Summary
It is well known that the blood supply of the greater omentum and female internal genital organs are not physiologically connected. There is also no mention of such anatomical variation in anatomical, radiological, or surgical textbooks. Here we present a very rare case report of atypical double arterial anastomosis (the first and second variant artery) between the right limb of the omental arcade of Barkow, uterus, and right ovary, which was found during a routine student anatomical dissection course. It is very challenging to find a proper explanation for the presence of the described anatomical variation; however, we hypothesized that it is based on their common embryonic origin - the mesentery. The first and second variant arteries could be remnants of transient anastomoses or collateral circulation, which were present during embryonic development and persisted until adulthood. Moreover, during our literature review, we noticed that the general description of omental blood supply and its possible variations is relatively poor; therefore, we emphasize the need for more precise knowledge regarding these anatomical parts, which could help surgeons who are performing abdominal or pelvic surgeries in preventing avoidable bleeding.
Keywords: Anatomical vascular variations, Internal female genital organs, Greater omentum, Omental arcade of Barkow, Uterine artery, Ovarian artery
Introduction
At first glance, the vascular supply of the greater omentum, a large peritoneal fold that spreads down from the greater curvature of the stomach, and of the female internal genital organs are unrelated and not connected. The internal female genital organs (ovaries, uterine tubes, and uterus) receive their blood supply from two sources, one of abdominal and one of pelvic origin, namely the ovarian and uterine arteries. The ovarian arteries, derived from the abdominal aorta, descend from the level of the second lumbar vertebra to the brim of the pelvis and pass through the suspensory ligament of the ovary (former infundibulopelvic cord) to enter the mesovarium (a part of the broad ligament of the uterus), by which it reaches the gonad. Within the mesovarium, it anastomoses with the ovarian branch of the uterine artery forming the ovarian arcade, and these two vessels together supply the ovary. The uterine artery is the chief blood supply to the uterus, although the ovarian artery can help to feed it through the anastomosis along the ovary (called the ovarian arcade) between the ovarian artery and the ovarian branch of the uterine artery. The uterine artery arises as a visceral branch from the internal iliac artery, usually from its anterior division (descending segment). It courses within the mesometrium (part of the broad ligament of the uterus) towards the uterine cervix (horizontal segment), where it crosses the ureter ventrally. As the uterine artery approaches the uterine cervix, after emanating the cervicovaginal branch, it turns upward along the uterine margin (ascending segment) and supplies the uterine body and fundus. The uterine artery then turns laterally in the upper border of the broad ligament of the uterus close to the uterine tube to split into an artery of the round ligament of the uterus, a tubal branch, supplying the uterine tube, and an ovarian branch. The ovarian branch of the uterine artery is one of two branches that extend laterally within the broad ligament of the uterus from the uterine horn; the tubal branch remains within the broad ligament proper and mesosalpinx, but the ovarian branch enters the mesovarium to give branches to the ovary [1–4].
Greater omentum comprises two mesothelial sheets which enclose predominantly adipocytes embedded in a loose connective tissue and aggregates of mononuclear phagocytic cells. But the greater omentum contains also large numbers of B- and T-lymphocytes [5]. The right and left gastroomental (gastroepiploic arteries) provide the principal blood supply to the greater omentum; both are branches of the coeliac trunk. The right gastroomental artery is a branch of the gastroduodenal artery, and the left gastroomental artery is a branch of the splenic artery and is thinner than the right one. The right, middle, and left omental arteries are the major arterial branches arising from the gastroomental arch (of Hyrtl). The anterior layer of the greater omentum is the terrain of blood supply coming mainly from the right gastroomental artery and its anterior omental (epiploic) branches (5 to 10); less number of them emanate from the left gastroomental artery. The posterior layer of the greater omentum below the transverse colon, constituting the free part of the omentum, is the terrain supplied by the left gastroomental artery and its left omental branch, which at the lower third of the greater omentum passes from the anterior to the posterior layer to establish the left limb of the omental arcade of Barkow, situated 2 to 4 cm below the transverse colon. The right limb of this arterial arcade is usually formed by the first or the second omental branch, which, after its origin from the right gastroomental artery, passes backward into the posterior layer of the greater omentum. The omental arcade, situated within the posterior layer of the greater omentum, was first described by Barkow in 1793 as the “arcus epiploicus magnus” [6–8].
In most anatomical, radiological or surgical textbooks, only the “normal” (usual/regular) arterial blood supply is described. This “normality,” however, is sometimes found in less than 30 % of all cases for some arteries, but in over 95 % for others [9]. In the present anatomical case study, we describe an unusual vascular anastomosis between the right limb of the omental arcade of Barkow and the female internal organ vessels on the right side. Further, we discussed the possible embryological background of this anatomical anomaly as well as its possible clinical significance.
Anatomical Case Study
A unique vascular variation was encountered during a routine student anatomical dissection course (at the First and Second Faculty of Medicine, Charles University, Prague, Czech Republic) in the cadaver of a female donor. Although her full medical history is not completely known, there were neither marks of surgical intervention inside body cavities nor scars on the skin of the trunk. Except for the usual arterial supply of the abdominal and pelvic organs, there were found two unusual vessels – variant arteries arising from the arterial network of the greater omentum and heading toward the uterus and right ovary (Figs. 1–3). The course of both variant arteries is shown in a schematic diagram (Fig. 4).
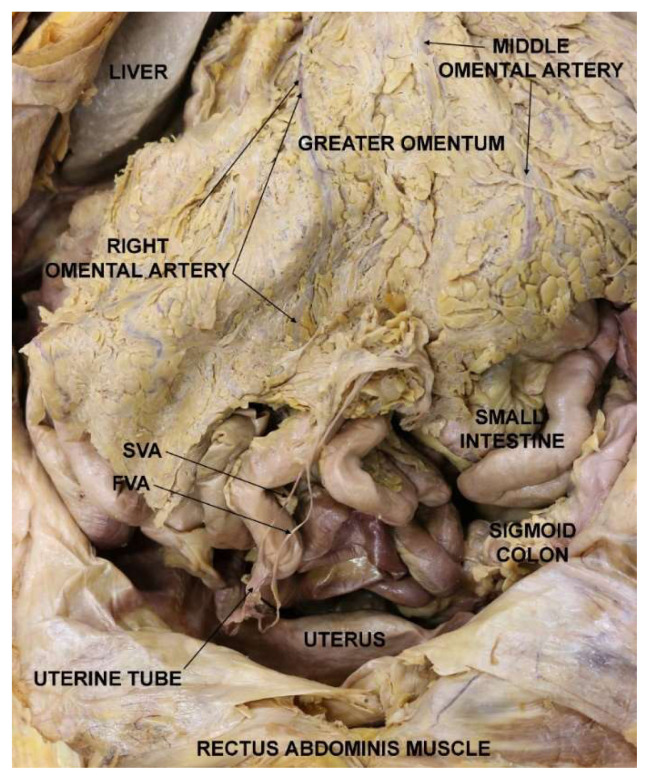
Fig. 1.
Cadaver with opened lower abdominal and upper pelvic cavities showing two variant arteries. Legend: FVA – first variant artery; SVA – second variant artery.
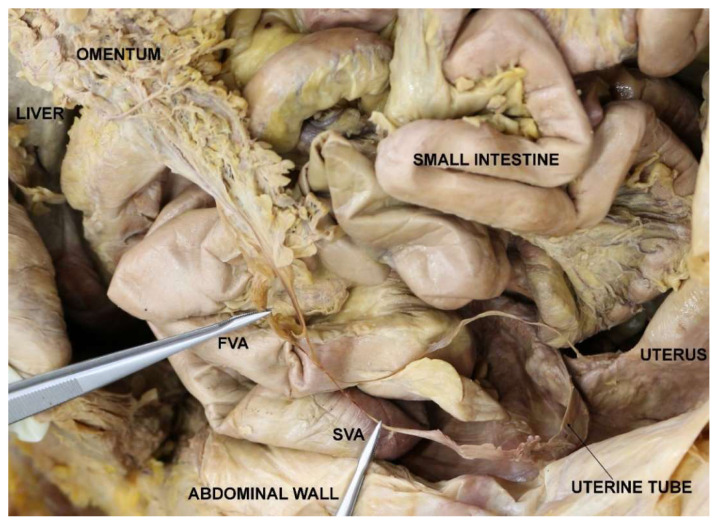
Fig. 2.
Detail of the situation with two variant vessels connecting the greater omentum and uterine tube/uterus. Legend: FVA – first variant artery; SVA – second variant artery.
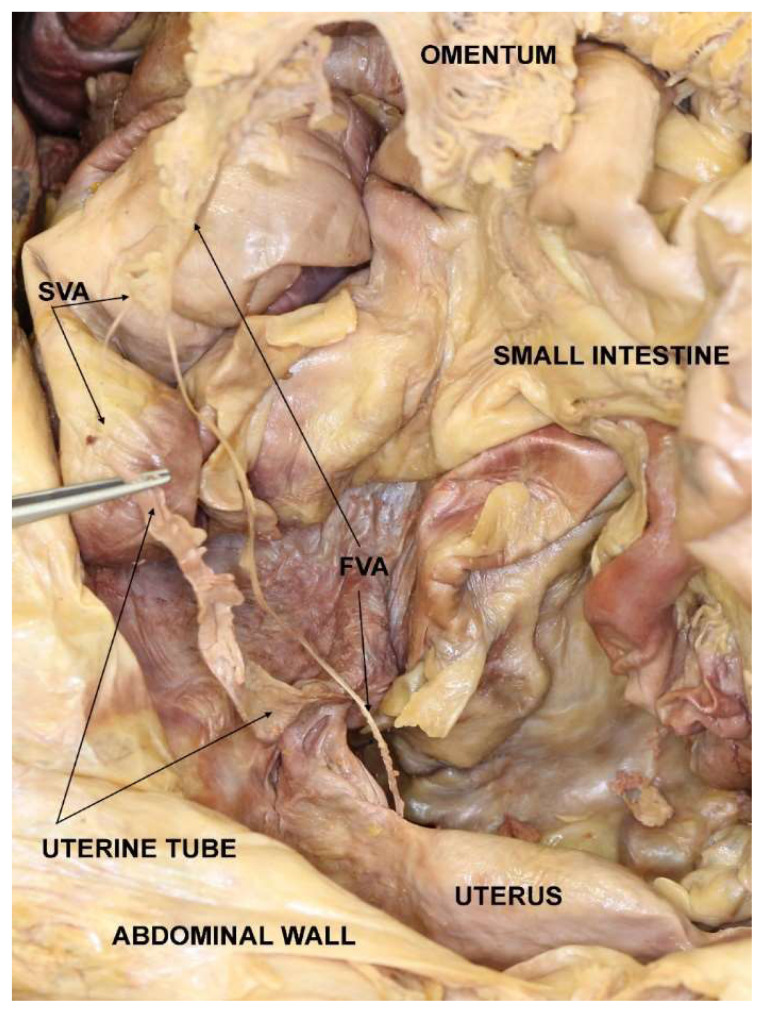
Fig. 3.
Detail of the situation with two variant vessels connecting the greater omentum and uterine tube/uterus. SVA and salpinx in tweezers. Legend: FVA – first variant artery; SVA – second variant artery.
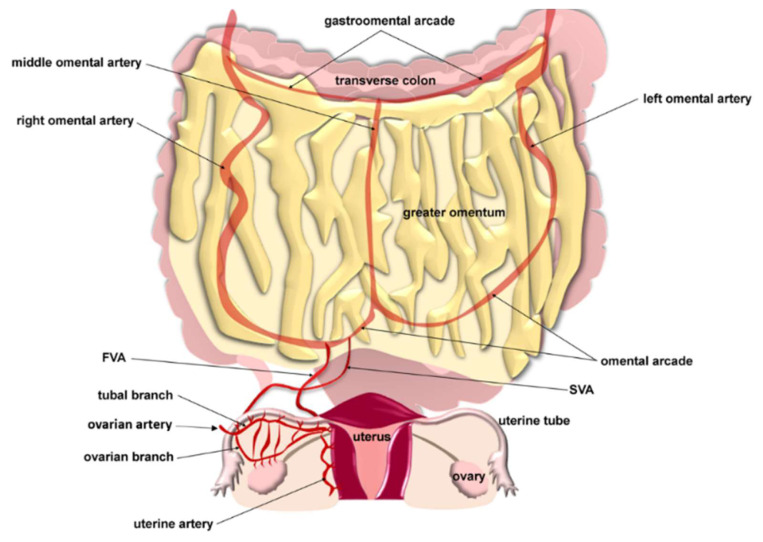
Fig. 4.
Scheme of the anatomical variant vessels connecting the greater omentum and uterine tube/uterus. Legend: FVA – first variant artery; SVA – second variant artery
Both variant arteries arose from the right inferior portion of the greater omentum, closer to the midline, near its caudal margin. The first variant artery (FVA) was 0.8 mm thick and originated more laterally than the second variant artery (SVA), which was 0.5 mm thick. They were branches from the right limb of the omental arcade of Barkow. The distance between their origins was about 1.5 cm. The FVA descended first lateral to the SVA, then after 5 cm, it crossed it ventrally with a very acute angle and continued approximately 13 cm in mediocaudal direction into the lesser pelvis to enter the right uterine margin about 2 cm below the right uterine horn to join the branches of the ascending segment of the uterine artery within the mesometrium (caudal part of the broad ligament of the uterus).
The second variant artery originated medially to the FVA, coursed dorsally to the FVA, and descended caudally approximately 10 cm towards the abdominal opening of the right uterine tube to join the branches of the tubal branch of the uterine artery within the mesosalpinx (cranial part of the broad ligament of the uterus).
Discussion
In this anatomical case study, we describe an unusual double arterial anastomosis between the greater omentum and the female internal genital organs incidentally found during routine anatomical dissection. It is difficult and unclear to explain how such a vascular connection could have arisen. We propose two hypotheses. According to the first one, both variant arteries represent remnants of some transient anastomoses or collateral circulation during the embryonic or fetal period of development. The second, less probable hypothesis, handles an acquired anastomosis after adhesions between omental and broad ligament tissues. But as we have found neither marks of surgical intervention inside body cavities nor scars on the skin of the trunk of the dissected cadaver, the latter hypothesis is highly improbable.
The above-described state of unusual vessel arrangement obviously traces back to the impaired embryological background. Rapid growth occurs during embryonic and fetal development, with anastomoses between arteries disappearing. However, some of these arteries, usually only present for a short period, persist throughout life. Furthermore, some organs as the gonads, wander during their development, and knowledge of their original localization may explain certain anatomical variations or abnormalities [9]. Embryologically, the greater omentum develops from the dorsal mesogastrium that connects the developing stomach to the posterior abdominal wall. The future spleen also develops from the mesenchyme within the dorsal mesogastrium. The rotation of the stomach, the more rapid growth of the greater curvature of the stomach (than of the lesser one), and the massive development of the dorsal mesogastrium and spleen between the sixth and seventh weeks of development cause the movement of the spleen from its original location within the median plane towards the left side of the abdominal cavity. This is very close to the primordia of the gonads and the mesonephric (Wolffian) duct [10]. The developing greater omentum from the 12th week of gestation fuses via connective tissue with the transverse colon, first close to the right colic (hepatic) flexure, second in the area of the spleen, and last in the middle of the transverse colon [8].
The female internal genital organs develop from the intermediate mesoderm, namely ovaries from the genital ridges and uterine tubes and uterus from paramesonephric (Müllerian) ducts. After the regression of mesonephric (Wolffian) ducts in the female embryo, the adjacent dorsal mesentery of these ducts transforms into the mesovarium. The broad ligament of the uterus develops from the urogenital mesentery, which is the peritoneum covering the mesonephroi and genital ridges. The urogenital mesentery is transformed into the broad ligament of the uterus as a result of three processes: fusion of the paramesonephric (Müllerian) ducts caudally, degeneration of the mesonephroi, and descent of the uterine tubes and attached ovaries. As the paramesonephric (Müllerian) ducts “zipper” together, the mesentery sweeps outwards, forming a broad sheet within which the ovaries are suspended. Thus, the broad ligament of the uterus runs from the lateral sides of the fused paramesonephric (Müllerian) ducts to the peritoneum of the pelvic wall [11].
The embryological explanation of the vascular connection of the greater omentum and the organs embedded in the broad ligament of the uterus can be the common embryonic origin of both of these structures – from the mesentery. Although both parts of the mesentery (dorsal mesogastrium and urogenital mesentery) are anatomically distant from each other in the postnatal period, during embryonic development, the primordia of ovaries are localized much more cranially. In addition, it is known that numerous temporary vascular connections are formed during embryonic development (important for collateral flow), which later disappear [12]. This is the basis of the enormous variability of the human vascular system. According to our hypothesis, the described case could be an example of the persistence of such a temporary vascular connection during embryonic/fetal development. However, it must be a very rare finding, as we have not found any similar cases in the scientific literature to the best of our knowledge. Even Settembre et al. [13], who performed systematic dissections of vessels of the greater omentum, did not describe any similar vascular connection with genital organs. Only Kuga et al. [14] present an embryologically similar case concerning the localization of a supernumerary ovary inside the greater omentum. Their hypothesis of origin is based on an aberrant migration of a part of the genital ridge after the incorporation of germ cells.
The blood supply of the greater omentum is rarely dealt with in detail, most textbooks devoting but a few lines to its vascularization. But the omental blood vessels are of fundamental importance, which is obvious from the fact that, in operative procedures on the upper abdominal organs, the greater omentum is subject not only to manipulations but also to manifold resections. Quick, inattentive incisions into gastrocolic, gastrosplenic, splenorenal, gastrophrenic, and phrenicocolic ligaments or the transverse mesocolon may cause sudden massive bleeding. The omental tissue should always be handled with care and understanding for the omental blood vessels, especially those comprising the large omental arcade (of Barkow) situated within the posterior layer of the greater omentum below the transverse colon, which plays an important role in the collateral circulation of the spleen, liver, and stomach when, respectively considered, the splenic, hepatic or one of the arteries along the greater curvature of the stomach becomes occluded [6]. The study of the vasculature of the greater omentum nowadays has a completely new dimension, which concerns the massive development of regenerative and reconstructive surgery. Omental flaps, with their associated rich and pliable vascular arcades, are used in clinical practice for a variety of soft tissue reconstructions or wound healing. Free omental flaps are usually created for head and neck surgery (e.g., in the treatment of tissue deficits in the craniofacial region), in total breast, chest wall, and intrathoracic reconstructions, in reconstructions of visceral organs and the pelvic floor, or in wound healing of upper or lower extremities (e.g., after complex injuries or reconstructions of large arterial ulcers). Well-vascularized omental tissue with unique immune and molecular properties promotes healing and improves function at recipient sites [15–17].
Conclusion
The extremely rare anatomical variant featuring a double connection between the blood supply of the greater omentum and the female internal genital organs not only poses a question of its embryological background but mainly draws attention to emphasize the need for detailed knowledge of anatomy for surgeons, performing large extent of procedures in the lower abdominal and upper pelvic cavity, including ovariectomy, salpingectomy, hysterectomy, resection of the stomach or harvest of the greater omentum. Neglecting anatomical vascular variants could lead to inadvertent bleeding and pointless complications.
Acknowledgements
This study was supported by grant from the Slovak Research and Development Agency, number APVV-18-0499. This publication was also supported from the Operational Program Integrated Infrastructure for the project: Increasing the capacities and competences of the Comenius University in research, development, and innovation 313021BUZ3, co-financed from the resources of the European Regional Development Fund.
The authors of the publication are very grateful to the Professor R. Shane Tubbs (Tulane University School of Medicine, New Orleans, USA) for supply with historical anatomical literature containing a detailed description of anatomical variations.
Footnotes
Conflict of Interest
There is no conflict of interest.
References
- 1.Hollinshead WH. Anatomy for Surgeons. Vol. 2. Thorax, Abdomen and Pelvis. A Hoeber-Harper Book; 1956. [Google Scholar]
- 2.Paulsen F, Waschke J, editors. Sobotta Atlas of Anatomy. 16th Edition. Internal Organs; Elsevier Munich: 2018. [Google Scholar]
- 3.Machado CAG, Neumann PE, Tubbs RS, editors. Classic Regional Approach. 8th Edition. Elsevier; Philadelphia: 2023. Netter Atlas of Human Anatomy. [Google Scholar]
- 4.Drake RL, Vogl AW, Mitchell AWM, Tibbitts RM, Richardson PE. Gray’s Atlas of Anatomy. Third Edition. Elsevier; Philadelphia: 2021. [Google Scholar]
- 5.Platell C, Cooper D, Papadimitriou JM, Hall JC. The omentum. World J Gastroenterol. 2000;6(2):169–176. doi: 10.3748/wjg.v6.i2.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Michels NA. Blood Supply and Anatomy of the Upper Abdominal Organs with a Descriptive Atlas. B. Lippincott Company; Philadelphia and Montreal: 1955. [Google Scholar]
- 7.Topor B, Acland RD, Kolodko V, Galandiuk S. Omental transposition for low pelvic anastomoses. Am J Surg. 2001;182(5):460–464. doi: 10.1016/S0002-9610(01)00764-4. [DOI] [PubMed] [Google Scholar]
- 8.Liebermann-Meffert D The greater omentum. Anatomy, embryology, and surgical applications. Surg Clin North Am. 2000;80(1):275–293. doi: 10.1016/S0039-6109(05)70406-0. [DOI] [PubMed] [Google Scholar]
- 9.Lippert H, Pabst R. In: Arterial variations in man. Classification and Frequency with 540 Drawing in 90 Two-color-plates. Bermann JF, editor. Verlag; München: 1985. [DOI] [Google Scholar]
- 10.Varga I, Babala J, Kachlik D. Anatomic variations of the spleen: current state of terminology, classification, and embryological background. Surg Radiol Anat. 2018;40(1):21–29. doi: 10.1007/s00276-017-1893-0. [DOI] [PubMed] [Google Scholar]
- 11.Miller A, Hong MK, Hutson JM. The broad ligament: a review of its anatomy and development in different species and hormonal environments. Clin Anat. 2004;17(3):244–251. doi: 10.1002/ca.10173. [DOI] [PubMed] [Google Scholar]
- 12.Lin PH, Chaikof EL. Embryology, anatomy, and surgical exposure of the great abdominal vessels. Surg Clin North Am. 2000;80(1):417–433. doi: 10.1016/S0039-6109(05)70413-8. [DOI] [PubMed] [Google Scholar]
- 13.Settembre N, Labrousse M, Magnan PE, Branchereau A, Champsaur P, Bussani R, Braun M, Malikov S. Surgical anatomy of the right gastro-omental artery: a study on 100 cadaver dissections. Surg Radiol Anat. 2018;40(4):415–422. doi: 10.1007/s00276-017-1951-7. [DOI] [PubMed] [Google Scholar]
- 14.Kuga T, Esato K, Takeda K, Sase M, Hoshii Y. A supernumerary ovary of the omentum with cystic change: report of two cases and review of the literature. Pathol Int. 1999;49(6):566–570. doi: 10.1046/j.1440-1827.1999.00882.x. [DOI] [PubMed] [Google Scholar]
- 15.Mazzaferro D, Song P, Massand S, Mirmanesh M, Jaiswal R, Pu LLQ. The omental free flap - a review of usage and physiology. J Reconstr Microsurg. 2018;34(3):151–169. doi: 10.1055/s-0037-1608008. [DOI] [PubMed] [Google Scholar]
- 16.Claro F, Jr, Sarian LO, Pinto-Neto AM. Omentum for mammary disorders: a 30-year systematic review. Ann Surg Oncol. 2015;22(8):2540–2550. doi: 10.1245/s10434-014-4328-8. [DOI] [PubMed] [Google Scholar]
- 17.Cancelli G, Zghari TA, Dimagli A, Audisio K, Dabsha A, Harik L, Olaria RP, Soletti GJ, Demetres M, Gaudino M. Mortality after sternal reconstruction with pectoralis major flap vs omental flap for postsurgical mediastinitis: A systematic review and meta-analysis. J Card Surg. 2022;37:1311–1316. doi: 10.1111/jocs.17189. [DOI] [PubMed] [Google Scholar]