Abstract
Purpose
The current study attempts to investigate the role of anterior cervical discectomy and fusion (ACDF) in alleviating symptoms in patients with cervical vertigo associated with cervical instability.
Methods
The patients of cervical instability with vertigo and dizziness who underwent ACDF between January 2011 and December 2019 were followed-up for more than two years. Demographic data (age, sex, follow up period and levels of instable cervical segments) were assessed; Symptoms of vertigo and dizziness before and after surgery were assessed by the 15-item version of the Vertigo Symptom Scale (VSS) and the 25-item Dizziness Handicap Inventory (DHI). The severity and frequency of other symptoms like neck and occipital pain, gastrointestinal discomfort, nausea, vomiting, tinnitus, palpitations, headache, diplopia and blurring of vision before and after surgery were also assessed.
Results
A total of 92 patients underwent ACDF for cervical instability with vertigo and dizziness between January 2011 and December 2019, of which 79 patients were included in the final analysis. The number of instable levels had no correlation with VSS and DHI scores before surgery (p > 0.05), while patients with C3/4 instability suffering a severer vertigo than other levels. Both DHI and VSS scores were significantly reduced after ACDF and this was sustained within two years after surgery (p < 0.001). Although there was no statistical difference in the ratio of patients with vertigo relief, patients with one-level cervical instability demonstrated a more rapid recovery than patients with multi-level cervical instability (p = 0.048). Also, there was improvement in other symptoms such as neck and occipital pain, gastrointestinal discomfort, nausea, vomiting, tinnitus, palpitations, headache and blurring of vision after surgery.
Conclusions
Vertigo caused by C3/4 instability was severer than other levels such as C4/5 and C5/6. During 2 years' follow-up the significant relief of vertigo and dizziness was observed after anterior cervical surgery. Other accompanying symptoms except hypomnesia were also extenuated in follow-up period.
Keywords: cervical spine, anterior cervical discectomy and fusion, vertigo, dizziness, instability
Introduction
Vertigo is “an illusion of movement”, and it may be rotational, oscillating or tilting in nature. Dizziness can be described as light-headedness, imbalance, giddiness, or unsteadiness, and it is perhaps closest to the definition of vertigo. There are a number of different causes of vertigo including central nervous system and central or peripheral vestibular dysfunction etc. Some patients are suspected that the cause of their problem is a disorder of the cervical spine, known as cervical vertigo (1). In 1955, Ryan and Cope used the term “cervical vertigo” to refer to a combination of cervical spine problems and dizziness (2). It is defined as vertigo induced by changes of position of the neck or vertigo originating from the cervical region. A proportion of patients having cervical instability can complain about varying degrees of symptoms of vertigo and dizziness without myelopathy and/or radiculopathy, and always accompanied by tinnitus, blurred vision, headache, nausea, vomiting, palpitations, and gastrointestinal discomfort etc. The pathophysiology behind the association of these clinical symptoms with mechanical problem is not very clearly known.
Anterior cervical discectomy and fusion (ACDF) is a commonly used approach for cervical instability (3). However, the effect of ACDF on these symptoms is yet to be explored. In this retrospective study, we aimed to investigate whether ACDF is effective in improving vertigo, dizziness, and these accompanied symptoms by comparing their severity before and after surgery.
Materials and methods
Patients
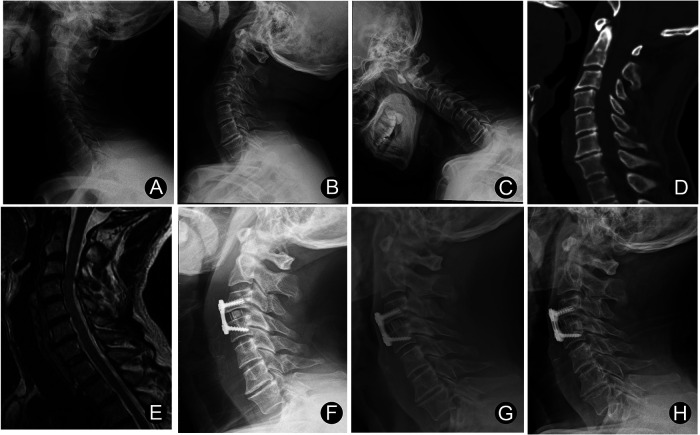
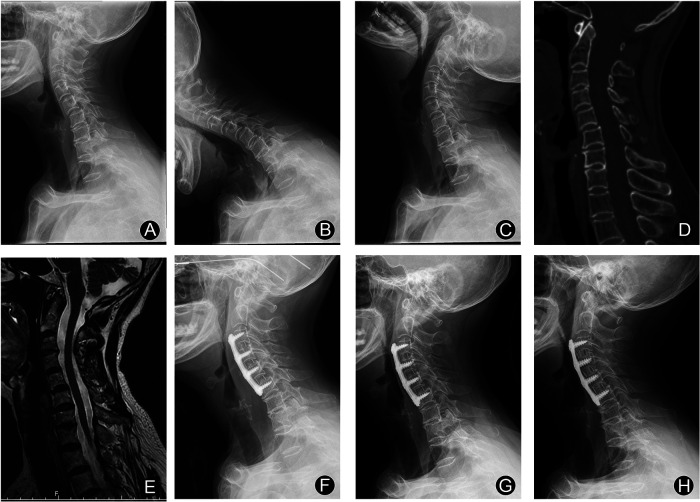
From January 2011 to December 2019, ninety-two cervical instability patients with vertigo and dizziness underwent ACDF with PEEK cages in our institution. Of these patients, 79 were available for follow-up evaluation for more than 2 years after surgery. All patients were followed up at least three times postoperatively, at three months, one year, and two years after surgery. The mean of last follow-up was 29.6 months (range: 24 to 96 months). There were 14 males and 65 females. The ages ranged from 49 to 82 years, with a mean of 67.4 years. For patients with only one level of cervical instability, we performed single-level ACDF (Figure 1). For patients with two or more cervical instability, we performed ACDF on the corresponding segments (Figure 2). At the follow-up, patients underwent postoperative cervical spine x-ray (anteroposterior and lateral projections) and assessment of clinical symptoms such as vertigo, dizziness, neck and occipital pain and so on. This study included patients who had 2 years' follow-up visit after surgery with the complete results of clinical and radiological assessments.
Figure 1.
Male, 57 years old: C3/4 ACDF was experienced. (A–C) Cervical spine x-ray showing C3/4 instability. (D) Preoperative cervical CT sagittal image. (E) Magnetic resonance imaging (MRI) showing no significant compression of the spinal cord. (F) x-ray of cervical spine 3 months after surgery. (G) x-ray of cervical spine 12 months after surgery. (H) x-ray of cervical spine 24 months after surgery.
Figure 2.
Female, 68 years old: three levels of ACDF was experienced. (A–C) Cervical spine x-ray showing C3/4, C4/5 and C5/6 instability. (D) Preoperative cervical CT sagittal image. (E) Magnetic resonance imaging (MRI) showing no significant compression of the spinal cord. (F) x-ray of cervical spine 3 months after surgery. (G) x-ray of cervical spine 12 months after surgery. (H) x-ray of cervical spine 24 months after surgery.
Inclusion and exclusion criteria
The inclusion criteria were as follows: (1) all patients presented vertigo and dizziness without myelopathy or radiculopathy. (2) Flexion-extension x-rays were used to assess stability of the cervical spine, and sagittal translation (>3.5 mm), or segmental angulation (>11°) was typically used to diagnose cervical instability (4). (3) Obvious cervical spinal cord compression was not demonstrated on magnetic resonance imaging (MRI). (4) Diseases relating to neurology, otolaryngology, ophthalmology, and cardiovascular diseases such as Meniere disease, cataract, lacunar infarcts, etc., were excluded. (5) The conservative treatment is ineffectual, and all the patients underwent ACDF. The exclusion criteria were as follows: (1) Alternative etiology of vertigo and dizziness revealed on consultation with neurology, otolaryngology, cardiology or ophthalmology. (2) A history of cervical spine trauma or surgery.
Methods
All the patients underwent a clinical evaluation. A cervical spine examination was mainly performed to assess cervical mobility by standard flexion-extension x-ray imaging. A neurological assessment was completed by the brain MRI examination and evaluating of the strength of the four limbs, surface and deep sensitivity and coordination. In addition, a comprehensive ENT examination including an electronystagmogram was used in order to rule out potentially balance-altering vestibular damage. In the absence of abnormal clinical examination results, we considered that a patient's vertigo and dizziness was non-vestibular.
Perceived frequency and severity of vertigo and dizziness was assessed by the 15-item version of the Vertigo Symptom Scale (VSS) (5). The scale has 5 response categories (0–4). Total scale scores range between 0 and 60 points, severe dizziness: ≥12 points. clinically significant change: ≥3 points.
Perceived disability was assessed by the 25-item Dizziness Handicap Inventory (DHI) which has 3 response categories (0; 2; 4). Total scores range from 0 to 100 points (23), interpreted as mild 0–30; moderate 31–60; severe 61–100 (6).
To evaluate the outcome of surgery, the closest minimally clinical important difference (MCID) in terms of follow-up was used 11 for the VSS and 17 for DHI at the term of 2 years.
In addition to vertigo and dizziness, other symptoms such as neck and occipital pain, gastrointestinal discomfort, nausea, vomiting, tinnitus, palpitations, headache, hypomnesia, diplopia and blurring of vision before and after surgery were also recorded.
As there is no standardized method to assess the severity and frequency of neck and occipital pain, gastrointestinal discomfort, nausea, vomiting, tinnitus, palpitations, headache, hypomnesia and blurring of vision, we used a scale to objectively record the data. The outcomes were the intensity and frequency of these symptoms. The intensity was measured with a 100 mm visual analogue scale (VAS). Total scale scores range between 0 and 100 points, clinically significant change: ≥10 points.
Statistical analysis
Quantitative information is presented as mean and standard deviation. The Shapiro–Wilk test was used to test the normality of continuous data. One-way repeated measures analysis of variance (ANOVA) was used to compare the indicators in the same group at different time points, while Friedman test was used for data that does not fit Gaussian distribution. Multiple comparison analysis between groups was analyzed using least significant difference (LSD). Binary and categorical indicators between groups were compared using the exact two-way Fisher criterion. The comparison of categorical variables before and after surgery was performed using the McNemar criterion. Binary logistic regression was used to investigate whether age, sex and surgery in different cervical levels influences the amelioration of vertigo and dizziness. The log-rank criterion was used to analyze the relief of vertigo after single-level and multi-levels cervical spine surgery in three weeks. Statistical significance was defined by p < 0.05. Data were analyzed using SPSS software version 21 for Windows 11.
Results
General results
A total of 79 patients underwent ACDF for cervical instability with cervical vertigo and dizziness were included in the final analysis. The main characteristics of patients are presented in Table 1. Most of the patients with cervical instability (65/79, 82.3%) were female. Among the patients, the majority had one-level cervical instability (60/79, 75.9%). The most common level of instability was C3–4 (n = 46, 46.0%) followed by C4–5 (n = 40, 40.0%) and C5–6 (n = 14, 14.0%). There was no significant association between the number of instability levels and symptoms of vertigo and dizziness as measured by VSS (p = 0.724) and DHI (p = 0.780) (Table 2). Vertigo and dizziness caused by the instability of C3/4 are significantly worse than those caused by C4/5 or C5/6, as evidenced by VSS and DHI scores (Table 3).
Table 1.
Basic data of patients (x ±, n = 79).
| Characteristics | No. of patients (n = 79) |
|---|---|
| Age at surgery | 67.4 center8.2 |
| Sex | |
| Male | 14 (17.7%) |
| Female | 65 (82.3%) |
| Levels of instability segments | |
| One-level | 60 (75.9%) |
| Two-levels | 17 (21.5%) |
| Three-levels | 2 (2.5%) |
| Numbers of surgical segments | |
| C3/4 | 46 (46.0%) |
| C4/5 | 40 (40.0%) |
| C5/6 | 14 (14.0%) |
| follow-up period, months | 29.6 ± 9.6 |
Table 2.
Preoperative VSS and DHI scores in patients with different numbers of instability segments (x ±, n = 79).
| Parameters | One-level | Two-levels | Three-levels | F | p |
|---|---|---|---|---|---|
| VSS | 22.8 ± 4.0 | 22.2 ± 4.5 | 24.5 ± 0.7 | 0.324 | 0.724 |
| DHI | 37.8 ± 4.7 | 38.5 ± 3.4 | 39.5 ± 2.1 | 0.250 | 0.780 |
VSS, Vertigo Symptom Scale; DHI, Dizziness Handicap Inventory.
Table 3.
Preoperative VSS and DHI scores in patients with different cervical segments (x ±, n = 79).
| Parameters | C3/4 (n = 32) | C4/5 (n = 21) | C5/6 (n = 7) | C3-5 (n = 12) | C4-6 (n = 5) | C3-6 (n = 2) | F | p |
|---|---|---|---|---|---|---|---|---|
| VSS | 24.4 ± 3.5 | 21.4 ± 4.0a | 19.9 ± 3.2b | 22.2 ± 3.7 | 22.4 ± 6.6 | 24.5 ± 0.7 | 2.63 | 0.031 |
| DHI | 39.7 ± 4.6 | 36.0 ± 4.3a | 34.9 ± 2.8b | 38.4 ± 3.7 | 38.6 ± 3.2 | 39.5 ± 2.1 | 2.91 | 0.019 |
Note: Comparison of preoperative VSS and DHI scores between C3/4 and C4/5.
p < 0.05; Comparison of preoperative VSS and DHI scores between C3/4 and C5/6.
p < 0.05.
Vertigo and dizziness
Vertigo and dizziness assessed by DHI and VSS were significantly relieved after ACDF and this was sustained at the final follow-up (Table 4). In fact, within 10 days after surgery, the relief of vertigo and dizziness was observed. Compared with single-level ACDF, two or three levels ACDF has slower symptom relief (Figure 3). About half of patients experienced significant improvement in vertigo within 4 days after single-level ACDF, while it extended to 9 days in multi-level ACDF. Although means of VSS and DHI scores decreased obviously at 12 and 24 months compared with those at 3 months, there was no statistically significant difference between scores at 12 months and 24 months after surgery.
Table 4.
VSS and DHI scores before and after surgery (x ±, n = 79).
| Parameters | before surgery | 3 months after surgery | 12 months after surgery | 24 months after surgery | F | p |
|---|---|---|---|---|---|---|
| VSS | 22.7 ± 4.0 | 6.8 ± 4.0a | 5.8 ± 2.9a | 5.4 ± 2.7a | 140.7 | <0.001 |
| DHI | 38.0 ± 4.4 | 13.8 ± 4.7a | 13.0 ± 3.7a | 12.9 ± 3.8a | 640.3 | <0.001 |
Note: Comparison of VSS and DHI scores between before surgery and after surgery.
p < 0.05.
Figure 3.
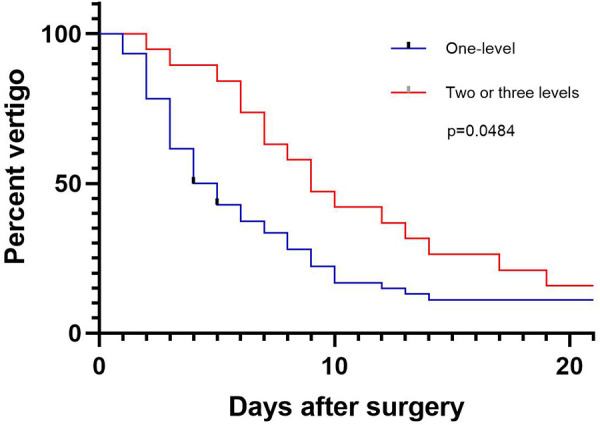
Percentage of patients with residual vertigo within three weeks after ACDF.
As an effective method of assessing the validity of scale, MCID is earning its place and recognition by patients and clinical doctors. Consequently, we evaluated the alleviating effects of ACDF on vertigo and dizziness using the MCID of VSS and DHI scales. As shown in Table 5, most patients (89.9%) achieved MCID after surgery and there is no significant difference in the ratio of achieving MCID between patients accepting one-level ACDF and multi-level ACDF. Figure 4 shows the number of patients who failed to achieve MCID at different cervical levels as measured by VSS and DHI scores.
Table 5.
Patient-reported outcomes during follow-up terms (n = 79).
| Parameter | Levels of instability segments | n | p | |
|---|---|---|---|---|
| One-level | > One-level | |||
| VSS | ||||
| Achieved MCID | 53 (88.3%) | 18 (94.7%) | 71 (89.9%) | 0.672 |
| Not achieved MCID | 7 (11.7%) | 1 (5.3%) | 8 (10.1%) | |
| DHI | ||||
| Achieved MCID | 54 (90.0%) | 17 (89.5%) | 71 (89.9%) | >0.99 |
| Not achieved MCID | 6 (10.0%) | 2 (10.5%) | 8 (10.1%) | |
MCID, Minimally clinical important difference.
Figure 4.
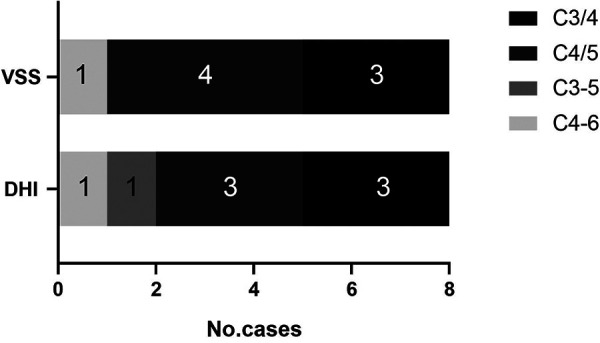
Distribution of levels of cervical spine failing to meet MCID assessed by VSS and DHI.
Furthermore, we investigated factors influencing the efficacy of ACDF on vertigo according to whether the MCID of VSS and DHI were both achieved. Although the preoperative scores of VSS and DHI varied with the levels of instable cervical segments, logistic regression showed that there was no significant correlation between postoperative amelioration of vertigo and the level of instable cervical segments such as involving C3/4 (OR = 0.386, p = 0.338), involving C4/5 (OR = 1.199, p = 0.849) and C5/6 (OR = 1.027, p = 0.980) (Table 6). Also, the correlation between postoperative amelioration of vertigo, age (OR = 1.046, p = 0.339) and sex (OR = 0.457, p = 0.371) was not observed.
Table 6.
Odds ratio, 95% CI and P value association using multiple factors logistic regression models for vertigo meeting the MCID including cervical levels.
| Parameter | Odds ratio | 95% CI | p |
|---|---|---|---|
| C3/4 (involved) | 0.386 | (0.055, 2.706) | 0.338 |
| C4/5 (involved) | 1.199 | (0.185, 7.785) | 0.849 |
| C5/6 (involved) | 1.027 | (0.133, 7.930) | 0.980 |
| Age | 1.046 | (0.954, 1.148) | 0.339 |
| Sex | 0.457 | (0.082, 2.536) | 0.371 |
Distribution of accompanying symptoms
The distribution of symptoms has been illustrated in Table 7. Besides vertigo and dizziness, out of 79 patients, blurring of vision (59/79, 74.7%) was the most common accompanying symptoms followed by tinnitus (58/79, 73.4%) and headache (56/79, 70.9%) before surgery. All accompanying symptoms were obviously extenuated 3 months after ACDF except hypomnesia (Table 8). Compared to preoperative symptoms, treatment with ACDF surgery has a significant effect on reducing the ratio of patients with neck and occipital pain (p < 0. 001), gastrointestinal discomfort (p = 0. 007), nausea (p = 0.004), tinnitus (p < 0.001), vomiting (p = 0.003), palpitation (p < 0.001), headache (p < 0.001) and blurred vision (p < 0.001). Diplopia in two patients disappeared after surgery. Although most patients experienced symptom relief after surgery, there was no significant effect on the relief of hypomnesia (p = 0.302) in patients experiencing ACDF (Tables 9–11).
Table 7.
Number and incidence of other symptoms accompanied with vertigo.
| symptoms | No. cases | Percent (%) |
|---|---|---|
| vertigo and dizziness | 79 | 100 |
| neck and occipital pain | 53 | 67.1 |
| gastrointestinal discomfort | 35 | 44.3 |
| nausea | 29 | 36.7 |
| vomiting | 17 | 21.5 |
| tinnitus | 58 | 73.4 |
| palpitations | 43 | 54.4 |
| headache | 56 | 70.9 |
| hypomnesia | 37 | 46.8 |
| diplopia | 2 | 2.5 |
| blurring of vision | 59 | 74.7 |
Table 8.
Severity of symptoms accompanied with vertigo before and after surgery (x ±).
| Parameter | Before surgery | 3 months after surgery | 12 months after surgery | 24 months after surgery | F | p |
|---|---|---|---|---|---|---|
| Neck and occipital pain (n = 53) | 38.0 ± 7.7 | 13.9 ± 6.7a | 10.8 ± 5.5b | 9.3 ± 4.6 | 303.1 | <0.001 |
| Gastrointestinal discomfort (n = 35) | 38.9 ± 6.5 | 11.0 ± 4.7a | 10.7 ± 4.6 | 10.3 ± 5.1 | 337.9 | <0.001 |
| Nausea (n = 29) | 31.4 ± 6.1 | 11.2 ± 4.3a | 9.9 ± 4.1 | 10.0 ± 4.3 | 162.1 | <0.001 |
| Vomiting (n = 17) | 36.7 ± 5.6 | 6.6 ± 3.7a | 5.7 ± 3.3 | 5.0 ± 2.6 | 306.9 | <0.001 |
| Tinnitus (n = 58) | 29.4 ± 4.4 | 11.9 ± 4.6a | 10.7 ± 4.4 | 9.6 ± 4.6 | 339.4 | <0.001 |
| Headache (n = 56) | 42.4 ± 7.3 | 11.8 ± 5.6a | 10.4 ± 5.7 | 10.0 ± 5.3 | 461.7 | <0.001 |
| Blurring of vision (n = 59) | 46.8 ± 8.3 | 16.2 ± 7.3a | 14.9 ± 7.5 | 14.0 ± 7.3 | 341.6 | <0.001 |
| Hypomnesia (n = 37) | 12.3 ± 2.1 | 11.9 ± 3.8 | 10.9 ± 4.8 | 11.4 ± 4.7 | 1.69FD | 0.6386 |
| Palpitations (n = 43) | 36.8 ± 6.3 | 13.4 ± 5.0a | 12.1 ± 5.3 | 10.1 ± 5.2c | 323.2 | <0.001 |
Note: Comparison of symptoms accompanied with vertigo between before surgery and 3 months after surgery.
p < 0.05; Comparison of symptoms accompanied with vertigo between 3 months after surgery and 12 months after surgery.
p < 0.05; Comparison of symptoms accompanied with vertigo between 12 months after surgery and 24 months after surgery.
p < 0.05; FD, Friedman test.
Table 9.
Number of patients with neck and occipital pain, gastrointestinal discomfort or blurring of vision before and after surgery. (x ±, n = 79).
| Symptom | Neck and occipital pain (After surgery) | Gastrointestinal discomfort (After surgery) | Blurring of vision (After surgery) | |||
|---|---|---|---|---|---|---|
| Symptomatic | Symptomless | Symptomatic | Symptomless | Symptomatic | Symptomless | |
| Symptomatic (Before surgery) | 28 | 25 | 22 | 13 | 41 | 18 |
| Symptomless (Before surgery) | 1 | 25 | 2 | 42 | 2 | 18 |
| P | <0.001 | 0.007 | <0.001 | |||
Note: Comparison of neck and occipital pain, gastrointestinal discomfort and blurring of vision before and after surgery.
Table 11.
Number of patients with hypomnesia, headache or palpitations before and after surgery. (x ±, n = 79).
| Symptom | Hypomnesia (After surgery) | Headache (After surgery) | Palpitations (After surgery) | |||
|---|---|---|---|---|---|---|
| Symptomatic | Symptomless | Symptomatic | Symptomless | Symptomatic | Symptomless | |
| Symptomatic (Before surgery) | 27 | 10 | 29 | 27 | 18 | 25 |
| Symptomless (Before surgery) | 5 | 37 | 3 | 20 | 2 | 34 |
| P | 0.302 | <0.001 | <0.001 | |||
Note: Comparison of hypomnesia, headache or palpitations before and after surgery.
Table 10.
Number of patients with nausea, vomiting or tinnitus before and after surgery. (x ±, n = 79).
| Symptom | Nausea (After surgery) | Vomiting (After surgery) | Tinnitus (After surgery) | |||
|---|---|---|---|---|---|---|
| Symptomatic | Symptomless | Symptomatic | Symptomless | Symptomatic | Symptomless | |
| Symptomatic (Before surgery) | 15 | 14 | 0 | 17 | 28 | 30 |
| Symptomless (Before surgery) | 3 | 47 | 3 | 59 | 1 | 20 |
| P | 0.004 | 0.003 | <0.001 | |||
Note: Comparison of nausea, vomiting or tinnitus before and after surgery.
Discussion
To date, the etiology and mechanisms of cervical vertigo are still unknown, conservative therapy has been the main treatment which has been unsatisfactory. Some studies (7–9) manifested that ACDF improved the sympathetic symptoms like vertigo, headache, nausea, vomiting and gastrointestinal discomfort in patients with cervical radiculopathy and/or myelopathy. This doesn't mean that all patients who have cervical spondylosis with concomitant vertigo and dizziness should be treated with anterior cervical surgery. Treatment of cervical vertigo is complicated in patients who have chronic neck pain and concomitant vertigo and dizziness but without cervical disc herniation or compression of nerve root and spinal cord.
In 1928, Pearce and Barré–Liéou (10) suggested that cervicogenic dizziness was due to an abnormal input from the cervical sympathetic nerves. They proposed that the posterior sympathetic plexus could be mechanically irritated by degenerative arthritis and induce reflex vertebrobasilar vasoconstriction and symptoms of vertigo and dizziness. It is well known that cervical spinal tissues are rich in sympathetic fibers. The cervical dura mater and the posterior longitudinal ligament have different sympathetic innervation patterns (11). In addition, the cervical sympathetic trunk consists of a main trunk and two to four ganglia which are located anterior to the transverse processes (12, 13). We speculated that abnormal motion of the cervical segment may stimulate the sympathetic nervous system other than the vertebral artery which induces symptoms such as vertigo, dizziness, tinnitus, nausea, vomiting, palpitations, headache, hypomnesia, and gastrointestinal discomfort.
Some authors have attributed cervical vertigo to the dynamic vertebrobasilar insufficiency (14, 15). In other words, at least in a subset of dizzy patients with degenerative cervical spine disorders, the cause of dizziness on turning the neck could be due to the reduced vertebral blood flow. The complementary tests used to diagnose vertebrobasilar insufficiency are still controversial. As a consequence of the fact that vertebral artery stenosis is transitory, the use of these tests in asymptomatic patients is usually negative. Vertebrobasilar insufficiency secondary to cervical instability may be a mechanism in patients with vertigo and dizziness in our study.
ACDF surgery contributing to segmental cervical vertebrae fixation and fusion seems to be an effective surgical treatment modality for alleviating vertigo, dizziness and other sympathetic symptoms caused by cervical instability. We included patients who have cervical instability with vertigo and dizziness, and the main symptoms are vertigo and dizziness but not neck pain in study. And our study revealed that symptoms of vertigo and dizziness relieved after anterior cervical surgery and the surgical results were encouraging.
MCID indicates minimum clinically important differences and is an important metric in evaluating resolution of symptoms (16, 17). However, there is no consensus on the MCID value for VSS and DHI. Emasithi A has reported 17 as the MCID of DHI-TH (Thai version of the Dizziness Handicap Inventory) (18). The MCID of VSS and DHI used in this study were obtained numerically by using anchor-based method. To better assess the effectiveness of ACDF surgery on vertigo and dizziness resolution, we divided patients into two groups depending on whether the MCID of VSS and DHI was achieved. About 90% patients get a satisfactory improvement in vertigo and dizziness while the number of surgical levels didn’t influence the symptom relief.
Also, there was improvement in severity and frequency of other symptoms such as neck and occipital pain, gastrointestinal discomfort, nausea, vomiting, tinnitus, palpitations, headache, diplopia and blurring of vision after surgery. Though the specific mechanism of ACDF in improving these symptoms are not clearcut, the anterior cervical surgery might be useful to reduce abnormal motion of the cervical segment which lead to the aberrant stimulation of sympathetic nerves.
Although our preliminary results are encouraging, long-term follow-up of the surgically treated cases are still needed. Moreover, randomized controlled studies are warranted to further investigate the surgical outcome of cervical vertigo.
In summary, the diagnosis and treatment of cervical vertigo still remain controversial. Patients with cervical instability may have symptoms of vertigo and dizziness, and successful clinical results in terms of symptom improvement can be obtained in such patients with anterior cervical surgery. Relief of vertigo and dizziness following anterior surgery can be attributed to stabilization of the cervical segment, the elimination of irritation of sympathetic plexus and vertebrobasilar insufficiency. With other causes of the symptoms dismissed, anterior cervical surgery becomes an option when conservative treatment fails.
Limitations
Our present study has limitation. Few patients underwent three-level cervical surgery, these patients were included in the two-level group in partial analysis.
Conclusion
The most severe symptoms of vertigo are caused by C3/4 instability and the number of levels of instability segments are not significantly influenced. The present study indicated that ACDF can relieve vertigo and dizziness caused by cervical instability and most of the accompanying symptoms could also be greatly extenuated.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by This study was approved by the Ethics Committee of Xinhua Hospital Affiliated to Shanghai Jiaotong University School of Medicine. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
HZ and BL wrote the article. SS and PC were responsible for data collection and analysis. SJ was responsible for reviewing the data. LJ and SJ were responsible for reviewing and revising the article. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1.Reid SA, Rivett DA. Manual therapy treatment of cervicogenic dizziness: a systematic review. Man Ther. (2005) 10(1):4–13. 10.1016/j.math.2004.03.006 [DOI] [PubMed] [Google Scholar]
- 2.Cope S, Ryan GM. Cervical and otolith vertigo. J Laryngol Otol. (1959) 73(2):113–20. 10.1017/S0022215100055018 [DOI] [PubMed] [Google Scholar]
- 3.Chung TT, Hueng DY, Lin SC. Hybrid strategy of two-level cervical artificial disc and intervertebral cage: biomechanical effects on tissues and implants. Medicine (Baltimore). (2015) 94(47):e2048. 10.1097/MD.0000000000002048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang XD, Feng MS, Hu YC. Establishment and finite element analysis of a three-dimensional dynamic model of upper cervical spine instability. Orthop Surg. (2019) 11(3):500–9. 10.1111/os.12474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yardley L, Masson E, Verschuur C, Haacke N, Luxon L. Symptoms, anxiety and handicap in dizzy patients: development of the vertigo symptom scale. J Psychosom Res. (1992) 36(8):731–41. 10.1016/0022-3999(92)90131-K [DOI] [PubMed] [Google Scholar]
- 6.Jacobson GP, Newman CW. The development of the dizziness handicap inventory. Arch Otolaryngol. (1990) 116(4):424–7. 10.1001/archotol.1990.01870040046011 [DOI] [PubMed] [Google Scholar]
- 7.Sharma R, Garg K, Agrawal S, Mishra S, Gurjar HK, Tandon V, et al. Atypical symptoms of cervical spondylosis: is anterior cervical discectomy and fusion useful? - an institutional experience. Neurol India. (2021) 69(3):595–601. 10.4103/0028-3886.319234 [DOI] [PubMed] [Google Scholar]
- 8.Hong L, Kawaguchi Y. Anterior cervical discectomy and fusion to treat cervical spondylosis with sympathetic symptoms. J Spinal Disord Tech. (2011) 24(1):11–4. 10.1097/BSD.0b013e3181dd80f5 [DOI] [PubMed] [Google Scholar]
- 9.Peng B, Yang L, Yang C, Pang X, Chen X, Wu Y. The effectiveness of anterior cervical decompression and fusion for the relief of dizziness in patients with cervical spondylosis: a multicentre prospective cohort study. Bone Joint J. (2018) 100-b(1):81–7. 10.1302/0301-620X.100B1.BJJ-2017-0650.R2 [DOI] [PubMed] [Google Scholar]
- 10.Pearce JM. Barré-Liéou “syndrome”. J Neurol Neurosurg Psychiatry. (2004) 75(2):319. 10.1136/jnnp.2003.014324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yamada H, Honda T, Yaginuma H, Kikuchi S, Sugiura Y. Comparison of sensory and sympathetic innervation of the dura mater and posterior longitudinal ligament in the cervical spine after removal of the stellate ganglion. J Comp Neurol. (2001) 434(1):86–100. 10.1002/cne.1166 [DOI] [PubMed] [Google Scholar]
- 12.Kiray A, Arman C, Naderi S, Güvencer M, Korman E. Surgical anatomy of the cervical sympathetic trunk. Clin Anat. (2005) 18(3):179–85. 10.1002/ca.20055 [DOI] [PubMed] [Google Scholar]
- 13.Saylam CY, Ozgiray E, Orhan M, Cagli S, Zileli M. Neuroanatomy of cervical sympathetic trunk: a cadaveric study. Clin Anat. (2009) 22(3):324–30. 10.1002/ca.20764 [DOI] [PubMed] [Google Scholar]
- 14.Piñol I, Ramirez M, Saló G, Ros AM, Blanch AL. Symptomatic vertebral artery stenosis secondary to cervical spondylolisthesis. Spine. (2013) 38(23):E1503–5. 10.1097/BRS.0b013e3182a43441 [DOI] [PubMed] [Google Scholar]
- 15.Shende C, Rathod T, Marathe N, Mohanty S, Kamble P, Mallepally AR, et al. Degenerative cervical spondylosis: a cause of vertigo? Global Spine J. (2021) 21925682211027840. 10.1177/21925682211027840. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sedaghat AR. Understanding the minimal clinically important difference (MCID) of patient-reported outcome measures. Otolaryngology. (2019) 161(4):551–60. 10.1177/0194599819852604 [DOI] [PubMed] [Google Scholar]
- 17.Bloom DA, Kaplan DJ, Mojica E, Strauss EJ, Gonzalez-Lomas G, Campbell KA, et al. The minimal clinically important difference: a review of clinical significance. Am J Sports Med. (2021) 3635465211053869. 10.1177/03635465211053869. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 18.Emasithi A, Pakdee S, Isaradisaikul SK, Uthaikhup S. Translation and validation of the dizziness handicap inventory into Thai language. OtolNeurotol. (2022) 43(2):e252–e8. 10.1097/MAO.0000000000003391 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.