Abstract
Simple Summary
To assess the association between clinical history and AML outcomes in the context of allogeneic hematopoietic cell transplantation (HCT), we retrospectively analyzed 739 patients with de novo AML, 125 with antecedent hematologic disorder (AHD)/AML, and 115 with therapy-related AML who received first allografts while in first or second remission. Relative to patients with de novo AML, relapse rates were similar for patients with AHD and therapy-related AML after multivariable adjustment, as were relapse-free survival and overall survival. Non-relapse mortality was, however, higher for AHD AML. These data suggest that the clinical history by itself contains limited prognostic value for adults with AML undergoing allografting, supporting the most recent approach to use this information as a diagnostic qualifier rather than a disease entity.
Abstract
(1) Background: Secondary acute myeloid leukemia (AML), i.e., AML arising from prior therapy (therapy-related) and/or an antecedent hematologic disorder (AHD) is generally associated with worse outcomes compared to de novo AML. However, recognizing the prognostic importance of genetic characteristics rather than clinical history, secondary AML is now considered a diagnostic qualifier rather than a separate disease entity. (2) Methods: To assess the association between clinical history and AML outcomes in the context of allogeneic hematopoietic cell transplantation (HCT), we retrospectively analyzed 759 patients with de novo AML, 115 with AHD AML, and 105 with therapy-related AML who received first allografts while in first or second remission. (3) Results: At the time of HCT, these three cohorts differed significantly regarding many patient and disease-specific characteristics, including age (p < 0.001), gender (p < 0.001), disease risk (p = 0.005), HCT-CI score (p < 0.001), blood count recovery (p = 0.003), first vs. second remission (p < 0.001), remission duration (p < 0.001), measurable residual disease (MRD; p < 0.001), and conditioning intensity (p < 0.001). Relative to patients with de novo AML, relapse rates were similar for patients with AHD (hazard ratio [HR] = 1.07, p = 0.7) and therapy-related AML (HR = 0.86, p = 0.4) after multivariable adjustment, as were relapse-free survival (HR = 1.20, p = 0.2, and HR = 0.89, p = 0.5) and overall survival (HR = 1.19, p = 0.2, and HR = 0.93, p = 0.6). Non-relapse mortality was higher for AHD AML (HR = 1.59, p = 0.047). (4) Conclusions: These data suggest that the clinical history by itself contains limited prognostic value for adults with AML undergoing allografting, supporting the most recent approach to use this information as a diagnostic qualifier rather than a disease entity.
Keywords: acute myeloid leukemia (AML), allogeneic hematopoietic cell transplantation (HCT), therapy-related, antecedent hematologic disease (AHD), prognostication
1. Introduction
Secondary acute myeloid leukemia (AML), i.e., AML arising after prior exposure to cytotoxic therapy (therapy-related AML) and/or antecedent hematological disorder (AHD), has generally been associated with a worse prognosis compared to de novo AML [1,2,3,4,5,6]. However, it is increasingly appreciated that genetics and patient characteristics rather than clinical history largely account for outcome differences [1,2,3,5,6,7,8]. As a result, the International Consensus Classification, the World Health Organization (WHO), and European LeukemiaNet (ELN) now consider secondary AML as a disease attribute and diagnostic qualifier rather than a separate disease entity [9,10,11]. For most adults with de novo or secondary AML, allogeneic hematopoietic cell transplantation (HCT) is an important part of curative-intent treatment [1,2,4,12,13,14,15]. In some [16,17,18] but not all studies [19], clinical history had been associated with post-HCT outcome, with increased relapse risk due to high-risk disease features (e.g., progressive disease, adverse cytogenetic/molecular abnormalities) and, possibly, pre-HCT measurable residual disease (MRD) in individuals with secondary AML [16,20,21]. In other studies, secondary AML was associated with higher non-relapse mortality (NRM) [17].
Given these mixed data, and the notion that post-HCT outcomes within the subset of patients with secondary AML might differ depending on the details of clinical history (e.g., whether therapy-related or after AHD, or the type of underlying AHD) [17,22], we examined a large cohort of adults with therapy-related AML and after AHD who underwent allogeneic HCT while in first or second remission at our institution between May 2006 and May 2021. In this analysis, we also assessed how the most recent changes in the classification for secondary AML might impact study findings.
2. Materials and Methods
2.1. Study Cohort
We included all adults with AML (2016 WHO criteria) [23] who proceeded to first allogeneic HCT while in first or second remission (i.e., had <5% marrow blasts) with or without peripheral blood count recovery between 5/2006 and 5/2021 at a single institution (Fred Hutchinson Cancer Center/University of Washington/Seattle Cancer Care Alliance, Seattle, WA, USA). High-dose fractionated total body irradiation (TBI; ≥12 Gy) with or without cyclophosphamide (CY) or fludarabine (FLU), high-dose TBI/thiotepa/FLU, busulfan (4 days) with CY or FLU, treosulfan/FLU with or without low-dose TBI, or any regimen containing a radiolabeled antibody were considered myeloablative conditioning (MAC) regimens [24]. Reduced-intensity conditioning (RIC) and non-myeloablative conditioning (i.e., 2–3 Gy TBI with or without fludarabine) were grouped together as non-MAC regimens. Data on post-HCT outcomes were obtained via the Long-Term Follow-Up Program from our outpatient clinic and local clinics that provided care for post-HCT patients; additionally, information was collected on patients in research studies. All treatments were on Institutional Review Board-approved research protocols (all registered within ClinicalTrials.gov) or standard protocols; patients gave informed consent in accordance with the Declaration of Helsinki. The cut-off date for follow-up was 10 February 2022.
2.2. Classification of Disease Risk and Treatment Response
Secondary AML was defined as disease following an AHD (i.e., myelodysplastic syndrome [MDS], myeloproliferative neoplasm [NPM], and MDS/MPN such as chronic myelomonocytic leukemia [CMML]) or treatment with systemic chemotherapy and/or radiotherapy for a different disorder. All previous cytotoxic regimens were considered for the main analysis, including methotrexate, mercaptopurine, and cyclophosphamide for auto-immune disease. Immunosuppressive treatment using nonchemotherapeutic agents was not considered cytotoxic. Patients developing MDS, MPN, or MDS/MPN between the chemotherapy or radiation treatment for their primary disease and the diagnosis of AML were classified as therapy-related AML unless stated otherwise. In sensitivity analyses, we explored the impact of new classification criteria for therapy-related AML (not including previous exposure to methotrexate, and, by analogy, mercaptopurine, and cyclophosphamide) and AHD (requirement for AHD diagnosis ≥3 months before AML diagnosis) [10,11]. The 2010 refined MRC/NCRI criteria were used to assess the cytogenetic risk at diagnosis [25]. The karyotype analysis was routinely based on 20 metaphases (if available); FISH studies were performed according to standard procedures in a subset of patients.
The HCT-specific comorbidity index (HCT-CI) and the Treatment-Related Mortality (TRM) score were calculated as previously described [26,27]. We categorized treatment responses according to the ELN (2017) except that we defined post-HCT relapse as emergence >5% blasts in blood or bone marrow, new cytogenetic abnormality, or any level of disease that led to a therapeutic intervention [28]. Multiparameter (10-color) flow cytometry was routinely performed on bone marrow before initiating conditioning therapy. The methodology of the MFC MRD assay and its performance has not changed throughout the study period, [29,30,31,32,33,34,35], with any measurable level of residual disease considered MRD-positive [29,30,31,32,33,35,36,37,38,39].
2.3. Statistical Analysis
Categorical variables were reported as numbers (with proportions) and compared using the Chi² test or Fisher’s exact test, as appropriate. Continuous variables were reported as medians (with interquartile range [IQR]) and compared using the Mann and Whitney test. We estimated unadjusted probabilities of relapse-free survival (RFS; events: relapse or death) and overall survival (OS; event: death) with the Kaplan–Meier method and compared them with the Log-Rank test. Associations with RFS and OS were assessed using Cox regression models. Probabilities of relapse (with NRM as a competing event) and NRM (death without relapse with relapse as a competing event) were reported using cumulative incidence estimates. Associations with relapse and NRM were assessed using cause-specific regression models [24]. All tests were two-sided with a significant level of p < 0.05. Statistical analyses were performed with R (R Foundation for Statistical Computing, Vienna, Austria; http://www.r-project.org).
3. Results
3.1. Characteristics of Study Cohort
Of 1011 adults undergoing a first allogeneic HCT for AML in first or second remission, 21 did not agree to data use for research while data from institutional pre-HCT MRD testing were not available for 11 patients. Among the remaining 979 patients, 115 patients had therapy-related AML, mainly following treatment for lymphoid hematologic malignancy (n = 39, 34%), breast cancer (n = 35, 30%), or an auto-immune condition (n = 13, 11%), and 125 patients had an AHD (MDS, n = 97, 78%; MPN, n = 18, 14%; CMML, n = 10, 8%; Supplementary Table S1). Among patients with AHD, 20 (16%) occurred post cytotoxic therapy for other conditions, and 50 (40%) were previously treated for AHD.
The characteristics of the 979 patients included in the analysis are summarized in Table 1. Patients with AHD were older than patients with either de novo or therapy-related AML (63 vs. 53 vs. 57 years, p < 0.001). Due to the high number of therapy-related AML after treatment for breast cancers, there were more females in the therapy-related group (60% vs. 46% vs. 35% for patients with de novo and AHD, respectively, p < 0.001) and, as prior cancer is used to calculate the HCT-CI, patients in this group were more likely considered as high-risk according to this score (68% vs. 25% vs. 27%, respectively, p < 0.001). On the other hand, patients with AHD were less likely to be classified as favorable risk (0 vs. 8% vs. 11% for patients with de novo and therapy-related AML, respectively, p = 0.005) and they were more likely to have incomplete blood count recovery (43% vs. 28% vs. 34%, respectively, p = 0.003) and pre-HCT MRD (38% vs. 16% vs. 24%, respectively, p < 0.001) whereas the time from the last remission to HCT was shorter (72 vs. 104 vs. 96 days, respectively, p < 0.001). Most patients with secondary AML, either therapy-related or AHD, were transplanted in first remission (91% and 87% vs. 73% for patients with de novo AML, p < 0.001) and they were more likely to receive non-MAC regimens (53% and 56% vs. 36%, respectively, p < 0.001).
Table 1.
Pre-HCT demographic and clinical characteristics of study cohort (n = 979), stratified according to disease status at diagnosis (de novo vs. therapy-related vs. after antecedent hematologic disorder [AHD]).
| Characteristic | All Patients (n = 979) |
De Novo (n = 759) | Therapy-Related (n = 115) |
AHD (n = 105) |
|---|---|---|---|---|
| Age at HCT (IQR), years | 55 (42–64) | 53 (40–62) | 57 (48–66) | 63 (56–68) |
| Female gender, n (%) | 454 (46%) | 348 (46%) | 69 (60%) | 37 (35%) |
| WBC count at diagnosis (IQR), G/L | 8 (2–40) | 9 (2–48) | 5 (2–33) | 3 (2–14) |
| Cytogenetic risk (MRC), n (%) | ||||
| Favorable | 72 (8%) | 60 (8%) | 12 (11%) | 0 |
| Intermediate | 659 (70%) | 520 (71%) | 68 (61%) | 71 (72%) |
| Adverse | 213 (23%) | 153 (21%) | 32 (29%) | 28 (28%) |
| Time from last remission to HCT (IQR), days | 98 (69–146) | 104 (72–150) | 96 (69–132) | 72 (53–105) |
| Disease status at HCT, n (%) | ||||
| First remission | 747 (76%) | 551 (73%) | 105 (91%) | 91 (87%) |
| Second remission | 232 (24%) | 208 (27%) | 10 (8.7%) | 14 (13%) |
| MFC MRD status before HCT, n (%) | ||||
| MRD-negative | 788 (80%) | 636 (84%) | 87 (76%) | 65 (62%) |
| MRD-positive | 191 (20%) | 123 (16%) | 28 (24%) | 40 (38%) |
| Recovered peripheral blood counts before HCT, n (%) |
680 (69%) | 544 (72%) | 76 (66%) | 60 (57%) |
| HCT-CI category, n (%) | ||||
| Low | 339 (35%) | 293 (39%) | 8 (7.0%) | 38 (36%) |
| Intermediate | 347 (35%) | 279 (37%) | 29 (25%) | 39 (37%) |
| High | 293 (30%) | 187 (25%) | 78 (68%) | 28 (27%) |
| Stem cell source, n (%) | ||||
| BM | 81 (8%) | 68 (9%) | 8 (7%) | 5 (5%) |
| PBSC | 766 (78%) | 584 (77%) | 91 (79%) | 91 (87%) |
| Cord blood | 132 (13%) | 107 (14%) | 16 (14%) | 9 (9%) |
| HLA matching, n (%) | ||||
| Identical related donor | 227 (23%) | 173 (23%) | 35 (30%) | 19 (18%) |
| Matched unrelated donor | 482 (49%) | 369 (49%) | 56 (49%) | 57 (54%) |
| 1–2 allele mismatch | 101 (10%) | 79 (10%) | 5 (4%) | 17 (16%) |
| Haplo-identical | 37 (4%) | 31 (4%) | 3 (3%) | 3 (3%) |
| Cord blood | 132 (13%) | 107 (14%) | 16 (14%) | 9 (9%) |
| Conditioning regimen intensity, n (%) | ||||
| MAC | 583 (60%) | 483 (64%) | 51 (44%) | 49 (47%) |
| Non-MAC | 396 (40%) | 276 (36%) | 64 (56%) | 56 (53%) |
Abbreviations: BM, bone marrow; ELN, European LeukemiaNet; HCT, hematopoietic cell transplantation; HCT-CI, HCT comorbidity index; HLA, human leukocyte antigen; MAC, myeloablative conditioning; MFC, multiparameter flow cytometry; MRC, U.K. Medical Research Council; MRD, measurable residual disease; PBSC, peripheral blood stem cells; WBC, white blood cell count.
As the definitions of sAML were recently changed [10,11], we also compared the three groups after reclassifying five patients with previous auto-immune conditions treated with either methotrexate (n = 3), and, by analogy, mercaptopurine (n = 1) or cyclophosphamide (n = 1), and 34 patients with AHD diagnosed ≤3 months before AML diagnosis (MDS, n = 28; CMML, n = 3; MPN, n = 3) as de novo AML. As summarized in Supplementary Table S2, the characteristics of the three patient subsets did not significantly change with this reclassification.
3.2. Relationship between Secondary AML Status and Post-HCT Outcome
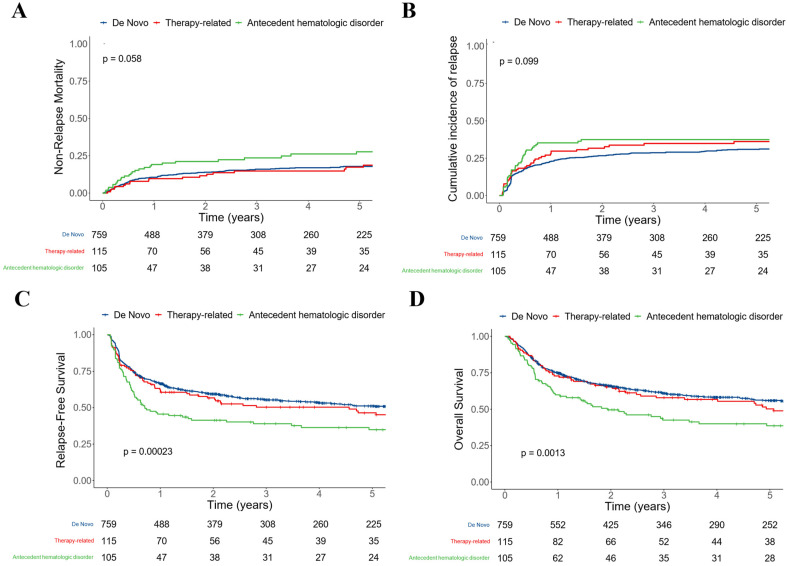
After a median follow-up of 5.13 years after HCT among survivors (IQR: 2.30–9.01), there were 308 relapses, 460 deaths, and 191 NRM events. Relapse was non significantly higher in patients with AHD (35% [26–45%] vs. 23% [20–26%] vs. 28% [20–36%] at three years for those with de novo and therapy-related AML, respectively, Log-Rank test: p = 0.099; Figure 1) as was NRM (24% [15–32%] vs. 16% [13–19%] vs. 15% [8–22%] at three years, p = 0.058). This translated into statistically significant lower RFS (39% [31–50%] vs. 55% [52–59%] vs. 50% [42–61%] at three years, p < 0.001) and OS (43% [34–54%] vs. 61% [58–65%] vs. 58% [49–68%] at three years, p = 0.001) in patients with AHD. Using the updated classification schemes for secondary AML moderately modified these observations, with relapse being statistically significantly higher in patients with AHD (44% [32–56%] vs. 29% [26–32%] vs. 34% [25–43%] at three years, p = 0.044; Supplementary Figure S1). As the 34 patients not considered as having AHD in this last analysis were more likely to have prior MDS or not have been previously treated for the AHD, we explored whether these characteristics were associated with post-HCT outcomes. After considering all patients with AHD, including those with prior exposure to cytotoxic therapy, neither type of AHD nor previous therapy for AHD were associated with post-HCT outcome (Supplementary Figures S2 and S3).
3.3. AML after AHD as an Independent Prognostic Factor for Post-HCT Outcome
To study the relationship between AML after AHD and post-HCT outcomes in more detail, we evaluated univariable and multivariable regression models for the endpoints of NRM, relapse, RFS, and OS. In univariable analysis, AML after AHD was associated with NRM (hazard ratio [HR] = 1.94 [1.30–2.88], p = 0.001), relapse (HR = 1.54 [1.11–2.15], p = 0.011), RFS (HR = 1.69 [1.31–2.18], p < 0.001), and OS (HR = 1.63 [1.25–2.12], p < 0.001) whereas therapy-related AML was not (Table 2). Similar results were observed when limiting patients with AHD to those with a three-month interval between AHD and AML diagnosis (as performed in the 2022 classification scheme), including NRM (HR = 2.13 [1.35–3.37], p = 0.001), relapse (HR = 1.81 [1.24–2.63], p = 0.002), RFS (HR = 1.93 [1.44–2.57], p < 0.001), and OS (HR = 1.69 [1.24–2.29], p < 0.001). Similar C-statistic values (indicating similar predictive accuracy) were observed when considering AHD without any time requirement before AML diagnosis or with a three-month time requirement (0.53 vs. 0.53 for NRM, 0.53 vs. 0.53 for relapse, 0.53 vs. 0.53 for RFS, and 0.53 vs. 0.52 for OS).
Table 2.
Univariable regression models of study cohort.
| Non-Relapse Mortality | Relapse | RFS | OS | |||||
|---|---|---|---|---|---|---|---|---|
| HR (95% CI) | p | HR (95% CI) | p | HR (95% CI) | p | HR (95% CI) | p | |
| Age at transplantation, years | 1.04 (1.02–1.05) | <0.001 | 1.01 (1.00–1.02) | 0.035 | 1.02 (1.01–1.03) | <0.001 | 1.02 (1.01–1.03) | <0.001 |
| Female gender | 0.71 (0.54–0.95) | 0.022 | 0.85 (0.68–1.06) | 0.2 | 0.79 (0.67–0.95) | 0.011 | 0.81 (0.67–0.97) | 0.022 |
| WBC count at diagnosis, G/L | 1.00 (1.00–1.00) | 0.3 | 1.00 (1.00–1.00) | 0.5 | 1.00 (1.00–1.00) | 0.3 | 1.00 (1.00–1.00) | 0.2 |
| Disease status at diagnosis | ||||||||
| De novo | Ref. | Ref. | Ref. | Ref. | ||||
| Therapy-related | 1.06 (0.68–1.66) | 0.88 | 1.19 (0.85–1.67) | 0.3 | 1.14 (0.88–1.50) | 0.3 | 1.12 (0.84–1.48) | 0.4 |
| Antecedent hematologic disorder | 1.94 (1.30–2.88) | 0.001 | 1.54 (1.11–2.15) | 0.011 | 1.69 (1.31–2.18) | <0.001 | 1.63 (1.25–2.12) | <0.001 |
| Cytogenetic risk (MRC) | ||||||||
| Favorable | Ref. | Ref. | Ref. | Ref. | ||||
| Intermediate | 1.43 (0.81–2.52) | 0.2 | 1.75 (0.99–3.06) | 0.052 | 1.59 (1.06–2.37) | 0.024 | 1.74 (1.13–2.69) | 0.012 |
| Adverse | 0.98 (0.51–1.89) | >0.9 | 3.20 (1.79–5.71) | <0.001 | 2.11 (1.38–3.21) | <0.001 | 2.22 (1.40–3.50) | <0.001 |
| Time from last remission to HCT, days | 1.00 (1.00–1.00) | 0.5 | 1.00 (1.00–1.00) | 0.034 | 1.00 (1.00–1.00) | 0.2 | 1.00 (1.00–1.00) | 0.3 |
| Disease status at HCT | ||||||||
| First remission | Ref. | Ref. | Ref. | Ref. | ||||
| Second remission | 1.20 (0.87–1.66) | 0.3 | 1.36 (1.06–1.74) | 0.016 | 1.30 (1.06–1.58) | 0.010 | 1.34 (1.09–1.64) | 0.005 |
| MFC MRD status before HCT | ||||||||
| MRD-negative | Ref. | Ref. | Ref. | Ref. | ||||
| MRD-positive | 1.60 (1.10–2.32) | 0.014 | 4.28 (3.40–5.40) | <0.001 | 3.11 (2.57–3.76) | <0.001 | 2.65 (2.18–3.23) | <0.001 |
| Recovered peripheral blood counts before HCT | 0.60 (0.45–0.80) | <0.001 | 0.95 (0.74–1.21) | 0.7 | 0.79 (0.66–0.95) | 0.014 | 0.76 (0.63–0.92) | 0.006 |
| HCT-CI category | ||||||||
| Low | Ref. | Ref. | Ref. | Ref. | ||||
| Intermediate | 1.25 (0.87–1.79) | 0.2 | 1.10 (0.84–1.44) | 0.5 | 1.15 (0.93–1.43) | 0.2 | 1.17 (0.93–1.46) | 0.2 |
| High | 1.70 (1.19–2.42) | 0.003 | 1.16 (0.87–1.53) | 0.3 | 1.34 (1.08–1.67) | 0.008 | 1.41 (1.12–1.77) | 0.003 |
| Stem cell source | ||||||||
| BM | Ref. | Ref. | Ref. | Ref. | ||||
| PBSC | 1.91 (0.97–3.74) | 0.060 | 0.69 (0.48–0.98) | 0.036 | 0.93 (0.68–1.27) | 0.6 | 0.93 (0.67–1.27) | 0.6 |
| Cord blood | 2.03 (0.96–4.30) | 0.065 | 0.56 (0.35–0.90) | 0.017 | 0.85 (0.58–1.25) | 0.4 | 0.94 (0.63–1.39) | 0.7 |
| HLA matching | ||||||||
| Identical related donor | Ref. | Ref. | Ref. | Ref. | ||||
| Matched unrelated donor | 1.09 (0.75–1.59) | 0.6 | 0.97 (0.74–1.28) | 0.8 | 1.02 (0.81–1.27) | 0.9 | 1.04 (0.82–1.32) | 0.7 |
| 1–2 allele mismatch | 2.53 (1.61–3.96) | <0.001 | 1.15 (0.77–1.73) | 0.5 | 1.61 (1.20–2.17) | 0.002 | 1.80 (1.32–2.44) | <0.001 |
| Haplo-identical | 1.48 (0.63–3.50) | 0.4 | 1.74 (1.02–2.94) | 0.040 | 1.68 (1.08–2.64) | 0.023 | 1.75 (1.08–2.82) | 0.022 |
| Cord blood | 1.37 (0.85–2.22) | 0.2 | 0.81 (0.54–1.22) | 0.3 | 1.00 (0.73–1.36) | >0.9 | 1.13 (0.82–1.56) | 0.4 |
| Conditioning regimen intensity | ||||||||
| MAC | Ref. | Ref. | Ref. | Ref. | ||||
| Non-MAC | 2.28 (1.72–3.04) | <0.001 | 1.36 (1.08–1.70) | 0.008 | 1.66 (1.39–1.98) | <0.001 | 1.60 (1.33–1.92) | <0.001 |
Abbreviations: BM, bone marrow; ELN, European LeukemiaNet; HCT, hematopoietic cell transplantation; HCT-CI, HCT comorbidity index; HLA, human leukocyte antigen; MAC, myeloablative conditioning; MFC, multiparameter flow cytometry; MRC, U.K. Medical Research Council; MRD, measurable residual disease; PBSC, peripheral blood stem cells; WBC, white blood cell count.
Figure 1.
Post-HCT outcomes for 979 adults with AML undergoing allogeneic HCT while in first or second morphologic remission, stratified by disease status at diagnosis (de novo vs. therapy-related vs. antecedent hematologic disorder); (A) Non-relapse mortality; (B) relapse; (C) relapse-free survival; and (D) overall survival.
After multivariable adjustment, AML after AHD remained significantly associated with NRM (HR = 1.59 [1.01–2.52], p = 0.047) but not relapse (HR = 1.07 [0.73–1.58], p = 0.7), RFS (HR = 1.20 [0.89–1.61], p = 0.2), or OS (HR = 1.19 [0.88–1.62], p = 0.2; Table 3). As AML after AHD was not independently associated with post-HCT outcomes other than NRM, we sought to identify variables that were associated with the outcome by performing univariable regression models in patients with AHD (n = 126). In these patients, adverse cytogenetic risk (HR = 1.80 [1.01–3.20], p = 0.046) and positive pre-HCT MRD by MFC (HR = 2.21 [1.28–3.81], p = 0.005) were associated with relapse and positive pre-HCT MRD was associated with RFS (HR = 1.70 [1.10–2.61], p = 0.016) and OS (HR = 1.75 [1.12–2.72], p = 0.014; Table 4). As patients with AHD were significantly older, we specifically explored the association between age and post-HCT outcomes, dichotomizing patients into those younger vs. older than 60 years old. While the NRM for younger and older patients was similar (at three years: 22% [10–34%] vs. 19% [7–31%], p = 0.99), as was OS (at three years: 55% [42–71%] vs. 38% [29–52%], p = 0.38), relapse was non-significantly higher (at three years: 26% [14–39%] vs. 48% [37–60%], p = 0.08) and RFS was non-significantly lower (at three years: 52% [39–68%] vs. 33% [24–45%], p = 0.07) in younger patients. In contrast to the whole study cohort, non-MAC was not associated with NRM, RFS, or OS.
Table 3.
Multivariable regression models of study cohort.
| Non-Relapse Mortality | Relapse | RFS | OS | |||||
|---|---|---|---|---|---|---|---|---|
| HR (95% CI) | p | HR (95% CI) | p | HR (95% CI) | p | HR (95% CI) | p | |
| Age at transplantation, years | 1.02 (1.00–1.04) | 0.012 | 1.00 (0.99–1.01) | 0.4 | 1.00 (1.00–1.01) | 0.3 | 1.01 (1.00–1.01) | 0.2 |
| Female gender | 0.75 (0.55–1.03) | 0.071 | 1.02 (0.80–1.30) | 0.9 | 0.91 (0.75–1.10) | 0.3 | 0.87 (0.71–1.06) | 0.2 |
| WBC count at diagnosis, G/L | 1.00 (1.00–1.01) | 0.068 | 1.00 (1.00–1.00) | 0.013 | 1.00 (1.00–1.00) | 0.002 | 1.00 (1.00–1.00) | 0.004 |
| Disease status at diagnosis | ||||||||
| De novo | Ref. | Ref. | Ref. | Ref. | ||||
| Therapy-related | 0.84 (0.51–1.39) | 0.5 | 0.86 (0.59–1.26) | 0.4 | 0.89 (0.66–1.21) | 0.5 | 0.93 (0.68–1.27) | 0.6 |
| Antecedent hematologic disorder | 1.59 (1.01–2.52) | 0.047 | 1.07 (0.73–1.58) | 0.7 | 1.20 (0.89–1.61) | 0.2 | 1.19 (0.88–1.62) | 0.2 |
| Cytogenetic risk (MRC) | ||||||||
| Favorable | Ref. | Ref. | Ref. | Ref. | ||||
| Intermediate | 1.28 (0.69–2.37) | 0.4 | 1.97 (1.06–3.65) | 0.031 | 1.58 (1.02–2.43) | 0.040 | 1.74 (1.09–2.77) | 0.020 |
| Adverse | 0.83 (0.40–1.72) | 0.6 | 3.20 (1.66–6.17) | <0.001 | 1.93 (1.20–3.10) | 0.007 | 2.07 (1.24–3.44) | 0.005 |
| Time from last remission to HCT, days | 1.00 (1.00–1.00) | >0.9 | 1.00 (1.00–1.00) | 0.5 | 1.00 (1.00–1.00) | 0.7 | 1.00 (1.00–1.00) | 0.7 |
| Disease status at HCT | ||||||||
| First remission | Ref. | Ref. | Ref. | Ref. | ||||
| Second remission | 1.18 (0.80–1.74) | 0.4 | 1.43 (1.05–1.94) | 0.023 | 1.31 (1.03–1.66) | 0.029 | 1.34 (1.05–1.71) | 0.020 |
| MFC MRD status before HCT | ||||||||
| MRD-negative | Ref. | Ref. | Ref. | Ref. | ||||
| MRD-positive | 1.29 (0.84–1.97) | 0.2 | 4.31 (3.31–5.62) | <0.001 | 2.95 (2.37–3.67) | <0.001 | 2.39 (1.91–2.99) | <0.001 |
| Recovered peripheral blood counts before HCT | 0.76 (0.55–1.05) | 0.10 | 1.17 (0.89–1.53) | 0.3 | 1.00 (0.81–1.22) | <0.9 | 0.91 (0.74–1.13) | 0.4 |
| HCT-CI category | ||||||||
| Low | Ref. | Ref. | Ref. | Ref. | ||||
| Intermediate | 1.16 (0.79–1.68) | 0.4 | 1.07 (0.80–1.43) | 0.6 | 1.10 (0.87–1.38) | 0.4 | 1.10 (0.86–1.40) | 0.4 |
| High | 1.52 (1.03–2.23) | 0.034 | 1.21 (0.88–1.65) | 0.2 | 1.29 (1.01–1.65) | 0.039 | 1.33 (1.04–1.72) | 0.026 |
| Stem cell source | ||||||||
| BM | Ref. | Ref. | Ref. | Ref. | ||||
| PBSC | 1.34 (0.66–2.75) | 0.4 | 0.64 (0.42–0.96) | 0.033 | 0.78 (0.55–1.11) | 0.2 | 0.85 (0.59–1.23) | 0.4 |
| Cord blood | 2.24 (0.96–5.23) | 0.062 | 0.46 (0.26–0.83) | 0.009 | 0.77 (0.49–1.23) | 0.3 | 0.97 (0.60–1.58) | >0.9 |
| HLA matching | ||||||||
| Identical related donor | Ref. | Ref. | Ref. | Ref. | ||||
| Matched unrelated donor | 0.94 (0.63–1.41) | 0.8 | 0.89 (0.66–1.20) | 0.4 | 0.90 (0.71–1.15) | 0.4 | 0.93 (0.72–1.19) | 0.5 |
| 1–2 allele mismatch | 1.80 (1.11–2.93) | 0.018 | 0.95 (0.62–1.47) | 0.8 | 1.28 (0.93–1.76) | 0.13 | 1.48 (1.06–2.05) | 0.021 |
| Haplo-identical | 1.70 (0.68–4.24) | 0.3 | 1.29 (0.72–2.32) | 0.4 | 1.41 (0.86–2.30) | 0.2 | 1.56 (0.92–2.65) | 0.10 |
| Conditioning regimen intensity | ||||||||
| MAC | Ref. | Ref. | Ref. | Ref. | ||||
| Non-MAC | 1.51 (1.03–2.22) | 0.033 | 1.71 (1.27–2.30) | <0.001 | 1.66 (1.31–2.09) | <0.001 | 1.48 (1.16–1.89) | 0.002 |
Abbreviations: BM, bone marrow; ELN, European LeukemiaNet; HCT, hematopoietic cell transplantation; HCT-CI, HCT comorbidity index; HLA, human leukocyte antigen; MAC, myeloablative conditioning; MFC, multiparameter flow cytometry; MRC, U.K. Medical Research Council; MRD, measurable residual disease; PBSC, peripheral blood stem cells; WBC, white blood cell count.
Table 4.
Univariable regression models of patients with AHD (n = 126).
| Non-Relapse Mortality | Relapse | RFS | OS | |||||
|---|---|---|---|---|---|---|---|---|
| HR (95% CI) | p | HR (95% CI) | p | HR (95% CI) | p | HR (95% CI) | p | |
| Age at transplantation, years | 1.00 (0.97–1.03) | 0.8 | 1.02 (0.99–1.04) | 0.2 | 1.01 (0.99–1.03) | 0.3 | 1.00 (0.98–1.02) | 0.8 |
| Female gender | 0.57 (0.26–1.23) | 0.2 | 0.80 (0.46–1.41) | 0.4 | 0.71 (0.45–1.12) | 0.14 | 0.66 (0.41–1.07) | 0.089 |
| WBC count at diagnosis, G/L | 1.00 (0.99–1.01) | 0.6 | 1.00 (0.99–1.01) | 0.8 | 1.00 (0.99–1.01) | >0.9 | 1.00 (0.99–1.01) | 0.9 |
| Cytogenetic risk (MRC) | ||||||||
| Favorable | ||||||||
| Intermediate | Ref. | Ref. | Ref. | Ref. | ||||
| Adverse | 0.51 (0.20–1.32) | 0.2 | 1.80 (1.01–3.20) | 0.046 | 1.18 (0.73–1.89) | 0.5 | 1.01 (0.61–1.66) | >0.9 |
| Time from last remission to HCT, days | 1.00 (0.99–1.01) | >0.9 | 1.00 (1.00–1.01) | 0.3 | 1.00 (1.00–1.01) | 0.3 | 1.00 (1.00–1.00) | 0.7 |
| Disease status at HCT | ||||||||
| First remission | Ref. | Ref. | Ref. | Ref. | ||||
| Second remission | 1.12 (0.39–3.22) | 0.8 | 1.71 (0.86–3.42) | 0.13 | 1.49 (0.84–2.65) | 0.2 | 1.23 (0.68–2.24) | 0.5 |
| MFC MRD status before HCT | ||||||||
| MRD-negative | Ref. | Ref. | Ref. | Ref. | ||||
| MRD-positive | 1.08 (0.52–2.25) | 0.8 | 2.21 (1.28–3.81) | 0.005 | 1.70 (1.10–2.61) | 0.016 | 1.75 (1.12–2.72) | 0.014 |
| Recovered peripheral blood counts before HCT | 0.91 (0.46–1.82) | 0.8 | 1.26 (0.72–2.20) | 0.4 | 1.11 (0.72–1.71) | 0.6 | 1.10 (0.70–1.71) | 0.7 |
| HCT-CI category | ||||||||
| Low | Ref. | Ref. | Ref. | Ref. | ||||
| Intermediate | 1.33 (0.57–3.11) | 0.5 | 1.06 (0.50–2.22) | 0.9 | 1.17 (0.67–2.04) | 0.6 | 1.51 (0.83–2.75) | 0.2 |
| High | 1.85 (0.76–4.49) | 0.2 | 2.51 (1.27–4.94) | 0.008 | 2.26 (1.32–3.86) | 0.003 | 2.58 (1.45–4.58) | 0.001 |
| Stem cell source | ||||||||
| BM | Ref. | Ref. | Ref. | Ref. | ||||
| PBSC | 0.21 (0.06–0.71) | 0.012 | 1.54 (0.21–11.2) | 0.7 | 0.54 (0.20–1.48) | 0.2 | 0.38 (0.14–1.06) | 0.066 |
| Cord blood | 0.52 (0.11–2.34) | 0.4 | 2.68 (0.32–22.3) | 0.4 | 1.07 (0.33–3.41) | >0.9 | 0.70 (0.21–2.29) | 0.6 |
| HLA matching | ||||||||
| Identical related donor | Ref. | Ref. | Ref. | Ref. | ||||
| Matched unrelated donor | 1.12 (0.47–2.68) | 0.8 | 1.70 (0.78–3.72) | 0.2 | 1.43 (0.80–2.54) | 0.2 | 1.14 (0.64–2.05) | 0.7 |
| 1–2 allele mismatch | 1.28 (0.42–3.95) | 0.7 | 1.57 (0.57–4.33) | 0.4 | 1.42 (0.67–3.02) | 0.4 | 1.36 (0.63–2.93) | 0.4 |
| Haplo-identical | 6.03 (0.69–52.5) | 0.10 | 5.39 (1.11–26.1) | 0.036 | 5.35 (1.51–19) | 0.009 | 4.33 (1.24–15.1) | 0.022 |
| Cord blood | 2.56 (0.75–8.74) | 0.13 | 2.73 (0.94–7.90) | 0.064 | 2.61 (1.17–5.81) | 0.019 | 2.05 (0.90–4.68) | 0.086 |
| Conditioning regimen intensity | ||||||||
| MAC | Ref. | Ref. | Ref. | Ref. | ||||
| Non-MAC | 0.88 (0.44–1.76) | 0.7 | 2.11 (1.18–3.77) | 0.012 | 1.48 (0.96–2.29) | 0.075 | 1.06 (0.68–1.65) | 0.8 |
Abbreviations: BM, bone marrow; ELN, European LeukemiaNet; HCT, hematopoietic cell transplantation; HCT-CI, HCT comorbidity index; HLA, human leukocyte antigen; MAC, myeloablative conditioning; MFC, multiparameter flow cytometry; MRC, U.K. Medical Research Council; MRD, measurable residual disease; PBSC, peripheral blood stem cells; WBC, white blood cell count.
3.4. Relationship between Disease Status, Conditioning Intensity, and Post-HCT Outcomes
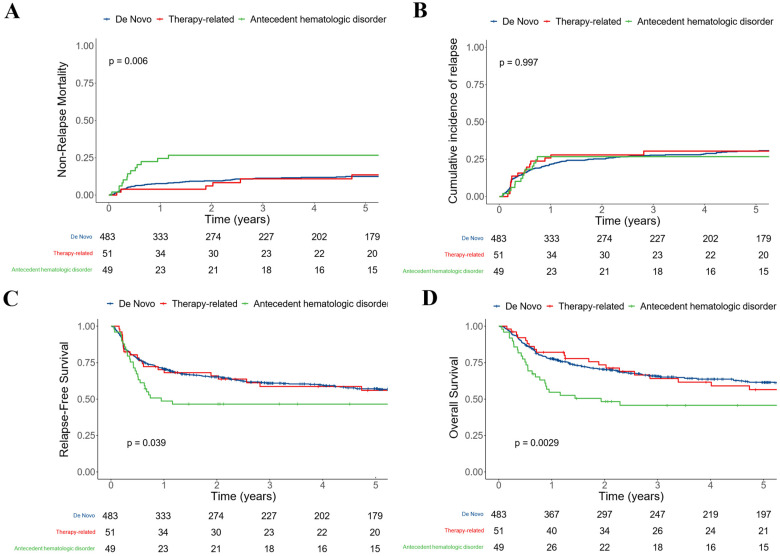
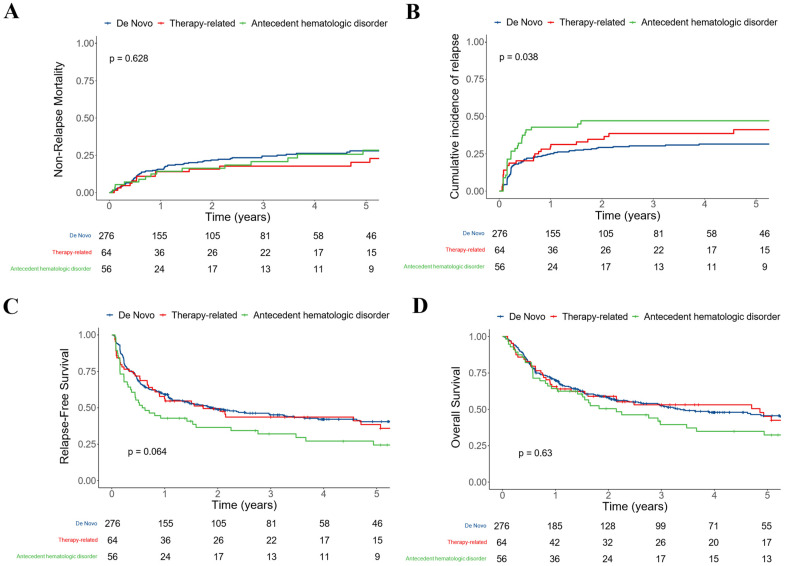
To further explore the relationship between disease status and post-HCT outcomes, we performed subset analyses in which we studied patients who underwent transplants after MAC or non-MAC conditioning separately. These analyses were further motivated by a significant interaction between conditioning intensity (MAC vs. non-MAC) and AHD for NRM (p = 0.043) but not relapse (p = 0.2), RFS (p = 0.8), or OS (p = 0.085). In patients who received MAC, AHD was significantly associated with NRM (26% [14–39%] vs. 11% [8–14%] vs. 11% [2–20%] at three years for those with de novo and therapy-related AML, respectively, p = 0.006) but not for relapse (27% [14–39%] vs. 28% [24–32%] vs. 31% [17–44%] at three years, respectively, p = 0.997; Figure 2). This translated into significantly lower RFS (47% [34–63%] vs. 61% [57–66%] vs. 59% [46–75%] at three years, respectively, p = 0.039) and OS (46% [34–63%] vs. 66% [62–70%] vs. 64% [52–80%] at three years, respectively, p = 0.0029). After multivariable adjustment, AHD remained statistically associated with NRM (HR = 2.71 [1.38–5.34], p = 0.004) but not with relapse (HR = 0.58 [0.31–1.07], p = 0.081), RFS (HR = 0.96 [0.61–1.52], p = 0.9), or OS (HR = 1.34 [0.84–2.13], p = 0.2) in patients receiving MAC. On the other hand, in patients who received non-MAC, AHD was not significantly associated with NRM (21% [10–32%] vs. 25% [19–30%] vs. 18% [8–28%] at three years, respectively, p = 0.628) but was associated with relapse (47% [34–61%] vs. 30% [25–36%] vs. 39% [26–51%] at three years, respectively, p = 0.038; Figure 3). This translated into non-significantly lower RFS (32% [22–48%] vs. 45% [39–52%] vs. 44% [33–58%] at three years, respectively, p = 0.064) whereas OS was similar (40% [28–56%] vs. 53% [47–59%] vs. 53% [42–67%] at three years, respectively, p = 0.63) in the subset of patients with AHD AML. Similar results were observed when distinguishing RIC from non-myeloablative conditioning (Supplementary Figures S4 and S5). After multivariable adjustment, AHD remained statistically associated with relapse (HR = 1.86 [1.11–3.13], p = 0.018) and showed a borderline association with RFS (HR = 1.47 [0.98–2.22], p = 0.062), but not NRM (HR = 1.19 [0.62–2.27], p = 0.6) or OS (HR = 1.15 [0.75–1.75], p = 0.5).
Figure 2.
Post-HCT outcomes for 583 adults with AML undergoing allogeneic HCT following myeloablative conditioning while in first or second morphologic remission, stratified by disease status at diagnosis (de novo vs. therapy-related vs. antecedent hematologic disorder): (A) Non-relapse mortality; (B) relapse; (C) relapse-free survival; and (D) overall survival.
Figure 3.
Post-HCT outcomes for 396 adults with AML undergoing allogeneic HCT following non-MAC while in first or second morphologic remission, stratified by disease status at diagnosis (de novo vs. therapy-related vs. antecedent hematologic disorder): (A) Non-relapse mortality; (B) relapse; (C) relapse-free survival; and (D) overall survival.
4. Discussion
Recently introduced classification systems consider secondary AML as a diagnostic qualifier, in line with the increasing understanding that underlying genetic characteristics rather than clinical history largely account for worse outcomes seen in this patient subset [9,10,11]. Consistent with this notion, in our large retrospective analyses, we found very little evidence of an independent prognostic role for clinical history in multivariable analyses, except for a significant interaction between conditioning intensity and AML arising from AHD. Specifically, we found that compared to patients with de novo or therapy-related AML, those with AML arising from an AHD had a significantly higher risk of NRM if treated with MAC (but this did not translate into differences in post-transplant relapse rates or OS).
In the 2022 disease classifications (Internal Consensus Classification, WHO), some of the parameters for when exactly an AML should be considered secondary have changed. Specifically, it is now proposed that patients who developed AML after receiving cytotoxic therapy such as methotrexate for auto-immune conditions, or patients for whom the time interval between AHD and AML diagnosis was less than three months, should no longer be considered as secondary AML. Nevertheless, for our main analysis, we chose to consider these patients as secondary AML for comparability with prior studies [1,2,4,12,16,17,18,19,22,40,41]. Complicating comparability, some of the older studies already used the 3-month time interval [5,15], but none classified AML cases after prior exposure to cytotoxic therapy such as methotrexate as de novo. However, we then performed sensitivity analyses considering these classification changes, which revealed a limited impact on the characteristics of each patient subgroup and the observed post-HCT outcomes. In these sensitivity analyses, our main findings were largely unchanged. As multilineage dysplasia is no longer recognized as a prognostic feature [42], these patients were considered as having de novo AML unless they were previously diagnosed with an AHD or had prior exposure to cytotoxic therapy.
Without adjustments, we observed that AML after AHD but not therapy-related AML was associated with post-HCT outcomes in our cohort. This finding is consistent with a recent report on a cohort of patients developing myeloid neoplasms after prior therapy for solid tumors [43]. The finding contrasts, however, with one previous report showing that both patients with AHD and therapy-related AML had inferior outcomes compared to patients with de novo AML [17]. A large part of these outcome differences could be attributed to differences in patient/disease characteristics. Patients with AHD were, on average, older and less likely to have favorable-risk cytogenetics but more likely to have pre-HCT MRD by MFC than the other patients. These differences explained why AHD was no longer associated with relapse or RFS after multivariable analyses [16,19], although one study previously observed an independent association between secondary AML and relapse [17].
As in previous reports [6,16,17], we observed in our study that secondary AML, and more specifically, AHD, was independently associated with NRM, suggesting that patients with AHD experienced more complications after transplant. Although there is no clear explanation for this observation with potential patient differences that are not fully captured in our multivariable adjustments, it is supported by the fact that the association between AHD and NRM was mostly observed in patients receiving MAC. As patients previously treated for AHD had similar outcomes to those who were not treated, increased exposure to pre-HCT therapies does not appear to have a role in increased NRM. Despite being older, patients with AHD had a similar number of comorbidities, as assessed by the HCT-CI. This may represent a bias toward selecting fitter subsets of patients for allografting. As stated, the association between AHD and NRM was attenuated after multivariable adjustment for other variables associated with increased NRM such as age.
Of note, conditioning intensity was not equally associated with post-HCT outcomes in patients with AHD. As in one previous report [16], but not another from the EBMT registry [44], we observed that patients with secondary AML receiving MAC were more likely to have increased NRM even after multivariable adjustment. In contrast to that previous report, but similar to a study from the EBMT registry [44], patients who received non-MAC had increased relapse and decreased RFS in our cohort, albeit not statistically significantly so after multivariable adjustment. Although we usually recommend that patients who are fit to tolerate MAC should receive a high-intensity conditioning regimen, more caution should be applied in patients with AHD. The intensity of conditioning was not associated with post-HCT outcomes in patients with therapy-related AML, which was observed in one study [45], but not in two others [46,47], in which relapse risk was higher in patients receiving non-MAC regimens.
The retrospective nature of our study analyzing post-HCT outcomes of patients for whom conditioning intensity was nonrandomly assigned limits our ability to draw definitive conclusions regarding the management of patients with AHD AML. Our general management has been to use MAC whenever it was felt that it could be safely administered based on patient age and comorbidities. Another limitation is the fact that mutational profiles were available only for a small subset of patients.
5. Conclusions
The fact that AML developed post cytotoxic therapy or after AHD provides little prognostic value (except for an increased risk of NRM in patients with AHD) supports the most recent proposal to use this information largely as a diagnostic qualifier rather than a prognostic variable.
Acknowledgments
The authors acknowledge the excellent care provided by the physicians and nurses of the HCT teams, the staff in the Long-Term Follow-up office at the Fred Hutchinson Cancer Center, the Hematopathology Laboratory at the University of Washington, and the patients for participating in our research protocols.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/cancers15020352/s1, Figure S1: Post-HCT outcomes for 990 adults with AML undergoing allogeneic HCT while in first or second morphologic remission, stratified by disease status at diagnosis (de novo vs. therapy-related vs. antecedent hematologic disorder) after considering as de novo AML, five patients with auto-immune disorders treated with methotrexate, mercaptopurine, and cyclophosphamide and 34 patients with AHD diagnosed less than three months before AML; Figure S2: Post-HCT outcomes for 125 adults with AHD AML undergoing allogeneic HCT while in first or second morphologic remission, stratified by type of disease (myelodysplastic syndrome [MDS] vs. chronic myelomonocytic leukemia [CMML] vs. myeloproliferative neoplasm [MPN]; Figure S3: Post-HCT outcomes for 125 adults with AHD AML undergoing allogeneic HCT while in first or second morphologic remission, stratified by prior treatment for AHD (yes vs. no); Figure S4: Post-HCT outcomes for 143 adults with AML undergoing allogeneic HCT following reduced-intensity conditioning while in first or second morphologic remission, stratified by disease status at diagnosis (de novo vs. therapy-related vs. antecedent hematologic disorder); Figure S5: Post-HCT outcomes for 253 adults with AML undergoing allogeneic HCT following non-myeloablative conditioning while in first or second morphologic remission, stratified by disease status at diagnosis (de novo vs. therapy-related vs. antecedent hematologic disorder); Table S1: Primary disease and treatment-related characteristics in patients with therapy-related acute myeloid leukemia (n = 115) and after antecedent hematologic disorder (n = 125); Table S2: Pre-HCT demographic and clinical characteristics of study cohort (n = 979), stratified according to disease status at diagnosis (de novo vs. post cytotoxic therapy vs. after antecedent hematologic disorder [AHD]), after considering as de novo AML, five patients with auto-immune disorders treated with methotrexate, mercaptopurine, and cyclophosphamide and 34 patients with AHD diagnosed less than three months before AML.
Author Contributions
Conceptualization, R.B.W.; methodology, C.O., M.O. and R.B.W.; validation, C.O., E.R.-A., M.O. and R.B.W.; formal analysis, C.O. and M.O.; investigation, C.O., E.R.-A., B.M.S., H.J.D., F.R.A. and R.B.W.; resources, R.B.W.; data curation, C.O., E.R.-A. and R.B.W.; writing—original draft preparation, C.O. and R.B.W.; writing—review and editing, all authors; visualization, C.O. and M.O.; supervision, R.B.W.; project administration, R.B.W.; funding acquisition, R.B.W. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
All patients were treated on Institutional Review Board-approved research protocols (FH-2562 initially approved on 10/10/2011) or standard treatment protocols.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The datasets analyzed during the current study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was funded by grants P01-CA078902, P01-CA018029, and P30-CA015704 from the National Cancer Institute/National Institutes of Health (NCI/NIH), Bethesda, MD, USA.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Hulegårdh E., Nilsson C., Lazarevic V., Garelius H., Antunovic P., Rangert Derolf Å., Möllgård L., Uggla B., Wennström L., Wahlin A., et al. Characterization and Prognostic Features of Secondary Acute Myeloid Leukemia in a Population-Based Setting: A Report from the Swedish Acute Leukemia Registry: Population-Based Study of Secondary AML. Am. J. Hematol. 2015;90:208–214. doi: 10.1002/ajh.23908. [DOI] [PubMed] [Google Scholar]
- 2.Martínez-Cuadrón D., Megías-Vericat J.E., Serrano J., Martínez-Sánchez P., Rodríguez-Arbolí E., Gil C., Aguiar E., Bergua Burgues J.M., Lopez-Lorenzo J.L., Bernal T., et al. Treatment Patterns and Outcomes of 2310 Patients with Secondary Acute Myeloid Leukemia: A PETHEMA Registry Study. Blood Adv. 2021;6:1278–1295. doi: 10.1182/bloodadvances.2021005335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Østgård L.S.G., Kjeldsen E., Holm M.S., Brown P.D.N., Pedersen B.B., Bendix K., Johansen P., Kristensen J.S., Nørgaard J.M. Reasons for Treating Secondary AML as de Novo AML: Reasons for Treating Secondary AML. Eur. J. Haematol. 2010;85:217–226. doi: 10.1111/j.1600-0609.2010.01464.x. [DOI] [PubMed] [Google Scholar]
- 4.Nilsson C., Hulegårdh E., Garelius H., Möllgård L., Brune M., Wahlin A., Lenhoff S., Frödin U., Remberger M., Höglund M., et al. Secondary Acute Myeloid Leukemia and the Role of Allogeneic Stem Cell Transplantation in a Population-Based Setting. Biol. Blood Marrow Transplant. 2019;25:1770–1778. doi: 10.1016/j.bbmt.2019.05.038. [DOI] [PubMed] [Google Scholar]
- 5.Granfeldt Østgård L.S., Medeiros B.C., Sengeløv H., Nørgaard M., Andersen M.K., Dufva I.H., Friis L.S., Kjeldsen E., Marcher C.W., Preiss B., et al. Epidemiology and Clinical Significance of Secondary and Therapy-Related Acute Myeloid Leukemia: A National Population-Based Cohort Study. J. Clin. Oncol. 2015;33:3641–3649. doi: 10.1200/JCO.2014.60.0890. [DOI] [PubMed] [Google Scholar]
- 6.Kayser S., Döhner K., Krauter J., Köhne C.-H., Horst H.A., Held G., von Lilienfeld-Toal M., Wilhelm S., Kündgen A., Götze K., et al. The Impact of Therapy-Related Acute Myeloid Leukemia (AML) on Outcome in 2853 Adult Patients with Newly Diagnosed AML. Blood. 2011;117:2137–2145. doi: 10.1182/blood-2010-08-301713. [DOI] [PubMed] [Google Scholar]
- 7.Lindsley R.C., Mar B.G., Mazzola E., Grauman P.V., Shareef S., Allen S.L., Pigneux A., Wetzler M., Stuart R.K., Erba H.P., et al. Acute Myeloid Leukemia Ontogeny Is Defined by Distinct Somatic Mutations. Blood. 2015;125:1367–1376. doi: 10.1182/blood-2014-11-610543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tariq H., Barnea Slonim L., Coty Fattal Z., Alikhan M.B., Segal J., Gurbuxani S., Helenowski I.B., Zhang H., Sukhanova M., Lu X., et al. Therapy-related Myeloid Neoplasms with Normal Karyotype Show Distinct Genomic and Clinical Characteristics Compared to Their Counterparts with Abnormal Karyotype. Br. J. Haematol. 2022;197:736–744. doi: 10.1111/bjh.18154. [DOI] [PubMed] [Google Scholar]
- 9.Arber D.A., Orazi A., Hasserjian R.P., Borowitz M.J., Calvo K.R., Kvasnicka H.M., Wang S.A., Bagg A., Barbui T., Branford S., et al. International Consensus Classification of Myeloid Neoplasms and Acute Leukemia: Integrating Morphological, Clinical, and Genomic Data. Blood. 2022;140:1200–1228. doi: 10.1182/blood.2022015850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khoury J.D., Solary E., Abla O., Akkari Y., Alaggio R., Apperley J.F., Bejar R., Berti E., Busque L., Chan J.K.C., et al. The 5th Edition of the World Health Organization Classification of Haematolymphoid Tumours: Myeloid and Histiocytic/Dendritic Neoplasms. Leukemia. 2022;36:1703–1719. doi: 10.1038/s41375-022-01613-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Döhner H., Ebert B., Godley L., Levine R., Ossenkoppele G. Diagnosis and Management of AML in Adults: 2022 ELN Recommendations from an International Expert Panel. Blood J. Am. Soc. Hematol. 2022;140:1345–1377. doi: 10.1182/blood.2022016867. [DOI] [PubMed] [Google Scholar]
- 12.Bertoli S., Tavitian S., Bories P., Luquet I., Delabesse E., Comont T., Sarry A., Huguet F., Bérard E., Récher C. Outcome of Patients Aged 60-75 Years with Newly Diagnosed Secondary Acute Myeloid Leukemia: A Single-institution Experience. Cancer Med. 2019;8:3846–3854. doi: 10.1002/cam4.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boddu P.C., Kantarjian H.M., Ravandi F., Garcia-Manero G., Verstovsek S., Jabbour E.J., Takahashi K., Bhalla K., Konopleva M., DiNardo C.D., et al. Characteristics and Outcomes of Older Patients with Secondary Acute Myeloid Leukemia According to Treatment Approach: Secondary AML by Treatment Approach. Cancer. 2017;123:3050–3060. doi: 10.1002/cncr.30704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lancet J.E., Uy G.L., Cortes J.E., Newell L.F., Lin T.L., Ritchie E.K., Stuart R.K., Strickland S.A., Hogge D., Solomon S.R., et al. CPX-351 (Cytarabine and Daunorubicin) Liposome for Injection Versus Conventional Cytarabine Plus Daunorubicin in Older Patients With Newly Diagnosed Secondary Acute Myeloid Leukemia. J. Clin. Oncol. 2018;36:2684–2692. doi: 10.1200/JCO.2017.77.6112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dumas P.-Y., Bertoli S., Bérard E., Médiavilla C., Yon E., Tavitian S., Leguay T., Huguet F., Forcade E., Milpied N., et al. Azacitidine or Intensive Chemotherapy for Older Patients with Secondary or Therapy-Related Acute Myeloid Leukemia. Oncotarget. 2017;8:79126–79136. doi: 10.18632/oncotarget.15988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jentzsch M., Grimm J., Bill M., Brauer D., Backhaus D., Goldmann K., Schulz J., Niederwieser D., Platzbecker U., Schwind S. ELN Risk Stratification and Outcomes in Secondary and Therapy-Related AML Patients Consolidated with Allogeneic Stem Cell Transplantation. Bone Marrow Transplant. 2021;56:936–945. doi: 10.1038/s41409-020-01129-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schmaelter A.-K., Labopin M., Socié G., Itälä-Remes M., Blaise D., Yakoub-Agha I., Forcade E., Cornelissen J., Ganser A., Beelen D., et al. Inferior Outcome of Allogeneic Stem Cell Transplantation for Secondary Acute Myeloid Leukemia in First Complete Remission as Compared to de Novo Acute Myeloid Leukemia. Blood Cancer J. 2020;10:26. doi: 10.1038/s41408-020-0296-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kida M., Usuki K., Uchida N., Fukuda T., Katayama Y., Kondo T., Eto T., Matsuoka K., Matsuhashi Y., Ota S., et al. Outcome and Risk Factors for Therapy-Related Myeloid Neoplasms Treated with Allogeneic Stem Cell Transplantation in Japan. Biol. Blood Marrow Transplant. 2020;26:1543–1551. doi: 10.1016/j.bbmt.2020.04.004. [DOI] [PubMed] [Google Scholar]
- 19.Michelis F.V., Atenafu E.G., Gupta V., Kim D.D., Kuruvilla J., Lipton J.H., Loach D., Seftel M.D., Uhm J., Alam N., et al. Comparable Outcomes Post Allogeneic Hematopoietic Cell Transplant for Patients with de Novo or Secondary Acute Myeloid Leukemia in First Remission. Bone Marrow Transplant. 2015;50:907–913. doi: 10.1038/bmt.2015.59. [DOI] [PubMed] [Google Scholar]
- 20.Maffini E. Measurable Residual Disease (MRD) Status before Allogeneic Hematopoietic Cell Transplantation Impact on Secondary Acute Myeloid Leukemia Outcome. A Study from the Acute Leukemia Working Party (ALWP) of the European Society for Blood and Marrow Transplantation (EBMT) Bone Marrow Transplant. 2022;57:1556–1563. doi: 10.1038/s41409-022-01748-w. [DOI] [PubMed] [Google Scholar]
- 21.Rodríguez-Arbolí E., Orvain C., Othus M., Walter R.B. Significance of Measurable Residual Disease in Adults with Secondary Acute Myeloid Leukemia Undergoing Allogeneic Hematopoietic Cell Transplantation. Bone Marrow Transplant. 2022;57:1732–1734. doi: 10.1038/s41409-022-01794-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kröger N., Eikema D., Köster L., Beelen D., de Wreede L.C., Finke J., Koenecke C., Niederwieser D., Bornhäuser M., Schoenland S., et al. Impact of Primary Disease on Outcome after Allogeneic Stem Cell Transplantation for Transformed Secondary Acute Leukaemia. Br. J. Haematol. 2019;185:725–732. doi: 10.1111/bjh.15819. [DOI] [PubMed] [Google Scholar]
- 23.Arber D.A., Orazi A., Hasserjian R., Thiele J., Borowitz M.J., Le Beau M.M., Bloomfield C.D., Cazzola M., Vardiman J.W. The 2016 Revision to the World Health Organization Classification of Myeloid Neoplasms and Acute Leukemia. Blood. 2016;127:2391–2405. doi: 10.1182/blood-2016-03-643544. [DOI] [PubMed] [Google Scholar]
- 24.Orvain C., Byelykh M., Othus M., Sandmaier B.M., Schoch G., Davis C., Appelbaum F.R., Walter R.B. Relationship Between Pre-Transplant Nutritional Status and Outcomes of Adults with Acute Myeloid Leukemia Undergoing Allogeneic Hematopoietic Cell Transplantation. Transplant. Cell Ther. 2022;28:846.e1–846.e9. doi: 10.1016/j.jtct.2022.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grimwade D., Hills R.K., Moorman A.V., Walker H., Chatters S., Goldstone A.H., Wheatley K., Harrison C.J., Burnett A.K., on behalf of the National Cancer Research Institute Adult Leukaemia Working Group Refinement of Cytogenetic Classification in Acute Myeloid Leukemia: Determination of Prognostic Significance of Rare Recurring Chromosomal Abnormalities among 5876 Younger Adult Patients Treated in the United Kingdom Medical Research Council Trials. Blood. 2010;116:354–365. doi: 10.1182/blood-2009-11-254441. [DOI] [PubMed] [Google Scholar]
- 26.Sorror M.L., Maris M.B., Storb R., Baron F., Sandmaier B.M., Maloney D.G., Storer B. Hematopoietic Cell Transplantation (HCT)-Specific Comorbidity Index: A New Tool for Risk Assessment before Allogeneic HCT. Blood. 2005;106:2912–2919. doi: 10.1182/blood-2005-05-2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Walter R.B., Othus M., Borthakur G., Ravandi F., Cortes J.E., Pierce S.A., Appelbaum F.R., Kantarjian H.A., Estey E.H. Prediction of Early Death After Induction Therapy for Newly Diagnosed Acute Myeloid Leukemia With Pretreatment Risk Scores: A Novel Paradigm for Treatment Assignment. J. Clin. Oncol. 2011;29:4417–4424. doi: 10.1200/JCO.2011.35.7525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Döhner H., Estey E., Grimwade D., Amadori S., Appelbaum F.R., Büchner T., Dombret H., Ebert B.L., Fenaux P., Larson R.A., et al. Diagnosis and Management of AML in Adults: 2017 ELN Recommendations from an International Expert Panel. Blood. 2017;129:424–447. doi: 10.1182/blood-2016-08-733196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Walter R.B., Gooley T.A., Wood B.L., Milano F., Fang M., Sorror M.L., Estey E.H., Salter A.I., Lansverk E., Chien J.W., et al. Impact of Pretransplantation Minimal Residual Disease, As Detected by Multiparametric Flow Cytometry, on Outcome of Myeloablative Hematopoietic Cell Transplantation for Acute Myeloid Leukemia. J. Clin. Oncol. 2011;29:1190–1197. doi: 10.1200/JCO.2010.31.8121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Walter R.B., Buckley S.A., Pagel J.M., Wood B.L., Storer B.E., Sandmaier B.M., Fang M., Gyurkocza B., Delaney C., Radich J.P., et al. Significance of Minimal Residual Disease before Myeloablative Allogeneic Hematopoietic Cell Transplantation for AML in First and Second Complete Remission. Blood. 2013;122:1813–1821. doi: 10.1182/blood-2013-06-506725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Walter R.B., Gyurkocza B., Storer B.E., Godwin C.D., Pagel J.M., Buckley S.A., Sorror M.L., Wood B.L., Storb R., Appelbaum F.R., et al. Comparison of Minimal Residual Disease as Outcome Predictor for AML Patients in First Complete Remission Undergoing Myeloablative or Nonmyeloablative Allogeneic Hematopoietic Cell Transplantation. Leukemia. 2015;29:137–144. doi: 10.1038/leu.2014.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Araki D., Wood B.L., Othus M., Radich J.P., Halpern A.B., Zhou Y., Mielcarek M., Estey E.H., Appelbaum F.R., Walter R.B. Allogeneic Hematopoietic Cell Transplantation for Acute Myeloid Leukemia: Time to Move Toward a Minimal Residual Disease–Based Definition of Complete Remission? J. Clin. Oncol. 2016;34:329–336. doi: 10.1200/JCO.2015.63.3826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhou Y., Othus M., Araki D., Wood B.L., Radich J.P., Halpern A.B., Mielcarek M., Estey E.H., Appelbaum F.R., Walter R.B. Pre- and Post-Transplant Quantification of Measurable (‘Minimal’) Residual Disease via Multiparameter Flow Cytometry in Adult Acute Myeloid Leukemia. Leukemia. 2016;30:1456–1464. doi: 10.1038/leu.2016.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wood B.L. Acute Myeloid Leukemia Minimal Residual Disease Detection: The Difference from Normal Approach. Curr. Protoc. Cytom. 2020;93:e73. doi: 10.1002/cpcy.73. [DOI] [PubMed] [Google Scholar]
- 35.Walter R.B., Sandmaier B.M., Storer B.E., Godwin C.D., Buckley S.A., Pagel J.M., Sorror M.L., Deeg H.J., Storb R., Appelbaum F.R. Number of Courses of Induction Therapy Independently Predicts Outcome after Allogeneic Transplantation for Acute Myeloid Leukemia in First Morphological Remission. Biol. Blood Marrow Transplant. 2015;21:373–378. doi: 10.1016/j.bbmt.2014.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hoffmann A.P., Besch A.L., Othus M., Morsink L.M., Wood B.L., Mielcarek M., Estey E.H., Appelbaum F.R., Walter R.B. Early Achievement of Measurable Residual Disease (MRD)-Negative Complete Remission as Predictor of Outcome after Myeloablative Allogeneic Hematopoietic Cell Transplantation in Acute Myeloid Leukemia. Bone Marrow Transplant. 2020;55:669–672. doi: 10.1038/s41409-019-0739-2. [DOI] [PubMed] [Google Scholar]
- 37.Morsink L.M., Bezerra E.D., Othus M., Wood B.L., Fang M., Sandmaier B.M., Mielcarek M.B., Deeg H.J., Schoch G., Appelbaum F.R., et al. Comparative Analysis of Total Body Irradiation (TBI)-Based and Non-TBI-Based Myeloablative Conditioning for Acute Myeloid Leukemia in Remission with or without Measurable Residual Disease. Leukemia. 2020;34:1701–1705. doi: 10.1038/s41375-019-0671-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Morsink L.M., Othus M., Bezerra E.D., Wood B.L., Fang M., Sandmaier B.M., Mielcarek M., Schoch G., Storb R., Deeg H.J., et al. Impact of Pretransplant Measurable Residual Disease on the Outcome of Allogeneic Hematopoietic Cell Transplantation in Adult Monosomal Karyotype AML. Leukemia. 2020;34:1577–1587. doi: 10.1038/s41375-020-0717-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Paras G., Morsink L.M., Othus M., Milano F., Sandmaier B.M., Zarling L.C., Palmieri R., Schoch G., Davis C., Bleakley M., et al. Conditioning Intensity and Peri-Transplant Flow Cytometric MRD Dynamics in Adult AML. Blood. 2022;139:1694–1706. doi: 10.1182/blood.2021014804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Boddu P., Kantarjian H.M., Garcia-Manero G., Ravandi F., Verstovsek S., Jabbour E., Borthakur G., Konopleva M., Bhalla K.N., Daver N., et al. Treated Secondary Acute Myeloid Leukemia: A Distinct High-Risk Subset of AML with Adverse Prognosis. Blood Adv. 2017;1:1312–1323. doi: 10.1182/bloodadvances.2017008227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Finke J., Schmoor C., Bertz H., Marks R., Wäsch R., Zeiser R., Hackanson B. Long-Term Follow-up of Therapy-Related Myelodysplasia and AML Patients Treated with Allogeneic Hematopoietic Cell Transplantation. Bone Marrow Transplant. 2016;51:771–777. doi: 10.1038/bmt.2015.338. [DOI] [PubMed] [Google Scholar]
- 42.Montalban-Bravo G., Kanagal-Shamanna R., Class C.A., Sasaki K., Ravandi F., Cortes J.E., Daver N., Takahashi K., Short N.J., DiNardo C.D., et al. Outcomes of Acute Myeloid Leukemia with Myelodysplasia Related Changes Depend on Diagnostic Criteria and Therapy. Am. J. Hematol. 2020;95:612–622. doi: 10.1002/ajh.25769. [DOI] [PubMed] [Google Scholar]
- 43.Portugese A.J., Albittar A., Gooley T.H., Deeg H.J. Transplantation for Myeloid Neoplasms with Antecedent Solid Tumor. Cancer. 2022;129:142–150. doi: 10.1002/cncr.34517. [DOI] [PubMed] [Google Scholar]
- 44.Sengsayadeth S., Gatwood K.S., Boumendil A., Labopin M., Finke J., Ganser A., Stelljes M., Ehninger G., Beelen D., Niederwieser D., et al. Conditioning Intensity in Secondary AML with Prior Myelodysplastic Syndrome/Myeloproliferative Disorders: An EBMT ALWP Study. Blood Adv. 2018;2:2127–2135. doi: 10.1182/bloodadvances.2018019976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kroger N., Brand R., van Biezen A., Zander A., Dierlamm J., Niederwieser D., Devergie A., Ruutu T., Cornish J., Ljungman P., et al. Risk Factors for Therapy-Related Myelodysplastic Syndrome and Acute Myeloid Leukemia Treated with Allogeneic Stem Cell Transplantation. Haematologica. 2009;94:542–549. doi: 10.3324/haematol.2008.000927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lee C.J., Labopin M., Beelen D., Finke J., Blaise D., Ganser A., Itälä-Remes M., Chevallier P., Labussière-Wallet H., Maertens J., et al. Comparative Outcomes of Myeloablative and Reduced-intensity Conditioning Allogeneic Hematopoietic Cell Transplantation for Therapy-related Acute Myeloid Leukemia with Prior Solid Tumor: A Report from the Acute Leukemia Working Party of the European Society for Blood and Bone Marrow Transplantation. Am. J. Hematol. 2019;94:431–438. doi: 10.1002/ajh.25395. [DOI] [PubMed] [Google Scholar]
- 47.Metheny L., Callander N.S., Hall A.C., Zhang M.-J., Bo-Subait K., Wang H.-L., Agrawal V., Al-Homsi A.S., Assal A., Bacher U., et al. Allogeneic Transplantation to Treat Therapy-Related Myelodysplastic Syndrome and Acute Myelogenous Leukemia in Adults. Transplant. Cell Ther. 2021;27:923.e1–923.e12. doi: 10.1016/j.jtct.2021.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets analyzed during the current study are available from the corresponding author upon reasonable request.