Abstract
In-person, individual counseling using the PLISSIT model is a well-known approach to help people with sexual problems. Evidence suggests that Grouped Sexuality Education (GSE) can be as effective as in-person sexuality education. The efficacy of PLISSIT versus GSE has not previously been evaluated in women with Breast Cancer (BC). In this paper, we report on the effect of PLISSIT versus GSE on self-reported sexual behaviors experienced by women after a BC diagnosis (n = 75). The women were randomly allocated into three groups, with 25 women in each arm. Data analysis of the intention-to-treat population (n = 65) revealed efficacy of both GSE and PLISSIT in improving sexual behaviors (p < 0.0001) with a positive change in sexual capacity, motivation and performance after 6- and 12-weeks post-intervention follow ups. We found the GSE model showed a greater efficacy than the PLISSIT model. Due to the substantial needs faced by women with cancer and the cost associated with implementing the PLISST model, GSE seems to be more effective. We recommend GSE for Iranian communities where management of sexual problems is at an early stage and where the sexuality of women with cancer is routinely overlooked.
Keywords: PLISSIT, sexual health model, breast cancer, Iran, RCT
Introduction
Sexual problems have always been an important consideration for women recovering from cancer. The prevalence of sexual problems in women without cancer is 40%, whereas this figure increases to 80% to 90% in women with genital cancers (De Vocht, Hordern, & Notter, 2011). In women with breast cancer (BC), the occurrence of sexual problems is often inevitable due to female body self-image, surgery, and loss of sexual or reproductive-related organs. Women with reproductive or breast cancers therefore often suffer from loss of libido, body image disorders, and related conditions (Kadkhodayan, Hasanzade Monfared, Saghafi, & Mokhber, 2015; Ussher, Perz, Gilbert, & The Australian Cancer and Study Team, 2015; Fahami, Mohamadirizi, & Savabi, 2017; Zaighami Mohammadi, 2009). Sexual problems lead to challenges and stress in the interpersonal relationships of affected women, and these problems may vary widely in scope depending on the severity of the disease. Women diagnosed with BC face a severe threat to their physical, mental and social health. Published studies have suggested that although the majority of affected women receive effective treatment for their cancer, sexual dysfunction may become an important untreated problem in the intimate lives of these patients (Zaighami Mohammadi, 2009). Many previous studies have focused on examining best approaches to help BC survivors make necessary changes in their sexual behaviors (Kadkhodayan et al., 2015; Sharif, Absharshari, Hazrati, Tahmasebi, & Najaf, 2011; Perz, Ussher, Gilbert, & The Australian Cancer and Sexuality Study Team, 2014; Safaee & Moghim Dehkordi, 2007). Evidence to date supports the use of behavioral therapy through in-person counseling such as the Permission, Limited Information, Specific Suggestion, and Intensive Therapy (PLISSIT) model. Je-hell et al. (2013) showed that counseling with the PLISSIT model was effective in improving sexual function, increasing sexual satisfaction, and improving sexual intimacy among women with cancer and their spouses (Nho, 2013).
A number of other studies with similar outcomes around the world have found an important impact of the psychiatric counseling model on improving sexual function among women exposed to various acute and chronic diseases (El-Sayed Saboula, 2015; Moradi, Abdollahzadeh, Zamanzadeh, Aswad, & Ghaleban, 2013; Faghani & Ghaffari, 2016). For instance, in a study with women with BC Faghani et al. (2016) reported effectiveness of the PLISSIT model in improving their sexual problems as well as quality of the couples’ sexual lives (Faghani & Ghaffari, 2016). However, other publications have highlighted the advantages of group interventions versus in-person counseling and education, due to factors including lack of patient compliance and participation. Grouped sexuality education may be a feasible timesaving alternative to one-on-one counseling sessions (Farnam, Janghorbani, Raisi, & Merghati-Khoei, 2014). GSE has been widely employed to encourage behavioral changes, and a recent study reported its potential for managing sexual distress in women with sexual problems (Robinson, Bockting, Rosser, & Miner, 2002). Similarly, Julia, Beth, Catherine, Thomas, and Patricia (2010) showed that group counseling could be effective in increasing the sexual satisfaction and intimacy of couples (Julia et al., 2010).
The primary aim of our study was to compare changes in sexual behavior scores (capacity, motivation, performance, and scripts) over a 12 week data collection period, with 75 women with BC allocated to three arms (PLISSIT, GSE, or routine care).
Materials and methods
This study was conducted among 75 women with BC referred to the Mehraneh Charity Cancer Center and Valiasr hospital from 2016–2017. The study protocol was approved by the ethics committee of Zanjan University of Medical Sciences (ZUMS.REC.1395.156). The women provided us with verbal and written informed consent before entering the study.
Inclusion and exclusion criteria
At the first visit we assessed women for the main inclusion criteria including: being sexually active, having no other cancers, having completed at least three months after surgical treatment or chemotherapy treatment, not having attended any formal sexuality education over the past six months, having no history of diagnosed mental illness before BC, and reporting no drug or alcohol use. Exclusion criteria included the relapse of BC, hospitalization during the intervention, pregnancy, and initiation of psychiatric pharmacotherapy at the time of our intervention.
Study protocol
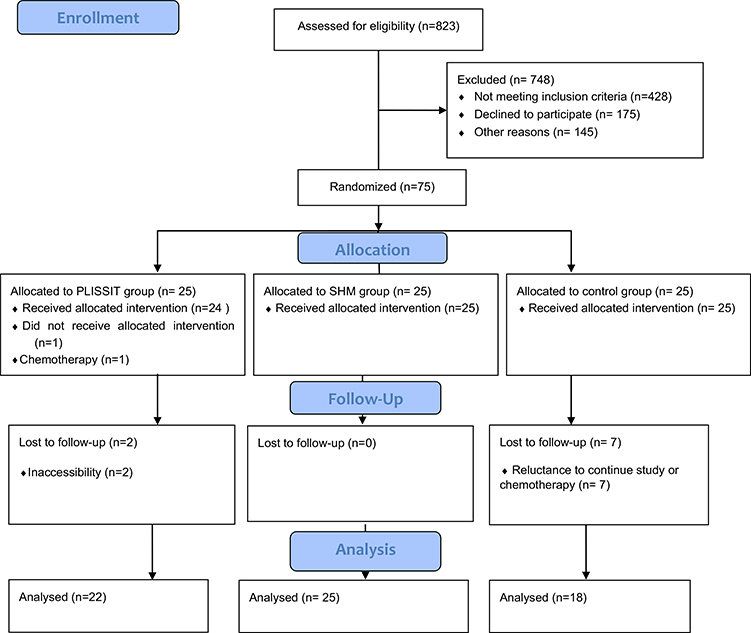
We assessed 823 medical records of women with BC in Valiasr Hospital and Mehraneh to identify eligible participants. Of 823 women, 407 met the primary inclusion criteria including being married, aged between 20 to 50 years old, and having completed their chemotherapy or radiotherapy treatments. All women underwent mastectomy before enrollment in the study. The main researcher (ME) contacted women to explain the study and invite participation. Of 407 eligible women, 232 women initially agreed to participate in the study. Of these women, only 75 accepted to enter the study. During the study, 10 participants were excluded due to initiation of a selective chemotherapy, moving out of the city or unwillingness to continue participation. One of the main reasons for greater attrition in the control group appeared to be because they did not receive any treatment, so they did not feel well, and therefore were less likely to continue the study (Figure 1).
Figure 1.
Flowchart of study participants.
Interventions and procedure
In this study, we randomized women to two intervention and one control groups. We employed two forms of sexuality education and counseling approaches: PLISSIT (intervention group A) and GSE (intervention group B). The PLISSIT group (intervention group A) attended 45–90 minute sessions (one to three in-person sessions), with session length varying based on the participant’s preferences and availability. All sessions were started after obtaining verbal and written informed consents. Instructions for PLISSIT were carefully applied in each session. The sex therapist (EMK) was a qualified sexologist and (ME) had been professionally trained to apply the PLISSIT model. The sessions were related to the specific problem each subject had brought up, and limited information as well as provision of solutions were provided through the sessions. In the GSE group (intervention group B), counseling was provided through group training focused on sexual health in an interactive six-hour workshop with 12–13 members per group. GSE is based on 10 building blocks to provide healthy sexual relations which include discussion of sexual issues, cultural and sexual identity, anatomy, sexual function and preferences, safe sexual relations, sexual health care, sexual challenges, body image, sexual imagination and arousal, and positive feelings about sexual desire. Education was presented using the PowerPoint slides and questions and answers.
Control group
The control group (group C) only received the center’s routine care. The control group was provided with the contact details for the therapist (ME), to seek help related to any sexual problems post BC treatment after completion of the 12-week study period.
Sample size
When designing this study, we were not aware of any previous study making an estimate of therapeutic impact that would have allowed us to estimate the sample size required to power this study for our primary comparison of interest. Therefore, based on our own experience, we assumed an anticipated difference of 2.0 on sexual behavior scores between the PLISSIT and GSE groups. Under this assumption, with a 20% loss to follow-up, we calculated a sample size of 25 women per group to achieve 80% power (with a two-sided alpha of 0.05).
Blinding
Masking the arm allocation was not possible by the behavioral nature of the intervention.
Randomization scheme
In this randomized, controlled, open-label, two-center TRAID with three parallel arms; a total of 75 women with BC from the Mehraneh Charity Cancer Center and Valiasr hospital in Zanjan, Iran are block-randomized (blocking factor: diagnosed with BC and completed treatment) into three arms, namely (a) individual counseling with the PLISSIT model; (b) group received GSE model; and (c) control group. The block numbers were selected from the random table numbers and 25 participants were assigned to each group.
Measurement
The study tools consisted of questionnaire items relating to demographics, disease characteristics, sexual distress, and quality of life. The sociodemographic and disease-specific tools included 19 items regarding age, marital status, education, urban/rural residence, employment, number of children, history of drug abuse, menopause status, treatment status, medicines used, and treatment duration. The sexual distress questionnaire included 13 items to assess distress level related to reduced sexual desire. The validity and reliability of the revised questionnaire was calculated by DeRogatis, Clayton, Lewis-D’Agostino, Wunderlich, and Fu (2008) based on a 13-item version, and Azimi Nekoo et al. (2014) validated its Farsi version with 2400 women. The scores are based on the Likert scale, with a score above 11 interpretable as a lack of distress and no need for medical intervention (DeRogatis et al., 2008). Finally, we included a 33-item sexual behavior questionnaire that was designed and validated (Cronbach’s alpha = 0.81) by Ghorashi, Yousefy, and Merghati-Khoei (2016). This sexual behavior questionnaire is based on Iranian culture, and we believe that sexual attitudes are deeply intertwined with the cultural milieu. Thus we believe this sexual behavior questionnaire is culturally appropriate for use in this population. The sexual behavior questionnaire assesses four subscales include capacity (10 Qs), performance (9 Qs), motivation (11 Qs), and sexuality scripts (last 3 Qs). Each question is assessed using a Likert scale from 0 to 5 (Ghorashi et al., 2016). Based on total score, the participant’s sexual behavior status is classified into three categories: low (poor), moderate, and high (desirable) sexual behavior.
Statistical analysis
We used the SPSS version 16.0 for all statistical analyses. Demographic characteristics were compared between the three groups using the Chi-squared test. The normal distribution of all continuous variables was investigated using the Kolmogrov-Smirnov test. Quantitative demographic data were analyzed using the ANOVA test, and the primary outcomes of sexual behavior dimensions were analyzed using the repeated measures.
Results
The mean age of participants in the PLISSIT, GSE, and control groups were 38.1 ± 5.5, 40.4 ± 7.2, and 41.4 ± 4.4, respectively. The mean age of spouses in the PLISSIT, GSE, and control groups were 42.3 ± 7.8, 45.2 ± 9.3, and 43.6 ± 5.09, respectively. There was no significant difference between the groups in terms of age, spouse’s age, or other demographic variables. All participants were treated with Tamoxifen or Herceptin. There was no statistically significant difference between the groups in terms of sexual problems in the spouse, or medical treatment of the participants (Tables 1 and 2).
Table 1.
Sociodemographic characteristics of participants by groups.
| PLISSIT group |
GSE group |
Control group |
|||||
|---|---|---|---|---|---|---|---|
| Variable | Mean | SD | Mean | SD | Mean | SD | p value |
|
| |||||||
| Age | 38.12 | 5.56 | 40.40 | 7.29 | 41.04 | 4.40 | 0.189 |
| Husband’s age | 42.36 | 7.86 | 45.28 | 9.34 | 43.68 | 5.09 | 0.405 |
| Number of children | 3.08 | 0.64 | 2.80 | 1.04 | 3.16 | 0.74 | 0.277 |
| Number of years of marriage | 16.48 | 5.93 | 19.20 | 9.72 | 19.92 | 7.16 | 0.262 |
Table 2.
Comparison of socioeconomic, disease and therapeutic characteristics of the participants between the three groups.
| PLISSIT group |
GSE group |
Control group |
||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Number | Percent | Number | Percent | Number | Percent | p value | |
|
| ||||||||
| Job | Housewife | 18 | 72 | 21 | 84 | 20 | 80 | 0.573 |
| Employed | 7 | 24 | 4 | 16 | 5 | 20 | ||
| Husband’s job | Employed | 9 | 36 | 8 | 32 | 5 | 20 | 0.433 |
| Self-employment | 16 | 64 | 17 | 68 | 20 | 80 | ||
| Education | Elementary | 7 | 28 | 6 | 24 | 12 | 48 | 0.821 |
| Middle to secondary | 5 | 20 | 4 | 16 | 4 | 16 | ||
| Diploma | 6 | 24 | 10 | 40 | 5 | 20 | ||
| College education | 7 | 28 | 5 | 20 | 4 | 16 | ||
| Husband’s education | Elementary | 6 | 24 | 3 | 12 | 9 | 36 | 0.821 |
| Middle to secondary | 7 | 28 | 8 | 32 | 7 | 28 | ||
| Diploma | 4 | 16 | 8 | 32 | 5 | 20 | ||
| College education | 8 | 32 | 5 | 20 | 4 | 16 | ||
| Sexual problem in spouse | Decreased libido | 21 | 84 | 15 | 60 | 21 | 84 | 0.780 |
| Premature ejaculation | 1 | 4 | 6 | 24 | 2 | 8 | ||
| Other | 3 | 12 | 4 | 16 | 2 | 8 | ||
| Medical treatment | Tamoxifen | 25 | 100 | 25 | 100 | 25 | 100 | 1 |
We found no significant baseline differences between the three groups in the mean score of participants’ sexual behavior (Table 3).
Table 3.
Comparison of the average sexual behavior of participants between the three study groups with repeated measures.
| Baseline |
6 weeks follow-up |
12 weeks follow-up |
||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Mean | SD | Mean | SD | Mean | SD | p value | |
|
| ||||||||
| PLISSIT group | Sexual capacity | 20.12 | 11.28 | 18.77 | 9.71 | 21.90 | 9.49 | 0.797 |
| Sexual function | 5.40 | 5.95 | 7.54 | 6.91 | 8.18 | 9.58 | 0.128 | |
| Sexual motivation | 22.12 | 11.03 | 24.45 | 9.77 | 22.77 | 8.99 | 0.541 | |
| Sexual scheme | 7.24 | 3.65 | 7.90 | 2.59 | 8.59 | 2.44 | 0.515 | |
| Total sexual behavior | 54.88 | 24.92 | 58.68 | 25.07 | 61.45 | 22.53 | 0.872 | |
| GSE group | Sexual capacity | 18.68 | 7.61 | 31.87 | 4.61 | 25.25 | 5.14 | 0.001 |
| Sexual function | 6.56 | 6.42 | 24 | 4.05 | 23.37 | 6.09 | 0.001 | |
| Sexual motivation | 24.68 | 9.94 | 27.58 | 7.16 | 27.7 | 7.51 | 0.125 | |
| Sexual scheme | 8.12 | 3.9 | 9.04 | 2.88 | 8.5 | 3.31 | 0.219 | |
| Total sexual behavior | 58.04 | 20.02 | 92.5 | 11.69 | 84.83 | 15.69 | 0.001 | |
| Control group | Sexual capacity | 20.36 | 9.29 | 17.57 | 7.87 | 19.73 | 9.79 | 0.095 |
| Sexual function | 3.36 | 4.07 | 8.15 | 8.89 | 10.55 | 8.34 | 0.001 | |
| Sexual motivation | 24.80 | 7.5 | 22.5 | 7.55 | 21.10 | 6.67 | 0.017 | |
| Sexual scheme | 8.36 | 3.21 | 9.2 | 2.33 | 9.45 | 2.32 | 0.453 | |
| Total sexual behavior | 56.88 | 19.25 | 57.27 | 20.62 | 61.89 | 16.81 | 0.001 | |
The mean sexual behavior of the participants increased at six and 12 weeks after the intervention in both intervention groups compared to the control group. This increase was statistically significant in the GSE group (p < 0.001). Examining the sexual behavior scores at six and 12 weeks after intervention, we found that scores improved among the GSE group relative to the PLISSIT and control groups for sexual capacity, sexual function, and the total sexual behavior scale after six weeks, as well as the sexual function subscale and the total sexual behavior score after 12 weeks. Mean sexual behavior scores also improved in the control group, which received routine intervention. This improvement may be attributed to various reasons such as: receiving education via television, self-referral to medical centers and conferences (Table 3).
In the intervention group with the PLISSIT model, the mean score for sexual behavior increased at six weeks and 12 weeks after intervention compared to before intervention; however, this increase was not statistically significant. In comparing the PLISSIT model with the GSE model, the mean increase was significant in the GSE group, whereas the PLISSIT group did not show a significant increase in the mean sexual behavior score compared to the control group (Table 4).
Table 4.
Pairwise comparison of the impact of PLISSIT and GSE counseling models and the control group.
| Group | Mean Difference | P value | |
|---|---|---|---|
|
| |||
| PLISSIT Model | GSE Model | −11.258 | 0.051 |
| Control Group | 6.362 | 0.279 | |
| GSE Model | PLISSIT Model | 11.258 | 0.051 |
| Control Group | 17.620 | 0.005 | |
| Control Group | PLISSIT Model | −6.362 | 0.279 |
| GSE Model | −17.620 | 0.005 | |
Discussion
Consultation using the GSE group had a positive impact on the sexual behavior of BC patients, with a statistically significant improvement in participants’ sexual behavior compared to the control group during the two follow-up periods of six and 12 weeks, but a similar impact was not noted among the group receiving the PLISSIT model. According to our finding, group counseling and education models seem to be more efficient than individualized sessions in some contexts with conservative culture such as Iran. We argue that cultural considerations about sexually-related discussion are more important than its content or means of application. Years of working experience (EMK) and her research findings reveal that Iranians are reluctant to unveil their own sexual life stories, but are interested in listening to generalized lessons related to sexuality or sexual health (Ghorashi, Merghati-Khoei, & Yousefy, 2014; Khoei, Whelan, & Cohen, 2008; Merghati-Khoei, 2006). Some findings from this study are supportive of results found by other studies. Ahmed, Marchand, Williams, Coscarelli, and Ganz (2016) showed that six group counseling sessions were effective in improving the sexual function and anxiety of cancer survivors (Ahmed et al., 2016). Similarly, Heravi Karimovi, Pourdehqan, Jadid Milani, Foroutan, and Aieen (2006)) showed that group counseling was effective in improving the sexual function of women with breast cancer.
Evidence from the current study showed that the GSE model was superior to the PLISSIT model in the studied population. In addition to a meaningful statistical difference between the GSE group and the control group, the effect of the GSE model was 68.1% greater in the intervention group versus control, based on the effect size formula. In contrast, using this formula, the PLISSIT model had no effect in our study group versus control. However, recent work by Faghani et al. (2015) was not consistent with the findings of this study. Faghani and Ghaffari (2016) showed that mean sexual function of women with BC significantly improved with the PLISSIT model compared to the control group. Similarly, the results of a study by El-Sayed Saboula (2015) showed that the use of the PLISSIT model was effective in improving sexual relationships in BC patients.
It is possible that differences in implementation of the interventions, the number of sessions, tools, and features of the community studied are among the reasons for these differences. The GSE model includes ten educational components, and has flexibility for use in different cultures and groups. Considering the results of our study, it seems that counseling based on the GSE model can be used as an effective tool for counseling and education among women being treated for or recovering from BC.
Conclusion
The Grouped Sexuality Education (GSE) had a significant beneficial effect on measures of sexual behavior in women with BC. Although PLISSIT has been recognized as an efficient therapeutic approach worldwide, GSE may be more efficient in conservative cultures, such as the Iranian culture of sexuality. We suggest that further research is needed to better understand the effect of sexual counseling during and after cancer treatment. These women deserve improved attention, support, and care.
Limitations
Our study had several limitations. First, we were unable to include the subjects’ spouses in counseling sessions. This limitation was predicated on our research experiences showing that Iranian men are less interested in participating in research related to sexuality. It was beyond the scope of this research funding opportunity to carry out interventions for couples suffering from breast cancer. Second, it is important to note that the results of this trial may not be generalizable to women with other types of cancer, or patients in different situations such as different stages of BC or different stages of sexual relationships. Third, we were aware that participant responses to sexuality-related questions may have been impacted by their recent loss of one or two of their sexual organs due to cancer. Measuring some of the outcomes before chemotherapy and mastectomy might allow an assessment of how much this possible bias may have affected our results. Nevertheless, this type of bias is not expected to substantially impact our comparison of efficacy between GSE, PLISSIT, and standard of care.
Supplementary Material
Acknowledgement
The authors sincerely thank the steering committee for the oncology clinic of Valiasr Hospital, and the Mehraneh charity clinic, for the approval of our research proposal and their invaluable contribution during the study. Our special thanks to Dr. Minush Moghimi, the selected Oncologist for her valuable assistance during the study. We sincerely appreciate the priceless support of the participants, who shared with us their private matters.
Funding
The trial is funded by Zanjan University of Medical Sciences (ZUMS.REC.1395.156). In this study tried to protect the rights of all participants and suppliers. We acknowledge the Research Ethics Committee of the Zanjan University of Medical Sciences’ approval of this research project (IRCT2016083025431N2).
Abbreviation:
- GSE
Grouped Sexuality Education
- PLISSIT
Permission, Limited Information, Specific Suggestion, and Intensive Therapy
- BC
Breast cancer
- ME
Mina Esmkhani
- EMK
Effat Merghaty Khoei
Footnotes
Disclosure statement
No potential conflict of interest was reported by the author(s).
Declarations
Statement of authorship
Category 1: 1.1. Conception and Design: Mina Esmkhani, Effat Merghati Khoei, Roghieh Kharaghani, Elham Shakibazadeh. 1.2. Acquisition of Data: Mina Esmkhani. 1.3. Analysis and Interpretation of Data: Mina Esmkhani, Soghrat Faghihzadeh.
Category 2: 2.1. Drafting the article: Mina Esmkhani, Effat Merghati Khoei. 2.2. Revising It for Intellectual Content: Mina Esmkhani, Effat Merghati Khoei, Jeffrey E. Korte, Elham Shakibazadeh.
Category 3: Final Approval of the Completed Article: Mina Esmkhani, Effat Merghati Khoei, Roghieh Kharaghani, Elham Shakibazadeh, Soghrat Faghihzadeh, Noura Aghajani, Jeffry E. Korte.
Ethics approval and consent to participate
This study has been approved by the Ethics Committee of Zanjan University of Medical Sciences. Informed consent obtained from all participants before participation in the study. Then after obtaining permission from the authorities of the Zanjan Cancer Clinic, obtaining permission from the research vice president and submitting the license to the sampling center, obtaining written and informed consent of the participants in the research, full introduction of the researcher to the participants to express the goals and method of work to the participants and to allow the person to step down at each stage of the research, and preservation of trusteeship about information obtained from research samples.
Supplemental data for this article is available online at https://doi.org/10.1080/14681994.2020.1732910.
References
- Ahmed K, Marchand E, Williams V, Coscarelli A, & Ganz PA (2016). Development and pilot testing of a psychosocial intervention program for young breast cancer survivors. PMC, 99(3), 414–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azimi Nekoo E, Burri A, Ashrafti F, Fridlund B, Koenig HG, Derogatis LR, & Pakpour AH (2014). Psychometric properties of the Iranian version of the female sexual distress scale-revised in women. The Journal of Sexual Medicine, 11(4), 995–1004. [DOI] [PubMed] [Google Scholar]
- De Vocht H, Hordern A, Notter J. H. W. d. (2011). A team approach towards communication about sexuality and intimacy in cancer and palliative care study. Australasian Medical Journal, 4(11), 610–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeRogatis L, Clayton A, Lewis-D’Agostino D, Wunderlich G, & Fu Y (2008). Validation of the female sexual distress scale-revised for assessing distress in women with hypoactive sexual desire disorder. The Journal of Sexual Medicine, 5, 357–364. [DOI] [PubMed] [Google Scholar]
- El-Sayed Saboula N, (2015). Effectiveness of application of PLISSIT counseling model on sexuality for breast cancer’s women undergoing treatment. American Journal of Nursing Science, 4(4), 218. [Google Scholar]
- Faghani S, & Ghaffari F, (2016). Effects of sexual rehabilitation using the PLISSIT model on quality of sexual life and sexual functioning in post-mastectomy breast cancer survivors. Asian Pacific Journal of Cancer Prevention: APJCP, 17(11), 4845–4851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fahami F, Mohamadirizi S, Savabi M, (2017). The relationship between sexual dysfunction and quality of marital relationship in genital and breast cancers women. Education of Health Promotion, 6, 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farnam F, Janghorbani M, Raisi F, & Merghati-Khoei E, (2014). Compare the effectiveness of PLISSIT and sexual health models on women’s sexual problems in Tehran, Iran: A randomized controlled trial. The Journal of Sexual Medicine, 11(11), 2679–2689. [DOI] [PubMed] [Google Scholar]
- Ghorashi Z, Merghati-Khoei E, & Yousefy A (2014). Measuring Iranian women’s sexual behaviors: Expert opinion. Journal of Education and Health Promotion, 3, 80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghorashi Z, Yousefy A, & Merghati-Khoei E (2016). Developing and validating a questionnaire to measure women’s sexual behaviors: A psychometric process. Galen Medical Journal (GMJ), 5(4), 208–214. [Google Scholar]
- Heravi Karimovi M, Pourdehqan M, Jadid Milani M, Foroutan SK, & Aieen F, (2006). Study of the effects of group counseling on quality of sexual life of patients with breast cancer under chemotherapy at Imam Khomeini Hospital. Journal of Mazandaran University of Medical Sciences, 16(54), 43–51. (Persion). [Google Scholar]
- Julia H, Beth E, Catherine, Thomas R, Patricia A (2010). Addressing intimacy and partner communication after breast cancer: A randomized controlled group intervention. Breast Cancer Research and Treatment, 118(1), 99–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kadkhodayan S, Hasanzade Monfared M, Saghafi M, & Mokhber M. N. r. (2015). Evaluation of sexual dysfunction in women with ovarian cancer admitted to Ghaem and Omid hospitals in Mashhad. Iranian Journal of Obstetrics, 18(141), 1–7. (persion). [Google Scholar]
- Khoei EM, Whelan A, & Cohen J, (2008). Sharing beliefs: What sexuality means to Muslim Iranian women living in Australia. Culture, Health & Sexuality, 10(3), 237–248. [DOI] [PubMed] [Google Scholar]
- Merghati-Khoei E (2006). Language of love in culture of silence: Iranian women’s sexual understandings and sociocultural context (UNSWPhD, Thesis). Public Health& Community Medicine, Faculty of Medicine.
- Moradi N, Abdollahzadeh F, Zamanzadeh V, Aswad I, & Ghaleban K (2013). Effects of husband’s education on meting supportive care needs of breast cancer patients: A clinical trial. Journal of Hamadan Nursing & Midwifery Faculty, 21(3), 40–50. [Google Scholar]
- Nho JH, (2013). Effect of PLISSIT model sexual health enhancement program for women with gynecologic cancer and their husbands. Journal of Korean Academy of Nursing, 43(5), 681–689. [DOI] [PubMed] [Google Scholar]
- Perz J, Ussher E, Gilbert J(2014). Feeling well and talking about sex: psycho-social predictors of sexual functioning after cancer. BMC Cancer, 14, 228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson B, Bockting W, Rosser S, Miner. (2002). The Sexual Health Model: Application of a sexological approach to HIV prevention. Health Education Research, 17(1), 43–57. [DOI] [PubMed] [Google Scholar]
- Safaee A, & Moghim Dehkordi B (2007). Validation study of a quality of life (QOL) questionnaire for use in Iran. Asian Pacific Journal of Cancer Prevention, 8(4), 543–546. (Persion). [PubMed] [Google Scholar]
- Sharif F, Absharshari N, Hazrati M, Tahmasebi S, & Najaf. (2011). The impact of peer education on quality of life in breast cancer patients after surgery. Payesh, 11(5), 703–710. (Persion). [Google Scholar]
- Ussher JM, Perz J, Gilbert E, & The Australian Cancer and Sexuality Study Team. (2015). Perceived causes and consequences of sexual changes after cancer for women and men: A mixed method study. BMC Cancer, 15(1), 268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaighami Mohammadi SH, (2009). Sexual dysfunction and relationship to quality of life in patients with cancer. Iranian Journal of Obstetrics, 12(2), 39–46. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.