Abstract
Background
Nonpneumatic antishock garment is one of the newly emerging technology advances that reduce blood loss which is caused by obstetric hemorrhage and help women survive during delays to get definitive care. Over 80% of maternal mortality due to hemorrhagic shock may have been prevented if a nonpneumatic antishock garment had been utilized by an obstetric care provider. However, to the current knowledge, the utilization of nonpneumatic antishock garments is low and even no single study was conducted in the study area. Hence, we found that it is necessary to assess the magnitude and factors affecting the utilization of antishock garments among obstetric care providers in public hospitals of the Sidama region, Ethiopia, 2022.
Methods
A facility-based cross-sectional study design was employed among 403 obstetric care providers from June 15 to July 15, 2022. A two-stage sampling technique was applied; the data was collected by 5 trained BSc midwives using pretested and structured self-administered questionnaires. Data was entered into EpiData Manager version 4.6 and exported to Statistical Package for Social Sciences (SPSS) version 26 software. Bivariate and multivariable logistic regression analyses were used.
Results
A total of 394 (97.8%) health professionals participated in this study. Overall, 30.71% (95% CI: 26.4%, 35%) of the obstetric care providers had utilized nonpneumatic antishock garments for the management of postpartum hemorrhage. Training on the antishock garment (AOR = 4.183, 95% CI: 2.167, 8.075, p < 0.00), tertiary hospital (AOR = 0.355, 95% CI: 0.132, 0.952, p < 0.04), having protocol in the facility (AOR = 2.758, 95% CI: 1.269, 5.996), availability of NASG in the facility (AOR = 4.6, 95% CI: 1.603, 13.24), good knowledge (AOR = 2.506, 95% CI: 1.26, 4.984), and positive attitude (AOR = 2.381, 95% CI: 1.189, 4.766) were significantly associated factors. Conclusion and Recommendation. We found that less than one-third of the study participants have used the antishock garment in the management of postpartum hemorrhage in the current study. In addition to enhancing in-service and ongoing professional development training, it is preferable to insure the availability and accessibility of antishock in the facilities in order to close the knowledge and attitude gap among obstetric care providers.
1. Introduction
A nonpneumatic antishock garment (NASG) is a first aid device that saves the lives of women who are in hypovolemic shock due to any type of obstetric hemorrhage [1]. As one of the most recent technological developments, NASG helps women survive while waiting for definitive therapy by treating hypovolemic shock brought on by hemorrhage and reducing blood loss [2].
The International Federation of Gynecology and Obstetrics (FIGO) recommended utilizing NASG for obstetric hemorrhage as the first aid before any other intervention or to reverse shock when other ways to control bleeding are unsuccessful [3]. Moreover, UNICEF, UNFPA, and WHO all suggest NASG as an immediate solution until women can obtain competent care [4]. The Ethiopian Federal Minister of Health added NASG to the standard treatment protocol for PPH and hypovolemic shock under its 2020 management protocols [5]. The Ethiopian Public Health Institute Public Health Emergency Management Center (PHEM) has recommended nonpneumatic antishock garment (NASG) use and affordability in all hospitals and health centers nationally [6].
The NASG is particularly applicable for use in developing nations due to its simplicity of use and low cost. In cost-effectiveness analyses, NASG has shown to be cost-effective [7]. In Hong Kong, the device costs USD 57.50, and it may be used at least 72 times [3].
Globally, in 2017, over 810 women died every day from pregnancy and childbirth-related causes, with 94 percent of all maternal deaths occurring in developing low- and middle-income countries [4]. Obstetric hemorrhage (OH), which causes around 27.1% of all maternal deaths each year, is the leading cause of death worldwide [8]. Postpartum hemorrhage (PPH) is the most common type of obstetric hemorrhage, accounting for the majority of the 14 million cases reported each year, and 25–28% of maternal mortalities are attributed due to postpartum hemorrhage [9]. Ethiopia has achieved success in reducing maternal mortality in recent decades but still has very high maternal mortality rates: 412 deaths per 100,000 live births [10]. According to the National Maternal Death Surveillance and Response (MDSR) report of Ethiopia, obstetric hemorrhage was the leading cause of reported maternal deaths, accounting for 41.3% of all deaths, and 76% of these deaths were from PPH [6]. In the Southern Nations, Nationalities, and Peoples' Region's Performance Monitoring and Accountability (PMA) report, 38 percent of all women experienced one or more complications during labor or delivery, with severe bleeding being the most common [11].
Using NASG effectively decreased maternal death by 55%, blood loss by 80%, emergency hysterectomy by 4%, and severe significant complications from 12.8% to 4.1 percent, as shown in a global study on maternal survival following PPH at tertiary-level hospitals [12]. As per CHAI data, maternal mortality due to hemorrhagic shock decreased by 80% due to the utilization of NASG between 2013 and 2015 [13].
Unless a woman receives fast and appropriate medical attention, a woman suffering from PPH can die within two hours. Mortality due to PPH is directly related to the duration and amount of bleeding [14]. Women are dying as a result of preventable causes associated with pregnancy and childbirth because the diagnosis of issues and the choice to take a woman to a health facility are frequently delayed and transportation may not be available [15].
Several policy initiatives have been introduced in many developing countries over the past few decades to improve maternal health, but these have not changed the rapidly increasing maternal mortality effectively, and the health system remains weak [16]. The UN Commission on Life-Saving Commodities for Women and Children (UNCoLSC), the Clinton Health Access Initiative (CHAI), the Safe Motherhood Program at the University of California, San Francisco (UCSF), and the Blue Fuzion Group agreed in 2015 to reduce the NASG's costs by 75% to accelerate its scale-up [17].
According to the study done at Jimma zone, 63.8% of health professionals never applied the first aid tool, NASG, for the management of PPH [18]. Ethiopia has the most rapid scale-up of NASG, followed by Nigeria, India, and Zimbabwe, but still, the utilization is low [19]. It has shown a wide range of variation from place to place in Ethiopia, with the highest rate (64.2%) in the northern Ethiopian Tigray region and the lowest in the Jimma zone with a rate of 36.2% [18].
Although there is a low utilization rate of nonpneumatic antishock garments, a few factors including sociodemographic characteristics, facility characteristics, provider knowledge, and attitude have been identified by previous studies [18, 20, 21]. Another significant worry was that even though obstetric care providers knew that NASG was available at their facility, they have not even seen or touched it [22]. It was found necessary to assess the magnitude and identify additional factors responsible for the nonutilization of NASG since the majority of previous studies included only midwives, and in fact, no single study was conducted in the study area to the best of current knowledge. Therefore, this study is aimed at assessing the utilization and associated factors of NASG among obstetric care providers in public hospitals in the Sidama region, Ethiopia, 2022.
2. Methods and Materials
2.1. Study Setting and Period
This study was conducted in selected public hospitals of the Sidama region from June 15, 2022, to July 15, 2022. Sidama National Regional State is one of the 11 regions found in Ethiopia and is located 273 kilometers from Addis Ababa, the capital of the country. It is located in the southern part of the country, and Hawassa city is the administrative city of the region. The region is bordered in the north and east by the Oromia region and in the south and west by Oromia and south regions. According to the 2007 Ethiopian Central statistical agency report estimation, the total population of the region was 4,369,214 [23]. According to the unpublished regional health bureau report of 2021, the region has a tertiary hospital, 5 general hospitals, 14 primary hospitals, 137 health centers, and 553 health posts.
Regarding human resources for health reports, 712 obstetric care providers are working in public hospitals in the Sidama region and 435 of them are midwives.
2.2. Study Design
A facility-based cross-sectional study design was employed.
2.3. Source and Study Population
2.3.1. Source Population
The source population was all obstetric care providers working at public hospitals in the Sidama region.
2.3.2. Study Population
The study population was all randomly selected obstetric care providers working at selected public hospitals in the Sidama region.
2.4. Inclusion and Exclusion Criteria
2.4.1. Inclusion Criteria
Inclusion criteria include all obstetric care providers (general practitioners, nurses, midwives, IEOS, and obstetricians) working in the maternity unit of selected hospitals during the time of data collection.
2.4.2. Exclusion Criteria
Exclusion criteria include obstetric care providers on annual and maternity leave at the time of data collection.
2.5. Sample Size Calculation
The sample size was calculated using a single population proportion formula:
| (1) |
where n is the minimum sample size required, Z is 1.96 for the 95% confidence interval, P is from the study conducted in southern zones which on utilization of NASG was found to be 48.5% [21], q = 1 − p, d is the margin of error, and n = (1.96)2∗(0.485∗1 − 0.485)/(0.05)2 = 383.8 ≈ 384.
Then by adding a 5% nonresponse rate, the total sample size was n = 403.
2.6. Sampling Technique and Procedures
A two-stage sampling technique was used. In the first stage, the simple random sampling method was applied to select hospitals. In the Sidama region, there are twenty hospitals in general (14 primary hospitals, 5 general hospitals, and 1 tertiary hospital). Forty percent of hospitals were selected by simple random sampling to get the maximum sample size, and since Hawassa University's comprehensive specialized hospital is the only tertiary hospital in the region, it was selected purposely. According to this, 1 tertiary hospital, 2 general hospitals (Adare and Yirgalem), and 6 primary hospitals (Yirba, Dore, Aleta Wondo, Wondo Genet, Hula, and Yaye) were included in this study. Based on proportional allocation to size, these 403 study subjects were distributed to each facility.
The total number of obstetric care providers in the 9 selected public hospitals was 451, and the total sample size was used to allocate to each public hospital proportionally. Finally, each study's participants were selected from the facility by a simple random sampling technique using a lottery method as shown in Figure 1.
Figure 1.
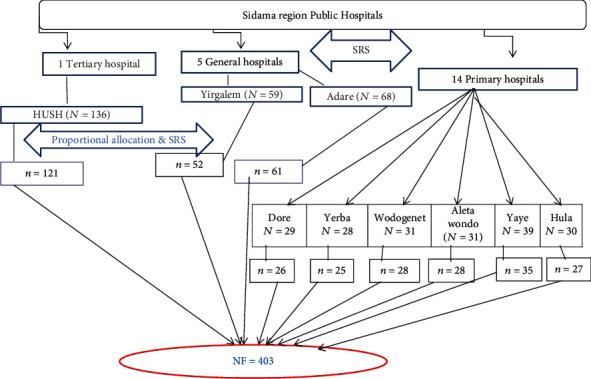
Schematic diagram of the sampling procedure for obstetric care providers of Sidama regional state public hospitals.
2.7. Study Variables
2.7.1. Dependent Variable
The dependent variable is the utilization of NASG.
2.7.2. Independent Variable
The independent variables are sociodemographic data, health system factors, good knowledge of NASG, and positive attitude towards NASG.
2.8. Operational Definitions
2.8.1. Utilization of Nonpneumatic Antishock Garment
Utilization of the nonpneumatic antishock garment is measured based on the response to the question of whether the obstetric care provider used NASG for the management of postpartum hemorrhage at least one time [18, 21, 24].
2.8.2. Knowledge Scale
A total of 10 questions (questions 3, 4, 5, 6, 7, 8, 9, 10, 11, and 12) adapted from previous studies were used to assess the respondents' knowledge. The possible total knowledge score ranged from 0 to 27, and respondents who scored 50% and above (score ≥ 13.5) on 10 knowledge-related questions were graded as having good knowledge [18].
2.8.3. Attitude Scale
The attitude was considered “positive” if the percentage score was 50% and above and “negative” if less than 50% [18, 21].
2.8.4. Experienced Human Power at the Facility
Experienced human power at the facility means having a perception of the presence of healthcare providers trained on NASG in the respective healthcare facility [25].
A self-administered structured questionnaire was used to collect data from study participants. The questionnaire was developed from literature and guidelines considering the study area and situation [18, 20, 21, 25].
The questionnaire was prepared in the English version and contains five parts which include sociodemographic characteristics, facility characteristics, knowledge of nonpneumatic antishock garments, and attitude regarding nonpneumatic antishock garments and respondents' utilization of NASG.
For most of the knowledge items, participants were asked to choose the correct answer based on the nature of the items, and for some questions asked, the response was yes, no, or I do not know.
10 items were used to assess the knowledge of obstetric care providers and to calculate the knowledge score; 1 and 0 points were given to correct and incorrect answers, respectively.
The responses to attitude-related questions consist of five Likert scales: strongly disagree, disagree, neutral, agree, and strongly agree to assess attitude; 1 to 5 points were given.
The attitude statements of five Likert scales for analysis become three Likert scales; for negative statements, responses including agree and strongly agree were labeled as “disagree,” disagree and strongly disagree were labeled as “agree,” and undecided responses were labeled as “neutral responses.” Five BSc midwives having experience in data collection have been recruited and trained in data collection. In addition, the 1 MSc supervisor supervised all activities in the data collection.
2.9. Data Quality Control
Data collectors have provided a daylong training on the data collection tool, and each section of the questionnaire was provided to ensure that both data collectors and supervisors had the correct understanding of the data collection procedure.
Before the actual data collection, the questionnaire was pretested on 5% [20] of the obstetric care providers in the southern region, Durame town public hospital. Based on the findings from the pretest, some ambiguous questions and logical order were corrected. An ongoing formative checkup for completeness and consistency of responses was made by the supervisors daily. Data cleaning and adjustments were conducted to avoid errors in the labeling or order of the variables of interest.
Overall standardized Cronbach's alpha for internal consistency or the reliability score of attitude measurement was 0.83.
2.10. Data Processing and Analysis
After data collection, data were entered into EpiData Manager version 4.6 and exported to Statistical Package for Social Sciences (SPSS) version 26 software for analysis. The outcome variable was utilization; those who utilized NASG were coded as “1,” and those who did not utilize were coded as “0.” In the binary logistic regression, both bivariable and multivariable analyses were carried out. The assumption for binary logistic regression was checked. The Hosmer-Lemeshow statistic was done for model fitness and was not significant (p = 0.698), and the Omnibus test was significant (p value = 0.000) which indicates that the model was fitted. Variables with a p value < 0.25 in the crude analysis were the candidate for multivariable logistic regression, and those with a p value < 0.05 in the multivariable analysis were considered having a statistically significant association.
Multicollinearity was checked to see the linear correlation among the independent variables by using the variance inflation factor and tolerance (t). The variance inflation factor (VIF) for all variables was less than 1.6, and no variable has tolerance (T) < 0.6. The adjusted odds ratio along with 95% CI was estimated to identify factors affecting health professionals' utilization of NASG. Then, simple frequencies, summary measures, tables, and figures were used to present the information.
3. Results
3.1. Sociodemographic Characteristics of the Study Participants
Of the total of 403 eligible participants, 394 participated in this study, with a response rate of 97.8%. The mean age and standard deviation of study participants were 28.44 ± SD 3.737 years. Among the respondents, 232 (58.9%) were male. Nearly 279 (70.5%) of respondents were married. More than half of the respondents, 219 (55.6%), were protestant by religion. Professionally, 346 (87.8%) were midwives. In terms of educational attainment, 281 (71.3%) of respondents had a bachelor's degree and 273 (69.1%) had 1–5 years of clinical work experience as shown in Table 1.
Table 1.
Sociodemographic characteristics of obstetric care providers who participated in the study and worked in public hospitals of Sidama region, Ethiopia, 2022 (N = 394).
| Variables | Category | Frequency | Percentage |
|---|---|---|---|
| Age in years | 20-25 | 94 | 24.1 |
| 25-29 | 159 | 40.4 | |
| 30-35 | 125 | 31.7 | |
| Above 35 | 16 | 3.8 | |
|
| |||
| Sex | Female | 162 | 41.1 |
| Male | 232 | 58.9 | |
|
| |||
| Religion | Protestant | 219 | 55.6 |
| Orthodox | 137 | 34.8 | |
| Muslim | 20 | 5.1 | |
| Catholic | 13 | 3.3 | |
| Other∗ | 5 | 1.3 | |
|
| |||
| Marital status | Single | 110 | 28.2 |
| Married | 279 | 70.5 | |
| Others∗∗ | 5 | 1.3 | |
|
| |||
| Educational level | Diploma | 83 | 21.1 |
| BSc | 281 | 71.3 | |
| Masters and above | 30 | 7.6 | |
|
| |||
| Professional | Midwives | 346 | 87.8 |
| Nurses | 15 | 3.8 | |
| GP | 16 | 4.1 | |
| IEOS | 9 | 2.3 | |
| Obstetrician | 8 | 2.0 | |
|
| |||
| Job experience | 1-5 | 273 | 69.3 |
| 6-10 | 104 | 26.4 | |
| >10 | 17 | 4.3 | |
∗Other = Apostolic, Jehovah's Witness. ∗∗Others = divorced, married but living apart.
3.2. Facility-Related Factors of Obstetric Care Providers in Public Hospitals of Sidama Region, Hawassa, Ethiopia, 2022
Regarding the distribution of participants by their organization, out of the total respondents, 162 (42.0%) of the obstetric care providers were working in primary hospitals. Of the total obstetric care providers, 86 (21.8%) had trained about NASG and 214 (54.3%) of the obstetric care providers had NASG available in their respective facilities, but from these, 105 (76.1%) know the placement of NASG after usage (see Table 2).
Table 2.
Facility-related characteristics of obstetric care providers who participated in the study and worked in public hospitals of Sidama region, Ethiopia, 2022 (N = 394).
| Variables | Category | Frequency | Percentage |
|---|---|---|---|
| Level of the hospital (N = 394) | Primary | 161 | 40.9 |
| General | 113 | 28.7 | |
| Tertiary | 120 | 30.5 | |
|
| |||
| Trained about NASG (N = 394) | Yes | 86 | 21.8 |
| No | 308 | 78.2 | |
|
| |||
| Availability of NASG in a facility (N = 394) | Yes | 214 | 54.3 |
| No | 117 | 29.7 | |
| I do not know | 63 | 16.0 | |
|
| |||
| Number of NASG (N = 214) | One | 132 | 61.7 |
| More than one | 38 | 17.8 | |
| I do not know | 44 | 120.6 | |
|
| |||
| Know the place of NASG (N = 214) | Yes | 138 | 64.5 |
| No | 76 | 33.5 | |
|
| |||
| Place of NASG after usage (N = 138) | Labor ward | 105 | 76.1 |
| Not labor ward | 33 | 23.9 | |
|
| |||
| Organization providing fund (N = 394) | Yes | 78 | 19.8 |
| No | 137 | 34.8 | |
| I do not know | 179 | 45.4 | |
|
| |||
| Protocols for NASG management (N = 394) | Yes | 148 | 36.5 |
| No | 190 | 49.2 | |
| I do not know | 56 | 14.2 | |
|
| |||
| Have wall chart displayed (N = 394) | Yes | 172 | 42.9 |
| No | 201 | 51.8 | |
| I do not know | 21 | 5.3 | |
|
| |||
| Working unit/ward∗ | Labor and delivery | 277 | 70.7 |
| ANC | 51 | 13.0 | |
| FP | 12 | 3.1 | |
| PNC | 32 | 8.2 | |
| Post OP (CS)/OR | 50 | 12.8 | |
| Gyn OPD | 23 | 5.9 | |
|
| |||
| Have experienced staff | Yes | 114 | 28.9 |
| No | 165 | 41.9 | |
| I do not know | 115 | 29.2 | |
|
| |||
| Is NASG part of the PPH protocol before referral? | Yes | 150 | 38.1 |
| No | 213 | 54.1 | |
| I do not know | 31 | 7.8 | |
∗Multiple responses.
3.3. Respondents' Knowledge of Nonpneumatic Antishock Garment
Out of 394 respondents who filled out the questionnaire, 220 (55.8%) obstetric care providers had good knowledge of nonpneumatic antishock garments. This study indicated that 216 (54.6%) of the respondents correctly mentioned that NASG has six parts. Regarding contraindication to the use of NASG, nearly one-third, 253 (72.90%), of the respondents correctly mentioned that NASG should not be applied in the case of a viable fetus. About 136 (64.8%) said that nonpneumatic antishock garments are removed from women when women are awake and stable as shown in Table 3.
Table 3.
Knowledge of respondents who participated in the study and were working in public hospitals of Sidama region, Ethiopia, 2022 (N = 394).
| Variable | Category | Frequency | Percent |
|---|---|---|---|
| Seen the NASG | Yes | 300 | 76.1 |
| No | 94 | 23.9 | |
|
| |||
| NASG looks like (N = 300) | The bottom half of a suit | 245 | 81.7 |
| A gown | 21 | 7.0 | |
| A trouser | 29 | 9.7 | |
| I do not know | 5 | 1.7 | |
|
| |||
| Knew NASG as it is used for preventing complications from PPH | Yes | 378 | 95.9 |
| No | 16 | 4.1 | |
|
| |||
| NASG is made from# | Velcro∗ | 115 | 29.3 |
| Neoprene∗ | 102 | 26.0 | |
| I do not know | 273 | 69.6 | |
|
| |||
| Number of segments of NASG | Nine | 105 | 26.6 |
| Six | 216 | 54.8 | |
| Five | 17 | 4.3 | |
| Four | 15 | 3.8 | |
| I do not know | 41 | 10.6 | |
|
| |||
| Starting segment while applying NASG | Lower or ankle∗ | 262 | 66.5 |
| Abdominal | 88 | 22.3 | |
| I do not know | 44 | 11.2 | |
|
| |||
| Starting segment while removing NASG | Lower or ankle∗ | 244 | 61.9 |
| Abdominal | 99 | 24.9 | |
| I do not know | 52 | 13.2 | |
|
| |||
| Segment adjusted when a woman experiences difficulty breathing with the NASG | Abdominal∗ | 261 | 66.2 |
| Thigh | 60 | 15.2 | |
| Leg | 36 | 9.1 | |
| I do not know | 37 | 9.4 | |
|
| |||
| NASG applied to women having PPH when# | Bleeding > 750 ml∗ | 434 | 115.1 |
| Systolic BP > 90 mm∗ | 162 | 43.0 | |
| Pulse < 110 bpm∗ | 140 | 37.0 | |
| I do not know | 139 | 36.9 | |
| After stabilizing for 2 or more hours∗ | 4 | 1.9 | |
| When the hg is 7 g/dl or more and hematocrit of about 20%∗ | 120 | 57.1 | |
| Pulse rate less than 100 bpm∗ | 130 | 61.9 | |
| Diastolic bp of 90 mmhg or more∗ | 97 | 46.2 | |
| When the woman is awake/stable∗ | 136 | 64.8 | |
| Bleeding < 50 ml/hr∗ | 93 | 44.3 | |
| I do not know | 32 | 15.2 | |
|
| |||
| Contraindication to the use of NASG# | Viable fetus∗ | 253 | 72.9 |
| Dyspnea∗ | 160 | 46.3 | |
| Mitral stenosis∗ | 93 | 26.8 | |
| Congestive heart failure∗ | 86 | 20.6 | |
| Pulmonary hypertension∗ | 71 | 25.1 | |
| Bleeding above the level of the diaphragm∗ | 98 | 27.7 | |
| I do not know | 108 | 31.6 | |
|
| |||
| Procedure can be performed on women on NASG# | IV line∗ | 288 | 74.0 |
| Vaginal surgery∗ | 157 | 40.4 | |
| Abdominal surgery∗ | 109 | 28.0 | |
| Transport to other facilities∗ | 184 | 47.3 | |
| I do not know | 64 | 26.5 | |
|
| |||
| Types of knowledge | |||
|
| |||
| Good knowledge | 220 | 55.8% | |
|
| |||
| Poor knowledge | 174 | 44.2% | |
#Multiple responses. ∗Correct response.
3.4. Attitude of Respondents towards NASG
The attitude of the respondents towards the utilization of antishock garments in the management of PPH as presented in Table 4 shows that 197 (50.5%) of the respondents agree that all health professionals should know about NASG. Nearly one-third of 272 (70.5%) disagree that the patient does not have to have the nonpneumatic antishock garment (NASG) applied upon. About half of the respondents, 205 (52.0%), agree that the garment should be a must in every healthcare facility that has maternity service. About 171 (43.4%) of respondents agree with the statement saying antishock garment (NASG) is only beneficial to people in rural areas/primary care settings whereas 195 (49.5%) disagree with it. Regarding total attitude, 228 (57.9%) obstetric care providers had a positive attitude towards NASG utilization.
Table 4.
Attitude of respondents who participated in the study and were working in public hospitals of Sidama region, Ethiopia, 2022 (N = 394).
| Variables | Disagree | Neutral | Agree |
|---|---|---|---|
| Every healthcare personnel should know about the use of the nonpneumatic antishock garment | 186 (47.2%) | 11 (2.8%) | 197 (50.0%) |
| The patient does not have to have the nonpneumatic antishock garment (NASG) applied upon | 276 (70.1%) | 19 (4.8%) | 98 (25.1%) |
| Antishock garment (NASG) is only beneficial to people in rural areas/primary care settings | 195 (49.5%) | 28 (7.1%) | 171 (43.4%) |
| The garment (NASG) is only meant to be applied by doctors | 199 (50.5%) | 27 (6.9%) | 168 (42.6%) |
| The garment should be a must in every healthcare facility that has maternity service | 205 (52.0%) | 19 (4.8%) | 170 (43.1%) |
| NASG is safe and effective in preventing complications of PPH | 155 (39.3%) | 103 (26.1%) | 136 (34.6%) |
| I am motivated to use NASG during PPH because of its effectiveness | 73 (18.1%) | 48 (12.4%) | 273 (69.4%) |
| There is no need for NASG since it is not readily available | 221 (56.1%) | 29 (7.5%) | 144 (36.5%) |
| NASG saves time, energy, and life | 50 (12.7%) | 146 (36.5%) | 198 (50.8%) |
| The garment is expensive, therefore not affordable | 162 (41.1%) | 51 (12.9%) | 181 (45.9%) |
| Attitude category | |||
| Positive | 228 (57.9%) | ||
| Negative | 166 (42.1%) | ||
3.5. Utilization of Nonpneumatic Antishock Garment
Regarding the utilization of NASG by obstetric care providers, 30.71% (95% CI: 27%, 36%) of obstetric care providers used NASG for postpartum hemorrhage management. Among those who used NASG, 46 (38.0%) of them used it during the last six months. Of the reasons reported by respondents who did not use nonpneumatic antishock garments, more than half, 228 (82.6%), were due to lack of training as shown in Table 5.
Table 5.
Utilization of nonpneumatic antishock garment by respondents who participated in the study and were working in public hospitals of Sidama region, Ethiopia, 2022.
| Variables | Category | Frequency | Percent |
|---|---|---|---|
| The last time an antishock garment was used (N = 121) | Less than 1 month ago | 27 | 22.3 |
| Between 1 month and 3 months | 7 | 5.8 | |
| Between 3 months and 6 months | 18 | 14.9 | |
| More than 6 months ago | 46 | 38.0 | |
| I do not remember it | 23 | 19.0 | |
|
| |||
| Reason for nonutilization# | Availability of another method | 160 | 58.0 |
| Lack of training | 229 | 82.6 | |
| Not aware of the existence of NASG in the facility | 105 | 38.0 | |
| No patient needs it | 57 | 20.7 | |
|
| |||
| Do you use NASG every time there is PPH (N = 121) | Yes | 7 | 5.83 |
| No | 114 | 94.16 | |
|
| |||
| If not, when do you use it# | When other methods fail | 18 | 9.4 |
| When PPH with shock | 84 | 44.2 | |
| When active bleeding | 71 | 37.3 | |
| I do not remember | 17 | 24.4 | |
# Multiple responses are possible.
Figure 2 shows utilization and nonutilization of NASG among obstetric care providers.
Figure 2.

Utilization and nonutilization of NASG among obstetric care providers in public hospitals of Sidama region, Hawassa, Ethiopia, 2022.
3.6. Factors Associated with Respondents' Utilization of NASG in Managing PPH
Before proceeding with the regression analysis, the assumptions of logistic regression and model fitness were checked using different methods. A total of fourteen variables were used for crude analysis: four sociodemographic variables (gender, job experience, professional category, and educational level), eight personal and facility-related variables (level of hospital, training, availability of NASG, number of NASG, having experienced staff, protocols in the facility, place of NASG after usage, and wall charts), and the respondent's knowledge and attitude towards NASG analyzed for associations with the utilization of NASG using binary logistic regression analysis. But there is no association between professional categories, number of NASGs, and place of NASG after usage with the dependent variable.
Six of the factors, level of the hospital, training about NASG, availability of NASG, availability of protocol, respondents' attitude, and knowledge, were found to be significantly associated with the use of antishock garments after controlling for confounders in multivariable analysis.
In this study, obstetric care providers working in tertiary hospitals are 35% less likely to utilize NASG for the management of PPH (AOR = 0.355, 95% CI: 0.132, 0.952, p < 0.04). Obstetric care providers who had training on NASG were 4 times more likely to use NASG as compared to those who had no training (AOR = 4.183, 95% CI: 2.167, 8.075, p < 0.000). The odds of the utilization of NASG among obstetric care providers who have NASG in their facility were 4.6 times more likely to use the NASG compared with those who have no NASG in their facility (AOR = 4.603, 95% CI: 1.603, 13.24, p < 0.005). Similarly, the obstetric care provider who has NASG protocol in their facility utilized NASG 2.7 times more likely than those who have no NASG in their facility (AOR = 2.758, 95% CI: 1.269, 5.996, p < 0.01).
In this study, having good knowledge has a statistically significant relationship with the utilization of NASG, and those who had good knowledge about NASG were 2.5 times more likely to use NASG (AOR = 2.506, 95% CI: 01.26, 4.984, p < 0.009), and similarly, those who had a positive attitude towards NASG were 2.3 times more likely to utilize NASG than those who have a negative attitude (AOR = 2.381, 95% CI: 1.189, 4.766, p < 0.015) (see Table 6).
Table 6.
Bivariable and multivariable logistic regression analyses for factors associated with the utilization of nonpneumatic antishock garments among obstetric care providers in public health facilities of Sidama region, Ethiopia, 2022.
| Variables | Utilization of NASG | COR (95% CI) | AOR (95% CI) | p value | ||
|---|---|---|---|---|---|---|
| No | Yes | |||||
| Gender | Female | 124 | 38 | 1 | 1 | |
| Male | 149 | 83 | 1.818 (1.157, 2.856)∗ | 1.402 (0.738, 2.664) | 1.020 | |
|
| ||||||
| Educational level | Diploma | 60 | 23 | 1 | ||
| Bachelor | 200 | 82 | 1.12 (0.64, 1.94) | 0.694 (0.321, 1.50) | 0.353 | |
| Masters and above | 13 | 17 | 3.41 (1.43, 8.12)∗ | 1.331 (0.382, 0.382) | 0.650 | |
|
| ||||||
| Job experience | 1-5 | 196 | 77 | 1 | 1 | |
| 6-9 | 68 | 36 | 1.78 (1.108, 2.87) | 1.581 (0.790, 3.161) | 0.196 | |
| ≥10 | 9 | 8 | 1.92 (0.704, 2.23) | 1.05 (0.272, 4.055) | 0.606 | |
|
| ||||||
| Level of hospital | Primary | 93 | 68 | 1 | 1 | |
| General | 73 | 40 | 6.012 (3.126, 11.587)∗ | 0.779 (0.412, 1.548) | 0.506 | |
| Tertiary | 107 | 13 | 4.51 (2.256, 9.017)∗ | 0.355 (0.132, 0.952) | 0.04∗∗ | |
|
| ||||||
| Training NASG | No | 244 | 64 | 1 | 1 | |
| Yes | 29 | 57 | 7.494 (4.433, 12.66)∗ | 4.183 (2.167, 8.075) | 0.000∗∗ | |
|
| ||||||
| Availability NASG | No | 111 | 6 | 1 | 1 | |
| Yes | 106 | 108 | 18.85 (7.94, 44.73)∗ | 4.603 (1.603, 13.24) | 0.005∗∗ | |
| I do not know | 56 | 7 | 2.312 (0.742, 7.27) | 2.593 (0.718, 9.364) | ||
|
| ||||||
| Protocol about NASG | No | 160 | 30 | 1 | ||
| Yes | 66 | 82 | 6.62 (3.99, 11.00)∗ | 2.758 (1.269, 5.996) | 0.010∗∗ | |
| I do not know | 47 | 9 | 1.021 (0.453, 2.30) | 1.562 (0.539, 4.521) | 0.625 | |
|
| ||||||
| Wall charts | No | 165 | 36 | 1 | ||
| Yes | 91 | 81 | 3.986 (2.494, 6.369)∗ | 1.012 (0.475, 2.157) | 0.957 | |
| I do not know | 17 | 4 | 1.432 (0.493, 4.163) | 0.924 (0.206, 4.140) | 0.917 | |
|
| ||||||
| Have experienced staff | No | 137 | 28 | 1 | 1 | |
| Yes | 40 | 74 | 9.05 (5.17, 15.84)∗ | 2.051 (0.945, 4.45) | 0.069 | |
| I do not know | 98 | 19 | 0.968 (0.511, 1.83) | 1.067 (0.445, 2.554) | 0.885 | |
|
| ||||||
| Knowledge | Poor | 151 | 23 | 1 | 1 | |
| Good | 122 | 98 | 5.274 (3.157, 8.808)∗ | 2.506 (1. 26, 4.984) | 0.009∗∗ | |
|
| ||||||
| Attitude | Negative | 136 | 30 | 1 | 1 | |
| Positive | 137 | 91 | 3.011 (1.871, 4.847)∗ | 2.381 (1.189, 4.766) | 0.015∗∗ | |
Note: ∗statistically significant at p value < 0.25. ∗∗p < 0.05, 95% CI. 1 = reference group.
4. Discussion
This study examined the magnitude of nonpneumatic antishock utilization among obstetric care providers working in public hospitals in Ethiopia's Sidama regional state in 2022. On the utilization of NASG, this study revealed that although 95.9% of the respondents reported they knew that NASG is used to prevent the complication of PPH, only 30.71% have used NASG in the management of PPH.
The magnitude of the utilization of NASG among obstetric care providers in the current study is comparable with the study done in the Maharashtra state of India, 35% [26], and the Ogun state of Nigeria, 36% [22]. The current study's finding is lower than those of studies among obstetric care providers conducted in Ibadan, Nigeria, 74% [27], and northern Ethiopian Tigray region, which had a rate of 64.2% [25], compared with the study done in Jimma, 36.2% [18], and study done in Addis Ababa, 39.3% [20]. This variation might be brought down due to the difference in the study setting, study participants, sample size, and availability of NASG. The other reason for the variation of NASG utilization might be due to country-to-country differences in scaling up and awareness creation among healthcare providers. In addition, the reason for the most significant difference between the current study and the study done in the Tigray region could be that the introduction of the instrument NASG in Ethiopia started in the northern part of the country in 2011. On the other hand, it was greater compared to the result that 14.1% of respondents used a nonpneumatic antishock garment to control postpartum hemorrhage in Ondo state, Nigeria [16]. The possible reason for the difference could be due to differences in the study setting, larger number of study participants, and larger number of public hospitals included in the current study.
This study indicated that obstetric care providers working in tertiary hospitals utilize NASG 35% less likely than those working in primary hospitals, and this could be because primary hospitals usually make referrals to tertiary and general hospitals for definitive management due to limited resources both material and human to manage a postpartum hemorrhage, so that the patients can be transported safely to a higher level of healthcare.
Findings from this study revealed that training on NASG was significantly associated with the utilization of NASG. Obstetric care providers who had training 4 times more utilized NASG than those who have no training. This finding agrees well with previous studies conducted in Addis Ababa [20]. This could be because attending training can help healthcare providers gain more understanding about how to apply and remove nonpneumatic antishock garments, enabling them to better utilize them.
This study result revealed statistical significance between providers' utilization of NASG and the existence of protocol; those who have protocol utilized it 2.7 more likely than those who did not have it. This is consistent with studies done in Ondo state of Nigeria [16] and done in Addis Ababa [20].
The protocol guides providers in how, when, and to which patient the NASG should be applied to; it also helps providers to build confidence and improve their readiness in utilizing NASG for PPH management. Contrary to this finding, a study done in selected southern zones in Arba Minch [21] reported no significant statistical relationship between the existence of NASG protocol and professionals' utilization of NASG. The possible reason for this could be due to differences in the study setting.
Another factor that was statically linked with the use of nonpneumatic antishock garments by healthcare workers in this study was the availability of nonpneumatic antishock garments.
Those who have nonpneumatic antishock garments in the facility are 4.6 times more likely to use them than those who have no nonpneumatic antishock garments in the facility. This agrees with studies done in Ondo state of Nigeria [16].
The results of the current study show that knowledge of NASG and its use is strongly correlated. People with good knowledge are around 2.5 times more likely to use nonpneumatic antishock garments than those with poor knowledge. Studies from the Edu state of Nigeria, northern Ethiopia, and Jimma, Ethiopia, support this [18, 25, 28].
This may be due to the fact that obstetric care providers will feel more confident applying the NASG if they have more knowledge. Contrary to the current study, findings from the Bayelsa state of Nigeria stated a nonsignificant association between professional's knowledge and utilization of NASG [24]. The discrepancy could be due to the different types of obstetric care providers included in the current study, whereas only midwives were included in the other study. The other reason might be the difference in sample size used and cross-country health policy differences.
In addition, a study conducted among midwives in Ogun state of Nigeria reported an inverse relationship between the midwives' knowledge and their utilization of nonpneumatic antishock garment in the management of postpartum hemorrhage [22]. This could be a result of the fact that the midwives have a good knowledge of NASG, but there was no NASG to be utilized in the management of postpartum hemorrhage.
Likewise, respondents' attitudes were significantly associated with their utilization of NASG for PPH management (p < 0.015). Compared with providers with a negative attitude towards the NASG, providers with a positive attitude were 2.4 times more likely to use the NASG. This finding is in line with studies conducted in the Ogun state of Nigeria and another 3 studies conducted in Ethiopia [18, 21, 22]. Contrary to this finding, a study from Ondo state, Nigeria [16], reported no relationship between attitude towards NASG and professionals' utilization of NASG. The possible reason for this could be due to methodological differences in computing attitude and items for assessing attitude and country-to-country differences.
5. Strength and Limitations of the Study
5.1. Strength of the Study
The study was conducted at the regional level and incorporated different professionals, obstetricians, IEOS, general practitioners, nurses, and midwives which can help to make appropriate inferences
5.2. Limitations of the Study
Recall bias was there because healthcare professionals were asked about their past utilization of NASG
6. Conclusion and Recommendation
However, the utilization of NASG can be greatly influenced by different factors, and we found that less than one-third of study participants have used the NASG in the management of PPH in Sidama regional state public hospitals, and this finding is low compared with other studies. Levels of hospitals, training about NASG, availability of NASG, availability of protocol, respondents' attitude, and knowledge are significantly associated factors in the current study.
Based on the findings of this study, the following recommendations are forwarded to the concerned bodies.
6.1. For Health Facilities
Health providers' in-service and ongoing professional development training on the use of nonpneumonic antishock clothing for the management of maternal hemorrhage has to be strengthened.
To make NASG available for healthcare providers, the hospital management needs to closely monitor its availability, location, and functionality.
6.2. For Health Professionals
They need to be motivated and interested in utilizing NASG accordingly to protocol whenever the need to utilize NASG rises. They also need to be familiar with the institution's policies regarding NASG utilization and PPH management.
6.3. For Researchers
Since this study included only obstetric care providers, further exploratory studies including program planners and hospital managers need to explore barriers that affect providers' utilization of NASG.
6.4. For Nongovernmental Organizations
Stakeholders and local nongovernmental organizations that are working on improving maternal health should use this opportunity to increase the accessibility of NASG and build the capacity of obstetric care providers.
Acknowledgments
We would like to appreciate Hawassa University College of Medicine and Health Sciences, Department of Midwifery, for allowing studying in the area of my interest and progress in this research thesis. Funding was obtained for this study from Hawassa University.
Abbreviations
- AOR:
Adjusted odds ratio
- CI:
Confidence interval
- COR:
Crude odds ratio
- CHAI:
Clinton Health Action Initiative
- EDHS:
Ethiopian Demographic Health Survey
- NASG:
Nonpneumatic antishock garment
- MMR:
Maternal mortality rate
- OH:
Obstetric hemorrhage
- PPH:
Postpartum hemorrhage.
Data Availability
Although the researcher cannot submit data to a repository due to prior agreement with the study participants, the datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Approval
All methods were performed in accordance with the relevant guidelines and regulations (Declaration of Helsinki). Ethical clearance was obtained from the Institutional Review Board of Hawassa University, College of Medicine and Health Sciences (Ref. number IRB-197/14). The Sidama region public health institute wrote a letter of permission to each institution, and before starting actual data collection, institution permission was obtained from each hospital. The respondents were informed of the purpose of the study. All the information obtained from study participants was held with confidential and used only for the intended purpose.
Consent
Written consent was obtained.
Conflicts of Interest
The authors report no conflicts of interest in this work.
Authors' Contributions
Merkin Bekele developed the initial concept for the study and refined the study design and carried out the study including data collection and analysis. Rekiku Fikre and Yitateku Alelegn wrote the manuscript together. Teketel Ermias read, provided substantial input to, and approved the final manuscript.
References
- 1.Miller S., Bergel E. F., El Ayadi A. M., et al. Non-pneumatic anti-shock garment (NASG), a first-aid device to decrease maternal mortality from obstetric hemorrhage: a cluster randomized trial. PLoS One . 2013;8(10, article e76477) doi: 10.1371/journal.pone.0076477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Suellen M. C. Technology solutions for global health non-pneumatic antishock garment . Johns Hopkins Bloomberg School of Public Health; 2012. [Google Scholar]
- 3.FIGO Safe Motherhood and Newborn Health Committee. Corrigendum to “Non‐pneumatic anti‐shock garment to stabilize women with hypovolemic shock secondary to obstetric hemorrhage” [Int J Gynecol Obstet 128 (2015) 194–5] International Journal of Gynecology & Obstetrics . 2015;132(2):p. 245. doi: 10.1016/j.ijgo.2015.10.003. [DOI] [PubMed] [Google Scholar]
- 4.WHO, UNICEF, UNFPA WBG and the UNPD. Trends in maternal mortality 2000 to 2017: estimates. Sexual and Reproductive Health . 2019 https://www.who.int/reproductivehealth/publications/maternal-mortality-2000-2017/en/ [Google Scholar]
- 5.MOH. Management protocol on selected obstetrics topics for hospitals . Johns Hopkins Bloomberg School of Public Health; 2020. [Google Scholar]
- 6.EPHI. National Maternal Death Surveillance and Response (MDSR) system annual report . EFY; 2010. [Google Scholar]
- 7.Downing J., El Ayadi A., Miller S., et al. Cost-effectiveness of the non-pneumatic anti-shock garment (NASG): evidence from a cluster randomized controlled trial in Zambia and Zimbabwe. BMC Health Services Research . 2015;15(1):1–10. doi: 10.1186/s12913-015-0694-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Say L., Chou D., Gemmill A., et al. Global causes of maternal death: a WHO systematic analysis. The Lancet Global Health . 2014;2(6):p. e323. doi: 10.1016/S2214-109X(14)70227-X. [DOI] [PubMed] [Google Scholar]
- 9.USAID. Ethiopia country profile. Humanit Cris Response Horn Africa . 2012:137–148. [Google Scholar]
- 10. Ethiopian Demographic And Health Survey . 2016. http://microdata.worldbank.org .
- 11.PMA. Results Brief . Johns Hopkins Bloomberg School of Public Health; 2020. [Google Scholar]
- 12.Pileggi-Castro C., Nogueira-Pileggi V., Tunçalp Ö., Oladapo O. T., Vogel J. P., Souza J. P. Non-pneumatic anti-shock garment for improving maternal survival following severe postpartum haemorrhage: a systematic review. Reproductive Health . 2015;12(1):p. 28. doi: 10.1186/s12978-015-0012-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Clinton Health Access Foundation. Clinton Health Access Initiative: HIV/AIDS. 2013. https://www.clintonfoundation.org/our-work/clinton-health-access-initiative/programs/hivaids .
- 14.Escobar M. F., Füchtner C. E., Carvajal J. A., et al. Experience in the use of non-pneumatic anti-shock garment (NASG) in the management of postpartum haemorrhage with hypovolemic shock in the Fundación Valle Del Lili, Cali Colombia. Reproductive Health . 2017;14(1):2–9. doi: 10.1186/s12978-017-0325-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ojengbede O. A., Morhason-Bello I. O., Galadanci H., et al. Assessing the role of the non-pneumatic anti-shock garment in reducing mortality from postpartum hemorrhage in Nigeria. Gynecologic and Obstetric Investigation . 2011;71(1):66–72. doi: 10.1159/000316053. [DOI] [PubMed] [Google Scholar]
- 16.Ohaeri B. M., Ogbeye G. B. Assessment of utilisation of non-pneumatic anti shock garment (NASG) in the control of post-partum haemorrhage among midwives in selected hospitals in Ondo-state, Nigeria. International Journal of Caring Sciences . 2017;10(1):327–334. [Google Scholar]
- 17.UN. 2014 Progress Report UN Commission on Life Saving Commoditie. 2015 http://www.who.int/woman_child_accountability/ierg/reports/UNCOLSC_submission_iERG_2015.pdf .
- 18.Bekele G., Terefe G., Sinaga M., Belina S. Utilization of non-pneumatic anti-shock garment and associated factors for postpartum hemorrhage management among health care professionals’ in public hospitals of Jimma zone, south-west Ethiopia, 2019. Reprod Health . 2020;17(1):p. 37. doi: 10.1186/s12978-020-0891-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jordan K., Butrick E., Yamey G., Miller S. Barriers and facilitators to scaling up the non-pneumatic anti-shock garment for treating obstetric hemorrhage: a qualitative study. PLoS One . 2016;11(3):1–13. doi: 10.1371/journal.pone.0150739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ababo Z., Woldesselese F. Utilization of non-pneumatic anti-shock garment and associated factors among health care professionals at public hospitals of Addis Ababa, Ethiopia. Central African Journal of Public Health . 2021;7(6):269–278. doi: 10.11648/j.cajph.20210706.14. [DOI] [Google Scholar]
- 21.Yeshitila Y. G., Bante A., Aschalew Z., Afework B., Gebeyehu S. Utilization of non-pneumatic anti-shock garment and associated factors for postpartum hemorrhage management among obstetric care providers in public health facilities of southern Ethiopia, 2020. PLoS One . 2021;16(10, article e0258784) doi: 10.1371/journal.pone.0258784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Adamu-Adepipe F. O., Owopetu C. A. Factors influencing utilization of non-pneumatic anti-shock garment in managing postpartum hemorrhage among midwives in primary healthcare centres in Ogun state. International Journal of Medicine, Nursing & Health Sciences (IJMNHS) . 2021;2:114–129. [Google Scholar]
- 23.Federal Democratic Republic of Ethiopia Population Census Commission. Summary and statistical Report of 2007 Population and Housing Census . منشورات جامعة دمشق.; 2007. [Google Scholar]
- 24.Onasoga O., Duke E., Danide I., Jack-Ide I. Midwives’ knowledge and utilization of non-pneumatic anti shock garment in reducing complication of postpartum haemorrhage in selected health care facilities in Bayelsa state Nigeria. International Journal of Reproduction, Contraception, Obstetrics and Gynecology . 2015;4(4):977–981. doi: 10.18203/2320-1770.ijrcog20150410. [DOI] [Google Scholar]
- 25.Desta A. A., Berhane M., Woldearegay T. W. Utilization rate and factors associated with non-utilization of non-pneumatic anti-shock garment in the management of obstetric hemorrhage in public health care facilities of northern Ethiopia: a cross-sectional study. International Journal of Women's Health . 2020;Volume 12:943–951. doi: 10.2147/IJWH.S266534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bangal V. B., Gavhane S., Raut S., Thorat U. Use of non-pneumatic anti shock garment in hemorrhagic shock. International Journal of Reproduction, Contraception, Obstetrics and Gynecology . 2019;8(2):p. 621. doi: 10.18203/2320-1770.ijrcog20190295. [DOI] [Google Scholar]
- 27.Akingbohungbe O., Ojewale L. Y., Akingbade O., Adejumo P. O. Knowledge and utilisation of anti-shock garment among midwives of Adeoyo Maternity Teaching Hospital, Ibadan, Nigeria. Midwifery . 2021;4(5):26–37. doi: 10.52589/AJHNM-U47SAEMP. [DOI] [Google Scholar]
- 28.Enuku C. A., Adeyemo F. O. Knowledge and use of anti-shock garment among midwives in central hospital, Benin City, Edo state. Lautech Journal of Nursing . 2018;23:23–38. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Although the researcher cannot submit data to a repository due to prior agreement with the study participants, the datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.


