Abstract
Panagglutination on the indirect antiglobulin test is one of the most challenging dilemmas of pretransfusion testing. It occurs when patient sera react with all red blood cells tested, that is, with both screening and identification panel cells. Two main questions must be answered. The first is to determine whether panagglutination results from the presence of autoantibody and/or alloantibody (single alloantibody or multiple alloantibodies or antibody to high-incidence antigen). The second problem is to detect the possible concomitant presence of clinically significant alloantibodies masked by panagglutination. The purpose of this mini-review is to describe the situations that can cause panagglutination and to develop algorithms which can resolve the problem. The two main points in the evaluation of panagglutination involve the assessment of the intensity of reactivity with the reagent red cells used and whether the autocontrol is positive or not. It is imperative to understand the laboratory results and the techniques available that guide the investigative process.
Keywords: Incompatibility, panagglutination, pretransfusion testing
Introduction
The detection of antibodies produced against red cell antigens in the serum of patients about to undergo transfusion is a critically important process during pretransfusion testing, with the ultimate aim being a safe transfusion. The detection and identification of antibodies is achieved by the indirect antiglobulin test (indirect Coombs, IAT) using patient serum and known phenotype red blood cells.[1,2] The presence of a single alloantibody is usually not a problem, and the identification is often easy. Problems arise when the number of alloantibodies is higher or when there are also autoantibodies in the serum.
Panagglutination during the antibody detection process occurs when the patient's serum reacts with all the reagent red cell samples used in both the screening test and the identification panel.[3] One of the key questions to be answered is whether panagglutination results from the presence of autoantibody and/or alloantibody (single alloantibody or multiple alloantibodies or antibody to high-incidence antigen). It is also important to be clarified if the panagglutination can mask clinically significant alloantibodies and can complicate pretransfusion testing. Prior to the laboratory investigation of each case, it is necessary to know the medical history of the patient as well as their history of transfusions and any past pregnancies. In particular, information is needed about the patient's age, sex, race, diagnosis, laboratory tests, current medications, intravenous solutions, and the time before last transfusion and previous antibody screening results as well. The next steps in the evaluation of panagglutination involve the assessment of the intensity of reactivity with the reagent red cells used and whether the autocontrol is positive or not.[4,5]
Variable Intensity of Reactivity
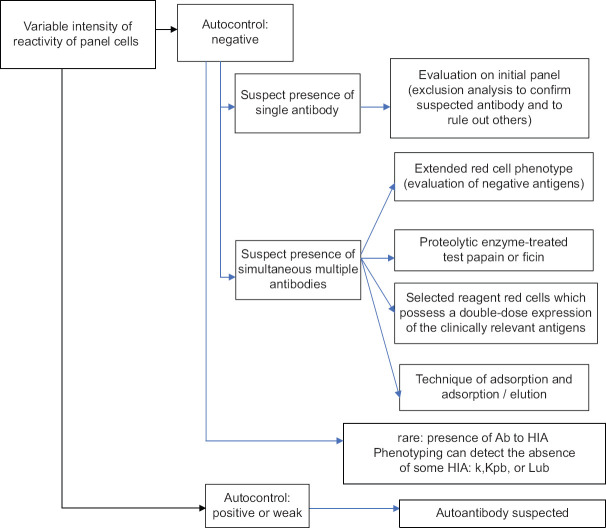
When all reagent red cell samples are positive with difference in the strengths of reactivity, and the autocontrol is negative, that suggests the possible presence of simultaneous multiple alloantibodies [Figure 1].
Figure 1.
Antibody identification in the case of panagglutination in indirect antiglobulin test with difference in the strength of reactivity of panel cells
For the separation and identification of alloantibodies, the following actions can be performed:
Complete patient's red cell phenotype of clinically significant antigens (evaluation of negative antigens)
Use of enzyme-treated test red cells such as papain and ficin (the inhibition of expression of some red cell antigens such as MNS/Duffy can help in the separation of antibodies)
Testing of the serum by means of reagent red cells which express in homozygous form the clinically relevant antigens (amplification of weakly expressed antibodies – the serologic phenomenon called “dosage” which is most commonly demonstrated in the Rh, Duffy, MNS, and Kidd systems)
-
Methods of adsorption and adsorption/elution (the adsorption of serum with known red cell phenotype allows the separation and identification of antibodies)
- For example, if a patient has produced anti-e and possible anti-S, it may be necessary to adsorb the anti-e onto ee/S (−) phenotype reagent red cells to remove the anti-e, which then it allows anti-S to be identified from the adsorbed serum.
-
Methods of combined adsorption-elution which consist of first incubating serum with selected red cells and then eluting antibody from the adsorbing red cells (they can be used to separate a mixture of antibodies in a single serum sample, detect weakly expressed antigens on red cells, or help identify weakly reactive antibodies)
- For example, if a patient has produced anti-c, anti-Kell, and possible anti-Jka, his serum absorption with reagent red cells phenotype CC/Kell (−)/Jka (+) will remove the anti-Jka which can be identified by elution from the absorbing red cells).
Another possibility is the presence of antibody to high-incidence antigen which reacts differently to panel cells. This is a rare occurrence which often manifests itself with the same degree of positivity in the different samples of the identification panel.
Similar Intensity of Reactivity
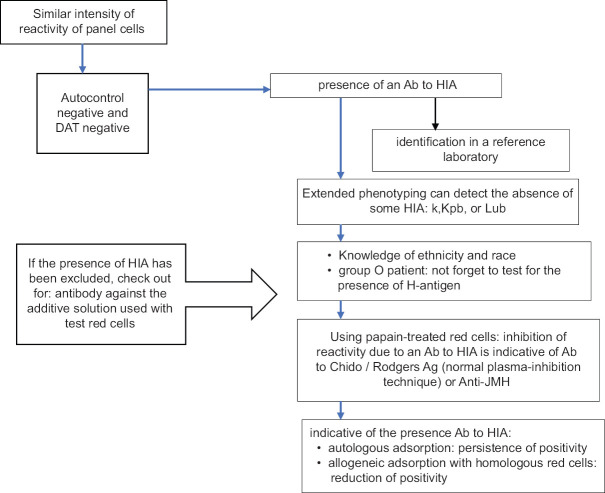
The techniques used aim at the differential diagnosis of autoantibody and antibody against high-frequency antigen. Performing autocontrol (testing the patient's serum with autologous red cells) allows a differential diagnosis since positive autocontrol is a manifestation of autoantibody, while the opposite suggests the existence of antibody to high-incidence antigen [Figures 2 and 3].
Figure 2.
Antibody identification in the case of panagglutination in indirect antiglobulin test with no difference in the strength of reactivity of panel cells and negative autocontrol
Figure 3.
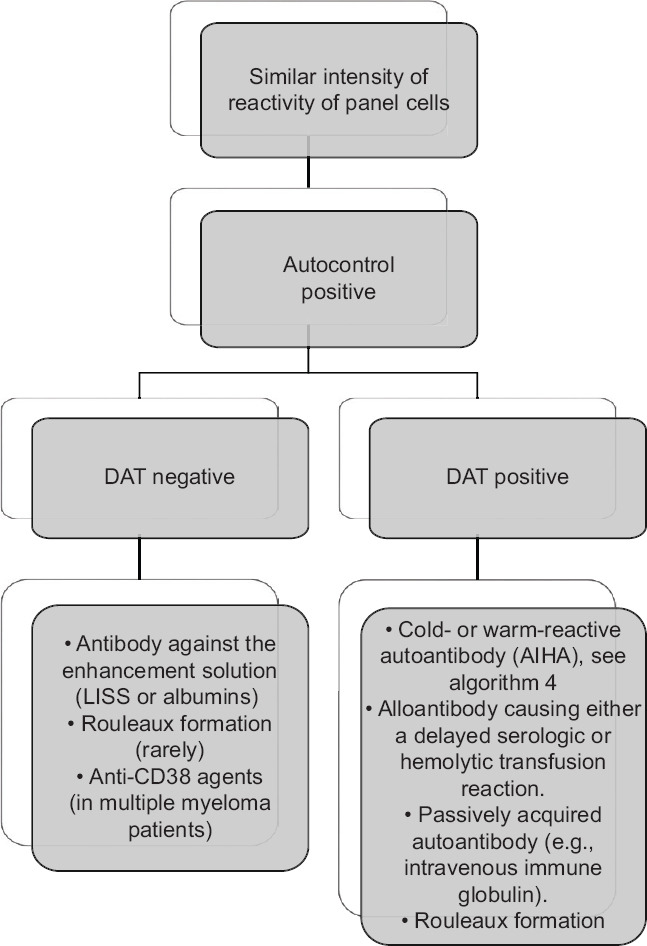
Causes * panagglutination in indirect antiglobulin test with no difference in the strength of reactivity of panel cells and negative autocontrol (*Causes depend on serologic methods used)
Antibodies to High-Incidence Antigens
For the identification of an antibody to high-incidence antigen, testing needs to take place in a reference laboratory; however, prior to this, some ancillary actions may be undertaken.
The full red cell phenotype can confirm the absence of some high-incidence antigens (such as k, Kpb, and Lub), while there is some additional information which accompanies the panels and which mentions the phenotype of selected reagent red cells for some high-incidence antigens.[6,7,8,9] Knowledge of ethnicity and race may be indicative of the absence of some high-incidence antigens, while we must not forget to test for the presence of H-antigen in each group O patient who manifests panagglutination, in order to rule out the rare case of Bombay phenotype with anti-H antibody in the patient serum. The inhibition of reactivity due to an antibody to high-incidence antigen using papain-treated red cells is indicative of antibody to Chido/Rodgers antigens (CH/RG, confirmed by means of normal plasma inhibition technique) or to John Milton Hagen antigen, known as high titer low avidity (HTLA).[10,11,12]
Finally, autologous adsorption and allogeneic adsorption with homologous red cells can be used to confirm the presence of an antibody to high-incidence antigen. Namely, the persistence of positivity after autologous adsorption and positivity reduction after allogeneic adsorption are indicative of the presence of antibody to high-incidence antigen.[1,2]
The persistence of positivity after autologous adsorption and after allogeneic adsorption can suggest two possibilities. The first is the presence of an anti-HTLA, particularly if sera continue to react at four dilutions beyond that which gives a 1+ reaction. Although knowing the specificity of such an antibody itself is not determinant for transfusion security, it may mask underlying alloantibodies with potentially clinical significance. In this case, plasma inhibition is performed to distinguish anti-CH/RG. The second possibility suggested by this pattern is the presence of a high-titer alloantibody without low avidity. Thus, the technique of allogeneic adsorption can be used to exclude the coexistence of another alloantibody in the presence of anti-HFA. In case of nonclarification, a sample of patient serum for further testing can be sent to a reference laboratory, which can provide consultation and assistance.
Autoantibodies
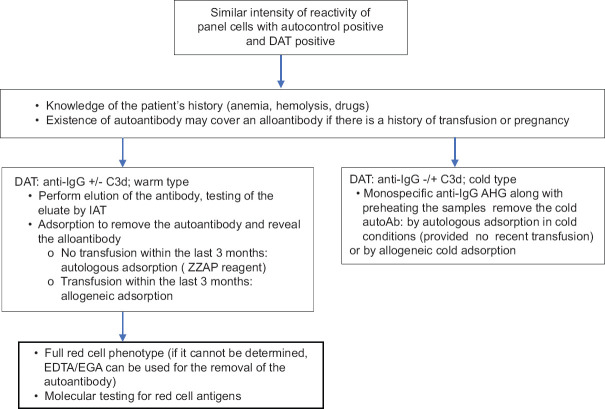
The presence of a positive autocontrol along with panagglutination in the screening and panel is evidence of the existence of autoantibodies. The follow-up actions are aimed at confirming the existence of autoantibody and at revealing a possible alloantibody which is covered by the autoantibody.[4]
Knowledge of the patient's history is essential, while it is also vital that a direct Coombs (DAT) using polyspecific antiglobulin serum is performed. In the event of DAT positivity, analysis using monospecific antiglobulin serum needs to be performed to identify the presence of warm or cold autoantibody.[4,5]
In the case of anti-immunoglobulin (IgG) ± C3d, the autoantibody is usually of the warm type. Confirmation of the presence of the antibody is done through elution of the antibody and through testing of the resulting eluate by IAT (which shows panagglutination). To test for the co-existence of alloantibodies, the transfusion history of the patient will determine further actions.[13,14] If the patient has not been transfused within the last 3 months, the autoantibody will be removed by means of autologous adsorption (the processing of red cells with ZZAP reagent) while allogeneic adsorption will be carried out if the patient has undergone transfusion.[15] The full red cell phenotype of clinically significant antigens may help in the identification of alloantibodies but may not be reliable in the presence of a warm autoantibody due to positive controls. To solve this problem, reagents that do not require the use of polyspecific antiglobulin serum can be used, or red blood cells can be processed with EGA (EDTA glycine-acid) for the removal of the autoantibody. These red cells can also be used for blood group testing with the classical methods, in case the blood group cannot be identified. Furthermore, in this case, the detection of red cell antigens by molecular testing may be useful [Figure 4].
Figure 4.
Investigation of autoantibodies (similar intensity of reactivity of panel cells with positive autocontrol and positive DAT)
A delayed hemolytic reaction from an antibody against a high-incidence antigen could initially produce similar laboratory findings to a warm antibody. In the differential diagnosis, the following things should be taken into consideration: that in the former condition, the patient has a recent transfusion history, that the symptoms are milder, and that this condition is usually self-limiting.
If the DAT is positive only with the anti C3d monospecific antihuman globulin (AHG), this means that the autoantibody is a cold-type immunoglobulin M. They are usually benign anti-I-specific cold antibodies which have a low titer, which act at temperatures of 4°C–24°C and which react more strongly with enzyme-treated red cells. If there is an activation of the complement following the interaction of the serum with reagent red cells, the cold antibodies may react at 37°C due to the use of polyspecific AHG which is used in pretransfusion procedures. In this case, the coexistence of clinically significant alloantibodies should be ruled out. The use of monospecific anti-IgG AHG along with preheating the samples could solve the problem. Alternative options are to remove the cold autoantibody either by autologous adsorption in cold conditions (provided there has not been a recent transfusion) or by allogeneic cold adsorption, or adsorption with rabbit erythrocytes or rabbit erythrocyte stroma.
Special Cases
There are certain specific conditions which may manifest panagglutination, such as antibodies against enhancement solutions, treatment using daratumumab (anti-CD38 monoclonal antibody) for multiple myeloma, and agglutinations due to the presence of paraprotein or in the administration of macromolecules such as intravenous immunoglobulin (IVIG) or volume expanders (such as dextrans, gelatin derivatives, hydroxyethyl starch, and human albumin solutions).
This type of antibodies has no clinical significance because they do not cause hemolysis. However, they can create panagglutination in the pretransfusion tests and they may mask the existence of a clinically significant alloantibody. The image of these antibodies may resemble that of the autoantibody or antibody to high-incidence antigen. Autocontrol and DAT can facilitate the differential diagnosis.
A panagglutination image with positive autocontrol and negative DAT suggests the presence of an antibody against the enhancement solution (in some Low-Ionic-Strength Solution (LISS) additives or albumins). To get around this problem, we could use a different enhancement solution or perform the pretransfusion tests with another company's reagents.
The presence of panagglutination with negative autocontrol and negative DAT suggests the presence of an antibody against the additive solution used with test red cells [Figure 2]. In this case, we need to perform a differential diagnosis to make sure that this is not a case of an antibody to high-incidence antigen. If the mixing of the additive solution of the reagent red cells in the autocontrol results in a positive reaction, that suggests the presence of an antibody against the additive solution. This problem could be solved by washing the test red cells and by performing tests with another company's reagents.
The daratumumab (anti-CD38 monoclonal antibody) is administered in relapsing and resistant multiple myeloma.[16,17,18] The binding of daratumumab to CD38 on the surface of the reagent red cells used for the IAT and the panel results in an image of panagglutination and a difficulty in detecting clinically significant alloantibodies. To get around this difficulty, the most popular technique used is the treatment of test red cells with dithiothreitol (DTT) which denatures CD38 in test red cells and does not allow daratumumab to bind. On the other hand, the above technique also denatures other erythrocyte antigens, most notably the Kell system. For this reason, the transfusion of patients with Kell-negative red blood cells is recommended. Should DTT be unavailable, an alternative would be to perform a full red cell phenotype prior to the administration of the drug and then to perform any transfusions required in accordance with negative antigens. Recently, there is commercially available reagent such as DARAEX which does not have side effects such as destruction of blood group antigens or hemolysis as described for the standard DTT treatment.[19]
The presence of paraprotein can cause agglutination in the blood group test, in IAT, and in the autocontrol. The problem can be resolved in the following ways: washing the reds to perform forward group, adding normal saline to dissolve the false agglutinations in the reverse group, and performing the IAT using a classic tube technique.
Drugs are known to cause antibody identification problems. Administration of IVIG and Rh immune globulin (RhIG) can interfere with antibody screening tests. Some lots of IVIG have been reported to contain unexpected antibodies, including anti-A and anti-B.[20] It has been reported that IVIG can induce immune hemolysis due to anti-A or anti-B antibodies. Intravenous RhIG, which is sometimes used to treat thrombocytopenia, could explain the presence of anti-D in an RhD-positive patient.
Conclusion
Panagglutination in IAT is a complex and often hard-to-solve problem in pretransfusion blood testing. Being methodical, thinking logically, and making the right choice among the various techniques at our disposal should, most of the time, lead to satisfactory solutions and eventually to safe transfusions which is the ultimate objective.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Er LS, Bailey DJ. Identification of antibodies to red cell antigens. In: Cohn CS, editor. Technical Manual. 20th. Bethesda (MD): AABB; 2020. pp. 389–428. [Google Scholar]
- 2.Bishop S, Trudell KS. Detection and identification of antibodies. In: Denise Harmening., editor. Modern Blood Banking & Transfusion Practices. 7th. Chicago, Illinois, USA: F. A. Davis Company; 2019. pp. 232–55. [Google Scholar]
- 3.Chiaroni J, Gouvitsos J, Dettori I, Ferrera V. How we evaluate panagglutinating sera. Transfusion. 2009;49:1540–5. doi: 10.1111/j.1537-2995.2009.02183.x. [DOI] [PubMed] [Google Scholar]
- 4.Yürek S, Mayer B, Almahallawi M, Pruss A, Salama A. Precautions surrounding blood transfusion in autoimmune haemolytic anaemias are overestimated. Blood Transfus. 2015;13:616–21. doi: 10.2450/2015.0326-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zantek ND, Koepsell SA, Tharp DR, Jr., Cohn CS. The direct antiglobulin test: A critical step in the evaluation of hemolysis. Am J Hematol. 2012;87:707–9. doi: 10.1002/ajh.23218. [DOI] [PubMed] [Google Scholar]
- 6.Lomas-Francis C. Clinical significance of antibodies to antigens in the International Society of Blood Transfusion collections, 700 series of low-incidence antigens, and 901 series of high-incidence antigens. Immunohematology. 2018;34:39–45. [PubMed] [Google Scholar]
- 7.Crottet SL. Clinical significance of antibodies to antigens in the Scianna, Dombrock, Colton, Landsteiner-Weiner, Chido/Rodgers, H, Kx, Cromer, Gerbich, Knops, Indian, and Ok blood group systems. Immunohematology. 2018;34:103–8. [PubMed] [Google Scholar]
- 8.Moulds MK. Antibodies to high-incidence antigens. Transfus Apher Sci. 2009;40:203–4. doi: 10.1016/j.transci.2009.03.014. [DOI] [PubMed] [Google Scholar]
- 9.Hoppe B, Pastucha L, Seltsam A, Greinacher A, Salama A. Acute haemolytic transfusion reactions due to weak antibodies that in vitro did not seem to be clinically significant. Vox Sang. 2002;82:207–10. doi: 10.1046/j.1423-0410.2002.00171.x. [DOI] [PubMed] [Google Scholar]
- 10.Rolih SD. High-titer, low-avidity (HTLA) antibodies and antigens: A review. Transfus Med Rev. 1989;3:128–39. doi: 10.1016/s0887-7963(89)70074-2. [DOI] [PubMed] [Google Scholar]
- 11.Mudad R, Rao N, Issitt PD, Roy RB, Combs MR, Telen MJ. JMH variants: Serologic, clinical, and biochemical analyses in two cases. Transfusion. 1995;35:925–30. doi: 10.1046/j.1537-2995.1995.351196110897.x. [DOI] [PubMed] [Google Scholar]
- 12.Das S, Priyamvada PS, Basavarajegowda A, Mathur A. Deciphering a delayed hemolytic transfusion reactions nightmare – Case of Chido/Roger antibodies. Asian J Transfus Sci. 2019;13:132–5. doi: 10.4103/ajts.AJTS_152_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jang MJ, Cho D, Park KU, Yazer MH, Shin MG, Shin JH, et al. Autoantibodies with mimicking specificity detected by the dilution technique in patients with warm autoantibodies. Ann Lab Med. 2013;33:343–8. doi: 10.3343/alm.2013.33.5.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Park SH, Choe WH, Kwon SW. Red blood cell transfusion in patients with autoantibodies: Is it effective and safe without increasing hemolysis risk? Ann Lab Med. 2015;35:436–44. doi: 10.3343/alm.2015.35.4.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chiaroni J, Touinssi M, Mazet M, De Micco P, Ferrera V. Adsorption of autoantibodies in the presence of LISS to detect alloantibodies underlying warm autoantibodies. Transfusion. 2003;43:651–5. doi: 10.1046/j.1537-2995.2003.00356.x. [DOI] [PubMed] [Google Scholar]
- 16.Quach H, Benson S, Haysom H, Wilkes AM, Zacher N, Cole-Sinclair M, et al. Considerations for pre- τransfusion immunohaematology testing in patients receiving the anti-CD38 monoclonal antibody daratumumab for the treatment of multiple myeloma. Intern Med J. 2018;48:210–20. doi: 10.1111/imj.13707. [DOI] [PubMed] [Google Scholar]
- 17.Werle E, Ziebart J, Wasmund E, Eske-Pogodda K. Daratumumab interference in pretransfusion testing is overcome by addition of daratumumab fab fragments to patients' plasma. Transfus Med Hemother. 2019;46:423–30. doi: 10.1159/000495773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lancman G, Arinsburg S, Jhang J, Cho HJ, Jagannath S, Madduri D, et al. Blood transfusion management for patients treated with anti-CD38 monoclonal antibodies. Front Immunol. 2018;9:2616. doi: 10.3389/fimmu.2018.02616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tenorio M, Jiménez GM, Gutiérrez VG, Jiménez A, Blanchard MJ, Vallés A, et al. Validation of daraex to resolve daratumumab-induced interferences in pre-transfusion screen tests. Blood. 2019;134(Suppl 1):4983. [Google Scholar]
- 20.Desborough MJ, Miller J, Thorpe SJ, Murphy MF, Misbah SA. Intravenous immunoglobulin-induced haemolysis: A case report and review of the literature. Transfus Med. 2014;24:219–26. doi: 10.1111/tme.12083. [DOI] [PubMed] [Google Scholar]