The importance of integrated One Health approaches to reduce the likelihood and impacts of emerging infectious disease outbreaks has been widely accepted, as the Lancet series on One Health emphasises.1, 2, 3, 4 However, implementing One Health requires transdisciplinary approaches, with a systemic focus on the health of animals, humans, and ecosystems worldwide, and potential solutions that are equitable, inclusive, and sustainable.
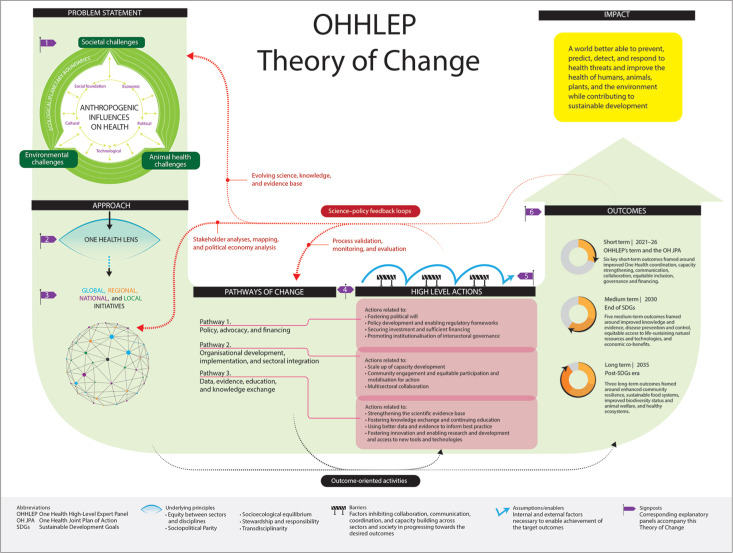
Actions that address the challenges identified in the four papers in this Series1, 2, 3, 4 are also included in the 2022 One Health Theory of Change from the One Health High-Level Expert Panel (OHHLEP).5 Formed in 2021, the OHHLEP advises the Quadripartite of the Food and Agriculture Organization of the United Nations, the UN Environment Programme, WHO, and the World Organisation for Animal Health on more effectively and collaboratively addressing their member states' needs in preventing and preparing for future health emergencies. The OHHLEP's definition and guiding principles of One Health endorsed by the Quadripartite6 have gained rapid global acceptance.7 Subsequently, the Quadripartite launched a One Health Joint Plan of Action with six action tracks,8 which paves the way for enhanced collaboration on communicable and non-communicable disease threats to sustainably optimise and balance the health of humans, animals, and ecosystems.
The One Health Theory of Change identifies more than 60 factors that adversely affect the health of humans, animals, plants, and ecosystems, and advances transdisciplinary approaches to navigate the complex nexus between health, food, water, and energy security and sustainability in a coherent way (figure ).5 Key to this coherence are the guiding principles of One Health, namely equity among sectors and disciplines, sociopolitical and multicultural parity, socioecological equilibrium, stewardship, and transdisciplinarity with multisectoral collaboration.6
Figure.
One Health Theory of Change
This figure is from the One Health High-Level Expert Panel's 2022 One Health Theory of Change.5
© 2023 One Health High-Level Expert Panel, 2022
Coordination, collaboration, communication, and capacity building are the operational dimensions of One Health. Although cross-sectoral coordination mechanisms exist for health emergencies, they do not always include all relevant partners and are usually dismantled after an emergency rather than keeping an integrated approach operational—eg, by addressing endemic disease burden and local health security priorities, including neglected diseases. In line with the first paper in this Lancet Series,1 moving towards an effective One Health operational system would shift disease control upstream, away from an overfocus on surveillance and response in humans, towards increased and proactive investment in preventive interventions, understanding drivers of disease, and integrating surveillance.
This Lancet Series provides options for the implementation of the OHHLEP's three pathways for change, which encompass policy, advocacy, and financing; organisational development, implementation, and sectoral engagement; and data, evidence, education, and knowledge exchange (figure). In relation to financing, as discussed by Azza Elnaiem and colleagues in the fourth Series paper, considering the benefits from a One Health approach versus business as usual is recommended when targeting investments.4 Crucially, there is the opportunity to embed One Health principles in the current negotiations around a global Pandemic Instrument and in guiding the direction of the World Bank-hosted Pandemic Fund.9, 10 A One Health approach is not yet adequately considered in the deliberations for the Pandemic Instrument and Fund, which currently focus primarily on controlling disease spread through early detection and response in humans rather than also tackling upstream drivers of emergence or assessing impacts on other sectors. These global governance and financing instruments should articulate boundaries for spillover prevention in their scope, and acknowledge the gaps in current proposals that require attention from other sectors and potential sources of funding—eg, the World Bank International Development Association funding or the Global Environment Facility. If One Health principles are not embedded in pandemic prevention, preparedness, and response, governments and the global community risk continuing the business-as-usual, siloed models that have failed to reduce the occurrence and impacts of disease outbreaks.
Existing legislation and global governance instruments do not adequately address the drivers of spillover and spread of emerging and endemic diseases. Historically, these instruments lack a synergistic approach to disease prevention, climate action, and biodiversity preservation.4, 11, 12 One immediate legislative activity could be statutory reforms to environmental and social impact assessment processes for land-use change so that they become One Health impact assessments that incorporate emerging infectious disease risks.13, 14 Additionally, to address inequities in access to countermeasures, affected countries could leverage health-related provisions of relevant treaties, such as the UN Convention on Biological Diversity, across the One Health spectrum. This approach could include provisions for sovereignty over biological samples, compulsory licensing of new medicines, or intellectual property waivers. Barriers in access to countermeasures vary depending on countries' health security capacity and capabilities, and One Health thinking can help address these.
The implementation of health security initiatives should be underpinned by ethical considerations including One Health principles.5 For example, the need to engage all relevant stakeholders and ensure that consideration of indigenous, local, and scientific forms of knowledge and perspectives are reflected in those principles, as highlighted in the second Series paper.2, 6 Athman Mwatondo and colleagues identify an opportunity for the One Health movement to help reform global health institutions and processes that were established in the colonial and post-World War 2 era, to better reflect an interconnected and interdependent world through more egalitarian networks and initiatives.2 Such reforms would align with the OHHLEP's second pathway for change, addressing institutional capacity necessary for implementation. This approach could help avoid the problems, notably a widening of inequalities, seen in tackling other global challenges such as climate change and the COVID-19 pandemic, by addressing the socioeconomic determinants of health equitably.15, 16
The One Health Joint Plan of Action monitoring and evaluation framework8 and other global instruments should systematically consider the principles underlying One Health. As Tieble Traore and colleagues propose in the third Series paper, multifaceted models for capacity assessment of health security are needed to monitor and assess outcomes across sectors, including added value, trade-offs, and co-benefits, and to ensure processes adhere to One Health principles.3 When calibrating risk and determining proportionate responses, a more sustainable approach to zoonotic outbreak control should include trade-off analysis of wider impacts on food security, animal health, ecosystems, livelihoods, and the carbon footprint—eg, when mass culling is instituted.
Crucially, improved governance is essential and with it greater accountability and transparency of global health security initiatives globally, regionally, and locally. For intergovernmental organisations, a re-examination of core budgets is required to move away from an overfocus on donor-defined projects and agendas towards adequate attention to locally identified needs and priorities.17 This change will require greater responsibility of donors and all countries to sustainably finance institutions and incentivise collaboration within and across sectors. Currently, the quantity of health security initiatives that receive short-term project funding undermines the utility and sustainability of partnerships.
Global health security is in everyone's interest and now stands at a crossroads. Continue a path plagued by short-termism, siloed working, wide power imbalances, and institutional rivalries. Or, as recommended in this Lancet Series, fully adopt and implement a One Health approach,5 centred around needs-based, evidence-driven interventions, shared values, and an intergenerational vision of health for people, animals, and the planet.
Acknowledgments
CM and VS report travel support from WHO. OD is a lead author of the Lancet One Health Series. The other authors declare no competing interests.
The members of the One Health High-Level Expert Panel are Catherine Machalaba, Wiku B Adisasmito, Salama Almuhairi, Casey Barton Behravesh, Pépé Bilivogui, Salome A Bukachi, Natalia Casas, Natalia Cediel Becerra, Dominique F Charron, Abhishek Chaudhary, Janice R Ciacci Zanella, Andrew A Cunningham, Osman Dar, Nitish Debnath, Baptiste Dungu, Elmoubasher Farag, George F Gao, David T S Hayman, Margaret Khaitsa, Marion P G Koopmans, John S Mackenzie, Wanda Markotter (Co-Chair), Thomas C Mettenleiter (Co-Chair), Serge Morand, Vyacheslav Smolenskiy, and Lei Zhou.
EcoHealth Alliance, New York, NY, USA (CM); Universitas Indonesia, Depok, West Java, Indonesia (WBA); National Emergency Crisis and Disasters Management Authority, Abu Dhabi, United Arab Emirates (SA); Centers for Disease Control and Prevention, Atlanta, GA, USA (CBB); World Health Organization, Guinea Country Office, Conakry, Guinea (PB); Institute of Anthropology, Gender and African Studies, University of Nairobi, Nairobi, Kenya (SAB); National Ministry of Health, Buenos Aires, Argentina (NC); School of Agricultural Sciences, Universidad de La Salle, Bogotá, Colombia (NCB); International Development Research Centre, Ottawa, ON, Canada (DFC); Indian Institute of Technology (IIT), Kanpur, India (AC); Brazilian Agricultural Research Corporation (Embrapa), Embrapa Swine and Poultry, Concórdia, Santa Catarina, Brazil (JRCZ); Institute of Zoology, Zoological Society of London, London, UK (AAC); Global Operations Division, UK Health Security Agency, London, UK (OD); Global Health Programme, Chatham House, Royal Institute of International Affairs, London, UK (OD); Fleming Fund Country Grant to Bangladesh, DAI Global, Dhaka, Bangladesh (ND); Afrivet B M, Pretoria, South Africa (BD); Faculty of Veterinary Science, University of Kinshasa, Kinshasa, Democratic Republic Congo (BD); Ministry of Public Health, Health Protection and Communicable Diseases Division, Doha, Qatar (EF); Chinese Center for Disease Control and Prevention, Beijing, China (GFG, LZ); Molecular Epidemiology and Public Health Laboratory, Massey University, Palmerston North, New Zealand (DTSH); Mississippi State University, Starkville, MS, USA (MK); Erasmus MC, Department of Viroscience, Rotterdam, the Netherlands (MPGK); Faculty of Health Sciences, Curtin University, Perth, WA, Australia (JSM); Centre for Viral Zoonoses, Department of Medical Virology, Faculty of Health Sciences, University of Pretoria, Pretoria, South Africa (WM); Friedrich-Loeffler-Institut, Federal Research Institute for Animal Health, Greifswald-Insel Riems, Germany (TCM); MIVEGEC, CNRS-IRD-Montpellier Université, Montpellier, France (SM); Faculty of Veterinary Technology, Kasetsart University, Bangkok, Thailand (SM); Federal Service for Surveillance on Consumer Rights Protection and Human Well-being (Rospotrebnadzor), Moscow, Russia (VS)
Contributor Information
One Health High-Level Expert Panel:
Wiku B Adisasmito, Salama Almuhairi, Casey Barton Behravesh, Pépé Bilivogui, Salome A Bukachi, Natalia Casas, Natalia Cediel Becerra, Dominique F Charron, Abhishek Chaudhary, Janice R Ciacci Zanella, Andrew A Cunningham, Osman Dar, Nitish Debnath, Baptiste Dungu, Elmoubasher Farag, George F Gao, David T S Hayman, Margaret Khaitsa, Marion P G Koopmans, Catherine Machalaba, John S Mackenzie, Wanda Markotter, Thomas C Mettenleiter, Serge Morand, Vyacheslav Smolenskiy, and Lei Zhou
References
- 1.Zinsstag J, Kaiser-Grolimund A, Heitz-Tokpa K, et al. Advancing One human–animal–environment Health for global health security: what does the evidence say? Lancet. 2023 doi: 10.1016/S0140-6736(22)01595-1. published online Jan 19. [DOI] [PubMed] [Google Scholar]
- 2.Mwatondo A, Rahman-Shepherd A, Hollmann L, et al. A global analysis of One Health Networks and the proliferation of One Health collaborations. Lancet. 2023 doi: 10.1016/S0140-6736(22)01596-3. published online Jan 19. [DOI] [PubMed] [Google Scholar]
- 3.Traore T, Shanks S, Haider N, et al. How prepared is the world? Identifying weaknesses in existing assessment frameworks for global health security through a One Health approach. Lancet. 2023 doi: 10.1016/S0140-6736(22)01589-6. published online Jan 19. [DOI] [PubMed] [Google Scholar]
- 4.Elnaiem A, Mohamed-Ahmed O, Zumla A, et al. Global and regional governance of One Health and implications for global health security. Lancet. 2023 doi: 10.1016/S0140-6736(22)01597-5. published online Jan 19. [DOI] [PubMed] [Google Scholar]
- 5.One Health High Level Expert Panel (OHHLEP) One Health Theory of Change. Nov 7, 2022. https://www.who.int/publications/m/item/one-health-theory-of-change
- 6.One Health High-Level Expert Panel (OHHLEP) Adisasmito WB, Almuhairi S, et al. One Health: a new definition for a sustainable and healthy future. PLoS Pathog. 2022;18 doi: 10.1371/journal.ppat.1010537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lefrançois T, Malvy D, Atlani-Duault L, et al. After 2 years of the COVID-19 pandemic, translating One Health into action is urgent. Lancet. 2022 doi: 10.1016/S0140-6736(22)01840-2. published online Oct 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Food and Agriculture Organization of the United Nations. UN Environment Programme. WHO. World Organisation for Animal Health One Health Joint Plan of Action (2022–2026). Working together for the health of humans, animals, plants and the environment. 2022. https://www.who.int/publications/i/item/9789240059139
- 9.WHO Pandemic prevention, preparedness and response accord. Nov 25, 2022. https://www.who.int/news-room/questions-and-answers/item/pandemic-prevention--preparedness-and-response-accord
- 10.World Bank The Pandemic Fund. 2023. https://www.worldbank.org/en/programs/financial-intermediary-fund-for-pandemic-prevention-preparedness-and-response-ppr-fif
- 11.Dobson AP, Pimm SL, Hannah L, et al. Ecology and economics for pandemic prevention. Science. 2020;369:379–381. doi: 10.1126/science.abc3189. [DOI] [PubMed] [Google Scholar]
- 12.World Bank Putting pandemics behind us: investing in One Health to reduce risks of emerging infectious diseases. 2022. https://documents1.worldbank.org/curated/en/099530010212241754/pdf/P17840200ca7ff098091b7014001a08952e.pdf
- 13.Seifman R, Kornblet S, Standley C, Sorrell E, Fischer J, Katz R. Think big, World Bank: time for a public health safeguard. Lancet Glob Health. 2015;3:e186–e187. doi: 10.1016/S2214-109X(15)70012-4. [DOI] [PubMed] [Google Scholar]
- 14.Keusch GT, Amuasi JH, Anderson DE, et al. Pandemic origins and a One Health approach to preparedness and prevention: solutions based on SARS-CoV-2 and other RNA viruses. Proc Natl Acad Sci USA. 2022;119 doi: 10.1073/pnas.2202871119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ketcham C. How scientists from the “Global South” are sidelined at the IPCC. The Intercept. Nov 17, 2022. https://theintercept.com/2022/11/17/climate-un-ipcc-inequality/
- 16.UN. Inter-agency Task Force on Financing for Development Financing for Sustainable Development Report 2022. 2022. https://www.un.org/ohrlls/content/financing-sustainable-development-report-2022
- 17.WHO . WHO; May 24, 2022. World Health Assembly agrees historic decision to sustainably finance.https://www.who.int/news/item/24-05-2022-world-health-assembly-agrees-historic-decision-to-sustainably-finance-who [Google Scholar]