Abstract
Background
Hospitals expanded critical care capacity during the COVID-19 pandemic by treating COVID-19 patients with high-flow nasal cannula oxygen therapy (HFNC) in non-traditional settings, including general internal medicine (GIM) wards. The impact of this practice on intensive care unit (ICU) capacity is unknown.
Objective
To describe how our hospital operationalized the use of HFNC on GIM wards, assess its impact on ICU capacity, and examine the characteristics and outcomes of treated patients.
Design
Retrospective cohort study of all patients treated with HFNC on GIM wards at a Canadian tertiary care hospital.
Participants
All patients admitted with COVID-19 and treated with HFNC on GIM wards from December 28, 2020, to June 13, 2021, were included.
Main Measures
We combined administrative data on critical care occupancy daily with chart-abstracted data for included patients to establish the total number of patients receiving ICU-level care at our hospital per day. We also collected data on demographics, medical comorbidities, illness severity, COVID-19 treatments, HFNC care processes, and patient outcomes.
Key Results
We treated 124 patients with HFNC on the GIM wards (median age 66 years; 48% female). Patients were treated with HFNC for a median of 5 days (IQR 3 to 8); collectively, they received HFNC for a total of 740 hospital days, 71% of which were on GIM wards. At peak ICU capacity strain (144%), delivering HFNC on GIM wards added 20% to overall ICU capacity by managing up to 14 patients per day. Patients required a median maximal fraction of inspired oxygen of 80% (IQR 60 to 95). There were 18 deaths (15%) and 85 patients (69%) required critical care admission; of those, 40 (47%) required mechanical ventilation.
Conclusions
With appropriate training and resources, treatment of COVID-19 patients with HFNC on GIM wards appears to be a feasible strategy to increase critical care capacity.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-022-07949-9.
Introduction
Coronavirus disease 2019 (COVID-19), a potentially fatal infection caused by severe acute respiratory syndrome coronavirus 2 virus, was declared a pandemic by the World Health Organization on March 11, 2020.1 Surges in community spread of COVID-19 placed immense pressures on hospitals, and in particular, intensive care unit (ICU) capacity.2–5 Among the many ways that hospitals augmented capacity in response to strained ICU resources was the expansion of critical care delivery into non-traditional spaces, including the provision of high-flow nasal cannula oxygen therapy (HFNC) on general internal medicine (GIM) wards.2
HFNC is an oxygen delivery system capable of providing 100% humidified oxygen at a flow rate of up to 60 liters per minute (lpm). Studies in patients with non-COVID-19-related acute hypoxemic respiratory failure demonstrated that HFNC reduced intubation rates and mortality when compared to conventional oxygen therapies, including oxygen delivered by nasal prongs or face masks.6, 7 Emerging data demonstrate that HFNC has similar efficacy for patients with COVID-19, both in and outside of critical care settings.8–13 Other benefits of HFNC include decreasing anatomic dead space, improving work of breathing and oxygenation, generation of positive pressure, reducing entrainment of room air, and improving secretion clearance.14 Prior to the COVID-19 pandemic, its use was typically restricted to ICU-type settings.15 However, during the pandemic, using HFNC has become common in the management of patients with COVID-19-induced acute hypoxemic respiratory failure, both in the ICU and on GIM wards.16
In response to increasing COVID-19 cases and pressure on critical care resources at our hospital, we began treating patients with COVID-19 requiring HFNC on GIM wards in December 2020. However, the impact of such practice on ICU capacity is unknown. We describe how our center operationalized the use of HFNC on the GIM wards and examine the effect of implementing ward-based HFNC on ICU capacity at our hospital. We also examined the characteristics and outcomes of treated patients.
Methods
Study Setting
We conducted a retrospective cohort study of patients treated with HFNC on GIM wards at Sunnybrook Health Sciences Centre, a 690-bed (approximately 70 ICU beds) tertiary care academic hospital in Toronto, Canada, from December 28, 2020, to June 13, 2021. Ontario (population of 14.8 million) experienced its second and third wave of the COVID-19 pandemic from September 2020 to March 2021, and from March to June 2021, respectively.3 At the peak of wave three, just under half of Ontario’s approximately 2000 ICU beds were occupied by patients with COVID-19, and there were greater than 30,000 new cases weekly (34.4 cases per 100,000).3, 17
Implementation of HFNC on General Medical Wards
HFNC was initiated in patients with refractory hypoxemia (oxygen saturation less than 88%) despite maximally delivered conventional oxygen therapy (e.g., nasal prongs, venturi mask), and not solely in response to low PaO2:FiO2 ratios. This treatment approach is recommended by the National Institutes of Health and used in other centers globally.18–20 At our hospital, HFNC was delivered using Airvo™ 2, a compact nasal high-flow system that delivers Optiflow nasal high-flow therapy. Patients were started on an initial flow of 40 lpm and their previous FiO2 from conventional oxygen therapy (usually FiO2 1.0). Settings were titrated to achieve SpO2 ≥ 92% using the lowest possible FiO2 to avoid the risks associated with hyperoxygenation. Patients were considered for intubation/ICU transfer using the following criteria7: hemodynamic instability (systolic blood pressure below 90 mmHg, mean arterial pressure below 65 mmHg or requirement for inotropic support), neurological deterioration (Glasgow coma scale below 12 points), or worsening respiratory failure defined as any two of the following: respiratory rate > 40 breaths per minute (bpm), no improvement in work of breathing, copious secretions, pH < 7.35, or SpO2 < 90% for 5 min.
At our hospital, delivering HFNC on GIM wards required a multidisciplinary approach, with support from respiratory therapy (RT) and ICU staff, and antecedent training for GIM physicians and nurses (Appendix 1). In preparation for providing HFNC on the GIM wards, an intensivist and RT delivered an interactive educational session for the GIM physicians that included (1) technical information about HFNC, (2) evidence for its use in hypoxemic respiratory failure, (3) evidence for its use in treating patients with COVID-19, and (4) patient selection, monitoring considerations, oxygen therapy titration, and indications for transfer to ICU. We arranged for the ICU outreach team to check in daily with the GIM ward physicians and nurses to monitor the status of patients with COVID-19 on HFNC who were felt to be at risk for clinical deterioration or who required time-sensitive assessments.
Respiratory therapists worked with an advanced practice nurse to develop and deliver educational materials to GIM ward nurses in advance of implementation, including an introductory video, a mobile application that simulates Airvo™ 2’s interface, and a quick reference document. An RT conducted training sessions in the days prior to implementation focusing on principles of therapy and operation of the Airvo™ 2 device. Finally, just-in-time training was provided by RT to the ward nurse upon initiation of HFNC. We used a comanagement model between RT and nursing whereby GIM ward nurses could titrate the HFNC oxygen settings, with support from the RT team who regularly rounded on the patients. One RT was responsible for caring for all patients on the GIM ward receiving HFNC (which ranged from 1 to 14 during the study interval). Recognizing that monitoring and caring for patients with moderate-to-severe hypoxemic respiratory failure required greater resources, the hospital adjusted the nursing staffing ratios (1 nurse to 3–4 patients) on the GIM COVID ward. We also employed remote continuous oxygen saturation monitoring of patients on HFNC from outside rooms, which reduced the number of times nurses needed to enter patient rooms for the purpose of checking oxygenation status.
Prior to opening the ward for patients receiving HFNC, air balancing to negative pressure was implemented along with enhancements in ventilation. All patients on the ward during their period of infectivity with COVID-19 were managed with appropriate personal protective equipment (PPE), including the use of fit-tested N95 masks (as HFNC is considered an aerosol-generating medical procedure), and safety officers were present to supervise donning and doffing of PPE. We also improved signage with PPE reminders to ensure staff safety.21
Study Patients
We included all patients who were admitted to Sunnybrook Health Sciences Centre with a diagnosis of COVID-19 and treated with HFNC on GIM wards from December 28, 2020, to June 13, 2021 (time frame HFNC was offered on GIM wards). HFNC could have been initiated on GIM wards, in the ICU, or in the emergency department (ED). We excluded patients solely treated with HFNC outside the GIM ward (e.g., only in the ED or ICU) or patients that did not receive HFNC during their hospitalization.
Data Sources
We performed a retrospective chart review of Sunnybrook’s electronic medical record to identify patients admitted with COVID-19 and treated with HFNC on GIM wards. Using a database that includes all patients admitted to our hospital with COVID-19, two investigators (WKS, JSZ) screened medical records and identified patients treated with HFNC on GIM wards. We used administrative data to measure critical care occupancy daily, which we combined with chart-abstracted data for patients treated with HFNC on GIM wards, to establish the total number of patients receiving ICU-level care at our hospital per day. We considered patients receiving HFNC on GIM wards as patients receiving ICU-level care since HFNC are traditionally offered in the ICU.15 For eligible patients, six investigators (WKS, JSZ, JN, ASW, BMW, LS) manually extracted study data, including patient demographics, medical comorbidities, illness severity22, 23, COVID-19 treatments, COVID-19 vaccination status, HFNC care processes, and patient outcomes (see Appendix 2 for all variables collected). All investigators first extracted data for the same three patients to ensure consistency of abstraction.
Data Analysis and Ethical Considerations
To estimate the effect of providing HFNC on GIM wards on ICU capacity, we measured ICU capacity strain daily. We calculated daily ICU capacity strain by dividing the total number of patients receiving ICU-level care by the number of available physical ICU beds. During the study period, other locations where patients received ICU-level care included the ED, and ICU surge spaces (e.g., perioperative units, coronary care units). This data allowed us to determine the ICU capacity added to our hospital by providing HFNC on GIM wards. Daily ICU strain capacity was analyzed using Microsoft Excel (Redmond, WA).
We analyzed patient demographics, medical comorbidities, illness severity, COVID-19 treatments, vaccination status, HFNC care processes, and patient outcomes using simple descriptive statistics in SAS (Cary, NC). We also examined the outcomes of patients who were started on HFNC on GIM wards, as well as patients who received maximal FiO2 less than 70% compared to those who received maximal FiO2 greater than 70%. Maximal FiO2 was defined as the maximum FiO2 that was applied to patients (regardless of duration). We reported continuous variables as mean and standard deviation (SD) or median and interquartile ranges (IQR), and categorical variables as counts and proportions. We used univariate statistics including Wilcoxon-rank sum and chi-square tests where appropriate.
Sunnybrook Health Sciences Centre’s Research Ethics Board approved this study.
Results
Patient Demographics
Between December 28, 2020, and June 13, 2021, 545 patients with COVID-19 received care on GIM wards. Of these, 143 (26%) received HFNC at some point during hospitalization; 124 (87% of all patients who received any HFNC) had some or all of their HFNC delivered on the GIM ward. Table 1 summarizes the demographic characteristics of the 124 patients treated with HFNC on GIM wards. The median patient age was 66 years (IQR 52 to 77), 60 (48%) were female, and the median Charlson comorbidity index score was 3 (IQR 2 to 5). The median modified APACHE score at admission was 25 (IQR 17 to 33). The mean admission C-reactive protein level was 105.4 mg/L (SD ± 68.8), mean lymphocyte count was 0.7 (SD ± 0.5), and approximately 50 (41%) patients had an acute kidney injury on admission. No patients were fully vaccinated against COVID-19 (mass vaccination programs in Ontario commenced during the study interval).
Table 1.
Baseline Patient Characteristics
| Characteristic | N=124 |
|---|---|
| Age, median (IQR) | 65.5 (51.5 to 76.5) |
| Sex at birth (F, %) | 60 (48.4%) |
| Comorbidities† | |
| Diabetes mellitus | 39 (31.5%) |
| Coronary artery disease | 18 (14.5%) |
| Solid organ malignancy | 16 (12.9%) |
| Non-COPD lung disease | 10 (8.1%) |
| Congestive heart failure | 9 (7.3%) |
| Chronic kidney disease | 9 (7.3%) |
| Stroke | 6 (4.8%) |
| COPD | 5 (4.0%) |
| Dementia | 4 (3.2%) |
| Peripheral arterial disease | 5 (4.1%), 1 missing |
| Connective tissue disease | 3 (2.4%) |
| Organ transplant | 3 (2.4%) |
| Hematologic malignancy | 1 (0.8%) |
| Immunosuppressive medications | 10 (8.1%) |
| Vaccine status | |
|
Full Partial None |
0 22 (17.7%) 102 (82.3%) |
| Obesity† | 25 (25.8%), 27 missing |
| Smoking† | |
|
Never Current Past |
89 (73.6%) 1 (0.8%) 31 (25.6%), 3 missing |
| Pregnant | 1 (0.8%) |
|
Charlson score, median (IQR)† 0–1 2–3 ≥ 4 Missing |
3 (1.5 to 5) 31 (29.0%) 21 (19.6%) 55 (51.4%) 17 |
| Days from symptom onset to hospitalization, median (IQR) | 8 (5 to 10) |
| Transfer from other acute care hospital | 16 (12.9%) |
| mAPACHE score, median (IQR)† | 25 (17 to 33), 21 missing |
| Admission vital signs, median (IQR)† | |
| Heart rate (bpm) | 96 (84 to 110), 18 missing |
| Mean arterial pressure (mmHg) | 88.5 (74.0 to 99.0), 2 missing |
| Respiratory rate (brpm) | 24 (20 to 28), 22 missing |
| Temperature (°C) | 37.4 (36.7 to 38.2), 19 missing |
| Acute kidney injury at admission† | 50 (41%), 2 missing |
| CRP (mean ± SD)† | 105.4 (± 68.8), 26 missing |
| Dexamethasone | 124 (100%) |
| Remdesivir | 35 (28.2%) |
| Tocilizumab | 84 (80.8%)* |
| Antibiotics (for secondary pneumonia) | 76 (61.3%) |
| Anticoagulation | |
|
Therapeutic Prophylactic None |
19 (15.3%) 104 (83.9%) 1 (0.8%) |
†Some totals may not add up due to missing data
*Tocilizumab first prescribed starting on February 10, 2021. There were 104 eligible patients for treatment
IQR, interquartile range; COPD, chronic obstructive pulmonary disease; mAPACHE, modified APACHE; CRP, C-reactive protein; bpm, beats per minute; brpm, breaths per minute; SD, standard deviation
ICU Capacity Strain
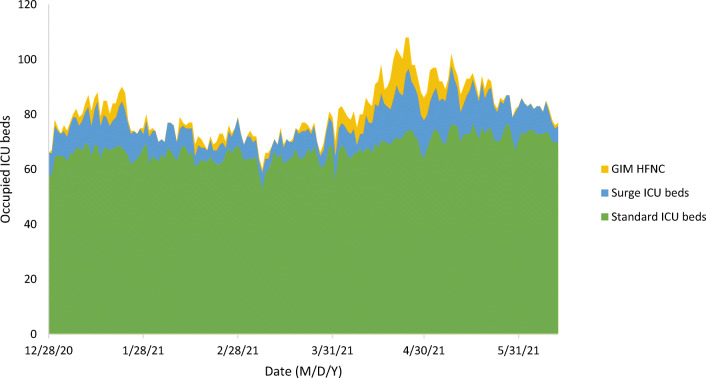
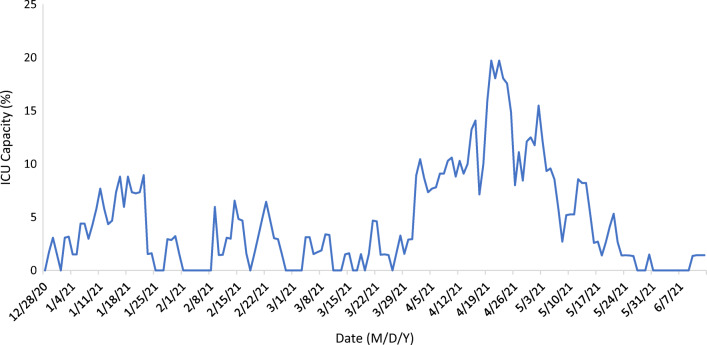
From December 28, 2020, to June 13, 2021, 124 included patients with COVID-19 received HFNC for a total of 740 hospital days; 524 (71%) of these days were delivered on GIM wards. Figure 1 shows the number of patients receiving ICU-level care during our study period, including patients admitted to standard ICU beds, surge ICU beds, and patients receiving HFNC on GIM wards. Appendix 3 outlines the number of patients admitted the to ICU for non-COVID indications. The median number of patients treated with HFNC on GIM wards per day was 2 (IQR 1 to 5). However, during the pandemic’s third wave (April 1 to May 15, 2021), as many as 14 patients requiring HFNC received care on our GIM ward on a single day (the highest census during this period on the GIM COVID-19 ward was 46 patients). ICU capacity strain, including patients requiring HFNC on GIM wards, ranged from 85 to 144% during the study period. Figure 2 summarizes the additional ICU capacity provided by using HFNC on GIM wards, which was as high as 20% during the peak of the pandemic’s third wave.
Figure 1.
Critical care capacity strain. Daily critical care capacity during the COVID-19 pandemic at Sunnybrook Health Sciences Centre. HFNC beds on GIM wards (yellow) are represented in addition to surge ICU beds (blue) and standard ICU beds (green). The greatest increase in critical care capacity from use of HFNC ward beds was during the third wave of the COVID-19 pandemic (April 1 to May 15, 2021).
Figure 2.
Additional critical care capacity added by HFNC on GIM wards. Daily surge capacity during the COVID-19 pandemic at Sunnybrook Health Sciences Centre. The blue line represents the percentage above the usual critical care capacity afforded by offering HFNC on the GIM wards.
HFNC Care Processes
Table 2 outlines HFNC care processes. The majority (N=102; 82%) of HFNC was initiated on GIM wards. Patients who required HFNC received it for a median of 5 days (IQR 3 to 8) during their hospitalization; the median number of days patients were treated with HFNC on the GIM ward was 3 (IQR 2 to 6), where they had a median of 3.5 (IQR 2.9 to 4.3) RT assessments per day. The median maximal fraction of inspired oxygen of patients on the GIM ward was 80% (IQR 60 to 95%) and the median maximal flow was 60 lpm (IQR 55 to 60). All patients who received HFNC on medical wards were treated with dexamethasone, and 35 (28%) received remdesivir. Tocilizumab was first prescribed to patients at our hospital on February 10, 2021. Of the 104 patients discharged after that date, 84 (81%) received tocilizumab. Antibiotics were administered for a presumed secondary bacterial infection to 76 (61%) patients receiving HFNC on GIM wards.
Table 2.
High-Flow Nasal Cannula Oxygen Therapy Care Processes
| Care process | N=124 |
|---|---|
| HFNC total days (GIM + ICU), median (IQR) | 5 (3 to 8) |
| HFNC days on GIM, median (IQR) | 3 (2 to 6) |
| Symptom onset to HFNC in days, median (IQR) | 10 (7 to 12) |
| Location of HFNC initiation | |
| GIM ward | 102 (82.3%) |
| ICU | 2 (1.6%) |
| ED to GIM | 9 (7.3%) |
| ED to ICU | 9 (7.3%) |
| Other | 2 (1.6%) |
| Max FiO2 administered via HFNC on GIM, median (IQR) | 80 (60 to 95) |
| <50% | 7 (5.7%) |
| 50–59% | 17 (13.7%) |
| 60–69% | 21 (16.9%) |
| 70–79% | 15 (12.1%) |
| 80–89% | 17 (13.7%) |
| ≥90% | 47 (37.9%) |
| Max flow (L/min) via HFNC on GIM, median (IQR) | 60 (55 to 60) |
| 40 L/min | 2 (1.6%) |
| 45 L/min | 5 (4.0%) |
| 50 L/min | 16 (12.9%) |
| 55 L/min | 19 (15.3%) |
| 60 L/min | 82 (66.1%) |
| Total number of respiratory therapy assessments per patient, median (IQR) | 12 (6 to 21) |
| Respiratory assessments per patient day on GIM ward, median (IQR)* | 3.5 (2.9 to 4.3) |
| Critical care outreach team activation† | 91 (73.4%) |
*Calculated by dividing the total number of respiratory therapy assessments per patient by the total number of days the patient was on HFNC oxygen therapy on the GIM ward
†This reflects the number of patients that the critical care outreach team was activated for
HFNC, high-flow nasal cannula oxygen therapy; GIM, general internal medicine; ICU, intensive care unit; IQR, interquartile range; ED, emergency department; FiO2, fraction of inspired oxygen
Patient Outcomes
Table 3 outlines outcomes of patients that received HFNC on the GIM ward. The median hospital length of stay was 15 days (IQR 10 to 27.5), and 18 (15%) patients died during hospitalization. Of the 18 that died, 11 died in the ICU and 7 died on the GIM ward. Most ICU patients died despite mechanical ventilation and maximal medical therapy. The majority of those that died on the ward were treated with a comfort measures approach at the end of life. Formal palliative care consultation was requested for 12 (10%) patients. Of the 106 patients that survived to discharge, 65 (61%) were discharged home. The ICU outreach team was involved in the care of 91 (73%) patients, and 85 (69%) patients required admission to an ICU at some point during their hospitalization with a median length of ICU stay of 7 days (IQR 4 to 15). Of those admitted to the ICU, 40 (47%) required mechanical ventilation and 26 (30%) were proned. Only one patient suffered a cardiac arrest outside the ICU, and 8 (9%) required intubation within 2 h of ICU admission. No patients were intubated on the GIM ward prior to ICU transfer. The outcomes of patients (N=102) initiated on HFNC on GIM wards were similar to the whole cohort (Appendix 4). We also compared outcomes of patients whose median maximal fraction of inspired oxygen was less than 70% to those greater than 70% (Appendix 5). Patients who required a median maximal fraction of inspired oxygen greater than 70% were more likely to die in the hospital (20% vs. 4%; p=0.02) and require ICU admission (80% vs. 49%; p<0.01).
Table 3.
Care Outcomes of Patients Receiving HFNC Oxygen Therapy on GIM Wards
| Outcome | N=124 |
|---|---|
| In-hospital death | 18 (14.5%) |
| Admission to critical care (ICU) | 85 (68.5%) |
| Re-admission to ICU* | 9 (10.7%) |
| Hospital length of stay in days, median (IQR) | 15 (10 to 27.5) |
| ICU length of stay in days, median (IQR) | 7 (4 to 15) |
| Cardiac arrest outside ICU | 1 (0.8%) |
| Intubation on arrival in ICU* | 8 (9.4%) |
| Mechanical ventilation* | 40 (47.1%) |
| Acute pulmonary embolism/deep vein thrombosis | 10 (8.1%) |
| Palliative care consult | 12 (9.7%) |
| Discharge destination† | |
| Home | 65 (61.3%) |
| Rehabilitation hospital | 18 (17.0%) |
| Other acute care hospital | 11 (10.4%) |
| Palliative care unit | 6 (5.7%) |
| Transitional care unit | 5 (4.7%) |
| Long-term care unit | 1 (0.9%) |
*Denominator is the number of patients that were treated with HFNC oxygen therapy on GIM wards that required ICU admission (N=85)
†Denominator is the total number of patients that were discharged alive from the hospital (N=106)
HFNC, high-flow nasal cannula oxygen therapy; GIM, general internal medicine; IQR, interquartile range; ICU, intensive care unit
Discussion
In this single-center retrospective cohort study, we found that the use of HFNC on medical wards helped to substantially offload critical care capacity strain at our hospital. Our study is the first, to our knowledge, to quantify the degree to which ICU capacity was offloaded by offering HFNC on GIM wards. During the study period, nearly 90% of all patients treated with HFNC received some or all their HFNC on the GIM ward, with nearly one-third of the patients treated exclusively on our GIM ward and never requiring admission to an ICU. We were also able to offer over two-thirds of HFNC days in this patient population on the GIM ward. At the peak of the pandemic’s third wave, we increased our hospital’s ICU capacity by as much as 20%.
Our ability to deliver HFNC on GIM wards was a result of multidisciplinary stakeholder engagement, early and ongoing professional development for front-line clinicians, clinician engagement in decision-making, clear communication to front-line workers, and low-barrier access to critical care expertise. The use of a similar multifaceted approach for the expansion of critical care services has been successful in other jurisdictions.24, 25 However, treating patients with HFNC on medical wards was resource-intensive and required significant support, particularly from RT and ICU outreach teams. We also utilized lower staffing ratios of patients to nurses, which required several innovative staffing models. The use of HFNC on GIM wards also allowed us to treat patients with high oxygen requirements whose goals of care were not to be intubated or receive further escalation of care. In doing so, we were able to provide end-of-life care for patients with severe hypoxemic respiratory failure, which was previously untenable (given prior to the pandemic, HFNC was only available in the ICU). This enabled the ICU to preserve physical beds for patients requiring mechanical ventilation.
Our findings suggest that treatment of COVID-19 patients with HFNC oxygen therapy on GIM wards did not expose patients to undue harm. Our mortality rate (15%) was comparable to studies of patients with COVID-19 managed in ICU settings with HFNC.10, 11, 23, 26–29 Additionally, the intubation rate was concordant with previous studies of patients with COVID-19 managed with HFNC in ICU settings.10, 11, 23, 26–29 The association we identified between higher FiO2 requirements and worse outcomes is also consistent with other studies.30
We also identified few adverse events associated with the use of HFNC outside of an ICU. There was one cardiac arrest outside the ICU and there were no intubations on the ward. We postulate that the use of continuous oximetry, lower patient-to-nurse ratios (3:1), frequent RT assessments, early involvement of ICU outreach teams, and clear criteria for ICU transfer contributed to the few measured adverse events on our GIM wards. Moreover, improved signage to remind clinicians to use appropriate PPE, presence of safety officers to supervise proper donning and doffing, and upgraded ventilation in clinical areas promoted staff safety.21
Our study has several limitations. First, we studied patients at a single tertiary care academic hospital, and, thus, the generalizability of our findings to the broader healthcare system might be limited. In addition, this care model required significant expertise, staffing resources, and infrastructure that might not be available elsewhere. Reassuringly though, other hospitals have successfully used HFNC to treat patients with COVID-19-associated hypoxemic respiratory failure in non-ICU settings.9, 13 Second, our study was descriptive, and due to sample size constraints, we were unable to compare outcomes of patients that received HFNC on GIM wards to those who received HFNC in the ICU. However, patient outcomes in our study did not differ significantly from studies evaluating HFNC for COVID-19 exclusively in ICU settings.10, 11, 23, 26–29 Third, we did not reliably have access to initial arterial blood gases, SpO2 or FiO2 values for all patients prior to initiating HFNC, and so are unable to provide P:F or S:F ratios. Fourth, our study took place at a time when most patients in our region were not fully vaccinated and therapeutics such as tocilizumab were not readily available; thus, it is possible that clinical outcomes related to HFNC use on GIM wards might differ in other settings, at different times during the pandemic, or as new therapeutics become available.
As the COVID-19 pandemic evolves with new highly transmissible variants of concern and waning vaccine immunity, health systems should prepare for the possibility of rapidly rising case counts and hospitalizations. Even beyond the pandemic, health systems will need strategies to maintain ICU capacity to shoulder non-COVID-related surges in ICU demand. The provision of intensive care in non-traditional spaces is one method to ease the strain on ICU resources. We believe that with appropriate training and resources, this care model could be potentially scaled to other hospitals.2 Future studies should validate the feasibility and safety of HFNC on GIM wards in the broader healthcare system. Our experience highlights that with appropriate training and resources, using HFNC on GIM wards to treat patients with COVID-19 may be a feasible strategy to offload ICU capacity.
Supplementary Information
(DOCX 506 kb)
Footnotes
William K. Silverstein and Jonathan S. Zipursky completed the intellectual and other work typical of the first author.
Brian M. Wong and Lynfa Stroud completed the intellectual and other work typical of the study supervisor.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization. Listings of WHO’s response to COVID-19. Published 2021. Accessed August 25, 2021. https://www.who.int/news/item/29-06-2020-covidtimeline
- 2.Barrett KA, VandeVyvere C, Haque N, et al. Critical Care Capacity During the COVID-19 Pandemic. Science Briefs of the Ontario COVID-19 Science Advisory Table. 10.47326/ocsat.2021.02.51.1.0
- 3.Detsky AS, Bogoch II. COVID-19 in Canada: Experience and Response to Waves 2 and 3. JAMA. Published online August 23, 2021. 10.1001/jama.2021.14797 [DOI] [PubMed]
- 4.Douin DJ, Ward MJ, Lindsell CJ, et al. ICU Bed Utilization During the Coronavirus Disease 2019 Pandemic in a Multistate Analysis—March to June 2020. Crit Care Explor. 2021;3(3). https://journals.lww.com/ccejournal/Fulltext/2021/03000/ICU_Bed_Utilization_During_the_Coronavirus_Disease.14.aspx [DOI] [PMC free article] [PubMed]
- 5.Kokudo N, Sugiyama H. Hospital capacity during the COVID-19 pandemic. Glob Heal Med. 2021;3(2):56–59. doi: 10.35772/ghm.2021.01031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ni Y-N, Luo J, Yu H, Liu D, Liang B-M, Liang Z-A. The effect of high-flow nasal cannula in reducing the mortality and the rate of endotracheal intubation when used before mechanical ventilation compared with conventional oxygen therapy and noninvasive positive pressure ventilation. A systematic review an. Am J Emerg Med. 2018;36(2):226–233. doi: 10.1016/j.ajem.2017.07.083. [DOI] [PubMed] [Google Scholar]
- 7.Frat J-P, Thille AW, Mercat A, et al. High-Flow Oxygen through Nasal Cannula in Acute Hypoxemic Respiratory Failure. N Engl J Med. 2015;372(23):2185–2196. doi: 10.1056/NEJMoa1503326. [DOI] [PubMed] [Google Scholar]
- 8.Fakhri S, Balaban E, Hippensteel J, et al. Assessing the Use of Heated High Flow Nasal Cannula in COVID-19. Am J Respir Crit Care Med. 2021;203(9):A2501. [Google Scholar]
- 9.Guy T, Créachcadec A, Ricordel C, et al. High-flow nasal oxygen: a safe, efficient treatment for COVID-19 patients not in an ICU. Eur Respir J. 2020;56(5):2001154. doi: 10.1183/13993003.01154-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mellado-Artigas R, Ferreyro BL, Angriman F, et al. High-flow nasal oxygen in patients with COVID-19-associated acute respiratory failure. Crit Care. 2021;25(1):58. doi: 10.1186/s13054-021-03469-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Demoule A, Vieillard Baron A, Darmon M, et al. High-Flow Nasal Cannula in Critically Ill Patients with Severe COVID-19. Am J Respir Crit Care Med. 2020;202(7):1039–1042. doi: 10.1164/rccm.202005-2007LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ospina-Tascón GA, Calderón-Tapia LE, García AF, et al. Effect of High-Flow Oxygen Therapy vs Conventional Oxygen Therapy on Invasive Mechanical Ventilation and Clinical Recovery in Patients With Severe COVID-19: A Randomized Clinical Trial. JAMA. 2021;326(21):2161–2171. doi: 10.1001/jama.2021.20714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jackson JA, Trump MW, Oetting TW, Spilman SK, Pelaez CA. High Flow Nasal Cannula for Acute Hypoxic Respiratory Failure in COVID-19. Respir Care. 2020;65(Suppl 10):3448481. [Google Scholar]
- 14.Drake MG. High-Flow Nasal Cannula Oxygen in Adults: An Evidence-based Assessment. Ann Am Thorac Soc. 2017;15(2):145–155. doi: 10.1513/AnnalsATS.201707-548FR. [DOI] [PubMed] [Google Scholar]
- 15.Zemach S, Helviz Y, Shitrit M, Friedman R, Levin PD. The Use of High-Flow Nasal Cannula Oxygen Outside the ICU. Respir Care. 2019;64(11):1333 LP–1342. doi: 10.4187/respcare.06611. [DOI] [PubMed] [Google Scholar]
- 16.National Institutes of Health’s COVID-19 Treatment Guidelines Panel. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. National Institutes of Health. Published 2021. Accessed August 25, 2021. https://www.covid19treatmentguidelines.nih.gov/ [PubMed]
- 17.Public Health Ontario. WEEKLY EPIDEMIOLOGICAL SUMMARY COVID-19 in Ontario: Focus on August 8, 2021 to August 14, 2021. Queen’s Printer for Ontario. Published 2021. Accessed August 25, 2021. https://www.publichealthontario.ca/-/media/documents/ncov/epi/covid-19-weekly-epi-summary-report.pdf?la=en
- 18.COVID-19 Treatment Guidelines Panel. COVID-19 Treatment Guidelines - Oxygenation and Ventilation for Adults. National Institutes of Health.
- 19.Hu M, Zhou Q, Zheng R, et al. Application of high-flow nasal cannula in hypoxemic patients with COVID-19: a retrospective cohort study. BMC Pulm Med. 2020;20(1):324. doi: 10.1186/s12890-020-01354-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Calligaro GL, Lalla U, Audley G, et al. The utility of high-flow nasal oxygen for severe COVID-19 pneumonia in a resource-constrained setting: A multi-centre prospective observational study. eClinicalMedicine 2020;28. 10.1016/j.eclinm.2020.100570 [DOI] [PMC free article] [PubMed]
- 21.Wong BM, Stroud L. How to claim MOC credit for everyday improvement projects (even in a pandemic). Royal College of Physicians and Surgeons of Canada. Published 2021. Accessed January 18, 2022. https://newsroom.royalcollege.ca/how-to-claim-moc-credit-for-everyday-improvement-projects-even-in-a-pandemic/
- 22.Fortis S, O’Shea AMJ, Beck BF, et al. An automated computerized critical illness severity scoring system derived from APACHE III: modified APACHE. J Crit Care. 2018;48:237–242. doi: 10.1016/j.jcrc.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 23.Verma AA, Hora T, Jung HY, et al. Characteristics and outcomes of hospital admissions for COVID-19 and influenza in the Toronto area. CMAJ. 2021;193(12):E410–E418. doi: 10.1503/cmaj.202795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Keene AB, Shiloh AL, Eisen L, et al. Critical Care Surge During the COVID-19 Pandemic: Implementation and Feedback From Frontline Providers. J Intensive Care Med. 2020;36(2):233–240. doi: 10.1177/0885066620973175. [DOI] [PubMed] [Google Scholar]
- 25.Vranas KC, Golden SE, Mathews KS, et al. The Influence of the COVID-19 Pandemic on ICU Organization, Care Processes, and Frontline Clinician Experiences: A Qualitative Study. Chest. 2021;160(5):1714–1728. doi: 10.1016/j.chest.2021.05.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.COVID-ICU group for the REVA network COVID-ICU Investigators Benefits and risks of noninvasive oxygenation strategy in COVID-19: a multicenter, prospective cohort study (COVID-ICU) in 137 hospitals. Crit Care. 2021;25(1):421. doi: 10.1186/s13054-021-03784-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Menga LS, Cese LD, Bongiovanni F, et al. High Failure Rate of Noninvasive Oxygenation Strategies in Critically Ill Subjects With Acute Hypoxemic Respiratory Failure Due to COVID-19. Respir Care. 2021;66(5):705 LP–714. doi: 10.4187/respcare.08622. [DOI] [PubMed] [Google Scholar]
- 28.Liu L, Xie J, Wu W, et al. A simple nomogram for predicting failure of non-invasive respiratory strategies in adults with COVID-19: a retrospective multicentre study. Lancet Digit Heal. 2021;3(3):e166–e174. doi: 10.1016/S2589-7500(20)30316-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Duan J, Chen B, Liu X, et al. Use of high-flow nasal cannula and noninvasive ventilation in patients with COVID-19: A multicenter observational study. Am J Emerg Med. 2021;46:276–281. doi: 10.1016/j.ajem.2020.07.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chatterjee NA, Jensen PN, Harris AW, et al. Admission respiratory status predicts mortality in COVID-19. Influenza Other Respi Viruses. 2021;15(5):569–572. doi: 10.1111/irv.12869. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 506 kb)