Key Points
Question
What is the efficacy of problem-solving treatment (PST) for veterans with Gulf War illness?
Findings
This randomized clinical trial of 268 veterans found no differences between PST and health education in reduction in disability at the end of the intervention (primary outcome). Results suggested that PST reduced problem-solving impairment (moderate effect, 0.42) and disability at follow-up (moderate effect, 0.39) compared with control.
Meaning
In this trial, PST did not improve the primary outcome compared with health education but improved some outcomes and was acceptable to veterans with Gulf War illness.
This randomized clinical trial of veterans with Gulf War illness examines whether problem-solving treatment is efficacious in reducing disability and problem-solving impairment.
Abstract
Importance
Few evidence-based treatments are available for Gulf War illness (GWI). Behavioral treatments that target factors known to maintain the disability from GWI, such as problem-solving impairment, may be beneficial. Problem-solving treatment (PST) targets problem-solving impairment and is an evidence-based treatment for other conditions.
Objective
To examine the efficacy of PST to reduce disability, problem-solving impairment, and physical symptoms in GWI.
Design, Setting, and Participants
This multicenter randomized clinical trial conducted in the US Department of Veterans Affairs compared PST with health education in a volunteer sample of 511 Gulf War veterans with GWI and disability (January 1, 2015, to September 1, 2019); outcomes were assessed at 12 weeks and 6 months. Statistical analysis was conducted between January 1, 2019, and December 31, 2020.
Interventions
Problem-solving treatment taught skills to improve problem-solving. Health education provided didactic health information. Both were delivered by telephone weekly for 12 weeks.
Main Outcomes and Measures
The primary outcome was reduction from baseline to 12 weeks in self-report of disability (World Health Organization Disability Assessment Schedule). Secondary outcomes were reductions in self-report of problem-solving impairment and objective problem-solving. Exploratory outcomes were reductions in pain, pain disability, and fatigue.
Results
A total of 268 veterans (mean [SD] age, 52.9 [7.3] years; 88.4% male; 66.8% White) were randomized to PST (n = 135) or health education (n = 133). Most participants completed all 12 sessions of PST (114 of 135 [84.4%]) and health education (120 of 133 [90.2%]). No difference was found between groups in reductions in disability at the end of treatment. Results suggested that PST reduced problem-solving impairment (moderate effect, 0.42; P = .01) and disability at 6 months (moderate effect, 0.39; P = .06) compared with health education.
Conclusions and Relevance
In this randomized clinical trial of the efficacy of PST for GWI, no difference was found between groups in reduction in disability at 12 weeks. Problem-solving treatment had high adherence and reduced problem-solving impairment and potentially reduced disability at 6 months compared with health education. These findings should be confirmed in future studies.
Trial Registration
ClinicalTrials.gov Identifier: NCT02161133
Introduction
Persistent, medically unexplained physical symptoms disproportionately burden individuals exposed to war.1,2 As many as 30% of military veterans of the Persian Gulf War (1990-1991) developed chronic disabling symptoms, collectively referred to as chronic multisymptom illness or Gulf War illness (GWI).1,2,3
The 2021 Clinical Practice Guidelines for the Management of Chronic Multisymptom Illness recommend cognitive behavioral treatment4,5,6 based on a clinical trial among veterans with GWI and indirect evidence from multiple trials for related conditions.7 More direct evidence is needed to support the efficacy of behavioral treatments that target mechanisms relevant for GWI and are acceptable to veterans.4,8,9 Developing acceptable treatments for GWI is critical because nonspecific treatments may not be acceptable to veterans who fought to legitimize GWI.10,11
One factor known to maintain the disability of GWI is impairment in problem-solving ability, an executive function defined as the ability to find solutions to problems without an easily identified solution.12,13 Impairment in problem-solving increases disability because it makes it difficult to overcome problems that affect daily activities14 and effectively manage chronic conditions, such as GWI.15 Problem-solving treatment (PST) is a cognitive behavioral treatment that remediates problem-solving impairment for other conditions (eg, traumatic brain injury).16,17 We performed a randomized clinical trial to examine the efficacy of telephone-delivered PST compared with an active control, telephone-delivered health education (HE), for reducing the disability and problem-solving impairment of veterans with GWI.
Methods
Procedure
This randomized clinical trial, conducted between January 1, 2015, and September 1, 2019, was a parallel-group, individually randomized trial with 1:1 allocation that compared telephone-delivered PST with telephone-delivered HE.18 Veterans with GWI were recruited nationwide with emphasis on local recruitment at the 3 study sites, each with local institutional review board approval. Veterans were screened via telephone to determine eligibility. Eligible veterans provided written informed consent. Near the end of the study, veterans who were unable to travel to 1 of the 3 sites could be mailed the written consent form. Research personnel at the primary site conducted all treatment sessions. Treatment was telephone delivered because disability from GWI can make in-person appointments difficult, and substantial research supports the efficacy of telephone-delivered behavioral treatments.19,20,21 The trial ended when sample size was reached. This clinical trial follows the Consolidated Standards of Reporting Trials (CONSORT) reporting guideline, and no changes to the outcomes, assessments, inclusion criteria, or treatments were made after the start of data collection.22 The full trial protocol can be found in Supplement 1.
Participants
Participants were included if they were deployed to the Persian Gulf War (August 1990 to November 1991), met the Kansas definition for GWI,2 and scored at least half an SD worse than the mean on the World Health Organization Disability Assessment Schedule (WHODAS 2.0).23 Participants were excluded if they had current suicidal or homicidal intent or plan, schizophrenia or current psychotic symptoms, a disability that would preclude telephone treatment, or self-reported diagnosis of a degenerative brain disorder or serious psychiatric or medical illness that could limit generalizability of the findings, limit safety, or account for the symptoms of GWI.
Problem-solving Treatment
Telephone-delivered PST included 12 one-hour sessions using a workbook and was modeled after established PSTs and tailored for veterans with GWI.16,24 Veterans were taught how to develop a positive mindset around problem-solving (“I can solve problems”). Veterans were also taught a 5-step approach to problem-solving. Veterans were supported to increase participation in activities of their choosing. Materials for both treatments are available from the corresponding author.
Health Education
The active control, telephone-delivered HE, included 12 sessions lasting up to 1 hour (typically approximately 40 minutes) using a workbook and was modeled after HE provided in a US Department of Veterans Affairs (VA) specialty clinic.25 Sessions were highly structured and emphasized the learning of key health concepts. Study practitioners did not provide behavioral change support.
Study Practitioners
Study practitioners delivered both interventions and were licensed mental health practitioners or postdoctoral trainees. These practitioners trained for at least 3 days and received peer group (2 times per week) and individual (once per week) supervision. Supervision focused on practitioner competency, adherence to both treatments, and treatment differentiation and included listening to taped sessions, reviewing treatment manuals, and discussing cases. Training included listening to taped sessions, reviewing treatment manuals, and discussing cases.
Treatment Fidelity
The PST and HE sessions were audiorecorded. We developed fidelity instruments to code sessions for fidelity to session-specific content (range, 0-100%). Selected HE sessions were coded with the PST fidelity instrument to ensure sessions did not include elements of PST. Multiple coders discussed coding inconsistencies until they reached agreement.
Randomization
Participants were randomized to PST or HE (1:1 ratio) using an urn randomization procedure in which matching was based on disability level and sex at each study site to ensure equitable distribution between groups.26 The statistician (S.-E.L.) generated the randomization sequence, and the study coordinator assigned participants to interventions.
Assessment Methods
Throughout the study, assessments could be completed in person, by mail, or over the telephone, and participants were compensated for completing the assessments. Veterans who were mailed the written consent form did not complete the neuropsychological assessment, because it had to be completed in person (n = 26). Veterans were assessed at baseline, 4 weeks, 12 weeks, and 6 months. Assessors and investigators were blinded to randomization.
Outcome Measures
The primary outcome was reduction in disability score (WHODAS 2.0) between baseline and 12 weeks; a secondary outcome was reduction in WHODAS 2.0 score between baseline and 6 months. The WHODAS 2.0 measures disability attributable to health conditions23 and reflects 2 underlying constructs: activity limitations and participation deficits. Higher scores indicate more disability (range, 1-100). The 12-item measure was used at screening23 and the 36-item measure at 4 weeks, 12 weeks, and 6 months. Additional secondary outcome measures were reductions in self-reported problem-solving impairment between baseline and 12 weeks and between baseline and 6 months with the Problem Solving Inventory,27 where higher scores indicate greater problem-solving impairment (range, 32-192). Reduction in objective problem-solving impairment between baseline and 12 weeks was assessed with a composite score (mean z scores) of performance on a Stroop Color and Word Test (standardized interference score),28 Trail Making Test B standardized score,29 Halstead Category Test–Russell revised,30 and Conners Continuous Performance Test 3 days’ standardized score.31 Lower scores indicate greater problem-solving impairment.
Our a priori exploratory outcomes were reduction between baseline and 12 weeks in the Multidimensional Pain Inventory 3-item pain scale (higher scores indicate greater pain; range, 0-18), the Pain Disability Index (higher scores indicate greater disability; range, 0-70),32 and the Fatigue Severity Scale (higher scores indicate greater fatigue severity; range, 9-63).33 The 6-month pain and fatigue outcomes were not registered but are provided here for context. Participants also completed a short assessment of treatment satisfaction.34
Participant Characterization
The Kansas definition of GWI requires that veterans endorse moderately severe and/or multiple symptoms that started during or after the Gulf War in at least 3 of 6 domains: fatigue; pain; neurologic, cognitive, or mood; skin; gastrointestinal; and respiratory.2 Patients with chronic conditions (eg, cancer) that can have diverse symptoms or interfere with respondents’ ability to accurately report their symptoms (eg, psychosis) are excluded.2 To improve generalizability in this aging population, we only excluded participants with a disorder that could clearly account for the symptoms of GWI (eg, multiple sclerosis). Participants also completed the Posttraumatic Checklist,35 the Patient-Health Questionnaire depression subscale,36 and demographic questions, with race and ethnicity classified by the veteran using predefined options (American Indian, Asian, Black, Latinx, Native Hawaiian, White, >1 race or ethnicity, or unknown) to characterize the sample.
Sample Size
We powered the study to test an effect size Cohen d of 0.38 based on a prior clinical trial of older patients with depression37 and the assumption that the intraparticipant correlation between the baseline and end of treatment assessment would be approximately 0.5. These assumptions led to a sample size estimate of 109 participants per group to test an effect size Cohen d = 0.38 with 80% power and α = .05 (2-sided). After accounting for approximately 15% attrition, we planned to recruit 129 participants per group, 258 in total.
Statistical Analysis
The primary statistical analysis was conducted between January 1, 2019, and December 31, 2020, with additional sensitivity analysis conducted in 2022. Analyses were performed on an intention-to-treat basis following our protocol and trial registry. Statistical significance was set at a 2-sided P < .05. We calculated means (SDs) and compared baseline demographic variables, depression, and posttraumatic stress symptoms between groups to determine the need for any covariates in the analysis for preexisting group differences. No differences required control.
We analyzed the data using a repeated mixed-model analysis, with participants nested within therapist, which was modeled as a random effect. In the first model, the WHODAS 2.0 summary score was treated as the dependent variable, and treatment assignment (PST vs HE), time (baseline, 4 weeks, 12 weeks, and 6-month follow-up) and treatment × time interactions were modeled as fixed effects. Linear contrasts were constructed to evaluate the reduction in disability for each treatment and between treatments at 12 weeks (primary end point) and 6 months (secondary end point). The same mixed-model analysis strategy was applied to address our secondary outcome of problem-solving impairment (self-reported and objective) and our planned exploratory analyses. We report the effect size (Cohen d) for each outcome.
Mixed-model analysis was used to assess whether PST produced greater reduction in disability through its effect on reducing problem-solving impairment. The indirect effect of self-reported problem-solving impairment was tested using the CI approach.38 A 97.5% CI was constructed for each indirect effect at 12 weeks and 6 months, after Bonferroni adjustment. If 0 was not included in the 97.5% CI, we considered the mediational relationship to be established. We also calculated the proportion of the total effect that was accounted for by the indirect effect (proportion mediated [PM]) at 12 weeks and 6 months.
To address missing data, we conducted sensitivity analyses using baseline and multiple imputations.39 Baseline imputation assumes that individuals with missing outcome variables at follow-up returned to baseline values. Thus, baseline imputation imputes the missing values of each outcome with the patient’s baseline values. For multiple imputation, we assumed missing at random39 and used the Markov chain Monte Carlo approach to impute missing data. Ten imputed data sets were generated using PROC MI in SAS software, version 9.4 (SAS Institute Inc).40 Analyses were performed on each imputed data set, with combined estimates calculated using the Rubin rule. PROC Mixed in SAS software, version 9.4 (SAS Institute Inc) was used to perform the mixed-model analysis.
Results
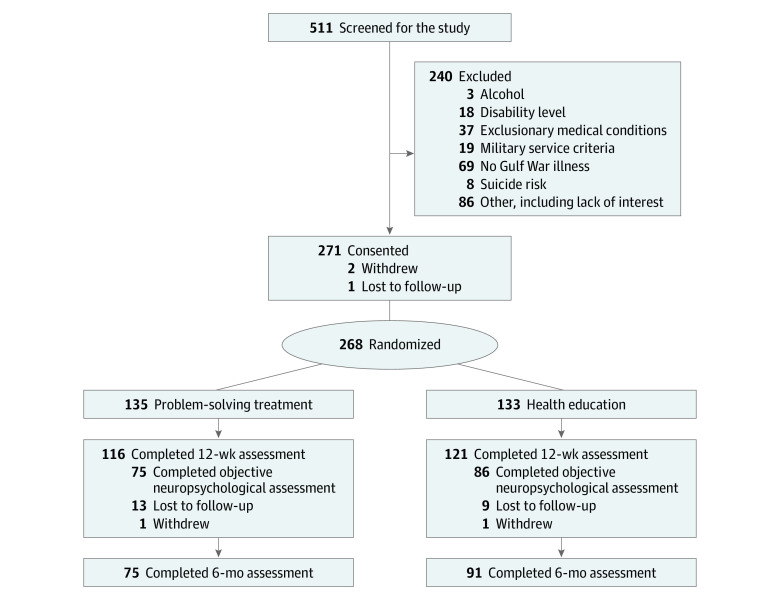
We screened 511 veterans, of whom 268 were randomized to PST (n = 135) or health education (n = 133) treatment (Figure). Participants’ mean (SD) age was 52.9 (7.3) years; 237 were male (88.4%) and 31 female (11.6%); 12 were American Indian (4.5%), 3 were Asian (1.1%), 63 were Black (23.5%), 18 were Latinx (6.6%), 1 was Native Hawaiian (0.4%), 179 were White (66.8%), 8 were of more than 1 race or ethnicity (3.0%), and 2 were of unknown race or ethnicity (0.7%). Our sample was generally demographically representative of the population of Gulf War veterans (Table 1 and Table 2).
Figure. Study Flow Diagram.
Table 1. Characterization of Participants at Baselinea.
| Characteristic | Total sample (N = 268) | Problem-solving treatment group (n = 135) | Health education group (n = 133) |
|---|---|---|---|
| Age, mean (SD), y | 52.9 (7.3) | 53.1 (7.6) | 52.8 (7.0) |
| Sex | |||
| Female | 31 (11.6) | 15 (11.1) | 16 (12.0) |
| Male | 237 (88.4) | 120 (88.9) | 117 (88.0) |
| Race and ethnicity | |||
| American Indian | 12 (4.5) | 6 (4.4) | 6 (4.5) |
| Asian | 3 (1.1) | 2 (1.5) | 1 (0.8) |
| Black | 63 (23.5) | 30 (22.2) | 33 (24.8) |
| Latinx | 18 (6.6) | 9 (6.7) | 9 (6.8) |
| Native Hawaiian | 1 (0.4) | 1 (0.7) | 0 |
| White | 179 (66.8) | 91 (67.4) | 88 (66.2) |
| >1 Race or ethnicity | 8 (3.0) | 5 (3.7) | 3 (2.3) |
| Unknownb | 2 (0.7) | 0 | 2 (1.5) |
| Posttraumatic Checklist score, mean (SD) | 36.6 (19.6) | 37.0 (20.0) | 36.2 (19.2) |
| Patient-Health Questionnaire depression subscale score, mean (SD) | 11.9 (5.7) | 11.2 (5.6) | 12.4 (5.8) |
Data are presented as number (percentage) of patients unless otherwise indicated.
Veteran self-report of unknown.
Table 2. Effects Within the Treatment Groups.
| Measure | Mean (SE) scores | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Problem-solving treatment | Health education | ||||||||||||
| Baseline | 4 wk | 12 wk | 6 mo | Change, baseline to 12 wk | Change, baseline to 6 mo | Baseline | 4 wk | 12 wk | 6 mo | Change, baseline to 12 wk | Change, baseline to 6 mo | ||
| Disabilitya | 46.7 (1.9) | 42.5 (2.0) | 43.9 (2.0) | 44.1 (2.2) | −2.8 (1.2) | −2.6 (1.5) | 45.1 (1.9) | 44.6 (2.0) | 42.8 (2.0) | 46.2 (2.1) | −2.2 (1.1) | 1.1 (1.3) | |
| Self-reported problem-solving impairmentb | 96.8 (2.5) | 94.3 (2.6) | 84.1 (2.6) | 89.7 (2.9) | −12.7 (1.8) | −7.0 (2.1) | 98.0 (2.5) | 95.5 (2.6) | 91.5 (2.6) | 98.3 (2.7) | −6.5 (1.7) | 0.3 (1.9) | |
| Objective problem-solvingc | 47.8 (0.4) | NA | 48.4 (0.5) | NA | 0.8 (0.5) | NA | 47.5 (0.4) | NA | 48.8 (0.5) | NA | 1.4 (0.4) | NA | |
| Paind | 3.7 (0.1) | NA | 3.7 (0.1) | 3.7 (0.2) | 0.0 (0.1) | 0.0 (0.1) | 3.6 (0.1) | NA | 3.5 (0.1) | 3.6 (0.2) | −0.1 (0.1) | 0.1 (0.1) | |
| Pain disabilitye | 35.2 (1.5) | NA | 33.2 (1.6) | 37.1 (1.8) | −2.1 (1.1) | 1.8 (1.4) | 35.1 (1.5) | NA | 34.4 (1.6) | 38.3 (1.7) | −0.7 (1.1) | 3.2 (1.3) | |
| Fatiguef | 48.3 (1.3) | NA | 45.5 (1.3) | 46.2 (1.5) | −2.7 (1.0) | −2.1 (1.2) | 46.5 (1.3) | NA | 45.7 (1.3) | 45.9 (1.4) | −0.8 (1.0) | −0.6 (1.1) | |
Abbreviation: NA, not applicable.
Self-reported disability was assessed with the World Health Organization Disability Assessment Schedule 2.0. Higher scores indicate more disability (range, 1-100). Primary outcome was disability at 12 weeks.
Self-reported problem-solving impairment was assessed with the Problem Solving Inventory. Higher scores indicate greater problem-solving impairment (range, 32-192).
Objective problem-solving impairment was assessed with a composite score (mean z scores) of performance on a Stroop Color and Word Test, Trail Making Test B, Halstead Category Test–Russell revised, and Conners Continuous Performance Test. Lower scores indicate greater problem-solving impairment.
Pain was assessed with the Multidimensional Pain Inventory 3-item pain scale. Higher scores indicate greater pain (range, 0-18).
Pain disability was assessed with Pain Disability Index. Higher scores indicate greater disability (range, 0-70).
Fatigue was assessed with the Fatigue Severity Scale. Higher scores indicate greater fatigue severity (range, 9-63).
Ten percent of veterans (n = 28) were randomly selected to have all their sessions coded for fidelity. There were 336 sessions and 4 were inaudible, resulting in 332 sessions being rated. The average fidelity to PST session-specific content (n = 167 sessions rated) was 97%. The average fidelity to HE session-specific content was 98%, and 99% of HE sessions were 100% differentiated from PST.
There was high adherence and satisfaction with the treatments. Adherence was similar between treatments (χ2 = 2.0; P = .16); 114 veterans (84.4%) randomized to PST attended all 12 sessions (mean [SD] number of sessions completed, 10.7 [3.3]), and 120 veterans (90.2%) randomized to HE attended all 12 sessions (mean [SD] number of sessions completed, 10.7 [3.3]). Satisfaction was similar for PST (mean [SD], 28.3 [1.8]) and HE (mean [SD], 28.0 [1.8]), with a mean (SD) difference between groups of 0.3 (0.3) (t = −1.4; P = .17). Veterans in this study had complex health concerns; 22 adverse events occurred in the PST group and 30 in the HE group. Three of the adverse events (increase in psychological symptoms in all 3) were considered potentially attributable to the study (1 in the PST group and 2 in the HE group).
Disability
The overall treatment × time interaction for disability (WHODAS 2.0) across time points (F3,569 = 2.62; P = .050) suggested that the changes in disability scores over time differed between PST and HE. The primary outcome was change in disability from baseline to 12 weeks. Both PST and HE had small reductions in disability at 12 weeks (PST: baseline mean [SE], 46.7 [1.9]; 12-week mean [SE], 43.9 [2.0]; Cohen d = 0.2, P = .02; HE: baseline mean [SE], 45.1 [1.9]; 12-week mean [SE], 42.8 [2.0]; Cohen d = 0.2, P = .051) (Table 2). No difference was found in disability reduction between treatments at 12 weeks (Cohen d = 0.1, P = .71) (Table 3), which suggested that PST did not reduce disability to a greater degree than HE at 12 weeks. This result was supported by sensitivity analyses (Table 4).
Table 3. Between-Treatment Group Effects: Intracorrelations for Therapist and Participant.
| Measure | Change in PST vs change in HE at 12 wk, mean (SE) | Effect size (Cohen d) | Change in PST vs change in HE at 6 mo, mean (SE) | Effect size (Cohen d) | Intracorrelationa | |
|---|---|---|---|---|---|---|
| Therapist | Participant | |||||
| Disabilityb | −0.6 (1.6) | 0.06 | −3.7 (2.0) | 0.4 | 0.01 | 0.79 |
| Self-reported problem-solving impairmentc | −6.2 (2.5) | 0.3 | −7.3 (2.9) | 0.4 | 0.00 | 0.79 |
| Objective problem-solvingd | −0.6 (0.6) | 0.1 | NA | NA | 0.00 | 0.64 |
| Paine | 0.1 (0.1) | 0.03 | −0.0 (0.2) | 0 | 0.00 | 0.77 |
| Pain disabilityf | −1.4 (1.6) | 0.1 | −1.4 (1.9) | 0.2 | 0.00 | 0.75 |
| Fatigueg | −1.9 (1.4) | 0.2 | −1.5 (1.6) | 0.2 | 0.00 | 0.77 |
Abbreviations: HE, health education; NA, not applicable; PST, problem-solving treatment.
Intratherapist and intraparticipant correlations were estimated using mixed-model analysis.
Self-reported disability was assessed with the World Health Organization Disability Assessment Schedule 2.0. Higher scores indicate more disability (range, 1-100). Primary outcome was disability at 12 weeks.
Self-reported problem-solving impairment was assessed with the Problem Solving Inventory. Higher scores indicate greater problem-solving impairment (range, 32-192).
Objective problem-solving impairment was assessed with a composite score (mean z scores) of performance on a Stroop Color and Word Test, Trail Making Test B, Halstead Category Test–Russell revised, and Conners Continuous Performance Test. Lower scores indicate greater problem-solving impairment.
Pain was assessed with the Multidimensional Pain Inventory 3-item pain scale. Higher scores indicate greater pain (range, 0-18).
Pain disability was assessed with the Pain Disability Index. Higher scores indicate greater disability (range, 0-70).
Fatigue was assessed with the Fatigue Severity Scale. Higher scores indicate greater fatigue severity (range, 9-63).
Table 4. Imputation Analyses.
| Variable | Imputation, mean (SE) | |||||||
|---|---|---|---|---|---|---|---|---|
| Multiple | Baseline | |||||||
| Change in PST vs change in HE at 12 wk | P value | Change in PST vs change in HE at 6 mo | P value | Change in PST vs change in HE at 12 wk | P value | Change in PST vs change in HE at 6 mo | P value | |
| Disabilitya | −0.1 (1.7) | .94 | −2.9 (1.8) | .11 | −0.4 (1.4) | .78 | −2.4 (1.1) | .04 |
| Self-reported problem-solving impairmentb | −6.0 (2.5) | .02 | −6.0 (3.0) | .045 | −5.3 (2.3) | .02 | −3.7 (1.7) | .03 |
| Objective problem-solvingc | −0.2 (0.6) | .72 | NA | NA | −0.3 (0.5) | .36 | NA | NA |
| Paind | 0.03 (0.1) | .81 | −0.04 (0.1) | .82 | 0.03 (0.1) | .79 | −0.02 (0.1) | .88 |
| Pain disabilitye | −1.06 (1.6) | .54 | −0.7 (2.1) | .72 | −1.0 (1.3) | .43 | −1.9 (1.2) | .21 |
| Fatiguef | −1.7 (1.5) | .24 | −1.5 (1.7) | .38 | −1.5 (1.2) | .18 | −0.8 (0.9) | .37 |
Abbreviations: HE, health education; NA, not applicable; PST, problem-solving treatment.
Self-reported disability was assessed with the World Health Organization Disability Assessment Schedule 2.0. Higher scores indicate more disability (range, 1-100). Primary outcome was disability at 12 weeks.
Self-reported problem-solving impairment was assessed with the Problem Solving Inventory. Higher scores indicate greater problem-solving impairment (range, 32-192).
Objective problem-solving impairment was assessed with a composite score (mean z scores) of performance on a Stroop color word test, Trail Making Test B, Halstead Category Test–Russell revised, and Conners Continuous Performance Test. Lower scores indicate greater problem-solving impairment.
Pain was assessed with the Multidimensional Pain Inventory 3-item pain scale. Higher scores indicate greater pain (range, 0-18).
Pain disability was assessed with the Pain Disability Index. Higher scores indicate greater disability (range, 0-70).
Fatigue was assessed with the Fatigue Severity Scale. Higher scores indicate greater fatigue severity (range, 9-63).
Reduction in disability at 6 months was a secondary outcome. The PST group had a small reduction in disability at 6-month follow-up (PST: baseline mean [SE], 46.7 [1.9]; 6-month mean [SE], 44.1 [2.2]; Cohen d = 0.24, P = .07), whereas the HE group had a slight increase in disability (HE: baseline mean [SE], 45.1 [1.9]; 12-week mean [SE], 46.2 [2.1]; Cohen d = 0.15, P = .39). A moderate difference in reduction in disability was found between treatments at 6 months (Cohen d = 0.39, P = .06), suggesting that the PST group maintained reductions in disability, whereas the HE group went back to near baseline levels. Sensitivity analyses with imputed data supported a possible difference between the treatments at 6 months (Table 4).
Problem-solving Impairment
The treatment × time interaction across time points was significant for self-reported problem-solving impairment (F3,580 = 4.12, P = .007), suggesting that changes in problem-solving impairment differed over time between the PST and HE groups. The PST group had a large reduction (Cohen d = 0.56, P < .001) (Table 2), whereas the HE group had a moderate reduction (Cohen d = 0.34, P < .001) in self-reported problem-solving impairment at 12 weeks. A moderate difference in reduction in self-reported problem-solving impairment was found between the treatments at 12 weeks (Cohen d = 0.33; P = .01) (Table 3), suggesting that PST resulted in greater reduction in self-reported problem-solving impairment compared with HE. This finding was supported by sensitivity analyses.
Problem-solving treatment led to a moderate reduction in self-reported problem-solving impairment at 6 months (Cohen d = 0.33, P = .001), whereas HE had no effect at 6 months (Cohen d = 0.07, P = .89). A moderate difference was found in reduction in self-reported problem-solving impairment between the treatments at 6 months (Cohen d = 0.42, P = .01), which suggested that PST maintained reductions in problem-solving impairment, whereas HE returned to near baseline levels. This suggestion was supported by sensitivity analyses.
The treatment × time interaction was not significant for objective problem-solving impairment (F1,165 = 0.75, P = .39), suggesting that changes in objective problem-solving impairment were similar between the PST and HE groups. The PST group had a small (Cohen d = 0.20, P = .07) and the HE group had a moderate (Cohen d = 0.31, P = .002) reduction in objective problem-solving impairment at 12 weeks (Table 2). Differences in reductions in objective problem-solving impairment between treatments at 12 weeks were similar (Cohen d = 0.09, P = .39) (Table 3), suggesting that PST did not reduce objective problem-solving impairment to a greater degree than HE. This outcome was supported by sensitivity analyses.
Mediational analysis showed that reduced self-reported problem-solving impairment mediated the relationship between PST and disability reduction (indirect effect, 1.55; 97.5% CI, 0.18-3.17; PM = 2.62 for 12 weeks; indirect effect, 1.90; 97.5% CI, 0.26-3.84; PM = 0.51 for 6 months). This finding suggests that reduced self-reported problem-solving impairment mediated disability reduction with PST.
Pain, Pain Disability, and Fatigue
No differences were found in reduction of pain, pain disability, or fatigue between treatments at 12 weeks or 6 months (Table 3). Sensitivity analyses also did not reveal any consistent differences on these outcomes between treatments at 12 weeks or 6 months (Table 4).
Discussion
The goal of this randomized clinical trial was to test whether PST would improve disability and problem-solving impairment in veterans with GWI compared with HE, an active control. We found no differences in the primary outcome, reductions in disability from baseline to 12 weeks, between PST and HE.
Although no meaningful differences were found between groups at 12 weeks, the overall mixed-model analysis for disability across all time points was significant. Results suggested that this was because PST sustained reductions in disability at 6 months, whereas disability levels in the HE groups returned to near-baseline levels (moderate effect). Caution is needed in interpreting this result, because the linear contrast did not reach statistical significance and data were missing at 6 months.
At 12 weeks and 6 months, PST reduced self-reported problem-solving impairment compared with HE (moderate effect). The meaningful reductions seen in problem-solving impairment in the PST group compared with the HE group may have enabled reductions in disability at follow-up for PST. We found reductions in problem-solving impairment–mediated reductions in disability for PST, suggesting the importance of targeting problem-solving impairment to improve long-term outcomes for GWI.
Of note, PST was acceptable to veterans with GWI. We found that 84.4% of veterans with GWI attended 100% of treatment sessions. This percentage is higher than in previous studies in which only 38% to 73% of veterans with symptoms consistent with GWI attended 40% to 60% of treatment sessions.7,41,42 We suspect the high acceptability is because the PST examined in this trial was tailored to veterans’ experiences with GWI. In addition, PST has been promulgated as an evidence-based practice in the VA, suggesting that PST could be disseminated to veterans with GWI through these trained providers.43,44
We unexpectedly found the acceptability of HE also to be high, likely because our HE was tailored for GWI.25 Furthermore, HE had a greater than anticipated immediate effect, which likely explained the lack of differences between groups at 12 weeks. However, the effects of HE on reductions in disability waned, suggesting the need for the future addition of behavioral support (eg, goal setting) to enhance its use as an active treatment, although further assessment is needed.45
We hypothesized, but did not find, that PST reduced objective problem-solving impairment, pain, and fatigue. Divergent self-report and objective problem-solving outcomes are consistent with findings from earlier clinical trials of PST16,46 and suggest the importance of using multidimensional assessments.47 The virtue of self-report is that it elicits the individual’s acknowledgment of relevant difficulties.48 In terms of pain and fatigue, our treatment was focused on reducing disability and was not designed to teach veterans symptom reduction skills. Treatments may need to specifically teach such skills to reduce pain and fatigue.
Limitations
This study has some limitations. The generalizability of these results to other populations is not known. In addition, significant attrition was seen at 6 months, and 6-month results should be confirmed in future studies. Furthermore, although telephone delivery is generally efficacious, we did not assess the efficacy compared with face-to-face delivery for this population.
Conclusions
The prespecified primary outcome of disability was not different between the PST and HE groups at the end of treatment in this randomized clinical trial. Secondary outcomes suggest that PST reduced problem-solving impairment and may have reduced disability at follow-up compared with HE, although this conclusion should be confirmed in future studies. Problem-solving treatment had high acceptability and is an evidence-based practice supported enterprise-wide in the VA.44 Together, the evidence that PST may reduce problem-solving impairment and disability at 6 months, has high acceptability, and is available in the VA, as well as the fact that there are few existing evidence-based treatments for GWI, suggests the potential for PST as a treatment for veterans with GWI.
Trial Protocol and Statistical Analysis Plan
Data Sharing Statement
References
- 1.McAndrew LM, Helmer DA, Phillips LA, Chandler HK, Ray K, Quigley KS. Iraq and Afghanistan veterans report symptoms consistent with chronic multisymptom illness one year after deployment. J Rehabil Res Dev. 2016;53(1):59-70. doi: 10.1682/JRRD.2014.10.0255 [DOI] [PubMed] [Google Scholar]
- 2.Steele L. Prevalence and patterns of Gulf War illness in Kansas veterans: association of symptoms with characteristics of person, place, and time of military service. Am J Epidemiol. 2000;152(10):992-1002. doi: 10.1093/aje/152.10.992 [DOI] [PubMed] [Google Scholar]
- 3.Blanchard MS, Eisen SA, Alpern R, et al. Chronic multisymptom illness complex in Gulf War I veterans 10 years later. Am J Epidemiol. 2006;163(1):66-75. doi: 10.1093/aje/kwj008 [DOI] [PubMed] [Google Scholar]
- 4.Robbins R, Helmer D, Monahan P, et al. Management of chronic multisymptom illness: synopsis of the 2021 US Department of Veterans Affairs and US Department of Defense Clinical Practice Guideline. Mayo Clin Proc. 2022;97(5):991-1002. doi: 10.1016/j.mayocp.2022.01.031 [DOI] [PubMed] [Google Scholar]
- 5.Nugent SM, Freeman M, Ayers CK, et al. A systematic review of therapeutic interventions and management strategies for Gulf War illness. Mil Med. 2020;186(1-2):e169-e178. doi: 10.1093/milmed/usaa260 [DOI] [PubMed] [Google Scholar]
- 6.Chester JE, Rowneki M, Van Doren W, Helmer DA. Progression of intervention-focused research for Gulf War illness. Mil Med Res. 2019;6(1):31. doi: 10.1186/s40779-019-0221-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Donta ST, Clauw DJ, Engel CC Jr, et al. ; VA Cooperative Study #470 Study Group . Cognitive behavioral therapy and aerobic exercise for Gulf War veterans’ illnesses: a randomized controlled trial. JAMA. 2003;289(11):1396-1404. doi: 10.1001/jama.289.11.1396 [DOI] [PubMed] [Google Scholar]
- 8.Medicine Io . Gulf War and Health: Treatment for Chronic Multisymptom Illness. National Academies Press; 2013. [PubMed] [Google Scholar]
- 9.Hotopf M. Treating Gulf War veterans’ illnesses—are more focused studies needed? JAMA. 2003;289(11):1436-1437. doi: 10.1001/jama.289.11.1436 [DOI] [PubMed] [Google Scholar]
- 10.Bloeser K, McCarron KK, Merker VL, et al. “Because the country, it seems though, has turned their back on me”: experiences of institutional betrayal among veterans living with Gulf War Illness. Soc Sci Med. 2021;284:114211. doi: 10.1016/j.socscimed.2021.114211 [DOI] [PubMed] [Google Scholar]
- 11.Zavestoski S, Brown P, McCormick S, Mayer B, D’Ottavi M, Lucove JC. Patient activism and the struggle for diagnosis: Gulf War illnesses and other medically unexplained physical symptoms in the US. Soc Sci Med. 2004;58(1):161-175. doi: 10.1016/S0277-9536(03)00157-6 [DOI] [PubMed] [Google Scholar]
- 12.Lange G, Tiersky LA, Scharer JB, et al. Cognitive functioning in Gulf War illness. J Clin Exp Neuropsychol. 2001;23(2):240-249. doi: 10.1076/jcen.23.2.240.1208 [DOI] [PubMed] [Google Scholar]
- 13.Janulewicz PA, Krengel MH, Maule A, et al. Neuropsychological characteristics of Gulf War illness: a meta-analysis. PLoS One. 2017;12(5):e0177121. doi: 10.1371/journal.pone.0177121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Allanson F, Pestell C, Gignac GE, Yeo YX, Weinborn M. Neuropsychological predictors of outcome following traumatic brain injury in adults: a meta-analysis. Neuropsychol Rev. 2017;27(3):187-201. doi: 10.1007/s11065-017-9353-5 [DOI] [PubMed] [Google Scholar]
- 15.Baird C, Lovell J, Johnson M, Shiell K, Ibrahim JE. The impact of cognitive impairment on self-management in chronic obstructive pulmonary disease: a systematic review. Respir Med. 2017;129:130-139. doi: 10.1016/j.rmed.2017.06.006 [DOI] [PubMed] [Google Scholar]
- 16.Rath JF, Simon D, Langenbahn DM, Sherr RL, Diller L. Group treatment of problem-solving deficits in outpatients with traumatic brain injury: a randomised outcome study. Neuropsychol Rehabil. 2003;13(4):461-488. doi: 10.1080/09602010343000039 [DOI] [Google Scholar]
- 17.Cuijpers P, de Wit L, Kleiboer A, Karyotaki E, Ebert DD. Problem-solving therapy for adult depression: an updated meta-analysis. Eur Psychiatry. 2018;48:27-37. doi: 10.1016/j.eurpsy.2017.11.006 [DOI] [PubMed] [Google Scholar]
- 18.Greenberg LM, Litke DR, Ray K, et al. Developing a problem-solving treatment for Gulf War illness: cognitive rehabilitation of veterans with complex post-deployment health concerns. Clin Soc Work J. 2018;46:100-109. doi: 10.1007/s10615-017-0616-7 [DOI] [Google Scholar]
- 19.Castro A, Gili M, Ricci-Cabello I, et al. Effectiveness and adherence of telephone-administered psychotherapy for depression: a systematic review and meta-analysis. J Affect Disord. 2020;260:514-526. doi: 10.1016/j.jad.2019.09.023 [DOI] [PubMed] [Google Scholar]
- 20.McClellan MJ, Osbaldiston R, Wu R, et al. The effectiveness of telepsychology with veterans: a meta-analysis of services delivered by videoconference and phone. Psychol Serv. 2022;19(2):294-304. doi: 10.1037/ser0000522 [DOI] [PubMed] [Google Scholar]
- 21.Irvine A, Drew P, Bower P, et al. Are there interactional differences between telephone and face-to-face psychological therapy? a systematic review of comparative studies. J Affect Disord. 2020;265:120-131. doi: 10.1016/j.jad.2020.01.057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med. 2010;152(11):726-732. doi: 10.7326/0003-4819-152-11-201006010-00232 [DOI] [PubMed] [Google Scholar]
- 23.Üstün TB, Kostanjsek N, Chatterji S, Rehm J. Measuring Health and Disability: Manual for WHO Disability Assessment Schedule WHODAS 2.0. World Health Organization; 2010. [Google Scholar]
- 24.Nezu AM, Nezu CM. Emotion-Centered Problem-Solving Therapy: Treatment Guidelines. Springer Publishing Co; 2018. doi: 10.1891/9780826143167 [DOI] [Google Scholar]
- 25.Lange G, McAndrew L, Ashford JW, Reinhard M, Peterson M, Helmer DA. War Related Illness and Injury Study Center (WRIISC): a multidisciplinary translational approach to the care of Veterans with chronic multisymptom illness. Mil Med. 2013;178(7):705-707. doi: 10.7205/MILMED-D-13-00053 [DOI] [PubMed] [Google Scholar]
- 26.Stout RL, Wirtz PW, Carbonari JP, Del Boca FK. Ensuring balanced distribution of prognostic factors in treatment outcome research. J Stud Alcohol Suppl. 1994;12(12):70-75. doi: 10.15288/jsas.1994.s12.70 [DOI] [PubMed] [Google Scholar]
- 27.Heppner PP, Petersen CH. The development and implications of a personal problem-solving inventory. J Couns Psychol. 1982;29(1):66. doi: 10.1037/0022-0167.29.1.66 [DOI] [Google Scholar]
- 28.Golden CJ. Stroop color and word Test: A Manual for Clinical and Experimental Uses. Stoelting Co; 1978.
- 29.Tombaugh TN. Trail Making Test A and B: normative data stratified by age and education. Arch Clin Neuropsychol. 2004;19(2):203-214. doi: 10.1016/S0887-6177(03)00039-8 [DOI] [PubMed] [Google Scholar]
- 30.Russell EW, Levy M. Revision of the Halstead Category Test. J Consult Clin Psychol. 1987;55(6):898-901. doi: 10.1037/0022-006X.55.6.898 [DOI] [PubMed] [Google Scholar]
- 31.Conners CK. Conners Continuous Performance Test (Conners CPT 3) & Conners Continuous Auditory Test of Attention (Conners CATA): Technical Manual. Multi-Health Systems; 2014.
- 32.Tait RC, Chibnall JT, Krause S. The pain disability index: psychometric properties. Pain. 1990;40(2):171-182. doi: 10.1016/0304-3959(90)90068-O [DOI] [PubMed] [Google Scholar]
- 33.Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD. The fatigue severity scale: application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989;46(10):1121-1123. doi: 10.1001/archneur.1989.00520460115022 [DOI] [PubMed] [Google Scholar]
- 34.Attkisson CC, Zwick R. The client satisfaction questionnaire: psychometric properties and correlations with service utilization and psychotherapy outcome. Eval Program Plann. 1982;5(3):233-237. doi: 10.1016/0149-7189(82)90074-X [DOI] [PubMed] [Google Scholar]
- 35.Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD checklist for DSM-5 (PCL-5). 2013. Accessed October 26, 2022. https://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp
- 36.Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann. 2002;32(9):509-515. doi: 10.3928/0048-5713-20020901-06 [DOI] [Google Scholar]
- 37.Alexopoulos GS, Raue PJ, Kiosses DN, et al. Problem-solving therapy and supportive therapy in older adults with major depression and executive dysfunction: effect on disability. Arch Gen Psychiatry. 2011;68(1):33-41. doi: 10.1001/archgenpsychiatry.2010.177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.MacKinnon DP, Fritz MS, Williams J, Lockwood CM. Distribution of the product confidence limits for the indirect effect: program PRODCLIN. Behav Res Methods. 2007;39(3):384-389. doi: 10.3758/BF03193007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schafer JL. Multiple imputation: a primer. Stat Methods Med Res. 1999;8(1):3-15. doi: 10.1177/096228029900800102 [DOI] [PubMed] [Google Scholar]
- 40.Schafer JL. Analysis of Incomplete Multivariate Data. Chapman & Hall; 1997. [Google Scholar]
- 41.McAndrew LM, Greenberg LM, Ciccone DS, Helmer DA, Chandler HK. Telephone-based versus in-person delivery of cognitive behavioral treatment for veterans with chronic multisymptom illness: a controlled, randomized trial. Mil Behav Health. 2018;6(1):56-65. doi: 10.1080/21635781.2017.1337594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kearney DJ, Simpson TL, Malte CA, Felleman B, Martinez ME, Hunt SC. Mindfulness-based stress reduction in addition to usual care is associated with improvements in pain, fatigue, and cognitive failures among veterans with Gulf War illness. Am J Med. 2016;129(2):204-214. doi: 10.1016/j.amjmed.2015.09.015 [DOI] [PubMed] [Google Scholar]
- 43.Beaudreau SA, Karel MJ, Funderburk JS, et al. Problem-solving training for veterans in home based primary care: an evaluation of intervention effectiveness. Int Psychogeriatr. 2022;34(2):165-176. doi: 10.1017/S104161022000397X [DOI] [PubMed] [Google Scholar]
- 44.Tenhula WN, Nezu AM, Nezu CM, et al. Moving forward: a problem-solving training program to foster veteran resilience. Prof Psychol Res Pr. 2014;45(6):416. doi: 10.1037/a0037150 [DOI] [Google Scholar]
- 45.Wolever RQ, Simmons LA, Sforzo GA, et al. A systematic review of the literature on health and wellness coaching: defining a key behavioral intervention in healthcare. Glob Adv Health Med. 2013;2(4):38-57. doi: 10.7453/gahmj.2013.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cantor J, Ashman T, Dams-O’Connor K, et al. Evaluation of the short-term executive plus intervention for executive dysfunction after traumatic brain injury: a randomized controlled trial with minimization. Arch Phys Med Rehabil. 2014;95(1):1-9.e3. doi: 10.1016/j.apmr.2013.08.005 [DOI] [PubMed] [Google Scholar]
- 47.Rath JF, Simon D, Langenbahn DM, Sherr RL, Diller L. Measurement of problem-solving deficits in adults with acquired brain damage. J Head Trauma Rehabil. 2000;15(1):724-733. doi: 10.1097/00001199-200002000-00010 [DOI] [PubMed] [Google Scholar]
- 48.Rath JF, Hradil AL, Litke DR, Diller L. Clinical applications of problem-solving research in neuropsychological rehabilitation: addressing the subjective experience of cognitive deficits in outpatients with acquired brain injury. Rehabil Psychol. 2011;56(4):320-328. doi: 10.1037/a0025817 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol and Statistical Analysis Plan
Data Sharing Statement