This comparative effectiveness research study investigates if zone 1 endovascular balloon occlusion of the aorta (REBOA) is an effective alternative to resuscitative thoracotomy in patients with severe hemorrhagic shock.
Key Points
Question
Is zone 1 endovascular balloon occlusion of the aorta (REBOA) a safe and effective alternative to resuscitative thoracotomy (RT) in the resuscitation of patients with severe traumatic hemorrhagic shock?
Findings
After controlling for confounders through propensity score matching, this comparative effectiveness research study including 991 patients from 28 trauma centers in the 2013 to 2021 Aortic Occlusion for Resuscitation in Trauma and Acute Care Surgery registry found that patients subjected to a REBOA zone 1 aortic occlusion were significantly more likely to survive their hospitalization than similar patients undergoing AO via RT.
Meaning
Results suggest that REBOA zone 1 aortic occlusion is a safe and effective alternative to RT.
Abstract
Importance
Aortic occlusion (AO) is a lifesaving therapy for the treatment of severe traumatic hemorrhagic shock; however, there remains controversy whether AO should be accomplished via resuscitative thoracotomy (RT) or via endovascular balloon occlusion of the aorta (REBOA) in zone 1.
Objective
To compare outcomes of AO via RT vs REBOA zone 1.
Design, Setting, and Participants
This was a comparative effectiveness research study using a multicenter registry of postinjury AO from October 2013 to September 2021. AO via REBOA zone 1 (above celiac artery) was compared with RT performed in the emergency department of facilities experienced in both procedures and documented in the prospective multicenter Aortic Occlusion for Resuscitation in Trauma and Acute Care Surgery (AORTA) registry. Propensity score matching (PSM) with exact institution matching was used, in addition to subgroup multivariate analysis to control for confounders. The study setting included the ED, where AO via RT or REBOA was performed, and participants were adult trauma patients 16 years or older.
Exposures
AO via REBOA zone 1 vs RT.
Main Outcomes and Measures
The primary outcome was survival. Secondary outcomes were ventilation-free days (VFDs), intensive care unit (ICU)–free days, discharge Glasgow Coma Scale score, and Glasgow Outcome Score (GOS).
Results
A total of 991 patients (median [IQR] age, 32 [25-48] years; 808 male individuals [81.9%]) with a median (IQR) Injury Severity Score of 29 (18-50) were included. Of the total participants, 306 (30.9%) had AO via REBOA zone 1, and 685 (69.1%) had AO via RT. PSM selected 112 comparable patients (56 pairs). REBOA zone 1 was associated with a statistically significant lower mortality compared with RT (78.6% [44] vs 92.9% [52]; P = .03). There were no significant differences in VFD greater than 0 (REBOA, 18.5% [10] vs RT, 7.1% [4]; P = .07), ICU-free days greater than 0 (REBOA, 18.2% [10] vs RT, 7.1% [4]; P = .08), or discharge GOS of 5 or more (REBOA, 7.5% [4] vs RT, 3.6% [2]; P = .38). Multivariate analysis confirmed the survival benefit of REBOA zone 1 after adjustment for significant confounders (relative risk [RR], 1.25; 95% CI, 1.15-1.36). In all subgroup analyses (cardiopulmonary resuscitation on arrival, traumatic brain injury, chest injury, pelvic injury, blunt/penetrating mechanism, systolic blood pressure ≤60 mm Hg on AO initiation), REBOA zone 1 offered an either similar or superior survival.
Conclusions and Relevance
Results of this comparative effectiveness research suggest that REBOA zone 1 provided better or similar survival than RT for patients requiring AO postinjury. These findings provide the ethically necessary equipoise between these therapeutic approaches to allow the planning of a randomized controlled trial to establish the safety and effectiveness of REBOA zone 1 for AO in trauma resuscitation.
Introduction
Aortic occlusion (AO) is an integral part of the armamentarium for treating exsanguinating hemorrhage in the emergency department (ED). Its goal is to redistribute the limited circulating blood to cerebral and coronary perfusion and attenuate ongoing blood loss from subdiaphragmatic bleeding.1 Traditionally, it was performed via a resuscitative thoracotomy (RT) for penetrating cardiac wounds2 and later for massive hemoperitoneum to prevent cardiac decompensation prior to laparotomy.3 However, this aggressive procedure is associated with morbidity not only to the patient but also to the health care team.4 Blood-borne illnesses (HIV, hepatitis C) have historically been the primary concern; however, the COVID-19 pandemic added further risk.5,6,7
Resuscitative endovascular balloon occlusion of the aorta (REBOA) is an intraaortic balloon occlusion device placed percutaneously and advanced into the descending aorta to achieve AO. Both REBOA and RT aim at achieving temporary AO in patients in extremis due to hemorrhagic shock. Contemporary investigations on their comparative effectiveness and safety lack appropriate control groups or provide disparate results. Harfouche et al8 found a survival benefit of REBOA in a single-center study matching patients requiring REBOA to non-REBOA. However, the study excluded patients who arrived in cardiac arrest, when AO can be lifesaving, and the non-REBOA group was not necessarily treated with RT. Studies using the multicenter Japan Trauma Data Bank (2004-20119 and 2004-201610) found opposing results regarding the survival benefit from REBOA compared with non-REBOA using propensity score matching. Again, both studies used controls not necessarily treated with RT. A 2019 study comparing the outcomes of REBOA with non-REBOA in propensity score–matched patients in the 2015 to 2016 American College of Surgeons Trauma Quality Improvement Program US national data set,11 reported increased mortality with REBOA. However, the study specifically excluded patients treated with RT from their control group. Finally, a meta-analysis12,13,14,15 comparing AO via RT and via REBOA reported a survival benefit from REBOA; however, the analytic approach required a number of questionable assumptions.
In addition to unsuitable control groups, most studies lacked granular data on the physiologic status at AO and the injury patterns, 2 essential elements to determine the indication of open vs endovascular AO. Furthermore, recent data suggest that there are sizable differences in indications and outcomes of REBOA AO at zone 1 (above the celiac artery) vs zone 3 (below the renal arteries),16 which most prior investigations did not distinguish. The prospective multicenter (28 trauma centers) Aortic Occlusion for Resuscitation in Trauma and Acute Care Surgery (AORTA) registry, sponsored by the American Association for the Surgery of Trauma, was designed to supply granular physiologic and injury data, as well AO zone, allowing for more accurate assessments of the effectiveness of AO via RT vs REBOA.15 The preliminary report from the AORTA registry17 reviewed the first 285 patients and concluded that REBOA zone 1 was superior to RT, particularly in patients not requiring cardiopulmonary resuscitation (CPR). A more recent report of the AORTA registry focusing on traumatic brain injury (TBI) confirmed a survival benefit of REBOA zone 1 vs RT.18
We produced a contemporaneous report of the AORTA registry comparing AO via REBOA zone 1 vs RT in the overall group of patients undergoing either procedure and in predetermined subgroups. We also identified the prognostic indicators of each procedure. We hypothesized that AO via REBOA zone 1 would result in better outcomes than RT among patients who underwent AO in the ED for severe hemorrhagic shock.
Methods
Study Design
This was a multicenter, observational, comparative effectiveness research study using the prospective AORTA registry. All participating centers were required to have institutional review board approval prior to enrollment of patients into the AORTA registry. The study was conducted with a waiver of consent due to minimal risk. Patients admitted between October 2013 and September 2021 were eligible for this study. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines.
Study Population
Included in this study were adult trauma patients 16 years and older undergoing AO during resuscitation in the ED. We excluded patients transferred from other hospitals. Race and ethnicity data were not collected during this time period in the AORTA registry. Future data collection will incorporate this important descriptor. The study was limited to facilities with 10 or more cases of RT and 10 or more cases of REBOA zone 1 in the AORTA registry during the study period to capture hospitals with experience in both procedures.
Outcomes and Subgroups
The primary outcome was in-hospital survival. Secondary outcomes included ventilation-free days and intensive care unit (ICU)–free days (both out of 28 days), calculated as proposed by Schoenfeld et al,19 as well as Glasgow Coma Scale (GCS) and Glasgow Outcome Score (GOS) on discharge.
Several subgroups were defined to refine the indication of REBOA vs RT: TBI Head Abbreviated Injury Score (AIS; score ≥3), severe chest injury (AIS chest ≥3), severe isolated chest injury (AIS chest ≥3 and AIS of all other regions ≤2), penetrating severe chest injury (AIS chest ≥3), severe pelvic injury (AIS pelvis ≥3), blunt and penetrating mechanisms, and arrival CPR requirement.
Statistical Analysis
We conducted propensity score matching (PSM) on all variables deemed clinically relevant and/or significantly associated univariately with the procedures (greedy matching, maximum caliper 0.15), with exact matching on institution. The latter has been often neglected in previous PSM studies, yet it is essential to avoid comparing hospitals rather than AO types. When variables were highly collinear (|r|>0.35), one of them was chosen based on availability and reliability to be included in the model. Survival between matched groups was compared with Kaplan-Meier curves and tested with the log-rank and Wilcoxon tests, whereas comparisons of continuous outcomes were done via the Wilcoxon rank sum test, and comparisons of categorical outcomes were done via the χ2 test. To adjust for any confounding remaining after matching, a Cox proportional hazards model was used.
In addition, we performed a multivariate analysis using generalized estimating equations with robust SEs (to account for clustered data by hospital) to adjust the correlation of AO type (RT vs REBOA) with hospital mortality for potential confounders. Only statistically significant confounders were kept in these models. The significant independent predictors of death in each one of the AO modes were detected by a stepwise selection procedure in generalized estimating equation models with robust SEs.
All analyses were conducted in SAS, version 9.4 (SAS Institute). Stratification variables and outcomes had negligible missingness (<5%); for other variables, listwise deletion was applied, and tables report the proportion of the actual denominator. Continuous data are presented as median (IQR). All tests were 2-tailed with significance declared at P < .05.
Results
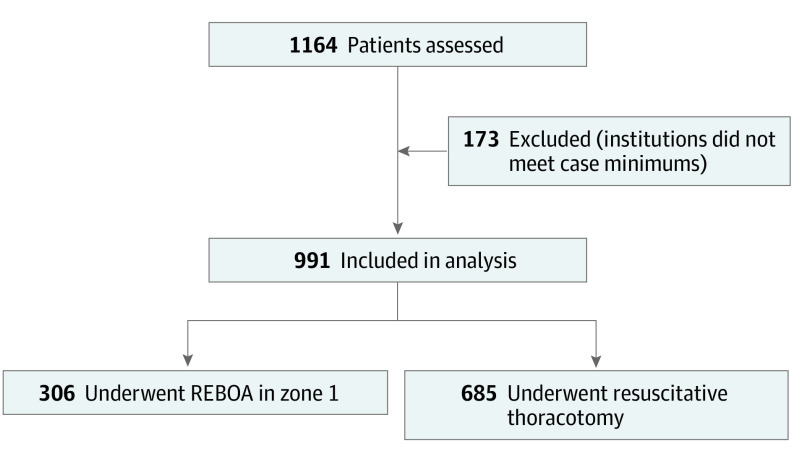
Figure 1 shows the flow diagram for study inclusion. Overall, of 1164 patients meeting inclusion criteria, 173 were removed due to the institution low procedure volume, leaving 991 patients (median [IQR] age, 32 [25-48] years; 808 male individuals [81.9%]; 183 female individuals [18.5%]) in the analytic data set, of whom 306 (30.9%) underwent RT, and 685 (69.1%) underwent REBOA zone 1. In the analytic data set, patients had a median (IQR) Injury Severity Score (ISS) of 29 (18-50). Table 1 depicts the patients characteristics and outcomes of the 2 groups. Overall, patients who underwent RT were more severely injured, had more physiologic derangement, and experienced worse outcomes than their REBOA zone 1 counterparts.
Figure 1. Flow Diagram for Patient Inclusion.
REBOA indicates resuscitative endovascular balloon occlusion of the aorta.
Table 1. Characteristics of the Population Studied.
| Characteristic | Median (IQR) or No. (%) | P value | ||
|---|---|---|---|---|
| Total (n = 991 [100%]) | REBOA zone 1 (n = 306 [30.9%]) | Resuscitative thoracotomy (n = 685 [69.1%]) | ||
| Facility’s annual patient volume, No. (%) | ||||
| 1000-2000 | 202 (20.4) | 11 (3.6) | 191 (27.9) | <.001 |
| >2000-3000 | 188 (19.0) | 21 (6.9) | 167 (24.4) | |
| >3000 | 601 (60.6) | 274 (89.5) | 327 (47.7) | |
| Age, y | 32.0 (25.0 to 48.0) | 40.0 (27.0 to 57.0) | 30.0 (24.0 to 42.0) | <.001 |
| Sex | ||||
| Male | 808 (81.5) | 238 (77.8) | 570 (83.2) | .03 |
| Female | 183 (18.5) | 68 (22.2) | 115 (16.8) | |
| BMIa | 25.8 (23.5 to 30.5) | 26.0 (23.7 to 30.4) | 25.8 (23.2 to 30.6) | .67 |
| Injury characteristics, No. (%) | ||||
| Blunt mechanism | 565 (57.1) | 64 (21.1) | 501 (73.1) | <.001 |
| Injury Severity Score | 29.0 (18.0 to 50.0) | 33.0 (21.0 to 43.0) | 26.0 (17.0 to 50.0) | .73 |
| Head/neck AIS | 0 (0 to 2.0) | 1.0 (0 to 4.0) | 0 (0 to 0) | <.001 |
| Traumatic brain injury | 211 (21.3) | 118 (38.6) | 93 (13.6) | <.001 |
| Chest AIS | 3.0 (0 to 4.0) | 3.0 (0 to 4.0) | 3.0 (0 to 5.0) | .001 |
| Severe chest injury | 577 (58.2) | 174 (56.9) | 403 (58.8) | .56 |
| Abdomen AIS | 0 (0 to 3.0) | 2.0 (0 to 4.0) | 0 (0 to 2.0) | <.001 |
| Severe abdomen injury | 315 (31.8) | 149 (48.7) | 166 (24.2) | <.001 |
| Pelvic AIS | 0 | 0 | 0 | .97 |
| Severe pelvic injury | 14 (1.4) | 5 (1.6) | 9 (1.3) | .69 |
| Extremity AIS | 0 | 0 (0 to 0) | 0 (0 to 0) | <.001 |
| Severe extremity injury | 56 (5.7) | 8 (2.6) | 48 (7.0) | .01 |
| Prehospital | ||||
| SBP, mm Hg | 76.0 (0 to 111.5) | 96.0 (62.0 to 129.0) | 40.0 (0 to 92.0) | <.001 |
| Heart rate, beats/min | 86.0 (22.0 to 120.0) | 100.0 (69.0 to 128.0) | 68.0 (0 to 110.0) | <.001 |
| Shock index | 0.8 (0 to 1.4) | 0.9 (0.6 to 1.3) | 0.8 (0 to 1.5) | .06 |
| GCS | 3.0 (3.0 to 10.0) | 3.0 (3.0 to 12.0) | 3.0 (3.0 to 8.0) | <.001 |
| CPR, No. (%) | 443 (45.4) | 97 (31.8) | 346 (51.6) | <.001 |
| Minutes from injury to hospital | 30.0 (20.0 to 53.0) | 43.0 (28.0 to 65.0) | 24.0 (16.0 to 40.0) | <.001 |
| Hospital admission | ||||
| SBP, mm Hg | 0 (0 to 83.5) | 77.0 (0 to 107.0) | 0 (0 to 56.0) | <.001 |
| Heart rate, beats/min | 0 (0 to 106.0) | 99.0 (24.0 to 129.0) | 0 (0 to 69.5) | <.001 |
| Shock index | 0 (0 to 1.2) | 1.0 (0.2 to 1.6) | 0 (0 to 0.7) | <.001 |
| GCS | 3.0 (3.0 to 3.0) | 3.0 (3.0 to 7.0) | 3.0 (3.0 to 3.0) | <.001 |
| CPR, No. (%) | 449 (45.4) | 94 (30.7) | 355 (51.9) | <.001 |
| CPR duration, No. (%) | ||||
| 60 min or more | 16 (1.7) | 6 (2.0) | 10 (1.5) | <.001 |
| <60 min | 387 (41.0) | 79 (26.6) | 308 (47.6) | |
| Not applicable | 541 (57.3) | 212 (71.4) | 329 (50.9) | |
| Laboratory tests | ||||
| Hemoglobin, g/dL | 11.0 (9.2 to 12.5) | 11.0 (9.4 to 12.3) | 11.0 (8.9 to 12.6) | .82 |
| Prothrombin INR | 1.6 (1.3 to 2.2) | 1.6 (1.2 to 2.0) | 1.7 (1.3 to 2.4) | .04 |
| Base excess, mEq/L | −14.0 (−20.0 to −8.0) | −11.5 (−16.0 to −8.0) | −16.0 (−23.0 to −9.5) | <.001 |
| Lactate, mmol/L | 9.3 (6.0 to 14.3) | 8.3 (4.9 to 12.1) | 11.3 (7.2 to 15.2) | <.001 |
| AO characteristics, No. (%) | ||||
| CPR during AO | 507 (51.7) | 114 (37.5) | 393 (58.1) | <.001 |
| AO initial SBP, mm Hg | 0 (0 to 40.0) | 53.0 (0 to 70.0) | 0 | <.001 |
| AO initial SBP ≤60 mm Hg | 154 (17.3) | 116 (41.0) | 38 (6.3) | <.001 |
| AO initial GCS | 3.0 (3.0 to 3.0) | 3.0 (3.0 to 3.0) | 3.0 (3.0 to 3.0) | <.001 |
| AO performer = trauma surgeon | 706 (72.5) | 239 (81.3) | 467 (68.7) | <.001 |
| Hemodynamic improvement | 440 (45.1) | 220 (72.6) | 220 (32.7) | <.001 |
| Hemodynamic stabilityb | 256 (26.4) | 108 (16.1) | 148 (49.2) | <.001 |
| SBP after first AO, mm Hg | 0 (0 to 107.0) | 105.0 (71.5 to 126.0) | 0 (0 to 51.5) | <.001 |
| GCS after first AO | 3.0 (3.0 to 3.0) | 3.0 (3.0 to 3.0) | 3.0 (3.0 to 3.0) | <.001 |
| First AO duration, min | 20.0 (9.0 to 48.0) | 30.0 (12.0 to 70.0) | 15.0 (8.0 to 36.0) | <.001 |
| Second AO needed | 51 (6.0) | 17 (6.0) | 34 (6.1) | .99 |
| Second AO type | ||||
| Endovascular | 28 (54.9) | 9 (52.9) | 19 (55.9) | .84 |
| Open | 23 (45.1) | 8 (47.1) | 15 (44.1) | |
| Minutes to start first AO | 5.0 (2.0 to 13.0) | 14.0 (7.0 to 23.0) | 3.0 (2.0 to 7.0) | <.001 |
| Minutes to first successful AO | 11.0 (6.0 to 20.0) | 20.0 (13.0 to 31.0) | 7.0 (5.0 to 12.0) | <.001 |
| Transfusions, fluids, inotropes, and TXA in first 24 h | ||||
| Red blood cell units | 6.0 (3.0 to 17.0) | 12.0 (4.0 to 26.0) | 5.0 (2.0 to 12.0) | <.001 |
| Plasma units | 4.0 (2.0 to 13.0) | 8.0 (3.0 to 21.0) | 3.0 (1.0 to 8.0) | <.001 |
| Platelets units | 1.0 (0 to 3.0) | 2.0 (0 to 5.0) | 0 (0 to 3.0) | <.001 |
| Cryoprecipitate units | 0 (0) | 0 (0 to 1.0) | 0 (0 to 0.0) | .001 |
| TXA, No. (%) | 221 (28.5) | 93 (34.3) | 128 (25.4) | .01 |
| Complications and outcomes, No. (%) | ||||
| Acute kidney injury | 70 (7.1) | 48 (15.7) | 22 (3.2) | <.001 |
| Acute lung injury | 50 (5.0) | 24 (7.8) | 26 (3.8) | .01 |
| Multiple organ failure | 28 (2.8) | 18 (5.9) | 10 (1.5) | <.001 |
| Pneumonia | 40 (4.0) | 22 (7.2) | 18 (2.6) | <.001 |
| Sepsis | 37 (3.7) | 31 (10.1) | 6 (0.9) | <.001 |
| Stroke | 7 (0.7) | 3 (1.0) | 4 (0.6) | .49 |
| Spinal ischemia with neurodeficit | 3 (0.3) | 2 (0.7) | 1 (0.1) | .18 |
| Vascular reconstruction | 27 (8.8) | 27 (10.1) | 0 | .03 |
| Extremity ischemia | 11 (1.1) | 10 (3.3) | 1 (0.1) | <.001 |
| Amputation | 4 (0.4) | 4 (1.3) | 0 | .01 |
| Ventilation days | 1.0 (0 to 1.0) | 1.0 (1.0 to 4.0) | 1.0 (0 to 1.0) | <.001 |
| VFD | 0 (0) | 0 (0 to 0.5) | 0 (0 to 0.0) | <.001 |
| VFD >0 | 100 (10.2) | 76 (25.0) | 24 (3.5) | <.001 |
| ICU days | 0 (0 to 1.0) | 1.0 (0 to 5.0) | 0 (0) | <.001 |
| ICU-free days | 0 (0 to 0.0) | 0 (0 to 0.0) | 0 (0) | <.001 |
| ICU-free days >0 | 99 (10.0) | 74 (24.3) | 25 (3.7) | <.001 |
| Discharge GCS (survivors only) | 15.0 (15.0 to 15.0) | 15.0 (15.0 to 15.0) | 15.0 (15.0 to 15.0) | .16 |
| Discharge GCS = 15 (survivors only) | 87 (84.5) | 68 (87.2) | 19 (76.0) | .18 |
| Discharge GOS | 1.0 (1.0 to 1.0) | 1.0 (1.0 to 1.0) | 1.0 (1.0 to 1.0) | <.001 |
| Discharge GOS ≥5 | 29 (3.1) | 22 (8.3) | 7 (1.0) | <.001 |
| Discharge disposition | ||||
| Home | 55 (5.5) | 36 (11.8) | 19 (2.8) | <.001 |
| Mortality | 869 (87.7) | 218 (71.2) | 651 (95.0) | |
| Rehabilitation/nursing facility | 67 (6.8) | 52 (17.0) | 15 (2.2) | |
| Death | 870 (87.8) | 218 (71.2) | 652 (95.2) | <.001 |
| Death location | ||||
| ED | 504 (57.9) | 83 (38.1) | 421 (64.6) | <.001 |
| ICU | 161 (18.5) | 86 (39.4) | 75 (11.5) | |
| Interventional radiology | 3 (0.3) | 2 (0.9) | 1 (0.2) | |
| Operating room | 201 (23.1) | 47 (21.6) | 154 (23.6) | |
Abbreviations: AIS, abbreviated injury score; AO, aortic occlusion; AORTA, Aortic Occlusion for Resuscitation in Trauma and Acute Care Surgery; BMI, body mass index; CPR, cardiopulmonary resuscitation; ED, emergency department; GCS, Glasgow Coma Scale; GOS, Glasgow Outcome Score; ICU, intensive care unit; INR, international normalized ratio; SBP, systolic blood pressure; TXA, tranexamic acid; VFD, ventilation-free days.
SI conversion factor: To convert hemoglobin from gram per deciliter to gram per liter, multiply by 10; to convert base excess from milliequivalent per liter to millimole per liter, multiply by 1; to convert lactate from millimole per liter to milligram per deciliter, divide by 0.111.
Calculated as weight in kilograms divided by height in meters squared.
Defined for the purposes of the AORTA registry systolic blood pressure consistently greater than 90 mm Hg for at least 5 minutes after AO.
PSM Analysis in the Overall Group
PSM controlled for the following variables: institution (exact matching) and age, sex, ISS, injury mechanism, TBI, severe chest injury, severe abdominal injury, severe pelvic injury, severe extremities injury, prehospital CPR, admission systolic blood pressure (SBP), admission GCS, CPR on arrival, CPR during AO, initial AO SBP of 60 mm Hg or less, AO initial GCS, and procedure performer (trauma surgeon vs others). PSM selected 112 patients (56 pairs) and substantially reduced the differences between groups (Table 2). Balance diagnostics included the standardized mean difference (SMD), which was below 20.0 for all variables, except for injury mechanism, which remained relatively unbalanced with an SMD of 0.23. Other balance diagnostics are available in supplemental digital content (eFigure in the Supplement).
Table 2. Characteristics of Propensity Score–Matched Patients.
| Characteristic | Median (IQR) | P value | SMDa | ||
|---|---|---|---|---|---|
| Total (n = 112) | REBOA zone 1 (n = 56) | Resuscitative thoracotomy (n = 56) | |||
| Facility annual patient volume, No. (%) | |||||
| 1000-2000 | 8 (7.1) | 4 (7.1) | 4 (7.1) | <.99 | 0 |
| >2000-3000 | 12 (10.7) | 6 (10.7) | 6 (10.7) | 0 | |
| >3000 | 92 (82.1) | 46 (82.1) | 46 (82.1) | 0 | |
| Age, y | 37.5 (27.0 to 52.5) | 40.0 (27.0 to 57.0) | 35.5 (26.5 to 51.5) | .42 | 2.0 |
| Male sex | 87 (77.7) | 44 (78.6) | 43 (76.8) | .82 | 4.3 |
| BMIb | 26.0 (24.2 to 30.0) | 26.1 (24.3 to 30.4) | 25.9 (24.1 to 29.3) | .65 | −0.4 |
| Injury characteristics, No. (%) | |||||
| Blunt mechanism | 76 (67.9) | 41 (73.2) | 35 (62.5) | .22 | 23.1 |
| Injury Severity Score | 29.0 (17.5 to 41.0) | 28.0 (19.5 to 39.5) | 30.0 (17.5 to 41.0) | <.99 | 0 |
| Head AIS | 0 (0 to 3.0) | 0 (0 to 3.0) | 0 (0 to 3.0) | .91 | 0 |
| Traumatic brain injury | 37 (33.0) | 18 (32.1) | 19 (33.9) | .84 | 3.8 |
| Chest AIS | 3.0 (0 to 4.0) | 3.0 (0 to 4.0) | 3.0 (0 to 4.0) | .90 | 0 |
| Severe chest injury | 65 (58.0) | 34 (60.7) | 31 (55.4) | .57 | 10.8 |
| Abdomen AIS | 2.5 (0 to 4.0) | 2.0 (0 to 4.0) | 3.0 (0 to 4.0) | .67 | 0 |
| Severe abdomen injury | 56 (50.0) | 27 (48.2) | 29 (51.8) | .71 | 7.2 |
| Pelvis AIS | 0 | 0 | 0 | .70 | 0 |
| Severe pelvic injury | 2 (1.8) | 1 (1.8) | 1 (1.8) | <.99 | 0 |
| Extremity AIS | 0 | 0 | 0 | .78 | 0 |
| Severe extremity injury | 7 (6.3) | 3 (5.4) | 4 (7.1) | .70 | 7.0 |
| Prehospital | |||||
| SBP, mm Hg | 82.0 (0 to 128.0) | 86.0 (27.0 to 132.0) | 80.0 (0 to 110.0) | .35 | −7.0 |
| Heart rate, beats/min | 96.5 (70.0 to 130.0) | 95.0 (68.0 to 137.0) | 96.5 (72.0 to 121.0) | .66 | −3.0 |
| GCS | 3.0 (3.0 to 10.0) | 3.5 (3.0 to 10.5) | 3.0 (3.0 to 9.0) | .24 | 0 |
| CPR, No. (%) | 37 (33.0) | 18 (32.1) | 19 (33.9) | .84 | 3.8 |
| Minutes from injury to ED | 48.0 (28.0 to 70.0) | 50.0 (28.0 to 75.0) | 46.0 (27.0 to 65.0) | .52 | −3.0 |
| Hospital admission | |||||
| SBP, mm Hg | 66.5 (0 to 105.0) | 61.0 (0 to 105.5) | 69.0 (0 to 101.5) | .98 | 0 |
| Heart rate, beats/min | 88.0 (0 to 114.0) | 95.0 (0 to 123.5) | 82.0 (0 to 105.0) | .19 | −7.0 |
| GCS | 3.0 (3.0 to 3.0) | 3.0 (3.0 to 3.0) | 3.0 (3.0 to 3.0) | .75 | 0 |
| CPR, No. (%) | 38 (33.9) | 19 (33.9) | 19 (33.9) | <.99 | 0 |
| CPR duration <60 min, No. (%) | 29 (27.9) | 16 (30.2) | 13 (25.5) | .53 | 10.5 |
| Hospital admission laboratory tests | |||||
| Hemoglobin, g/dL | 11.2 (8.9 to 12.8) | 11.8 (9.0 to 13.1) | 10.7 (8.4 to 12.6) | .26 | −0.8 |
| Prothrombin INR | 1.6 (1.4 to 2.2) | 1.6 (1.4 to 2.2) | 1.6 (1.4 to 2.1) | .78 | 0 |
| Base deficit, mEq/L | −12.0 (−20.0 to −9.0) | −12.0 (−16.0 to −8.0) | −12.5 (−24.0 to −10.0) | .20 | −3.0 |
| AO characteristics, No. (%) | |||||
| CPR during AO | 62 (55.4) | 31 (55.4) | 31 (55.4) | <.99 | 0 |
| AO initial SBP, mm Hg | 0 (0 to 51.0) | 0 (0 to 53.5) | 0 | .05 | 0 |
| AO initial SBP <60 mm Hg | 19 (17.0) | 8 (14.3) | 11 (19.6) | .45 | 14.2 |
| AO initial GCS | 3.0 (3.0 to 3.0) | 3.0 (3.0 to 3.0) | 3.0 (3.0 to 3.0) | <.99 | 0 |
| AO performer = trauma surgeon | 84 (75.0) | 40 (71.4) | 44 (78.6) | .38 | 16.7 |
| Hemodynamic improvement | 67 (59.8) | 38 (67.9) | 29 (51.8) | .08 | 33.3 |
| Hemodynamic stabilityc | 37 (33.0) | 22 (39.3) | 15 (26.8) | .16 | 26.8 |
| SBP post first AO, mm Hg | 64.0 (0 to 110.0) | 90.0 (0.0 to 115.0) | 0 (0 to 98.0) | .02 | −20.0 |
| GCS post first AO | 3.0 (3.0 to 3.0) | 3.0 (3.0 to 3.0) | 3.0 (3.0 to 3.0) | .34 | 0 |
| First AO duration, min | 26.0 (11.0 to 45.0) | 28.0 (11.0 to 41.0) | 20.0 (11.0 to 45.0) | .68 | −1.5 |
| Second AO needed | 8 (7.7) | 4 (7.7) | 4 (7.7) | <.99 | 0 |
| Second AO type | |||||
| Endovascular | 5 (62.5) | 2 (50.0) | 3 (75.0) | .47 | 53.5 |
| Open | 3 (37.5) | 2 (50.0) | 1 (25.0) | 53.5 | |
| Minutes to start first AO | 11.0 (4.0 to 21.0) | 14.0 (6.0 to 24.0) | 8.0 (4.0 to 16.0) | .01 | 5.0 |
| Minutes to successful first AO | 17.0 (11.0 to 26.0) | 21.0 (13.5 to 30.0) | 12.0 (8.0 to 19.0) | <.001 | −8.0 |
| Transfusions, fluids, inotropes, and TXA in the first 24 h | |||||
| Red blood cell units | 9.0 (4.0 to 22.5) | 9.5 (4.0 to 23.0) | 8.5 (4.0 to 22.0) | .89 | 0 |
| Plasma units | 6.0 (2.0 to 18.0) | 5.0 (3.0 to 19.0) | 6.0 (2.0 to 17.5) | .99 | 0 |
| Platelets units | 1.0 (0 to 5.0) | 1.0 (0.0 to 3.5) | 1.0 (0 to 6.0) | .31 | 0 |
| Cryoprecipitate units | 0 | 0 | 0 | .42 | 0 |
| TXA, No. (%) | 25 (24.0) | 13 (25.5) | 12 (22.6) | .73 | 6.8 |
| Complications and outcomes, No. (%) | |||||
| Acute kidney injury | 11 (9.8) | 6 (10.7) | 5 (8.9) | .75 | 6.1 |
| Acute lung injury | 7 (6.3) | 3 (5.4) | 4 (7.1) | .70 | 7.0 |
| Pneumonia | 6 (5.4) | 3 (5.4) | 3 (5.4) | <.99 | 0 |
| Sepsis | 4 (3.6) | 3 (5.4) | 1 (1.8) | .31 | 19.4 |
| Stroke | 2 (1.8) | 0 | 2 (3.6) | .15 | 346.0 |
| Multiple organ failure | 2 (1.8) | 1 (1.8) | 1 (1.8) | <.99 | 0 |
| Spinal ischemia with neurodeficit | 0 | 0 | 0 | NA | 0 |
| Extremity ischemia | 1 (0.9) | 1 (1.8) | 0 | .32 | 380.1 |
| Amputation | 0 | 0 | 0 | NA | 0 |
| Ventilation days | 1.0 (0 to 1.0) | 1.0 (1.0 to 2.0) | 1.0 (0 to 1.0) | .14 | 0 |
| VFD | 0 (0 to 0.0) | 0 | 0 | .07 | 0 |
| VFD >0 | 14 (12.7) | 10 (18.5) | 4 (7.1) | .07 | 34.6 |
| ICU days | 0 (0 to 1.5) | 1.0 (0 to 3.0) | 0 (0 to 1.0) | .01 | 0 |
| ICU-free days | 0 | 0 | 0 | .07 | 0 |
| ICU-free days >0 | 14 (12.6) | 10 (18.2) | 4 (7.1) | .08 | 33.9 |
| Discharge GCS (survivors only) | 15.0 (15.0 to 15.0) | 15.0 (15.0 to 15.0) | 15.0 (13.0 to 15.0) | .92 | 0 |
| Discharge GCS = 15 (survivors only) | 3 (21.4) | 2 (20.0) | 1 (25.0) | .84 | 12.0 |
| Discharge GOS | 1.0 (1.0 to 1.0) | 1.0 (1.0 to 1.0) | 1.0 (1.0 to 1.0) | .29 | 0 |
| Discharge GOS ≥5 | 6 (5.6) | 4 (7.5) | 2 (3.6) | .38 | 17.1 |
| Discharge disposition | |||||
| Home | 9 (8.0) | 7 (12.5) | 2 (3.6) | .09 | 33.2 |
| Mortality | 96 (85.7) | 44 (78.6) | 52 (92.9) | 41.8 | |
| Rehab/nursing facility | 7 (6.3) | 5 (8.9) | 2 (3.6) | 22.0 | |
| Death | 96 (85.7) | 44 (78.6) | 52 (92.9) | .03 | 41.8 |
| Survival hours | 2.0 (1.0 to 48.0) | 6.0 (1.0 to 288.0) | 1.8 (1.0 to 4.0) | .02 | 1.0 |
| Death location | |||||
| NA | 16 (14.3) | 12 (21.4) | 4 (7.1) | .05 | 41.8 |
| Emergency department | 42 (43.8) | 21 (47.7) | 21 (40.4) | 14.7 | |
| ICU | 24 (25.0) | 15 (34.1) | 9 (17.3) | 39.2 | |
| Operating room | 29 (30.2) | 8 (18.2) | 21 (40.4) | 50.3 | |
Abbreviations: AIS, abbreviated injury score; AO, aortic occlusion; AORTA, Aortic Occlusion for Resuscitation in Trauma and Acute Care Surgery; BMI, body mass index; CPR, cardiopulmonary resuscitation; ED, emergency department; GCS, Glasgow Coma Scale; GOS, Glasgow Outcome Score; ICU, intensive care unit; INR, international normalized ratio; SBP, systolic blood pressure; SMD, standardized mean difference; TXA, tranexamic acid; VFD, ventilation-free days.
SI conversion factor: To convert hemoglobin from gram per deciliter to gram per liter, multiply by 10; to convert base excess from milliequivalent per liter to millimole per liter, multiply by 1; to convert lactate from millimole per liter to milligram per deciliter, divide by 0.111.
SMD ideal less than 0.20 for confounders.
Calculated as weight in kilograms divided by height in meters squared.
Defined for the purposes of the AORTA registry as systolic blood pressure consistently greater than 90 mm Hg for at least 5 minutes after AO.
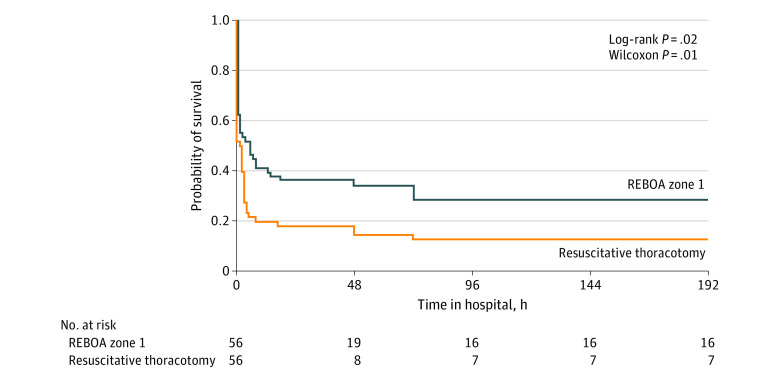
All matched patients were treated in level I trauma centers. REBOA zone 1 was associated with significantly lower mortality than RT (78.6% [44] vs 92.9% [52]; log-rank P = .02; Wilcoxon tests, P = .01; Cox proportional hazards model, P = .03) (Figure 2). A Cox proportional hazards model adjusting for blunt/penetrating mechanism was performed because mechanism of injury remained relatively unbalanced between matched groups. The significant survival benefit for REBOA zone 1 remained. Most deaths in the REBOA zone 1 group occurred in the ED, followed by the ICU, whereas patients who underwent RT were equally likely to die in the ED or in the operating room, with a minority (17.3% [9 of 56]) dying in the ICU. There were no significant differences in ventilator-free days greater than 0 (REBOA, 18.5% [10] vs RT, 7.1% [4]; P = .07), ICU-free days greater than 0 (REBOA, 18.2% [10] vs RT, 7.1% [4]; P = .08), or discharge GOS of 5 or more (REBOA, 7.5% [4] vs RT, 3.6% [2]; P = .38). REBOA zone 1 resulted in more ventilator-free days and ICU-free days, although these differences were not significant. There were no statistically significant differences in discharge GOS or GCS (the latter only in survivors). Complications following AO for both procedures are shown in Table 2. It should be noted that all complications are subject to survivor bias, thus they were more likely in the group with the longest survival.
Figure 2. Survival Curves for Propensity Score–Matched Patients (n = 112).
Resuscitative endovascular balloon occlusion of the aorta (REBOA) aortic occlusion had a significantly higher patient survival than aortic occlusion via resuscitative thoracotomy.
Matched and unmatched patients had similar demographic characteristics (albeit matched patients were slightly older), ISS, and SBP at AO initiation as well as acid-base and coagulation status on hospital arrival (eTable in the Supplement). However, compared with unmatched patients, the matched group was more likely to be treated in high-volume centers, to have had blunt injuries resulting in less physiologic derangement and requirement for CPR, and survived longer transportation times from injury to ED (eTable in the Supplement). The outcomes were very similar between the matched and unmatched groups.
Multivariate Analysis
After adjustment for statistically significant confounders (TBI, severe chest injury, severe pelvic injury, admission GCS, CPR on arrival, AO initial GCS), RT was associated with significantly higher mortality than REBOA zone 1 (adjusted relative risk [aRR], 1.25; 95% CI, 95% CI, 1.15-1.36) in the overall study sample (Table 3). Subgroup confounder-adjusted analyses (Table 3) showed higher mortality associated with RT compared with REBOA zone 1 in all stratified analyses, reaching statistical significance in both blunt and penetrating injuries, as well as in other subgroups, including patients not requiring CPR on arrival and without severe TBI, as well as in those with severe chest injury (isolated or in combination with other injuries, regardless of blunt or penetrating mechanism). There were very few patients with pelvic injuries thus precluding a meaningful analysis, but a statistically significant survival benefit was detected among patients without severe pelvic trauma. Patients with SBP of 60 mm Hg or less benefited significantly from REBOA zone 1 compared with those subjected to RT.
Table 3. Multivariate Analysis for Outcome Death for the Overall Study Sample and for Prespecified Subgroupsa.
| Outcome | No. | Adjusted relative risk (95% CI) | P value | |
|---|---|---|---|---|
| RT | REBOA zone 1 | |||
| Overall sample | 685 | 306 | 1.25 (1.15-1.36) | <.001 |
| Required CPR on arrival | ||||
| Yes | 355 | 94 | 1.05 (0.80-1.37) | .72 |
| No | 329 | 212 | 1.43 (1.22-1.68) | <.001 |
| Traumatic brain injury | ||||
| Yes | 93 | 118 | 1.04 (0.98-1.10) | .19 |
| No | 592 | 188 | 1.35 (1.11-1.64) | .003 |
| Chest injury | ||||
| Severe | 403 | 174 | 1.30 (1.16-1.45) | <.001 |
| Penetrating | 289 | 19 | 1.49 (1.16-1.91) | .002 |
| Isolated severe | 234 | 38 | 1.34 (1.01-1.77) | .04 |
| No severe | 282 | 132 | 1.14 (0.86-1.52) | .37 |
| Pelvic injury | ||||
| Severe | 5 | 9 | NA | |
| No severe | 676 | 301 | 1.24 (1.11-1.38) | <.001 |
| Mechanism | ||||
| Blunt | 184 | 240 | 1.22 (1.11-1.34) | <.001 |
| Penetrating | 501 | 64 | 1.36 (1.25-1.47) | <.001 |
| AO initial SBP, mm Hg | ||||
| >60 | 38 | 116 | 1.44 (0.92-2.27) | .11 |
| ≤60 | 570 | 167 | 1.18 (1.07-1.31) | .001 |
Abbreviations: CPR, cardiopulmonary resuscitation; NA, not applicable; REBOA, resuscitative endovascular balloon occlusion of the aorta; RT, resuscitative thoracotomy.
All multivariate models adjusted for significant confounders unless confounder was the stratification variable (traumatic brain injury, severe chest injury, severe pelvic injury, admission Glasgow Coma Scale, CPR on arrival, aortic occlusion initial Glasgow Coma Scale).
Prognostic Indicators in REBOA Zone 1 and RT AO
Significant independent predictors of death in REBOA zone 1 AO were as follows: TBI (aRR, 1.20; 95% CI, 1.01-1.43), admission GCS (aRR, 0.95; 95% CI, 0.91-0.98), CPR on arrival (aRR, 1.16; 95% CI, 1.04-1.30), CPR during AO (aRR, 1.23; 95% CI, 1.13-1.33), and AO initial GCS (aRR, 0.89; 95% CI, 0.83-0.96). The only significant predictor of death in RT AO was prehospital CPR (aRR, 1.07; 95% CI, 1.05-1.09).
Discussion
Results of this contemporaneous comparative effectiveness research study of the multicenter AORTA registry suggest that AO with REBOA zone 1 resulted in overall better survival compared with RT. This survival benefit was observed in all subgroups, reaching significance in several of them. More importantly, in none of the stratified analyses was REBOA zone 1 AO significantly inferior to RT. This included the subgroup with penetrating chest injuries, traditionally considered a REBOA contraindication.
The current study is in line with other recent studies reporting a survival benefit of ED REBOA over ED RT in the US as well as in other countries.8,9,10,12,14,17,18,20,21 A recent meta-analysis22 observed a similar benefit. These are in contrast with the US study by Joseph at al11 and 2 studies using the Japan Trauma Data Bank,9,23 which found REBOA to be associated with higher mortality. However, the former specifically excluded patients undergoing RT, which would be the alternative therapeutic approach for these patients. The latter did not specify what were the therapies used in the comparison group, and Inoue et al23 excluded patients requiring CPR on arrival, among whom AO can be a lifesaving procedure. We believe these choices of comparison groups and sampling strategies have hindered the assessment of the effectiveness of AO by REBOA. Our study advances the knowledge brought by these latter studies for several reasons: (1) it used a more contemporary data set; (2) the AORTA registry was developed specifically to assess the outcomes of AO modalities and contains the required data granularity to do so, as opposed to data sets/registries developed for nonspecific quality improvement purposes; (3) our comparison group was the current alternative AO approach (as opposed to the patients who did not require AO); (4) our study specifically compared REBOA zone 1 AO (ie, excluding zones 2 and 3), an information that is missing in most data sets; and (5) our sample included patients requiring CPR on arrival, for whom AO can be lifesaving. In addition, our study is, to our knowledge, the only one to require exact matching on institution, an essential step to avoid comparing different institutions as opposed to different procedures, especially when the indication of either treatment varies widely by institution.
There are several potential benefits that may explain the improved survival with REBOA over RT. After traumatic circulatory arrest, CPR is critical to the return of spontaneous circulation. Teeter et al24 demonstrated that the total duration of interruptions of cardiac compressions was shorter for REBOA vs RT, before and during resuscitation with AO. The same group showed that REBOA patients who underwent closed chest compression had a higher rate of return of spontaneous circulation and higher end-tidal carbon dioxide than patients who underwent RT with open cardiac massage.25 The availability of partial REBOA inflation may mitigate the detrimental effects of complete aortic occlusion such as supraphysiologic proximal pressure, increased cardiac afterload, and distal visceral ischemia.26,27 In patients who attain return of spontaneous circulation, the ability to incrementally decrease balloon volume in REBOA may also allow for safer and more controlled restoration of aortic blood flow.
REBOA has complications with arterial access (eg, pseudoaneurysm) and ischemia-reperfusion complications (eg, arterial thromboses, lower extremity amputation, and kidney failure).28,29 The assessment of post-AO complications are subject to survivor bias, and although competing risk analytic methods can minimize this effect, they do not eliminate it. Only through randomized clinical trials (RCTs) would a more definitive assessment of the complications of REBOA compared with RT be possible.
From a health care professional standpoint, RT is a high-risk procedure. Use of scalpels and studded Finochietto retractors in an emergency setting, can result in percutaneous injury to the performer.30 A prospective multiinstitutional study found a 7.2% exposure rate per RT and 1.6% per RT participant.4 Given the elevated rates of HIV (4.3%) and HCV (14%) in trauma patients,4 the exposure from RT may have significant health consequences to the health care team.
Although our findings pertain primarily to civilian trauma, they support recommendations for the use of REBOA in military settings, especially in austere environments where RT is not a viable alternative. Several studies assessed REBOA in combat settings, albeit with limited sample sizes (<20).31 The 2020 Joint Trauma System REBOA practice guideline acknowledges the successful use of REBOA in austere military locations, especially for triage of multiple casualties.32,33,34
Limitations
Our study has limitations. The propensity score matching excluded a large proportion of the individuals, indicating the 2 procedures are indicated for substantially different types of injury patterns and limiting the conclusions about the comparative effectiveness and safety of the 2 AO procedures. Overall matched patients presented with less severe physiologic derangement than unmatched patients, thus suggesting that matching did not select a representative sample. Multivariate analyses in the overall sample and in each analyzed subgroup, however, confirmed the results of the matched group. Moreover, the subgroup analyses showed that REBOA zone 1 consistently resulted in similar or superior outcomes than RT. We were limited in the assessment of post-AO complications as they were subject to survivor bias. Because the AORTA registry (as most of the current trauma data sets) does not yet include the date of the complication, the appropriate analytic approach (competing risk analysis) was not possible. Although this is a prospective registry, we anticipate that at least some of the data may not be obtained in real time, thus potentially subject to recall bias. Finally, our findings were generated in US institutions with ample experience with both REBOA placement and RT; thus, their generalizability is limited to centers with similar skills set and trauma care systems. For example, in US level I trauma centers, trauma surgeons take call in-house, whereas in other health care systems, trauma surgeons may not be immediately available.
Overall, these limitations do not preclude the conclusion that equipoise was sufficiently established, thus permitting an RCT. Such an RCT will require the coordination of multiple trauma centers, appropriate training of all REBOA operators, and standardization of several processes and procedures (both within and between institutions). Given the severity of the eligible cases, this will need to be conducted as emergency research with a waiver of consent. Randomization may require alternative methods, such as the system used by the Denver group in testing the effectiveness of goal-directed hemostatic resuscitation (ie, alternate weeks for each study group).35 Such a trial would be labor intensive, costly, and long lasting to accrue the sample size necessary to allow stratifications by injury pattern with adequate statistical power. We recognize, therefore, that the likelihood of such a trial is not high, given its magnitude and current competing interests and conditions (eg, COVID-19 pandemic, monkeypox public health emergency, climatic changes). Thus, we believe our study, given its rigor in data collection, sampling strategy and statistical analysis, contributes to what has been labeled focused empiricism, ie, using the best data available to make incremental changes until more powerful study designs can be conducted.36,37
Conclusions
Results of this comparative effectiveness research study suggest that overall and in all subgroups of injury and physiologic patterns, REBOA was associated with a similar or better survival benefit compared with RT. These findings suggest that in critically injured patients requiring AO due to severe hemorrhagic shock who are admitted to trauma systems with immediate availability of skilled, experienced trauma surgeons, REBOA may be an effective alternative to RT. In addition, the collective body of evidence justifies the ethical requirement of equipoise for the planning of an RCT to provide more definitive answers, while contributing to the current body of knowledge regarding emergency aortic occlusion for severe traumatic hemorrhage.
eFigure. Propensity Score Matching Balance Diagnostics
eTable. Comparison Between Unmatched and Matched Patients (by Propensity Score Matching)
Nonauthor Collaborators
References
- 1.Qasim ZA, Sikorski RA. Physiologic considerations in trauma patients undergoing resuscitative endovascular balloon occlusion of the aorta. Anesth Analg. 2017;125(3):891-894. doi: 10.1213/ANE.0000000000002215 [DOI] [PubMed] [Google Scholar]
- 2.Beall AC Jr, Diethrich EB, Crawford HW, Cooley DA, De Bakey ME. Surgical management of penetrating cardiac injuries. Am J Surg. 1966;112(5):686-692. doi: 10.1016/0002-9610(66)90105-X [DOI] [PubMed] [Google Scholar]
- 3.Ledgerwood AM, Kazmers M, Lucas CE. The role of thoracic aortic occlusion for massive hemoperitoneum. J Trauma. 1976;16(08):610-615. doi: 10.1097/00005373-197608000-00004 [DOI] [PubMed] [Google Scholar]
- 4.Nunn A, Prakash P, Inaba K, et al. Occupational exposure during emergency department thoracotomy: a prospective, multi-institution study. J Trauma Acute Care Surg. 2018;85(1):78-84. doi: 10.1097/TA.0000000000001940 [DOI] [PubMed] [Google Scholar]
- 5.Pieracci FM, Burlew CC, Spain D, et al. Tube thoracostomy during the COVID-19 pandemic: guidance and recommendations from the AAST Acute Care Surgery and Critical Care Committees. Trauma Surg Acute Care Open. 2020;5(1):e000498. doi: 10.1136/tsaco-2020-000498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zuo YY, Uspal WE, Wei T. Airborne transmission of COVID-19: aerosol dispersion, lung deposition, and virus-receptor interactions. ACS Nano. 2020. doi: 10.1021/acsnano.0c08484 [DOI] [PubMed] [Google Scholar]
- 7.van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382(16):1564-1567. doi: 10.1056/NEJMc2004973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harfouche MN, Madurska MJ, Elansary N, et al. Resuscitative endovascular balloon occlusion of the aorta associated with improved survival in hemorrhagic shock. PLoS One. 2022;17(3):e0265778. doi: 10.1371/journal.pone.0265778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Norii T, Crandall C, Terasaka Y. Survival of severe blunt trauma patients treated with resuscitative endovascular balloon occlusion of the aorta compared with propensity score-adjusted untreated patients. J Trauma Acute Care Surg. 2015;78(4):721-728. doi: 10.1097/TA.0000000000000578 [DOI] [PubMed] [Google Scholar]
- 10.Yamamoto R, Cestero RF, Suzuki M, Funabiki T, Sasaki J. Resuscitative endovascular balloon occlusion of the aorta (REBOA) is associated with improved survival in severely injured patients: A propensity score matching analysis. Am J Surg. 2019;218(6):1162-1168. doi: 10.1016/j.amjsurg.2019.09.007 [DOI] [PubMed] [Google Scholar]
- 11.Joseph B, Zeeshan M, Sakran JV, et al. Nationwide analysis of resuscitative endovascular balloon occlusion of the aorta in civilian trauma. JAMA Surg. 2019;154(6):500-508. doi: 10.1001/jamasurg.2019.0096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Manzano Nunez R, Naranjo MP, Foianini E, et al. A meta-analysis of resuscitative endovascular balloon occlusion of the aorta (REBOA) or open aortic cross-clamping by resuscitative thoracotomy in non-compressible torso hemorrhage patients. World J Emerg Surg. 2017;12:30. doi: 10.1186/s13017-017-0142-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aso S, Matsui H, Fushimi K, Yasunaga H. Resuscitative endovascular balloon occlusion of the aorta or resuscitative thoracotomy with aortic clamping for noncompressible torso hemorrhage: a retrospective nationwide study. J Trauma Acute Care Surg. 2017;82(5):910-914. doi: 10.1097/TA.0000000000001345 [DOI] [PubMed] [Google Scholar]
- 14.Abe T, Uchida M, Nagata I, Saitoh D, Tamiya N. Resuscitative endovascular balloon occlusion of the aorta versus aortic cross clamping among patients with critical trauma: a nationwide cohort study in Japan. Crit Care. 2016;20(1):400. doi: 10.1186/s13054-016-1577-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.DuBose JJ, Scalea TM, Brenner M, et al. ; AAST AORTA Study Group . The AAST prospective Aortic Occlusion for Resuscitation in Trauma and Acute Care Surgery (AORTA) registry: data on contemporary utilization and outcomes of aortic occlusion and resuscitative balloon occlusion of the aorta (REBOA). J Trauma Acute Care Surg. 2016;81(3):409-419. doi: 10.1097/TA.0000000000001079 [DOI] [PubMed] [Google Scholar]
- 16.Tibbits EM, Hoareau GL, Simon MA, et al. Location is everything: the hemodynamic effects of REBOA in zone 1 vs zone 3 of the aorta. J Trauma Acute Care Surg. 2018;85(1):101-107. doi: 10.1097/TA.0000000000001858 [DOI] [PubMed] [Google Scholar]
- 17.Brenner M, Inaba K, Aiolfi A, et al. ; AAST AORTA Study Group . Resuscitative endovascular balloon occlusion of the aorta and resuscitative thoracotomy in select patients with hemorrhagic shock: early results from the American Association for the Surgery of Trauma’s Aortic Occlusion in Resuscitation for Trauma and Acute Care Surgery Registry. J Am Coll Surg. 2018;226(5):730-740. doi: 10.1016/j.jamcollsurg.2018.01.044 [DOI] [PubMed] [Google Scholar]
- 18.Brenner M, Zakhary B, Coimbra R, et al. ; AAST Multi-Institutional Trials Committee . Resuscitative endovascular balloon occlusion of the aorta (REBOA) may be superior to resuscitative thoracotomy (RT) in patients with traumatic brain injury (TBI). Trauma Surg Acute Care Open. 2022;7(1):e000715. doi: 10.1136/tsaco-2021-000715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schoenfeld DA, Bernard GR; ARDS Network . Statistical evaluation of ventilator-free days as an efficacy measure in clinical trials of treatments for acute respiratory distress syndrome. Crit Care Med. 2002;30(8):1772-1777. doi: 10.1097/00003246-200208000-00016 [DOI] [PubMed] [Google Scholar]
- 20.Moore LJ, Brenner M, Kozar RA, et al. Implementation of resuscitative endovascular balloon occlusion of the aorta as an alternative to resuscitative thoracotomy for noncompressible truncal hemorrhage. J Trauma Acute Care Surg. 2015;79(4):523-530. doi: 10.1097/TA.0000000000000809 [DOI] [PubMed] [Google Scholar]
- 21.Otsuka H, Sato T, Sakurai K, et al. Effect of resuscitative endovascular balloon occlusion of the aorta in hemodynamically unstable patients with multiple severe torso trauma: a retrospective study. World J Emerg Surg. 2018;13:49. doi: 10.1186/s13017-018-0210-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khalid S, Khatri M, Siddiqui MS, Ahmed J. Resuscitative endovascular balloon occlusion of aorta vs aortic cross-clamping by thoracotomy for noncompressible torso hemorrhage: a meta-analysis. J Surg Res. 2022;270:252-260. doi: 10.1016/j.jss.2021.09.016 [DOI] [PubMed] [Google Scholar]
- 23.Inoue J, Shiraishi A, Yoshiyuki A, Haruta K, Matsui H, Otomo Y. Resuscitative endovascular balloon occlusion of the aorta might be dangerous in patients with severe torso trauma: a propensity score analysis. J Trauma Acute Care Surg. 2016;80(4):559-566. doi: 10.1097/TA.0000000000000968 [DOI] [PubMed] [Google Scholar]
- 24.Teeter W, Romagnoli A, Wasicek P, et al. Resuscitative endovascular balloon occlusion of the aorta improves cardiac compression fraction vs resuscitative thoracotomy in patients in traumatic arrest. Ann Emerg Med. 2018;72(4):354-360. doi: 10.1016/j.annemergmed.2018.02.020 [DOI] [PubMed] [Google Scholar]
- 25.Teeter WA, Bradley MJ, Romagnoli A, et al. Treatment effect or effective treatment—cardiac compression fraction and end-tidal carbon dioxide are higher in patients resuscitative endovascular balloon occlusion of the aorta compared with resuscitative thoracotomy and open-chest cardiac massage. Am Surg. 2018;84(10):1691-1695. doi: 10.1177/000313481808401031 [DOI] [PubMed] [Google Scholar]
- 26.Davidson AJ, Russo RM, DuBose JJ, Roberts J, Jurkovich GJ, Galante JM. Potential benefit of early operative utilization of low profile, partial resuscitative endovascular balloon occlusion of the aorta (P-REBOA) in major traumatic hemorrhage. Trauma Surg Acute Care Open. 2016;1(1):e000028. doi: 10.1136/tsaco-2016-000028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Johnson MA, Neff LP, Williams TK, DuBose JJ, EVAC Study Group . Partial resuscitative balloon occlusion of the aorta (P-REBOA): clinical technique and rationale. J Trauma Acute Care Surg. 2016;81(5 Suppl 2 Proceedings of the 2015 Military Health System Research Symposium):S133-S137. doi: 10.1097/TA.0000000000001146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Manzano-Nunez R, Orlas CP, Herrera-Escobar JP, et al. A meta-analysis of the incidence of complications associated with groin access after the use of resuscitative endovascular balloon occlusion of the aorta in trauma patients. J Trauma Acute Care Surg. 2018;85(3):626-634. doi: 10.1097/TA.0000000000001978 [DOI] [PubMed] [Google Scholar]
- 29.Davidson AJ, Russo RM, Reva VA, et al. ; BEST Study Group . The pitfalls of resuscitative endovascular balloon occlusion of the aorta: risk factors and mitigation strategies. J Trauma Acute Care Surg. 2018;84(1):192-202. doi: 10.1097/TA.0000000000001711 [DOI] [PubMed] [Google Scholar]
- 30.Seamon MJ, Haut ER, Van Arendonk K, et al. An evidence-based approach to patient selection for emergency department thoracotomy: a practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2015;79(1):159-173. doi: 10.1097/TA.0000000000000648 [DOI] [PubMed] [Google Scholar]
- 31.Stokes SC, Theodorou CM, Zakaluzny SA, DuBose JJ, Russo RM. Resuscitative endovascular balloon occlusion of the aorta in combat casualties: the past, present, and future. J Trauma Acute Care Surg. 2021;91(2S Suppl 2):S56-S64. doi: 10.1097/TA.0000000000003166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Northern DM, Manley JD, Lyon R, et al. Recent advances in austere combat surgery: use of aortic balloon occlusion as well as blood challenges by special operations medical forces in recent combat operations. J Trauma Acute Care Surg. 2018;85(1S Suppl 2):S98-S103. doi: 10.1097/TA.0000000000001966 [DOI] [PubMed] [Google Scholar]
- 33.Glaser J, Stigall K, Jensen CS, Morrison UJJ, Snyder S, Russo MR. Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) for hemorrhagic shock (CPG ID:38). Joint Trauma Syst Clin Pract Guideline. 2020;31:1-28. [Google Scholar]
- 34.Fisher AD, Teeter WA, Cordova CB, et al. The role I resuscitation team and resuscitative endovascular balloon occlusion of the aorta. J Spec Oper Med. 2017;17(2):65-73. doi: 10.55460/ME32-0LIR [DOI] [PubMed] [Google Scholar]
- 35.Gonzalez E, Moore EE, Moore HB, et al. Goal-directed hemostatic resuscitation of trauma-induced coagulopathy: a pragmatic randomized clinical trial comparing a viscoelastic assay to conventional coagulation assays. Ann Surg. 2016;263(6):1051-1059. doi: 10.1097/SLA.0000000000001608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Committee on Military Trauma Care’s Learning Health System and Its Translation to the Civilian Sector; Board on Health Sciences Policy; Board on the Health of Select Populations ; eds. A National Trauma Care System: Integrating Military and Civilian Trauma Systems to Achieve Zero Preventable Deaths After Injury. The National Academies Press; 2016. [PubMed] [Google Scholar]
- 37.Elster EA, Butler FK, Rasmussen TE. Implications of combat casualty care for mass casualty events. JAMA. 2013;310(5):475-476. doi: 10.1001/jama.2013.167481 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure. Propensity Score Matching Balance Diagnostics
eTable. Comparison Between Unmatched and Matched Patients (by Propensity Score Matching)
Nonauthor Collaborators