Abstract
Workplaces are nodes for Severe Acute Respiratory Syndrome Coronavirus 2 transmission and require strategies to protect workers’ health. This article reports on the South African national coronavirus disease 2019 (COVID-19) strategy that sought to ensure workers’ health, protect the economic activity, safeguard livelihoods and support health services. Data from the Occupational Health Surveillance System, Surveillance System of Sentinel Hospital Sites, and government databases (public sector health worker and Compensation Fund data) was supplemented by peer-reviewed articles and grey literature. A multipronged, multi-stakeholder response to occupational health and safety (OHS) policy development, risk management, health surveillance, information, and training was adopted, underpinned by scientific input, through collaboration between government, organized labour, employer bodies, academia, and community partners. This resulted in government-promulgated legislation addressing OHS, sectoral guidelines, and work-related COVID-19 worker's compensation. The OHS Workstream of the National Department of Health provided leadership and technical support for COVID-specific workplace guidelines and practices, surveillance, information, and training, as well as a workplace-based vaccination strategy.
Keywords: COVID-19, workplaces, multistakeholder collaboration, framework response, risk mitigation
Introduction
As the coronavirus disease 2019 (COVID-19) pandemic unfolded, it became apparent that workplaces were important nodes for Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) transmission.1–4 It is estimated that about 20% of SARS-CoV-2 infections in adults are work-related.2 At the outset of the pandemic, specific categories of workers, such as health care, food and agriculture, public utilities and safety, manufacturing, transportation, and communications, were declared essential by governments and were legally required to continue working.5 Many sectors involved face-to-face contact (such as health care, police, social services, and frail care settings) and congregate settings, resulting in high-risk exposures for SARS-CoV-2 transmission. Studies showed that 10% of the workforce was employed in occupations that involved potential exposure at least once per week.6 Workers faced many intersecting factors such as precarious contracts, job insecurity, inadequate paid sick leave, limited bargaining power, and low socioeconomic status, which contributed to adverse consequences to their health and well-being during the pandemic.3,7,8
This understanding of the pandemic highlighted the need for effective South African national occupational health and safety (OHS) policies and COVID-19 responses to protect the workforce. This was to ensure minimal impacts on economic activities, safeguard livelihoods, and support healthcare delivery, amid the widespread economic upheaval associated with multiple lockdowns. The objective of this paper was to understand the impact of SARS-CoV-2 on South African workers and to provide an analysis of key stakeholder responses to mitigate adverse health and safety workplace risks.
Methodology
Secondary data was sourced from surveillance databases: the national Occupational Health Surveillance System (OHSS) hosted by the National Institute for Occupational Health (NIOH), the DATCOV Surveillance System of Sentinel Hospital sites hosted by the National Institute for Communicable Diseases (NICD), the National Department of Health (NDOH) public sector health worker data, and the national Compensation Fund within the Department of Employment and Labour (DEL). PubMed and Medline search on SARS-CoV-2 workplace responses from South Africa and internationally were conducted to identify other published data of relevance.
Work-Related COVID-19 in South Africa
Apart from studies among health workers (HWs) and reports among miners, there have been no studies on work-related COVID-19 in other groups of South African workers.9–14
HW Infections and Worker's Compensation Claims
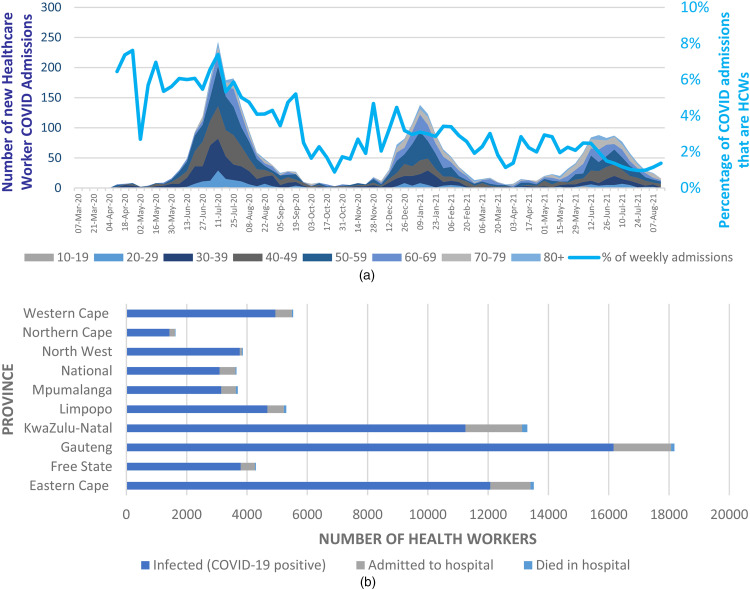
HWs remain at the highest risk of SARS-CoV-2 infections globally and in South Africa (Figure 1).15,16 World Health Organisation (WHO) estimates indicated that up to 14% of COVID-19 cases were attributable to HWs.17 The incidence of infection in HWs at a major tertiary hospital in Gauteng province, South Africa was reported to be 132.1 infections per 1000 person-months (95% confidence interval, 111.8-156.2).11 HW infection patterns and their peaks closely followed those in the general population in South Africa (Figure 1). During the first peak, HWs comprised almost 8 percent of all hospital admissions, declining to about 1% in the third peak. This decline may have been due to the workplace interventions implemented earlier in the pandemic and supplemented by the prioritization of HWs for vaccination (Figure 1a). As of October 8, 2021, 64 325 South African public sector HWs had contracted COVID-19 with 7928 (12.3%) hospitalized and 706 (1.1%) had died (Figure 1b).18 Provincial-level data provided insights into HW infections across public and private sector workers. In the public sector, an estimated 68 212 cases of COVID-19 were reported nationally, with the highest incidence in the industrialized provinces of Gauteng (n = 15 971), and KwaZulu-Natal (n = 10 629) by August 2021 (Table 1). Most infections (86%) were in the public sector. Approximately 1% to 2% of these HWs had died. Nurses were the most commonly affected job category comprising over half (53%) of all infected HWs. Other published data suggested that community health workers and administration staff may have been at greater risk as well.11 In the large Gauteng tertiary hospital study, increased odds of COVID-19 infection were found in women, older workers, nurses, those using public transport, and those with one co-morbidity or more.10 Similar findings were reported in hospitalized HWs employed across the public and private sectors.9
Figure 1.
(a) COVID-19 Admissions per age Category from March 7, 2020, to August 7, 2021 (Source: NICD DATCOV19 Hospital Surveillance System, August 15, 2021). (Key dates: First South African Case: March 5, 2020; Alert Level 5: March 27, 2020; Return of Mineworkers: April 30, 2020; Alert Level 4: April 30, 2020; Alert Level 3: June 1, 2020; Alert Level 2: August 18, 2020; Alert Level 1: September 21, 2020; Alert Level 3: December 29, 2020; Alert Level 1: March 1, 2021; Level 2: May 30, 2021; Level 3: June 15, 2021; Level 4: June 27, 2021; Level 3: July 25, 2021; Level 2: September 12, 2021). (b) COVID-19 Infections and Their Outcomes in Health Workers by Province from April 14, 2020, to October 8, 2021 (Data source: National Department of Health, COVID-19 Infected Public Healthcare Workers Dashboard, October 8, 2021).
Table 1.
Public Sector Health Worker COVID-19 Disease Data per Province (March 2020-Mid August 2021).
| Province | Public HW COVID-19 infected | HW ever admitted in reporting hospital | % of infected HW admitted to hospital (severity rate) | Total died in reporting hospital | % deaths of infected HW (mortality rate) |
|---|---|---|---|---|---|
| Eastern Cape | 11 440 | 1237 | 10.8 | 93 | 0.8 |
| Free State | 3526 | 434 | 12.3 | 29 | 0.8 |
| Gauteng | 15 971 | 1842 | 11.5 | 103 | 0.6 |
| KwaZulu- Natal | 10 629 | 1772 | 16.7 | 158 | 1.5 |
| Limpopo | 4549 | 514 | 11.3 | 78 | 1.7 |
| Mpumalanga | 3001 | 463 | 15.4 | 54 | 1.8 |
| North West | 3664 | 627 | 17.1 | 32 | 0.9 |
| Northern Cape | 1273 | 158 | 12.4 | 17 | 1.3 |
| Western Cape | 4604 | 499 | 10.8 | 37 | 0.8 |
| National | 2923 | 500 | 17.1 | 30 | 1.0 |
| Total | 68 212 | 8046 | 11.8 | 631 | 0.9 |
Source: National Department of Health.21
There were 20 525 HW claims for work-related COVID-19 infection submitted to the Compensation Fund for the period ending March 31, 2021 (Table 2).19 The majority of claims were from women workers, reflecting the demographics of the healthcare sector. Data from the Western Cape confirmed that HW infections were driving the compensation claims.20 Most claims (n = 6833) were from HWs (n = 5324; 77.9%), with 51% originating in the public health sector.
Table 2.
Worker Compensation Claims for Work-related COVID-19 Infections as of March 31, 2021.
| Province | Claims received | F | M | Cases in which liability accepted (%) | Fatal claims (%) |
|---|---|---|---|---|---|
| Eastern Cape | 2858 | 2065 | 793 | 1741 (60.9) | 19 (0.66) |
| Free State | 161 | 99 | 62 | 94 (58.4) | 2 (1.2) |
| Gauteng | 7177 | 3770 | 3412 | 2169 (30.2) | 6 (0.08) |
| KwaZulu-Natal | 2609 | 1856 | 754 | 992 (38.02) | 2 (0.08) |
| Limpopo | 27 | 7 | 20 | 2 (7.4) | 0 (0.00) |
| Mpumalanga | 501 | 372 | 129 | 288 (57.5) | 2 (0.4) |
| Northern Cape | 289 | 239 | 127 | 108 (37.4) | 3 (1.04) |
| North West | 176 | 32 | 67 | 50 (28.4) | 3 (1.7) |
| Western Cape | 6727 | 5045 | 1682 | 4983 (74.07) | 17 (0.3) |
| South Africa | 20 525 | 13 485 | 7046 | 10 427 (50.8) | 54 (0.3) |
Source: Compensation Fund (Department of Employment and Labour – DEL, Rand Mutual Assurance, and Federated Mutual), March 31, 2021.19
Mineworker Infections and Worker's Compensation Claims
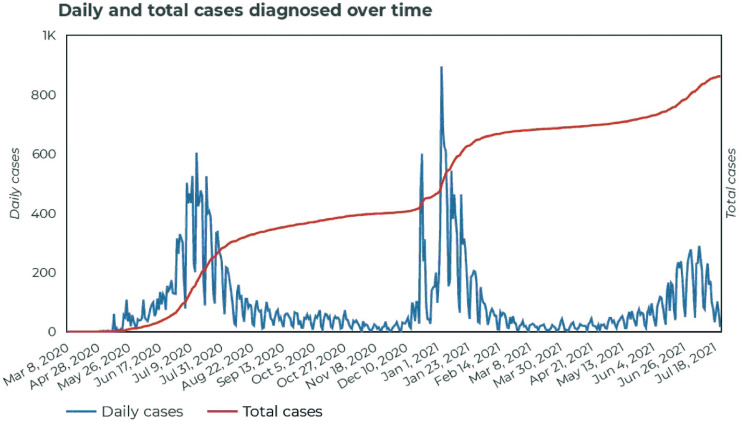
Mine workers were considered to be at increased risk for infection due to the migratory nature of employment as well as close underground contact characterized by inadequate ventilation and elevated dust exposures.12 A review of SARS-CoV-2 in SA mines suggested that specific socio-geographic and mining exposure factors combined with co-morbid respiratory conditions (silicosis, tuberculosis, chronic obstructive pulmonary disease) and HIV (human immunodeficiency virus) infection can increase the severity of SARS-CoV-2. The pattern of infections observed in the mines was similar to the rest of the country.22 Miner infections accounted for 2% of the total caseload and less than 1% of the total fatalities in SA (Figure 2). The mining sector fatality rate was estimated at 1.16%, which was lower than the 3.43% reported for the whole SA population.23 The reasons for this trend appear unclear since additional data to investigate this further was not available. It is probable that the sudden repatriation of a large number of migrant miners to their home countries in the early phase of the epidemic, and screening of at-risk workers prior to the return to the mines, may have played a role. In provinces with considerable mining activity, a high proportion of community cases and fatalities emanated from the mines.12 Mining-related cases were concentrated in areas situated close to provincial borders implying an increased interprovincial transmission risk, exacerbated by work-related transmission. Workers involved in high dust-generating jobs such as rock drill operators were reported to have the majority of infections.24
Figure 2.
Daily and total COVID-19 cases diagnosed in the South African mining industry for the period March 2020 to July 2021. Source: Minerals Council of South Africa, 2021.21
Mining contributed 23% (n = 4734) of compensation claims compared to the building industry 2.5% (n = 522) submitted to the Compensation Fund by March 31, 2021 (Table 2).19
Surveillance Data From Other Workplaces
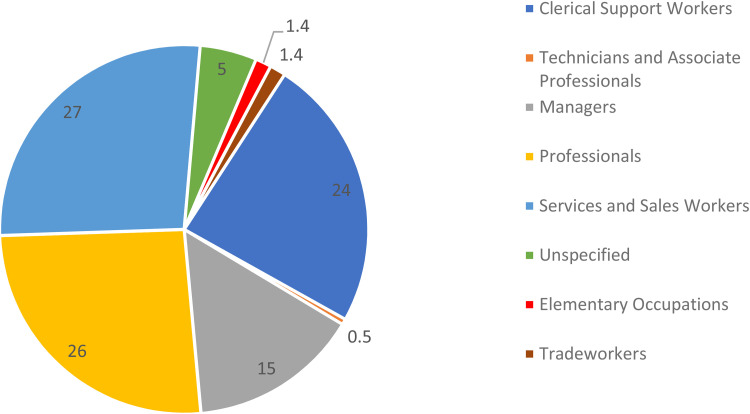
Reporting surveillance data from workplaces to the OHSS became mandatory in October 2020. From October 1, 2020, to October 31, 2021, there were 3657 positive COVID-19 cases reported (Supplemental Figure S1) with the majority from Gauteng (41.2 percent), followed by Western Cape (17 percent) and KwaZulu-Natal (Supplemental Figure S2).25 Most COVID-19-positive workers reported to the OHSS were employed as service workers (27%), professionals (26%), and clerical workers (24%). Among those with COVID-19 who reported an outcome (n = 364), there were 13% (n = 47) had died and 87% (n = 317) had been discharged following hospitalization. It needs to be emphasized that the OHSS is dependent on employers reporting the legally required information and does not necessarily represent the actual disease burden experienced by workers since a relatively small proportion of employers had been compliant with reporting. Furthermore, COVID-19 data from HWs were not reported to the OHSS, but to the NICD in the NDOH. Similarly, the mining industry developed its own reporting system overseen by the Minerals Council of South Africa. However, the OHSS does provide some insight into the patterns of distribution of the pandemic across the various job categories and industries (Figure 3).
Figure 3.
Distribution of COVID-19-positive employees by job category, for the period October 1, 2020, to October 31, 2021.
In summary, the data from South African workplaces, in keeping with studies reported internationally, highlighted the increased risk for infection in the health sector, while for other sectors the trends were less consistent.
National Stakeholder Responses and Interventions
The national government departments rapidly developed regulatory “Directions” to support the overarching regulation, under the Disaster Management Act of 1957.26 Since Alert Level 5 restricted work to HWs and essential workers, most Directions from other government departments addressed the epidemic's public health impacts. The NDOH as well as the National Department of Public Service and Administration, recognizing the impact on HWs, released internal instructions on the management of these workers (Table 3).27,28 The national OHS Workstream in the NDOH published the “Guidance for symptom monitoring and management of essential staff with COVID-19-related illness,” the first nationally available guideline that focused on the health of workers, followed by several additional COVID-19 workplace management worker guidelines.
Table 3.
COVID-19 Regulations, Directions, and Guidelines Relating to Workers and Workplaces in South Africa.
| Agency | Title | Date issued | Last amendment |
|---|---|---|---|
| Regulations | |||
| Co-operative Governance and Traditional Affairs | Regulations (GN R.398) of the Disaster Management Act, 1957 (Act 57 of 2002) (and subsequent amendments) | March 18, 2020 | September 12, 2021 |
| Directions and notices | |||
| Employment and Labor, Compensation Fund | Notice on Compensation for Occupationally-acquired Novel Corona Virus (COVID-19) under Compensation for Occupational Injuries and Diseases Act, 130 of 1993, later amended to Compensation for workplace-acquired Novel Corona Virus disease (COVID-19) | March 20, 2020 | July 23, 2020 |
| Transport | Directions: Measures to address, prevent and combat the spread of COVID-19 in the public transport services | March 25, 2020 | March 25, 2021 |
| Trade, Industry, and Competitions | Directions Regarding Call Centers Providing Essential Services | April 9, 2020 | – |
| Employment and Labor | COVID-19 Occupational Health and Safety Measures in Workplaces COVID-19 (C19 OHS), later amended to Consolidated Direction on Occupational Health and Safety Measures in Certain Workplaces | April 29, 2020 | June 11, 2021 |
| Small Business Development | Directions issued in terms of Regulation 4(9) of the Regulations made under section 27(2) of the Disaster Management Act, 2002 (Act No.57 of 2002): Measures to prevent and combat the spread of COVID-19 | May 12, 2020 | – |
| Basic Education | The re-opening of schools and measures to address, prevent and combat the spread of COVID-19 in the National Department of Basic Education, all provincial departments of education, all education district offices, and all schools in the Republic of South Africa | June 23, 2020 | April 22, 2021 |
| Employment and Labor | Direction extending COVID-19 TERS Benefits for specific categories of employee, September 7, 2020 | September 7, 2020 | April 8, 2021 |
| Guidelines | |||
| Public Service and Administration | Guidelines for the Containment/Management of the Coronavirus (COVID-19) in the public service. Circular 07 of 2020. | March 16, 2020 | – |
| Employment and Labor | Workplace Preparedness: COVID-19 (SARS-CoV-19 virus) | March 22, 2020 | – |
| Mineral Resources and Energy | Guiding principles on prevention and management of COVID-19 in the South African Mining Industry | March 26, 2020 | – |
| Health | Infection Control and Prevention Guidelines | April 8, 2020 | May 21, 2020 |
| Health | Guidance for symptom monitoring and management of essential staff/workers with COVID-19-related illness | April 14, 2020 | August 10, 2021 |
| Health | Psychosocial support for health workers during the COVID-19 response | May 2020 | – |
| Mineral Resources and Energy | Guidelines for a Mandatory Code of Practice on the Mitigation and Management of the COVID-19 outbreak | May 11, 2020 | – |
| Health | Guidance notes for workplaces in the event of identification of a COVID-19-positive employee | May 14, 2020 | – |
| Health | Guidance on vulnerable employees and workplace accommodation concerning COVID-19 | May 25, 2020 | – |
| Health | Disinfection tunnels and spray booths in the context of COVID-19 | June 4, 2020 | – |
| Health | Cleaning and Decontamination of Workplaces in the Context of COVID-19 | June 10, 2020 | August 10, 2021 |
| Health | Guideline on the submission of COVID-19-related health data from workplaces to the National Department of Health | August 19, 2020 | July 30, 2021 |
| Health | Guidance notice: Return to work of vulnerable employees | November 10, 2020 | – |
| Health | Guidelines for ventilation to prevent the spread of the SARS-CoV-2 virus | August 15, 2021 | – |
| Tools | |||
| Health | Worker COVID-19 Risk Assessment | April 17, 2020 | – |
| Health | COVID-19 Walk-through Risk Assessment | May 1, 2020 | – |
| Health | Specialized health risk assessment for workplaces (by employers and self-employed persons) | May 1, 2020 | – |
Note: This is not a comprehensive list, but it contains those that impact the working environment instead of broader public health aspects. The comprehensive listings are available at: https://www.gov.za/covid-19/resources/regulations-and-guidelines-coronavirus-covid-19 and https://www.nioh.ac.za/home/national-resources-directives-guidelines/
Alert levels legend for highlighted sections: Level 5: March 27, 2020; Level 4: April 30, 2020 (return of mineworkers); Level 3: June 1, 2020; Level 2: August 18, 2020; Level 1: September 21, 2020; Level 3: December 29, 2020; Level 1: March 1, 2021; Level 2: May 30, 2021; Level 3: June 15, 2021; Level 4: June 27, 2021; Level 3: July 25, 2021; Level 2: Sept 12, 2021. Version in color of this table can be seen online.
With the re-entry of workers in specific sectors into the working environment in Alert Level 4, policies for workers beyond the health sector became a national priority. Several government departments that had responsibility for workers within their sectors, produced relevant Directions, Codes of Practice, or Guidelines. These were prepared jointly with occupational health experts, from the OHS Workstream, or independently. Dissatisfied with the Department of Mineral Resources and Energy (DMRE) “Guiding Principles” document (Table 3), the Association of Mineworkers and Construction Union (AMCU), instituted a legal challenge. On May 11, 2020, following the Labor Court instruction and through a process of engaging occupational health experts, as well as representatives of workers and employers, the DMRE published a notice mandating mining employers to prepare Codes of Practice.29 The Department of Small Business and the Department of Trade, Industry, and Competition (DTIC) engaged with the OHS Workstream in preparing their Directions. Directions issued by the Departments of Transport, Education, and Tourism, focused on public health but indirectly benefitted workers (Table 3).
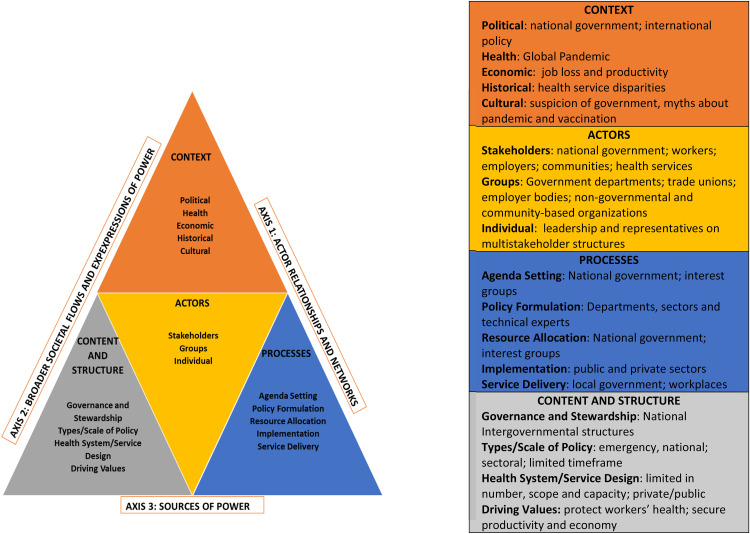
Further opening up of the economy required a concerted, multistakeholder approach to address the protection of workers (Figure 4). The National Economic Development and Labor Council (NEDLAC), a statutory national multistakeholder agency, became the vehicle to achieve this engagement.30 NEDLAC established an OHS Group in which the OHS Workstream technical experts participated, resulting in the DEL promulgating the COVID-19 Direction in April 2020, consolidating it further in September 2020. This Direction, applicable to all workplaces under the OHS Act (85 of 1993), with certain exceptions, provided the minimum basis for all other sectoral directions, and a more coherent inclusive response addressing workers and workplaces emerged.
Figure 4.
The power-policy triangle adapted for interventions in workers’ health during the COVID-19 pandemic (adapted from Topp et al 31).
Recognizing the work-relatedness of the transmission of SARS-CoV-2, the Compensation Fund, within the DEL, issued a notice for compensation for occupationally-acquired COVID-19 in March 2020, subsequently amending it to encompass a broader definition of “work-relatedness.”
By March 2021, the DEL had conducted 26 669 inspections, but only 57% of employers, across private, and public sectors, were compliant with the direction. This sub-optimal level of compliance contributed to further infection transmission in workplace contexts.32 Furthermore, a large proportion of the inspectorate did not have the necessary expertise in dealing with biological hazards,33 despite the DEL having generic hazardous biological agents legislation prior to the epidemic.34 This resulted in unnecessary workplace closures or another workplace punitive action.
The Interventions of the National OHS Workstream
Establishment of the National OHS Workstream
Even before the first case was reported in South Africa, it was clear that the protection of workers’ health and safety was a priority. Recognizing this, the centers of occupational health expertise in the public sector in the country, initially led the way in their provinces: the NIOH (Gauteng) and the Universities of Cape Town, KwaZulu-Natal, Pretoria, and Stellenbosch began engaging with the occupational health directorates within their respective provincial Departments of Health. The National Directorate of Occupational Health in the NDOH immediately established a national coordinating structure, the OHS Workstream as part of the Incident Management Team (IMT) of the NDOH.35 This structure brought together technical and academic expertise, employer and trade union representatives, and provincial government leadership in occupational health, to develop appropriate policy inputs, strategies, and interventions. The provincial coordinators provided weekly updates on developments in the health sector regarding the unfolding epidemic in the health sector (public and private sector), personal protective equipment (PPE) supply, education and training activities, psychosocial support activities, and the progress of vaccinations. The provincial coordinators also provided input into the policies and guidelines that were developed nationally by the experts and disseminated them through their respective provincial coordinating structures that were established to oversee their implementation. Members of the OHS Workstream engaged and provided inputs to the African Union and WHO/International Labour Organisation (ILO) meetings on OHS and the COVID-19 response.
Workplace Risk Assessments
Since workplaces were legally obligated to conduct COVID-19 risk assessments, risk assessment tools were designed by the OHS Workstream to assist workplaces. They were adapted for use by specific sectors and unique workplaces (Table 3). Stakeholders received focussed training in identifying risks and implementing control measures to prevent and curb the spread of COVID-19 in workplaces through the Occupational Health Outbreak Response Team of the NIOH and provincial structures. The guidelines of June 2020 (Table 3) addressed controversial issues around the closure of workplaces and “deep-cleaning” strategies advocated by non-expert private sector entrepreneurs.
The DEL Direction contributed towards improved compliance for specific workplaces such as the retail sector, where there was a greater risk for transmission in the community. These workplace risk assessments also highlighted the importance of psychosocial and ergonomic hazards. As evidence began emerging of the importance of ventilation to reduce bioaerosol transmission in workplaces, it was incorporated into the amended DEL Direction and a guidance note on ventilation was issued by the OHS Workstream (Table 3).
Personal Protective Equipment (PPE) Provision for HWs
Given the sparse information available on the effectiveness of PPE in the early days of the pandemic, a PPE Workstream was established as part of the IMT. A list of PPE derived from the WHO for different health worker categories and levels of health service was compiled. The PPE Workstream worked closely with the OHS Workstream and the Infection, Prevention, and Control teams to set quality standards for PPE and provide guideline documents. The PPE Workstream also worked with funding agencies and the private business sector, the National Treasury, and the quality assurance agencies such as the South African Health Products Regulatory Authority and the South African National Accreditation System to assist with testing samples given the reported deficiency of respiratory PPE sold by workplaces.36 The DTIC assisted with expediting local manufacturing of PPE given the initial shortage, high importation costs, and global scarcity. Initial attempts at centralizing PPE procurement and distribution failed to address provincial supply chain processes to source and distribute PPE. Trade union complaints of limited supply at the healthcare facility level led to an online tool being developed nationally by the NDOH and implemented at the facility level to report on stock levels of PPE.37
Health Screening, Testing, and Ongoing Monitoring of Workers at Workplaces and Occupational Health Services
In line with international best practice, the OHS Workstream provided guidelines on symptom monitoring and management of workers for SARS-CoV-2 (Table 3).38 The guidelines advocated for symptom screening, instead of temperature checks as temperature scanners had limited value.39,40 Ill-advised employers purchased temperature scanners in large numbers, but these, used by poorly trained officers, led to inaccurate assessments. As the pandemic progressed, studies in HWs and non-HWs showed that between 40% and –48% of workers were asymptomatic, posing further challenges to screening strategies.8,11 Several workplace digital software applications were also designed to assist workplaces with screening their workers before entering the workplace.41
The challenges to screening, testing, and monitoring workers were attributed to the entrenched inequitable access of many workers to occupational health services, estimated to be less than 20% for South African workplaces.42 This was particularly evident in small and medium enterprises, the informal and public sector workers. Most could not administer the tools and maintain health records due to their reliance on manual rather than digital electronic systems, inadequate infrastructure, equipment, and occupational health professional expertise.43
Management of Vulnerable Workers
Workers with underlying co-morbid health conditions and those older than 60 years of age, who were at high risk of developing severe illness and death due to SARS-CoV-2 infection, required additional protection.44 The OHS Workstream guideline outlined a process for identifying vulnerable employees, their medical evaluation and management, and workplace protection (Table 3). The DEL Direction reinforced the need to accommodate such employees, designated as high-risk. Employers had to mitigate health risks faced by these workers by providing low-risk work or alternative work arrangements. As lockdown measures eased, the NDOH outlined the management of return to work for vulnerable employees (Table 3), with consideration of individual worker vulnerability, workplace risk, and community transmission (based on district positivity rates).
A substantial reliance was placed on occupational health professionals to manage these programs. The integration of workplace exposure information and individual co-morbidities in workplace risk assessments was complex and required high clinical and occupational health expertise. This challenge was compounded by limited occupational health capacity in the public sector and negatively impacted workers in small and medium-scale enterprises, where occupational health services are nonexistent.42 Furthermore, the capacity to accommodate vulnerable workers was uneven since some jobs, especially in essential services, did not lend itself to remote working or alternative placement options for employers. However, the DEL Direction made provision for those who experienced a loss of income from their usual job to be remunerated through the Temporary Employer-Employee Relief Scheme (TERS). This scheme had its own administrative and upscaling challenges including long delays in payments to workers or failure of employers to remit to workers the payments they received for them. In addition, the amounts paid did not totally replace the lost income nor was the scheme sustained throughout the pandemic.45
Submission of COVID-19 Related Health Data by Workplaces
In response to poor work-related COVID-19 data and in the absence of a comprehensive worker health surveillance program, the OHSS was established, through a collaboration between the NDOH, NIOH, NICD, Council for Scientific and Industrial Research (CSIR), occupational medicine academic experts from the Universities of Cape Town and KwaZulu-Natal, and the private sector, in October 2020, The DEL Direction required all employers to submit COVID-19 related data to the NIOH as per the OHS Workstream guidelines.46
The OHSS intended to provide an overview of the COVID-19 infection spectrum in the South African workforce with timely identification of industries and occupational groups at high risk of infection to inform appropriate interventions. To date, information has been collected on symptomatic employees including symptoms, COVID-19 positivity, high-risk contacts, vulnerability assessments, and fitness on return to work. A total of 5363 businesses employing 2 025 675 employees, were registered in the one-year period. This represented under 3% of all registered businesses and approximately 14% of employees in South Africa.47
The absence of reliable denominator data to calculate infection rates per sector prevented optimal utilization of the data. The under-reporting of data despite its legal requirement has been a major challenge.
OHS Education and Training of Workers and Health Facility Audits
The OHS Workstream identified the need for education, training, and information advisory services (through a dedicated NIOH helpline) for workplaces. It was informed by a national online survey of South African HWs early into the epidemic, which showed that below half (47.4%) of 5530 respondents reported confidence about their overall knowledge about COVID-19.48 This was underscored by a national COVID-19 OHS facilities audit in the public health sector, which found lack of awareness of OHS regulations and responsibilities by facility managers as well as poor compliance relating to health and safety committees, health risk assessments, employee training and awareness.49 A study of HWs from multiple health facilities reported that only 55.6% of participants had received infection prevention and control training.50
A COVID-19 OHS syllabus covering topics from primary prevention (health risk assessment, infection prevention, and control), secondary prevention (epidemiology and management of disease, and medical surveillance), and tertiary prevention (return to work and rehabilitation) was developed and implemented by the NIOH using online platforms (https://www.nioh.ac.za/) facilitated by interdisciplinary academic and professional teams across South Africa.
Vaccine Strategy for Workers
In December 2020, the NDOH announced a vaccines rollout strategy, in which HWs were to be the recipients in Phase I, and among others, “essential workers” in Phase II.51 The OHS Workstream engaged with the relevant policymakers, the Vaccine Rollout Workstream of the Ministerial Advisory Committee, and NEDLAC representatives to determine the most appropriate implementation strategy for workers and workplace-based operational plans.
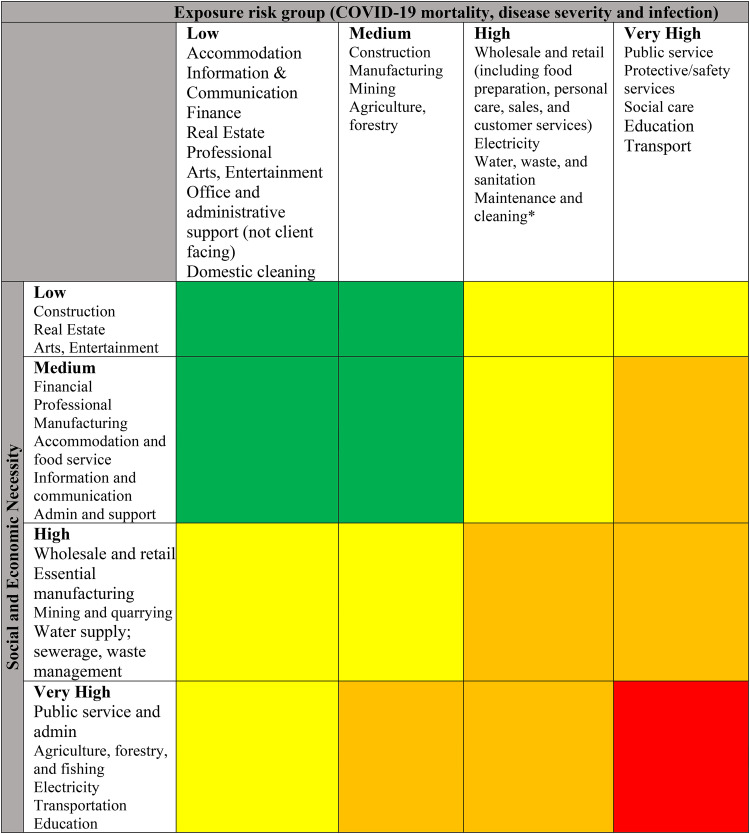
The OHS Workstream arrived at a consensus that workers, mainly blue-collar workers, using public transport for work, client-facing, and working in close proximity to fellow workers were at increased risk. However, constrained vaccine access would not allow for the vaccination of all workers simultaneously. A sequenced approach, with sectoral segmentation, became necessary, underpinned by 2 principles. First, the vaccine strategy focused on the reduction of risk for severe disease including death. Second, specific working sectors were at greater risk for these outcomes, based on the review of South African data, and international studies. Stratification by economic importance and social necessity were combined with available scientific data that resulted in a matrix (Figure 5), which proposed sectoral banding (Supplemental Figure S3) in a context of constrained vaccine access.
Figure 5.
COVID-19 matrix for exposure risk group versus social and economic necessity. Vaccination priority coding: Red: highest, orange: medium-high, yellow: medium-low, green: low. Note (*): Maintenance and cleaning—is a subcategory of administrative support, but needs to be elevated to a higher category than that of nonclient-facing administrative workers.
Once the phase II rollout extended to the 40-plus age groups, workplaces became an important entry point for vaccination of the economically active sector of the population. The OHS Workstream convened a multi-stakeholder group to coordinate the rollout in workplaces. Guidelines for the application, review and registration of vaccine sites in workplaces were also developed. To ensure that the frameworks developed by this working group had broader civil society acceptance, they were presented at the NEDLAC structures for discussion. These engagements led to a further revision of the DEL Direction to include vaccination-related aspects of COVID-19 (Table 3). While employer stakeholders strongly supported the concept of mandatory vaccination once vaccines were more readily accessible in the country, the response from trade unions was more constrained for various reasons including the lack of autonomy that this implied for individual workers. The interpretation by the Commission for Conciliation, Mediation, and Arbitration (CCMA), a legal body established to facilitate workplace disputes of any source, also varied but in the main appeared to support this approach, provided that there was sufficient consultation with employees.52 In general, there was a high uptake of vaccination among HWs, with the overall acceptance of vaccination reported in one study as being 90%.53 Uptake in the mining industry was also very high (75%) due to the pro-active approach and the well-resourced mining occupational health services. The latter is legally required by the Mine Health and Safety Act for surveillance of occupational diseases in this high-risk industry.54 No other industry data was available but the vaccination rates followed the trends in the general population, among whom 51.7% were vaccinated to date.55 The lack of easily accessible workplace-based occupational health services, the particularly onerous accreditation procedures of these services, and the low proportion of workers covered by medical insurance were barriers to the efficient operationalization of the vaccination campaigns. As vaccine supply became more freely available, vaccine hesitancy emerged as an important challenge, especially among workers across these other work sectors.56
Conclusions
While the SARS-CoV-2 pandemic in South Africa highlighted OHS challenges, the collaborative and coordinated response by the DEL and NDOH and social partners supported by OHS experts contributed towards slowing down infections in workplaces that were potential infection nodes. Based on international studies, specific sectors appear to be more prominent due to daily activities requiring proximity when working with others.3,6 They include protective services (eg, police officers, correctional officers, and firefighters), construction and maintenance workers (eg, plumbers, septic tank installers, and elevator repair); personal care and service workers, food production and serving workers, education, drivers and transport workers services and sales workers, cleaning and domestic workers.57–60 Apart from greater risks experienced by HWs globally, increased risk for severe COVID-19 outcomes have been reported in social care, education, transport, police and protective services, transport, and food workers.61 Furthermore, HWs, transportation, food preparation, and protective services have also been reported to have a higher risk for mortality.62
The Directorate of Occupational Health within the NDOH, the NIOH, the various specialist occupational medicine academic departments at universities throughout the country, provincial departments of health and other stakeholders as well as other non-governmental organizations and private sector organizations at the provincial and district levels, rapidly assembled to develop workplace strategies, including, policies and legislation, field instruments for assessing high-risk workers and workplaces, health information surveillance systems and training programs.
COVID-19 highlighted the importance of the occupational health response. Despite initiatives being successfully implemented by the OHS Workstream, the lack of workers’ health being centrally integrated into the broader public health response, was evident. For example, there was a narrow infection and prevention control approach adopted in the public health response. At a national level, there was no formal representation of occupational health in any of the official Ministerial Advisory Committee structures and this resulted in slow implementation and disparate efforts at the workplace level. Since competing agendas characterize occupational health by the different national stakeholders, this occasionally led to conflicting positions presented to the pandemic's national oversight structures. It also is unclear the extent to which the recommendations made by national stakeholders (OHS workstream and the NDOH) also resulted in differential implementation by provincial and district/primary levels of the health system and beyond.
The low level of occupational health services provision and expertise contributed to poor compliance, especially in small and medium-scale enterprises and the informal sector. The inadequate expertise was further compounded by the challenges faced by the enforcement inspectorate in dealing with biological hazards such as COVID-19 in workplaces.
The inadequate and relatively slow information dissemination from the national to provincial health departments and public sector health facilities in the early stages of the pandemic meant that HWs at the coalface were ill-equipped to implement adequate health and safety measures, thereby increasing their risk. The relatively low level of digital literacy or capacity in workplaces resulted in suboptimal use of technology necessitated by the nature of the epidemic for information, education and training, and routine health surveillance of workers.
The assessment and accommodation of vulnerable workers were vital to limit poor outcomes and mortality related to COVID-19 infection. This required a flexible approach and optimal occupational health expertise to integrate clinical knowledge to understand workplace exposure and job demands. The pandemic highlighted the importance of occupational health professionals in protecting and ensuring the workforce's health.
An integrated health surveillance system is crucial to have insights into workplace patterns of infection, morbidity, and mortality across economic sectors and occupational groups, and the factors contributing to these trends to develop interventions to reduce workplace transmission. This required concerted efforts from multiple stakeholders and government departments to provide and share this data, but this was not forthcoming even within the NDOH, which has resulted in a suboptimal OHS response nationally. This has been compounded by poor employer compliance to provide data for the OHSS designed for this purpose.
Recommendations for Occupational Health Policy
Despite the rapid responses by various stakeholders in OHS at a national and provincial level, the pandemic highlighted the need for a dedicated policy-developing agency in OHS. A structure independent of direct stakeholder influence, which approaches policy development based on the best available science, as evident in other jurisdictions, is necessary.63 Policies emerging from such an agency should be legally enforceable.
The NDOH and DEL in collaboration with employers and trade unions should establish a technical committee on developing an occupational health system for South Africa in the context of a low level of occupational health service provision in both the public and private sectors. Further impetus on the ratification of ILO's Convention 161 on Occupational Health Services is necessary.
Reporting occupational injuries and diseases to a national database is essential to provide job and sector-specific prevention interventions. Due to fragmented reporting and poorly analyzed data, a comprehensive picture of the prevalence and nature of occupational injuries and diseases has been absent for over a decade, especially in industries other than mining. A new approach to reporting, such as the OHSS, is proposed. The OHSS could be adapted to serve as a dynamic monitor for all occupational diseases and injuries in the country in the long term. Such systems have been successfully implemented internationally.64
There is an urgent need to link infectious diseases notifiable data routinely submitted to government departments such as NICD positive case data, hospital admissions data, and compensation data. They need to be easily accessible by stakeholders to inform decisions made as epidemics unfold in the workplace.
A strategy for improved access to occupational health expertise is needed to assist employers in small and medium-scale enterprises to manage OHS risks in general and specifically to pandemics and other outbreaks. The DEL should drive this in consultation with the NDOH. Due consideration should also be given to establishing a medical inspectorate.
Rapid epidemiological approaches are required for work-related outbreaks such as COVID-19 or other acute infectious outcomes as has been observed with Ebola infection in other parts of Africa. The DEL was directed by stakeholders through NEDLAC discussions to incorporate the approach contained in its Consolidated Directive on COVID-19 into the Hazardous Biological Agents Regulations and to ensure compensation for work-related COVID-19 remains in force to deal with other epidemic surges. This was necessary as the Directives ceased to have legal force once the DMA Regulations were lifted as the pandemic in the country subsided. In addition, the specific details of managing COVID-19 transmission in workplaces, previously contained in the DEL Direction were codified into a Code of Practice: Managing exposure to SARS-CoV-2 in the workplace.65 The mainstreaming of these important policy interventions in the workplace provided workers with ongoing protection, as well as clear guidelines for employers to ensure safe and productive workplaces.
Supplemental Material
Supplemental material, sj-docx-1-new-10.1177_10482911221150237 for Strengthening Social Compact and Innovative Health Sector Collaborations in Addressing COVID-19 in South African Workplaces by Mohamed F. Jeebhay, Rajen N. Naidoo, Saloshni Naidoo, Shahieda Adams, Muzimkhulu Zungu, Spo Kgalomono, Nisha Naicker and Barry Kistnasamy in NEW SOLUTIONS: A Journal of Environmental and Occupational Health Policy
Acknowledgments
We would like to thank the OHSS team for the provision of OHSS data (Dr J. Mtsweni—CSIR; Mr M. Rambau—NIOH), the NICD for the DATCOV surveillance data (Dr Natalie Mayet and the epidemiology team), the National Department of Health for the COVID-19 public sector HW data on PERSAL (Dr Nicholas Crisp and Dr Sipho Senabe) and the Compensation Fund in the DEL (Dr Lulama Magubane and Dr Iqram Bux).
Author Biographies
Mohamed F. Jeebhay is an occupational medicine specialist (physician) and obtained his PhD at the University of Michigan in 2003. He is a full professor and the Head of the Occupational Medicine Division, School of Public Health, University of Cape Town. He is globally recognized for his work in occupational allergies and asthma. He was a member of the Occupational Health and Safety Workstream that was formed by the national Department of Health in response to the COVID-19 pandemic and was responsible for the drafting of several of the Guidelines directed at protecting workers. He was a member of the multiparty structures established by the government in developing legislation during the pandemic.
Rajen N. Naidoo is an occupational medicine specialist (physician) and obtained his PhD at the University of Michigan in 2002. He is a full professor and the Head of the Discipline of Occupational and Environmental Health at the University of Kwa-Zulu Natal. His area of research is occupational and environmental respiratory diseases. He was a member of the Occupational Health and Safety Workstream that was formed by the national Department of Health in response to the COVID-19 pandemic and was responsible for the drafting of several of the Guidelines directed at protecting workers. He was a member of the multiparty structures established by the government in developing legislation during the pandemic.
Saloshni Naidoo, is a public health medicine and occupational medicine specialist (physician), having graduated with her PhD from the University of Utrecht, Netherlands in 2012. She is an Associate Professor and the Head of the Discipline of Public Health Medicine at the School of Nursing and Public Health at the University of Kwa-Zulu Natal. Her areas of research interest are agricultural exposures and neurocognitive health outcomes. During the COVID-19 pandemic, she was a member of the provincial “War Room,” which was tasked by the Provincial Premier to manage all aspects of the pandemic in the province, including policy interventions, stakeholder engagements, and health systems management.
Shahieda Adams, is an occupational medicine specialist (physician) and completed her doctoral training at the University of Cape Town (UCT). She is Associate Professor in the Occupational Medicine Division, School of Public Health, University of Cape Town. She has a dual appointment at the latter institution as well as at the Western Cape Department of Health. Her areas of research focus are occupational tuberculosis. She was instrumental in assisting the Department of Health in establishing its guidelines and protocols during the COVID-19 pandemic.
Muzimkhulu Zungu, is a public health medicine specialist (physician) and doctoral candidate. He is a Centre Head at the National Institute for Occupational Health, National Health Laboratory Service, and an Adjunct Professor at the School of Health Systems and Public Health, Faculty of Health Sciences University of Pretoria. He was the Chair of the Technical Committee on COVID-19 within the Occupational Health and Safety Workstream under the National Department of Health. He is currently leading the program on national worker education for COVID-19 at the National Institute.
Spo Kgalomono is an occupational medicine specialist (physician) and a doctoral candidate at the University of Witwatersrand. She is the Executive Director of the National Institute for Occupational Health, National Health Laboratory Service. She was responsible for ensuring the National Institute played a leadership role in protecting the health of workers during the pandemic, through the development of education programs, surveillance systems, policy interventions, and workplace toolkits within the National Institute.
Nisha Naicker, is a specialist in Public Health Medicine (physician), and receiving her doctorate from the University of Witwatersrand in 2012. She currently heads the Epidemiology and Surveillance with the National Institute for Occupational Health in National Health Laboratory Service. She has an appointment as associate professor at the Department of Environmental Health, University of Johannesburg. She played an important role in developing the Occupational Health Surveillance System for workers, including during the COVID-19 pandemic.
Barry Kistnasamy is an occupational medicine specialist (physician). He is currently the Chief Director of the Directorate of Occupational Health in the National Department of Health, and the Compensation Commission of Occupational Diseases, responsible for the Medical Bureau for Occupational Diseases within the National Department of Health. His area of the current focus is on the health of miners in Southern Africa and developing effective systems of compensation for current and former miners that work or have worked in South African mines. During the COVID-19 pandemic, he headed the Occupational Health and Safety Workstream within the National Department of Health and provided inputs to the Inter-Ministerial Teams and the Ministerial Advisory Council which was responsible for the legislative and policy frameworks, resource allocations, vaccination programs, and service provision during the pandemic.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Supplemental Material: Supplemental material for this article is available online.
ORCID iD: Rajen N. Naidoo https://orcid.org/0000-0002-2318-4004
References
- 1.Burdorf A, Porru F. The COVID-19 pandemic: one year later – an occupational perspective. Scand J Work Environ Health 2021; 47(4): 245–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marinaccio A, Boccuni F, Rondinone BM, et al. Occupational factors in the COVID-19 pandemic in Italy: compensation claims applications support establishing an occupational surveillance system. Occup Environ Med 2020; 77(12): 818–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Purkayastha D, Vanroelen C, Bircan T, et al. Work, health and COVID-19: a literature review. Report 2021.03, European Trade Union Institute, Brussels, 2021. [Google Scholar]
- 4.Koh D. Occupational risks for COVID-19 infection. Occup Med (Lond) 2020; 70(1): 3–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gaitens J, Condon M, Fernandes E, et al. COVID-19 and essential workers: a narrative review of health outcomes and moral injury. Int J Environ Res Public Health 2021; 18(4): 1446. doi: 10.3390/ijerph18041446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baker MG, Peckham TK, Seixas NS. Estimating the burden of United States workers exposed to infection or disease: a key factor in containing risk of COVID-19 infection. PLoS One 2020; 15(4): e0232452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goldman N, Pebley AR, Lee K, et al. Racial and ethnic differentials in COVID-19-related job exposures by occupational standing in the US. PLoS One 2021; 16(9): e0256085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shaw JA, Meiring M, Cummins T, et al. Higher SARS-CoV-2 seroprevalence in workers with lower socioeconomic status in Cape Town, South Africa. PLoS One 2021; 16(2): e0247852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rees K, Dunlop JL, Patel-Abrahams S, et al. Primary healthcare workers at risk during COVID-19: an analysis of infections in HIV service providers in five districts of South Africa. S Afr Med J 2021; 111(4): 309–314. [DOI] [PubMed] [Google Scholar]
- 10.Tlotleng N, Jassat W, Cohen C. et al. National COVID-19 hospital admissions and mortality among healthcare workers in South Africa, 2020–2021. Res Sq, 10.21203/rs.3.rs-637985/v1 (2021, accessed 17 March 2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nunes MC, Baillie VL, Kwatra G, et al. Severe acute respiratory syndrome coronavirus 2 infection among healthcare workers in South Africa: a longitudinal cohort study. Clin Infect Dis 2021; ciab398. doi: 10.1093/cid/ciab398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Naidoo R, Jeebhay MF. COVID-19 – a new burden of respiratory disease among South African miners? Curr Opin Pulm Med 2021; 26: 000–000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mdzinwa N, Voigt M, van Rensburg C Jet al. et al. SARS-CoV-2 infection prevalence in healthcare workers and administrative and support staff: The first-wave experience at three academic hospitals in the Tshwane district of Gauteng province, South Africa. S Afr Med J 2021; 111: 1092–1097. [DOI] [PubMed] [Google Scholar]
- 14.Ntatamala I, Naidoo RN, Ncayiyana JNet al. et al. COVID-19: Work, Economic Activity and the Spatiotemporal Distribution of Infection in South Africa. In: Akhtar R. (eds) Coronavirus (COVID-19) Outbreaks, Vaccination, Politics and Society. Cham: Springer, 2022. [Google Scholar]
- 15.Dramowski A, Zunza M, Dube K. South African healthcare workers and COVID-19: a shared responsibility to protect a precious and limited resource. S Afr Med J 2020; 10. [DOI] [PubMed] [Google Scholar]
- 16.Chersich MF, Gray G, Fairlie L, et al. COVID-19 in Africa – care and protection for frontline healthcare workers. Global Health 2020; 16: 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organization. Prevention, identification and management of health worker infection in the context of COVID-19. Interim guidance, https://www.who.int/publications-detail-redirect/10665-336265. (2020, accessed 10 December 2022).
- 18.Department of Health. COVID-19 public healthcare workers dashboard, https://www.nioh.ac.za/wp-content/uploads/2021/03/COVID-19-vaccine-for-Workers-Occupational-Health-Perspective-Dr-Senabe.pdf. (2021, accessed 10 December 2022).
- 19.Compensation Fund. Presentation to NEDLAC OHS Subcommittee Meeting. (Presentation). Department of Employment and Labour, Rand Mutual Assurance and Federated Mutual. (31 March 2021).
- 20.Bux I (Office of the Compensation Fund, Western Cape). Personal Communication to: MFJ. 5 June 2021.
- 21.Crisp N (National Department of Health). Personal Communication to: MFJ. 10 October 2021.
- 22.Minerals Council of South Africa. COVID-19 Provincial comparison and scenario planning COVID-19 Industry Working Group, https://www.mineralscouncil.org.za/downloads/send/7-2015/1377-covid-19-provincial-comparison. (2021, accessed 10 December 2022).
- 23.Minerals Council South Africa. Minerals Council Position on COVID-19, https://www.mineralscouncil.org.za/downloads/send/14-current/1573-integrated-annual-review-2020-industry-response-to-covid-19 (2020, accessed 10 December 2022).
- 24.Muchiri E, Charalambous S. Minerals Council COVID-19 response and surveillance progress report. Report, Minerals Council, South Africa, July 2020.
- 25.National Institute for Occupational Health. Occupational Health Surveillance System Report March 2021, https://www.nioh.ac.za/wp-content/uploads/2021/06/NIOH-Occupational-Health-Surveillance-System-Report-Volume-1.pdf. (2021, accessed 10 December 2022).
- 26.Department of Co-operative Governance and Traditional Affairs. Regulations (GN R.398) of the Disaster Management Act 1957 (Act 57 of 2002). Pretoria. 18 March 2020.
- 27.Department of Public Service and Administration. State of Disaster: Guidelines for the Containment/Management of the Coronavirus (COVID-19) in the public service. Pretoria. 16 March 2020.
- 28.National Department of Health. COVID-19 Disease: Infection Control and Prevention Guidelines version 1. Pretoria, https://www.nicd.ac.za/wp-content/uploads/2020/04/Covid-19-Infection-and-Prevention-Control-Guidelines-1-April-2020.pdf (2020, accessed 10 December 2022).
- 29.Southern African Legal Information Institute. Judgement in the case of Association of Mineworkers and Construction Union v Minister of Mineral Resources and Energy and Others, http://www.saflii.org/za/cases/ZALCJHB/2020/68.html (2020, accessed 10 December 2022).
- 30.National Economic Development and Labour Council. Act 35 of 1995. National Economic Development and Labour Council Act, https://nedlac.org.za/wp-content/uploads/2020/11/NEDLAC-ACTS.pdf (1994, accessed 10 December 2022).
- 31.Topp SM, Schaaf M, Sriram V, et al. Power analysis in health policy and systems research: A guide to research conceptualisation. BMJ Global Health 2021; 6: e007268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Department of Employment and Labour. Lack of workplace behaviour change is driving covid-19 infections at work. Media Statement, https://www.labour.gov.za/lack-of-workplace-behaviour-change-is-driving-covid-19-infections-at-work (2021, accessed 10 December 2022).
- 33.Sizana T (Department of Employment and Labour). Personal Communication To: RNN. 16 September 2021.
- 34.Department of Labour. Regulations for Hazardous Biological Agents, https://www.gov.za/documents/occupational-health-and-safety-act-regulations-hazardous-biological-agents (2001, accessed 10 December 2022).
- 35.Moonasar D, Pillay A, Leonard E, et al. COVID-19 lessons and experiences from South Africa’s first surge. BMJ Global Health 2021: 6e004393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mottay L, le Roux J, Perumal R, et al. KN95 filtering facepiece respirators distributed in South Africa fail safety testing protocols. S Afr Med J. Epub ahead of print 9 December 2020. DOI: 10.7196/SAMJ. 2021.v111i3.15381. [DOI] [PubMed] [Google Scholar]
- 37.National Department of Health. Strategy to protect the health and safety of health workers in the face of the COVID-19 pandemic, https://www.knowledgehub.org.za/elibrary/strategy-protect-health-and-safety-health-workers-face-covid-19-pandemic (2020, accessed 10 December 2022).
- 38.National Institute for Communicable Diseases. Guidelines for case-finding, diagnosis, and public health response in South Africa, https://www.nicd.ac.za/diseases-a-z-index/disease-index-covid-19/covid-19-guidelines/ (2020, accessed10 December 2022).
- 39.Buckley RG, Conine M. Reliability of subjective fever in triage of adult patients. Ann Emerg Med 1996; 27: 693–695. [DOI] [PubMed] [Google Scholar]
- 40.Quilty BJ, Clifford S, Flasche S, et al. Effectiveness of airport screening at detecting travellers infected with novel coronavirus (2019-nCoV). Euro Surveill 2020; 25: pii=2000080. doi: 10.2807/1560-7917.ES.2020.25.5.2000080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Friedman A. Introducing a free COVID-19 workplace screening tool, https://blog.mobenzi.com/2020/05/12/introducing-a-free-covid-19-workplace-screening-tool/ (2020, accessed 10 December 2022).
- 42.Jeebhay M, Jacobs B. Occupational health services in South Africa. In: Crisp N, Ntuli A. (eds) South African Health Review. 5th ed. Durban, South Africa: Health Systems Trust, 1999; pp.19:257-276. [Google Scholar]
- 43.Leyden S (NEDLAC OHS subcommittee). Personal Communication to: MFJ. 12 June 2021.
- 44.Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 2020; 584: 430–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Parliamentary Monitoring Group. UIF on challenges experienced with the financial administration of TERS in WC. COVID-19 TERS public participation process, https://pmg.org.za/committee-meeting/32878/ (2021, accessed 9 December 2022).
- 46.National Institute for Occupational Health. Occupational Health Surveillance System (OHSS) Business Portal, https://www.nioh.ac.za/covid-19/occupational-health-surveillance-system-ohss-business-portal/ (2020, accessed 10 December 2022).
- 47.National Institute for Occupational Health. Occupational Health Surveillance System, https://www.nioh.ac.za/wp-content/uploads/2021/10/OHSS-CHARTER-DOCUMENT-version-10-Sept-2021.pdf (2021, accessed 10 December 2022).
- 48.Manyaapelo T, Mokhele T, Sifunda S, et al. Determinants of confidence in overall knowledge about COVID-19 among healthcare workers in South Africa: Results from an online survey. Front Public Health 2021; 9: 614858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.National Institute for Occupational Health. The national verification (audit) of occupational health services and health and safety committees in public and private health facilities in South Africa. Report, NIOH: Johannesburg, South Africa, 2021.
- 50.Moodley SV, Zungu M, Malotle M, et al. A health worker knowledge, attitudes and practices survey of SARS-CoV-2 infection prevention and control in South Africa. BMC Infect Dis 2021; 21: 138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.National Department of Health. Vaccine rollout strategy. Pretoria, https://sacoronavirus.co.za/2021/01/03/south-africas-vaccine-rollout-strategy/ (2021, accessed 10 December 2022).
- 52.Commission for Conciliation, Mediation and Arbitration. Mandatory COVID-19 vaccination policy in the workplace, https://www.ccma.org.za/wp-content/uploads/2022/06/Mandatory-Covid-19-Vaccination-Policy-in-the-Workplace-2022-01.pdf (2022, accessed 10 December 2022).
- 53.Adeniyi OV, Stead D, Singata-Madliki M, et al. Acceptance of COVID-19 vaccine among the healthcare workers in the eastern cape, South Africa: A cross-sectional study. Vaccines (Basel) 2021; 9: 666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Minerals Council South Africa. COVID-19 and the Mining Industry – COVID-19 Dashboard, https://www.mineralscouncil.org.za/minerals-council-position-on-covid-19#dashboard. (2022, accessed 9 December 2022).
- 55.Department of Health. COVID-19 Vaccination Summary, https://sacoronavirus.co.za/latest-vaccine-statistics/ (2022, accessed 9 December 2022).
- 56.Cooper S, van Rooyen H, Wiysonge CS. COVID-19 vaccine hesitancy in South Africa: How can we maximize uptake of COVID-19 vaccines? Expert Rev Vaccines 2021; 20: 921–933. [DOI] [PubMed] [Google Scholar]
- 57.Carlsten C, Gulati M, Hines S, et al. COVID-19 as an occupational disease. Am J Ind Med 2021; 64: 227–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhang M. Estimation of differential occupational risk of COVID-19 by comparing risk factors with case data by occupational group. Am J Ind Med 2021; 64: 39–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cox-Ganser JM, Henneberger PK. Occupations by proximity and indoor-outdoor work - relevance to COVID-19 in all workers and Black-Hispanic workers. Am J Prev Med 2021; 60: 621–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lan F-Y, Wei CF, Hsu Y-T, et al. Work-related COVID-19 transmission in six Asian countries and areas - A follow-up study. PLOS One 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mutambudzi M, Niedwiedz C, Macdonald EB, et al. Occupation and risk of severe COVID-19: Prospective cohort study of 120 075 UK Biobank participants. Occup Environ Med 2020; 0: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hawkins D, Davis L, Kriebel D. COVID-19 deaths by occupation, Massachusetts, March 1-July 31, 2020. Am J Ind Med 2021; 64: 238–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.The Health and Safety Executive. The HSE Story: United Kingdom, https://www.hse.gov.uk/aboutus/hse-story.htm (2021, accessed 17 March 2022).
- 64.US National Institute for Occupational Safety and Health. Worker Health Surveillance, https://www.cdc.gov/niosh/topics/surveillance/default.html (2021, accessed 17 March 2022).
- 65.Department of Employment and Labour. Code of Practice: Managing exposure to SARS-CoV-2 in the workplace, https://www.gov.za/sites/default/files/gcis_document/202203/46043rg11405gon1876.pdf (2022, accessed 9 December 2022).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-new-10.1177_10482911221150237 for Strengthening Social Compact and Innovative Health Sector Collaborations in Addressing COVID-19 in South African Workplaces by Mohamed F. Jeebhay, Rajen N. Naidoo, Saloshni Naidoo, Shahieda Adams, Muzimkhulu Zungu, Spo Kgalomono, Nisha Naicker and Barry Kistnasamy in NEW SOLUTIONS: A Journal of Environmental and Occupational Health Policy