed plaques, defined as layered plaques on OCT, were seen at 28.7% of culprit lesions. Hyperlipidemia, diabetes, and prior history of MI were more frequent in patients with healed plaques, as were overt plaque rupture, TCFA, macrophage accumulation, and greater area stenosis. These results provide a window into past subclinical events and suggest again a dynamic environment of plaque destabilization and healing taking place. Recent studies by Russo et. al looking at healed plaques in patients with stable angina(39) and acute coronary syndromes(40) further support this picture of subclinical rupture and healing contributing to plaque vulnerability. Layered plaques, as well as lipid-rich plaques and TCFA were shown by Araki et al. to be predictors of subsequent rapid plaque progression (41). Step-wise rapid progression is hypothesized to contribute to ACS and sudden death, as opposed to slow linear progression associated with stable angina.
Limitations of Cardiac OCT
With the advent of high-speed frequency domain OCT, the need for balloon occlusion or prolonged saline flush of the coronary artery has been eliminated. Nonetheless, OCT imaging does still have the limitation of requiring brief contrast or dextran flush of the artery similar to the injection needed for an angiogram loop. In addition, the need to clear blood from the lumen limits the ability to examine ostial lesions, and the catheter diameter (2.7-F in modern systems) limits the ability to image the most distal aspects of the artery. Nonetheless, OCT is capable of mapping plaque features over the proximal 8-10 cm of all three vessels (23), which covers the sites of the majority of culprit lesions. Imaging depth also remains a limitation of OCT when compared to IVUS, which restricts the ability to image underlying plaque features in arteries with heavy thrombus burden. Studies have utilized aspiration thrombectomy to successfully image the underlying plaque features in occlusive thrombotic lesions before PCI. Future technology advances with OCT may circumvent some of these limitations, but they also highlight a role for use of multi-modality approaches to image the coronaries and to leverage strengths of other imaging methods.
Conclusions and Future Directions
OCT has enabled plaque characterization at an unprecedented resolution in vivo and has therefore offered a unique window into the complex, dynamic biology of coronary atherosclerosis in humans. The following general conclusions on plaque rupture and plaque vulnerability are supported by published OCT studies and represent key take-home points:
Plaque rupture is the most common cause of ACS, including STEMI and NSTEMI/UA.
Features of plaque vulnerability including large lipid pool, thin fibrous cap, fibrous cap macrophage density, and plaque neovascularization are associated with culprit lesions.
OCT features of vulnerable plaque and TCFA are more prevalent in lesions with greater plaque burden and higher degree of stenosis.
TCFAs cluster in the proximal segments of coronary arteries particularly in patients presenting with ACS.
Coronary atherosclerosis is a panvascular process and plaque rupture is associated with panvascular inflammation.
Nonculprit plaque ruptures are common in patients presenting with ACS and even with stable symptoms.
Healed plaque ruptures are frequently present at the culprit site in ACS and are risk factors for rapid progression of atherosclerosis.
Intravascular OCT imaging will continue to be a powerful tool for in vivo plaque characterization in the years ahead. As new biological and clinical insights on plaque rupture emerge, investigators can turn to OCT for microscopic validation of new hypotheses. Identifying patients with highly active, progressive atherosclerosis vs. those with rather inert disease will continue to be a very active field of investigation. OCT should be particularly promising for investigating new pharmacotherapies at the plaque level.
Highlights.
OCT confirms plaque rupture as the most common cause of ACS in vivo.
OCT features of plaque vulnerability including TCFA are more prevalent in lesions with greater plaque burden and higher degree of stenosis.
ACS is a panvascular process with a local manifestation.
Funding:
Dr. Jang’s research was supported by the Allan Gray Fellowship Fund and by Mr. and Mrs. Michael and Kathryn Park. Dr. Aguirre’s research has been supported by the National Institutes of Health (R21EB026762, R01HL144515) and the American Heart Association (14FTF20380185).
Disclosures:
Dr. Jang has received educational grants from Abbott Vascular and a consulting fee from Svelte Medical Systems Inc. and Mitobridge Inc. Dr. Aguirre has received research grant funding from Amgen Inc. and Philips Healthcare Inc. Dr. Arbab-Zadeh has received grant support from Canon Medical Systems.
Abbreviations
- ACS
Acute Coronary Syndromes
- LAD
Left Anterior Descending Artery
- LCx
Left Circumflex Artery
- NSTEMI
Non-ST Elevation Myocardial Infarction
- OCT
Optical Coherence Tomography
- RCA
Right Coronary Artery
- STEMI
ST Elevation Myocardial Infarction
- TCFA
Thin Cap Fibroatheroma
References
- 1.Huang D, Swanson EA, Lin CP et al. Optical coherence tomography. Science 1991;254:1178–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brezinski ME, Tearney GJ, Bouma BE et al. Imaging of coronary artery microstructure (in vitro) with optical coherence tomography. Am J Cardiol 1996;77:92–3. [DOI] [PubMed] [Google Scholar]
- 3.Tearney GJ, Jang IK, Kang DH et al. Porcine coronary imaging in vivo by optical coherence tomography. Acta Cardiol 2000;55:233–7. [DOI] [PubMed] [Google Scholar]
- 4.Jang IK, Bouma BE, Kang DH et al. Visualization of coronary atherosclerotic plaques in patients using optical coherence tomography: comparison with intravascular ultrasound. J Am Coll Cardiol 2002;39:604–9. [DOI] [PubMed] [Google Scholar]
- 5.Jang IK, Tearney GJ, MacNeill B et al. In vivo characterization of coronary atherosclerotic plaque by use of optical coherence tomography. Circulation 2005;111:1551–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yabushita H, Bouma BE, Houser SL et al. Characterization of human atherosclerosis by optical coherence tomography. Circulation 2002;106:1640–5. [DOI] [PubMed] [Google Scholar]
- 7.Davies MJ. Detecting vulnerable coronary plaques. Lancet 1996;347:1422–3. [DOI] [PubMed] [Google Scholar]
- 8.Falk E Plaque rupture with severe pre-existing stenosis precipitating coronary thrombosis. Characteristics of coronary atherosclerotic plaques underlying fatal occlusive thrombi. Br Heart J 1983;50:127–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kolodgie FD, Burke AP, Farb A et al. The thin-cap fibroatheroma: a type of vulnerable plaque: the major precursor lesion to acute coronary syndromes. Curr Opin Cardiol 2001;16:285–92. [DOI] [PubMed] [Google Scholar]
- 10.Virmani R, Kolodgie FD, Burke AP, Farb A, Schwartz SM. Lessons from sudden coronary death: a comprehensive morphological classification scheme for atherosclerotic lesions. Arterioscler Thromb Vasc Biol 2000;20:1262–75. [DOI] [PubMed] [Google Scholar]
- 11.Tearney GJ, Yabushita H, Houser SL et al. Quantification of macrophage content in atherosclerotic plaques by optical coherence tomography. Circulation 2003;107:113–9. [DOI] [PubMed] [Google Scholar]
- 12.Kubo T, Imanishi T, Takarada S et al. Assessment of culprit lesion morphology in acute myocardial infarction: ability of optical coherence tomography compared with intravascular ultrasound and coronary angioscopy. J Am Coll Cardiol 2007;50:933–9. [DOI] [PubMed] [Google Scholar]
- 13.Tearney GJ, Jang IK, Bouma BE. Optical coherence tomography for imaging the vulnerable plaque. J Biomed Opt 2006;11:021002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.MacNeill BD, Jang IK, Bouma BE et al. Focal and multi-focal plaque macrophage distributions in patients with acute and stable presentations of coronary artery disease. J Am Coll Cardiol 2004;44:972–9. [DOI] [PubMed] [Google Scholar]
- 15.Raffel OC, Tearney GJ, Gauthier DD, Halpern EF, Bouma BE, Jang IK. Relationship between a systemic inflammatory marker, plaque inflammation, and plaque characteristics determined by intravascular optical coherence tomography. Arterioscler Thromb Vasc Biol 2007;27:1820–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tian J, Hou J, Xing L et al. Significance of intraplaque neovascularisation for vulnerability: optical coherence tomography study. Heart 2012;98:1504–9. [DOI] [PubMed] [Google Scholar]
- 17.Raffel OC, Merchant FM, Tearney GJ et al. In vivo association between positive coronary artery remodelling and coronary plaque characteristics assessed by intravascular optical coherence tomography. Eur Heart J 2008;29:1721–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tian J, Ren X, Vergallo R et al. Distinct morphological features of ruptured culprit plaque for acute coronary events compared to those with silent rupture and thin-cap fibroatheroma: a combined optical coherence tomography and intravascular ultrasound study. J Am Coll Cardiol 2014;63:2209–16. [DOI] [PubMed] [Google Scholar]
- 19.Higuma T, Soeda T, Abe N et al. A Combined Optical Coherence Tomography and Intravascular Ultrasound Study on Plaque Rupture, Plaque Erosion, and Calcified Nodule in Patients With ST-Segment Elevation Myocardial Infarction: Incidence, Morphologic Characteristics, and Outcomes After Percutaneous Coronary Intervention. JACC Cardiovasc Interv 2015;8:1166–1176. [DOI] [PubMed] [Google Scholar]
- 20.Niccoli G, Montone RA, Di Vito L et al. Plaque rupture and intact fibrous cap assessed by optical coherence tomography portend different outcomes in patients with acute coronary syndrome. Eur Heart J 2015;36:1377–84. [DOI] [PubMed] [Google Scholar]
- 21.Yonetsu T, Lee T, Murai T et al. Plaque morphologies and the clinical prognosis of acute coronary syndrome caused by lesions with intact fibrous cap diagnosed by optical coherence tomography. Int J Cardiol 2016;203:766–74. [DOI] [PubMed] [Google Scholar]
- 22.Cheruvu PK, Finn AV, Gardner C et al. Frequency and distribution of thin-cap fibroatheroma and ruptured plaques in human coronary arteries: a pathologic study. J Am Coll Cardiol 2007;50:940–9. [DOI] [PubMed] [Google Scholar]
- 23.Araki M, Soeda T, Kim HO et al. Spatial Distribution of Vulnerable Plaques: Comprehensive In Vivo Coronary Plaque Mapping. JACC Cardiovasc Imaging 2020;13:1989–1999. [DOI] [PubMed] [Google Scholar]
- 24.Arbab-Zadeh A, Fuster V. The myth of the “vulnerable plaque”: transitioning from a focus on individual lesions to atherosclerotic disease burden for coronary artery disease risk assessment. J Am Coll Cardiol 2015;65:846–855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arbab-Zadeh A, Fuster V. From Detecting the Vulnerable Plaque to Managing the Vulnerable Patient: JACC State-of-the-Art Review. J Am Coll Cardiol 2019;74:1582–1593. [DOI] [PubMed] [Google Scholar]
- 26.Choi SY, Mintz GS. What have we learned about plaque rupture in acute coronary syndromes? Curr Cardiol Rep 2010;12:338–43. [DOI] [PubMed] [Google Scholar]
- 27.Mazzone A, De Servi S, Ricevuti G et al. Increased expression of neutrophil and monocyte adhesion molecules in unstable coronary artery disease. Circulation 1993;88:358–63. [DOI] [PubMed] [Google Scholar]
- 28.Buffon A, Biasucci LM, Liuzzo G, D’Onofrio G, Crea F, Maseri A. Widespread coronary inflammation in unstable angina. N Engl J Med 2002;347:5–12. [DOI] [PubMed] [Google Scholar]
- 29.Maehara A, Mintz GS, Bui AB et al. Morphologic and angiographic features of coronary plaque rupture detected by intravascular ultrasound. J Am Coll Cardiol 2002;40:904–10. [DOI] [PubMed] [Google Scholar]
- 30.Mintz GS, Maehara A, Bui AB, Weissman NJ. Multiple versus single coronary plaque ruptures detected by intravascular ultrasound in stable and unstable angina pectoris and in acute myocardial infarction. Am J Cardiol 2003;91:1333–5. [DOI] [PubMed] [Google Scholar]
- 31.Kato K, Yonetsu T, Kim SJ et al. Nonculprit plaques in patients with acute coronary syndromes have more vulnerable features compared with those with non-acute coronary syndromes: a 3-vessel optical coherence tomography study. Circ Cardiovasc Imaging 2012;5:433–40. [DOI] [PubMed] [Google Scholar]
- 32.Vergallo R, Uemura S, Soeda T et al. Prevalence and Predictors of Multiple Coronary Plaque Ruptures: In Vivo 3-Vessel Optical Coherence Tomography Imaging Study. Arterioscler Thromb Vasc Biol 2016;36:2229–2238. [DOI] [PubMed] [Google Scholar]
- 33.Davies MJ, Bland JM, Hangartner JR, Angelini A, Thomas AC. Factors influencing the presence or absence of acute coronary artery thrombi in sudden ischaemic death. Eur Heart J 1989;10:203–8. [DOI] [PubMed] [Google Scholar]
- 34.Kubo T, Maehara A, Mintz GS et al. The dynamic nature of coronary artery lesion morphology assessed by serial virtual histology intravascular ultrasound tissue characterization. J Am Coll Cardiol 2010;55:1590–7. [DOI] [PubMed] [Google Scholar]
- 35.Stone GW, Maehara A, Lansky AJ et al. A prospective natural-history study of coronary atherosclerosis. N Engl J Med 2011;364:226–35. [DOI] [PubMed] [Google Scholar]
- 36.Xing L, Higuma T, Wang Z et al. Clinical Significance of Lipid-Rich Plaque Detected by Optical Coherence Tomography: A 4-Year Follow-Up Study. J Am Coll Cardiol 2017;69:2502–2513. [DOI] [PubMed] [Google Scholar]
- 37.Xie Z, Hou J, Yu H et al. Patterns of coronary plaque progression: phasic versus gradual. A combined optical coherence tomography and intravascular ultrasound study. Coron Artery Dis 2016;27:658–666. [DOI] [PubMed] [Google Scholar]
- 38.Fracassi F, Crea F, Sugiyama T et al. Healed Culprit Plaques in Patients With Acute Coronary Syndromes. J Am Coll Cardiol 2019;73:2253–2263. [DOI] [PubMed] [Google Scholar]
- 39.Russo M, Fracassi F, Kurihara O et al. Healed Plaques in Patients With Stable Angina Pectoris. Arterioscler Thromb Vasc Biol 2020;40:1587–1597. [DOI] [PubMed] [Google Scholar]
- 40.Russo M, Kim HO, Kurihara O et al. Characteristics of non-culprit plaques in acute coronary syndrome patients with layered culprit plaque. Eur Heart J Cardiovasc Imaging 2020;21:1421–1430. [DOI] [PubMed] [Google Scholar]
- 41.Araki M, Yonetsu T, Kurihara O et al. Predictors of Rapid Plaque Progression: An Optical Coherence Tomography Study. JACC Cardiovasc Imaging 2020. [DOI] [PubMed] [Google Scholar]


