Abstract
Background and objectives
Frozen shoulder (FS) is characterized by pain and significant loss of active and passive shoulder motion. Strengthening exercises are among the standard exercises used for FS. Neuromuscular exercise (NME) effectively improved pain and the range of motion in shoulder. However, no prior research has looked into the effects of NME compared to strengthening exercises in FS rehabilitation. The aim of the present study was to evaluate the effects of NME compared to strengthening exercises on pain and active range of motion (AROM) in individuals with idiopathic frozen shoulder.
Methods
Forty individuals with idiopathic frozen shoulder were randomly assigned to either the experimental group (NME with regular physical therapy, n = 20) or the control group (strengthening exercises with regular physical therapy, n = 20). In both groups, the interventions were performed once a day, 5 days a week for 8 weeks. Pain scores on the visual analogue scale (VAS) and AROM of the shoulder were assessed at baseline and after the 8-week treatment. The primary analysis was the group × time interaction.
Results
Two-by-two mixed analysis of variance (ANOVA) revealed a significant group × time interaction for VAS (F = 29.67; p < 0.01); AROM in flexion (F = 12.05; p < 0.01), internal rotation (F = 6.62; p < 0.05) and external rotation (F = 16.93; p < 0.01) in favor of the experimental group. The two-by-two mixed ANOVA revealed a significant main effect of time for VAS (F = 1648.47; p < 0.01); AROM in flexion (F = 591.70; p < 0.01), extension (F = 114.57; p < 0.01), abduction (F = 1602.04; p < 0.01), internal rotation (F = 664.14; p < 0.01) and external rotation (F = 1096.92; p < 0.01). No other significant differences were found.
Conclusions
NME is superior to strengthening exercises in terms of pain and AROM of shoulder flexion, internal rotation and external rotation in individuals with idiopathic FS. NME could be used to treat individuals with FS.
Trial registration
Trial registration number: ChiCTR2100054453. Registration date: 17/12/2021.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12891-023-06173-8.
Keywords: Neuromuscular exercise, Maitland technique, Idiopathic frozen shoulder, Regular physical therapy, Rehabilitation
Introduction
Frozen shoulder (FS) or adhesive capsulitis is an unknown intrinsic disease associated with spontaneously progressive inflammation and fibrosis of the shoulder joint capsule, characterised by pain and significant loss of active and passive shoulder motion [1]. Frozen shoulder (FS) or adhesive capsulitis is an unknown intrinsic disease associated with spontaneously progressive inflammation and fibrosis of the shoulder joint capsule, characterised by pain and significant loss of active and passive shoulder motion [2]. The prevalence rate is 2–5%, affecting more women than men aged 40–60 years, and the incidence rate increases with age [3–5]. The clinical presentation of FS is described in three overlapping stages. The freezing stage is associated with pain that is typically worst at night and can last from weeks to 9 months. The frozen stage is characterized by progressive loss of range of motion and marked stiffness with gradual reduction in pain and can last from 9 to 15 months. In the thawing stage, the pain and stiffness gradually subside, but significant stiffness persists for 15 to 24 months [6, 7]. Pain and limitation of movement are the most common complaints affecting shoulder function in activities of daily living and quality of life [4, 8, 9]. Apart from surgery, conservative treatments are common for FS and include individual education, oral or intra-articular glucocorticoids, physiotherapy and exercise programmes [10–12]. Strengthening exercises are among the standard exercises used for FS [13–15].
Sensory and proprioceptive input may be reduced if the shoulder cannot be moved due to pain in FS [16, 17]. And proprioception plays an important role in sensorimotor control, especially in the shoulder complex, which depends significantly on joint stability during movement [18]. Stabilisation must be offered to allow smooth movement of the distal joints. Neuromuscular control is crucial for maintaining dynamic stabilisation [19]. Neuromuscular exercise (NME) involves motor control, (re) learning and proprioceptive training that addresses the quality of movement and emphasises joint control [20]. It is increasingly used to facilitate faster recovery in individuals with shoulder dysfunction with shoulder pain and impaired proprioceptive function such as traumatic anterior shoulder dislocation [21, 22], It is increasingly used to facilitate faster recovery in individuals with shoulder dysfunction with shoulder pain and impaired proprioceptive function such as traumatic anterior shoulder dislocation [23] and rotator cuff tendinopathy [24].
As for comparing the effects of NME and strengthening exercises for the shoulder, Eshoj et al. [21] showed that NME improved shoulder pain and function more than strengthening exercises in individuals with traumatic anterior dislocation. Gin et al. [25] showed that NME is as effective as strengthening exercises in treating chronic shoulder pain. Ageberg et al. [26] showed that NME was as effective as strengthening exercises in degenerative knee disease. Risberg et al. [27] demonstrated that NME significantly improved pain and knee function compared to strengthening exercises at the 6-month follow-up after anterior cruciate ligament reconstruction. As far as we know, no study has looked at the effects of NME compared to strengthening exercises in the rehabilitation of FS.
Therefore, the aim of the current study was to compare the effects of NME and strengthening exercises at FS. We hypothesised that NME may improve the symptoms of FS better than strengthening exercises.
Materials and methods
Study design
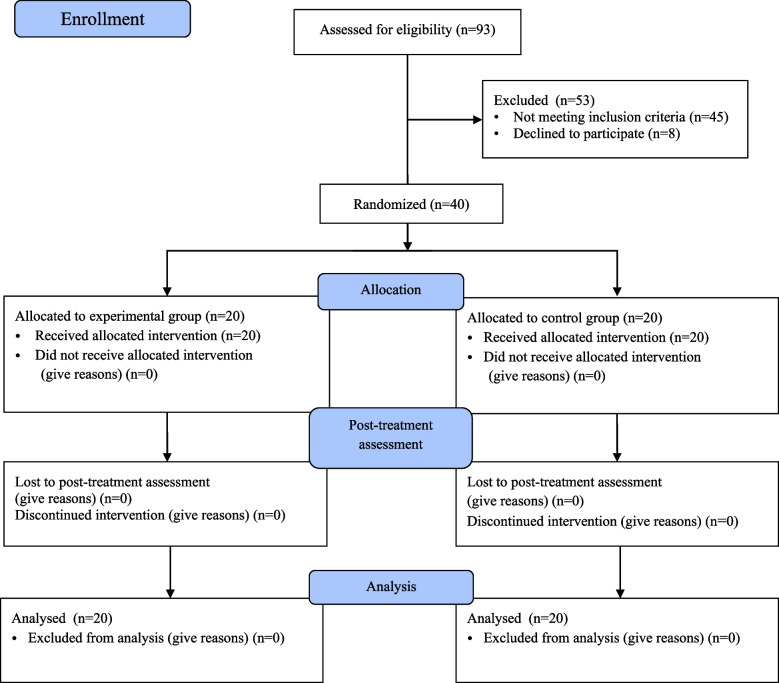
This was a single-blinded, randomised controlled trial conducted in the rehabilitation medicine department of a regional hospital. Forty participants were recruited from December 2021 to May 2022. They were randomly assigned to either NME plus regular physical therapy (experimental group) or regular physical therapy with strengthening exercises (control group). Assessment was performed at baseline and 8 weeks after the intervention (Fig. 1). This study was conducted in accordance with the Declaration of Helsinki. All individuals were informed about the study and signed an informed consent form before the study. And this study was approved by the ethics committee of the regional hospital and registered with ChiCTR.org.cn (www.chictr.org.cn, 17/12/2021, ChiCTR2100054453).
Fig. 1.
CONSORT flow diagram
Randomization and blinding
Eligible participants were randomly assigned to the experimental or control group by a blinded investigator using computer-generated random numbers through concealed opaque envelopes. An independent blinded therapist assessed participants and collected data at baseline and 8 weeks after treatment. After the baseline examination, another blinded therapist opened the envelope and started the therapy according to the group assignment.
Participants
Forty participants who have been diagnosed with idiopathic frozen shoulder were recruited from a regional hospital for this study. The inclusion criteria include: (1) FS (adhesive capsulitis) diagnosed at the freezing or frozen stage. (2) symptoms such as shoulder pain, stiffness and joint mobility limitations (limited range of motion of the shoulder in abduction, flexion, extension, internal or external rotation). (3) age over 40 years. (4) unilateral idiopathic FS [28]. Exclusion criteria include: (1) shoulder trauma (rotator cuff injury, etc.). (2) co-occurrence of other neurological or mental disorders (severe cardiac, pulmonary or renal dysfunction, etc.). (3) a previous shoulder surgery. (4) in additional treatments and medications. (5) contraindications to joint mobilization (e.g. osteoporosis). (6) rheumatic diseases (e.g. rheumatoid arthritis). (7) in connection with systemic diseases such as diabetes mellitus and thyroid diseases [29, 30]. Restriction of passive external rotation in the affected shoulder by less than 50% compared to the opposite shoulder was not considered excluded in this study [7].
Interventions
Participants in both the experimental group (EG) and the control group (CG) performed a 5-minute warm-up exercise in the form of wall climbing at the beginning and received 40 minutes of regular physical therapy. Participants from CG performed 20 minutes of strengthening exercises. Participants in EG performed NME for 20 minutes.
Regular physical therapy
Regular physical therapy included Maitland mobilization techniques, stretching exercises and active range of motion exercises [15]. Maitland mobilization techniques [30, 31] consisted of distraction of the glenohumeral joint, glenohumeral caudal gliding movements, glenohumeral posterior-anterior gliding movements and glenohumeral anterior-posterior gliding movements. The oscillatory movements were performed with 2–3 gliding movements/second, 30 seconds/set and 5 sets for each gliding movement. The degree of Maitland mobilization depended on the stiffness and pain tolerance of the individual. Shoulder stretching exercises [15] were performed in a standing position using a wand for flexion, extension, abduction, internal rotation and external rotation. Ten seconds/set, 20 sets for each direction. Five seconds rest between two sets. AROM exercises [15] were performed in a standing position for flexion, extension and abduction and in a lying position for internal rotation and external rotation. Ten repetitions/set, 3 sets for each direction. Five seconds rest between two sets.
Strengthening exercises
Strengthening exercises included isometric and isotonic exercises. Theraband isometric exercises and 1–2-kg dumbbells isotonic exercises were performed for flexion, extension, abduction, internal rotation and external rotation in a standing and lying position. Ten seconds/set, 10 sets for each direction for isometric exercises. 10 repetitions/set, 3 sets for each direction for isotonic exercises. 5 seconds rest between two sets [13].
NME
NME used the HUBER360a in this study, integrating strength, coordination, balance and proprioception exercise [21]. The device provides a multi-axis motorized rotating platform, which can capture a variety of different speeds, amplitude, acceleration trajectory, and real-time monitoring of the individual’s body center of gravity, and provide visual feedback [32]. Individuals tried their best to keep the center of gravity within the target zone through the visual feedback on the screen by holding the elastic belt tied to the armrest when standing on the swaying platform. A stop bottom was controlled by a therapist in case of an emergency. The NME includes six exercises (for the left shoulder, as an example): holding the elastic belt with the shoulder in (1) external rotation (Fig. 2); (2) internal rotation; (3) abduction 90° and external rotation (Fig. 3); (4) abduction 90° and internal rotation; (5) flexion 90° and external rotation (Fig. 4); and (6) flexion 90° and internal rotation (10 seconds of training with 10 seconds rest/repetition × 8 repetitions). There is a one-minute interval for changing directions. Each exercise includes five levels. A score would be shown on the screen according to the exercise performance of the individuals after each session of exercise. If the score was more than 90 points (full score of 100 points), the exercise would go to the next level with higher speed, acceleration, and amplitude of the platform. All treatments are performed and supervised by the same professional, experienced physiotherapist in a quiet environment (once a day, 5 days per week for 8 weeks).
Fig. 2.

NME for the left shoulder in external rotation
Fig. 3.

NME for the left shoulder in abduction 90° and external rotation
Fig. 4.

NME for the left shoulder in flexion 90° and external rotation
Outcome assessments
After the treatment and at the beginning of the study, all outcomes were assessed. The same experienced therapist collected data on basic demographic factors such as age, gender, duration of symptoms, stage, affected side and clinical outcomes such as pain and active range of motion (AROM).
Pain intensity was assessed using the visual analogue scale (VAS), which ranks pain from 0 (no pain) to 10 (most severe pain) and has good reliability with an intraclass correlation coefficient (ICC) of 0.71–0.99. The standard error of measurement (SEM) of VAS was 0.03 and the minimum detectable change (MDC) was 0.08 [33, 34].
The shoulder active range of motion (AROM) including flexion (FL), extension (EX), abduction (AB), external rotation (ER), and internal rotation (IR) was measured with a two-arm standard goniometer with a good reliability (ICC 0.91 to 0.99) [35]. The MDC was 6° to 11° and the SEM was 2.4° to 17.1° [36, 37].
For each movement, three measurements were recorded, and the mean was used for statistical analysis. In the standing posture, shoulder flexion and abduction were assessed. In the prone position, shoulder extension was measured with the elbow flexed to 90°. In the prone position, shoulder internal rotation was measured with the shoulder abducted to 90° and the elbow flexed to 90°. Finally, in the supine position, the external rotation of the shoulder was measured with the shoulder abducted to 90° and the elbow flexed to 90° [38].
Sample size calculation
The sample size calculation was based on the time-by-group interaction of a two-by-two mixed analysis of variance (ANOVA). The effect size was estimated to be 0.25 with 80% power and an α-value of 0.05. G*Power v.3.1.9.2 was used for this calculation. The estimated required sample size was 17 individuals per group. Considering the potential for loss, we aimed to recruit 20 participants per group.
Statistical analysis
All statistical analyses were performed using SPSS version 19.0b. The Kolmogorov-Smirnov test was performed to assess the normal distribution of the data. Continuous variables were presented as means with SDs for normal distribution or median (95% CI) for abnormal distribution. Independent t-tests or Mann-Whitney U test were used to compare demographic data such as age, duration and stage between the two groups. The chi-square test was used to compare differences in gender and affected side between the two groups. Comparisons of VAS and AROM between the experimental and control groups were performed using two-by-two mixed ANOVA with time (pre-intervention and post-intervention) as within-subjects factor and group (NME and control) as between-subjects factor, and effect sizes (η2) were calculated. The main hypothesis of interest was the group × time interaction. Statistical significance was set at 0.05.
Results
Forty participants (21 males and 19 females) with an average age of 54.23 ± 5.51 years who were diagnosed with idiopathic frozen shoulder were recruited from a regional hospital from December 2021 to May 2022. They were randomly assigned to the experimental or control group and completed the study without adverse effects. The data for age, duration, VAS score and all AROM were normally distributed, the data for stage was not normally distributed. At baseline, there were no differences in demographics between groups as seen in Table 1. The two-by-two mixed ANOVA revealed a significant group-by-time interaction for VAS (F = 29.67; p < 0.01; η2 = 0.438); AROM in FL (F = 12.05; p < 0.01; η2 = 0.241), IR (F = 6.62; p < 0.05; η2 = 0.148), ER (F = 16.93; p < 0.01; η2 = 0.308). There was a non-significant time-by-group interaction for AB (p = 0.05) and EX (p > 0.05). The two-by-two mixed ANOVA revealed a significant main effect of time for VAS (F = 1648.47; p < 0.01; η2 = 0.977); AROM in FL (F = 591.70; p < 0.01; η2 = 0.940), EX (F = 114.57; p < 0.01; η2 = 0.751), AB (F = 1602.04; p < 0.01; η2 = 0.977), IR (F = 664.14; p < 0.01; η2 = 0.946) and ER (F = 1096.92; p < 0.01; η2 = 0.967). There was a non-significant main effect of the group for VAS and all AROM as seen in Table 2.
Table 1.
Demographic characteristics
| Characteristics | Experimental group | Control group | P |
|---|---|---|---|
| (EG) n = 20 | (CG) n = 20 | ||
| Age, years | 53.60 ± 5.18 | 54.85 ± 5.89 | 0.480 |
| Gender,male/female | 12/8 | 9/11 | 0.342 |
| Duration, months | 2.79 ± 1.05 | 3.13 ± 1.07 | 0.310 |
| Stage | 1.30 (1.08–1.52) | 1.15 (0.98–1.32) | 0.262 |
| Affected side, R/L | 13/7 | 15/5 | 0.490 |
n number, R Right, L Left
Table 2.
Comparison of VAS and AROM
| Experimental Group | Control Group | P | η2 | |||
|---|---|---|---|---|---|---|
| Pre-intervention | Post-intervention | Pre-intervention | Post-intervention | |||
| Pain on VAS | 7.05 ± 1.57 | 2.40 ± 1.43 | 6.95 ± 1.32 | 3.40 ± 1.50 | < 0.01 | 0.438 |
| AROM of FL | 92.10 ± 25.00 | 149.75 ± 21.42 | 89.60 ± 27.42 | 132.85 ± 21.31 | 0.001 | 0.241 |
| AROM of EX | 31.15 ± 7.29 | 42.05 ± 2.54 | 32.45 ± 7.98 | 41.00 ± 4.01 | 0.204 | 0.042 |
| AROM of AB | 93.80 ± 12.59 | 156.65 ± 14.62 | 89.15 ± 11.05 | 145.95 ± 15.46 | 0.05 | 0.097 |
| AROM of ER | 22.80 ± 6.61 | 72.80 ± 14.34 | 23.90 ± 8.96 | 62.85 ± 15.05 | < 0.01 | 0.308 |
| AROM of IR | 31.65 ± 9.35 | 69.10 ± 13.93 | 29.40 ± 9.02 | 60.05 ± 17.43 | 0.014 | 0.148 |
Discussion
This study aims to investigate the effects of NME compared to strengthening exercises on pain intensity and AROM in individuals with FS. Significant improvements in VAS, AROM of flexion, internal rotation, and external rotation in the experimental group have been observed in this study.
Evaluation of the effect of neuromuscular exercise on pain
The results show that pain intensity improved significantly in individuals with FS after an intervention of 40 sessions of NME plus regular physical therapy. These results are consistent with the results of other studies [21, 23, 24] indicating that shoulder pain can be alleviated after NME. Eshoj et al. [21] demonstrated that NME was superior to standard exercises in terms of pain reduction in individuals with anterior shoulder dislocation. Juul-Kristensen et al. [23] proved that shoulder NME was an effective pain treatment in individuals with subacromial pain syndrome. Ager et al. [24] reported a positive effect of upper extremity NME on pain in rotator cuff tendinopathy. Ginn et al. [25] demonstrated that exercises to restore neuromuscular control were as effective as corticosteroid injections in treating shoulder pain in the short term. In addition to the shoulder, NME has a significant therapeutic effect on many other musculoskeletal pain conditions, such as low back pain [39, 40], neck pain [41], chronic musculoskeletal pain in the elderly [42], chronic pain after primary total knee arthroplasty [43], and knee and hip osteoarthritis [44, 45]. NME includes active exercises of strength, coordination, balance, and proprioception. Multimodal active exercises have been proposed for affected individuals to participate in, which may contribute to pain management by activating endogenous pain-inhibitory mechanisms and reducing sensitivity to noxious stimuli, which has been termed “exercise-induced hypoalgesia” [46–48]. Individuals with FS can be prescribed NME as a pain reliever.
Evaluation of the effect of neuromuscular exercise on AROM
A significant difference was found in the AROM of flexion, internal rotation, and external rotation between the group with NME plus regular physical therapy and the group with regular physical therapy plus strengthening exercises. Shoulder AROM improved after 5 weeks of neuromuscular control exercises in subjects with chronic shoulder pain, as reported by Ginn et al. [25]. Fernandez et al. [49] showed that neuromuscular warm-up exercises in young tennis players resulted in significant improvement in internal and external rotation of the shoulder passive range of motion (PROM). The ability to produce regulated movements through coordinated muscle activity is referred to as neuromuscular control. NME has effects on muscle activation patterns and biomechanics of the surrounding joint musculature [50]. The strength and coordination of muscle exercises involved in NME may be the reason for the increase in AROM, as the shoulder complex relies on muscles to provide dynamic stability and flexibility for AROM [51]. However, evidence for NME is lacking at ROM in FS, and no previous study was found. RCTs of sufficiently good quality are needed to investigate NME in individuals with FS.
Limitations of the study
First, the sample size in this study was relatively small. Second, it is unclear whether the frequency, intensity, and duration of NME by the motorized device were the best in this study, and there is no previous study to compare it with. Third, only the VAS score and AROM of the shoulder were measured in this study, and no disability questionnaires were reported. Finally, no long-term effect of NME was observed at FS. Therefore, further studies with a larger sample and different frequencies, intensities, and durations on long-term and functional effects are desirable.
Conclusions
This study shows that NME performed with a motorized device in combination with regular physical therapy in the form of joint mobilization, stretching, and AROM at FS is more effective for pain relief and improvement of AROM compared with regular physical therapy with strengthening exercises. Considering the positive effects on FS, it is recommended that NME could be used in the treatment of individuals with FS. However, the long-term and functional effects of NME on frozen shoulder need to be investigated in future large-scale studies.
Suppliers
Huber360 MD; LPG Systems.
SPSS; IBM Corp.
Supplementary Information
Acknowledgements
We would like to thank every individual who participated in this study.
Abbreviations
- FS
Frozen Shoulder
- NME
Neuromuscular Exercise
- RCT
Randomized Controlled Trial
- ROM
Range of Motion
- PROM
Passive Range of Motion
- AROM
Active Range of Motion
- EG
Experimental Group
- CG
Control Group
- VAS
Visual Analogue Scale
- SEM
Standard error of measurement
- MDC
Minimal detectable change
- Fl
Flexion
- EX
Extension
- AB
Abduction
- ER
External Rotation
- IR
Internal Rotation
- ANOVA
Analysis of variance
Authors’ contributions
L.W. and Y.C. designed the research study. L.W. participated in the data collection/analysis and writing of the manuscript. G.Y., R.Z., G.W., L.H. participated in the data collection and analysis. Y.C. provided experimental guidance during the study and revised the paper critically. All authors read and approved the final manuscript.
Funding
The study did not receive any specific funding from funding agencies in the public, commercial or non-profit sectors.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was performed in accordance with the Declaration of Helsinki. All individuals were informed about the study and signed an informed consent before the study. And this study was approved by the ethics committee of Beijing Tongren Hospital Capital Medical University and registered with ChiCTR.org.cn (ChiCTR2100054453).
Consent for publication
The individual images and evaluation data involved in the paper were published with the informed consent of the individuals.
Competing interests
All authors declare that they have no potential conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Carmignano SM. Frozen shoulder: symptoms, causes, diagnosis, and treatment. In: Dimitrios, DN, George, KS, editors. Shoulder surgery for RC pathology, arthropathy and tumors. Rijeka: IntechOpen; 2022. p. Ch. 3.
- 2.Tamai K, Akutsu M, Yano Y. Primary frozen shoulder: brief review of pathology and imaging abnormalities. J Orthop Sci. 2014;19:1–5. doi: 10.1007/s00776-013-0495-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sarasua SM, Floyd S, Bridges WC, Pill SG. The epidemiology and etiology of adhesive capsulitis in the U.S. medicare population. BMC Musculoskelet Disord. 2021;22:828. doi: 10.1186/s12891-021-04704-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De la Serna D, Navarro-Ledesma S, Alayón F, López E, Pruimboom L. A comprehensive view of frozen shoulder: a mystery syndrome. Front Media. 2021;8:663703. doi: 10.3389/fmed.2021.663703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ramirez J. Adhesive capsulitis: diagnosis and management. Am Fam Physician. 2019;99:297–300. [PubMed] [Google Scholar]
- 6.Dias R, Cutts S, Massoud S. Frozen shoulder. BMJ. 2005;331:1453–1456. doi: 10.1136/bmj.331.7530.1453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kelley MJ, Shaffer MA, Kuhn JE, Michener LA, Seitz AL, Uhl TL, et al. Shoulder pain and mobility deficits: adhesive capsulitis. J Orthop Sports Phys Ther. 2013;43(5):A1–31. doi: 10.2519/jospt.2013.0302. [DOI] [PubMed] [Google Scholar]
- 8.Toprak M, Erden M. Sleep quality, pain, anxiety, depression and quality of life in patients with frozen shoulder. J Back Musculoskelet Rehabil. 2019;32(2):287–291. doi: 10.3233/BMR-171010. [DOI] [PubMed] [Google Scholar]
- 9.Fernandes MR. Correlation between functional disability and quality of life in patients with adhesive capsulitis. Acta Ortop Bras. 2015;23:81–84. doi: 10.1590/1413-78522015230200791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoffmeister E. Review compares treatments for frozen shoulder. Topics Pain Manag. 2022;37(6):1–4. doi: 10.1097/01.TPM.0000805652.58395.5c. [DOI] [Google Scholar]
- 11.Rex SS, Kottam L, McDaid C, Brealey S, Dias J, Hewitt CE, et al. Effectiveness of interventions for the management of primary frozen shoulder: a systematic review of randomized trials. Bone Jt Open. 2021;2(9):773–784. doi: 10.1302/2633-1462.29.BJO-2021-0060.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Minns Lowe C, Barratt E, McCreesh K, De Burca N, Lewis J. Clinical effectiveness of non-surgical interventions for primary frozen shoulder: a systematic review. J Rehabil Med. 2019;51:539–556. doi: 10.2340/16501977-2578. [DOI] [PubMed] [Google Scholar]
- 13.Rawat P, Eapen C, Seema KP. Effect of rotator cuff strengthening as an adjunct to standard care in subjects with adhesive capsulitis: a randomized controlled trial. J Hand Ther. 2017;30(3):235–41.e8. doi: 10.1016/j.jht.2016.10.007. [DOI] [PubMed] [Google Scholar]
- 14.Abd Elhamed HB, Koura GM, Hamada HA, Mohamed YE, Abbas R. Effect of strengthening lower trapezius muscle on scapular tipping in patients with diabetic frozen shoulder: a randomized controlled study. Biomed Res. 2018;29(3):442–447. doi: 10.4066/biomedicalresearch.29-17-2367. [DOI] [Google Scholar]
- 15.Chan HBY, Pua PY, How CH. Physical therapy in the management of frozen shoulder. Singap Med J. 2017;58(12):685–689. doi: 10.11622/smedj.2017107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Breckenridge JD, McAuley JH, Ginn KA. Motor imagery performance and tactile spatial acuity: are they altered in people with frozen shoulder? Int J Environ Res Public Health. 2020;17(20):7464. doi: 10.3390/ijerph17207464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fabis J, Rzepka R, Fabis A, Zwierzchowski J, Kubiak G, Stanula A, et al. Shoulder proprioception – lessons we learned from idiopathic frozen shoulder. BMC Musculoskelet Disord. 2016;17(1):123. doi: 10.1186/s12891-016-0971-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ager AL, Borms D, Deschepper L, Dhooghe R, Dijkhuis J, Roy JS, et al. Proprioception: how is it affected by shoulder pain? A systematic review. J Hand Ther. 2020;33(4):507–516. doi: 10.1016/j.jht.2019.06.002. [DOI] [PubMed] [Google Scholar]
- 19.Duzgun I, Turhan E. Proprioception after shoulder injury, surgery, and rehabilitation. Proprioception in Orthopaedics, sports medicine and rehabilitation. Springer; 2018. pp. 35–45. [Google Scholar]
- 20.Ageberg E, Link A, Roos EM. Feasibility of neuromuscular training in patients with severe hip or knee OA: the individualized goal-based NEMEX-TJR training program. BMC Musculoskelet Disord. 2010;11(1):126. doi: 10.1186/1471-2474-11-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eshoj HR, Rasmussen S, Frich LH, Hvass I, Christensen R, Boyle E, et al. Neuromuscular exercises improve shoulder function more than standard care exercises in patients with a traumatic anterior shoulder dislocation: a randomized controlled trial. Orthop J Sports Med. 2020;8(1):2325967119896102. doi: 10.1177/2325967119896102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eshoj H, Rasmussen S, Frich LH, Hvass I, Christensen R, Jensen SL, et al. A neuromuscular exercise programme versus standard care for patients with traumatic anterior shoulder instability: study protocol for a randomised controlled trial (the SINEX study) Trials. 2017;18(1):90. doi: 10.1186/s13063-017-1830-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Juul-Kristensen B, Larsen CM, Eshoj H, Clemmensen T, Hansen A, Bo Jensen P, et al. Positive effects of neuromuscular shoulder exercises with or without EMG-biofeedback, on pain and function in participants with subacromial pain syndrome - a randomised controlled trial. J Electromyogr Kinesiol. 2019;48:161–168. doi: 10.1016/j.jelekin.2019.07.009. [DOI] [PubMed] [Google Scholar]
- 24.Ager AL, Roy JS, Gamache F, Hébert LJ. The effectiveness of an upper extremity neuromuscular training program on the shoulder function of military members with a rotator cuff tendinopathy: a pilot randomized controlled trial. Mil Med. 2019;184(5–6):e385–ee93. doi: 10.1093/milmed/usy294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ginn K, Cohen M. Exercise therapy for shoulder pain aimed at restoring neuromuscular control: a randomized comparative clinical trial. J Rehabil Med. 2005;37(2):115–122. doi: 10.1080/16501970410023443. [DOI] [PubMed] [Google Scholar]
- 26.Ageberg E, Roos EM. Neuromuscular exercise as treatment of degenerative knee disease. Exerc Sport Sci Rev. 2015;43(1):14–22. doi: 10.1249/JES.0000000000000030. [DOI] [PubMed] [Google Scholar]
- 27.Risberg MA, Holm I, Myklebust G, Engebretsen L. Neuromuscular training versus strength training during first 6 months after anterior cruciate ligament reconstruction: a randomized clinical trial. Phys Ther. 2007;87(6):737–750. doi: 10.2522/ptj.20060041. [DOI] [PubMed] [Google Scholar]
- 28.Rangan A, Hanchard N, McDaid C. What is the most effective treatment for frozen shoulder? BMJ. 2016;354:i4162. [DOI] [PubMed]
- 29.Sathe S, Khurana SK, Damke U, Agrawal PV. To compare the effects of maitland mobilization with conventional physiotherapy in adhesive capsulitis. Int J Cur Res Rev Vol. 2020;12(14):99–102.
- 30.Zahoor M, Ali B, Khan A, Zeb GS, Sumayyah E, Qamar G. Effectiveness of Maitland manual therapy technique in management of idiopathic adhesive capsulitis. Ann Allied Health Sci. 2021;7(1):3–7. [Google Scholar]
- 31.Jivani RR, Hingarajia DN. Effect of spencer muscle energy technique versus maitland’s mobilization technique on pain, rom and disability in patients with frozen shoulder: a comparative study. Int J Physiother Res. 2021;9(4):3928–3936. doi: 10.16965/ijpr.2021.148. [DOI] [Google Scholar]
- 32.Couillandre A, Duque Ribeiro MJ, Thoumie P, Portero P. Changes in balance and strength parameters induced by training on a motorised rotating platform: a study on healthy subjects. Ann Readapt Med Phys. 2008;51(2):59–73. doi: 10.1016/j.annrmp.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 33.Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: visual analog scale for pain (VAS pain), numeric rating scale for pain (NRS pain), Mcgill pain questionnaire (MPQ), short-form Mcgill pain questionnaire (SF-MPQ), chronic pain grade scale (CPGS), short form-36 bodily pain scale (SF-36 BPS), and measure of intermittent and constant osteoarthritis pain (ICOAP) Arthritis Care Res. 2011;63(Suppl 11):S240–S252. doi: 10.1002/acr.20543. [DOI] [PubMed] [Google Scholar]
- 34.Alghadir AH, Anwer S, Iqbal A, Iqbal ZA. Test-retest reliability, validity, and minimum detectable change of visual analog, numerical rating, and verbal rating scales for measurement of osteoarthritic knee pain. J Pain Res. 2018;11:851–856. doi: 10.2147/JPR.S158847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mullaney MJ, McHugh MP, Johnson CP, Tyler TF. Reliability of shoulder range of motion comparing a goniometer to a digital level. Physiother Theory Pract. 2010;26(5):327–333. doi: 10.3109/09593980903094230. [DOI] [PubMed] [Google Scholar]
- 36.Kolber MJ, Saltzman SB, Beekhuizen KS, Cheng M-SS. Reliability and minimal detectable change of inclinometric shoulder mobility measurements. Physiother. Theory Pract. 2009;25(8):572–581. doi: 10.3109/09593980802667995. [DOI] [PubMed] [Google Scholar]
- 37.Werner BC, Holzgrefe RE, Griffin JW, Lyons ML, Cosgrove CT, Hart JM, et al. Validation of an innovative method of shoulder range-of-motion measurement using a smartphone clinometer application. J Shoulder Elb Surg. 2014;23(11):e275–e282. doi: 10.1016/j.jse.2014.02.030. [DOI] [PubMed] [Google Scholar]
- 38.Delgado-Gil JA, Prado-Robles E, Rodrigues-de-Souza DP, Cleland JA, Fernández-de-las-Peñas C, et al. Effects of mobilization with movement on pain and range of motion in patients with unilateral shoulder impingement syndrome: a randomized controlled trial. J Manip Physiol Ther. 2015;38(4):245–252. doi: 10.1016/j.jmpt.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 39.Taulaniemi A, Kankaanpää M, Tokola K, Parkkari J, Suni JH. Neuromuscular exercise reduces low back pain intensity and improves physical functioning in nursing duties among female healthcare workers; secondary analysis of a randomised controlled trial. BMC Musculoskelet Disord. 2019;20(1):328. doi: 10.1186/s12891-019-2678-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Alvani E, Shirvani H, Shamsoddini A. Neuromuscular exercises on pain intensity, functional disability, proprioception, and balance of military personnel with chronic low back pain. J Can Chiropr Assoc. 2021;65(2):193–206. [PMC free article] [PubMed] [Google Scholar]
- 41.Lee J-D, Shin W-S. Immediate effects of neuromuscular control exercise on neck pain, range of motion, and proprioception in persons with neck pain. Phys Ther Rehab Sci. 2020;9(1):1–9. doi: 10.14474/ptrs.2020.9.1.1. [DOI] [Google Scholar]
- 42.Sit RWS, Choi SYK, Wang B, Chan DCC, Zhang D, Yip BHK, et al. Neuromuscular exercise for chronic musculoskeletal pain in older people: a randomised controlled trial in primary care in Hong Kong. Br J Gen Pract. 2021;71(704):e226–ee36. doi: 10.3399/bjgp20X714053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Larsen JB, Skou ST, Arendt-Nielsen L, Simonsen O, Madeleine P. Neuromuscular exercise and pain neuroscience education compared with pain neuroscience education alone in patients with chronic pain after primary total knee arthroplasty: study protocol for the NEPNEP randomized controlled trial. Trials. 2020;21(1):218. doi: 10.1186/s13063-020-4126-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Holm PM, Petersen KK, Wernbom M, Schrøder HM, Arendt-Nielsen L, Skou ST. Strength training in addition to neuromuscular exercise and education in individuals with knee osteoarthritis—the effects on pain and sensitization. Eur J Pain. 2021;25(9):1898–1911. doi: 10.1002/ejp.1796. [DOI] [PubMed] [Google Scholar]
- 45.Villadsen A, Overgaard S, Holsgaard-Larsen A, Christensen R, Roos EM. Immediate efficacy of neuromuscular exercise in patients with severe osteoarthritis of the hip or knee: a secondary analysis from a randomized controlled trial. J Rheumatol. 2014;41(7):1385–1394. doi: 10.3899/jrheum.130642. [DOI] [PubMed] [Google Scholar]
- 46.Dong W, Goost H, Lin XB, Burger C, Paul C, Wang ZL, et al. Treatments for shoulder impingement syndrome: a PRISMA systematic review and network meta-analysis. Medicine (Baltimore) 2015;94(10):e510. doi: 10.1097/MD.0000000000000510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gosling AP. Physical therapy action mechanisms and effects on pain management. Revista Dor. 2012;13:65–70. doi: 10.1590/S1806-00132012000100012. [DOI] [Google Scholar]
- 48.Black CD, Huber JK, Ellingson LD, Ade CJ, Taylor EL, Griffeth EM, et al. Exercise-induced hypoalgesia is not influenced by physical activity type and amount. Med Sci Sports Exerc. 2017;49(5):975–982. doi: 10.1249/MSS.0000000000001186. [DOI] [PubMed] [Google Scholar]
- 49.Fernandez-Fernandez J, García-Tormo V, Santos-Rosa FJ, Teixeira AS, Nakamura FY, Granacher U, et al. The effect of a neuromuscular vs. dynamic warm-up on physical performance in young tennis players. J Strength Cond Res. 2020;34(10):2776–2784. doi: 10.1519/JSC.0000000000003703. [DOI] [PubMed] [Google Scholar]
- 50.Clausen B. Neuromuscular exercise as treatment for knee osteoarthritis in middle aged patients. University of Southern Denmark; 2016. [Google Scholar]
- 51.Page P. Shoulder muscle imbalance and subacromial impingement syndrome in overhead athletes. Int J Sports Phys Ther. 2011;6(1):51. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.