Abstract
Complex femur fractures are defined as combined fractures of shaft and proximal or the distal femur. It usually occurs in young adults due to high energy trauma. Treatment of this type of fracture is challenging. Herein, we present the management of multi-level complex femoral fracture in 38 years old using minimally invasive overlapping dual plating with bridge proximal femoral locking plate from above and distal femoral locking plate from below. Favourable clinical and radiologic outcomes were observed. The result demonstrates dual plating of complex femoral fracture using MIPO could be considered as a suitable treatment option for complex femoral fracture.
Keywords: Complex femoral fracture, Dual plating, Minimally invasive plate osteosynthesis
Introduction
Complex femur fractures are defined as combined fractures of shaft and proximal or distal femur [1]. Multifocal femoral fractures are responsible for only 5 % of femoral fractures [2]. Treatment of this type of fracture is challenging [3]. Single implant option may be grossly inadequate to manage the fractures. Multiple methods were used to manage complex femoral fractures with varying degree of successes [4]. In this case report a patient with markedly comminuted proximal femoral diaphyseal and distal segmental fractures is presented. The fractures are grossly unstable and require operative care. To the best of our knowledge this pattern of complex fracture is rare in the literature with little or no report on the type of fixation. In this case, a minimally invasive approach which involves over-lapping of dual plating is used. A bridge proximal femoral locking plating and a rigid distal femoral locking plating were used above and below, respectively.
Case report
A 38 year old male patient presented to our accident and emergency with closed injury to the right thigh following a road traffic accident that was characterised by pain, deformity, swelling and inability to bear weight. He was a back-seat passenger of a car that had a head-on collision with another car at high speed with impact from his right side. There was no loss of consciousness or injury to any other part of the body. Examination revealed a patient in painful distress, having markedly swollen and tender right thigh. Plain radiograph of the right thigh showed segmental comminuted fracture involving proximal half of the right femur and two distal transverse fractures (Fig. 1).
Fig. 1.
Preoperative plain radiograph showing multi-level complex femoral fracture.
He had initial resuscitation and was counselled for open reduction and internal fixation using dual plating. The patient was booked for elective surgery and consultation was sent to the anaesthesia department for review. The Anaesthetist after reviewing the patient made a confirmation that the patient was fit for the surgery with American society of Anaesthesiologist class 11. Written informed consent was gotten from the patient and fasting guidelines were given to the patient. Two pints of blood were grouped and cross matched for the surgery. Also, the patient was counselled for subArachnoid block on which the patient consented.
On the day of the surgery, the patient was brought into the theatre. The patient vitals were taken after attaching a multi-parameter monitor. The patient was pre-loaded with intravenous fluid before the SubArachnoid block was given using 12.5 mg of heavy bupivacaine using size 25 spinal needle at l3/l4 interspace.
The surgery was commenced after confirmation of motor blockade up to T6 level. Surgical asepsis was ensured. Minimally invasive plate osteosynthesis approach was employed with aid of image intensifier. Three lateral incisions were made to access the femur (Fig. 2).
Fig. 2.
Minimally invasive plate osteosynthesis incisions.
Indirect reduction using ligamentotaxis was employed to have a relative reduction of the proximal fragments as well as fluoroscopic guidance. Two locking plates were inserted. The proximal femoral Locking Plate (PFLP) antegrade and the distal femoral Locking Plate (DFLP) retrograde. The two plates were overlapped and transfixed to the bone via corresponding holes using two cortical screws around the overlap (Fig. 3).
Fig. 3.
Clinical photograph showing both PFLP and DFLP after fixation.
Wounds were copiously irrigated and closed over a suction drain having two drainage tubes.
He was put on analgesics, DVT prophylactic and antibiotics prophylactic. He had a suitable post-operative recovery. The drain was removed on the second postoperative day. He was mobilised using axillary crutches, non-weight bearing on the right lower limb. He was discharged on the 5th day post-operative to present at 2 weeks for removal of wound stitches. Partial weight bearing and full weight bearing ambulation were allowed at 6 weeks and 12 weeks respectively under the supervision of a physiotherapist.
Result
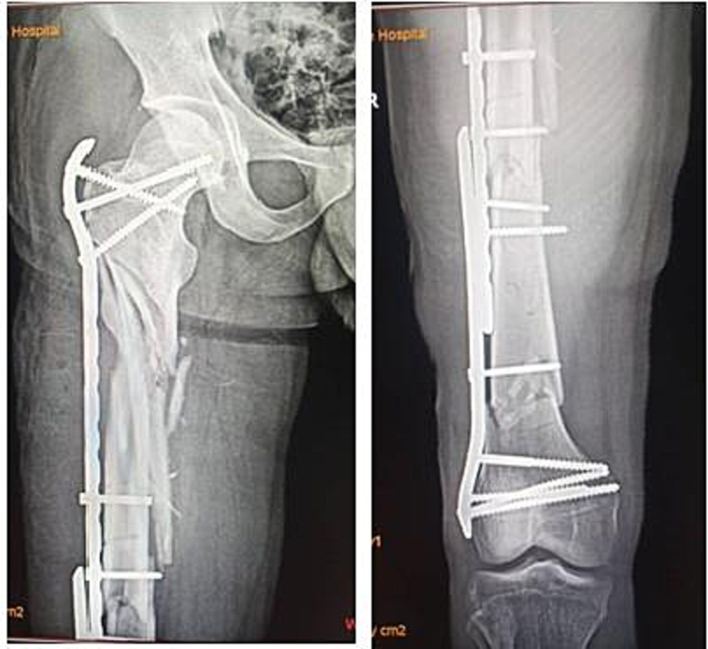
Clinical and radiographic parameters were used to evaluate the patient post operatively. He had 1 year post-operative follow up at a surgical outpatient clinic using serial radiographs, taken at immediate post, 6 weeks, 12 weeks, 6 months and 9 months. Immediate Post-operative radiograph showed acceptable fixation (Fig. 4).
Fig. 4.
Immediate post-operative radiograph.
Radiographic union score for tibia (RUST) [5] was used to assess the union of proximal bridge plating bridging callus was noticed on all cortices with RUST scores 8 and 12 noticed on 6 months (Fig. 5) and 9 months (Fig. 6) post-operative radiographs respectively. Progressive obliteration of fracture lines of distal segmental fracture was noted with complete obliteration on the 9 month postoperative radiograph (Fig. 6).
Fig. 5.
6 month postoperative radiograph showing bridging callus at the comminuted fracture site and obliteration of segmental fracture sites.
Fig. 6.
Nine month's postoperative radiographs showing united fracture sites.
Parker and palmer mobility score [6] was used to assess the clinical recovery of this patient. At 6 months post-operative, he was able to walk around his daily activities unaided with a full parker and Palmer score of 9.
Discussion
Management of complex femoral fracture is challenging. Neither a suitable classification nor treatment options and implant designs are available [7]. Many combination of implants were used to solve different scenarios [8], [9], [10].
In this patient two fixation methods; bridge plating for relative stability of comminuted subtrochanteric fracture and a rigid fixation for absolute stability of segmental distal femoral diaphyseal fracture were used. Both methods had been reported as acceptable fixations [11], [12], [13]. Bridging callus was noticed at the proximal comminuted fracture site as early as 12 weeks. Evidence of union was established with a RUST score of 8 on 6 months post-operative radiograph as shown in Fig. 5. This can be related to the outcome of bridge plating of comminuted subtrochanteric fractures as reported [14], [15].
Obliteration of distal segmental fracture lines was noticed from the 6 months post-operative radiograph and complete obliteration at 9 months. Virk's et al. [16] described distal femoral locking plate as the implant of choice for distal femoral fracture.
In order to improve the stability and prevent a stress raiser, the two implants were overlapped and transfixed with locking screws. Harris et al. [17] describe overlapping femoral implants as being a more biomechanically stable construct. Similar to the reported finding [18], a favourable clinical outcome assessed by Parker and Palmer scores was noted.
Conclusion
Complex femoral fractures of this nature are rare high energy trauma. We reported a successful treatment of complex femoral fracture using minimally invasive plate osteosynthesis with dual plates. Our results demonstrate timely union and good clinical outcome.
References
- 1.Kulkarni S.L., Mannual S., Daragad M., Patil N., Ernest D. Management of complex femur fractures in children: a report of three cases. J. Orthop. Case Rep. 2021 Oct;11(10):33–37. doi: 10.13107/jocr.2021.v11.i10.2456. PMID: 35415096; PMCID: PMC8930314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Swiontkowski M.F. Ipsilateral femoral shaft and hip fractures. Orthop. Clin. North Am. 1987 Jan;18(1):73–84. PMID: 3796962. [PubMed] [Google Scholar]
- 3.Russell G.V., Jr., Kregor P.J., Jarrett C.A., Zlowodzki M. Complicated femoral shaft fractures. Orthop. Clin. North Am. 2002 Jan;33(1):127–142. doi: 10.1016/s0030-5898(03)00076-2. PMID: 11832317. [DOI] [PubMed] [Google Scholar]
- 4.Douša P., Bartoníček J., Pavelka T., Luňáček L. Ipsilaterální zlomeniny proximálního konce a diafýzy femuru [Ipsilateral fractures of the proximal femur and the femoral shaft] Acta Chir Orthop Traumatol Cech. 2010;77(5):378–388. Oct. Czech. PMID: 21040649. [PubMed] [Google Scholar]
- 5.Whelan D.B., Bhandari M., Stephen D., Kreder H., McKee M.D., Zdero R., Schemitsch E.H. Development of the radiographic union score for tibial fractures for the assessment of tibial fracture healing after intramedullary fixation. J. Trauma. 2010 Mar;68(3):629–632. doi: 10.1097/TA.0b013e3181a7c16d. PMID: 19996801. [DOI] [PubMed] [Google Scholar]
- 6.Parker M.J., Palmer C.R. A new mobility score for predicting mortality after hip fracture. J. Bone Joint Surg. Br. 1993 Sep;75(5):797–798. doi: 10.1302/0301-620X.75B5.8376443. PMID: 8376443. [DOI] [PubMed] [Google Scholar]
- 7.Juskovic A., Pesic G., Kezunovic M., Jeremic J., Bulatovic N., Dasic Z. Treatment of complex femoral fractures with the long intramedullary gamma nail. Serb. J. Exp. Clin. Res. 2019;20(4):337–341. doi: 10.2478/sjecr-2018-0038. [DOI] [Google Scholar]
- 8.von Rüden C., Tauber M., Woltmann A., Friederichs J., Hackl S., Bühren V., Hierholzer C. Surgical treatment of ipsilateral multi-level femoral fractures. J. Orthop. Surg. Res. 2015 Jan;24(10):7. doi: 10.1186/s13018-014-0149-5. PMID: 25616698; PMCID: PMC4335365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barei D.P., Schildhauer T.A., Nork S.E. Noncontiguous fractures of the femoral neck, femoral shaft, and distal femur. J. Trauma. 2003 Jul;55(1):80–86. doi: 10.1097/01.TA.0000046259.43886.25. PMID: 12855885. [DOI] [PubMed] [Google Scholar]
- 10.Griffin M., Dick A.G., Umarji S. Outcomes after trifocal femoral fractures. Case Rep. Surg. 2014; 2014 doi: 10.1155/2014/528061. Epub 2014 Apr 1. PMID: 24800097; PMCID: PMC3995313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oh C.W., Kim J.J., Byun Y.S., Oh J.K., Kim J.W., Kim S.Y., Park B.C., Lee H.J. Minimally invasive plate osteosynthesis of subtrochanteric femur fractures with a locking plate: a prospective series of 20 fractures. Arch. Orthop. Trauma Surg. 2009 Dec;129(12):1659–1665. doi: 10.1007/s00402-009-0815-y. Epub 2009 Jan 24 PMID: 19169695. [DOI] [PubMed] [Google Scholar]
- 12.Kregor P.J., Stannard J.A., Zlowodzki M., Cole P.A. Treatment of distal femur fractures using the less invasive stabilisation system: surgical experience and early clinical results in 103 fractures. J. Orthop. Trauma. 2004 Sep;18(8):509–520. doi: 10.1097/00005131-200409000-00006. PMID: 15475846. [DOI] [PubMed] [Google Scholar]
- 13.Andalib A., Sheikhbahaei E., Andalib Z., Tahririan M.A. Effectiveness of minimally invasive plate osteosynthesis (MIPO) on comminuted tibial or femoral fractures. Arch. Bone Jt. Surg. 2017 Sep;5(5):290–295. PMID: 29226199; PMCID: PMC5712394. [PMC free article] [PubMed] [Google Scholar]
- 14.Kayali C., Ağuş H., Zincircioğlu G. The role of biological fixation with bridge plating for comminuted subtrochanteric fractures of the femur. Ulus. Travma Acil Cerrahi Derg. 2008 Jan;14(1):53–58. PMID: 18306068. [PubMed] [Google Scholar]
- 15.Saini P., Kumar R., Shekhawat V., Joshi N., Bansal M., Kumar S. Biological fixation of comminuted subtrochanteric fractures with proximal femur locking compression plate. Injury. 2013 Feb;44(2):226–231. doi: 10.1016/j.injury.2012.10.037. Epub 2012 Nov 30 PMID: 23200761. [DOI] [PubMed] [Google Scholar]
- 16.Virk J.S., Garg S.K., Gupta P., Jangira V., Singh J., Rana S. Distal femur locking plate: the answer to all distal femoral fractures. J Clin Diagn Res. 2016;10(10):RC01–RC05. doi: 10.7860/JCDR/2016/22071.8759. Oct. Epub 2016 Oct 1. PMID: 27891409; PMCID: PMC5121747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harris T., Ruth J.T., Szivek J., Haywood B. The effect of implant overlap on the mechanical properties of the femur. J. Trauma. 2003 May;54(5):930–935. doi: 10.1097/01.TA.0000060999.54287.39. PMID: 12777906. [DOI] [PubMed] [Google Scholar]
- 18.Hu S.J., Zhang S.M., Yu G.R. Treatment of femoral subtrochanteric fractures with proximal lateral femur locking plates. Acta Ortop. Bras. 2012 Dec;20(6):329–333. doi: 10.1590/S1413-78522012000600003. PMID: 24453626; PMCID: PMC3861956. [DOI] [PMC free article] [PubMed] [Google Scholar]