Abstract
This study evaluates changes in overall and drug-specific overdose mortality among pregnant and postpartum persons before and during the COVID-19 pandemic.
Drug overdose deaths, particularly deaths involving synthetic opioids like fentanyl, reached record highs in 2020 and 2021,1 likely exacerbated by social, economic, and health care disruptions associated with the COVID-19 pandemic. Pregnant and postpartum persons are at high risk for fatal overdose. However, recent national trends in pregnancy-associated overdose mortality are undercharacterized.2,3 This study evaluated changes in overall and drug-specific overdose mortality among pregnant or postpartum persons before and during the COVID-19 pandemic.
Methods
Data were from the restricted National Vital Statistics System mortality files for 2017 to 2020. The Columbia University institutional review board approved this analysis and waived informed consent. Pregnancy-associated deaths were identified based on International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) pregnancy-related codes4 and death certificate pregnancy checkbox status (eTable 1 in the Supplement).
The checkbox ascertains whether decedents were pregnant at the time of death, within 42 days of death (early postpartum), and within 43 to 365 days of death (late postpartum). Since 2016, the checkbox has been included on all state death certificates except West Virginia where the checkbox was added in 2017. California used a nonstandard question categorizing all deaths within 12 months as having occurred “late postpartum” even though they may have occurred in the early postpartum period. Drug overdoses were identified using underlying and contributing ICD-10 codes, disaggregated by the drug types involved (eTable 2 in the Supplement).
We calculated annual overdose mortality rates, examining changes over time in absolute and relative terms and by drug type and pregnancy timing. For comparison, we present overdose mortality rates among reproductive age persons (aged 15-44 years) identified on death certificates as female, excluding those identified as pregnant or postpartum. The 95% CIs were estimated using the Wilson score interval method.5 Significant differences at P < .05 were assessed with 2-sample tests for equality of proportions with continuity correction. We calculated absolute changes as the difference between the rates and the corresponding 95% CIs. The relative changes were calculated as the absolute change divided by the prior rate multiplied by 100. All analyses were conducted using R version 4.2.1 (R Foundation for Statistical Computing).
Results
Of the 7642 pregnancy-associated deaths between 2017 and 2020, 1249 were overdose-related, corresponding to a cumulative overdose mortality rate of 8.35 per 100 000 (95% CI, 7.89-8.83 per 100 000). Over the study period, pregnancy-associated overdose mortality increased from 6.56 to 11.85 per 100 000 (absolute change rate, 5.30 [95% CI, 3.90-6.72] per 100 000; relative increase of 81%). Overdose mortality among reproductive age persons identified on death certificates as female similarly increased from 14.37 to 19.76 per 100 000 (absolute change rate, 5.39 [95% CI, 4.94-5.85] per 100 000; relative increase of 38%). For both groups, increases in overdose mortality in 2020 were more pronounced than increases during any prior year (Table).
Table. Drug Overdose Mortality Rates Among Pregnant or Postpartum Persons and Those of Reproductive Age From 2017 to 2020a.
| Pregnant or postpartum | Reproductive age (aged 15-44 y)b | |||||
|---|---|---|---|---|---|---|
| No. of persons | No. of live birthsc | Drug overdose mortality rate per 100 000 (95% CI)d |
No. of persons | Population | Drug overdose mortality rate per 100 000 (95% CI)d |
|
| Year | ||||||
| 2017 | 252 | 3 844 260 | 6.56 (5.78-7.43) | 9191 | 63 958 243 | 14.37 (14.08-14.67) |
| 2018 | 266 | 3 780 401 | 7.04 (6.23-7.95) | 9198 | 64 171 698 | 14.33 (14.04-14.63) |
| 2019 | 304 | 3 736 144 | 8.14 (7.26-9.12) | 9433 | 64 325 356 | 14.66 (14.37-14.96) |
| 2020 | 427 | 3 602 653 | 11.85 (10.77-13.05) | 12 756 | 64 543 832 | 19.76 (19.42-20.11) |
| Total | 1249 | 14 963 458 | 8.35 (7.89-8.83) | 40 578 | 256 999 129 | 15.79 (15.64-15.94) |
| Absolute change rate (95% CI) [relative change %]e | ||||||
| 2017-2020 | 5.30 (3.90-6.72) [80.81] | 5.39 (4.94-5.85) [37.53] | ||||
| 2019-2020 | 3.72 (2.25-5.20) [45.67] | 5.10 (4.65-5.55) [34.77] | ||||
Data are from the restricted National Vital Statistics System for Health Statistics mortality files for 2017 to 2020.
Excludes persons identified as pregnant or postpartum at the time of death.
Among US residents aged 15 to 44 years and identified on the death certificate as female.
The 95% CIs were calculated using the Wilson score interval method.5
Absolute changes were calculated as the difference between the rates and the corresponding 95% CIs. The relative changes were calculated as the absolute change/prior rate × 100.
Pregnancy-associated overdose deaths involving benzodiazepines, heroin, and prescription opioids were mostly stable from 2017 to 2020, whereas large increases in deaths involving fentanyl and other synthetics and psychostimulants (eg, methamphetamine, cocaine) were observed (Figure). Increases in deaths due to fentanyl and other synthetics were especially marked in 2020, increasing from 5.73 per 100 000 (95% CI, 5.00-6.56 per 100 000) to 9.47 per 100 000 (95% CI, 8.50-10.54 per 100 000).
Figure. Pregnancy-Associated Drug Overdose Mortality.
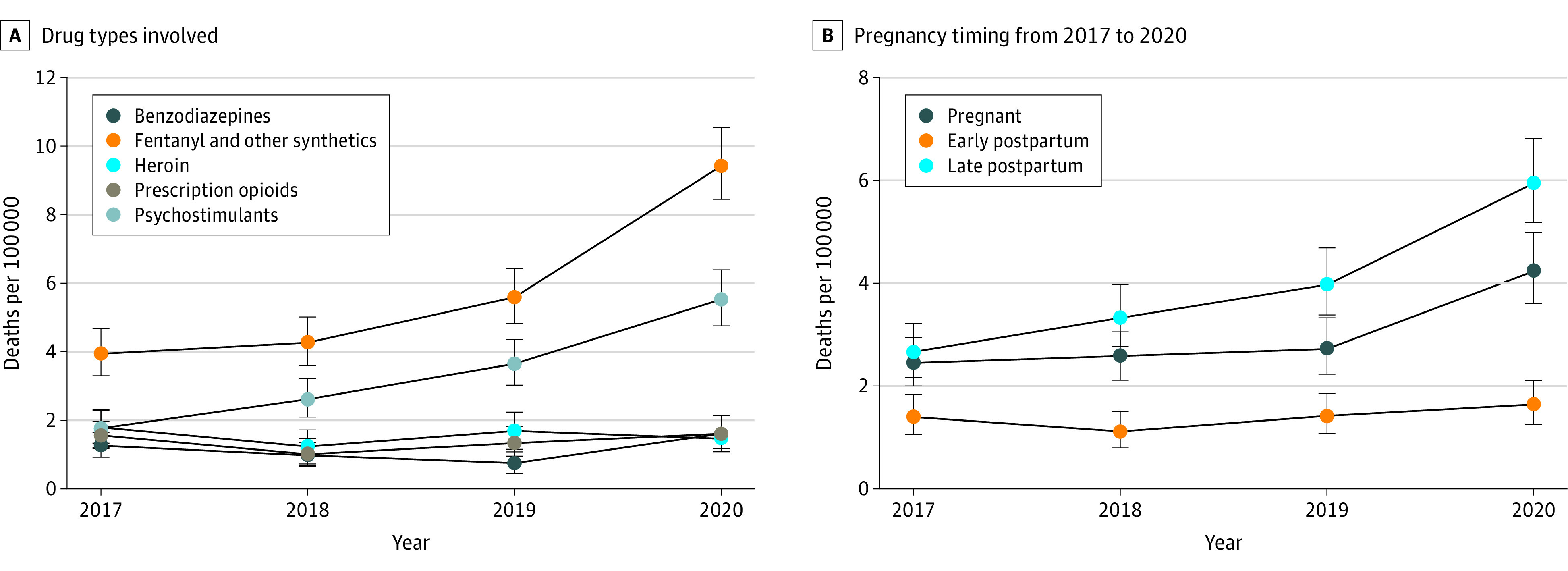
In A, deaths were identified using the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, underlying and multiple cause of death codes. Deaths involving more than 1 type of drug were included in rates for each applicable type such that categories are not mutually exclusive. The psychostimulants category included deaths due to psychostimulants with abuse potential, primarily methamphetamine and cocaine. In B, California used a nonstandard question identifying pregnancy within 12 months of death, therefore, deaths occurring late postpartum may be overstated and deaths occurring during pregnancy or early postpartum may be undercounted. Observations with indeterminate timing in mortality records were excluded.
Higher cumulative overdose mortality rates were observed among persons identified as late postpartum (3.95 per 100 000 [95% CI, 3.64-4.28 per 100 000]) compared with those pregnant at the time of death (2.99 per 100 000 [95% CI, 2.73-3.29 per 100 000]) or identified as early postpartum (1.39 per 100 000 [95% CI, 1.21-1.60 per 100 000]) (Figure).
Discussion
Among pregnant and postpartum persons, drug overdose mortality increased approximately 81% from 2017 to 2020, mirroring trends observed among persons of reproductive age overall. Increases in drug overdose mortality were most pronounced in 2020, coinciding with the onset of the COVID-19 pandemic. Pregnancy-associated overdose deaths were also progressively characterized by synthetic opioid and psychostimulant involvement, highlighting the roles of fentanyl and polysubstance use in shaping current overdose risk patterns.
Although steady increases in pregnancy-associated overdose deaths have been observed previously from 2007 to 2019,2,3 the increase observed in 2020 was more pronounced than in previous years. Pregnant and postpartum persons are known to face barriers to accessing drug treatment and harm reduction services,6 which when compounded by pandemic-associated stressors, health care shutdowns, and an increasingly volatile unregulated drug supply may have increased fatal overdose risk.
This study has limitations, including small numbers in some subgroups, limited pregnancy information, potential undercounting of early postpartum and overcounting of late postpartum deaths due to California’s death certificate question on timing, and potential misclassification for pregnancy status and drug involvement. The findings indicate that enhanced strategies supporting substance use prevention, treatment, and harm reduction efforts among pregnant and postpartum persons are needed.
Section Editors: Jody W. Zylke, MD, Deputy Editor; Kristin Walter, MD, Senior Editor.
eTable 1. ICD-10 codes identifying and classifying pregnancy-associated deaths
eTable 2. ICD-10 codes identifying and classifying drug overdose deaths
References
- 1.O’Donnell J, Tanz LJ, Gladden RM, Davis NL, Bitting J. Trends in and characteristics of drug overdose deaths involving illicitly manufactured fentanyls—United States, 2019-2020. MMWR Morb Mortal Wkly Rep. 2021;70(50):1740-1746. doi: 10.15585/mmwr.mm7050e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gemmill A, Kiang MV, Alexander MJ. Trends in pregnancy-associated mortality involving opioids in the United States, 2007-2016. Am J Obstet Gynecol. 2019;220(1):115-116. doi: 10.1016/j.ajog.2018.09.028 [DOI] [PubMed] [Google Scholar]
- 3.Margerison CE, Roberts MH, Gemmill A, Goldman-Mellor S. Pregnancy-associated deaths due to drugs, suicide, and homicide in the United States, 2010-2019. Obstet Gynecol. 2022;139(2):172-180. doi: 10.1097/AOG.0000000000004649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rossen LM, Womack LS, Hoyert DL, Anderson RN, Uddin SFG. The impact of the pregnancy checkbox and misclassification on maternal mortality trends in the United States, 1999–2017. Vital Health Stat 3. 2020;3(44):1-61. [PubMed] [Google Scholar]
- 5.Wilson EB. Probable inference, the law of succession, and statistical inference. J Am Stat Assoc. 1927;22(158):209-212. doi: 10.1080/01621459.1927.10502953 [DOI] [Google Scholar]
- 6.Meinhofer A, Hinde JM, Ali MM. Substance use disorder treatment services for pregnant and postpartum women in residential and outpatient settings. J Subst Abuse Treat. 2020;110:9-17. doi: 10.1016/j.jsat.2019.12.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. ICD-10 codes identifying and classifying pregnancy-associated deaths
eTable 2. ICD-10 codes identifying and classifying drug overdose deaths


