Highlights
-
•
Evaluation of the FISS and TRISS SpO2 to obtain greater rigor in a standardized epidemiological profile of injury severity.
-
•
More accurate determination of trauma severity in child and adolescent victims of traffic accidents for improved urgency and emergency care.
-
•
Relation between the scales allows for better decisions on patient hospitalization, adequate treatment and the prevention of irreversible injuries.
1. Introduction
In the paediatric population, a high number of factors may be associated with mortality, disability and multiple injuries. In this regard, maxillofacial and cranioencephalic injuries have a significant influence, among which traffic accidents are the most common cause, representing 34.2–57.8% of all cases [1,2,3,4,5]. Such accidents are commonly associated with recklessness and disobeying the local traffic laws [6,7].
To better define the standard summary measure of human trauma, Baker and collaborators in 1974 proposed the creation of the Injury Severity Score based on the Abbreviated Injury Scale [8,9] Some methods, such as the Trauma and Injury Severity Scale (TRISS) [10] offered changes using characteristics such as age, the Glasgow Coma Scale, systolic systemic pressure and respiratory rate to quantify the probability of survival following the consequences of the trauma. Thus, assigning a numerical score that provides a standardized epidemiological profile is of great importance for decisions regarding hospitalization, for improving the proper treatment of injuries and concomitant complications and also for preventing irreversible damage [11,12].
Previous studies performed some adjustments to the TRISS to improve its accuracy [12,13]. One of these was the TRISS peripheral oxygen saturation (TRISS SpO2), which in emergency situations allows the quality of tissue perfusion in trauma patients to be assessed more quickly and measured more easily compared to the respiratory rate [14]In addition, more specifically in the maxillofacial region, the Facial Injury Severity Scale (FISS) is widely used for classifying the severity of facial injuries, verifying numerical scores for fractures and lacerations in all regions of the face [15,16].
Facial fractures in young people are proportionally rare (5–15%) compared with adults [6,7,17] [[6], [7], [17], [18], [19], [20], [21]] [21]. However, the singularities of this age group make the treatment a challenge due to the difficulty of the youngest in expressing their symptoms, as well as the influence on anatomical development and the psychosocial influences that trauma causes [19,22,23].
Although an efficient scale has been established to measure patient trauma, it is not possible to accurately determine the severity in paediatric patients. Thus, it is necessary to establish a better measure for more accurate verification of the trauma severity and mortality in paediatric patients [24,25]. This study aims to evaluate the possible relation between the FISS and TRISS SpO2 for facial trauma in child and adolescent victims of traffic accidents, and the characteristics associated with each scale, in a referral urgency and emergency hospital in the north of Brazil.
2. Materials and methods
2.1. Study design
A cross-sectional retrospective observational study was carried out based on an analysis of electronic medical data records of cases involving oral and maxillofacial fracture in a referral urgency and emergency hospital in the north of Brazil. The fracture establishments were determined by retrieving computed tomography images and three-dimensional reconstruction. The presented institution receives high complexity trauma, meeting the demands of one of the main cities in the region and supporting 75 neighbouring cities, covering a population of more than 5.5 million people. The study was carried out in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [26].
2.2. Eligibility criteria
Data from medical records of patients aged 0–19 years with maxillofacial traumas and aetiology strictly related to traffic accidents from January 2014 to December 2019 were included. This study defines the group ages according to the World Health Organization (WHO): 0–4 years, early childhood; 5–9 years, late childhood; 10–14 years, early adolescence; 15–19 years, late adolescence [27]. All electronic medical records were used in the research and none were considered inconsistent or incomplete.
2.3. Data collection
Data regarding age, gender, bone fracture [temporal/frontal bone, orbital, zygomatic complex, naso-orbital-ethmoid complex, nasal bone, maxilla and mandible (including fractures of the symphysis, parasymphysis, body, angle, ramus, coronoid, extra-articular condyle and intra-articular condyle)], traffic trauma aetiology (motorcycle, car, cycling, maritime, pedestrian and animal riding accidents), the affected facial third (upper, middle and lower), the FISS, the TRISS SpO2 and hospitalization days to treatment were collected.
The SpO2 was evaluated in this study because it was the measure adopted by the medical team and presented in the electronic medical records.
Ethical approval
The Ethics Committee of approved the realization of the present study (CAAE 34572820.3.0000.0018).
2.4. Severity scales
The FISS is a numerical scale that measures the severity of maxillofacial bone injuries by considering the patient's individual fracture pattern. The scale divides the face into three horizontal thirds (mandible, middle face and upper face) and also incorporates the sum of the size of all lacerations on the face. The score is obtained by the sum of each fracture, and the total sum predicts the hospital length of stay and recovery. The scale assists the communication between clinicians and health professionals in surgical planning as a tool for researching maxillofacial injuries [13]. Among the scales presented in previous studies, the FISS is considered to be the most reliable and specific for facial trauma [28].
The TRISS SpO2 offers an accurate and personalized standard approach for assessing trauma care outcome using the original TRISS variation with adjusted coefficients. Anatomical, physiological and age characteristics are used to quantify the probability of survival in relation to the severity of the injury. The values obtained are based on the data for age, the Glasgow Coma Scale, systolic systemic pressure, injury severity score and SpO2 [10,14].
2.5. Statistical analysis
Averages and percentages are presented as descriptive statistics. Statistical analysis was performed using R statistical software (version 3.0.1). Data normalization of the severity scales involved was performed and the variables were tested using the t-test. The degree of statistical significance was considered to be p < 0.05.
3. Results
A total of 93,250 patients who suffered any trauma were reviewed during the research. Among them, 20,516 (22%) were aged 0–19 years. Of these, 537 children and adolescents with oral and/or maxillofacial fractures were admitted, 330 due to traffic accidents. Male patients (257; 77.88%) were more affected than females (73; 22.11%), with a male/female ratio of 3.5:1 (Table 1). Motorcycle accidents were the most commonly reported aetiology (264; 80%), followed by being run over (31; 9.39%) and cycling accidents (12; 3.64%).
Table 1.
Types of traffic accidents (%).
| Aetiology of traffic accidents | Gender |
Age (years) |
Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | 0–04 |
05–09 |
10–14 |
15–19 |
||||||
| Male | Female | Male | Female | Male | Female | Male | Female | ||||
| Number of cases | 257 (77.88) | 73 (22.12) | 9 (2.73) | 3 (0.91) | 11 (3.33) | 3 (0.91) | 23 (6.97) | 11 (3.33) | 214 (64.85) | 56 (16.97) | 330 (100.00) |
| Motocicle | 211 (63.94) | 53 (16.06) | 1 (0.3) | 1 (0.30) | 2 (0.61) | 1 (0.30) | 12 (3.64) | 3 (0.91) | 196 (59.39) | 48 (14.54) | 264 (80.00) |
| Run over | 20 (6.06) | 11 (3.33) | 4 (1.21) | 1 (0.30) | 5 (1.51) | 2 (0.61) | 5 (1.51) | 4 (1.21) | 6 (1.82) | 4 (1.21) | 31 (9.39) |
| Maritime | 6 (1.82) | 4 (1.21) | 1 (0.30) | – | 2 (0.61) | – | 1 (0.30) | 1 (0.30) | 2 (0.61) | 3 (0.91) | 10 (3.03) |
| Car | 8 (2.42) | 1 (0.30) | 1 (0.30) | 1 (0.30) | 1 (0.30) | – | 1 (0.30) | – | 5 (1.51) | – | 9 (2.73) |
| Cycling | 8 (2.42) | 4 (1.21) | – | – | 1 (0.30) | – | 3 (0.91) | 3 (0.91) | 4 (1.21) | 1 (0.30) | 12 (3.64) |
| Transport animal | 4 (1.21) | – | 2 (0.61) | – | – | – | – | – | 2 (0.61) | – | 4 (1.21) |
Averages of 154.83 cases per year and 2.81 fractures per patient were presented. The middle third of the face was the most affected (578; 62.22%), followed by the lower (280; 30.14%) and upper (71; 7.64%) thirds. When the mandible was observed, the angle (61; 6.57%) and condyle (61; 6.57%) were mostly affected, followed by the body (56; 6.03%) and parasymphysis (56; 6.03%) (Table 2). The mean values obtained on the FISS were 5.20 for male and 4.96 for female. On the TRISS SpO2, the corresponding values were 0.148 for male and 0.160 for female.
Table 2.
Number of fracture variables (%).
| Fracture variables | Gender |
Age (years) |
Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | 0–04 |
05–09 |
10–14 |
15–19 |
||||||
| Male | Female | Male | Female | Male | Female | Male | Female | ||||
| Number of fractures | 740 (79.65) | 189 (20.34) | 19 (2.04) | 13 (1.40) | 30 (3.23) | 5 (1.52) | 47 (5.06) | 26 (2.80) | 644 (69.32) | 145 (15.61) | 929 (100) |
| Zygomatic | 159 (17.12) | 39 (4,20) | 3 (0,32) | 1 (0,11) | 7 (0.75) | – | 16 (1.72) | 6 (0.65) | 133 (14.32) | 32 (3.44) | 198 (21.31) |
| Mandible | 218 (23.47) | 58 (6,24) | 10 (1,08) | 6 (0,65) | 10 (1.08) | 3(0.32) | 11 (1.18) | 13 (3,94) | 187 (20,13) | 36 (3.88) | 276 (29.71) |
| Maxilla | 117 (12.59) | 25 (2,69) | – | 2 (0,22) | 2(0.22) | 1 (0.11) | 4 (0.43) | 1 (0,11) | 111 (11,95) | 21 (2.26) | 142 (15.29) |
| Nasal | 49 (5.27) | 14 (1.51) | 1 (0.11) | 1 (0.11) | 1 (0.11) | 1 (0.11) | 4 (0.43) | 3 (0.32) | 43 (4.63) | 9 (0.97) | 63 (6.78) |
| Orbit | 75 (8.07) | 17 (1.83) | 2 (0.22) | 1 (011) | 4 (0.43) | – | 4 (0.43) | 2 (0.22) | 65 (7.00) | 14 (1.51) | 92 (9.90) |
| Naso-orbital-ethmoidal | 48 (5.17) | 12 (1.29) | 2 (0.22) | 1 (0.11) | 3 (0.32) | – | 1 (0.11) | – | 42 (4.52) | 11 (1.18) | 60 (6.46) |
| Frontal | 59 (6.35) | 17 (1.83) | 1 (0.11) | 1 (0.11) | 2 (0.22) | – | 5 (1.52) | – | 51 (5.49) | 16 (1.72) | 76 (8.18) |
| Dentoalveolar | 15 (1.61%) | 7 (0.75%) | – | – | 1 (0.11%) | – | 2 (0.22%) | 1 (0.11%) | 12 (1.29%) | 6 (0.65%) | 22 (2.37%) |
To assess general trauma severity, the TRISS SpO2 was performed. It is observed that when the trauma involves a bicycle accident (0.059) or riding accident (0.058), the mean score is relatively low, with higher values for car accidents (0.242), being run over (0.218), motorcycle accidents (0.136) and maritime accidents (0.135). The FISS, on the other hand, had the highest average values for car accidents (7.00), maritime accidents (6.70), motorcycle accidents (5.25) and being run over (4.39), with the lowest values for accidents involving cycling (3.00) and animal transport (2.75) (Table 3).
Table 3.
Study average TRISS SpO2 and FISS in aetiology of traffic accidents.
| TRISS SpO2 and FISS variables |
Gender |
Age (years) |
Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Male |
Female |
0–4 |
05–09 |
10–14 |
15–19 |
||||||
| Male | Female | Male | Female | Male | Female | Male | Female | ||||
| TRISS SpO2 average | |||||||||||
| Score average | 0.148 | 0.160 | 0.086 | 0.592 | 0.178 | 0.177 | 0.121 | 0.200 | 0.152 | 0.127 | 0.151 |
| Motocicle | 0.149 | 0.132 | 0.031 | 0.032 | 0.039 | 0.060 | 0.075 | 0.335 | 0.155 | 0.123 | 0.136 |
| Pedestrian | 0.172 | 0.300 | 0.137 | 0.946 | 0.179 | 0.236 | 0.308 | 0.265 | 0.077 | 0.208 | 0.218 |
| Maritime | 0.179 | 0.069 | 0.047 | – | 0.091 | – | 0.060 | 0.032 | 0.393 | 0.082 | 0.135 |
| Car | 0.173 | 0.799 | 0.424 | 0.799 | 0.825 | – | 0.051 | – | 0.091 | – | 0.242 |
| Cycling | 0.056 | 0.065 | – | – | 0.047 | – | 0.042 | 0.037 | 0.068 | 0.150 | 0.059 |
| Animal riding | 0.058 | – | 0.047 | – | – | – | – | – | 0.068 | – | 0.058 |
| FISS variables | |||||||||||
| Score average | 5.20 | 4.96 | 3.88 | 8.66 | 5.18 | 2.33 | 3.69 | 3.54 | 5.41 | 5.18 | 5.14 |
| Motocicle | 5.32 | 4.94 | 2.00 | 5.00 | 2.50 | 3.00 | 4.75 | 5.66 | 5.40 | 4.94 | 5.25 |
| Pedestrian | 4.85 | 3.54 | 5.00 | 4.00 | 4.8 | 2.00 | 2.8 | 2.75 | 6.5 | 5.00 | 4.39 |
| Maritime | 6.33 | 7.25 | 4.00 | – | 11.00 | – | 6.00 | 5.00 | 3.00 | 8.00 | 6.70 |
| Car | 5.75 | 17.00 | 4.00 | 17.00 | 2.00 | – | 2.00 | – | 7.60 | – | 7.00 |
| Cycling | 2.62 | 3.75 | – | – | 4.00 | – | 1.00 | 2.00 | 3.50 | 9.00 | 3.00 |
| Animal riding | 2.75 | – | 2.50 | – | – | – | – | – | 3.00 | – | 2.75 |
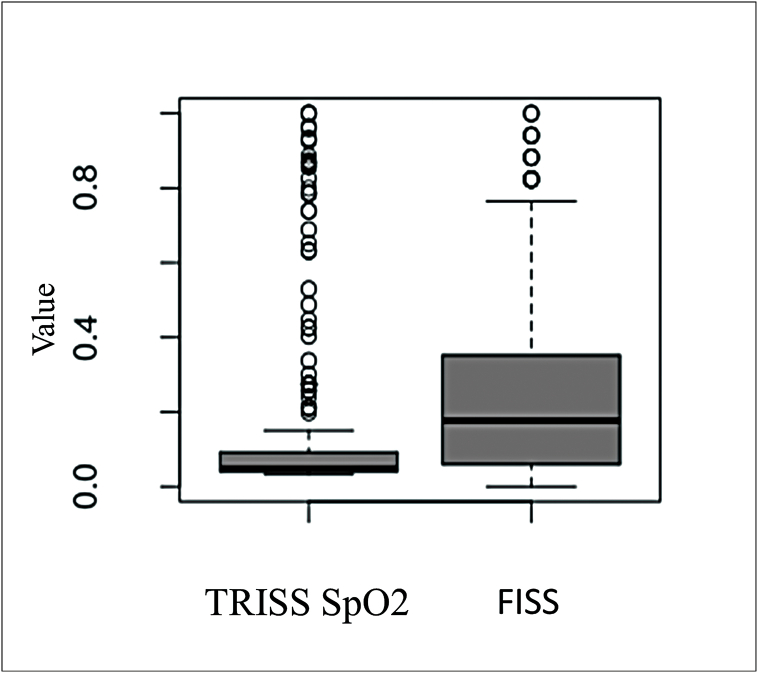
In the boxplot of Fig. 1, the TRISS SpO2 variable has a high concentration of values and a median well below the FISS variable, indicating a significant difference between them that was confirmed with the t-test (Table 4). In addition, it is possible to observe a high number of outliers in the two variables.
Fig. 1.
Boxplot of TRISS SpO2 and FISS variables between 0 and 19 years of age after normalization.
Table 4.
t-test for the age variable in a traffic accident.
| Age (Years group) | Means |
t | p_Valor | |
|---|---|---|---|---|
| TRISS | FISS | |||
| 0–4 | 0,1070 | 0,4140 | −2998 | 0,006 |
| 5–9 | 0,1471 | 0,3967 | −3051 | 0,005 |
| 10–14 | 0,1274 | 0,2728 | −2469 | 0,016 |
| 15–19 | 0,1511 | 0,2393 | −4193 | 0,000 |
| 0–19 | 0,1460 | 0,2431 | −5272 | 0,000 |
The boxplot in Fig. 2 follows the same pattern, indicating a significant difference between the TRISS SpO2 and FISS in all age groups, the greatest difference between the scales being in the age group of 0–4 years.
Fig. 2.
Boxplots of TRISS SpO2 and FISS variables after normalization. a) Boxplots to 0–04 years of age; b) Boxplots to 05–09 years of age; c) Boxplots to 10–14 years of age; d) Boxplots to 15–19 years of age.
After normalization of the scales, the observed averages of the TRISS SpO2 and FISS variables are 0.1460 and 0.2431, respectively. When looking at age groups, the following averages were obtained for the TRISS SpO2 and FISS, respectively: 0–4 years, 0.1070 and 0.4140; 5–9 years, 0.1471 and 0.3967; 10–14 years, 0.1274 and 0.2728; and 15–19 years, 0.1511 and 0.2393 (Fig. 2).
The average days of hospitalization showed a relationship with the FISS and TRISS SpO2: the higher the mean value of the FISS and TRISS SpO2, the greater the mean number of days of hospitalization. It can be observed that when the score in the scales is lower, the average number of days of hospitalization is 10.32 days, whereas a maximum score leads to an average of 29.50 days of hospitalization.
4. Discussion
Traffic accidents in children are accepted as one of the leading causes of maxillofacial fractures and a major cause of mortality and disability worldwide [29]. Scoring systems to determine severity in paediatric trauma depend on age and mechanism of injury, as there are significant differences in the physiology of infants, children and adolescents, and their responses to injuries are not the same as in adults [24].
In this study, we showed that the number of facial fractures substantially increased with the age group. We support the view that adolescents’ lifestyle is closer to the adult lifestyle, whereas children are less involved in dangerous activities because they are usually under supervision [20,21]. In addition, paediatric craniofacial bone has unique characteristics to protect the facial bones from trauma, being more stable due to the greater elasticity of the bone, the nature of the adipose tissue and the lack of pneumatization of the sinuses, with the unerupted permanent dentition giving additional strength to the jaw bones [29]. Even with a higher number of fractures in the 15–19-year age group of this study, there was no proportionally higher statistical significance for the severity of body trauma with the TRISS SpO2 and facial fracture with the FISS in relation to the other age groups. Among the aetiologies, there is a prevalence of traumas in motorcycle accidents but no absolute prevalence of statistical significance in relation to the other aetiologies.
Our data are also in accord with the very recent evidence supporting males as presenting more fractures than females [20,30] [[20], [30], [31], [32]] [32]. This may be related to several factors: male participate in activities that are more physical and often are more aggressive than female, involving themselves in a greater number of aetiologies, whereas female are more associated with aetiologies that have less trauma exposure [20,33]. Previous literature has reported that the mean severity of general and maxillofacial trauma is higher in male patients; however, this factor was not observed in our study, where similar means were observed in both males and females on the FISS and TRISS SpO2 scales [34,35].
Studies indicate that injuries to different parts of the body act to increase or decrease the severity of trauma in young people [35]. The present study compared the FISS and TRISS SpO2 scales to verify whether there is a relationship between the severity of trauma on the face and injuries in other regions of the body. In this context, when analyzing severity through two scales – general (TRISS SpO2) and specific (FISS) – better accuracy and precision can be obtained. This measure makes it possible to verify whether the general significance level of severity is related to local values of severity in a given population, as in the case of the age groups of children and young people.
In this study, a statistically significant difference was observed between the median values of the FISS and TRISS SpO2 severities. Regarding age group, the greatest significant discrepancy was found in children aged 0–4 years, with high local severity significance (FISS) and low overall severity value (TRISS SpO2). This demonstrates that even with a high value observed on a local scale, a high general value will not necessarily be obtained, requiring a more accurate assessment of this relationship.
In this study, mandibular fractures were the most frequently encountered facial fractures in all age groups and this agrees with previously published studies [20,21,36,37]. Condyle and mandibular angle fractures are the most prevalent in the bones of the lower third of the face, mainly in the group aged 0–4 years [21,36,38]. However, orbital fractures involving the walls and floor are more common in patients older than 7 years of age [39].
The aetiology of facial fractures varies depending on social, cultural and environmental factors [40]. Traffic accidents, which are high-energy impacts, are reported as aetiologies with high severity in general and maxillofacial trauma and can be graded within the TRISS SpO2 and FISS scales [35,40,41]. In this study, among the traffic accidents there is a prevalence of motorcycle accidents. The high percentage of male victims aged 15–19 years is noteworthy. There is currently a consensus in the literature that the vast majority of maxillofacial trauma is associated with this aetiology [30] [[30], [31], [32]] [32]. Children using motorcycles, either as drivers or pillion riders, is a reality in many Brazilian cities and infants are often carried on motorcycles by the driver or another passenger. This makes children and adolescents vulnerable to accidents. Furthermore, many of these individuals do not use crash helmets.
A lack of public transport in the metropolitan area of the city forces the population, especially young people, to use motorcycles and bicycles as a means of public transport, often with little or no safety equipment [28,42,43]. Accidents involving pedestrians are also very common and have a high rate of morbidity due to the relatively small mass of a pedestrian compared to a car, thus offering little resistance and absorbing the energy of the impact [42] The data on aetiology were significantly related to being run over, car accidents and motorcycle accidents in the TRISS SpO2 and to motorcycle and cycling accidents in the FISS, showing a variety of significance within the severity of the trauma according to the means of transport (two- or four-wheel vehicles).
In the countries of Asia, 14.28% of maxillofacial traumas are associated with falls due to animal riding. In these countries, horse breeding is prevalent and is the oldest traditional branch of livestock in Asia [44]. Regarding maritime traffic, in some places this form of transport is commonly used due to the large network of waterways found or used in sporting activities, as in the region of this study. Although accidents are not so common, the absence of safety equipment can lead to an emergency in most cases [45]. In our research, we found significant data on maritime accidents for the TRISS SpO2 in male aged 15–19 years and for the FISS in male aged 5–9 and 10–14 years, showing the great severity of this aetiology.
As with previous studies [7], in traffic accidents the middle third of the face is more affected by facial fractures in children and adolescents, with the zygomatic complex mostly affected [29,46]. In other studies, even the results indicating the same prevalence in relation to age showed a greater number of fractures in the lower third of the face, in contrast to the results of this study. Another point is that the authors report the lower third of the face as more accessible during trauma, but in many cases the victim assumes a defensive position, lowering the chin before facial trauma and making the middle of the face more susceptible to injuries or fractures [19,21,47,48]. As in this study, other research indicated that more than one-third of the face can be involved in facial trauma, with one or more bone fractures [49].
Considering our study, the severity of maxillofacial trauma according to the FISS in paediatric patients has higher statistical significance than injuries in the rest of the body if we consider the TRISS SpO2 [40]. Regarding severity, greater severity was observed in multiple facial trauma patients, which corroborates with other findings in the literature [31,49]. In this study, mandible fractures had the most numerical significant data, with emphasis on males aged 15–19 years.
Our study corroborates the literature, where patients with the highest means of the TRISS SpO2 and FISS scores also had the highest mean days of hospitalization for treatment [43].
5. Conclusion
We conclude that there is a statistically significant difference in the relationship between the FISS and TRISS SpO2 with general age and between groups of child and adolescents in the aetiology of traffic accidents with facial trauma.
However, this relationship corroborated with more efficiency, amplitude and precision in determining the severity and mortality of these patients.
Author contribution
TBX: literature search, study design, data collection and writing.; CLSM: data collection, writing and data interpretation.; JGRL: data collection, literature search and writing.; LLS: study design, data analysis and data interpretation.; DPF: data collection and writing.; DVM: data collection and data analysis.; MSM: data collection and critical review.; NCN: data collection and critical review.; HARP: study design, writing and critical review
Contributor Information
Thiago Brito Xavier, Email: thiagohujbb@gmail.com.
Clarina Louis Silva Meira, Email: clarinalouiscks@hotmail.com.
Jeanne Gisele Rodrigues de Lemos, Email: jgrlemos@gmail.com.
Lucas Lacerda de Souza, Email: lucaslac@hotmail.com.
Diego Pacheco Ferreira, Email: dr.diegopacheco@hotmail.com.
Diogo de Vasconcelos Macedo, Email: diogo.v.macedo@gmail.com.
Marcelo Silva Monnazzi, Email: monnazzi@hotmail.com.
Nicolau Conte Neto, Email: nicolauneto@ufpa.br.
Hélder Antônio Rebelo Pontes, Email: harp@ufpa.br.
References
- 1.Srinivas S., McLoughlin R.J., Hazeltine M.D., Green J., Hirsh M.P., Cleary M.A., Aidlen J.T. Pediatric snow sport injuries differ by age. J. Pediatr. Surg. 2021;56:520–525. doi: 10.1016/j.jpedsurg.2020.05.034. [DOI] [PubMed] [Google Scholar]
- 2.Yesantharao P.S., Lopez J., Chang A., Hicks J., Reategui M.L., Thomas G., Manson P.N., Dorafshar A., Redett R.J. The association of zygomaticomaxillary complex fractures with naso-orbitoethmoid fractures in pediatric populations. Plast. Reconstr. Surg. 2021:777E–786E. doi: 10.1097/PRS.0000000000007836. [DOI] [PubMed] [Google Scholar]
- 3.Tashakkori P., Unkel J., Berry E. Section on Oral Health Program. American Academy of Pediatrics; 2021. Challenging diagnosis of mandibular fractures in the pediatric emergency department: a clinical case report; pp. 770.1–77770. [DOI] [Google Scholar]
- 4.de Macedo Bernardino, Santos L.M., Ferreira A.V.P., de Almeida Lima T.L.M., da Nóbrega L.M., d'Avila S. Multiple correspondence analysis as a strategy to explore the association between categories of qualitative variables related to oral–maxillofacial trauma and violent crimes at the community level. Int. J. Oral Maxillofac. Surg. 2018;47:339–344. doi: 10.1016/j.ijom.2017.08.001. [DOI] [PubMed] [Google Scholar]
- 5.Boffano P., Roccia F., Zavattero E., Dediol E., Uglešić V., Kovačič Ž., Vesnaver A., Konstantinović V.S., Petrović M., Stephens J., Kanzaria A., Bhatti N., Holmes S., Pechalova P.F., Bakardjiev A.G., Malanchuk V.A., Kopchak A.v., Galteland P., Mjøen E., Skjelbred P., Grimaud F., Fauvel F., Longis J., Corre P., Løes S., Lekven N., Laverick S., Gordon P., Tamme T., Akermann S., Karagozoglu K.H., Kommers S.C., Meijer B., Forouzanfar T. European Maxillofacial Trauma (EURMAT) in children: a multicenter and prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;119:499–504. doi: 10.1016/J.OOOO.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 6.AlAli A.M., Ibrahim H.H.H., Algharib A., Alsaad F., Rajab B. Characteristics of pediatric maxillofacial fractures in Kuwait: a single-center retrospective study. Dent. Traumatol. 2021 doi: 10.1111/edt.12662. [DOI] [PubMed] [Google Scholar]
- 7.Khan S.R., Khan Z.A., Hanif S., Riaz N., Warraich R.A. Patterns of facial fractures in children. Br. J. Oral Maxillofac. Surg. 2019;57:1009–1013. doi: 10.1016/j.bjoms.2019.08.020. [DOI] [PubMed] [Google Scholar]
- 8.Osler T.M., Baker S.P.M., Long W.M. A modification of the injury severity score that both improves accuracy and simplifies scoring. J. Trauma Inj. Infect. Crit. Care. 1997;43:922–926. doi: 10.1097/00005373-199712000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Baker S., O′neill B., Haddon W., Long W. The injury severity score: a method for describing patients with multiple injures and evaluating emergency care. Journal of Trauma and Acute Care Surgery. 1974:187–196. [PubMed] [Google Scholar]
- 10.Boyd C.R., Tolson M.A., Copes W.S. Evaluating trauma care: the TRISS method. Trauma score and the injury severity score. J. Trauma. 1987;27:370–378. doi: 10.1097/00005373-198704000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Verlag G.T., Stuttgart′ S., York′issn S., York′issn Y., Maldini B., Skuric J., Visnjic S., Fattorini I. Authors own assessment of TRISS method studies in the treatment of major trauma in children. Eur. J. Pediatr. Surg. 2003;13:260–265. doi: 10.1055/s-2003-42244. [DOI] [PubMed] [Google Scholar]
- 12.Lin C., Wu J., Yang C., Zhang C., Xu B., Zhang Y., Zhang S. Classifying and standardizing panfacial trauma according to anatomic categories and Facial Injury Severity Scale: a 10-year retrospective study. BMC Oral Health. 2021;21 doi: 10.1186/s12903-021-01900-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bagheri S.C., Dierks E.J., Kademani D., Holmgren E., Bryan Bell R., Hommer L., Potter B.E. Application of a facial injury severity scale in craniomaxillofacial trauma. Oral and Maxillofacial Surgeons J Oral Maxillofac Surg. 2006;64:408–414. doi: 10.1016/j.joms.2005.11.013. [DOI] [PubMed] [Google Scholar]
- 14.Domingues C. de A., Coimbra R., Poggetti R.S., Nogueira L. de S., de Sousa R.M.C. New trauma and injury severity score (TRISS) adjustments for survival prediction. World J. Emerg. Surg. 2018;13 doi: 10.1186/s13017-018-0171-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Magee F., Wilson A., Bailey M., Pilcher D., Gabbe B., Bellomo R. Comparison of intensive care and trauma-specific scoring systems in critically ill patients. Injury. 2021;52:2543–2550. doi: 10.1016/j.injury.2021.03.049. [DOI] [PubMed] [Google Scholar]
- 16.Gai Aita T., Luiz C., Stabile P., Dezan Garbelini C., Alex G., Stabile V. American association of oral and maxillofacial surgeons. J. Oral Maxillofac. Surg. 2018;76:1280–1281. doi: 10.1016/j.joms.2018.02.002. [DOI] [PubMed] [Google Scholar]
- 17.Goedecke M., Thiem D.G.E., Schneider D., Frerich B., Kämmerer P.W. Through the ages—aetiological changes in maxillofacial trauma. Dent. Traumatol. 2019;35:115–120. doi: 10.1111/edt.12462. [DOI] [PubMed] [Google Scholar]
- 18.Ilyas N., Green A., Karia R., Sood S., Fan K. Demographics and management of paediatric dental-facial trauma in the ‘lockdown’ period: a UK perspective. Dent. Traumatol. 2021 doi: 10.1111/edt.12667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guo H.Q., Yang X., Wang X.T., Li S., Ji A.P., Bai J. Epidemiology of maxillofacial soft tissue injuries in an oral emergency department in Beijing: a two-year retrospective study. Dent. Traumatol. 2021;37:479–487. doi: 10.1111/edt.12655. [DOI] [PubMed] [Google Scholar]
- 20.Boffano P., Roccia F., Zavattero E., Dediol E., Uglešić V., Kovačič Ž., Vesnaver A., Konstantinović V.S., Petrović M., Stephens J., Kanzaria A., Bhatti N., Holmes S., Pechalova P.F., Bakardjiev A.G., Malanchuk V.A., Kopchak A.v., Galteland P., Mjøen E., Skjelbred P., Koudougou C., Mouallem G., Corre P., Løes S., Lekven N., Laverick S., Gordon P., Tamme T., Akermann S., Karagozoglu K.H., Kommers S.C., Forouzanfar T. European Maxillofacial Trauma (EURMAT) project: a multicentre and prospective study. J. Cranio-Maxillofacial Surg. 2015;43:62–70. doi: 10.1016/j.jcms.2014.10.011. [DOI] [PubMed] [Google Scholar]
- 21.Bilgen F., Ural A., Bekerecioǧlu M. Our treatment approach in pediatric maxillofacial traumas. J. Craniofac. Surg. 2019 doi: 10.1097/SCS.0000000000005896. [DOI] [PubMed] [Google Scholar]
- 22.Hirobe Y., Koshinuma S., Nakamura M., Baba M., Yamamoto G., Hitosugi M. Factors influencing the long-term hospitalization of bicyclists and motorcyclists with oral and maxillofacial injuries. Dent. Traumatol. 2021;37:234–239. doi: 10.1111/edt.12622. [DOI] [PubMed] [Google Scholar]
- 23.Joachim M., Tuizer M., Araidy S., Abu El-Naaj I. Pediatric maxillofacial trauma: epidemiologic study between the years 2012 and 2015 in an Israeli medical center. Dent. Traumatol. 2018;34:221–228. doi: 10.1111/edt.12406. [DOI] [PubMed] [Google Scholar]
- 24.Keskey R.C., Hampton D.A., Biermann H., Cirone J., Zakrison T.L., Cone J.T., Wilson K.L., Slidell M.B. Novel Trauma Composite Score is a more reliable predictor of mortality than Injury Severity Score in pediatric trauma. Journal of Trauma and Acute Care Surgery. 2021;91:599–604. doi: 10.1097/TA.0000000000003235. [DOI] [PubMed] [Google Scholar]
- 25.Reppucci M.L., Acker S.N., Cooper E., Meier M., Stevens J., Phillips R., Moulton S.L., Bensard D.D. Improved identification of severely injured pediatric trauma patients using reverse shock index multiplied by Glasgow Coma Scale. Journal of Trauma and Acute Care Surgery. 2022;92:69–73. doi: 10.1097/ta.0000000000003432. [DOI] [PubMed] [Google Scholar]
- 26.von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. 2022 doi: 10.1016/j.jclinepi.2007.11.008. n.d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.World Health Organization Young people's health-a challenge for society: report of a WHO study group on young people and" health for all by the year 2000. Tecnical Report Series. 1986 [PubMed] [Google Scholar]
- 28.Kelton D., Cavalcante F., Raiane S., Veloso M., Arcia De Almeida Dur∼ Ao M., De V., Melo C., Queiroz De Melo Monteiro G., Porto G.G. Do helmet use and type influence facial trauma occurrence and severity in motorcyclists? A systematic review and metanalysis. J. Oral Maxillofac. Surg. 2021;79:1492–1506. doi: 10.1016/j.joms.2021.02.028. [DOI] [PubMed] [Google Scholar]
- 29.Yazici A., Aytaç I. Pediatric maxillofacial trauma patterns among different types of road traffic accidents. J. Craniofac. Surg. 2019;30:2039. doi: 10.1097/SCS.0000000000005749. –2041. [DOI] [PubMed] [Google Scholar]
- 30.Bregagnolo L.A., Bregagnolo J.C., da Silveira F., Bérgamo A.L., de Santi L.N., Watanabe M.G. de C. Oral and maxillofacial trauma in Brazilian children and adolescents. Braz. Dent. J. 2013;24:397–401. doi: 10.1590/0103-6440201302227. [DOI] [PubMed] [Google Scholar]
- 31.Rêgo I.C.Q., Vilarinho S.M.M., Rodrigues C.K.F., de AR Correia P.V., Junqueira J.L.C., Oliveira L.B. Oral and cranio-maxillofacial trauma in children and adolescents in an emergency setting at a Brazilian hospital. Dent. Traumatol. 2020;36:167–173. doi: 10.1111/edt.12515. [DOI] [PubMed] [Google Scholar]
- 32.Barbosa K.G.N., de Macedo Bernardino Í., d'Avila S., Ferreira E.F.e., Ferreira R.C. Systematic review and meta-analysis to determine the proportion of maxillofacial trauma resulting from different etiologies among children and adolescents. Oral Maxillofac. Surg. 2017;21:131–145. doi: 10.1007/s10006-017-0610-9. [DOI] [PubMed] [Google Scholar]
- 33.Zhou H.H., Lv K., Yang R.T., Li Z., Yang X.W., Li Z.B. Mandibular condylar fractures in children and adolescents: 5-Year retrospective cohort study. Int. J. Pediatr. Otorhinolaryngol. 2019;119:113–117. doi: 10.1016/j.ijporl.2019.01.025. [DOI] [PubMed] [Google Scholar]
- 34.Lin C., Wu J., Yang C., Zhang C., Xu B., Zhang Y., Zhang S. Classifying and standardizing panfacial trauma according to anatomic categories and Facial Injury Severity Scale: a 10-year retrospective study. BMC Oral Health. 2020;21:557. doi: 10.1186/s12903-021-01900-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Alonge O., Agrawal P., Khatlani K., Mashreky S., Emdadul D., Hoque M., Hyder A.A. Developing a systematic approach for Population-based Injury Severity Assessment (PISA): a million-person survey in rural Bangladesh. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2020-042572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hanna S.Y., Ismael W.K., Al-Assaf D. Patterns of pediatric maxillofacial injuries. J. Craniofac. Surg. 2016;27 doi: 10.1097/SCS.0000000000002502. e271–e275. [DOI] [PubMed] [Google Scholar]
- 37.Boyette J.R. Facial fractures in children. Otolaryngol. Clin. 2014;47:747–761. doi: 10.1016/J.OTC.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 38.Chandra S.R., Zemplenyi K.S. Issues in pediatric craniofacial trauma. Facial Plast. Surg. Clin. 2017;25:581–591. doi: 10.1016/J.FSC.2017.06.009. [DOI] [PubMed] [Google Scholar]
- 39.Pullos A.N., Krishnan D.G. Complicated maxillofacial fractures: pediatric and geriatric. Atlas Oral Maxillofac Surg Clin North Am. 2019;27:113–118. doi: 10.1016/j.cxom.2019.05.003. [DOI] [PubMed] [Google Scholar]
- 40.Imahara S.D., Hopper R.A., Wang J., Rivara F.P., Klein M.B. 2008. Patterns and Outcomes of Pediatric Facial Fractures in the United States: A Survey of the National Trauma Data Bank. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mitchell R.J., Cameron C.M., Mcmaugh A., Lystad R.P., Badgery-Parker T., Ryder T. The impact of childhood injury and injury severity on school performance and high school completion in Australia: a matched population-based retrospective cohort study. BMC Pedriatrics. 2021 doi: 10.1186/s12887-021-02891-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cavalcanti A.L., Lino T.H.D.A., de Oliveira T.B.S., de Oliveira T.S.B., Cardoso A.M.R., de Macedo R.F., Padilha W.W.N., Xavier A.F.C. Head and maxillofacial injuries in child and adolescent victims of automotive accidents. Sci. World J. 2014;(2014) doi: 10.1155/2014/632720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hirobe Y., Koshinuma S., Nakamura M., Baba M., Yamamoto G., Hitosugi M. Factors influencing the long-term hospitalization of bicyclists and motorcyclists with oral and maxillofacial injuries. Dent. Traumatol. 2021;37:234–239. doi: 10.1111/EDT.12622. [DOI] [PubMed] [Google Scholar]
- 44.Yuldashev I., Rakhmanov A., Urgunaliev B., Yuldasheva G., Tynaliev U., Kulnazarov A. Frequency of midfacial traumatic injuries - a report from the maxillofacial reconstructive and plastic surgery department of Kyrgyz Republic Health Service Ministry's National Hospital, Bishkek from 2013-17 - a retrospective study. Ann Maxillofac Surg. 2020;10:377. doi: 10.4103/AMS.AMS_2_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Garri J.I., Perlyn C.A., Johnson M.J., Mobley S.R., Shatz D.v., Kirton O.C., Thaller S.R. Patterns of maxillofacial injuries in powered watercraft collisions. Plast. Reconstr. Surg. 1999;104:922–927. doi: 10.1097/00006534-199909020-00005. [DOI] [PubMed] [Google Scholar]
- 46.Reich W., Aust O., Eckert A. Prospective analysis of mid-facial fractures in a single-center pediatric-adolescent cohort. Int. J. Pediatr. Otorhinolaryngol. 2019;119:151–160. doi: 10.1016/j.ijporl.2019.01.028. [DOI] [PubMed] [Google Scholar]
- 47.Yamamoto K., Matsusue Y., Horita S., Murakami K., Sugiura T., Kirita T. Maxillofacial fractures associated with interpersonal violence. J. Craniofac. Surg. 2019;30 doi: 10.1097/SCS.0000000000005306. E312–E315. [DOI] [PubMed] [Google Scholar]
- 48.Roccia F., Sotong J., Savoini M., Ramieri G., Zavattero E. Maxillofacial injuries due to traffic accidents. J. Craniofac. Surg. 2019;30:E288–E293. doi: 10.1097/SCS.0000000000005158. [DOI] [PubMed] [Google Scholar]
- 49.Rodrigues L.G., Barbosa K.G.N., Silva C.J. de P., Alencar G.P., D’avila S., Ferreira E.F.e., Ferreira R.C. Trends of maxillofacial injuries resulting from physical violence in Brazil. Dent. Traumatol. 2020;36:69–75. doi: 10.1111/edt.12509. [DOI] [PubMed] [Google Scholar]