Abstract
Juvenile obesity is associated with a lower self-concept. Given the continued prevalence of obesity, we examined the secular trend of body mass index standard deviation score (BMI-SDS) and self-concept in participants of a German weight management programme (n = 242, 53.3% female, mean age 12.5 ± 2.1 years, mean BMI-SDS 2.45 ± 0.46) over a period of 15 years. Anthropometric data, physical fitness (watt/kg), and demographic data were assessed. The years 2005 to 2020 were grouped into six sections containing a mean of n = 40 participants. The questionnaire for the assessment of self and competence in children (FSK-K) was used to assess the following domains: “scholastic competence”, “social competence”, “physical appearance”, “global self-worth”, and “behavioural conduct”. No significant between-group differences in self-assessment across self-concept domains were found. In all time periods, heavier children assigned the lowest rating to physical appearance. Social competence increased with higher physical fitness. Even though no negative trend in the self-concept of children with obesity was found in this cohort, the findings confirmed an association between juvenile overweight/obesity and lower physical self-concept, and between a better social competence and increasing physical fitness. Accompanying psychosocial care, therefore, rightly remains an important pillar of obesity therapy.
Keywords: childhood obesity, psychosocial distress, secular trend, self-concept, physical appearance, physical fitness
1. Introduction
In 2016, 124 million children (50 million girls and 74 million boys) were obese worldwide, while another 123 million children were overweight [1]. In Germany, 15.4% of children were overweight and 5.9% of them were obese between 2014 and 2017, according to KiGGS Wave 2 (“Children and Adolescents Health Survey”; authors translation) of the Robert Koch Institute [2]. The recent coronavirus pandemic (COVID-19) has exacerbated this trend, especially in families with lower socioeconomic status and particularly in children and adolescents who were already overweight pre-pandemic [3]. Another German study confirmed these findings, indicating that during the pandemic there was excess weight gain in every sixth child [4].
In addition to physical co-morbidities, such as arterial hypertension, elevated lipids [5,6,7], and the presence of insulin resistance—even manifested as type-2 diabetes [8]—affected children and adolescents can be particularly burdened by psychosocial issues. Thus, 40% suffer from anxiety disorders, 15% have somatization disorders, and 17% suffer from eating disorders [9]. Additional issues include low self-esteem [10], discrimination and stigmatization [11], social exclusion and deficits in social skills [12,13], bullying [14], difficulties in school matters (for example, negative attitudes towards children with higher bodyweight were observed among teachers) [15], other psychological disorders, and body dissatisfaction, as well as lower health-related quality of life [13]. Topçu et al. [16] applied the Piers–Harris children’s self-concept scale and found that children who were obese experienced more psychiatric disorders than their peers without obesity. In sum, weight-related stressors lead to increased social withdrawal, further weight gain [17], and depressed mood [18], and manifest as depression in 10.4% of cases [19].
Given the increasing rates of obesity, it is of interest whether this is accompanied by a parallel increase in psychosocial distress. However, data regarding the secular trend of mental comorbidities accompanying juvenile obesity are sparse.
Family-based multicomponent weight management programmes, with behavioural, dietary, and physical activity components, are the best practice for achieving successful weight loss and alleviating the associated psychosocial burden in affected children and adolescents [20]. However, if the prevalence of psychosocial problems has increased in parallel with growing obesity rates in recent years, programmes may need to be adapted to address this problem.
The primary aim of this analysis was therefore to investigate whether the body mass index standard deviation score (BMI-SDS) and self-concepts of children and adolescents participating in a weight management programme have changed over the past 15 years. As a secondary objective, we examined predictors of self-concept domains across different time spans to uncover any trends.
2. Materials and Methods
2.1. Population Sample/Study Design
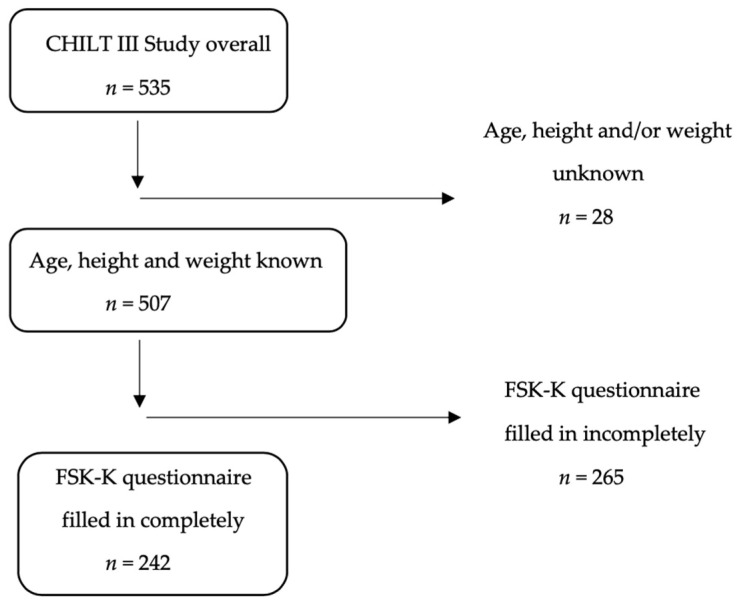
Data from the children’s health interventional trial (CHILT) III, an outpatient, multimodal, family-based weight management programme for children and adolescents aged eight to sixteen years [21] (n = 535), were examined. The CHILT Project is registered in the German Clinical Trials Register under ID DRKS00026785. To be included in the study, complete records on sex, age, height, and weight, as well as the FSK-K questionnaire (questionnaire for the assessment of self and competence in children) of the participants had to be available (n = 242; Figure 1).
Figure 1.
Inclusion criteria for the study population.
The years between 2005 and 2020 were divided into six time periods of two to three years each. Each time span or period contained a similar number of study participants, with a mean of n = 40, a maximum of n = 45 (2015–2017) and a minimum of n = 34 (2009–2011) participants per group. (Table 1) The first period of available data from 2003 to 2004 was excluded from the evaluation due to insufficient data.
Table 1.
Population characteristics.
| Total (n = 242) |
Boys (n = 113) |
Girls (n = 129) |
p-Value | |
|---|---|---|---|---|
| (1) Sex n (%) | 113 (46.7%) | 129 (53.3%) | ||
| (2) Age (in years) | 12.5 ± 2.1 (242) | 12.7 ± 2.1 (113) | 12.3 ± 2.2 (129) | 0.110 † |
| (3) Height (in m) | 1.59 ± 0.11 (242) | 1.62 ± 0.12 (113) | 1.56 ± 0.10 (129) | <0.001 † |
| (4) Weight (in kg) | 76.4 ± 19.6 (242) | 81.3 ± 22.3 (113) | 72.1 ± 15.8 (129) | <0.001 † |
| (5) BMI (in kg/m2) | 30.0 ± 4.8 (242) | 30.7 ± 5.4 (113) | 29.4 ± 4.2 (129) | 0.038 † |
| (6) BMI-SDS | 2.45 ± 0.46 (242) | 2.45 ± 0.47 (113) | 2.45 ± 0.45 (129) | 0.974 † |
| (7) Adolescent status | ||||
| <13 years old | 135 (55.8%) | 57 (50.44%) | 78 (60.47%) | |
| ≥13 years old | 107 (44.2%) | 56 (49.56%) | 51 (39.53%) | 0.117 ‡ |
| Overall (n = 205) |
Boys (n = 97) |
Girls (n = 108) |
||
| (8) Migration background (yes) | 23 (11.2%) | 10 (10.3%) | 13 (12.0%) | 0.696 ‡ |
| (9) Media consumption (h/day) |
3.23 ± 3.27 (205) | 3.45 ± 3.82 (97) | 3.02 ± 2.69 (108) | 0.349 † |
The data are presented as the mean ± SD; BMI = body mass index; BMI SDS = body mass index standard deviation score; p-values calculated with the † unpaired t-test; ‡ Chi square test.
Of the n = 242 participants, 46.7% were male (n = 113) and 53.3% were female (n = 129). Participants were on average 12.5 ± 2.1 years old, had a mean height of 1.59 ± 0.11 m, weighed an average of 76.4 ± 19.6 kg, and had a mean BMI of 30.0 ± 4.8 kg/m2. The mean BMI-SDS was 2.45 ± 0.46. Overall, 55.8% were younger than 13 years of age (pre-adolescent), while 44.2% were 13 years of age or older (adolescent) [22]. Sex differences can be found in Table 1. Descriptive statistics of all time clusters separated by sex can be found in the Supplemental Materials (Table S1).
2.2. Anthropometric Data
The height and weight (including light sportswear) of the study participants were measured barefoot. Standard calibrated scales were used (weight: Seca® scale, type 225; height Seca® scale, type 761). Following Kromeyer-Hauschild et al., the children were classified according to German percentiles, i.e., those in the 90% percentile and above were classified as overweight, while those in the 97% percentile and above were classified as obese [23]. BMI standard deviation scores (BMI-SDS) were expressed age- and sex-specifically according to the LMS method for non-normally distributed sizes. M, L, and S were the individual parameters for the child’s age and sex.
Adolescent status was distinguished by age: below 13 years (pre-adolescent) or 13 years and above (adolescent) [24].
2.3. Demographics and Media Consumption
Demographic data, socioeconomic status, and information on family lifestyle were requested using a standardized parental questionnaire [25,26]. Migration background was determined by the language spoken at home (yes or no to speaking German) [27].
Media consumption (hours per day) was assessed by asking parents to estimate their child’s total daily engagement with television, video games, internet use, and mobile phone, as well as time spent listening to music.
2.4. Self-Concept
The assessment of self-concept was completed using the “Questionnaire for the Assessment of Self and Competence for Children (FSK-K)” by Wünsche and Schneewind, a German version of Harter’s Self-Perception Profile for Children (SPPC) [28,29]. The 30 items were divided into five domains of six questions each: “scholastic competence”, “social competence”, “physical appearance”, “global self-worth”, and “behavioural conduct”. The items were presented as positively or negatively worded statements. Each participant had to choose between “true for me” or “somewhat true for me” for each statement. The answers were coded from 1 to 4, with 4 always representing the most positive response possible. For example, the statement “I have many friends” could be answered with “true for me” (coded 4) or “somewhat true for me” (coded 3). This statement’s counterpart, “I do not have many friends”, could be answered with “somewhat true for me” (coded 2) or “true for me” (coded 1). The data were then recoded, with the highest domain-specific competence defined as 100 on the mean scale. Thus, the participants’ self-concept ratings could be compared across domains using their mean values. The internal consistencies (Cronbach’s alpha) of the self-concept domains were 0.79 for “scholastic competence” (n = 234), 0.82 for “social competence” (n = 225), 0.76 for “physical appearance” (n = 218), 0.77 for “behavioural conduct” (n = 231), and 0.71 for “global self-worth” (n = 216).
2.5. Physical Fitness
Physical fitness was calculated as the relative wattage, i.e., watts per kilogram of body weight. The physical fitness measure “Peak Mechanical Power (PMP [watt])” was determined via bicycle ergometry (Ergoline® ergometrics 900). For this purpose, the participants pedalled to exhaustion, with testing starting at 25 watts and increasing by 25 watts every two minutes (WHO (World Health Organization) scheme) [30]. Discontinuation criteria included, but were not limited to, clinical symptoms (such as dizziness or a severe headache), abnormalities during medical monitoring (such as non-physiological abnormalities in an ECG or blood pressure), and technical problems [31].
2.6. Statistical Analysis
A repeated cross-sectional design was used. This study derives from a post-hoc analysis of the data collected in a weight management programme. Therefore, the sample size was not established since the aims of the present study, and we performed a post-hoc power calculation. The post-hoc power analysis was performed with G*Power version 3.1.9.6 (Heinrich-Heine-Universität Düsseldorf, Germany). At least 177 participants were required for this study to perform an analysis of covariance (ANCOVA) comparing six groups with f2 = 0.35, a power of 0.95 at an alpha level of 0.05, five degrees of freedom and four covariates [32].
All analyses were performed using the IBM programme SPSS Statistics version 27.0 (IBM Corp., Armonk, NY, USA). Categorical variables were expressed as percentages and frequencies, while continuous variables were expressed in terms of means, standard deviations (SD), maximums (max), and minimums (min). Unpaired t-tests and chi-squared tests were used to detect possible differences between sexes.
Analysis of covariance (ANCOVA) was used to analyse differences between the six time periods between 2005 and 2020 in the five domains of self-concept as well as BMI-SDS as dependent variables.
In addition, moderation analyses were run to determine whether the interaction between BMI-SDS and time significantly predicted the subdomains of self-concept. For this purpose, multiple linear regression analyses were performed including the mean centred variables of BMI-SDS and time and their interaction effect while controlling for age, adolescent status, and sex.
Lastly, a backward stepwise linear regression was performed to examine factors that were consistently associated with the domains of self-concept across time spans. Sex (m/f), age, BMI-SDS, and adolescent status (<13/≥13 years) as well as migration background (yes/no), media consumption (h/day), and physical fitness (watts/kg) were included as predictors in the baseline models. Only significant variables were included in the final model, as insignificant variables were removed step by step. A p-value of <0.05 was considered significant.
3. Results
3.1. Secular Trends in Anthropometric Data
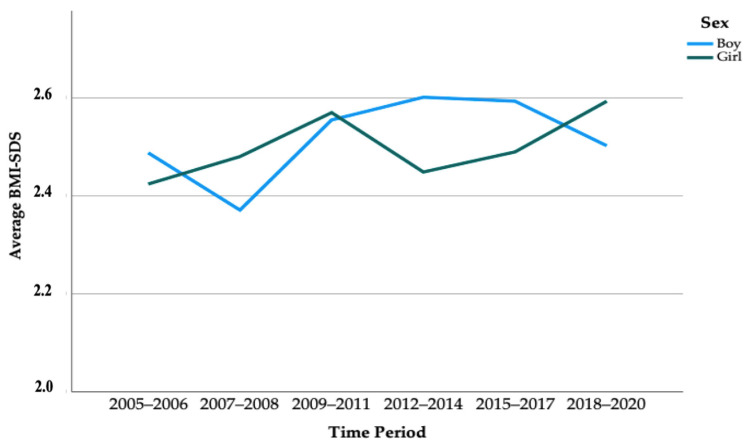
The analysis showed no significant change in height, weight, BMI, and BMI-SDS over time among children who were overweight and participating in a weight management programme (Table 2, Figure 2). The same analysis separated by sex is shown in the Supplemental Materials (Table S1).
Table 2.
Descriptive statistics separated by time period.
| Overall (n = 242) |
2005–2006 (n = 40) |
2007–2008 (n = 38) |
2009–2011 (n = 34) |
2012–2014 (n = 42) |
2015–2017 (n = 45) |
2018–2020 (n = 43) |
p-Value |
|---|---|---|---|---|---|---|---|
| (1) Sex n (%) | |||||||
| male | 15 (37.5%) | 19 (50.0%) | 14 (41.2%) | 22 (52.4%) | 20 (44.4%) | 23 (53.5%) | 0.642 ‡ |
| female | 25 (62.5%) | 19 (50.0%) | 20 (58.8%) | 20 (47.6%) | 25 (55.6%) | 20 (46.5%) | |
| (2) Age (in years) | 12.3 ± 2.1 | 12.9 ± 2.0 | 12.6 ± 1.6 | 12.4 ± 2.5 | 12.4 ± 2.2 | 12.4 ± 1.9 | 0.835 † |
| (3) Height (in m) | 1.58 ± 0.11 | 1.62 ± 0.13 | 1.57 ± 0.09 | 1.59 ± 0.12 | 1.56 ± 0.12 | 1.60 ± 0.11 | 0.233 † |
| (4) Weight (in kg) | 74.4 ± 19.3 | 78.2 ± 20.5 | 73.7 ± 15.0 | 77.8 ± 18.6 | 74.4 ± 22.0 | 79.7 ± 21.2 | 0.670 † |
| (5) BMI (in kg/m2) | 29.5 ± 4.9 | 29.4 ± 4.3 | 29.7 ± 4.1 | 30.4 ± 4.5 | 30.1 ± 6.1 | 30.5 ± 4.7 | 0.867 † |
| (6) BMI-SDS | 2.41 ± 0.51 | 2.37 ± 0.40 | 2.41 ± 0.46 | 2.52 ± 0.49 | 2.46 ± 0.46 | 2.51 ± 0.44 | 0.631 † |
| (7) Adolescent status | |||||||
| <13 years old | 24 (60.0%) | 20 (52.6%) | 17 (50.0%) | 21 (50.0%) | 26 (57.8%) | 27 (62.8%) | 0.791 ‡ |
| ≥13 years old | 16 (40.0%) | 18 (47.4%) | 17 (50.0%) | 21 (50.0%) | 19 (42.2%) | 16 (37.2%) | |
| Overall (n = 205) |
2005–2006 (n = 31) |
2007–2008 (n = 36) |
2009–2011 (n = 29) |
2012–2014 (n = 30) |
2015–2017 (n = 39) |
2018–2020 (n = 40) |
|
| (8) Migration background (yes) | 2 (6.4%) | 3 (8.3%) | 1 (3.4%) | 6 (20%) | 3 (7.7%) | 8 (20%) | 0.616 ‡ |
| (9) Media consumption (in h/day) | 1.90 ± 1.11 | 1.67 ± 0.96 | 1.35 ± 0.95 | 1.44 ± 0.89 | 5.25 ± 3.65 | 6.38 ± 4.11 | <0.001 † |
The data are presented as the mean ± SD; BMI = body mass index; BMI SDS = body mass index standard deviation score; p-values calculated with the † analysis of variance (ANOVA); ‡ chi square test.
Figure 2.
Secular trend of average BMI-SDS between 2005 and 2020 separated by time periods and sex. p = 0.631 according to an analysis of covariance (ANCOVA).
3.2. Secular Trends in Self-Concept
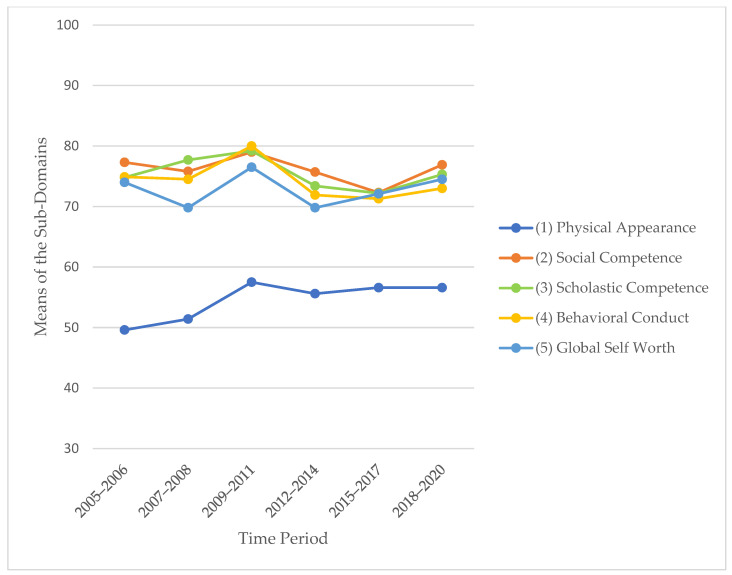
With regard to the secular trend in self-concept, we could not find any significant differences (Table 3, Figure 3).
Table 3.
Results analysing differences in the domains of self-concept over time.
| Periods of Analysis | ||||||||
|---|---|---|---|---|---|---|---|---|
| Overall (n = 242) |
2005–2006 (n = 40) |
2007–2008 (n = 38) |
2009–2011 (n = 34) |
2012–2014 (n = 42) |
2015–2017 (n = 45) |
2018–2020 (n = 43) |
p-Value | |
| (1) Physical appearance | 54.6 ± 15.7 | 49.6 ± 14.5 | 51.4 ± 15.9 | 57.5 ± 12.3 | 55.6 ± 15.7 | 56.6 ± 17.1 | 56.6 ± 16.9 | 0.063 † |
| (2) Social competence | 76.0 ± 18.5 | 77.3 ± 19.2 | 75.8 ± 21.7 | 79.0 ± 18.5 | 75.7 ± 15.4 | 72.3 ± 19.2 | 76.9 ± 17.4 | 0.713 † |
| (3) Scholastic competence | 75.2 ± 16.6 | 74.8 ± 19.5 | 77.7 ± 14.8 | 79.2 ± 14.5 | 73.4 ± 15.8 | 72.2 ± 15.9 | 75.3 ± 18.2 | 0.466 † |
| (4) Behavioural conduct | 74.0 ± 16.3 | 74.9 ± 17.1 | 74.5 ± 16.8 | 80.0 ± 15.5 | 71.9 ± 17.6 | 71.3 ± 13.8 | 73.0 ± 16.2 | 0.269 † |
| (5) Global self-worth | 72.7 ± 16.0 | 74.0 ± 16.8 | 69.8 ± 16.9 | 76.5 ± 12.8 | 69.8 ± 14.0 | 72.1 ± 18.1 | 74.5 ± 16.2 | 0.377 † |
The data are presented as the mean ± SD; p-values are calculated with an † analysis of covariance (ANCOVA) adjusting for sex, age, adolescent status and BMI-SDS.
Figure 3.
Means of the five sub-domains of self-concept (recoded data scaled 0–100) in the different time periods.
Analysing differences in the domains of self-concept over time separated by sex is shown in the Supplemental Materials (Table S2). Additional calculations in terms of self-concept domains considering migration background, media consumption, and physical fitness are shown in the Supplemental Materials as well (Table S3).
Examining the interaction effect of time and BMI-SDS on the subdomains of self-concept, we did not find significance (all results had p > 0.5), except in the physical appearance model. The results showed that time significantly moderated the effect between BMI-SDS and perceived physical appearance; adj. R2 = 0.16, F (6, 236) = 8.4, p < 0.001.
3.3. Consistent Predictors of Self-Concept across Time Spans
In four of six time clusters of the physical appearance domain, a lower BMI-SDS was associated with a higher “physical appearance” rating in the final models (ß = −0.420, p = 0.005 in 2007–2008; ß = −0.605, p = 0.007 in 2009–2011; ß = −0.651, p = 0.001 in 2012–2014, and ß = −0.391, p = 0.014 in 2015–2017; Table 4).
Table 4.
Linear regression analysis (backward) of the physical appearance domain.
| Domain | Periods of Analysis of Final Model | Unstandardized Coefficients | Standardized Coefficients | T | p-Value | 95.0% Confidence Interval for B | Adjusted R2 | |||
|---|---|---|---|---|---|---|---|---|---|---|
| B | std. error | ß | lower limit | upper limit | ||||||
| Physical appearance | 2005–2006 | media consumption |
−6.510 | 2.204 | −0.481 | −2.954 | 0.006 * | −11.02 | −2.00 | 0.205 |
| 2007–2008 | age | −3.728 | 1.186 | −0.466 | −3.143 | 0.004 * | −6.14 | −1.32 | 0.423 | |
| BMI-SDS | −15.173 | 4.992 | −0.420 | −3.040 | 0.005 * | −25.33 | −5.02 | |||
| media consumption |
6.150 | 2.408 | 0.357 | 2.553 | 0.015 * | 1.25 | 11.05 | |||
| 2009–2011 | BMI-SDS | −17.225 | 5.840 | −0.605 | −2.950 | 0.007 * | −29.23 | −5.22 | 0.226 | |
| physical fitness | −27.541 | 10.140 | −0.557 | −2.716 | 0.012 * | −48.39 | −6.70 | |||
| 2012–2014 | age | −6.791 | 1.972 | −0.988 | −3.443 | 0.002 * | −10.85 | −2.74 | 0.343 | |
| adolescent status |
22.076 | 9.294 | 0.648 | 2.375 | 0.025 * | 2.97 | 41.18 | |||
| BMI-SDS | −23.201 | 6.178 | −0.651 | −3.756 | 0.001 * | −35.90 | −10.50 | |||
| 2015–2017 | BMI-SDS | −13.787 | 5.334 | −0.391 | −2.585 | 0.014 * | −24.59 | −2.98 | 0.130 | |
| 2018–2020 | physical fitness | −7.611 | 3.937 | −0.299 | −1.933 | 0.061 | −15.58 | 0.36 | 0.066 | |
Final models of the backward linear regression analysing sub-domains of self-concept as dependent variable and the independent factors sex, age, BMI-SDS, adolescent status (<13 or ≥13 years old), migration background, media consumption in h/day, and physical fitness in watts/kg bodyweight in different time periods (n = 205). * significant results (p < 0.05).
Regarding the scholastic competence domain across time periods, the final models built with backward stepwise linear regression did not identify any consistent factors (Table 5). Only adolescent status (2009–2011 (ß = 0.801, p = 0.009) and 2012–2014 (ß = −0.456, p = 0.009)) and physical fitness (2005–2006 (ß = 0.474, p = 0.004) and 2007–2008 (ß = 0.512, p = 0.027)) had significant influences on this domain in more than one time span.
Table 5.
Linear regression analysis (backward) of the scholastic competence domain.
| Domain | Periods of Analysis of Final Model | Unstandardized Coefficients | Standardized Coefficients | T | p-Value | 95.0% Confidence Interval for B | Adjusted R2 | |||
|---|---|---|---|---|---|---|---|---|---|---|
| B | std. error | ß | lower limit | upper limit | ||||||
| Scholastic competence | 2005–2006 | sex | −10.928 | 5.147 | −0.315 | −2.123 | 0.043 * | −21.49 | −0.37 | 0.350 |
| adolescent status |
−10.386 | 5.283 | −0.296 | −1.966 | 0.060 | −21.23 | 0.45 | |||
| physical fitness | 23.025 | 7.274 | 0.474 | 3.165 | 0.004 * | 8.10 | 37.95 | |||
| 2007–2008 | BMI-SDS | 13.381 | 7.482 | 0.398 | 1.788 | 0.083 | −1.83 | 28.59 | 0.086 | |
| physical fitness | 19.616 | 8.512 | 0.512 | 2.305 | 0.027 * | 2.32 | 36.91 | |||
| 2009–2011 | age | −6.088 | 2.614 | −0.654 | −2.329 | 0.028 * | −11.47 | −0.70 | 0.294 | |
| adolescent status |
22.953 | 8.128 | 0.801 | 2.824 | 0.009 * | 6.21 | 39.69 | |||
| migration background |
−26.634 | 12.689 | −0.341 | −2.099 | 0.046 * | −52.77 | −0.50 | |||
| 2012–2014 | adolescent status |
−14.536 | 5.189 | −0.456 | −2.801 | 0.009 * | −25.18 | −3.89 | 0.236 | |
| migration background |
12.496 | 6.428 | 0.316 | 1.944 | 0.062 | −0.69 | 25.69 | |||
| 2015–2017 | BMI-SDS | −6.879 | 5.124 | −0.216 | −1.343 | 0.188 | −17.26 | 3.50 | 0.021 | |
| 2018–2020 | age | 1.317 | 1.479 | 0.143 | 0.891 | 0.379 | −1.68 | 4.31 | −0.005 | |
Final models of the backward linear regression analysing sub-domains self-concept as dependent variable and the independent factors sex, age, BMI-SDS, adolescent status (<13 or ≥13 years old), migration background, media consumption in h/day, and physical fitness in watts/kg bodyweight in different time periods (n = 205). * significant results (p < 0.05).
In the social competence domain, higher physical fitness was associated with better social competence in almost all final models except those of 2005–2006 and 2009–2011 (ß = 0.340, p = 0.042 in 2007–2008; ß = 0.347, p = 0.009 in 2012–2014; ß = 0.536, p = 0.001 in 2015–2017 and ß = −0.481, p = 0.010 in 2018–2020) (Table 6).
Table 6.
Linear regression analysis (backward) of the social competence domain.
| Domain | Periods of Analysis of Final Model | Unstandardized Coefficients | Standardized Coefficients | T | p-Value | 95.0% Confidence Interval for B |
Adjusted R2 | |||
|---|---|---|---|---|---|---|---|---|---|---|
| B | std. error | ß | lower limit | upper limit | ||||||
| Social competence |
2005–2006 | media consumption |
−4.315 | 2.863 | −0.269 | −1.507 | 0.143 | −10.17 | 1.54 | 0.041 |
| 2007–2008 | physical fitness | 19.640 | 9.314 | 0.340 | 2.109 | 0.042 * | 0.71 | 38.57 | 0.090 | |
| 2009–2011 | BMI-SDS | 13.887 | 7.460 | 0.337 | 1.862 | 0.074 | −1.42 | 29.19 | 0.081 | |
| 2012–2014 | age | −3.797 | 1.572 | −0.617 | −2.415 | 0.023 * | −7.04 | −0.56 | 0.329 | |
| adolescent status |
17.552 | 7.731 | 0.575 | 2.270 | 0.032 * | 1.63 | 33.47 | |||
| physical fitness | 12.211 | 5.378 | 0.347 | 2.271 | 0.032 * | 1.14 | 23.29 | |||
| media consumption |
8.313 | 2.684 | 0.480 | 3.097 | 0.005 * | 2.79 | 13.84 | |||
| 2015–2017 | adolescent status |
−11.492 | 6.633 | −0.284 | −1.733 | 0.092 | −24.96 | 1.97 | 0.271 | |
| physical fitness | 31.041 | 8.147 | 0.536 | 3.810 | 0.001 * | 14.50 | 47.58 | |||
| media consumption |
1.793 | 0.917 | 0.325 | 1.955 | 0.059 | −0.07 | 3.65 | |||
| 2018–2020 | BMI-SDS | −12.029 | 6.762 | −0.317 | −1.779 | 0.083 | −25.73 | 1.67 | 0.122 | |
| physical fitness | −12.031 | 4.458 | −0.481 | −2.698 | 0.010 * | −21.06 | −3.00 | |||
Final models of the backward linear regression analysing sub-domains-concept as dependent variable and the independent factors sex, age, BMI-SDS, adolescent status (<13 or ≥13 years old), migration background, media consumption in h/day, and physical fitness in watts/kg bodyweight in the different time periods (n = 205). * significant results (p < 0.05).
After accounting for all other variables, BMI-SDS remained a predictor in the final models of the global self-worth domain in the years of 2007–2008 (ß = −0.247, p = 0.140), 2012–2014 (ß = −0.727, p < 0.001) and 2015–2017 (ß = 0.433, p = 0.006) (Table 7).
Table 7.
Linear regression analysis (backward) of the global self-worth domain.
| Domain | Periods of Analysis of Final Model | Unstandardized Coefficients | Standardized Coefficients | T | p-Value | 95.0% Confidence Interval for B |
Adjusted R2 | |||
|---|---|---|---|---|---|---|---|---|---|---|
| B | std. error | ß | lower limit | upper limit | ||||||
| Global self-worth | 2005–2006 | media consumption |
−6.380 | 2.498 | −0.428 | −2.554 | 0.016 * | −11.49 | −1.27 | 0.155 |
| 2007–2008 | BMI-SDS | −9.828 | 6.516 | −0.247 | −1.508 | 0.140 | −23.06 | 3.40 | 0.034 | |
| 2009–2011 | adolescent status | 7.532 | 4.779 | 0.290 | 1.576 | 0.127 | −2.27 | 17.34 | 0.050 | |
| 2012–2014 | sex | −8.326 | 4.857 | −0.272 | −1.714 | 0.100 | −18.37 | 1.72 | 0.493 | |
| age | −9.238 | 1.826 | −1.482 | −5.060 | <0.001 * | −13.02 | −5.46 | |||
| adolescent status |
33.217 | 7.893 | 1.075 | 4.209 | <0.001 * | 16.89 | 49.54 | |||
| BMI-SDS | −23.491 | 5.799 | −0.727 | −4.051 | <0.001 * | −35.50 | −11.50 | |||
| migration background | −21.038 | 6.180 | −0.549 | −3.404 | 0.002 * | −33.82 | −8.25 | |||
| media consumption |
8.509 | 2.747 | 0.484 | 3.098 | 0.005 * | 2.83 | 14.19 | |||
| 2015–2017 | BMI-SDS | −17.232 | 5.891 | −0.433 | −2.925 | 0.006 * | −29.17 | −5.30 | 0.166 | |
| 2018–2020 | migration background | 5.534 | 6.452 | 0.138 | 0.858 | 0.396 | −7.53 | 18.60 | −0.007 | |
Final models of the backward linear regression analysing sub-domains of self-concept as dependent variable and the independent factors sex, age, BMI-SDS, adolescent status (<13 or ≥13 years old), migration background, media consumption in h/day, and physical fitness in watts/kg bodyweight in different time periods (n = 205). * significant results (p < 0.05).
In the behavioural conduct domain, migration background remained in the final models in 2012–2014 (ß = −0.396, p = 0.029), 2015–2017 (ß = −0.402, p = 0.011) and 2018–2020 (ß = −0.252, p = 0.117) (Table 8).
Table 8.
Linear regression analysis (backward) of the behavioural conduct domain.
| Domain | Periods of Analysis of Final Model | Unstandardized Coefficients | Standardized Coefficients | T | p-Value | 95.0% Confidence Interval for B | Adjusted R2 | |||
|---|---|---|---|---|---|---|---|---|---|---|
| B | std. error | ß | lower limit | upper limit | ||||||
| Behavioural conduct | 2005–2006 | adolescent status |
−10.512 | 4.556 | −0.328 | −2.307 | 0.029 * | −19.85 | −1.18 | 0.413 |
| physical fitness | 23.668 | 6.312 | 0.533 | 3.750 | 0.001 * | 10.74 | 36.60 | |||
| 2007–2008 | age | −1.160 | 1.437 | −0.135 | −0.808 | 0.425 | −4.08 | 1.76 | −0.010 | |
| 2009–2011 | adolescent status |
8.297 | 5.166 | 0.295 | 1.606 | 0.120 | −2.30 | 18.90 | 0.053 | |
| 2012–2014 | sex | −16.685 | 5.841 | −0.478 | −2.856 | 0.009 * | −28.77 | −4.60 | 0.435 | |
| age | −9.977 | 2.196 | −1.405 | −4.544 | <0.001 * | −14.52 | −5.44 | |||
| adolescent status |
31.483 | 9.493 | 0.894 | 3.317 | 0.003 * | 11.85 | 51.12 | |||
| BMI-SDS | −13.831 | 6.975 | −0.376 | −1.983 | 0.059 | −28.26 | 0.60 | |||
| migration background |
−17.257 | 7.433 | −0.396 | −2.322 | 0.029 * | −32.63 | −1.88 | |||
| media consumption |
10.595 | 3.304 | 0.529 | 3.207 | 0.004 * | 3.76 | 17.43 | |||
| 2015–2017 | migration background |
−20.648 | 7.727 | −0.402 | −2.672 | 0.011 * | −36.31 | −4.99 | 0.139 | |
| 2018–2020 | migration background |
−10.326 | 6.436 | −0.252 | −1.604 | 0.117 | −23.35 | 2.70 | 0.039 | |
Final models of the backward linear regression analysing sub-domains of self-concept as the dependent variable and the independent factors sex, age, BMI-SDS, adolescent status (<13 or ≥13 years old), migration background, media consumption in h/day, and physical fitness in watts/kg bodyweight in different time periods (n = 205). * significant results (p < 0.05).
4. Discussion
The prevalence of overweight and obesity, or high weights, among children and adolescents is increasing worldwide [1,33]. This has significant consequences for physical and mental health [34,35,36], which may be relevant within weight management programmes. Therefore, the current study collated and analysed data on BMI-SDS as well as on five subdomains of the self-concept in children and adolescents who participated in a German weight-management programme between 2005 and 2020. Contrary to global trends, this sample showed that BMI-SDS remained stable during this period. Although there were shifts in favour of younger and male participants, these trends were not significant. In addition, the results did not suggest either an improvement or a decline in the self-concept of overweight youths over time. The domain “physical well-being” was consistently rated with the lowest values. Furthermore, BMI-SDS was found to negatively correlate with almost all domains of self-concept, especially physical self-concept, at all different points in time. However, this negative correlation between BMI-SDS and physical appearance became weaker over time. The possible influence of additional factors such as migration background, physical fitness, media consumption, adolescent status, age, and gender on the different domains of the self-concept varied over the years. In the domains “physical appearance” and “global self-worth”, a higher BMI-SDS was most often associated with a lower score. In the domains “scholastic competence” and “behavioural conduct” no clear factor was found, whereas in the domain of “social competence,” higher physical fitness was associated with a better assessment in almost all final models.
In earlier studies, Ottova et al. [36] described the effects of being overweight on the health-related quality of life of children and adolescents in a European cohort with 17,159 participants between the ages of 8 and 18. Consistent with the current findings, they found that the most impaired areas of health-related quality of life were physical well-being and self-perception. Older children and adolescents tended to have a negative self-image and a poorer assessment of their own bodies [11,12,37]. In general, girls appear to be more dissatisfied with their bodies and thus more susceptible to possible psychological disorders, such as eating disorders [11,37,38]. However, Molina-García et al. [39] found higher BMI to be associated with body dissatisfaction in both sexes.
In contrast, physical activity (or fitness as a proxy) has already been associated with better physical and mental health. For example, the self-concept of normal-weight children and adolescents was positively associated with physical activity in Babic et al. [40] and with cardiovascular fitness in Vedul-Kjelsås et al. [41]. Prior research has also found a significant association between physical activity and physical self-concept in normal-weight children and adolescents, with age and gender being key moderators of this association [40]. This association has also been observed among children and adolescents with overweight and obesity [42,43]. In their study, Perez-Sousa et al. [42] demonstrated an association between the Z-scores of physical fitness and several HRQoL dimensions (i.e., the physical, emotional, social, and psychosocial dimensions) in overweight children and adolescents. It was only for the dimension of school competence that no correlation was found. In our data, however, there was a significant correlation between physical fitness and school and social competence. It is possible that better fitness ensures a higher ability to connect, and prevents social withdrawal in the school environment. In a systematic review, Silva et al. (2018) showed that increasing fitness was one motivating factor for weight loss in adolescents with overweight or obesity in at least 2 of 6 integrated studies. However, the main motive out of 17 mentioned factors was the desire for health improvements followed by an increase of self-esteem and avoidance of bullying [44]. In an earlier analysis, we already proved the connection between physical fitness and quality of life or self-concept [43]. Improving physical fitness may be more promising for positive mental health outcomes in weight management programmes than weight loss or participation in physical activities alone.
5. Strengths and Limitations
One of the strengths of this study is the continuous and standardized recording of parameters over almost two decades. For example, height, weight, BMI-SDS, physical fitness, and migration background of each participant were measured by qualified personnel. The FSK-K questionnaire is also considered a standardized instrument for assessing self-concept in children and has been used several times. However, these measurements might be considered as only snapshots in time, rather than comprehensive. In addition, we cannot exclude the possibility of distorted data resulting from self-reporting. Furthermore, our collective consisted of small monocentric groups in the different year clusters. Finally, potential confounding factors such as family structure or diet could not be integrated into the analysis. Thus, the generalisability of the current results is limited.
6. Conclusions
Considering the limitations, the available data do not suggest any trends within the individual psychosocial self-concept domains and the BMI-SDS for children and adolescents with obesity over the past decades. However, in most time clusters, the domains “physical appearance” and “social competence” correlated negatively with BMI-SDS and positively with physical fitness. On the one hand, these results therefore underline the well-known importance of psychosocial support as a therapy pillar in weight management programmes. On the other hand, more attention should also be paid to the promotion of physical fitness, as it could contribute not only to the reduction of BMI-SDS but also to an improvement of the participants’ self-concepts. To corroborate the current findings, future multicentred research should undertake analysis on larger groups of participants.
Acknowledgments
We gratefully acknowledge all CHILT III participants and their parents. We would also like to thank Susanne Vandeven, Hidayet Oruc and Jonas Juretzko for their support during the trial and Selina Müller for her help in researching and calculating the HRoQL scores.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/children10010127/s1, Table S1: Descriptive statistics of all time clusters separated by sex; Table S2: Results analysing differences in the domains of self-concept over time separated by sex; Table S3: Results of the ANCOVA analysing the domains of the self-concept adjusted for sex, age, BMI SDS, adolescent status, migration background, media consumption and physical fitness.
Author Contributions
L.G., N.E. and C.J. conceptualized and designed the study. M.K., D.F., F.H., N.F., L.S. and C.J. drafted and carried out the analyses. L.G. and C.J. had overall responsibility for the manuscript. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee Ethics of the German Sport University Cologne for the ethic request with the number 107/2014 which was updated on 17 May 2021 (“Children’s Health InterventionaL Trial III—ein ambulantes, multimodales, familienbasiertes Schulungsprogamm zur Therapie von Übergewicht und Adipositas im Kindes- und Jugendalter”).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent was obtained from the participants’ parents to publish this paper.
Data Availability Statement
The data used and analysed during the current study involve sensitive patient information and indirect identifiers. As a result, the datasets are available from the corresponding author only on reasonable request.
Conflicts of Interest
All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf (accessed on 5 May 2022). The authors have declared that no competing interests exist.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Abarca-Gómez L., Abdeen Z.A., Hamid Z.A., Abu-Rmeileh N.M., Acosta-Cazares B., Acuin C., Adams R.J., Aekplakorn W., Afsana K., Aguilar-Salinas C.A., et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390:2627–2642. doi: 10.1016/S0140-6736(17)32129-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schienkiewitz A., Brettschneider A.-K., Damerow S., Schaffrath Rosario A. Übergewicht und Adipositas im Kindes- und Jugendalter in Deutschland—Querschnittergebnisse aus KiGGS Welle 2 und Trends. J. Health Monit. 2018;3 doi: 10.17886/RKI-GBE-2018-005.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vogel M., Geserick M., Gausche R., Beger C., Poulain T., Meigen C., Körner A., Keller E., Kiess W., Pfäffle R. Age- and weight group-specific weight gain patterns in children and adolescents during the 15 years before and during the COVID-19 pandemic. Int. J. Obes. 2022;46:144–152. doi: 10.1038/s41366-021-00968-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weihrauch-Blüher S., Huizinga O., Joisten C., Pflanz J., Torbahn G., Wiegand S., Holzapfel C., Hauner H. Changes in lifestyle and body weight in children and adolescents during the COVID-19 pandemic: A representative survey of parents in Germany. Obes. Facts. 2022 doi: 10.1159/000529116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Flechtner-Mors M., Thamm M., Rosario A.S., Goldapp C., Hoffmeister U., Mann R., Bullinger M., van Egmond-Fröhlich A., Ravens-Sieberer U., Reinehr T., et al. Hypertension, dyslipoproteinemia and BMI-category characterise the cardiovascular risk in overweight or obese children and adolescents: Data of the BZgA-observational study (EvAKu-J-project) and the KiGGS-study. Klin. Padiatr. 2011;223:445–449. doi: 10.1055/s-0031-1280766. [DOI] [PubMed] [Google Scholar]
- 6.Flechtner-Mors M., Neuhauser H., Reinehr T., Roost H.P., Wiegand S., Siegfried W., Zwiauer K., Molz E., Holl R.W. Blood pressure in 57,915 pediatric patients who are overweight or obese based on five reference systems. Am. J. Cardiol. 2015;115:1587–1594. doi: 10.1016/j.amjcard.2015.02.063. [DOI] [PubMed] [Google Scholar]
- 7.Hoffmeister U., Bullinger M., Egmond-Fröhlich A., Goldapp C., Mann R., Ravens-Sieberer U., Reinehr T., Westenhöfer J., Holl R.W. Treatment of obesity in pediatric patients in Germany: Anthropometry, comorbidity and socioeconomic gradients based on the BZgA Observational Study. Klin. Padiatr. 2010;222:274–278. doi: 10.1055/s-0030-1248318. [DOI] [PubMed] [Google Scholar]
- 8.Kelsey M.M., Zaepfel A., Bjornstad P., Nadeau K.J. Age-related consequences of childhood obesity. Gerontology. 2014;60:222–228. doi: 10.1159/000356023. [DOI] [PubMed] [Google Scholar]
- 9.Britz B., Siegfried W., Ziegler A., Lamertz C., Herpertz-Dahlmann B.M., Remschmidt H., Wittchen H.U., Hebebrand J. Rates of psychiatric disorders in a clinical study group of adolescents with extreme obesity and in obese adolescents ascertained via a population based study. Int. J. Obes. 2000;24:1707–1714. doi: 10.1038/sj.ijo.0801449. [DOI] [PubMed] [Google Scholar]
- 10.Griffiths L.J., Parsons T., Hill A. Self-esteem and quality of life in obese children and adolescents: A systematic review. Int. J. Pediatr. Obes. 2010;5:282–304. doi: 10.3109/17477160903473697. [DOI] [PubMed] [Google Scholar]
- 11.Helfert S., Warschburger P. The face of appearance-related social pressure: Gender, age and body mass variations in peer and parental pressure during adolescence. Child Adolesc. Psychiatry Ment. Health. 2013;7:16. doi: 10.1186/1753-2000-7-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harrist A., Swindle T., Hubbs-Tait L., Topham G., Shriver L., Page M. The Social and Emotional Lives of Overweight, Obese, and Severely Obese Children. Child Dev. 2016;87:1564–1580. doi: 10.1111/cdev.12548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wabitsch M., Schnurbein J.v., Vollbach H., Lennerz B., Weyhreter H., Wiegand S., Kiess W., Hebebrand J., Brandt S. Innovative medizinische Betreuungskonzepte für Jugendliche mit extremer Adipositas. Bundesgesundheitsblatt-Gesundh. Gesundh. 2020;63:831–838. doi: 10.1007/s00103-020-03167-y. [DOI] [PubMed] [Google Scholar]
- 14.Janicke D.M., Marciel K.K., Ingerski L.M., Novoa W., Lowry K.W., Sallinen B.J., Silverstein J.H. Impact of psychosocial factors on quality of life in overweight youth. Obesity. 2007;15:1799–1807. doi: 10.1038/oby.2007.214. [DOI] [PubMed] [Google Scholar]
- 15.Puhl R.M., Latner J.D. Stigma, obesity, and the health of the nation’s children. Psychol. Bull. 2007;133:557. doi: 10.1037/0033-2909.133.4.557. [DOI] [PubMed] [Google Scholar]
- 16.Topçu S., Şimşek Orhon F., Ulukol B., Başkan S. Anxiety, depression and self-esteem levels in obese children: A case-control study. J. Pediatr. Endocrinol. Metab. 2016;29:357–361. doi: 10.1515/jpem-2015-0254. [DOI] [PubMed] [Google Scholar]
- 17.Buttitta M., Rousseau A., Guerrien A. A New Understanding of Quality of Life in Children and Adolescents with Obesity: Contribution of the Self-determination Theory. Curr. Obes. Rep. 2017;6:432–437. doi: 10.1007/s13679-017-0281-8. [DOI] [PubMed] [Google Scholar]
- 18.Morrison K.M., Shin S., Tarnopolsky M., Taylor V.H. Association of depression & health related quality of life with body composition in children and youth with obesity. J. Affect. Disord. 2015;172:18–23. doi: 10.1016/j.jad.2014.09.014. [DOI] [PubMed] [Google Scholar]
- 19.Sutaria S., Devakumar D., Yasuda S.S., Das S., Saxena S. Is obesity associated with depression in children? Systematic review and meta-analysis. Arch. Dis. Child. 2019;104:64–74. doi: 10.1136/archdischild-2017-314608. [DOI] [PubMed] [Google Scholar]
- 20.Murray M., Dordevic A.L., Bonham M.P. Systematic Review and Meta-Analysis: The Impact of Multicomponent Weight Management Interventions on Self-Esteem in Overweight and Obese Adolescents. J. Pediatr. Psychol. 2017;42:379–394. doi: 10.1093/jpepsy/jsw101. [DOI] [PubMed] [Google Scholar]
- 21.Lier L.M., Breuer C., Ferrari N., Friesen D., Maisonave F., Schmidt N., Graf C. Individual Physical Activity Behaviour and Group Composition as Determinants of the Effectiveness of a Childhood Obesity Intervention Program. Obes. Facts. 2021;14:100–107. doi: 10.1159/000512293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arbeitsgemeinschaft Adipositas im Kindes und Jugendalter (AGA), D.A.G.D Therapie und Prävention der Adipositas im Kindes- und Jugendalter, in Evidenzbasierte (S3-) Leitlinie der Arbeitsgemeinschaft Adipositas im Kindes- und Jugendalter (AGA) der Deutschen Adipositas-Gesellschaft (DAG) und der Deutschen Gesellschaft für Kinder-und Jugendmedizin (DGKJ) 2019. [(accessed on 18 March 2020)]. D.A.G.D. Arbeitsgemeinschaft Adipositas im Kindes und Jugendalter (AGA) Available online: https://register.awmf.org/assets/guidelines/050-002l_S3_Therapie-Praevention-Adipositas-Kinder-Jugendliche_2019-11.pdf.
- 23.Kromeyer-Hauschild K., Wabitsch M., Kunze D., Geller F., Geiß H.C., Hesse V., von Hippel A., Jaeger U., Johnsen D., Korte W., et al. Perzentile für den Body-mass-Index für das Kindes- und Jugendalter unter Heranziehung verschiedener deutscher Stichproben. Mon. Kinderheilkd. 2001;149:807–818. doi: 10.1007/s001120170107. [DOI] [Google Scholar]
- 24.Kliegman R.N.W.E. Nelson Textbook of Pediatrics. 19th ed. Elsevier/Saunders; Philadelphia, PA, USA: 2011. [Google Scholar]
- 25.Graf C. Rolle der körperlichen Aktivität und Inaktivität für die Entstehung und Therapie der juvenilen Adipositas. Bundesgesundheitsblatt-Gesundh. Gesundh. 2010;53:699–706. doi: 10.1007/s00103-010-1088-x. [DOI] [PubMed] [Google Scholar]
- 26.Graf C. In: Übergewicht im Kindes- und Jugendalter: Ein ganzheitliches Betreuungskonzept. Graf C., Dordel S., Koch B., editors. Verl. Modernes Lernen; Dortmund, Germany: 2009. [Google Scholar]
- 27.Bau A.M., Sannemann J., Ernert A., Babitsch B. Association between health-related quality of life and selected indicators for 10- to 15-year-old girls in Berlin. Gesundheitswesen. 2011;73:273–279. doi: 10.1055/s-0030-1247583. [DOI] [PubMed] [Google Scholar]
- 28.Reinehr T., Kersting M., Wollenhaupt A., Alexy U., Kling B., Strobele K., Andler W. Evaluation of the training program “OBELDICKS” for obese children and adolescents. Klin. Padiatr. 2005;217:1–8. doi: 10.1055/s-2004-816246. [DOI] [PubMed] [Google Scholar]
- 29.Warschburger P., Kröller K. Adipositas im Kindes- und Jugendalter. Z. Für. Gesundh. 2005;13:69–78. doi: 10.1026/0943-8149.13.2.69. [DOI] [Google Scholar]
- 30.Trappe H.-J., Löllgen H. Leitlinien zur Ergometrie. Z. Kardiol. 2000;89:821–837. doi: 10.1007/s003920070190. [DOI] [PubMed] [Google Scholar]
- 31.Menrath I., Graf C., Granacher U., Kriemler S. Pädiatrische Sportmedizin: Kompendium für Kinder- und Jugendärzte, Hausärzte und Sportärzte. Springer; Berlin/Heidelberg, Germany: 2021. [Google Scholar]
- 32.Faul F., Erdfelder E., Lang A.-G., Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods. 2007;39:175–191. doi: 10.3758/BF03193146. [DOI] [PubMed] [Google Scholar]
- 33.Gausche R., Beger C., Spielau U., Pfaeffle R., Körner A., Siekmeyer W. Epidemiologische Aspekte zum säkularen Trend bei Übergewicht und Adipositas bei Kindern und Jugendlichen. Adipositas-Ursachen Folgeerkrankungen Ther. 2018;12:4–9. [Google Scholar]
- 34.Loth K., Wall M., Larson N., Neumark-Sztainer D. Disordered eating and psychological well-being in overweight and nonoverweight adolescents: Secular trends from 1999 to 2010. Int. J. Eat. Disord. 2015;48:323–327. doi: 10.1002/eat.22382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Roth B., Munsch S., Meyer A., Metzke C., Isler E., Steinhausen H.-C., Schneider S. Die psychische Befindlichkeit übergewichtiger Kinder. Z. Kinder Jugendpsychiatrie Psychother. 2008;36:163–176. doi: 10.1024/1422-4917.36.3.163. [DOI] [PubMed] [Google Scholar]
- 36.Ottova V., Erhart M., Rajmil L., Dettenborn-Betz L., Ravens-Sieberer U. Overweight and its impact on the health-related quality of life in children and adolescents: Results from the European KIDSCREEN survey. Qual. Life Res. 2012;21:59–69. doi: 10.1007/s11136-011-9922-7. [DOI] [PubMed] [Google Scholar]
- 37.Mäkinen M., Puukko-Viertomies L.-R., Lindberg N., Siimes M.A., Aalberg V. Body dissatisfaction and body mass in girls and boys transitioning from early to mid-adolescence: Additional role of self-esteem and eating habits. BMC Psychiatry. 2012;12:35. doi: 10.1186/1471-244X-12-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sánchez-Miguel P.A., León-Guereño P., Tapia-Serrano M.A., Hortigüela-Alcalá D., López-Gajardo M.A., Vaquero-Solís M. The Mediating Role of the Self-Concept between the Relationship of the Body Satisfaction and the Intention to Be Physically Active in Primary School Students. Front. Public Health. 2020;8:113. doi: 10.3389/fpubh.2020.00113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Molina-García J., Castillo I., Queralt A., Alvarez O. Precursors of body dissatisfaction and its implication for psychological well-being in young adults. Univ. Psychol. 2019;18:1–11. doi: 10.11144/Javeriana.upsy18-2.pbdi. [DOI] [Google Scholar]
- 40.Babic M.J., Morgan P.J., Plotnikoff R.C., Lonsdale C., White R.L., Lubans D.R. Physical activity and physical self-concept in youth: Systematic review and meta-analysis. Sport. Med. 2014;44:1589–1601. doi: 10.1007/s40279-014-0229-z. [DOI] [PubMed] [Google Scholar]
- 41.Vedul-Kjelsås V., Sigmundsson H., Stensdotter A.K., Haga M. The relationship between motor competence, physical fitness and self-perception in children. Child Care Health Dev. 2012;38:394–402. doi: 10.1111/j.1365-2214.2011.01275.x. [DOI] [PubMed] [Google Scholar]
- 42.Perez-Sousa M.A., Olivares P.R., Escobar-Alvarez J.A., Parraça J.A., Gusi N. Fitness as mediator between weight status and dimensions of health-related quality of life. Health Qual. Life Outcomes. 2018;16:155. doi: 10.1186/s12955-018-0981-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Eisenburger N., Friesen D., Haas F., Klaudius M., Schmidt L., Vandeven S., Joisten C. Predicting Psychosocial Health of Children and Adolescents with Obesity in Germany: The Underappreciated Role of Physical Fitness. Int. J. Environ. Res. Public Health. 2021;18:11188. doi: 10.3390/ijerph182111188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Silva D.F.O., Sena-Evangelista K.C.M., Lyra C.O., Pedrosa L.F.C., Arrais R.F., Lima S. Motivations for weight loss in adolescents with overweight and obesity: A systematic review. BMC Pediatr. 2018;18:364. doi: 10.1186/s12887-018-1333-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data used and analysed during the current study involve sensitive patient information and indirect identifiers. As a result, the datasets are available from the corresponding author only on reasonable request.