SUMMARY
Objective
To investigate whether patients with conductive hearing loss (CHL) and normal preoperative investigations may benefit from exploratory tympanotomy (ET) and tailored treatment performed according to intraoperative findings.
Methods
Patients treated with ET for CHL with normal pre-operative otoscopy, tympanometry and CT scan from 2011 to 2019 were reviewed. Data regarding demographics, audiometry, intraoperative findings and surgery were collected and analysed to assess if they can predict post-operative air bone gap (ABG) closure and patient satisfaction.
Results
Forty-eight cases were included. Mean ABG significantly reduced (p < 0.001) from preoperative (38.4 dB) to postoperative (14.8 dB). Post-operative ABG closure within 10 dB was observed in 20 cases (41.7%). Overall satisfaction was reported in 60% of cases. Stapes fixation was the most common diagnosis (47.9%) and significantly associated with lower post-operative ABG and higher satisfaction.
Conclusions
In CHL with normal pre-operative investigations, ET represents the mainstay of treatment, even if audiological outcomes may widely vary. Intraoperative finding of stapes fixation (thus stapedotomy) ensures the best audiological and satisfaction outcomes.
KEY WORDS: hearing loss, conductive, exploratory tympanotomy, otosclerosis, stapes surgery, ossicular replacement
RIASSUNTO
Obiettivo
Studio dell’outcome audiologico nei pazienti con ipoacusia trasmissiva (CHL) e indagini preoperatorie normali trattati con timpanotomia esplorativa (ET).
Metodi
È stata condotta una revisione dei casi di CHL con normale otoscopia, timpanometria e TC pre-operatorie trattati con ET dal 2011 al 2019. I dati demografici, audiometrici e relativi alla diagnosi intra-operatoria sono stati raccolti e analizzati per valutarne il valore predittivo in termini di riduzione post-operatoria dell’air bone gap (ABG) e di soddisfazione dei pazienti.
Risultati
Sono stati inclusi 48 casi. L’ABG medio si è ridotto significativamente (p < 0,001) dal pre-operatorio (38,4 dB) al post-operatorio (14,8 dB). Un ABG post-operatorio entro i 10 dB è stato osservato in 20 casi (41,7%). La soddisfazione generale è stata riportata nel 60% dei casi. La fissità stapediale è stata la diagnosi più frequente (47,9%) e significativamente associata a un ABG post-operatorio più basso e a una migliore qualità di vita percepita.
Conclusioni
Nella CHL con indagini pre-operatorie normali, l’ET rappresenta il trattamento di prima scelta, sebbene i risultati audiometrici possano variare. Il riscontro intra-operatorio di fissità stapediale si associa a migliori risultati audiologici e di soddisfazione del paziente.
PAROLE CHIAVE: ipoacusia trasmissiva, timpanotomia esplorativa, otosclerosi, chirurgia della staffa, ossiculoplastica
Introduction
Conductive hearing loss (CHL) is a frequently encountered condition in the practice of otolaryngologists and can result from a variety of pathologic conditions 1-3. An accurate diagnosis is essential to offer patients the best treatment option. Patients affected by CHL presenting with normal tympanic membrane, tympanometry and temporal bone computed tomography (CT) represent a clinical challenge. Exploratory tympanotomy (ET) is a diagnostic option that allows surgeons to assess the middle ear (ME), eventually tailoring treatment according to intraoperative findings.
The aim of this study is to investigate whether patients presenting with CHL, normal ME pressure and negative/non-diagnostic pre-operative CT scan may benefit from a surgical intervention of exploratory tympanotomy, quantifying the air bone gap (ABG) reduction that tailored surgery according to intraoperative findings may offer. Moreover, patient and treatment-related factors, as well as pre-operative audiologic data, were studied to assess their potential predictive role on restoration of air-conduction. We also collected data on the benefit perceived by patients following surgery, investigating variables that may influence patient satisfaction.
Materials and methods
A retrospective analysis of consecutive patients undergoing ET under local anaesthesia for CHL between September 2011 and November 2019 was conducted at the Department of Otolaryngology of the University of Brescia, Italy. All patients presenting with CHL and normal tympanic membrane underwent high-resolution temporal bone CT scan to confirm eligibility for surgical procedures of hearing restoration, and for better definition of ME anatomy and potential surgical risks. Advantages and disadvantages of any possible interventions were thoroughly discussed with patients.
Inclusion criteria were: a) patients undergoing elective ET; b) with a preoperative air-bone gap (ABG) ≥ 20 dB at least in 2 frequencies (500-3000 Hz) 4 determined with a pure-tonal audiometry (PTA); c) normal pre-operative microscopy and oto-endoscopy; d) normal tympanometry (i.e. pattern A); e) normal/non-diagnostic pre-operative ear CT scan. Exclusion criteria were: a) age < 18-years; b) previous surgery in the affected ear; c) reporting symptoms consistent with third window disorders.
Surgical strategies were tailored according to intraoperative findings to restore hearing.
Data regarding demographics, radiological, pre-and post-operative PTA, intraoperative findings and surgical details were anonymously collected in a dedicated database. PTA findings were analysed according to the “Committee on Hearing and Equilibrium guidelines for the evaluation of the results of treatment of conductive hearing loss” 5. ABG was defined as the mean value of the differences between the air- and bone-conductions at 500, 1000, 2000 and 3000 Hz. ABG reduction was defined as the difference between pre-operative and post-operative ABGs. Patient-referred outcomes after surgery were measured by administration of the 18-question “Glasgow Benefit Inventory (GBI)” questionnaire at the latest follow-up evaluation 6. Patients were also asked if they were satisfied by the surgical procedure overall, and if they would recommend the procedure.
Statistical analysis
Characteristics of patients were expressed in terms of percentages, mean and relative standard deviation, median, inter-quartile range (IQR) and range.
Continuous variables were tested for normal distribution with Shapiro-Wilk test. Parametric tests (ANOVA) and non-parametric tests (Mann-Whitney, Kruskall-Wallis, Wilcoxon signed-rank tests) were used as appropriate. Spearman’s and Pearson’s rho were calculated to study correlation between continuous variables. Relationship between discrete variables was conducted with Fisher exact and Chi-squared tests, as appropriate.
ROC curve analysis was used to determine the ideal cut-off according to Youden’s index in age at presentation, pre- and post-operative ABG and ABG reduction according to overall satisfaction. AUC values > 0.70 were considered satisfactory.
Statistical analysis was performed using R (version 4.0.5, R Foundation for Statistical Computing, Vienna, Austria); p-values < 0.05 were considered statistically significant.
Results
During the period of investigation, 515 ears were scheduled for surgical treatment of CHL with normal pre-operatory tympanic membrane and ear pressure. In 467 patients, the preoperatory CT scan was diagnostic for otosclerosis and stapedotomy was performed.
The remaining 48 cases (9.3%) with a non-diagnostic pre-operatory CT scan were scheduled for exploratory tympanotomy and included in the current study. Cone beam CT (CBCT) was performed in 28 patients (58.3%). Of these patients, most were female (54.2%), with a mean age at surgery of 51.7 ± 14.0 years. Family history for otosclerosis was recorded in 2 cases. Medical history revealed previous contralateral ear surgery and long-standing head trauma in 1 (2.1%) and 4 (8.3%) cases, respectively (Tab. I). Stapedial reflexes were absent in all patients.
Table I.
Most relevant patient and treatment-related variables.
| Variable | N. | % | |
|---|---|---|---|
| Mean age ± SD (range) - yr | 51.7 ± 14.0 (20-78) | ||
| Gender | Female | 26 | 54.2% |
| Male | 22 | 45.8% | |
| Side | Left | 25 | 53.1% |
| Right | 23 | 47.9% | |
| CT scan | MSCT | 20 | 41.7% |
| CBCT | 28 | 58.3% | |
| History | Family history of otosclerosis | 2 | 4.2% |
| Head trauma (long-term, > 1 year) | 4 | 8.3% | |
| Intraoperative findings | Stapes fixation | 23 | 47.9% |
| Incudo-malleolar ankylosis | 6 | 12.5% | |
| Ossicular chain discontinuity | 11 | 22.9% | |
| - Incudo-stapedial dislocation | (6) | (54.5%) | |
| - Erosion of the long process of the incus | (2) | (18.2%) | |
| - Severe erosion of the incus | (2) | (18.2%) | |
| - Stapes superstructure fracture | (1) | (9.1%) | |
| Tympanosclerosis | 8 | 16.7% | |
| Surgical procedure | Stapedotomy | 24 | 50% |
| Ossiculoplasty with remodeled incus | 18 | 37.5% | |
| Interposition of bone or cartilage fragment between the incus and the stapes | 4 | 8.3% | |
| TORP | 1 | 2.1% | |
| Positioning of stapedial prosthesis without stapedotomy | 1 | 2.1% | |
| Lysis of ME adherences | 1 | 2.1% | |
| Intraoperative complications | Injury of the chorda tympani | 7 | 14.6% |
| Post-operative complications | Temporary dizziness | 3 | 6.2% |
| Median GBI score (range) | 18, IQR:33.3 (-47.2, 55.5) | ||
| Overall satisfaction | Yes | 24 | 60% |
| No | 16 | 40% | |
| Unknown | (8) | ||
CBCT: cone beam computed tomography; IQR: Interquartile range; ME: middle ear; MSCT: multi-slice computed tomography; TORP: total ossicular replacement prosthesis.
The most frequent intraoperative finding was stapes fixation (23 cases, 47.9%), followed by ossicular chain discontinuity (11 cases, 22.9%), tympanosclerosis (8 cases, 16.7%) and ossicular chain ankylosis (6 cases, 12.5%) (Fig. 1). Ossicular chain discontinuity was mostly caused by incudo-stapedial dislocation (6 cases, 54.5%), followed by erosion of the long process of the incus (2 cases, 18.2%). Ossicular chain ankylosis was always at the level of the incudo-malleolar joint. In patients affected by tympanosclerosis, along with ME adherences, an incudo-malleolar ankylosis was observed (4 cases, 50%), whereas stapes fixation, incudo-stapedial dislocation and malleolar partial erosion was found in 1 case each (12.5%).
Figure 1.

Intraoperative findings and relative frequency (drawing by Michele Tomasoni).
Stapedotomy was the most common procedure performed (24 cases, 50%), followed by ossiculoplasty (23 cases, 47.9%) and lysis of ME adherences (1 case, 2.1%). Ossiculoplasty was mostly performed by interposition of remodeled incus (18 cases, 37.5%), whereas in the remaining cases interposition of bone or cartilage fragment (4 cases, 8.3%), total ossicular replacement prosthesis (TORP, 1 case, 2.1%) and stapedial prosthesis without stapedotomy (1 case, 2.1%) was performed. Intraoperative complications were limited to chorda tympani injury, reported in 7 cases (14.6%). Details of each patient included are reported in Table S1 (supplementary material). Except for 3 cases of temporary dizziness, no other post-operative complications were recorded.
Table S1.
Details of each patient included in the study.
| Patient | AGE | GENDER | SIDE | ABGPRE | Intra-operative findings | Diagnosis proposed | Surgical procedure | Intra-operative complications | ABGPOST | ABG reduction | ABG closure | Overall satisfaction | GBI total score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N1 | 68 | F | Left | 26.25 | Incudo-malleolar ankylosis | Ossicular chain ankylosis | Ossiculoplasty with remodeled incus | None | 20 | 6 | <10 | ||
| N2 | 67 | F | Right | 57.5 | Incudo-stapedial dislocation, incudo-malleolar ankylosis | Ossicular chain discontinuity | Ossiculoplasty with remodeled incus | None | 17.5 | 40 | >20 | No | 17 |
| N3 | 78 | F | Left | 37.5 | Incudo-stapedial dislocation | Ossicular chain discontinuity | Ossiculoplasty with remodeled incus | None | 17.5 | 20 | 10-20 | No | -47 |
| N4 | 72 | M | Right | 28.75 | Stapes fixation | Otosclerosis | Stapedotomy | Lesion of the Chorda Tympani | 47.5 | -19 | X | No | |
| N5 | 49 | F | Right | 30 | Erosion of the long process of the incus | Ossicular chain discontinuity | Ossiculoplasty with remodeled incus | None | 0 | 30 | >20 | ||
| N6 | 32 | F | Right | 41.25 | Incudo-stapedial dislocation | Ossicular chain discontinuity | Interposition of bone (from the EAC) between the incus and the stapes, stabilized with cement | None | 5 | 36 | >20 | Yes | 50 |
| N7 | 56 | F | Left | 23.75 | Stapes fixation | Otosclerosis | Stapedotomy | None | 11.25 | 13 | 10-20 | Yes | 28 |
| N8 | 62 | M | Right | 36.25 | ME adherences with incudo-malleolar ankylosis | Tympanosclerosis | Ossiculoplasty with remodeled incus | None | 15 | 21 | >20 | No | -11 |
| N9 | 22 | M | Right | 20 | Stapes fixation | Otosclerosis | Stapedotomy | None | 0 | 20 | 10-20 | Yes | 31 |
| N10 | 68 | M | Left | 28.75 | Incudo-malleolar ankylosis | Ossicular chain ankylosis | Ossiculoplasty with remodeled incus | Lesion of the Chorda Tympani | 18.75 | 10 | 10-20 | No | -6 |
| N11 | 38 | F | Right | 36.25 | Stapes fixation | Otosclerosis | Stapedotomy | None | 0 | 36 | >20 | Yes | 39 |
| N12 | 58 | F | Left | 18.75 | Stapes fixation | Otosclerosis | Stapedotomy | None | 10 | 9 | <10 | No | 8 |
| N13 | 20 | M | Right | 30 | Erosion of the long process of the incus | Ossicular chain discontinuity | Ossiculoplasty with remodeled incus | None | 23.75 | 6 | <10 | ||
| N14 | 35 | M | Right | 55 | Stapes fixation | Otosclerosis | Stapedotomy | Lesion of the Chorda Tympani | 12,5 | 43 | >20 | Yes | 42 |
| N15 | 42 | F | Left | 45 | Severe erosion of the incus | Ossicular chain discontinuity | Tympanoplasty type IV (interposition of cartilage fragment) | None | 13,75 | 31 | >20 | ||
| N16 | 46 | F | Right | 35 | Stapes fixation | Otosclerosis | Stapedotomy | Lesion of the Chorda Tympani | 0 | 35 | >20 | Yes | 33 |
| N17 | 34 | M | Right | 46.25 | ME adherences and incudo-stapedial dislocation | Tympanosclerosis, ossicular chain discontinuity | Lysis of ME adherences, ossiculoplasty with remodeled incus | None | 11.25 | 35 | >20 | Yes | 25 |
| N18 | 50 | F | Left | 45 | Stapes fixation | Otosclerosis | Stapedotomy | None | 10 | 35 | >20 | Yes | 11 |
| N19 | 31 | F | Left | 38.75 | Stapes fixation | Otosclerosis | Stapedotomy | None | 15 | 24 | >20 | No | -17 |
| N20 | 49 | M | Left | 27.5 | ME adherences, malleolar partial erosion (incudo-malleolar dislocation) | Tympanosclerosis, ossicular chain discontinuity | Lysis of ME adherences, tympanoplasty type II | None | 22.5 | 5 | <10 | No | -17 |
| N21 | 38 | F | Left | 63.75 | Incudo-malleolar ankylosis | Ossicular chain ankylosis | Ossiculoplasty with remodeled incus | None | 56.25 | 8 | <10 | No | -42 |
| N22 | 44 | F | Right | 61.25 | ME adherences with stapes fixation | Tympanosclerosis | Stapedotomy | Lesion of the Chorda Tympani | 21.25 | 40 | >20 | No | 0 |
| N23 | 26 | M | Left | 36.25 | Severe erosion of the incus and stapes superstructure | Ossicular chain discontinuity | TORP | None | 28.75 | 8 | <10 | Yes | 47 |
| N24 | 35 | F | Right | 23.75 | Incudo-stapedial and incudo-malleolar dislocation | Ossicular chain discontinuity | Ossiculoplasty with remodeled incus | Lesion of the Chorda Tympani | 0 | 24 | >20 | Yes | 11 |
| N25 | 57 | F | Left | 40 | ME adherences with incudo-malleolar ankylosis | Tympanosclerosis | Ossiculoplasty with remodeled incus | None | 20 | 20 | 10-20 | ||
| N26 | 54 | F | Left | 35 | Stapes fixation | Otosclerosis | Stapedotomy | None | 12.5 | 23 | >20 | Yes | 31 |
| N27 | 55 | M | Left | 48.75 | Stapes fixation | Otosclerosis | Stapedotomy | None | 5 | 44 | >20 | ||
| N28 | 37 | F | Left | 38.75 | Stapes fixation | Otosclerosis | Stapedotomy | None | 11.25 | 28 | >20 | No | 0 |
| N29 | 42 | M | Left | 32.5 | Incudo-malleolar ankylosis | Ossicular chain ankylosis | Ossiculoplasty with remodeled incus | None | 2,5 | 30 | >20 | Yes | 28 |
| N30 | 66 | F | Left | 37.5 | Incudo-stapedial dislocation | Ossicular chain discontinuity | Interposition of cartilage fragment between the incus and the stapes | None | 37.5 | 0 | <10 | No | |
| N31 | 72 | M | Right | 15 | Stapes fixation | Otosclerosis | Stapedotomy | None | 6.25 | 9 | <10 | Yes | 33 |
| N32 | 64 | F | Right | 41.25 | Incudo-malleolar ankylosis | Ossicular chain ankylosis | Ossiculoplasty with remodeled incus | None | 13.75 | 28 | >20 | No | -44 |
| N33 | 52 | M | Right | 28.75 | Stapes fixation | Otosclerosis | Stapedotomy | None | 8.75 | 20 | 10-20 | Yes | 47 |
| N34 | 56 | F | Left | 23.75 | Stapes fixation | Otosclerosis | Stapedotomy | None | 6.25 | 18 | 10-20 | Yes | 11 |
| N35 | 45 | M | Left | 62.5 | Stapes fixation | Otosclerosis | Stapedotomy | None | 0 | 63 | >20 | Yes | 19 |
| N36 | 45 | M | Right | 35 | Stapes fixation | Otosclerosis | Stapedotomy | None | 2.5 | 33 | >20 | Yes | 19 |
| N37 | 56 | M | Right | 22.5 | Stapes fixation | Otosclerosis | Stapedotomy | None | 22.5 | 0 | <10 | No | -28 |
| N38 | 60 | F | Left | 46.25 | Incudo-stapedial dislocation | Ossicular chain discontinuity | Interposition of cartilage fragment between the incus and the stapes | None | 22.5 | 24 | >20 | 11 | |
| N39 | 51 | M | Right | 35 | Stapes fixation | Otosclerosis | Stapedotomy | None | 7.5 | 28 | >20 | ||
| N40 | 71 | M | Right | 51.25 | ME adherences | Tympanosclerosis | Lysis of ME adherences | None | 41.25 | 10 | 10-20 | No | 0 |
| N41 | 54 | M | Right | 46.25 | Stapes fixation | Otosclerosis | Stapedotomy | None | 10 | 36 | >20 | Yes | 39 |
| N42 | 61 | M | Left | 53.75 | ME adherences with incudo-malleolar ankylosis | Tympanosclerosis | Ossiculoplasty with remodeled incus | None | 21.25 | 33 | >20 | Yes | 33 |
| N43 | 55 | M | Left | 22.5 | Stapes fixation | Otosclerosis | Stapedotomy | Lesion of the Chorda Tympani | 15 | 8 | <10 | Yes | 11 |
| N44 | 49 | F | Right | 38.75 | Stapes fixation | Otosclerosis | Stapedotomy | None | 3.75 | 35 | >20 | Yes | 56 |
| N45 | 61 | F | Left | 41.25 | Incudo-malleolar ankylosis | Ossicular chain ankylosis | Ossiculoplasty with remodeled incus | None | 21.25 | 20 | 10-20 | Yes | 36 |
| N46 | 63 | F | Right | 41.25 | ME adherences with incudo-malleolar ankylosis | Tympanosclerosis | Ossiculoplasty with remodeled incus | None | 26.25 | 15 | 10-20 | ||
| N47 | 67 | M | Right | 53.75 | Stapes suprastructure fracture | Ossicular chain discontinuity | Positioning of stapedial prosthesis without stapedotomy | None | 7.5 | 46 | >20 | No | 6 |
| N48 | 71 | F | Right | 58.75 | Stapes fixation | Otosclerosis | Stapedotomy | None | 6.25 | 53 | >20 | Yes | 44 |
Hearing outcomes
Mean values of pre- and post-operative air- and bone-conduction at 500, 1000, 2000 and 3000 Hz are depicted in Figure 2.
Figure 2.
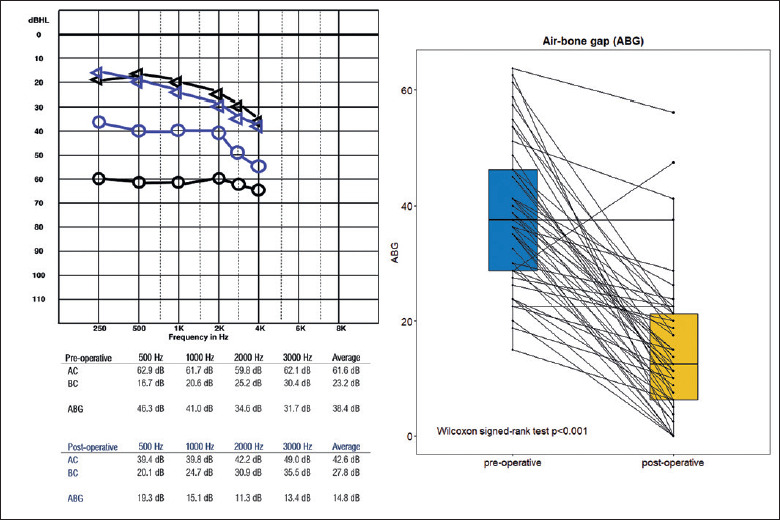
On the left, pure tone audiometry reporting the mean pre-operative (black) and post-operative (blue) air-conduction and bone-conduction thresholds. Values are reported with symbols for left ear by way of example. On the right, p-paired test showing the significant reduction in air-bone gap following surgery in our cohort of patients.
Mean pre-operative and post-operative ABG were 38.4 (range: 15-64) and 14.8 (range: 0-56), with a significant ABG reduction after surgery (Wilcoxon signed-rank test, p < 0.001) of 24 ± 15 dB (Fig. 2). In 1 case, (2.1%) an increase of ABG after surgery was observed (stapedotomy performed for a pre-operative CHL of 29 dB).
Post-operative ABG < 10 dB was observed in 20 cases (41.7%) and between 10-20 dB in 15 cases (31.2%). Non-satisfactory postoperative ABG (> 20 dB) was observed in 14 cases (29.2%) (Tab. S1). A significant positive correlation was observed between pre-operative ABG and ABG reduction (R = 0.62, p < 0.001) (Fig. 3A).
Figure 3.

(A) positive correlation between pre-operative air-bone gap (ABG) and ABG reduction (r = 0.64, p < 0.001); (B) negative correlation between post-operative ABG (r = -0.44, p = 0.005) and perceived benefit from surgery reported by patients through the “Glasgow Benefit Inventory (GBI)” questionnaire; (C) positive correlation between ABG reduction and GBI score (r = 0.41, p = 0.009).
Age at surgery, gender and side of treated ear were not significantly associated with any auditory measure, namely pre- and post-operative ABG and ABG.
Pre-operative ABG was not significantly associated with intraoperative findings (p = 0.510), as well.
Post-operative ABG was significantly influenced by intraoperative findings (p=0.006) and surgical procedure (p = 0.009) (Fig. 4). Patients affected by stapes fixation had a median post-operative ABG of 8.7 (IQR = 7.5), and significantly lower than patients affected by ossicular chain discontinuity (17.5, IQR = 16.9), ankylosis (19.4, IQR = 5.9) or tympanosclerosis (21.2, IQR = 4.7). Similarly, patients treated with stapedotomy showed significantly lower ABG after treatment (9.4, IQR = 7.8) compared to patients treated with ossiculoplasty with remodelled incus (18.1, IQR = 8.1) or other procedures (22.5, IQR = 18.7).
Figure 4.

(A) box-plots showing the significant difference (p = 0.011) in post-operative ABG according to intraoperative findings; (B) box-plots showing the significant difference (p = 0.018) in post-operative ABG according to surgery performed, tailored on intraoperative findings.
No significant differences in ABG reduction were observed according to intraoperative findings (p = 0.53) or surgical procedure performed (p = 0.39) (Fig. S1).
Figure S1.

(A) Box-plots showing the non-significant difference in ABG reduction according to intraoperative findings; (B) Box-plots showing the non-significant difference in ABG reduction according to surgery performed, tailored on intraoperative findings.
Patient-reported outcomes
GBI total score was available for 38 patients (79.2%) and ranged from -47.2 to 55.5, with a median value of 18 (IQR = 33.3).
Both post-operative ABG (R = -0.45, p = 0.004) and ABG reduction (R = 0.36, p = 0.024) were significantly correlated with perceived benefit (Fig. 3B-C). No correlation was found with pre-operative ABG (p = 0.660), age at surgery (p = 0.683), gender (p = 0.672), side (p = 0.110), or chorda tympani injury (p = 0.840). Better GBI scores were reported by patients affected by otosclerosis (p = 0.063) (Fig. S2).
Figure S2.
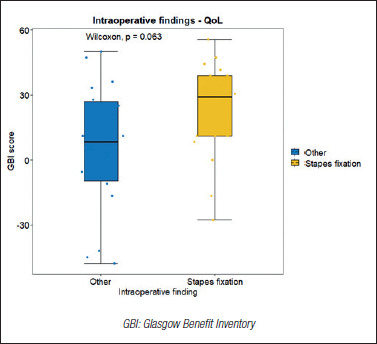
Box-plots showing the close-to-significant (p = 0.063) difference in GBI score according to intra-operative findings.
Overall satisfaction was reported by 60% of patients, with a mean GBI score of 31.9 (IQR = 20.2, range: 11.1-55.5). Patients who declared not to be satisfied with the surgical procedure reported a mean GBI of -8.3 (IQR = 25, range: -47.2-11.2). Patients affected by otosclerosis were significantly more satisfied (p = 0.025), whereas no significant association was found between overall satisfaction and gender (p = 0.990), side (p = 0.486), chorda tympani injury (p = 0.844), pre-operative mean air-conduction thresholds (p = 0.280), or pre-operative ABG (p = 0.930).
ROC curve analysis showed better results in terms of personal satisfaction in patients aged < 57-years (AUC = 0.706), showing post-operative ABG closure < 13.1 dB (AUC = 0.855) or ABG reduction > 28.7 dB (AUC = 0.725) (Fig. S3). No ideal cut-offs were found according to pre-operative ABG.
Figure S3.
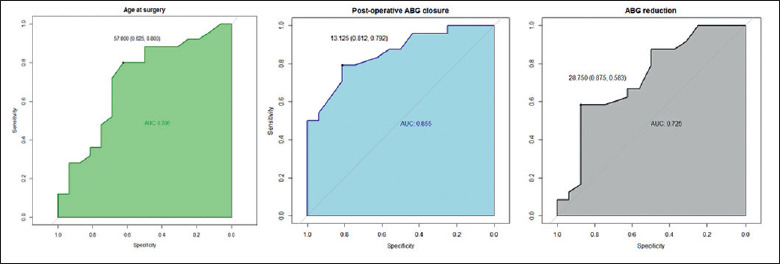
ROC curve analysis showing the ideal cut-off in age (57 years, AUC = 0.706), post-operative ABG closure (13.1 dB, AUC = 0.855) and ABG reduction (28.7 dB, AUC = 0.750) according to overall satisfaction reported by patients using the “Glasgow Benefit Inventory (GBI)” questionnaire.
Discussion
The main goal of the current study was to investigate intraoperative findings, auditory outcomes and related predictive factors in a population of patients affected by CHL presenting with normal pre-operative otoscopy, ME pressure and CT scan.
In this subset of patients, pre-operative PTA showed mean threshold values of air- and bone-conduction of 61.6 and 23.2 dB, respectively, with a relative ABG of 38.4 dB. The wide pre-operative ABG may be explained with the fact that there were patients suffering from CHL with no pre-operative evidence of ME disorders. In this setting, the surgeon cannot provide a reliable prediction of hearing restoration and surgical risks, commonly resulting in a delay of the procedure.
The diagnostic accuracy of CT scan in the setting of CHL has been widely demonstrated in acute and chronic inflammatory disorders and otosclerosis, whereas it is not well established in the rare occurrence of ossicular malformations or dislocation 7-9. In our experience, in 467 cases stapedotomy was scheduled following a radiological diagnosis of otosclerosis, whereas in 23 cases the exploratory tympanotomy revealed stapes fixation with normal pre-operative temporal bone CT scan. The overall accuracy of CT scan was 95.3%. Patients included in the current study often underwent preoperative CBCT (58.3%), which was at least as accurate as multi-slice CT or even superior in assessing structures related to conductive hearing loss, with lower radiation exposure 10.
In our cohort, a slightly higher proportion of female patients was observed (54.2%), with a mean age of 51.7 ± 14 years. These results reflect the well-known distribution of CHL in the general population, primarily driven by otosclerosis 7,11-13. Previous head trauma (8.3%) was reported less frequently compared to similar studies (Choi et al., 29%) 7, whereas family history of otosclerosis was rarely reported (4.2%), even if we consider only patients with stapes fixation (8.7%). Since all these patients had a normal pre-operative CT scan, the form of otosclerosis might be considered “mild” and potentially unrecognised and misdiagnosed within the family 12.
As described by Hong et al. 14, patients with CHL and absent acoustic reflexes generally are affected by ossicular disorders, most commonly, but not exclusively, secondary to otosclerosis. The detection of even one acoustic reflex should prompt further workup prior to ME exploration in the suspicion of third-window disorders. In our cohort, all patients undergoing ET had absent acoustic reflexes. However, in the experience of Hong et al. 14, a non-negligible rate of patients with an ossicular aetiology of CHL had detectable acoustic reflexes, concluding that the reflex test should not be considered infallible. For this reason, we do not recommend considering the stapedial reflex as a relevant variable in the decision-making algorithm for an ET in the case of a CHL with normal otoscopy, radiology and tympanogram.
The relative frequency (47.9%) of occult otosclerosis in our cohort was also reported by previous studies 7,11,15. In these cases, the degenerative otospongiotic process, originating from the fissula ante-fenestram, was probably wide enough to cause footplate fixation but not to be clearly depictable on pre-operative CT scan. In our experience, ossicular chain discontinuity (22.9%), ankylosis (12.5%) and tympanosclerosis (16.7%) were less common. The relative proportion of pathologic conditions underlying CHL is similar to previous publications 11,16.
As expected, stapedotomy was the most common surgery performed (50%), followed by ossiculoplasty with remodeled incus (37.5%). Similar results were reported by Kim et al., reporting most patients undergoing stapedotomy (77%) 11. On the contrary, the most common surgical procedure reported by Choi et al. was ossiculoplasty with PORP (49%), followed by stapedotomy (23%) and TORP (23%), although in that study pre-operative CT findings were not considered 7.
In our cohort, ET was a safe and effective procedure. Intraoperative complications consisted exclusively of accidental injury of the chorda tympani (14.6%), whereas after surgery only 3 cases of transitory dizziness were observed. However, it should be kept in mind that occult otosclerosis is the most common finding during ET. Since stapedotomy carries a non-negligible rate of potentially severe complications, surgical indication is discussed with patients when at least 20 dB of ABG is present.
Mean air-conduction threshold on 0.5-3 kHz went from a preoperative value of 61.6 to 42.6 dB after surgery, with a net mean gain of 23.1 dB, regardless the undergoing disease or surgery performed. Similar findings were reported by Kim et al. (17.3 dB) 11 and Choi et al. (19.4 dB) 7.
Most of our patients showed an excellent (< 10 dB, 41.7%) or good post-operative ABG (10-20 dB, 31.2%), whereas non-satisfactory post-operative ABG (> 20 dB) was observed in 14 cases (29.2%). Only 1 patient (2.1%) experienced an increase in the ABG (secondary to stapedotomy). Similar results were reported by Kim et al. 11, with excellent, good and non-satisfactory ABG closure found in 47.8, 32.8 and 19.4% of cases, respectively. The increase in the proportion of cases of ABG was comparable as well (5.3%), but in the experience of Kim et al. 11 this occurred after surgery for ossicular fixation and discontinuity.
None of the preoperative variables under study (sex, side and age at diagnosis) were useful in predicting auditory recovery after treatment. The only positive association found was between preoperative ABG and postoperative ABG reduction, suggesting that good ABG closure is achievable even in worst-case scenarios of large preoperative gap.
Conversely, intra-operative findings and the surgical procedure performed accordingly were better prognosticators of successful auditory recovery. When ET was diagnostic for stapes fixation and stapedotomy was performed, patients experienced better outcomes in terms of post-operative ABG closure, confirming what was previously described by Kim et al. and Choi et al. 7,11.
These results make audiological outcomes poorly predictable in the pre-operative setting, apart from the general expectation of greater ABG reduction in patients with higher pre-operative ABG 11.
As expected, higher GBI score was reported when lower postoperative ABG (R = -0.45) and greater ABG reduction (R = 0.36) were achieved, and when patients were diagnosed with otosclerosis, although only a close-to-significant association was found (p = 0.063).
When asked to express their general satisfaction, younger patients (< 57-years at surgery), with excellent post-operative auditory outcomes (ABG < 13.1 dB or ABG reduction > 28.7 dB) were more satisfied. The possible explanation for better satisfaction outcomes in younger patients may come from the higher proportion of otosclerosis, as confirmed by the significantly greater satisfaction reported by patients diagnosed with otosclerosis (p = 0.025).
The current study presents some limitations. First, this is a retrospective study based on a relatively small number of patients given the rarity of the condition. Second, the wide spectrum of disease and the low number of cases for each condition did not allow further sub-analysis. Third, GBI score was not available for all patients.
Conclusions
Despite the high accuracy demonstrated by CT scan, CHL with normal ME pressure, otoscopy and radiological findings is still possible. In this setting, ET represents the mainstay of treatment, but pre-operative predictions of both auditory recovery and patients perceived benefit after surgery are extremely challenging, with only younger age offering a partial clue of better results. Surgeons should be prepared to tailor surgery according to intraoperative findings with variable auditory outcomes. In our experience, occult otosclerosis was the most common diagnosis, with the best results in terms of post-operative ABG and patient satisfaction. Although rare (about 2%), patients should be informed of a non-negligible risk of worsening of their ABG.
Conflict of interest statement
The authors declare no conflict of interest.
Author contributions
Study design and concept: TS. Material preparation and ethical aspects: ADer, TS, ADeg. Data collection: ADer, MT. Data analysis: MT, DB, TS. Writing and editing: MT, DB, MA, AS, SZ. Critical Revision: LRdZ, CP, ADeg, TS.
Ethical consideration
This study was approved by the Institutional Ethics Committee of the University of Brescia (approval number N4357).
The research was conducted ethically, with all study procedures being performed in accordance with the requirements of the World Medical Association’s Declaration of Helsinki.
Written informed consent was obtained from each participant/patient for study participation and data publication.
Figures and tables
Funding Statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Lin FR, Niparko JK, Ferrucci L. Hearing loss prevalence in the United States. Arch Intern Med 2011;171:1851-1852. https://doi.org/10.1001/archinternmed.2011.506 10.1001/archinternmed.2011.506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Michels TC, Duffy MT, Rogers DJ. Hearing loss in adults: differential diagnosis and treatment. Am Fam Physician 2019;100:98-108. [PubMed] [Google Scholar]
- 3.Sooriyamoorthy T. Conductive hearing loss. Treasure Island: StatPearls Publishing; 2021. [PubMed] [Google Scholar]
- 4.Lippy WH, Burkey JM, Schuring AG, et al. Stapedectomy in patients with small air-bone gaps. Laryngoscope 1997;107:919-922. https://doi.org/10.1097/00005537-199707000-00016 10.1097/00005537-199707000-00016 [DOI] [PubMed] [Google Scholar]
- 5.Committee on Hearing and Equilibrium. Committee on Hearing and Equilibrium guidelines for the evaluation of results of treatment of conductive hearing loss. Otolaryngol Head Neck Surg 1995;113:186-187. https://doi.org/10.1016/S0194-5998(95)70103-6 10.1016/S0194-5998(95)70103-6 [DOI] [PubMed] [Google Scholar]
- 6.Robinson K, Gatehouse S, Browning GG. Measuring patient benefit from otorhinolaryngological surgery and therapy. Ann Otol Rhinol Laryngol 1996;105:415-422. https://doi.org/10.1177/000348949610500601 10.1177/000348949610500601 [DOI] [PubMed] [Google Scholar]
- 7.Choi JH, Lee MY, Park JH, et al. Conductive hearing loss with an intact tympanic membrane due to non-inflammatory causes. Auris Nasus Larynx 2016;43:144-148. https://doi.org/10.1016/j.anl.2015.06.004 10.1016/j.anl.2015.06.004 [DOI] [PubMed] [Google Scholar]
- 8.Lagleyre S, Sorrentino T, Calmels MN, et al. Reliability of high-resolution CT scan in diagnosis of otosclerosis. Otol Neurotol 2009;30:1152-1159. https://doi.org/10.1097/MAO.0b013e3181c2a084 10.1097/MAO.0b013e3181c2a084 [DOI] [PubMed] [Google Scholar]
- 9.Shin YJ, Deguine O, Cognard C, et al. Fiabilité du scanner dans le diagnostic des surdités de transmission à tympan normal. Rev Laryngol Otol Rhinol (Bord) 2001;122:81-84. [PubMed] [Google Scholar]
- 10.Kemp P, Stralen JV, De Graaf P, et al. Cone-beam CT compared to Multi-Slice CT for the diagnostic analysis of conductive hearing loss: a feasibility study. J Int Adv Otol 2020;16:222-226. https://doi.org/10.5152/iao.2020.5883 10.5152/iao.2020.5883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim SH, Cho YS, Kim HJ, et al. Operative findings of conductive hearing loss with intact tympanic membrane and normal temporal bone computed tomography. Eur Arch Otorhinolaryngol 2014;271:1409-1414. https://doi.org/10.1007/s00405-013-2585-y 10.1007/s00405-013-2585-y [DOI] [PubMed] [Google Scholar]
- 12.Gapany-Gapanavicius B. The incidence of otosclerosis in the general population. Isr J Med Sci 1975;11:465-468. [PubMed] [Google Scholar]
- 13.Cajade Frías J, Labella Caballero T. Aspectos epidemiológicos de la otosclerosis (II). Sexo, factores hereditarios, tiempo de evolución hasta el diagnóstico, edad de diagnóstico y de comienzo. An Otorrinolaringol Ibero Am 2003;30:17-30. [PubMed] [Google Scholar]
- 14.Hong RS, Metz CM, Bojrab DI, et al. Acoustic reflex screening of conductive hearing loss for third window disorders. Otolaryngol Head Neck Surg. 2016;154:343-348. https://doi.org/10.1177/0194599815620162 10.1177/0194599815620162 [DOI] [PubMed] [Google Scholar]
- 15.Robertson G, Mills R. Findings at exploratory tympanotomy for conductive hearing loss. J Laryngol Otol 2009;123:1087-1089. https://doi.org/10.1017/S0022215109005696 10.1017/S0022215109005696 [DOI] [PubMed] [Google Scholar]
- 16.Ghonim MR, Shabana YK, Ashraf B, et al. Traumatic ossicular disruption with intact tympanic membrane: treatment modalities in 42 patients: our experience. Clin Otolaryngol 2016;41:176-179. https://doi.org/10.1111/coa.12461 10.1111/coa.12461 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


