Over the past 2 years, coronavirus disease 2019 (COVID-19) has turned out to be a cardiovascular disease as much as a respiratory one, contrary to what was initially assumed [1]. Several studies have highlighted that troponin could be a biological marker of interest in the risk stratification of COVID-19 at admission [2], with a potential association with right ventricular afterload and systolic dysfunction on transthoracic cardiac ultrasound, leading to heart failure [3]. However, few studies have focused on exploring the prognostic value of monitoring troponin [4]. We hypothesize that measurement of cardiac troponin may be useful for the risk stratification of patients with COVID-19 at hospitalization, independent of myocardial injury.
The SARCODO study (ClinicalTrials.gov identifier: NCT04624997) was conducted at the Georges Pompidou European Hospital, located in Paris, during the first COVID-19 wave. We retrospectively analysed troponin measurements at admission and throughout hospitalization, to evaluate their ability to predict in-hospital mortality in patients with COVID-19, by using logistic regression and Cox models. High-sensitivity cardiac troponin (Beckman Coulter, Brea, CA, USA) was measured on a DXI analyser in plasma collected on sodium heparin. We used an association of linear interpolation, last observation carried forward and next observation carried backward to impute for missing data. All patients who had at least two measurements were included for monitoring analyses.
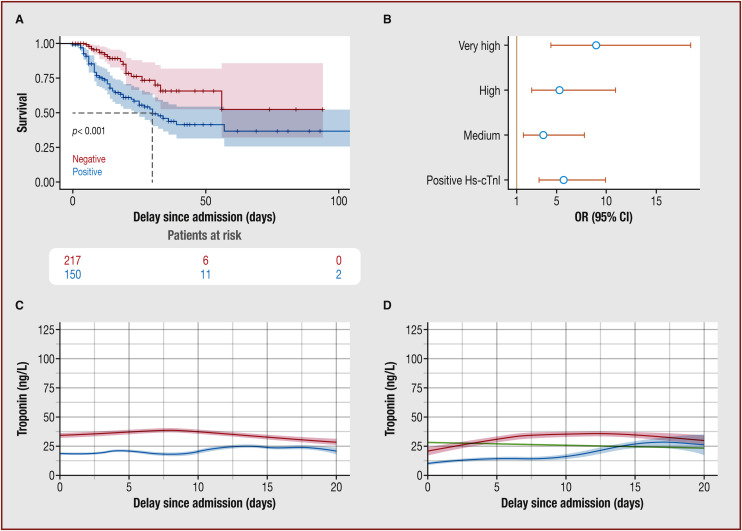
Between January and July 2020, among 399 patients enrolled with confirmed COVID-19 on polymerase chain reaction and analysed for troponin at admission, 247 had at least two troponin measurements during hospitalization. The patients who had several troponin measurements were more critical on arrival and had significantly more deaths and intensive care unit (ICU) admissions than those who only had one measurement (P < 0.001). There was a majority of males (67%), and the mean age was 66 ± 16 years. A total of 134 patients (34%) were transferred immediately to an ICU, 265 (66%) were transferred to a medical ward and 37 (9%) were transferred secondarily to an ICU. During hospitalization, 80 (20%) patients did not survive. Increased troponin on arrival (defined as above the hospital's upper limit of normal, according to sex) was significantly associated with mortality (hazard ratio 2.59, 95% confidence interval [CI] 1.56–4.28; P < 0.001), as well as intubation and ICU admission (P < 0.01) (Fig. 1A ). Increased troponin at admission was significantly associated with the occurrence of cardiovascular complications during hospitalization, such as myocardial infarction, myocarditis, pericarditis or arrhythmia (odds ratio [OR] 2.26, 95% CI 1.08–4.72; P = 0.027); after adjustment on cardiovascular complications, elevated troponin at admission was still associated with mortality (adjusted OR 5.5, 95% CI 3.18–9.8; P < 0.001). At admission, the prognostic ability of troponin seemed to be concentration dependent (P < 0.01), as previously stated in other studies that found a significant association between troponin concentration and death or cardiovascular complications in patients with COVID-19 [5] (Fig. 1B). During the first 10 days, we observed that the troponin concentration throughout hospitalization was significantly higher in patients who died during their hospital stay (P < 0.001) (Fig. 1C). We observed a similar variation in troponin in patients who required an ICU during hospitalization (directly or secondarily) (Fig. 1D). After 10 days, troponin concentration curves intersected, had similar patterns and were very close (Fig. 1C and Fig. 1D). Maximum troponin (peak of troponin) throughout hospitalization was significantly higher in patients who required an ICU during their hospital stay, whether at admission or during follow-up (P < 0.001), and this peak occurred mainly during the first 10 days. This concurs with previous studies, which highlighted the difference in troponin evolution between survivors and non-survivors among critically ill patients during the first week of hospitalization [6]. Furthermore, this choice of period was supported in our study by a mixed model analysis, which showed a strong elevation of troponin during the first 10 days of hospitalization, followed by a plateau phase. To assess the ability of troponin monitoring to predict in-hospital mortality, we analysed the ratio between the highest troponin concentration during the first 10 days and the baseline troponin measurement, which was drawn during the first 48 hours of hospitalization. This ratio of troponin concentrations was significantly associated with in-hospital mortality (OR 1.022, 95% CI 1.005–1.04; P = 0.01), which could be predicted by a 75% increase in the ratio (with a corresponding area under the curve of 71.7, 95% CI 62.5–80.9).
Fig. 1.
The association between the concentration of high-sensitivity cardiac troponin (Hs-cTnI) and outcome at admission and during hospitalization. A. Survival curves of patients with coronavirus disease 2019 (COVID-19), stratified to the concentration of Hs-cTnI at admission, defined as either positive (blue line) if the concentration of Hs-cTnI was above the hospital's upper limit of normal, according to sex, or negative (red line). B. Odds ratios (ORs) and 95% confidence interval (CIs) for death according to the concentration of Hs-cTnI at admission (terciles above normal value). C. Temporal trend of concentration of Hs-cTnI among survivors (blue line) and deceased patients (red line) with COVID-19. D. Temporal trend of concentration of Hs-cTnI in patients with COVID-19, according to their hospitalization ward: patients admitted to an intensive care unit (ICU) directly from the emergency department (green line); patients admitted secondarily to an ICU after initial hospitalization in a medical ward (red line); and patients solely admitted to a medical ward throughout hospitalization (blue line).
Our results provide further proof that troponin could and should be used as a tool to stratify patients at admission in hospital, as it is reproducible, concentration-dependent and strongly predictive of severity and in-hospital mortality, even independent of cardiovascular damage. On the other hand, we did not manage to demonstrate the utility of troponin measurement throughout hospitalization. This goes against other strong retrospective studies that showed a constant increase in troponin concentrations until day 25 of hospitalization for critical patients compared with those with mild disease [7]. This might be because of a lack of power or the great number of missing troponin values. Indeed, troponin measurements were not systematic throughout the study, but were left at the physician's discretion, and thus varied considerably from patient to patient. In addition, our study differs from previous studies exploring the predictive value of D-dimer elevation, which highlighted its strong association with disease severity, whether at admission or during in-hospital monitoring. Indeed, D-dimer levels were highly increased in ICU patients throughout hospitalization, either when admitted directly from the emergency room or transferred secondarily from another ward [8]. In that study [8], those two biomarkers were associated with right ventricle failure at admission, and this discrepancy concerning their evolution through hospitalization could thus be explained by an extracardiovascular aetiology. Indeed, D-dimers could be increased as a result of endotheliopathy secondary to the inflammatory state of patients with COVID-19, which has less effect on troponin concentrations.
All in all, our results underscore the importance of troponin measurement at admission for patients with COVID-19, where it seems to be a relevant factor for in-hospital mortality and risk stratification. Meanwhile, its monitoring during follow-up does not appear to be valuable in predicting disease progression towards a fatal outcome. Our finding highlighted that troponin needed to be measured only once in the first 10 days, and this strategy seem to be sufficient to evaluate the severity of the disease.
Sources of funding
This work was funded with a grant from the French national agency for research, ANR Flash-COVID SARCODO (Fondation de France).
Disclosure of interest
The authors declare that they have no competing interest.
Footnotes
Tweet: Usefulness of troponin in COVID-19. Twitter handle: @RichardChocron.
References
- 1.Smadja D.M., Mentzer S.J., Fontenay M., Laffan M.A., Ackermann M., Helms J., et al. COVID-19 is a systemic vascular hemopathy: insight for mechanistic and clinical aspects. Angiogenesis. 2021;24:755–788. doi: 10.1007/s10456-021-09805-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guo T., Fan Y., Chen M., Wu X., Zhang L., He T., et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:811–818. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goudot G., Chocron R., Augy J.L., Gendron N., Khider L., Debuc B., et al. Predictive factor for COVID-19 worsening: insights for high-sensitivity troponin and D-Dimer and correlation with right ventricular afterload. Front Med (Lausanne) 2020;7:586307. doi: 10.3389/fmed.2020.586307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Majure D.T., Gruberg L., Saba S.G., Kvasnovsky C., Hirsch J.S., Jauhar R., et al. Usefulness of elevated troponin to predict death in patients with COVID-19 and myocardial injury. Am J Cardiol. 2021;138:100–106. doi: 10.1016/j.amjcard.2020.09.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bonnet G., Weizman O., Trimaille A., Pommier T., Cellier J., Geneste L., et al. Characteristics and outcomes of patients hospitalized for COVID-19 in France: the critical COVID-19 France (CCF) study. Arch Cardiovasc Dis. 2021;114:352–363. doi: 10.1016/j.acvd.2021.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li C., Jiang J., Wang F., Zhou N., Veronese G., Moslehi J.J., et al. Longitudinal correlation of biomarkers of cardiac injury, inflammation, and coagulation to outcome in hospitalized COVID-19 patients. J Mol Cell Cardiol. 2020;147:74–87. doi: 10.1016/j.yjmcc.2020.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smadja D.M., Bory O.M., Diehl J.L., Mareau A., Gendron N., Jannot A.S., et al. Daily monitoring of D-Dimer allows outcomes prediction in COVID-19. TH Open. 2022;6:e21–e25. doi: 10.1055/a-1709-5441. [DOI] [PMC free article] [PubMed] [Google Scholar]