Abstract
Background:
Social and psychosocial factors are associated with cardiovascular health (CVH). Our objective was to examine the contributions of individual-level social and psychosocial factors to racial and ethnic differences in population CVH in the National Health and Nutrition Examination Surveys (NHANES) 2011-2018, to inform strategies to mitigate CVH inequities.
Methods:
In NHANES participants aged ≥20 years, Kitagawa-Blinder-Oaxaca decomposition estimated the statistical contribution of individual-level factors (education, income, food security, marital status, health insurance, place of birth, depression) to racial and ethnic differences in population mean CVH score (range 0-14, accounting for diet, smoking, physical activity, body mass index, blood pressure, cholesterol, blood glucose) among Hispanic, non-Hispanic Asian, or non-Hispanic Black adults compared with non-Hispanic White adults.
Results:
Among 16,172 participants (representing 255 million US adults), 24% were Hispanic, 12% non-Hispanic Asian, 23% non-Hispanic Black, and 41% non-Hispanic White. Among males, mean (standard error [SE]) CVH score was 7.45 (2.3) in Hispanic, 8.71 (2.2) in non-Hispanic Asian, 7.48 (2.4) in non-Hispanic Black, and 7.58 (2.3) in non-Hispanic White adults. In Kitagawa-Blinder-Oaxaca decomposition, education explained the largest component of CVH differences among males (if distribution of education were similar to Non-Hispanic White, CVH score would be 0.36 [0.04] points higher in Hispanic, 0.24 [0.04] points lower in Non-Hispanic Asian, and 0.23 [0.03] points higher in Non-Hispanic Black, p<0.05). Among females, mean (SE) CVH score was 8.03 (2.4) in Hispanic, 9.34 (2.1) in non-Hispanic Asian, 7.43 (2.3) in non-Hispanic Black, and 8.00 (2.5) in non-Hispanic White adults. Education explained the largest component of CVH difference in Non-Hispanic Black females (if distribution of education were similar to NH White, CVH score would be 0.17 [0.03] points higher in NH Black, p<0.05). Place of birth (US-born versus born outside the US) explained the largest component of CVH difference in Hispanic and Non-Hispanic Asian females (if distribution of place of birth were similar to Non-Hispanic White, CVH score would be 0.36 [0.07] points lower and 0.49 [0.16] points lower, respectively, p<0.05).
Conclusions:
Education and place of birth confer the largest statistical contributions to the racial and ethnic differences in mean CVH score among US adults.
Keywords: Social determinants, psychosocial factors, cardiovascular health, race, ethnicity
Introduction
Racial and ethnic differences in cardiovascular disease (CVD) are persistent in the United States (US) with 2-fold higher risk of death from CVD in non-Hispanic Black adults compared with non-Hispanic White adults.1–3 In the Coronary Artery Risk Development in Young Adults (CARDIA) study, the difference in risk of incident CVD between Black and White adults was attenuated by adjustment for clinical factors (including fasting glucose and total cholesterol), socioeconomic factors (including education and healthcare access), and neighborhood-level factors (including neighborhood-level poverty and segregation).4 Since race and ethnicity are social constructs, not biological factors, underlying social and structural determinants of health likely result in differences in CVD risk among racial and ethnic groups by conferring advantages or disadvantages related to environment, opportunity, and access to resources.5, 6
Clinical and behavioral factors are commonly aggregated as the American Heart Association Life’s Simple 7 cardiovascular health (CVH) score including dietary quality, smoking, physical activity, body mass index, blood pressure, cholesterol, and blood glucose.7 A 1-point higher CVH score in young adulthood was associated with a 27% lower risk for incident CVD events over 32 years’ follow-up in the CARDIA study.8 In longitudinal follow-up of the Atherosclerosis Risk in Communities study, compared with adults who had consistently poor CVH (0-2 factors in at ideal levels), participants with consistently high CVH had a 74% lower risk of CVD events and 65% lower risk of mortality.9 A range of interrelated social and psychosocial factors are associated with worse CVH, including lower education10 and food insecurity.11 In addition, place of birth (i.e., nativity) is variably associated with CVH for immigrant populations.12 While these individual-level factors are important CVH determinants, the relative contributions of these factors to racial and ethnic differences in CVH has not been quantified. This may inform strategies to address disparities in CVH and CVD by identifying the factors that contribute most to CVH differences. Accordingly, we quantified the racial and ethnic differences in CVH statistically explained by individual-level social and psychosocial determinants, among Hispanic, non-Hispanic Asian, and non-Hispanic Black adults compared with non-Hispanic White adults in the National Health and Nutrition Examination Surveys (NHANES).
Methods
Participants
We used nationally representative data from NHANES cycles between 2011-2018. All data are publicly available at the NHANES website, which can be accessed at https://www.cdc.gov/nchs/nhanes/index.htm. We began the analysis in 2011 because this was the first NHANES cycle to include “non-Hispanic Asian” as a separate response category for race and ethnicity.13 The 2019-2020 NHANES surveys were not included because enrollment challenges related to the coronavirus disease 2019 pandemic limit the use of survey weights to the overall sample and not specific subgroups and because dietary quality data are not available.14 The sample included non-institutionalized adults aged ≥20 years who participated in the Mobile Examination Center (MEC) exams. Participants were excluded if they were currently pregnant, breastfeeding, or had missing data for any of the variables (Supplemental Figure S1). Participants self-identified their race and ethnicity as Hispanic, non-Hispanic Asian, non-Hispanic Black, or non-Hispanic White.
Cardiovascular Health Score
CVH was defined by the American Heart Association score, which integrates seven health factors and behaviors: dietary quality, smoking, physical activity, body mass index, blood pressure, cholesterol, and blood glucose.7 Each of the factors was rated as poor (0 points), intermediate (1 point), or ideal (2 points), as summarized in Supplemental Table S1. A composite CVH score ranging from 0 to 14 was calculated as the sum of points across seven categories, with a higher score indicating better CVH.
Individual-Level Factors
Individual-level factors associated with both CVH and CVD were identified based on published literature,15 guided by factors identified in the World Health Organization’s Social Determinants of Health conceptual framework.16 Educational attainment was categorized as less than high school, high school graduate, associate’s degree or some college, college graduate or above. Annual household income was categorized as $0-$44,999, $45,000-$99,999, or ≥$100,000. Food insecurity was defined as no or marginal food insecurity (i.e., full or marginal food security), versus severe food insecurity (i.e., low or very low food security). Marital status was categorized as never married; divorced, separated, or widowed; or married or living with partner. Health insurance was characterized as not covered by insurance, covered by private insurance, or covered by other insurance. Depression was defined by the PHQ-9 scale (0-27, with a higher score indicating more depression symptoms), and categorized as 0-4 (no or minimal depression symptoms) and 5-27 (mild, moderate, or severe depression symptoms). Participant place of birth was defined as born in the US (50 states and Washington, DC), versus born outside the US.
Statistical Analysis
The participant sample was described by calculating mean (standard error of the mean, SE) and frequency (percent) of demographic variables, CVH score, and individual-level factors. Two complementary strategies quantified the extent to which individual-level factors may explain racial and ethnic differences in CVH. First, we used sex-stratified multivariable-adjusted linear regression models with composite CVH score as the dependent variable and race and ethnicity category as an independent variable, comparing Hispanic, non-Hispanic Asian, and non-Hispanic Black participants to non-Hispanic White participants of the same sex. Data were stratified by sex a priori given known sex differences in CVH. The amount of the racial and ethnic difference in CVH explained by individual or aggregated factors was estimated as the percent reduction in the regression ß coefficient for race and ethnicity group, corresponding to adjustment for an individual-level factor, per the formula: 100 * ([ß0] − [ßNEW]) / (ß0). The percent reduction in the ß coefficient representing racial and ethnic group from ß0 in the referent model to ßNEW in the new (adjusted) model reflects the percent reduction in the association with CVH when comparing racial and ethnic group participants to non-Hispanic White participants, after adjustment for the additional factor(s) in the new model.
The base model (model 1 [M1]) was adjusted for age and study cycle year (to account for year fixed effects). Each factor was subsequently separately added to the M1 model. The percent reduction in the regression ß coefficient for race and ethnicity relative to the regression ßM1 coefficient for race and ethnicity was calculated for each of seven individually adjusted models compared with M1, to represent the amount of the racial and ethnic difference in CVH statistically explained by each factor individually. A fully adjusted model was also estimated, adjusted for age, study cycle, and all factors. We performed bootstrapping based on 500 resamples to calculate the standard errors of beta percent changes.
Next, Kitagawa-Blinder-Oaxaca (KBO) decomposition was used to simultaneously quantify the extent to which individual-level factors statistically explained the CVH difference between racial and ethnic groups. The KBO decomposition is a statistical method developed in the economics literature to explain inequalities between groups.17–19 It has been used in public health research to understand and identify potential intervention targets to reduce health inequities20–22 such as to identify the contribution of social determinants to diabetes health disparities in Hispanic and Latinx populations,23, 24 and to characterize factors that explain the racial and ethnic differences in CVD risk factors among mid-life women.25 Here, we applied the KBO decomposition to statistically quantify the amount of the difference in mean CVH between racial and ethnic groups that is associated with (1) “explained differences,” which are the between-group differences in the levels of the factors of interest (i.e., differences based on the observable factors as included in the statistical regression models), and (2) “unexplained differences,” which are differences due unobserved factors (e.g., discrimination) that result in differential magnitudes of association (i.e., differences in regression coefficients, or slope of regression line) of the individual-level factors with CVH within each racial and ethnic group. KBO decomposition uses a counterfactual approach by setting factor levels (in the explained component) and the regression coefficients (in the unexplained component) to the level or distribution of the reference group (non-Hispanic White) to estimate the associated magnitude difference in mean CVH score. Statistical methods and interpretation for KBO decomposition are described in detail in the Supplemental Methods. We performed bootstrapping based on 500 resamples to calculate the standard errors of the differences in CVH.
Analyses were performed with Stata version 17 and used survey analysis procedures to account for the complex, multi-stage, probability sampling design, using MEC sample weights. NHANES participants provided written informed consent. This analysis was exempt from institutional review board approval due to the use of de-identified, public data.
Results
Among 16,172 participants in NHANES representing 254,315,002 adults in the US, there were 7,969 males, of whom 24% were Hispanic (mean age 41.2 [SE 14.6] years), 12% were non-Hispanic Asian (mean age 43.1 [15.4] years), 22% were non-Hispanic Black (mean age 44.5 [16.2] years), and 42% were non-Hispanic White (mean age 49.2 [17.1] years). There were 8,203 females of whom 25% were Hispanic (mean age 42.9 [SE 15.5] years), 12% were non-Hispanic Asian (mean age 45.2 [15.7] years), 23% were non-Hispanic Black (mean age 45.7 [16.2] years), and 40% were non-Hispanic White (mean age 51.2 [17.1] years).
Table 1 shows participant demographics, mean CVH scores, and individual-level social and psychosocial factors. Among males, mean (SE) CVH score ranged from 7.45 (2.3) in Hispanic adults to 8.71 (2.2) in non-Hispanic Asian adults. Among females, mean CVH score ranged from 7.43 (2.3) in non-Hispanic Black adults to 9.34 (2.1) in non-Hispanic Asian adults. The weighted distribution of individual CVH factors is shown in Table 2.
Table 1.
Participant characteristics by racial and ethnic group and sex
| Male | Female | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Non-Hispanic White | Non-Hispanic Black | Hispanic | Non-Hispanic Asian | Non-Hispanic White | Non-Hispanic Black | Hispanic | Non-Hispanic Asian | |
| N | 3,384 | 1,751 | 1,884 | 950 | 3,322 | 1,896 | 2,035 | 950 |
| Weighted N | 96,791,827 | 10,714,825 | 18,281,043 | 4,840,506 | 89,757,601 | 12,239,383 | 16,599,341 | 5,090,476 |
| Age, mean (SE) | 49.2 (17.1) | 44.5 (16.2) | 41.2 (14.6) | 43.1 (15.4) | 51.2 (17.1) | 45.7 (16.2) | 42.9 (15.5) | 45.2 (15.7) |
| Cardiovascular health score | 7.58 (2.3) | 7.48 (2.4) | 7.45 (2.3) | 8.71 (2.2) | 8.00 (2.5) | 7.43 (2.3) | 8.03 (2.4) | 9.34 (2.1) |
| History of CVD | 10.3% | 8.6% | 5.0% | 4.4% | 7.4% | 8.4% | 4.2% | 3.0% |
| Education level | ||||||||
| Less than high school | 9.0% | 17.4% | 36.0% | 8.9% | 7.9% | 14.1% | 33.3% | 11.4% |
| High school graduate | 23.6% | 31.1% | 26.1% | 13.0% | 21.8% | 24.3% | 21.9% | 12.9% |
| Some college | 30.9% | 33.4% | 24.9% | 18.4% | 35.4% | 39.3% | 29.6% | 21.9% |
| College graduate or above | 36.5% | 18.0% | 13.1% | 59.6% | 35.0% | 22.3% | 15.2% | 53.8% |
| Household income | ||||||||
| $0 - $44,999 | 28.6% | 48.9% | 49.9% | 24.5% | 34.6% | 56.0% | 52.0% | 24.9% |
| $45,000 - $99,999 | 38.1% | 35.9% | 38.1% | 36.8% | 35.8% | 32.2% | 36.3% | 38.1% |
| $100,000 and over | 33.4% | 15.2% | 12.0% | 38.8% | 29.6% | 11.7% | 11.7% | 37.0% |
| Food security | ||||||||
| Severe food insecurity | 11.3% | 26.3% | 29.6% | 6.7% | 13.0% | 26.5% | 31.0% | 8.1% |
| No or marginal food insecurity | 88.7% | 73.7% | 70.4% | 93.3% | 87.0% | 73.5% | 69.0% | 91.9% |
| Marital status | ||||||||
| Never married | 18.3% | 32.0% | 20.1% | 24.5% | 12.5% | 35.7% | 18.5% | 17.6% |
| Divorced, separated or widowed | 12.5% | 16.4% | 10.6% | 5.1% | 24.7% | 28.5% | 20.6% | 13.3% |
| Married or living with partner | 69.2% | 51.6% | 69.3% | 70.4% | 62.9% | 35.8% | 60.9% | 69.1% |
| Health insurance | ||||||||
| Not covered | 12.4% | 26.5% | 39.4% | 14.2% | 9.2% | 17.4% | 32.5% | 11.4% |
| Covered by other insurance | 18.6% | 28.3% | 19.1% | 20.5% | 21.4% | 36.5% | 27.4% | 22.6% |
| Covered by private insurance | 68.9% | 45.2% | 41.5% | 65.3% | 69.4% | 46.1% | 40.0% | 66.0% |
| Place of birth | ||||||||
| Born outside the US | 3.9% | 11.5% | 59.7% | 83.6% | 3.9% | 9.4% | 56.9% | 85.8% |
| US-born | 96.1% | 88.5% | 40.3% | 16.4% | 96.1% | 90.6% | 43.1% | 14.2% |
| Depression level | ||||||||
| No/minimal depression | 82.0% | 79.8% | 81.7% | 87.3% | 74.3% | 70.7% | 72.5% | 84.7% |
| Depression symptoms | 18.0% | 20.2% | 18.3% | 12.7% | 25.7% | 29.3% | 27.5% | 15.3% |
CVD: Cardiovascular disease. Data are from NHANES 2011-2018. The sample includes participants aged≥20 who were not pregnant or breastfeeding at the time of data collection. Data shown as mean (standard error) or weighted percent of the study sample for each characteristic, within each sex-ethnicity-race group.
Table 2.
Weighted distribution of CVH factors and behaviors by race and ethnicity and sex
| Male | Female | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Non-Hispanic White | Non-Hispanic Black | Hispanic | Non-Hispanic Asian | Non-Hispanic White | Non-Hispanic Black | Hispanic | Non-Hispanic Asian | |
| Diet | ||||||||
| Poor | 81.2% | 80.7% | 83.4% | 57.5% | 68.3% | 74.0% | 73.2% | 47.4% |
| Intermediate | 18.7% | 18.0% | 16.3% | 41.2% | 30.7% | 24.4% | 25.3% | 50.3% |
| Ideal | 0.2% | 1.3% | 0.2% | 1.3% | 0.9% | 1.6% | 1.5% | 2.3% |
| Smoking | ||||||||
| Poor | 19.5% | 29.2% | 19.0% | 13.5% | 17.9% | 17.7% | 10.2% | 3.3% |
| Intermediate | 13.5% | 8.5% | 15.2% | 11.1% | 9.7% | 6.0% | 7.7% | 3.6% |
| Ideal | 67.1% | 62.3% | 65.8% | 75.4% | 72.4% | 76.3% | 82.1% | 93.1% |
| Physical activity | ||||||||
| Poor | 42.0% | 43.9% | 48.9% | 34.6% | 43.5% | 53.5% | 54.5% | 43.3% |
| Intermediate | 10.1% | 11.2% | 9.5% | 12.5% | 10.6% | 9.5% | 8.4% | 14.1% |
| Ideal | 47.8% | 44.9% | 41.6% | 52.9% | 46.0% | 36.9% | 37.2% | 42.6% |
| Body mass index | ||||||||
| Poor | 37.6% | 39.0% | 43.5% | 12.3% | 38.5% | 58.1% | 46.6% | 14.3% |
| Intermediate | 37.5% | 31.3% | 39.7% | 39.6% | 28.2% | 23.1% | 31.2% | 24.8% |
| Ideal | 24.9% | 29.7% | 16.8% | 48.1% | 33.3% | 18.8% | 22.2% | 60.9% |
| Blood pressure | ||||||||
| Poor | 17.5% | 24.3% | 14.0% | 16.1% | 15.6% | 22.4% | 12.3% | 12.6% |
| Intermediate | 49.2% | 48.8% | 45.8% | 40.6% | 41.5% | 41.9% | 32.1% | 33.6% |
| Ideal | 33.4% | 27.0% | 40.2% | 43.3% | 42.9% | 35.7% | 55.6% | 53.8% |
| Cholesterol | ||||||||
| Poor | 10.6% | 8.4% | 12.9% | 12.9% | 14.3% | 10.3% | 9.9% | 10.5% |
| Intermediate | 44.2% | 35.0% | 34.3% | 39.7% | 44.4% | 34.4% | 34.0% | 37.8% |
| Ideal | 45.2% | 56.5% | 52.8% | 47.4% | 41.4% | 55.3% | 56.1% | 51.7% |
| Blood glucose | ||||||||
| Poor | 13.1% | 15.6% | 13.2% | 13.4% | 9.9% | 15.1% | 13.9% | 10.6% |
| Intermediate | 25.8% | 17.0% | 24.5% | 23.4% | 19.0% | 15.2% | 17.4% | 17.8% |
| Ideal | 61.1% | 67.4% | 62.3% | 63.2% | 71.0% | 69.7% | 68.7% | 71.5% |
The percent reduction in regression ß coefficients associated with adjustment for individual-level factors relative to the base model (ßM1) for the association of race and ethnicity with CVH is displayed in Table 3, with regression coefficients in the fully adjusted models in Supplemental Table S2. Among non-Hispanic Black, Hispanic, and non-Hispanic Asian males compared with non-Hispanic White males, adjustment for all factors was associated with a 100% (SE 12%), 67% (SE 16%), and 71% (SE 12%) reduction in the regression ß coefficient for the association of race/ethnicity with CVH, respectively. Among non-Hispanic Black, Hispanic, and non-Hispanic Asian females compared with non-Hispanic White females, adjustment for all factors was associated with a 38% (SE 6%), 62% (SE 18%), and 85% (SE 9%) reduction in the regression ß coefficient for race/ethnicity, respectively.
Table 3.
Percent of differences in cardiovascular health between race and ethnic groups versus non-Hispanic White adults that is statistically explained by individual-level factors
| NH Black versus NH White | Hispanic versus NH White | NH Asian versus NH White | ||||
|---|---|---|---|---|---|---|
| ß (SE) | ß % reduction (SE) | ß (SE) | ß % reduction (SE) | ß (SE) | ß % reduction (SE) | |
| Males | ||||||
| Model 1 (adjusted for age, year) | −0.29 (0.09)* | Reference | −0.45 (0.08)* | Reference | 0.89 (0.10)* | Reference |
| Model 1 + Education | −0.02 (0.08) | 93.1 (12.2) | −0.03 (0.09) | 93.3 (10.0) | 0.61 (0.10)* | 31.5 (5.3) |
| Model 1 + Income | −0.11 (0.08) | 62.1 (14.9) | −0.25 (0.08)* | 44.4 (9.1) | 0.85 (0.10)* | 4.5 (2.2) |
| Model 1 + Food security | −0.17 (0.08)* | 41.4 (15.1) | −0.31 (0.09)* | 31.1 (7.5) | 0.84 (0.10)* | 5.6 (1.6) |
| Model 1 + Marital status | −0.29 (0.09)* | 0.0 (5.0) | −0.42 (0.08)* | 6.7 (1.9) | 0.87 (0.10)* | 2.2 (1.0) |
| Model 1 + Insurance | −0.15 (0.09) | 48.3 (15.9) | −0.28 (0.09)* | 37.8 (10.6) | 0.91 (0.10)* | ** |
| Model 1 + Place of birth | −0.32 (0.09)* | ** | −0.65 (0.11)* | ** | 0.61 (0.14)* | 31.5 (10.6) |
| Model 1 + Depression | −0.27 (0.08)* | 6.9 (4.3) | −0.45 (0.08)* | 0.0 (1.7) | 0.85 (0.10)* | 4.5 (1.6) |
| Model 1 + All determinants | 0.00 (0.08) | 100.0 (11.6) | −0.15 (0.10) | 66.7 (15.7) | 0.26 (0.13) | 70.8 (11.7) |
| Females | ||||||
| Model 1 (adjusted for age, year) | −0.86 (0.09)* | Reference | −0.42 (0.07)* | Reference | 1.02 (0.10)* | Reference |
| Model 1 + Education | −0.61 (0.07)* | 29.1 (3.6) | 0.07 (0.07) | ** | 0.80 (0.09)* | 21.6 (4.0) |
| Model 1 + Income | −0.57 (0.08)* | 33.7 (4.2) | −0.14 (0.07) | 66.7 (13.9) | 0.92 (0.09)* | 9.8 (3.3) |
| Model 1 + Food security | −0.71 (0.09)* | 17.4 (2.8) | −0.22 (0.07)* | 47.6 (11.4) | 0.94 (0.10)* | 7.8 (1.8) |
| Model 1 + Marital status | −0.83 (0.10)* | 3.5 (2.6) | −0.40 (0.07)* | 4.8 (1.5) | 1.00 (0.10)* | 2.0 (0.7) |
| Model 1 + Insurance | −0.69 (0.08)* | 19.8 (3.2) | −0.19 (0.07)* | 54.8 (14.1) | 1.04 (0.09)* | ** |
| Model 1 + Place of birth | −0.89 (0.09)* | ** | −0.72 (0.10)* | ** | 0.55 (0.13)* | 46.1 (9.0) |
| Model 1 + Depression | −0.81 (0.08)* | 5.8 (2.0) | −0.40 (0.07)* | 4.8 (4.2) | 0.90 (0.10)* | 11.8 (2.7) |
| Model 1 + All determinants | −0.53 (0.07)* | 38.4 (6.0) | −0.16 (0.09) | 61.9 (17.5) | 0.15 (0.12) | 85.3 (9.0) |
NH: Non-Hispanic, SE: Standard error. Beta coefficients represent the regression coefficient of the term for race and ethnicity in linear models evaluating cardiovascular health as the dependent variable. Beta percent reduction represents the percent reduction in the beta coefficient of the term for race and ethnicity in regression models, associated with adjustment for the social determinant listed.
P<0.05 for the beta coefficient for race and ethnic group in the linear regression model.
Percent reduction in ß <0 not reported (i.e., adjustment for this factor did not result in a reduction in the ß coefficient).
Results of the KBO decomposition is shown in Figure 1 (for males) and Figure 2 (for females), and Supplemental Table S3. The figures show the quantified statistical contribution of the individual-level factors associated with the “explained” portion of racial and ethnic net differences in mean CVH. The magnitude difference corresponding to each factor indicates the amount of the absolute difference in mean CVH score between race and ethnic groups that is statistically significantly explained by between-group differences in the distribution of that factor. For instance, for non-Hispanic Black males compared with non-Hispanic White males, age, education, food security, marital status, and place of birth contributed to the explained portion of the difference in mean CVH between the two groups, with the largest magnitude of the difference explained by education: if non-Hispanic Black males had the same distribution of educational attainment as non-Hispanic White males, their mean CVH score would be significantly higher by 0.23 [SE 0.03] points (p<0.05). For Hispanic and non-Hispanic Asian males compared with non-Hispanic White males, the largest magnitude of the CVH difference was also explained by education: if Hispanic or non-Hispanic Asian males had the same distribution of educational attainment as non-Hispanic White males, their mean CVH score would be significantly higher by 0.36 [0.04] points or lower by 0.24 [0.04] points, respectively (p<0.05 for both).
Figure 1. Decomposition of the net difference in mean cardiovascular health score between racial and ethnic group among males.
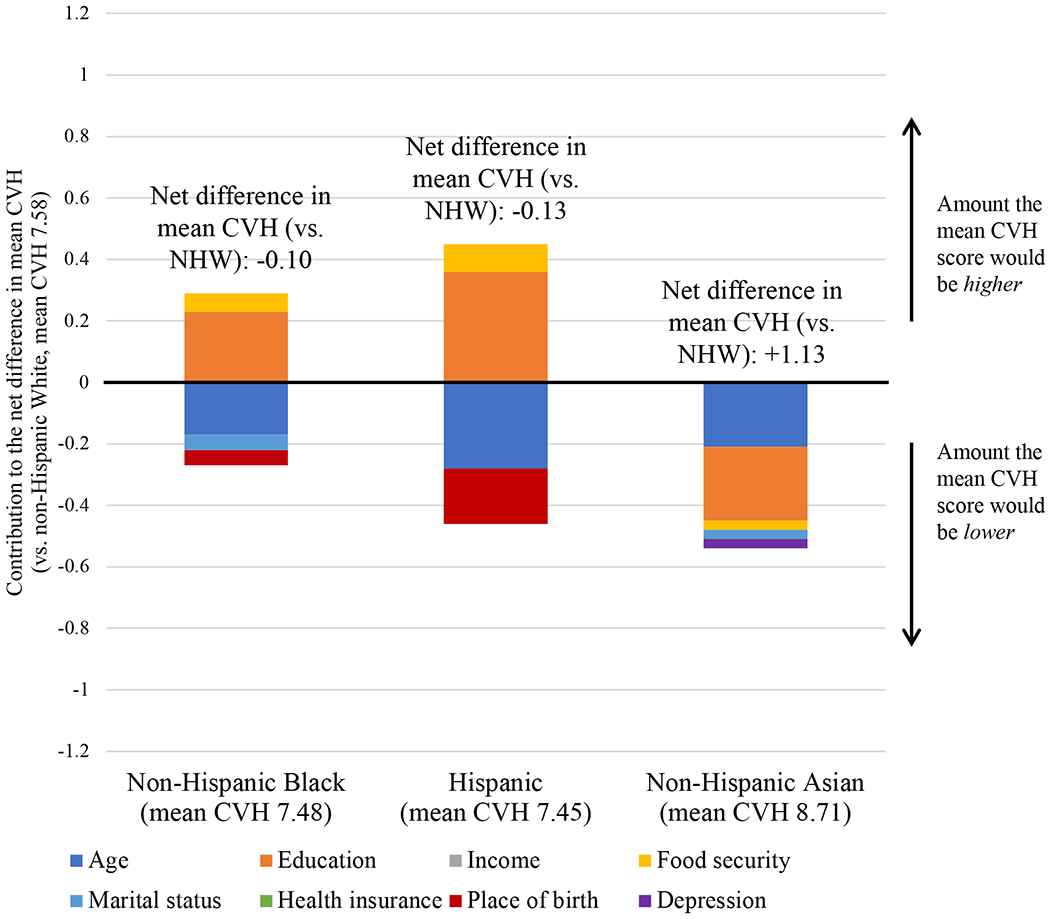
CVH: Cardiovascular health, NHW: Non-Hispanic White. Values above/below 0 indicate the amount the mean CVH score would be higher/lower (respectively) if the distribution of the individual-level factor was equivalent to that of non-Hispanic White males. Factors represented in the bar graphs statistically significantly contributed to the explained component of the net difference in mean CVH between racial and ethnic group compared with non-Hispanic White males (p<0.05). Factors not included in each respective bar did not significantly contribute to the explained component of the difference in mean CVH between racial and ethnic group compared with non-Hispanic White males. Net difference in CVH between racial and ethnic groups is shown in Table 1. The sum of the decomposed effects displayed that are associated with each factor may not equal the overall net difference in mean CVH, because the unexplained component of racial and ethnic differences also contributes to differences in mean CVH between racial and ethnic groups. Quantitative results showing the unexplained component of the difference in mean CVH between racial and ethnic groups is shown in Table 3. Corresponding quantitative results showing the explained component of the difference in mean CVH between racial and ethnic groups is shown in Supplemental Table S3.
Figure 2. Decomposition of the net difference in mean cardiovascular health score between racial and ethnic group among females.
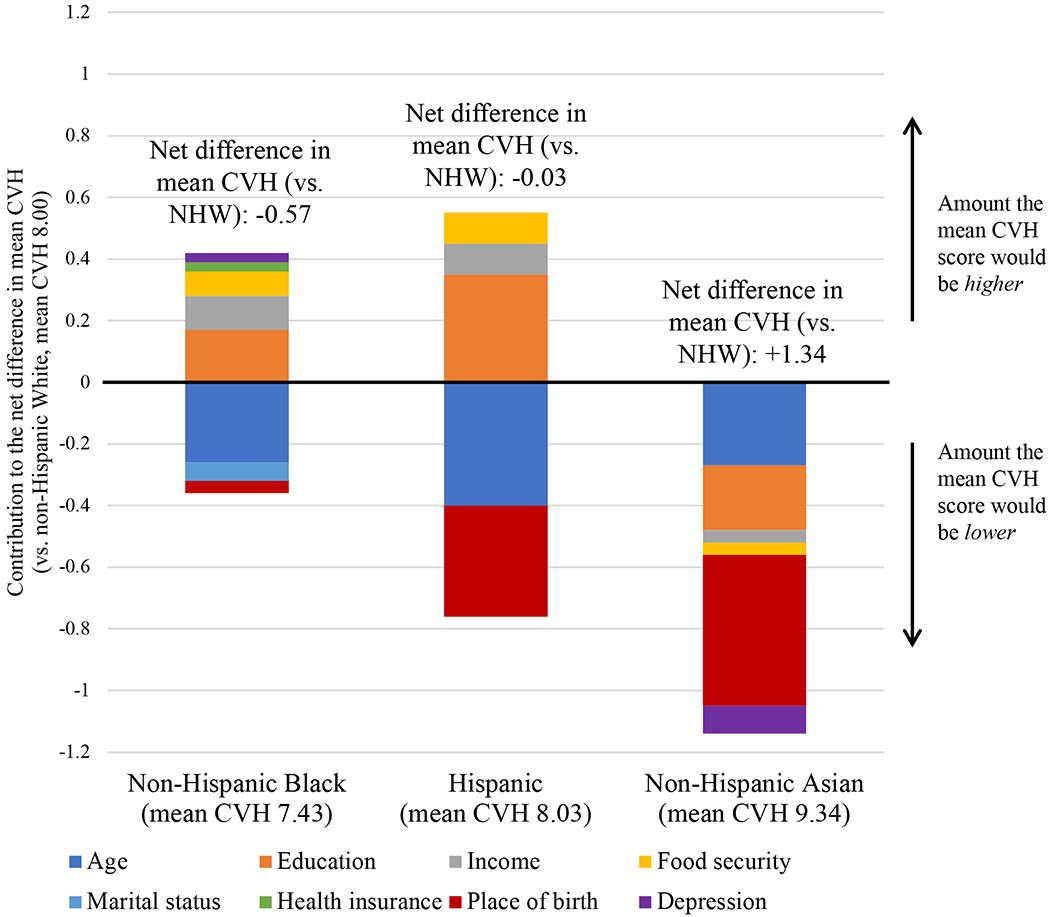
CVH: Cardiovascular health, NHW: Non-Hispanic White. Values above/below 0 indicate the amount the mean CVH score would be higher/lower (respectively) if the distribution of the individual-level factor was equivalent to that of non-Hispanic White females. Factors represented in the bar graphs statistically significantly contributed to the explained component of the net difference in mean CVH between racial and ethnic group compared with non-Hispanic White females (p<0.05). Factors not included in each respective bar did not significantly contribute to the explained component of the difference in mean CVH between racial and ethnic group compared with non-Hispanic White females. Net difference in CVH between racial and ethnic groups is shown in Table 1. The sum of the decomposed effects displayed that are associated with each factor may not equal the overall net difference in mean CVH, because the unexplained component of racial and ethnic differences also contributes to differences in mean CVH between racial and ethnic groups. Quantitative results showing the unexplained component of the difference in mean CVH between racial and ethnic groups is shown in Table 3. Corresponding quantitative results showing the explained component of the difference in mean CVH between racial and ethnic groups is shown in Supplemental Table S3.
For non-Hispanic Black females compared with non-Hispanic White females (Figure 2, Supplemental Table S3), among the individual-level factors the largest magnitude of the CVH difference was explained by education: if non-Hispanic Black females had the same distribution of educational attainment as non-Hispanic White females, their mean CVH score would be significantly higher by 0.17 (0.03) points. For Hispanic and non-Hispanic Asian females compared with non-Hispanic White females, among the individual-level factors the largest magnitude of the CVH difference was explained by place of birth: if Hispanic and non-Hispanic Asian females had the same place of birth distribution as non-Hispanic White females, the mean CVH score of each group would be significantly lower by 0.36 (0.07) points and 0.28 (0.15) points, respectively.
The statistical contributions of the individual-level factors to the “unexplained” component of racial and ethnic differences in CVH are shown in Table 4 for both males and females, reflecting the degree to which between-group differences in the magnitude of association (i.e., regression ß coefficient) of each factor with CVH statistically accounted for differences in mean CVH between groups. The individual-level factors minimally contributed to the unexplained component of the differences in mean CVH. Notably, food security, marital status, and place of birth contributed to the unexplained component of the CVH difference comparing non-Hispanic Black with non-Hispanic White males (p<0.05).
Table 4.
Unexplained component of the Kitagawa-Blinder-Oaxaca decomposition of cardiovascular health differences between racial and ethnic groups, stratified by sex
| NH Black vs. NH White | Hispanic vs. NH White | NH Asian vs. NH White | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Male | Female | Male | Female | Male | Female | |||||||
|
| ||||||||||||
| Diff. in mean CVH | SE | Diff. in mean CVH | SE | Diff. in mean CVH | SE | Diff. in mean CVH | SE | Diff. in mean CVH | SE | Diff. in mean CVH | SE | |
| Age | 0.91 * | 0.22 | 0.72 * | 0.21 | 0.53 * | 0.21 | 1.09 * | 0.19 | −0.05 | 0.27 | 0.42 * | 0.20 |
| Education | −0.03 | 0.03 | 0.03 | 0.03 | −0.04 | 0.02 | −0.03 * | 0.02 | 0.14 | 0.08 | 0.31 * | 0.05 |
| Income | −0.02 | 0.04 | −0.03 | 0.05 | 0.06 | 0.05 | −0.03 | 0.05 | 0.02 | 0.02 | 0.02 | 0.02 |
| Food security | 0.60 * | 0.18 | 0.22 | 0.15 | 0.28 | 0.17 | 0.31 * | 0.12 | 0.50 | 0.26 | −0.12 | 0.26 |
| Marital status | 0.09 * | 0.04 | 0.01 | 0.01 | 0.11 | 0.07 | −0.06 | 0.04 | −0.04 | 0.10 | −0.07 | 0.06 |
| Health insurance | −0.13 | 0.13 | −0.02 | 0.14 | −0.04 | 0.12 | 0.01 | 0.12 | −0.17 | 0.24 | 0.14 | 0.17 |
| Place of birth | 0.84 * | 0.21 | 0.31 | 0.31 | −0.05 | 0.17 | −0.03 | 0.18 | −0.08 | 0.08 | −0.20 * | 0.09 |
| Depression | 0.01 | 0.03 | −0.02 | 0.04 | −0.05 | 0.04 | −0.06 | 0.04 | −0.05 | 0.04 | −0.06 | 0.03 |
| Year | 0.00 | 0.01 | 0.00 | 0.00 | 0.00 | 0.01 | 0.00 | 0.01 | 0.00 | 0.02 | 0.00 | 0.01 |
CVH: Cardiovascular health, NH: Non-Hispanic, SE: Standard error. Difference in mean CVH refers to the absolute difference in mean CVH score related to the unexplained component of racial and ethnic differences in CVH associated with each individual-level factor.
p<0.05.
Discussion
In this sample of participants representing 255 million US adults, several individual-level social and psychosocial factors statistically contributed to differences in CVH among racial and ethnic groups. Fully adjusting for these factors completely attenuated the difference in CVH between non-Hispanic Black and non-Hispanic White males, but only partially attenuated the differences in CVH between non-Hispanic Black and non-Hispanic White females, Hispanic and non-Hispanic White adults, and non-Hispanic Asian and non-Hispanic White adults, suggesting that other factors may additionally contribute to racial and ethnic differences in CVH between these groups. Overall, given the significant association of CVH with incident CVD,8 the statistical contributions of the studied individual-level factors to racial and ethnic differences in CVH suggest that these social and psychosocial determinants may contribute to racial and ethnic differences in CVD incidence in the US population.
Decomposition analysis demonstrated varying magnitudes of contribution of these factors to the net difference in mean CVH between groups. In the “explained” component of the CVH difference between groups, education statistically contributed the largest component of the CVH differences among males, and between non-Hispanic Black females compared with non-Hispanic White females. Educational attainment is inversely associated with the lifetime risk of CVD,26 and directly associated with CVH27 and individual cardiovascular risk factors including diabetes,28 hypertension,29 and obesity.30 The role of education in health may operate through several socioeconomic factors, including literacy, employment opportunity, and healthcare access. Our findings suggest that policy and community strategies to improve educational attainment may be particularly effective to reduce population-level racial and ethnic disparities in CVH.
Differences in place of birth (being born outside or in the US) statistically contributed the greatest magnitude to the net difference in mean CVH in Hispanic and non-Hispanic Asian females compared with non-Hispanic White females. These findings suggest that if a higher percentage of Hispanic and non-Hispanic Asian females were born in the US (i.e., similar to the place of birth distribution of non-Hispanic White females), CVH would be lower (worse) in these groups. These observations are consistent with the “healthy immigrant effect,” which suggests that selective immigration to the US of individuals who are healthier contributes to better population-level health among immigrants in the US.31 While place of birth is not a modifiable factor, these findings should prompt focused efforts to better understand the aspects of birthplace and immigration that may contribute to better CVH. Place of birth is a complex social determinant that reflects a range of factors including immigration, acculturation, and environmental exposures, which in turn may influence CVH-related health behaviors (such as dietary patterns) and socioeconomic position. Our results are consistent with prior findings that place of birth contributes substantially to racial and ethnic differences in population-level CVH,32 particularly for Hispanic and non-Hispanic Asian adults. While our analysis models independent effects of these individual-level factors, these factors interact and operate through multiple pathways to influence CVH.
Few individual-level factors contributed significantly to the “unexplained” component of the difference in CVH between groups. Statistically, the unexplained component of CVH differences accounts for between-group differences in the magnitude of association of each factor with CVH. The “magnitude of association” refers to the regression coefficient for the association of the individual-level factor and CVH score, i.e., the slope of the regression line. For example, the unexplained component captures differences in how much benefit in population-level CVH is conferred by higher educational attainment. Some racial and ethnic groups may derive less health benefits from the same level of education than do others due to unmeasured factors (e.g., discrimination, structural and systemic racism).6 In our findings, the differential magnitude of association of education, food security, marital status, and place of birth with CVH significantly contributed to differences in mean CVH, particularly among non-Hispanic Black males, and Hispanic and non-Hispanic Asian females. Importantly, structural factors like racism are likely captured by several of these explanatory factors, such as income and food insecurity.
Further, age contributed significantly to the unexplained component of CVH differences for non-Hispanic Black and Hispanic adults and non-Hispanic Asian females, which aligns with the weathering hypothesis that chronic exposure to socioeconomic disadvantage over time leads to accelerating declines in health among disadvantaged racial and ethnic groups.33
Several limitations should be considered. First, these cross-sectional observational data are subject to unmeasured confounding. Our findings are intended to be a foundation for potential community- and population-level interventions and policies to address differences and disparities in CVH. Future research with longitudinal data allowing for statistical mediation analyses will supplement our findings about the role of social and psychosocial factors in racial and ethnic differences in CVH. Second, fasting data were available only on a subset of NHANES participants, so our data may underestimate the prevalence of suboptimal glucose. Third, this analysis is limited to the race and ethnicity categories identified in NHANES. Additionally, non-Hispanic White adults were used as the reference group to understand the contributors to differences in CVH experienced by minoritized groups, but we acknowledge that the precedent for using the White racial group as the reference category in population research may contribute to structural biases experienced by individuals in these minoritized groups. Heterogeneity in CVH among Hispanic and Asian subgroups could not be assessed. Fourth, the NHANES data do not identify other groups in the US, including (but not limited to) American Indian/Alaska Native, Middle Eastern and North African, or Native Hawaiian populations. Fifth, these data represent the role of several factors at the population level. Individual-level CVH may be influenced differentially by social and psychosocial determinants depending on personal and environmental contexts. Sixth, this analysis uses the Life’s Simple 7 CVH score (a validated measure of CVH robustly associated with CVD and mortality outcomes) rather than the revised Life’s Essential 8 CVH score that accounts for sleep. While the Life’s Essential 8 CVH score remains to be validated, it is highly correlated to the Life’s Simple 7 score (r=0.88).34 Seventh, a limitation to the KBO decomposition method is its dependence on the factors selected for inclusion in the models. Omitted variables, information bias, or model misspecification may influence the quantification of the explained and unexplained components of CVH differences.20 In the case of this analysis, other factors not included in the analysis likely also contribute to racial and ethnic differences in CVH, such as neighborhood-level factors (e.g., area deprivation, social cohesion).
Conclusions
In this nationally representative sample of US adults, significant differences in CVH among Hispanic, non-Hispanic Asian, and non-Hispanic Black adults compared with non-Hispanic White adults were attenuated by adjusting for a comprehensive set of individual-level factors. Education and place of birth statistically contributed substantially to differences in CVH among racial and ethnic groups. These results may help identify public health intervention strategies to mitigate racial and ethnic differences in CVH.
Supplementary Material
Clinical Perspective.
What is new?
Population-level racial and ethnic differences in cardiovascular health are related to differences in underlying social and psychosocial factors.
Education and place of birth (US nativity) statistically contributed the largest magnitude to racial and ethnic differences in cardiovascular health among US adults.
What are the clinical implications?
Social and psychosocial determinants are important to query and address to improve cardiovascular health and reduce cardiovascular disease disparities.
Addressing underlying factors through clinical, population, and policy interventions may mitigate racial and ethnic differences in cardiovascular health.
Funding Sources
This study was supported in part by National Heart, Lung, and Blood Institute grants K23HL157766 to NSS, and R01HL161514 and R01HL159250 to SSK.
Non-standard Abbreviations and Acronyms
- CARDIA
Coronary Artery Risk Development in Young Adults
- CVD
Cardiovascular disease
- CVH
Cardiovascular health
- KBO
Kitagawa-Blinder-Oaxaca
- NHANES
National Health and Nutrition Examination Surveys
- MEC
Mobile Examination Center
- SE
Standard error
Footnotes
Conflict of Interest Disclosures
The authors report no disclosures or conflicts of interest.
References
- 1.Shah NS, Molsberry R, Rana JS, Sidney S, Capewell S, O’Flaherty M, Carnethon M, Lloyd-Jones DM and Khan SS. Heterogeneous trends in burden of heart disease mortality by subtypes in the United States, 1999-2018: observational analysis of vital statistics. BMJ. 2020;370:m2688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khan SU, Lone AN, Yedlapati SH, Dani SS, Khan MZ, Watson KE, Parwani P, Rodriguez F, Cainzos-Achirica M and Michos ED. Cardiovascular Disease Mortality Among Hispanic Versus Non-Hispanic White Adults in the United States, 1999 to 2018. J Am Heart Assoc. 2022;11:e022857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shah NS, Xi K, Kapphahn KI, Srinivasan M, Au T, Sathye V, Vishal V, Zhang H and Palaniappan LP. Cardiovascular and Cerebrovascular Disease Mortality in Asian American Subgroups. Circ Cardiovasc Qual Outcomes. 2022:101161CIRCOUTCOMES121008651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shah NS, Ning H, Petito LC, Kershaw KN, Bancks MP, Reis JP, Rana JS, Sidney S, Jacobs DR Jr., Kiefe CI, Carnethon MR, Lloyd-Jones DM, Allen NB and Khan SS. Associations of Clinical and Social Risk Factors With Racial Differences in Premature Cardiovascular Disease. Circulation. 2022:101161CIRCULATIONAHA121058311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Havranek EP, Mujahid MS, Barr DA, Blair IV, Cohen MS, Cruz-Flores S, Davey-Smith G, Dennison-Himmelfarb CR, Lauer MS, Lockwood DW, Rosal M and Yancy CW. Social Determinants of Risk and Outcomes for Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2015;132:873–98. [DOI] [PubMed] [Google Scholar]
- 6.Churchwell K, Elkind MSV, Benjamin RM, Carson AP, Chang EK, Lawrence W, Mills A, Odom TM, Rodriguez CJ, Rodriguez F, Sanchez E, Sharrief AZ, Sims M, Williams O and American Heart A. Call to Action: Structural racism as a fundamental driver of health disparities: A Presidential Advisory from the American Heart Association. Circulation. 2020;142:e454–e468. [DOI] [PubMed] [Google Scholar]
- 7.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW, Rosamond WD, American Heart Association Strategic Planning Task F and Statistics C. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. [DOI] [PubMed] [Google Scholar]
- 8.Perak AM, Ning H, Khan SS, Bundy JD, Allen NB, Lewis CE, Jacobs DR Jr., Van Horn LV and Lloyd-Jones DM. Associations of Late Adolescent or Young Adult Cardiovascular Health With Premature Cardiovascular Disease and Mortality. J Am Coll Cardiol. 2020;76:2695–2707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gaye B, Tajeu GS, Vasan RS, Lassale C, Allen NB, Singh-Manoux A and Jouven X. Association of Changes in Cardiovascular Health Metrics and Risk of Subsequent Cardiovascular Disease and Mortality. J Am Heart Assoc. 2020;9:e017458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leng B, Jin Y, Li G, Chen L and Jin N. Socioeconomic status and hypertension: a meta-analysis. J Hypertens. 2015;33:221–9. [DOI] [PubMed] [Google Scholar]
- 11.Leung C, Tester J and Laraia B. Household Food Insecurity and Ideal Cardiovascular Health Factors in US Adults. JAMA Intern Med. 2017;177:730–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brown AF, Liang LJ, Vassar SD, Escarce JJ, Merkin SS, Cheng E, Richards A, Seeman T and Longstreth WT Jr. Trends in Racial/Ethnic and Nativity Disparities in Cardiovascular Health Among Adults Without Prevalent Cardiovascular Disease in the United States, 1988 to 2014. Ann Intern Med. 2018;168:541–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey Data. 2019. Accessed at: https://wwwn.cdc.gov/nchs/nhanes/. Access date: March 31, 2022.
- 14.National Center for Health Statistics. NHANES analytic guidance and brief overview for the 2017-March 2020 pre-pandemic data files. 2021. Accessed at: https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/overviewbrief.aspx?Cycle=2017-2020. Access date: April 11, 2022.
- 15.Havranek EP, Mujahid MS, Barr DA, Blair IV, Cohen MS, Cruz-Flores S, Davey-Smith G, Dennison-Himmelfarb CR, Lauer MS and Lockwood DW. Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015;132:873–898. [DOI] [PubMed] [Google Scholar]
- 16.Solar O and Irwin A. A Conceptual Framework for Action on the Social Determinants of Health: Social Determinants of Health Discussion Paper 2 (Policy and Practice). World Health Organization. 2010. [Google Scholar]
- 17.Kitagawa EM. Components of a difference between two rates. Journal of the American Statistical Association. 1955;50:1168–1194. [Google Scholar]
- 18.Blinder AS. Wage discrimination: Reduced form and structural estimates. The Journal of Human Resources. 1973;8:436–455. [Google Scholar]
- 19.Oaxaca R. Male-female wage differentials in urban labor markets. International Economic Review. 1973;14:693–709. [Google Scholar]
- 20.Rahimi E and Hashemi Nazari SS. A detailed explanation and graphical representation of the Blinder-Oaxaca decomposition method with its application in health inequalities. Emerg Themes Epidemiol. 2021;18:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jackson JW and VanderWeele TJ. Decomposition Analysis to Identify Intervention Targets for Reducing Disparities. Epidemiology. 2018;29:825–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.O’Donnell O, van Doorslaer E, Wagstaff A and Lindelow M. Explaining differences between groups: Oaxaca decomposition. In: Analyzing Health Equity using Household Survey Data: A Guide to Techniques and Their Implementation Washington, DC: The World Bank; 2008. [Google Scholar]
- 23.Cartwright K. Social determinants of the Latinx diabetes health disparity: A Oaxaca-Blinder decomposition analysis. SSM Popul Health. 2021;15:100869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carabello M and Wolfson JA. Mexican immigrant health advantage in metabolic syndrome? Examining the contributions of demographic, socioeconomic, and health behavior characteristics. SSM Popul Health. 2021;16:100932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gaskin DJ, Zare H, Jackson JW, Ibe C and Slocum J. Decomposing Race and Ethnic Differences in CVD Risk Factors for Mid-life Women. J Racial Ethn Health Disparities. 2021;8:174–185. [DOI] [PubMed] [Google Scholar]
- 26.Kubota Y, Heiss G, MacLehose RF, Roetker NS and Folsom AR. Association of Educational Attainment With Lifetime Risk of Cardiovascular Disease: The Atherosclerosis Risk in Communities Study. JAMA Intern Med. 2017;177:1165–1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Johnson AE, Herbert BM, Stokes N, Brooks MM, Needham BL and Magnani JW. Educational Attainment, Race, and Ethnicity as Predictors for Ideal Cardiovascular Health: From the National Health and Nutrition Examination Survey. J Am Heart Assoc. 2022;11:e023438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Borrell LN, Dallo FJ and White K. Education and diabetes in a racially and ethnically diverse population. Am J Public Health. 2006;96:1637–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Howard G, Cushman M, Moy CS, Oparil S, Muntner P, Lackland DT, Manly JJ, Flaherty ML, Judd SE, Wadley VG, Long DL and Howard VJ. Association of Clinical and Social Factors With Excess Hypertension Risk in Black Compared With White US Adults. JAMA. 2018;320:1338–1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cohen AK, Rai M, Rehkopf DH and Abrams B. Educational attainment and obesity: a systematic review. Obes Rev. 2013;14:989–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kennedy S, Kidd MP, McDonald JT and Biddle N. The Healthy Immigrant Effect: Patterns and evidence from four countries. Journal of International Migration and Integration. 2015;16:317–332. [Google Scholar]
- 32.Fryar CD, Fakhouri TH, Carroll MD, Frenk SM and Ogden CL. The association of nativity/length of residence and cardiovascular disease risk factors in the United States. Prev Med. 2020;130:105893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Forde AT, Crookes DM, Suglia SF and Demmer RT. The weathering hypothesis as an explanation for racial disparities in health: a systematic review. Ann Epidemiol. 2019;33:1–18 e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lloyd-Jones DM, Ning H, Labarthe D, Brewer L, Sharma G, Rosamond W, Foraker RE, Black T, Grandner MA, Allen NB, Anderson C, Lavretsky H and Perak AM. Status of Cardiovascular Health in US Adults and Children Using the American Heart Association’s New “Life’s Essential 8” Metrics: Prevalence Estimates from the National Health and Nutrition Examination Survey (NHANES), 2013-2018. Circulation. 2022;146:822–835. [DOI] [PubMed] [Google Scholar]
- 35.Jann B. The Blinder–Oaxaca Decomposition for Linear Regression Models. The Stata Journal. 2008;8:453–479. [Google Scholar]
- 36.Oaxaca RL and Ransom MR. Identification in detailed wage decompositions. Review of Economics and Statistics. 1999;81:154–157. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


