Abstract
Although the COVID-19 pandemic caused significant stress and anxiety among many, individuals’ experiences varied. We examined if specific forms of anxiety predicted distinct trajectories of anxiety, perceived stress, and COVID-related worries during three early months of the pandemic. In a longitudinal study (N = 291), adolescents’ (n = 194) social and generalized anxiety levels were assessed via parent- and self-reports and clinical diagnostic interviews. In young adulthood (n = 164), anxiety, stress, and COVID-related worries were assessed thrice during the pandemic. Pre-pandemic generalized anxiety predicted higher initial levels and maintenance of anxiety, stress, and COVID-related worries during the pandemic. In contrast, pre-pandemic social anxiety predicted lower initial levels of anxiety, stress, and COVID-related worries, but this initial effect on anxiety and stress was offset over time by social anxiety’s positive effect on the slope. Our results highlight the importance of understanding how pre-pandemic factors influence individuals’ experiences during the pandemic.
Keywords: Anxiety, Social Anxiety, Generalized Anxiety, Adolescent Development, COVID-19 pandemic
Introduction
The COVID-19 pandemic and its associated public health emergency measures have significantly disrupted individuals’ lives, increasing stress, worries, and anxiety among many, especially young adults (Czeisler et al., 2020). From the start of the COVID-19 pandemic, there were concerns that this crisis would lead to increases in stress and anxiety (Holmes et al., 2020; Prime et al., 2020). The initial restrictions (e.g., social distancing) coupled with heightened health dangers were seen as risk factors for psychological distress and mental health problems. Recent evidence supports these initial concerns. Across studies, measures of stress, anxiety, and other forms of psychopathology were considerably higher during the pandemic than in the times preceding the pandemic (Czeisler et al., 2020; Daly et al., 2020; Prati & Mancini, 2021; Shanahan et al., 2020).
However, these effects varied between individuals. For example, young adults seemed to be disproportionally impacted during the pandemic, displaying the highest levels of stress, anxiety, and other mental health problems, compared to other age groups (Czeisler et al., 2020; Daly et al., 2020; McGinty et al., 2020). Nevertheless, even among young adults, most individuals were not experiencing impairing levels of stress and anxiety. Furthermore, recent reports suggest that some young adults and children were experiencing a reduction in mental health problems like anxiety during the pandemic (Cost et al., 2021; León, 2021; Luthar et al., 2021; Shanahan et al., 2020). This highlights the need to better understand this heterogeneity in anxiety and perceived stress responses to the pandemic by identifying pre-pandemic factors that predict which individuals are at the highest risk and when during the pandemic. Better understanding these differential responses may provide important insights for improved early identification of individuals at highest risk for psychopathology during situations with high levels of uncertainty, potential physical harm, and that require social distancing.
Previous studies examining risk factors for increased anxiety during the pandemic have reported that a wealth of sociodemographic factors predict being more adversely affected, including being a young adult, woman, Latinx/Hispanic or Black person, as well as having lower educational attainment or financial resources (Czeisler et al., 2020; Daly et al., 2020; McGinty et al., 2020; Shanahan et al., 2020). Moreover, pre-existing mental health problems represent one of the strongest predictors of mental health problems during the pandemic (Czeisler et al., 2020; Fancourt et al., 2021; Holman et al., 2020; McGinty et al., 2020; Shanahan et al., 2020). For example, in a longitudinal study, young adults with higher levels of psychopathology before the pandemic were at a considerably increased risk for heightened psychopathology and stress during the pandemic, compared to young adults with lower levels of psychopathology before the pandemic (Shanahan et al., 2020). Moreover, statistically accounting for the effects of previous levels of psychopathology significantly reduced the effects of other risk factors (e.g., being a female or low social support) on psychopathology during the pandemic, suggesting that pre-pandemic psychopathology is one of the most important risk factors for experiencing increased mental health problems during the pandemic.
However, most existing studies examining pre-pandemic psychopathology have either compared individuals with any pre-existing mental health diagnosis to individuals without a diagnosis or have used broad dimensions of psychopathology (e.g., internalizing); thus, obscuring what could be a specific impact of different forms of psychopathology. For example, a recent study found that having any pre-existing clinical diagnosis was associated with deterioration in mental health during the pandemic compared to before the pandemic for some youth, but improvement in mental health during the pandemic for other youth (Cost et al., 2021). This suggests that pre-pandemic psychopathology can act both as a risk and a protective factor for individuals’ mental health during the pandemic likely depending on the specific type of psychopathology. Cost et al. (2021) speculated that for some children with previous mental health problems, the loss of consistency and increased stress caused by the pandemic led to deterioration in mental health. In contrast, for other children with specific forms of pre-existing mental health diagnosis (e.g., social anxiety disorder), the COVID-related restrictions (e.g., stay-at-home orders) may have provided relief from sources of stress and anxiety (vis-à-vis a reduction in social interactions), leading to improvements in mental health (Cost et al., 2021). This possibility has been considered both by lay press (Gold, 2020; Richtel, 2021; Schroeder, 2020) and other scientists (Bruining et al., 2020; Morrissette, 2021), but such effects have not been empirically demonstrated. If this interpretation was correct, a dissociation between specific forms of psychopathology depending on the causes of distress between forms of psychopathology (e.g., distress in social situations) should be evident. Moreover, the “protective” effects of the COVID-related restrictions should have changed during the course of the pandemic and as the restrictions were lifted. However, no studies to our knowledge have examined differential mental health trajectories during the pandemic based on different forms of pre-pandemic psychopathology.
Different types of pre-pandemic anxiety, in particular, may predict differential stress responses to the pandemic, allowing us to examine such a potential dissociation. Although pre-pandemic anxiety predicted increased anxiety levels during the pandemic (Hawes et al., 2021), prior studies failed to differentiate associations among different forms of anxiety. For instance, individuals with generalized anxiety, who tend to have persistent and excessive levels of worry about many aspects of life that became relatively uncertain during the pandemic (e.g., future, health, finances), might have faced heightened risk for exacerbated worries and stress during the pandemic. In contrast, individuals high in social anxiety may have been less worried, stressed, and anxious, given changes in social interactions during the pandemic. Thus, initial disruptions caused by the pandemic, including social distancing, may have reduced stress among people high in social anxiety, but as restrictions were lifted and re-opening occurred, anxiety and stress levels may have increased for these individuals.
In addition to helping better understand the heterogeneity of individuals’ responses during the pandemic, examining the potential dissociation between generalized and social anxiety will inform theoretical discussions about the nature of anxiety disorders. Some researchers suggest that because different types of anxiety are highly comorbid, their differences are not clinically meaningful (Rutter, 2011). On the other hand, others highlight the importance of the differences between types of anxiety (Pine, 2007, 2011), as they show differences in emotion processing and responding (Blair et al., 2008; Kessel et al., 2015; Mennin et al., 2009; Salum et al., 2013) – which might ultimately lead to differential outcomes (e.g., Zeytinoglu, Neuman, et al., 2021). In this way, by using the pandemic and its associated restrictions as a natural experiment, we were able to examine if different types of anxiety predicted different outcomes, informing theoretical discussions of anxiety-disorder research.
Current Study
In the current study, we leveraged a longitudinal study on the development of anxiety to test whether adolescent social vs. generalized anxiety symptoms pre-pandemic predict distinct trajectories of young adult worry, stress, and anxiety during three initials months of the COVID-19 pandemic in the United States. We used latent growth curve modeling to characterize the trajectories of COVID-related worries, perceived stress, and anxiety during three consecutive months early on in the pandemic. When designing the study, we originally hypothesized that, on average, levels of COVID-related worries, perceived stress, and anxiety would increase across the pandemic. However, recent long-term studies suggest that, on average, anxiety and stress peaked during the initial months of the pandemic as restrictions began, followed by a significant decline in anxiety and stress during the following months (Fancourt et al., 2021; Hawes et al., 2021). For example, in a study of young adults in New York (United States), Hawes et al. (2021) report that the highest levels of anxiety and other forms of psychopathology occurred in the early stages of pandemic (April and May), followed by significant declines over the summer. These trajectories suggest that anxiety was highest when the most stringent restrictions were in place and the uncertainty about the virus was highest. However, as individuals adapted to the life changes and restrictions were gradually eased, mental health improved. Based on these recent studies and the first assessments of our own data (Lorenzo et al., 2021; Zeytinoglu, Morales, et al., 2021), we hypothesized that COVID-related worries, perceived stress, and anxiety would decrease across the months sampled early on during the pandemic.
After characterizing the average trajectories of COVID-related worries, perceived stress, and anxiety, we examined whether these trajectories differed based on individuals’ pre-pandemic social and generalized anxiety. We hypothesized that young adults with higher levels of generalized anxiety pre-pandemic (i.e., during adolescence) would display trajectories of higher initial worries, stress, and anxiety with increases during the pandemic, compared to individuals lower in generalized anxiety pre-pandemic. In contrast, we hypothesized that young adults with higher levels of adolescent social anxiety pre-pandemic would display trajectories of lower initial worries, stress, and anxiety (as the pressure to interact socially was removed) with increases as re-opening gradually occurred, compared to individuals lower in social anxiety pre-pandemic.
Method
Participants
Participants were involved in an ongoing prospective longitudinal, multi-method study of temperament and socioemotional development conducted at the University of Maryland in the United States. Two hundred ninety one families with a four month old infant of whom 156 were girls were selected based on displays of positive and negative affect and motor reactivity to novel stimuli (Hane et al., 2008) and followed across childhood and adolescence. The demographics of the original longitudinal sample were characterized based on maternal reports of their own race/ethnicity and education (when participants were infants). The sample of mothers was 69.4% Caucasian, 16.5% African American, 7.2% Hispanic, 3.1% Asian, and 3.4% other; 0.3% of mothers did not report their race and ethnicity. Mothers in the sample were highly educated; 35.7% had completed graduate school, 41.9% were college graduates, 16.2% were high school graduates, 5.5% had other forms of education; 0.7% of mothers did not report their education. Mothers reported the race and ethnicity of their children (i.e., the participants) in a follow-up assessment during the children's adolescence. The sample of adolescents (n = 182) was 67.6% White, 12.6% African American, 12.1% mixed race, 1.1% Asian, 1.1% American Indian or Alaska Native, 2.7% other, and 2.7% no race reported. For ethnicity, the sample was 85.2% White 8.2% Hispanic or Latino, and 6.6% no ethnicity reported.
Of the original sample (N = 291), 194 had at least one measure of anxiety during adolescence and 164 had at least one measure of anxiety, stress, or COVID-related worries during the COVID-19 pandemic. Table 1 displays the sample sizes for each measure. Examining the patterns of missing data revealed that mothers’ race/ethnicity (non-Hispanic Caucasian vs. other minority groups) was associated with missing data during the pandemic (p = .021), such that participants with data during the pandemic were more likely to have non-Hispanic Caucasian mothers. As such, a dummy-coded variable of maternal race and ethnicity (non-Hispanic Caucasian vs. other minority groups) was included as a covariate in the SEM analyses. Patterns of missing data on all other variables were not associated with maternal race/ethnicity or education, children’s gender, or child anxiety at any assessment (ps > .08).
Table 1.
Means, standard deviations, and correlations
| Variable | N | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Gender | 291 | * | ||||||||||||||||||
| 2. Maternal Ethnicity | 290 | ** | −.05 | |||||||||||||||||
| 3. Maternal Education | 273 | 1.21 | 0.72 | .01 | .19 | |||||||||||||||
| 4. Gen Anx Self | 162 | 7.64 | 4.42 | −.27 | .11 | −.07 | ||||||||||||||
| 5. Gen Anx Parent | 177 | 4.38 | 3.98 | −.20 | .14 | −.10 | .41 | |||||||||||||
| 6. Gen Anx Clinical | 151 | *** | −.07 | .07 | −.00 | .40 | .49 | |||||||||||||
| 7. Social Anx Self | 162 | 5.58 | 3.80 | −.31 | −.09 | −.14 | .52 | .38 | .33 | |||||||||||
| 8. Social Anx Parent | 178 | 3.81 | 3.65 | −.26 | .06 | −.15 | .27 | .60 | .21 | .55 | ||||||||||
| 9. Social Anx Clinical | 151 | *** | −.09 | .11 | −.07 | .22 | .33 | .26 | .43 | .34 | ||||||||||
| 10. Anxiety T1 | 155 | 5.69 | 5.62 | −.16 | .05 | .16 | .29 | .29 | .17 | .07 | .02 | .06 | ||||||||
| 11. Anxiety T2 | 153 | 5.07 | 5.06 | −.10 | .14 | .08 | .38 | .29 | .30 | .12 | .00 | .07 | .81 | |||||||
| 12. Anxiety T3 | 141 | 4.50 | 4.82 | −.17 | .13 | .07 | .31 | .25 | .31 | .30 | .06 | .25 | .65 | .71 | ||||||
| 13. Stress T1 | 136 | 19.77 | 7.22 | −.23 | .03 | .09 | .24 | .17 | .12 | −.02 | −.08 | .04 | .70 | .63 | .50 | |||||
| 14. Stress T2 | 151 | 17.67 | 6.70 | −.17 | .02 | .13 | .32 | .10 | .12 | −.02 | −.10 | −.01 | .59 | .68 | .48 | .70 | ||||
| 15. Stress T3 | 140 | 16.13 | 7.55 | −.36 | .02 | .07 | .40 | .16 | .27 | .31 | .04 | .23 | .51 | .55 | .73 | .58 | .62 | |||
| 16. COVID Worries T1 | 158 | 2.75 | 0.73 | −.31 | −.01 | .11 | .23 | .08 | .19 | −.00 | −.04 | −.07 | .48 | .46 | .47 | .58 | .52 | .58 | ||
| 17. COVID Worries T2 | 155 | 2.49 | 0.72 | −.28 | .02 | .13 | .23 | .04 | .11 | −.01 | −.05 | .02 | .54 | .59 | .52 | .67 | .66 | .62 | .79 | |
| 18. COVID Worries T3 | 143 | 2.31 | 0.74 | −.30 | .03 | .09 | .27 | .14 | .26 | .04 | −.02 | .08 | .39 | .48 | .53 | .52 | .55 | .69 | .73 | .76 |
Note. M and SD are used to represent mean and standard deviation, respectively. N is the sample size for that measure. Bold indicates p < .05.
0 = Girls (53.6%) and 1 = Boys (46.4%).
1 = Non-Hispanic Caucasian (69.4%) and 0 = Other (30.2%).
1 = Clinical diagnosis (13.2% General and 15.9% Social) and 0 = no diagnosis. Maternal education was coded as High school graduate = 0, College Graduate = 1, Graduate school graduate = 2, and Other = missing. Gen Anx is generalized anxiety. Social Anx is social anxiety. Self is adolescent self-report. Parent is parent-reports. Clinical is clinical diagnosis. T1, T2, and T3 represent the first, second, and third assessments during the COVID-19 pandemic, respectively. COVID is the coronavirus disease of 2019.
Procedure
Adolescents’ social and generalized anxiety were assessed via parent and adolescent reports and structured clinical diagnostic interviews between March of 2017 and August of 2019 (Mage = 16.16, SD = 0.61; Rangeage = 15.04-17.98 years). Anxiety, COVID-related worries, and perceived stress were measured at approximately age 18 across 3 assessments during the COVID-19 pandemic (Mage = 18.26, SD = 0.67). One hundred fifty-eight participants completed their first assessment (Month 1) of online questionnaires between April 20 and May 15 of 2020, approximately 1 month (M = 29.67 days, SD = 6.01 days) after the stay-at-home order was implemented in Maryland, the state where most participants resided, and similar restrictions were enacted in nearby states. During the stay-at-home order, Maryland residents were ordered to not leave their home unless it was for an essential job or for an essential reason, such as obtaining medicine or food, seeking urgent medical attention, or for other necessary purposes. Approximately 1 month later (M = 26.48 days, SD = 7.31 days), 155 participants completed the second assessment (Month 2), as gradual reopening started in Maryland and nearby states. During the gradual reopening, residents were allowed to leave their homes, but some restrictions remained in place (e.g., indoor dining, gyms, and shopping malls remained closed), face coverings were mandated when out in public near others, and social distancing was encouraged. Approximately another month later (M = 28.86 days, SD = 5.83 days), 143 participants completed the third assessment, after stay at home orders were lifted and non-essential businesses reopened in limited capacity in Maryland and nearby states. Among the 164 participants who completed at least one measure of anxiety, stress, or COVID-related worries during the pandemic, 144 were residing in mid-Atlantic states (83% in Maryland), 10 were residing in southeastern states, 9 were residing in other US states, and 1 participant resided in England, UK. The Institutional Review Board of the University of Maryland approved all study protocols and all participants received compensation for their time.
Measures
Adolescent Social Anxiety and Generalized Anxiety (16 years).
Approximately two years prior to the pandemic, social anxiety and generalized anxiety were assessed via three methods: (a) adolescent self-report, (b) parent-report, and (c) diagnosis via clinical interview. Adolescents and mothers independently completed the social phobia (7 items) and the generalized anxiety (9 items) scales of the Screen for Child Anxiety Related Emotional Disorders (SCARED; Birmaher et al., 1997). Participants and mothers rated items from 0 (not true) to 2 (very true or often true) based on the extent to which behaviors were true over the last three months. Both scales had strong internal consistency in our sample (social anxiety scale: α = .89 for child-report, α =.91 for parent-report; generalized anxiety scale: α =.87 for adolescent-report, α =.89 for parent-report). These scales have demonstrated good discriminant validity, test-retest reliability, and moderate adolescent-mother agreement (Birmaher et al., 1997). Item sums indicated greater anxiety with higher scores for each subscale.
Clinicians conducted semi-structured diagnostic interviews with parents and adolescents using the Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children (KSADS) (Kaufman et al., 1997). All clinicians were trained, supervised, and monitored in weekly meetings with a supervisor where details of each case were discussed. Moreover, a senior investigator made independent diagnoses on a subset of interviews using audiotapes, yielding acceptable reliability for the diagnoses examined in the current paper (k > .80). Among the 151 adolescents evaluated, 15.9% (24) met criteria for social anxiety disorder, 13.2% (20) met criteria for generalized anxiety disorder, and 5.3% (8) participants met criteria for both.
Measures during the COVID-19 Pandemic.
Perceived Stress (18 years).
Perceived stress was measured using The Perceived Stress Scale (PSS-10; Cohen et al., 1994). Participants rated 10 items on a scale from 0 (Never) to 4 (Very Often). The PSS-10 has been shown to have good internal reliability as well as construct and concurrent validity (Mitchell et al., 2008). In this sample, the scale showed adequate internal consistency at all time points (αs > .84) and good test re-test reliability (rs > .58).
Anxiety (18 years).
Generalized anxiety was measured using the Generalized Anxiety Disorder 7-Item Scale (Spitzer et al., 2006). The items consisted of various anxiety symptoms and were summed to create an overall score. Higher scores indicated greater anxiety and scores ≥10 were considered to be in the clinical range. This scale has been shown to have high test-retest reliability and good convergent validity (Spitzer et al., 2006). In the present sample, the scale showed excellent internal consistency at all time points (αs > .92) and good test re-test reliability (rs > .65).
COVID-19 Worry Scale (age 18).
COVID-related worries were measured using an adapted version of the COVID-19 Adolescent Symptom & Psychological Experience Questionnaire (CASPE; Ladouceur, 2020). Participants responded to 18 items regarding various concerns and stressors about the COVID-19 pandemic or concerns related to disruptions caused by the pandemic. For each item, participants were asked to rate their level of worry or stress using a scale from 1 (very little or not at all) to 5 (A great deal or extremely) with an option for non-applicable. A full list of the items and questions is included in the supplement. Example statements included “having to stay home,” “someone in your household or extended family might become sick,” “missing events that are important to me,” “not having enough money,” and “doing something that may cause someone else to get sick.” Item scores were averaged to create an overall score with higher scores indicating greater COVID-19 related worries. For the present sample, the scale showed adequate internal consistency at all time points (α’s > .88) and good test re-test reliability (rs > .73).
Analytic Strategy
First, to examine the average trajectories of anxiety, perceived stress, and COVID-related worries across the initial three months of the pandemic, we conducted an unconditional latent growth curve model for each outcome, separately. The latent intercept factor, representing levels at the first COVID-19 assessment (Month 1), was estimated by constraining the paths of each month to 1. The latent slope factor, representing the linear change in anxiety across the three monthly COVID-19 assessments, was estimated by constraining the paths for each month, Month 1, Month 2, and Month 3, to 0, 1, and 2, respectively. The intercept and slope were allowed to covary.
To evaluate if the trajectories of anxiety varied as a function of previous anxiety levels, we examined if two anxiety latent factors – social anxiety and generalized anxiety – predicted the intercept and slope of each outcome: anxiety, COVID-related worries, and perceived stress. Each adolescent anxiety factor included three measures (adolescent report, parent report, and clinical diagnosis) as indicators of social or generalized anxiety, respectively. We allowed the anxiety factors to correlate, which they did significantly, r = .61, p < .001. Moreover, we covaried the residuals from the same type of measure with each other (i.e., adolescent report, parent report, or clinical interview indicators). As shown in the supplementary materials, we first fit a confirmatory factor analysis of only the measurement model (i.e., social and generalized anxiety factors), finding that all measures significantly loaded onto their respective anxiety factor (Table S1), with the model showing excellent fit, χ2(6) = 3.36, p = .76, RMSEA = .00, CFI = 1.0, SRMR = .03. As such, we added these social and generalized anxiety factors as predictors of the anxiety, COVID-related worries, and perceived stress trajectories.
In line with previous studies with this sample (Morales et al., 2020, 2021), additional predictor variables were selected based on the preliminary analyses described below with covariates and the sociodemographic variables related to missing data. Specifically, we attempted to control for the effects of maternal education, maternal ethnicity, participant gender, and participants’ average age during the COVID-19 assessments on the anxiety intercept and slope factors. In addition, we attempted to control for the effects of date of the first assessment (Month 1) as number of days since the stay-at-home order on the intercept and the date of the last assessment (Month 3) as number of days since the stay-at-home order on the slope. Missing data were handled using full information maximum likelihood estimation (FIML) to reduce potential bias in the parameter estimates (Enders & Bandalos, 2001). Due to missing data and potential departures from multivariate normality, the model was estimated using a robust maximum likelihood estimator (MLR) (Yuan & Bentler, 2000). Model fit was evaluated using a combination of fit indices including χ2, the comparative fit index (CFI; ≥ 0.90), root-mean-square error of approximation (RMSEA; ≤ 0.06), and the standardized root mean-squared residual (SRMR; ≤ 0.08; Hu & Bentler, 1999). All data cleaning, analyses, and figures were done in R (Version 3.6; R Development Core Team, 2008) using the following packages: lavaan (Rosseel, 2012), psych (Revelle, 2017), and ggplot2 (Wickham, 2016).
Results
Descriptive Results
Descriptive statistics and the relations among all study variables appear in Table 1. Compared to males, females generally manifested consistently higher pre-pandemic anxiety levels, COVID-related worries, perceived stress, and anxiety during the pandemic. Pre-pandemic adolescent reports of generalized anxiety significantly predicted anxiety, COVID-related worries, and stress across the three pandemic data collection periods. Pre-pandemic parent reports of generalized anxiety predicted anxiety across all three pandemic time points. Clinical diagnosis of generalized anxiety before the pandemic predicted anxiety in the last two pandemic time points. Clinical diagnosis of generalized anxiety before the pandemic predicted stress at T3 and COVID-related worries at T1 and T3. Notably, adolescent reports and clinical diagnosis of social anxiety only predicted T3 anxiety and T3 stress. Anxiety, stress, and COVID-related worries during the pandemic correlated with each other within and across time.
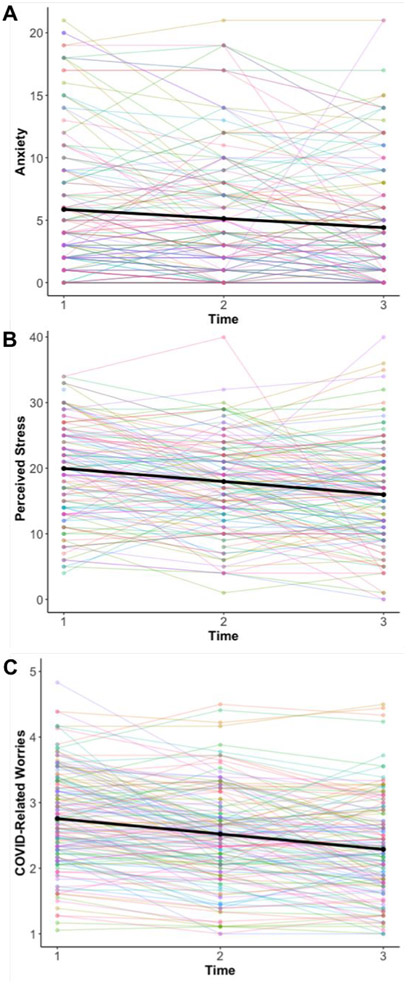
Anxiety, perceived stress, and COVID-19 worries trajectories
We first examined the trajectories of anxiety, perceived stress, and COVID-related worries during the pandemic using unconditional growth curve models. Results from these models suggested that all three outcomes significantly decreased across time for the sample as a whole. As shown in Figure 1, anxiety, perceived stress, and COVID-related worries all declined as individuals and families adapted to the pandemic-related restrictions, the stay-at-home orders were lifted, and reopening gradually occurred. Specifically, the initial average levels of anxiety were 5.86 and then declined 0.73 on average across each month. The initial average levels of perceived stress were 19.97 and then decreased 2.00 on average across each month. Finally, the starting average levels of COVID-related worries were 2.76 and then dropped 0.24 on average across each month. Regarding clinical levels, the percentage of participants considered in the clinical range (≥10) decreased from 20.0% at Month 1 to 17.0% at Month 3. Similarly, the percentage of participants reporting high levels of perceived stress (≥27) decreased from 19.1% at Month 1 to 8.6% at Month 3. Examining the variability in the intercept and slope estimates revealed significant variability in the intercept of all three outcomes (anxiety = 29.57; p < .001; perceived stress = 35.90; p < .001; COVID-related worries = 0.43; p < .001). However, the variability of the slopes was not significant (anxiety = 2.64; p = .084; perceived stress = 0.95; p = .775; COVID-related worries = 0.02; p = .436). Even though variances of the slopes were not significant, in order to examine our main hypotheses, we next examined if pre-pandemic generalized and social anxiety predicted these individual differences in the intercepts and slopes.
Figure 1.
Average trajectories of anxiety, perceived stress, and COVID-related worries from T1 (April-May) to T3 (June-July). Black lines represent predicted trajectory based on growth curve parameters. Color lines represent each individual’s trajectory based on their raw data. COVID represents the coronavirus disease of 2019. All unconditional models had acceptable fit: Anxiety model (χ2(1) = 0.01, p = .94, RMSEA = .00, SRMR = .00, CFI = 1.00), Perceived Stress model (χ2(1) = 0.79, p = .373, RMSEA = .00, SRMR = .02, CFI = 1.00), and COVID-related worries model (χ2(1) = 1.94, p = .16, RMSEA = .07, SRMR = .02, CFI = 1.00).
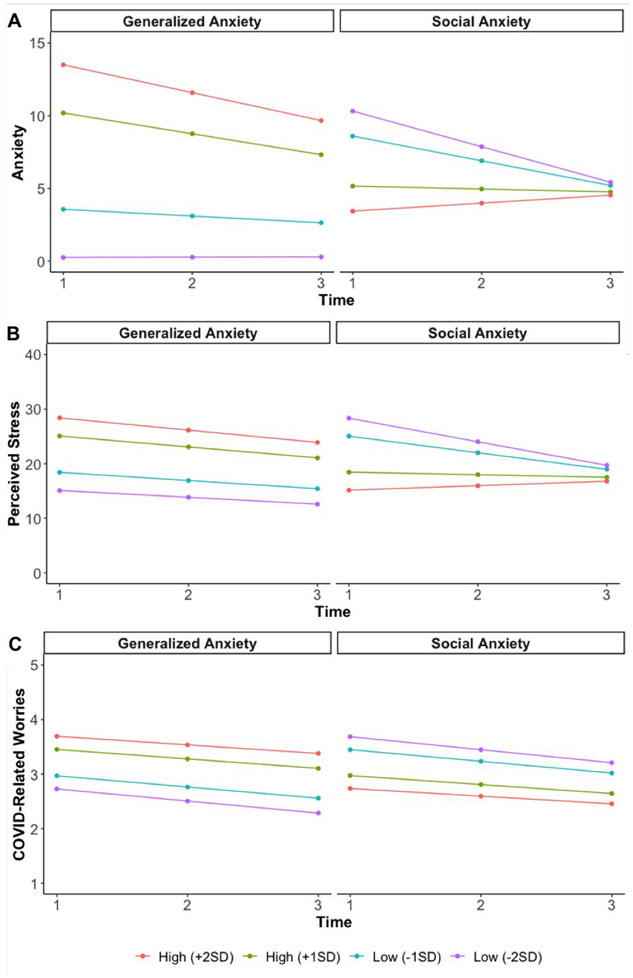
Trajectories of anxiety, perceived stress, and COVID-19 worries differ between generalized anxiety and social anxiety
As expected, anxiety trajectories differed based on pre-pandemic levels of social and generalized anxiety. As shown in Figure 2A and Table 2, generalized anxiety in adolescence predicted the anxiety intercept (b= 1.26, p < .001) but not the slope (b= −0.18, p = .195). Namely, after accounting for the effects of social anxiety, adolescents higher in pre-pandemic generalized anxiety, compared to those lower in generalized anxiety, displayed greater anxiety in Month 1 of the pandemic and maintained this difference during the following months. In contrast, social anxiety in adolescence predicted a smaller intercept (b= −0.55, p = .026), but had a positive effect on the value of the slope (b= 0.24, p = .038). In other words, while accounting for the effects of generalized anxiety, adolescents higher in pre-pandemic social anxiety, compared to those lower in social anxiety, displayed less anxiety in Month 1 of the pandemic. However, in the following months, as the sample decreased in anxiety on average, adolescents higher in social anxiety remained stable across time, reducing the initial difference with adolescents lower in social anxiety.
Figure 2.
Trajectories of anxiety, perceived stress, and COVID-related worries from T1 (April-May) to T3 (June-July) for different levels of generalized and social anxiety. For reference, when extracting factor scores from the generalized and social anxiety factors measurement model (see supplement), individuals diagnosed with generalized anxiety are 2.1 SDs above from the mean and individuals diagnosed with social anxiety are 1.4 SDs above the from the mean. COVID is the coronavirus disease of 2019. SD represents standard deviation.
Table 2.
Conditional latent growth curve analysis regression results for three models including pre-pandemic anxiety predictors.
| Predictors/Outcome | β | b | p | β | b | p | β | b | p |
|---|---|---|---|---|---|---|---|---|---|
| Anxiety Intercept |
Perceived Stress Intercept |
COVID-Related Worries Intercept |
|||||||
| Maternal Education | 0.12 | 0.89 | 0.136 | 0.08 | 0.72 | 0.379 | 0.05 | 0.05 | 0.521 |
| Maternal Ethnicity | −0.03 | −0.32 | 0.765 | −0.07 | −0.96 | 0.502 | −0.06 | −0.09 | 0.433 |
| Gender | −0.08 | −0.83 | 0.363 | −0.22 | −2.72 | 0.011 | −0.31 | −0.43 | 0.000 |
| Age (Adolescence) | 0.02 | 0.21 | 0.809 | 0.14 | 1.41 | 0.191 | 0.23 | 0.26 | 0.014 |
| Date of 1st Assessment | −0.06 | −0.05 | 0.394 | −0.04 | −0.04 | 0.572 | −0.05 | −0.01 | 0.380 |
| Age (Pandemic) | −0.03 | −0.27 | 0.701 | −0.13 | −1.19 | 0.200 | −0.02 | −0.02 | 0.823 |
| Generalized Anxiety | 0.63 | 1.26 | 0.000 | 0.55 | 1.21 | 0.000 | 0.36 | 0.09 | 0.003 |
| Social Anxiety | −0.33 | −0.55 | 0.026 | −0.54 | −1.03 | 0.001 | −0.35 | −0.08 | 0.012 |
| Anxiety Slope |
Perceived Stress Slope |
COVID-Related Worries Slope |
|||||||
| Maternal Education | −0.04 | −0.09 | 0.712 | 0.16 | 0.33 | 0.443 | −0.01 | 0.00 | 0.920 |
| Maternal Ethnicity | 0.17 | 0.51 | 0.228 | 0.01 | 0.02 | 0.970 | 0.18 | 0.08 | 0.237 |
| Gender | 0.08 | 0.23 | 0.526 | −0.12 | −0.35 | 0.516 | 0.07 | 0.03 | 0.558 |
| Age (Adolescence) | −0.11 | −0.26 | 0.456 | −0.38 | −0.93 | 0.128 | −0.18 | −0.06 | 0.214 |
| Date of 3rd Assessment | −0.13 | −0.04 | 0.195 | −0.23 | −0.06 | 0.207 | 0.15 | 0.01 | 0.109 |
| Age (Pandemic) | 0.07 | 0.14 | 0.651 | 0.35 | 0.78 | 0.117 | 0.33 | 0.10 | 0.005 |
| Generalized Anxiety | −0.34 | −0.18 | 0.195 | −0.17 | −0.09 | 0.690 | 0.08 | 0.01 | 0.692 |
| Social Anxiety | 0.53 | 0.24 | 0.038 | 0.86 | 0.40 | 0.033 | 0.12 | 0.01 | 0.549 |
Note: Generalized Anxiety and Social Anxiety are latent factors composed of pre-pandemic clinical diagnoses, parent and child reports of anxiety; Gender is coded as 0 = Girls and 1 = Boys; Maternal Ethnicity is coded as Non-Hispanic Caucasian = 1 and Other = 0; Maternal education was coded as High school graduate = 0, College Graduate = 1, Graduate school graduate = 2, and Other = missing. All models had acceptable fit: Anxiety model (χ2(72) = 106.88, p = .005, RMSEA = .04, SRMR = .07, CFI = .94), Perceived Stress model (χ2(72) = 121.47, p < .001, RMSEA = .05, SRMR = .08, CFI = .91), and COVID-related worries model (χ2(72) = 101.51, p = .013, RMSEA = .04, SRMR = .08, CFI = .95). COVID is the coronavirus disease of 2019. β and b represent the standardized and unstandardized regression coefficients, respectively. p represents the p value.
We found similar patterns for the perceived stress trajectories. As shown in Figure 2B and Table 2, we found that generalized anxiety in adolescence predicted a larger perceived stress intercept (b= 1.21, p < .001), but did not predict the slope (b= −.09, p = .690). That is, after accounting for the effects of social anxiety, adolescents higher in pre-pandemic generalized anxiety, compared to those lower in generalized anxiety, displayed greater stress in Month 1 of the pandemic, maintaining this difference across the following months. In contrast, social anxiety in adolescence predicted a smaller perceived stress intercept (b= −1.03, p = .001), but had a positive effect on the value of the slope (b= 0.40, p = .033). Namely, while accounting for the effects of generalized anxiety, adolescents higher in pre-pandemic social anxiety, compared to adolescents lower in social anxiety, displayed less stress in Month 1 of the pandemic. However, in the following months, as the sample decreased in stress on average, adolescents higher in social anxiety remained stable across time, compared to adolescents lower in social anxiety – reducing the differences observed initially.
Finally, as shown in Figure 2C and Table 2, for the COVID-related worries trajectory, we found that generalized anxiety in adolescence predicted a larger intercept (b= 0.09, p = .003), but did not predict the slope (b= .01, p = .692). Namely, after accounting for the effects of social anxiety, adolescents higher in pre-pandemic generalized anxiety, compared to those lower in generalized anxiety, reported greater levels of COVID-related worries in Month 1 of the pandemic, maintaining this difference during the following months. In contrast, social anxiety in adolescence predicted a smaller intercept (b= −0.08, p = .012), and did not predict the slope (b= .01, p = .549). Specifically, while accounting for the effects of generalized anxiety, adolescents higher in pre-pandemic social anxiety, compared to those lower in social anxiety, reported less COVID-related worries in Month 1 of the pandemic, and maintained this difference across the following months.
Supplemental Sensitivity Analyses
As a further exploratory test of the specificity of our results predicting COVID-related worries, we examined social-related worries (i.e., concerns about having to stay at home, not seeing friends in person, and missing social events; items 4, 5, & 18 on The CASPE Questionnaire; αs > .74) and illness-related worries (e.g., worries about getting sick or their family getting sick; items 3, 6-9, & 11 on The CASPE Questionnaire; αs > .91), separately. We found that the dissociation between generalized and social anxiety was only present for social-related worries (e.g., having to stay home) and not for illness-related worries. Specifically generalized anxiety in adolescence predicted a larger social-related worries intercept (b= 0.13, p = .001), whereas social anxiety predicted a smaller intercept (b= −0.16, p = .001), and neither predicted the slope (ps > .396). Notably, neither generalized nor social anxiety predicted the intercept and slope of illness-related worries (ps > .134).
In exploratory analyses, we evaluated potential gender differences. To do this, we first fit a multi-group model where all the regression parameters were estimated separately for male and female adolescents and tested whether constraining the regression paths to be equal across groups significantly worsened model fit using a chi-square difference test (Satorra & Bentler, 2001). We performed this separately for each outcome and did not observe a significant difference across models (anxiety Δχ2(14) = 7.72, p = .904; perceived stress Δχ2(14) = 10.87, p = .700; COVID-related worries Δχ2(14) = 19.65, p = .142), indicating that the relations between pre-COVID predictors and outcomes during the pandemic did not differ between male and female adolescents. Moreover, as sensitivity analyses examining potential non-linear relations, we modeled the latent trajectories using the means of the sample – such that we used 0, 1, and 1.93 (rather than 0, 1, & 2) for anxiety; 0, 1, 1.73 for perceived stress; and 0, 1, 1.69 for COVID-related worries. As shown in the supplement (Table S3), the fit of these models were similar to the original models testing a linear trajectory. Moreover, the results using these non-linear trajectories and the linear trajectories were comparable, leading to the same conclusions, suggesting that our results are robust to this methodological decision. In another sensitivity analysis, we explored the potential impact of the variability in age in the adolescent assessment by examining interactions between the social and generalized anxiety factors and the age of the participants during the adolescent assessment. As shown in the supplement (Table S4), none of the interactions were significant, suggesting that the age of assessment in adolescence did not significantly impact the main results.
Finally, in order to examine if the results found were specific to the pandemic, we conducted the same analyses in a subsample of participants (n = 56) that reported on their anxiety using the SCARED (Birmaher et al., 1997) right before the start of the pandemic in February 2020. As shown in the supplement (Table S5), examining relations between anxiety in adolescence and this assessment before the pandemic, we found that both social and generalized anxiety adolescent variables are longitudinally related with the generalized anxiety scale from the SCARED (except clinical diagnosis of social anxiety – albeit this was with a small sample, n = 37). Moreover, as shown in Table S6, when examining these relations in a SEM model including both social and generalized anxiety as latent predictors of later anxiety, only generalized anxiety was predictive of later anxiety. Although social anxiety was not significantly related after accounting for generalized anxiety, social anxiety was not significantly negatively related to anxiety as observed at the start of the pandemic – a few months after. The results from this analysis suggests that generalized and social anxiety showed more similar predictions to anxiety before the pandemic than the pattern of relations observed shortly after during the initial phase of the pandemic. Importantly, this analysis is only supplemental and should be interpreted with caution as it is only with a subsample of participants and does not use the same anxiety scale as the main analyses.
Discussion
The current study considers the unique effects of pre-pandemic generalized and social anxiety on the trajectories of anxiety, perceived stress, and COVID-related worries during three initial months of the COVID-19 pandemic. The results suggest that individuals higher in pre-pandemic generalized anxiety, compared to those lower in generalized anxiety, experienced greater levels of initial anxiety, stress, and COVID-related worries and maintained these differences across three months’ time. In contrast, individuals higher compared to lower in pre-pandemic social anxiety experienced lower levels of initial anxiety, stress, and COVID-related worries, but these initial differences in anxiety and stress were reduced in the following months of the pandemic. Our results highlight the differential effects of pre-pandemic factors on trajectories of psychological distress during the first few months of the pandemic. Further, these findings have important implications for early identification and intervention efforts to support at-risk individuals at times of heightened stress.
The results from the unconditional growth curve models indicated average trajectories of anxiety, perceived stress, and COVID-related worries with higher levels at the first assessment (April-May) and then decreased levels in the subsequent months of the pandemic (Figure 1). These results are consistent with recent longitudinal evidence from the United States and Europe indicating that, on average, anxiety and stress peaked during the initial months of the pandemic and was then followed by a significant decline in the following months (Daly et al., 2020; Fancourt et al., 2021; Hawes et al., 2021). This pattern may reflect an acute increase in individuals’ psychological distress because of the uncertainty about the virus and the public health restriction measures put in place to mitigate its spread. Following this increase, individuals’ distress typically decreased during the ensuing months. One possibility is that the observed decreases in distress reflect individuals’ resilience and ability to adapt to the pandemic and restrictions eased in the following months. However, with our current data, we are not able to provide causal interpretations, as there might be other factors that led to the observed decreases in psychological distress (e.g., transition from school to summer months). Although other factors not related to the pandemic may also explain the patterns observed, we believe that the pandemic likely played an important role given that similar trajectories of initial increases in distress, followed by decreases over the summer, were observed around the world and across age groups (for a review, see Aknin et al., 2021).
Importantly, further analysis revealed that these average trajectories might not adequately represent all individuals. Knowledge of pre-pandemic risk factors helped describe individuals at the highest risk for psychological distress during the pandemic. Generalized anxiety in adolescence, after accounting for its shared effects with social anxiety, uniquely predicted higher levels of initial anxiety, stress, and COVID-related worries and predicted maintenance of these levels during three months at the start of the pandemic. These results closely parallel previous studies which have found that previous overall (total) anxiety or internalizing problems predicted increased stress and anxiety during the pandemic, relative to before the pandemic (Shanahan et al., 2020), or increased anxiety trajectories during the pandemic (Hawes et al., 2021). Our results suggest that this pattern of results may reflect the experiences of individuals high in generalized anxiety, who may be more prone to worrying and catastrophizing about the uncertainty at the start of the pandemic across several life domains (e.g., future, health, finances). As such, focusing on pre-existing levels of generalized anxiety may particularly be important for identifying individuals at risk for psychological distress during novel stressful life events, such as the COVID-19 pandemic.
In contrast, social anxiety in adolescence, after accounting for the shared effects with generalized anxiety, predicted lower levels of initial anxiety, stress, and COVID-related worries. However, in the following months, as the sample on average decreased in anxiety and stress, adolescents higher in social anxiety remained stable across time compared to adolescents lower in social anxiety, decreasing these initial differences. These findings support popular press coverage (Gold, 2020; Richtel, 2021; Schroeder, 2020) and hypotheses of other researchers based on clinical experiences speculating that the initial decrease in social interaction was not as distressing for those high in social anxiety (Bruining et al., 2020; Cost et al., 2021; Morrissette, 2021). To our knowledge, this is the first empirical evidence documenting a dissociation during the pandemic between different types of anxiety, such that the unique effects of some forms of anxiety may predict less psychological distress at the start of the pandemic. Individuals with higher levels of social anxiety before the pandemic – provided they did not have elevated generalized anxiety – likely experienced an initial improvement or at least not an increase in anxiety, stress, and COVID-related worries, compared to individuals lower in social anxiety. This may be because individuals high in social anxiety experienced a decrease in the very social interactions and situations that are anxiety-provoking for them, plausibly leading to reductions in psychological distress. Conversely, individuals lower in social anxiety were likely initially anxious and concerned about the uncertainty of not seeing others and missing out on important social events (e.g., weddings and graduation parties). Our supplemental exploratory analyses separately examining social-related worries (e.g., not seeing friends in person) and illness-related worries support that interpretation, as the dissociation between generalized and social anxiety was evident for social-related worries, while it was not present for illness-related worries. Similarly, a recent study found greater decreases in mood during the pandemic for young adults higher in extraversion, compared to those lower in extraversion (Rettew et al., 2021).
These findings are relevant to broader discussions in anxiety disorder research, such as debates around the similarities and differences between social anxiety disorder and generalized anxiety disorder. Some suggest that differences among anxiety symptoms during adolescence are not clinically meaningful (Rutter, 2011), whereas others suggest that these differences might predict differential outcomes (Pine, 2007, 2011). Other positions fall somewhere in between, suggesting the existence of both shared and more specific features (Kotov et al., 2021). The most consistent evidence of specificity arises for a domain involving fears, including symptoms of social anxiety disorder, and a domain involving distress, including symptoms of generalized anxiety disorder. The current findings, demonstrating distinct longitudinal patterns related to social and generalized anxiety disorder symptoms, are consistent with previous work demonstrating unique features of these two anxiety-related symptom domains.
From a temporal perspective, our data also suggest that the difference in psychological functioning during the pandemic based on pre-pandemic social anxiety was particularly evident at the start of the pandemic, when stay-at-home orders were first put in place and schools as well as other extracurricular activities were halted. However, as individuals adapted to the pandemic and its associated restrictions, and re-opening progressively occurred, the differences in anxiety and stress based on social anxiety were no longer apparent. This highlights the importance of specifying when during prolonged stressful events risk or protective factors may significantly impact mental health, speaking to the need for prospective longitudinal research during times of crisis such as COVID-19. Importantly, the lack of differences in anxiety and stress based on social anxiety during the last assessment also suggests that the lower psychological distress associated with social anxiety may be relatively short lived, emphasizing the need for continued mental health support (e.g., therapy) or treatment during the pandemic, despite improvements in mental health at the outset. It is possible that, as the pandemic continued and social interactions adapted (e.g., virtual or masked outdoor social gatherings), social anxiety symptoms once again increased, as individuals felt the need to attend and participate in social interactions. Finally, our data did not capture the in-person re-opening of schools and universities. Future research should examine the mental health impact of returning to in-person social situations, particularly among individuals high in social anxiety, after the prolonged reduction in such events due to the pandemic.
The present study has several important limitations that should be considered when interpreting results. It is important to note that participants in the current study were relatively homogenous (i.e., largely Caucasian from moderate-to-high SES households) and few experienced significant COVID-related health issues during the time sampled (i.e., themselves or their family members getting seriously sick or hospitalized), relative to the documented disproportionate effects of the pandemic on lower-income, non-white individuals (Garg et al., 2020; Perry et al., 2021). As such, care should be taken when generalizing our results to other populations, and in particular, it should not be used as a population estimate for the prevalence of heightened stress and anxiety during the pandemic. Although our study had three assessments during the pandemic, allowing us to examine trajectories, we did not have an assessment directly before the pandemic; thus, we could not estimate absolute changes from before to during the pandemic. However, we were able to capture the decreases in individuals’ anxiety, stress, and worries from our first pandemic assessment – which, based on data from other studies, we believe was close to the peak of anxiety and stress in the larger population. Although having a multi-method assessment of pre-pandemic anxiety and a longitudinal design are strengths of our study, this led to missing data across measures. To reduce the potential biases created by missing data, we employed a statistical approach that utilizes all of the available data, controlling for demographic differences associated with the likelihood of missing data.
In conclusion, not all young adults high in pre-pandemic adolescent anxiety experienced elevated anxiety during the pandemic. The unique effects of social anxiety suggest an initial reduction in anxiety, stress, and COVID-related concerns, for adolescents high in social anxiety compared to adolescents lower in social anxiety. In contrast, the unique effects of generalized anxiety suggest that individuals higher in generalized anxiety, compared to those lower in generalized anxiety, experienced more anxiety, stress, and COVID-related worries during the three initial months of the pandemic. Our study provides a more nuanced picture regarding which specific types of anxiety may lead to increased vs. reduced anxiety, stress, and worries, as well as when during the pandemic these different forms of prior anxiety may be most predictive. Our study highlights the importance of considering pre-COVID predictors in response to the pandemic and its associated restrictions (e.g., stay-at-home orders). Moreover, our findings have clinical implications for early identification of individuals at risk and may help inform prevention and intervention efforts aimed to alleviate different forms of anxiety problems.
Supplementary Material
Acknowledgements
We thank the many research assistants involved in collecting the data presented in this manuscript. We also thank the participating families without whom the study would not have been possible. This research was supported by a Coronavirus Research Seed Grant from the University of Maryland and grants from the National Institute of Health (MH093349 and HD017899) awarded to NAF and the Intramural Research Program at the National Institute of Mental Health (ZIA-MH-002782) awarded to DSP.
Footnotes
The authors report no biomedical financial interests or potential conflicts of interest.
References
- Aknin L, Neve J-ED, Dunn E, Fancourt D, Goldberg E, Helliwell J, Jones SP, Karam E, Layard R, Lyubomirsky S, Rzepa A, Saxena S, Thornton E, VanderWeele T, Whillans A, Zaki J, Caman OK, & Amour YB (2021). Mental Health During the First Year of the COVID-19 Pandemic: A Review and Recommendations for Moving Forward. PsyArXiv. 10.31234/osf.io/zw93g [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, & Neer SM (1997). The Screen for Child Anxiety Related Emotional Disorders (SCARED): Scale construction and psychometric characteristics. Journal of the American Academy of Child and Adolescent Psychiatry, 36(4), 545–553. 10.1097/00004583-199704000-00018 [DOI] [PubMed] [Google Scholar]
- Blair K, Shaywitz J, Smith BW, Rhodes R, Geraci M, Jones M, McCaffrey D, Vythilingam M, Finger E, Mondillo K, Jacobs M, Charney DS, Blair R. j. r., Drevets WC, & Pine DS (2008). Response to Emotional Expressions in Generalized Social Phobia and Generalized Anxiety Disorder: Evidence for Separate Disorders. American Journal of Psychiatry, 165(9), 1193–1202. 10.1176/appi.ajp.2008.07071060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruining H, Bartels M, Polderman TJC, & Popma A (2020). COVID-19 and child and adolescent psychiatry: An unexpected blessing for part of our population? European Child & Adolescent Psychiatry, 30, 1139–1140. 10.1007/s00787-020-01578-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1994). Perceived stress scale. Measuring Stress: A Guide for Health and Social Scientists, 10(2), 1–2. [Google Scholar]
- Cost KT, Crosbie J, Anagnostou E, Birken CS, Charach A, Monga S, Kelley E, Nicolson R, Maguire JL, Burton CL, Schachar RJ, Arnold PD, & Korczak DJ (2021). Mostly worse, occasionally better: Impact of COVID-19 pandemic on the mental health of Canadian children and adolescents. European Child & Adolescent Psychiatry. 10.1007/s00787-021-01744-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler MÉ, Lane RI, Petrosky E, Wiley JF, Christensen A, Njai R, Weaver MD, Robbins R, Facer-Childs ER, & Barger LK (2020). Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. Morbidity and Mortality Weekly Report, 69(32), 1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly M, Sutin AR, & Robinson E (2020). Longitudinal changes in mental health and the COVID-19 pandemic: Evidence from the UK Household Longitudinal Study. Psychological Medicine, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders CK, & Bandalos D (2001). The Relative Performance of Full Information Maximum Likelihood Estimation for Missing Data in Structural Equation Models. Structural Equation Modeling: A Multidisciplinary Journal, 8(3), 430–457. 10.1207/S15328007SEM0803_5 [DOI] [Google Scholar]
- Fancourt D, Steptoe A, & Bu F (2021). Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: A longitudinal observational study. The Lancet Psychiatry, 8(2), 141–149. 10.1016/S2215-0366(20)30482-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garg S, Kim L, Whitaker M, O’Halloran A, Cummings C, Holstein R, Prill M, Chai SJ, Kirley PD, Alden NB, Kawasaki B, Yousey-Hindes K, Niccolai L, Anderson EJ, Openo KP, Weigel A, Monroe ML, Ryan P, Henderson J, … Fry A (2020). Hospitalization Rates and Characteristics of Patients Hospitalized with Laboratory-Confirmed Coronavirus Disease 2019—COVID-NET, 14 States, March 1–30, 2020. Morbidity and Mortality Weekly Report, 69(15), 458–464. 10.15585/mmwr.mm6915e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold J (2020). Feeling Less Anxiety Since The Coronavirus Lockdown? You’re Not Alone. Forbes. https://www.forbes.com/sites/jessicagold/2020/06/08/feeling-less-anxiety-since-the-coronavirus-lockdown-youre-not-alone/ [Google Scholar]
- Hane AA, Fox N. a, Henderson H. a, & Marshall PJ (2008). Behavioral reactivity and approach-withdrawal bias in infancy. Developmental Psychology, 44(5), 1491–1496. 10.1037/a0012855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawes MT, Szenczy AK, Olino TM, Nelson BD, & Klein DN (2021). Trajectories of depression, anxiety and pandemic experiences; A longitudinal study of youth in New York during the Spring-Summer of 2020. Psychiatry Research, 298, 113778. 10.1016/j.psychres.2021.113778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holman EA, Thompson RR, Garfin DR, & Silver RC (2020). The unfolding COVID-19 pandemic: A probability-based, nationally representative study of mental health in the United States. Science Advances, 6(42), eabd5390. 10.1126/sciadv.abd5390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes EA, O’Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, Ballard C, Christensen H, Cohen Silver R, Everall I, Ford T, John A, Kabir T, King K, Madan I, Michie S, Przybylski AK, Shafran R, Sweeney A, … Bullmore E (2020). Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. The Lancet Psychiatry, 7(6), 547–560. 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, & Ryan N (1997). Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry, 36(7), 980–988. 10.1097/00004583-199707000-00021 [DOI] [PubMed] [Google Scholar]
- Kessel EM, Kujawa A, Hajcak Proudfit G, & Klein DN (2015). Neural reactivity to monetary rewards and losses differentiates social from generalized anxiety in children. Journal of Child Psychology and Psychiatry, 56(7), 792–800. 10.1111/jcpp.12355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotov R, Krueger RF, Watson D, Cicero DC, Conway CC, DeYoung CG, Eaton NR, Forbes MK, Hallquist MN, Latzman RD, Mullins-Sweatt SN, Ruggero CJ, Simms LJ, Waldman ID, Waszczuk MA, & Wright AGC (2021). The Hierarchical Taxonomy of Psychopathology (HiTOP): A Quantitative Nosology Based on Consensus of Evidence. Annual Review of Clinical Psychology, 17(1), annurev-clinpsy-081219-093304. 10.1146/annurev-clinpsy-081219-093304 [DOI] [PubMed] [Google Scholar]
- Ladouceur CD (2020). COVID-19 Adult Symptom & Psychological Experience Questionnaire. https://www.nlm.nih.gov/dr2/CASPE_AdolSelfReport_Qualtrics.pdf [Google Scholar]
- León MIG (2021). Disminución de la ansiedad en las víctimas del bullying durante el confinamiento por el COVID-19. Revista de Educación a Distancia (RED), 21(65), Article 65. 10.6018/red.439601 [DOI] [Google Scholar]
- Lorenzo NE, Zeytinoglu S, Morales S, Listokin J, Almas AN, Degnan KA, Henderson H, Chronis-Tuscano A, & Fox NA (2021). Transactional Associations Between Parent and Late Adolescent Internalizing Symptoms During the COVID-19 Pandemic: The Moderating Role of Avoidant Coping. Journal of Youth and Adolescence, 50(3), 459–469. 10.1007/s10964-020-01374-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar SS, Ebbert AM, & Kumar NL (2021). Risk and resilience during COVID-19: A new study in the Zigler paradigm of developmental science. Development and Psychopathology, 33(2), 565–580. [DOI] [PubMed] [Google Scholar]
- McGinty EE, Presskreischer R, Anderson KE, Han H, & Barry CL (2020). Psychological Distress and COVID-19–Related Stressors Reported in a Longitudinal Cohort of US Adults in April and July 2020. JAMA, 324(24), 2555. 10.1001/jama.2020.21231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mennin DS, McLaughlin KA, & Flanagan TJ (2009). Emotion regulation deficits in generalized anxiety disorder, social anxiety disorder, and their co-occurrence. Journal of Anxiety Disorders, 23(7), 866–871. 10.1016/j.janxdis.2009.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell AM, Crane PA, & Kim Y (2008). Perceived stress in survivors of suicide: Psychometric properties of the Perceived Stress Scale. Research in Nursing & Health, 31(6), 576–585. 10.1002/nur.20284 [DOI] [PubMed] [Google Scholar]
- Morales S, Miller NV, Troller-Renfree SV, White LK, Degnan KA, Henderson HA, & Fox NA (2020). Attention bias to reward predicts behavioral problems and moderates early risk to externalizing and attention problems. Development and Psychopathology, 32(2), 397–409. 10.1017/S0954579419000166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morales S, Tang A, Bowers ME, Miller NV, Buzzell GA, Smith E, Seddio K, Henderson HA, & Fox NA (2021). Infant temperament prospectively predicts general psychopathology in childhood. Development and Psychopathology, 1–10. 10.1017/S0954579420001996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrissette M (2021). School Closures and Social Anxiety During the COVID-19 Pandemic. Journal of the American Academy of Child & Adolescent Psychiatry, 60(1), 6–7. 10.1016/j.jaac.2020.08.436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry BL, Aronson B, & Pescosolido BA (2021). Pandemic precarity: COVID-19 is exposing and exacerbating inequalities in the American heartland. Proceedings of the National Academy of Sciences, 118(8). 10.1073/pnas.2020685118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pine DS (2007). Research Review: A neuroscience framework for pediatric anxiety disorders. Journal of Child Psychology and Psychiatry, 48(7), 631–648. 10.1111/j.1469-7610.2007.01751.x [DOI] [PubMed] [Google Scholar]
- Pine DS (2011). Commentary: Diagnosis and classification: There must be something left about which to argue – reflections on Rutter (2011). Journal of Child Psychology and Psychiatry, 52(6), 663–664. 10.1111/j.1469-7610.2011.02382.x [DOI] [PubMed] [Google Scholar]
- Prati G, & Mancini AD (2021). The psychological impact of COVID-19 pandemic lockdowns: A review and meta-analysis of longitudinal studies and natural experiments. Psychological Medicine, 51(2), 201–211. 10.1017/S0033291721000015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prime H, Wade M, & Browne DT (2020). Risk and resilience in family well-being during the COVID-19 pandemic. American Psychologist, 75(5), 631–643. 10.1037/amp0000660 [DOI] [PubMed] [Google Scholar]
- R Development Core Team. (2008). R: A language and environment for statistical computing. http://www.R-project.org.
- Rettew DC, McGinnis EW, Copeland W, Nardone HY, Bai Y, Rettew J, Devadenam V, & Hudziak JJ (2021). Personality trait predictors of adjustment during the COVID pandemic among college students. PLOS ONE, 16(3), e0248895. 10.1371/journal.pone.0248895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Revelle WR (2017). psych: Procedures for personality and psychological research. [Google Scholar]
- Richtel M (2021, March 17). The U.S. Is Opening Up. For the Anxious, That Comes With a Cost. The New York Times. https://www.nytimes.com/2021/03/17/health/US-reopening-anxiety-ocd.html [Google Scholar]
- Rosseel Y (2012). Lavaan: An R package for structural equation modeling and more. Version 0.5–12 (BETA). Journal of Statistical Software, 48(2), 1–36. [Google Scholar]
- Rutter M (2011). Research Review: Child psychiatric diagnosis and classification: concepts, findings, challenges and potential. Journal of Child Psychology and Psychiatry, 52(6), 647–660. 10.1111/j.1469-7610.2011.02367.x [DOI] [PubMed] [Google Scholar]
- Salum GA, Mogg K, Bradley BP, Gadelha A, Pan P, Tamanaha AC, Moriyama T, Graeff-Martins AS, Jarros RB, Polanczyk G, do Rosário MC, Leibenluft E, Rohde LA, Manfro GG, & Pine DS (2013). Threat bias in attention orienting: Evidence of specificity in a large community-based study. Psychological Medicine, 43(4), 733–745. 10.1017/S0033291712001651 [DOI] [PubMed] [Google Scholar]
- Satorra A, & Bentler PM (2001). A scaled difference chi-square test statistic for moment structure analysis. Psychometrika, 66(4), 507–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schroeder J (2020, August 10). Opinion ∣ What if Some Kids Are Better Off at Home? The New York Times. https://www.nytimes.com/2020/08/10/opinion/coronavirus-school-closures.html [Google Scholar]
- Shanahan L, Steinhoff A, Bechtiger L, Murray AL, Nivette A, Hepp U, Ribeaud D, & Eisner M (2020). Emotional distress in young adults during the COVID-19 pandemic: Evidence of risk and resilience from a longitudinal cohort study. Psychological Medicine, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW, & Löwe B (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- Wickham H (2016). ggplot2: Elegant graphics for data analysis. Springer. [Google Scholar]
- Yuan KH, & Bentler PM (2000). Three Likelihood-Based Methods for Mean and Covariance Structure Analysis with Nonnormal Missing Data. Sociological Methodology, 30, 165–200. [Google Scholar]
- Zeytinoglu S, Morales S, Lorenzo NE, Chronis-Tuscano A, Degnan KA, Almas AN, Henderson H, Pine DS, & Fox NA (2021). A Developmental Pathway From Early Behavioral Inhibition to Young Adults’ Anxiety During the COVID-19 Pandemic. Journal of the American Academy of Child & Adolescent Psychiatry, 60(10), 1300–1308. 10.1016/j.jaac.2021.01.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeytinoglu S, Neuman KJ, Degnan KA, Almas AN, Henderson H, Chronis-Tuscano A, Pine DS, & Fox NA (2021). Pathways from maternal shyness to adolescent social anxiety. Journal of Child Psychology and Psychiatry, jcpp.13477. 10.1111/jcpp.13477 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.