Key Points
Question
Are academic medical centers compliant with the Price Transparency Final Rule, and how does the price of urologic procedures vary among hospitals and by insurance class ?
Findings
In this cross-sectional analysis of 153 academic hospitals, compliance with the mandate was low, and there were large variations in the price of procedures among hospitals. There were also significant differences in the price of 5 urologic procedures by insurance class (Medicare, Medicaid, commercial insurance, and cash price), with the cash price being the lowest reported at 16% of hospitals.
Meaning
These findings suggest that more than 1 year after the implementation of the Price Transparency Final Rule, there are still large variations in the prices of urologic procedures among academic hospitals and by insurance class.
This cross-sectional study examines compliance with the Price Transparency Final Rule and quantifies variations in the price of urologic procedures among academic hospitals and by insurance class.
Abstract
Importance
Patients with urologic diseases often experience financial toxicity, defined as high levels of financial burden and concern, after receiving care. The Price Transparency Final Rule, which requires hospitals to disclose both the commercial and cash prices for at least 300 services, was implemented to facilitate price shopping, decrease price dispersion, and lower health care costs.
Objective
To evaluate compliance with the Price Transparency Final Rule and to quantify variations in the price of urologic procedures among academic hospitals and by insurance class.
Design, Setting, and Participants
This was a cross-sectional study that determined the prices of 5 common urologic procedures among academic medical centers and by insurance class. Prices were obtained from the Turquoise Health Database on March 24, 2022. Academic hospitals were identified from the Association of American Medical Colleges website. The 5 most common urologic procedures were cystourethroscopy, prostate biopsy, laparoscopic radical prostatectomy, transurethral resection of the prostate, and ureteroscopy with laser lithotripsy. Using the corresponding Current Procedural Terminology codes, the Turquoise Health Database was queried to identify the cash price, Medicare price, Medicaid price, and commercial insurance price for these procedures.
Exposures
The Price Transparency Final Rule, which went into effect January 1, 2021.
Main Outcomes and Measures
Variability in procedure price among academic medical centers and by insurance class (Medicare, Medicaid, commercial, and cash price).
Results
Of 153 hospitals, only 20 (13%) listed a commercial price for all 5 procedures. The commercial price was reported most often for cystourethroscopy (86 hospitals [56%]) and least often for laparoscopic radical prostatectomy (45 hospitals [29%]). The cash price was lower than the Medicare, Medicaid, and commercial price at 24 hospitals (16%). Prices varied substantially across hospitals for all 5 procedures. There were significant variations in the prices of cystoscopy (χ23 = 85.9; P = .001), prostate biopsy (χ23 = 64.6; P = .001), prostatectomy (χ23 = 24.4; P = .001), transurethral resection of the prostate (χ23 = 51.3; P = .001), and ureteroscopy with laser lithotripsy (χ23 = 63.0; P = .001) by insurance type.
Conclusions and Relevance
These findings suggest that, more than 1 year after the implementation of the Price Transparency Final Rule, there are still large variations in the prices of urologic procedures among academic hospitals and by insurance class. Currently, in certain situations, health care costs could be reduced if patients paid out of pocket. The Centers for Medicare & Medicaid Services may improve price transparency by better enforcing penalties for noncompliance, increasing penalties, and ensuring that hospitals report prices in a way that is easy for patients to access and understand.
Introduction
The US spends almost twice as much on health care as other developed nations, in part because of the higher prices US individuals pay for health care products and services.1 For the 31.6 million US individuals without health insurance and the 40% of privately insured US individuals with high-deductible health plans, these high prices can translate to high out-of-pocket costs.2,3,4 High out-of-pocket costs represent a substantial financial burden for some patients, who may then forgo or delay necessary care.5,6
To improve patient care and combat rising prices, the Centers for Medicare & Medicaid Services (CMS) passed the Hospital Price Transparency Final Rule, which requires that hospitals publish their standard charges in a publicly available, machine-readable file.7 Price transparency is a prerequisite for price shopping, and according to standard economic theory, price shopping ensures that identical goods at different locations have the same price (the Law of One Price). Theoretically, the Hospital Price Transparency Final Rule would make it possible for patients to price shop, which should encourage competition and lead to lower and more uniform prices.7
Approximately 1 in 4 patients with a urologic disease experiences financial toxicity, which are defined as the financial burden and stress associated with receiving care.8,9,10 High levels of financial toxicity are associated with care delays and poor health care–related quality of life. For these patients, price transparency, and the subsequent reductions in cost, could greatly improve the affordability of care and reduce financial toxicity.11,12 To better understand the impact of price transparency on urologic care, we examined prices for 5 common urologic procedures among academic medical centers. We also compared prices among different insurances classes, including commercial, Medicaid, Medicare, and the cash price.
Methods
Hospitals and Procedures
This cross-sectional study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines. This study did not involve any human participants and so did not require institutional review board approval or informed consent, in accordance with 45 CFR §46. Using the Association of American Medical Colleges website, we identified all academic hospitals. Exclusion criteria included duplicate hospitals (identified by the same address or if 1 address corresponded to a corporate office building), health care systems (with multiple hospitals that were not independently listed on the website), specialty hospitals that do not provided urologic care, children’s hospitals, and Veterans Affairs hospitals (which are not required to disclose prices).
Using data from our multihospital, academic institution, we identified the 5 most common urological procedures performed during 2020 and 2021. These were cystourethroscopy, prostate biopsy, laparoscopic radical prostatectomy, transurethral resection of the prostate (TURP), and ureteroscopy with laser lithotripsy (URS/LL). We used the Current Procedural Terminology (CPT) codes for these procedures (52000, 55700, 55866, 52601, and 52353, respectively) to determine the associated costs. To ensure that case volumes at our institution were representative of those at other academic medical centers, we identified the most common procedures performed by urology residents according to Accreditation Council for Graduate Medical Education case logs. As described by Silvestre et al,13 from 2010 to 2018, the most commonly logged procedures were transurethral surgery (which would include both cystoscopy and TURP as well as others), ureteroscopy (with or without laser lithotripsy), prostate biopsy, and radical prostatectomy (with or without laparoscopic assistance).
Data Source
We obtained all pricing information from Turquoise Health, a data service company that compiles pricing information from the machine-readable files hospitals must provide to comply with CMS regulations.14 Hospitals are required to disclose 5 standard charges, including (1) the gross prices, (2) the payer-specific negotiated prices, (3) the discounted cash prices, (4) the deidentified minimum negotiated prices, and (5) the deidentified maximum negotiated prices for at least 300 shoppable services. The gross price is the price as listed on the hospital chargemaster before any negotiations with third-party payers (which would then be the payer-specific negotiated charges), and the discounted cash price is the price that would apply to self-pay or uninsured patients. Shoppable services are defined as “a service package that can be scheduled by a healthcare consumer in advance.”7 CMS has identified 70 required shoppable services, and the remaining 230 are chosen by the hospital.7 Of the 5 procedures included in our analysis, only prostate biopsy (CPT code 55700) and laparoscopic radical prostatectomy (CPT code 55866) are included in the CMS-specified list of shoppable services
The Turquoise Health Database has been used for several recent analyses.15,16,17 Using CPT codes, we queried the database for procedure costs as of March 24, 2022. We included costs for the following payer classes: commercial, Medicaid, Medicare, and the cash price. The Medicaid price was generated by Turquoise Health from Medicare’s outpatient prospective payment system and accounts for both the hospitals’ location and the wage index. Although hospitals are not required to disclose Medicare or Medicaid prices, we included these in our analysis to help contextualize commercial and discounted cash prices. Among commercial payers, we included Aetna, Blue Cross/Blue Shield, Cigna, and United Healthcare. If our query did not yield a unique cost in the Turquoise Health Database, we referenced the hospital’s chargemaster to determine which price to include. If the chargemaster was uninformative, we used the median price for analysis. The median commercial insurance price was defined as the median price of all the plans listed for each commercial insurer.
When provided by the hospitals, the database included details on where the procedure was performed (eg, office, operating room, ambulatory care center, or interventional radiology suite), if it was performed inpatient or outpatient, and any associated professional fees. However, these data were not consistently reported for several reasons. First, the CMS mandate only requires hospitals (not ambulatory care centers or clinics) to report prices. Second, hospitals are not required to report professional fees. Third, hospitals have to report both the inpatient and outpatient procedure price only if these prices are different (or if the hospital withholds this information and is not in full compliance).
Because cost was determined by CPT code, we excluded all prices that were specifically identified as an inpatient price; outpatient prices and prices that did not have a designation were included. We also excluded costs for services provided in the emergency department. To make our findings more applicable to everyday practice, we included the prices of only procedures performed in clinic or at an unspecified location for cystourethroscopy (CPT code 52000) and prostate biopsy (CPT code 55700). Similarly, we included prices only for procedures performed in the operating room or at an unspecified location for URS/LL (CPT code 52353), TURP (CPT code 52601), and laparoscopic radical prostatectomy (CPT code 55866).
Statistical Analysis
First, we determined the percentage of chosen hospitals that reported a procedure price for all 4 insurance classes and for all 4 commercial insurance types. Next, we determined how often the cash price was the lowest price reported for each of the 5 procedures among the hospitals. For each procedure, we compared prices among both the 4 insurance classes and among the 4 commercial insurance types using Kruskal-Wallis tests. We created violin plots to illustrate variations in the price among the different insurance classes for each procedure. We calculated the medians and IQRs of prices among insurance classes and commercial insurance types, to examine how the prices varied among reporting hospitals. As a sensitivity analysis, we compared both the highest and lowest negotiated prices by insurance class and by commercial insurance type. Analysis was performed with SAS statistical software version 9.4 (SAS Institute, Inc) and R statistical software version 4.1.0 (R Project for Statistical Computing). All tests were 2-sided and the probability of a type I error was set at α = .05.
Results
Among the 153 academic hospitals, commercial prices were reported more often for cystourethroscopy (86 hospitals [56%]) and prostate biopsy (81 hospitals [53%]) than for URS/LL (46 hospitals [30%]), TURP (47 hospitals [31%]), and laparoscopic radical prostatectomy (45 hospitals [29%]). The commercial prices were reported more often than the cash price (Table 1). Because laparoscopic prostatectomy is on the list of 70 shoppable services, just 29% of hospitals were compliant with the price transparency legislation. Compared with the other insurance classes, the cash price was the lowest reported price among 24 of 152 hospitals (16%) that reported prostate biopsy charges, 9 of 74 hospitals (12%) that reported laparoscopic prostatectomy, 17 of 141 hospitals (12%) that reported cystourethroscopy charges, 7 of 71 hospitals (10%) that reported URS/LL charges, and 5 of 67 hospitals (7%) that reported TURP charges (Table 2).
Table 1. Hospitals With Price Listed for Each Procedure by Insurance Type.
| Procedure and insurance type | Hospitals, No. (%) (N = 153) |
|---|---|
| Cystourethroscopy | |
| Commercial | 86 (56) |
| Medicaid | 51 (33) |
| Medicare reference pricing | 131 (86) |
| Cash | 70 (46) |
| Prostate biopsy | |
| Commercial | 81 (53) |
| Medicaid | 45 (29) |
| Medicare reference pricing | 141 (92) |
| Cash | 71 (46) |
| Prostatectomy | |
| Commercial | 45 (29) |
| Medicaid | 25 (16) |
| Medicare reference pricing | 68 (44) |
| Cash | 31 (20) |
| Transurethral resection of the prostate | |
| Commercial | 47 (31) |
| Medicaid | 27 (18) |
| Medicare reference pricing | 60 (39) |
| Cash | 24 (16) |
| Ureteroscopy with laser lithotripsy | |
| Commercial | 46 (30) |
| Medicaid | 32 (21) |
| Medicare reference pricing | 65 (42) |
| Cash | 30 (20) |
Table 2. Hospitals With the Lowest Price by Insurance Type for Each Procedure.
| Procedure and insurance type | Hospitals, No. (%)a |
|---|---|
| Cystourethroscopy (n = 141) | |
| Commercial | 4 (3) |
| Medicaid | 11 (8) |
| Medicare reference pricing | 109 (77) |
| Cash | 17 (12) |
| Prostate biopsy (n = 152) | |
| Commercial | 6 (4) |
| Medicaid | 29 (19) |
| Medicare reference pricing | 93 (61) |
| Cash | 24 (16) |
| Prostatectomy (n = 74) | |
| Commercial | 5 (7) |
| Medicaid | 22 (30) |
| Medicare reference pricing | 38 (51) |
| Cash | 9 (12) |
| Transurethral resection of the prostate (n = 67) | |
| Commercial | 1 (2) |
| Medicaid | 27 (40) |
| Medicare reference pricing | 35 (51) |
| Cash | 5 (7) |
| Ureteroscopy with laser lithotripsy (n = 71) | |
| Commercial | 3 (4) |
| Medicaid | 30 (42) |
| Medicare reference pricing | 31 (44) |
| Cash | 7 (10) |
To be included, each hospital had to list at least 3 of 4 insurance types.
There were significant variations in negotiated prices among hospitals (Table 3). There were significant variations in the prices of cystoscopy (χ23 = 85.9; P = .001), prostate biopsy (χ23 = 64.6; P = .001), prostatectomy (χ23 = 24.4; P = .001), TURP (χ23 = 51.3; P = .001), and URS/LL (χ23 = 63.0; P = .001) by insurance type. There was a significant difference in price among the 4 insurance classes for all 5 procedures (Figure 1). The prices ranged from $572 to $1179 for cystouretheroscopy, $1081 to $2465 for prostate biopsy, $3559 to $11 044 for radical prostatectomy, $2894 to $6445 for TURP, and $1746 to $5962 for URS/LL. Among the 4 private insurers, prices ranged from $1044 to $1316 for cystouretheroscopy, $2155 to $2514 for prostate biopsy, $9186 to $9800 for radical prostatectomy, $5228 to $7098 for TURP, and $5250 to $6588 for URS/LL.There were no significant differences in price among the different commercial insurance types (Figure 2). Results from the sensitivity analyses, during which we compared both the lowest (eTable 1 in Supplement 1) and highest (eTable 2 in Supplement 1) negotiated prices among insurance classes and among commercial insurance types, were similar.
Table 3. Cash Fee, Medicaid, Medicare, and Private Insurance Prices for Cystourethroscopy, Prostate Biopsy, Prostatectomy, Transurethral Resection of the Prostate, and Ureteroscopy With Laser Lithotripsy.
| Procedure and insurance type (CPT code) | Price, median (IQR), $ |
|---|---|
| Cystourethroscopy (52000) | |
| Commercial | 1179 (766-1728) |
| Medicaid | 757 (440-1147) |
| Medicare | 572 (534-606) |
| Cash | 1073 (591-1308) |
| Prostate biopsy (55700) | |
| Commercial | 2465 (1740-3747) |
| Medicaid | 1081 (667-1711) |
| Medicare | 1784 (1667-1890) |
| Cash | 2149 (1284-3392) |
| Prostatectomy (55866) | |
| Commercial | 8894 (7838-13 631) |
| Medicaid | 3559 (2882-5353) |
| Medicare | 8891 (8306-9391) |
| Cash | 11 044 (4434-25 555) |
| Transurethral resection of the prostate (52601) | |
| Commercial | 5666 (4264-8209) |
| Medicaid | 2894 (1770-3017) |
| Medicare | 4392 (4116-4771) |
| Cash | 6445 (4034-12 054) |
| Ureteroscopy with laser lithotripsy (52353) | |
| Commercial | 5962 (4103-8084) |
| Medicaid | 1746 (1055-2547) |
| Medicare | 4392 (4100-5122) |
| Cash | 4784 (3085-9812) |
Abbreviation: CPT, Current Procedural Terminology.
Figure 1. Variations in Procedure Price by Insurance Class.
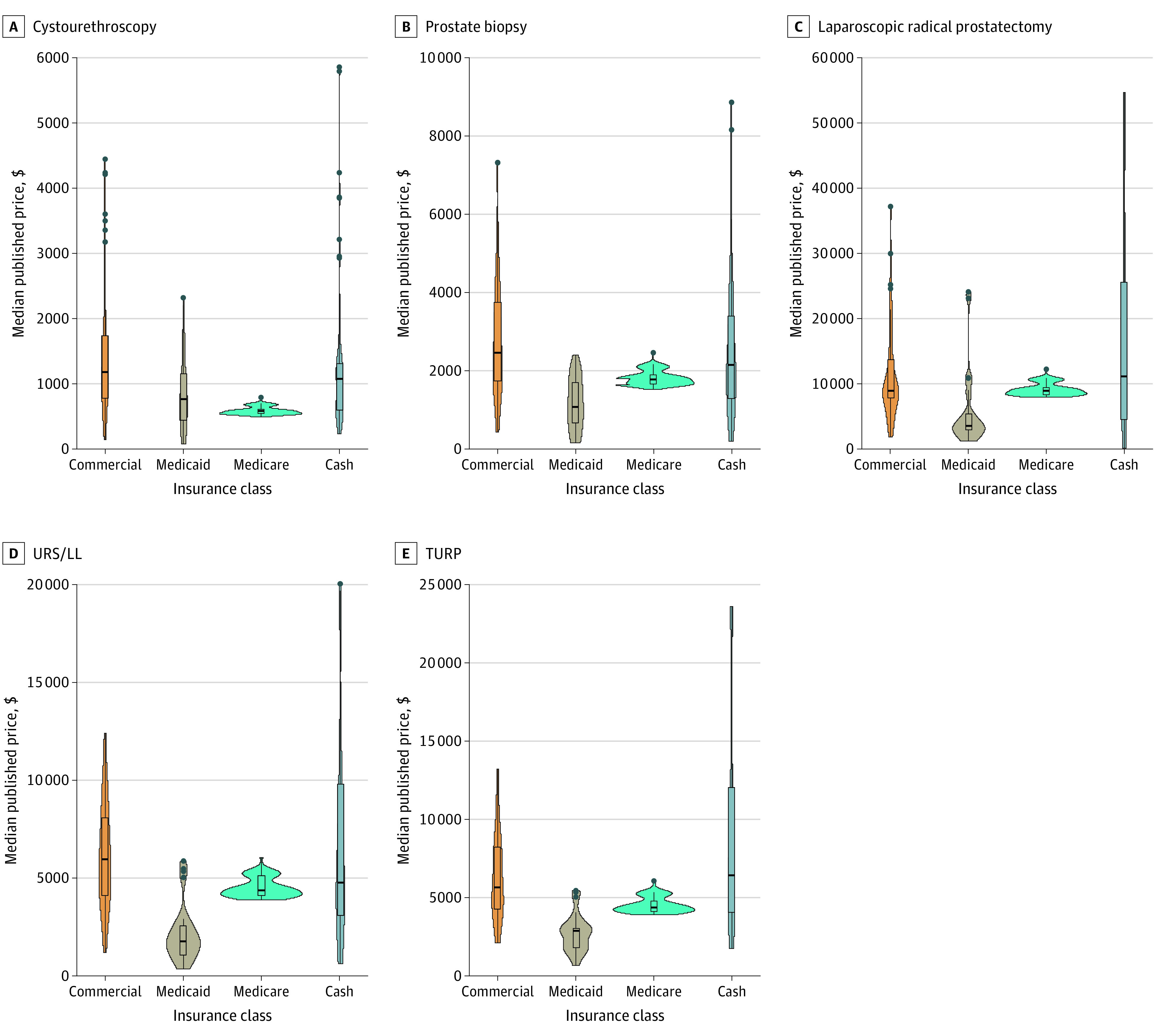
TURP indicates transurethral resection of the prostate; URS/LL, ureteroscopy with laser lithotripsy.
Figure 2. Variations in Procedure Price Among Commercial Insurance Types.
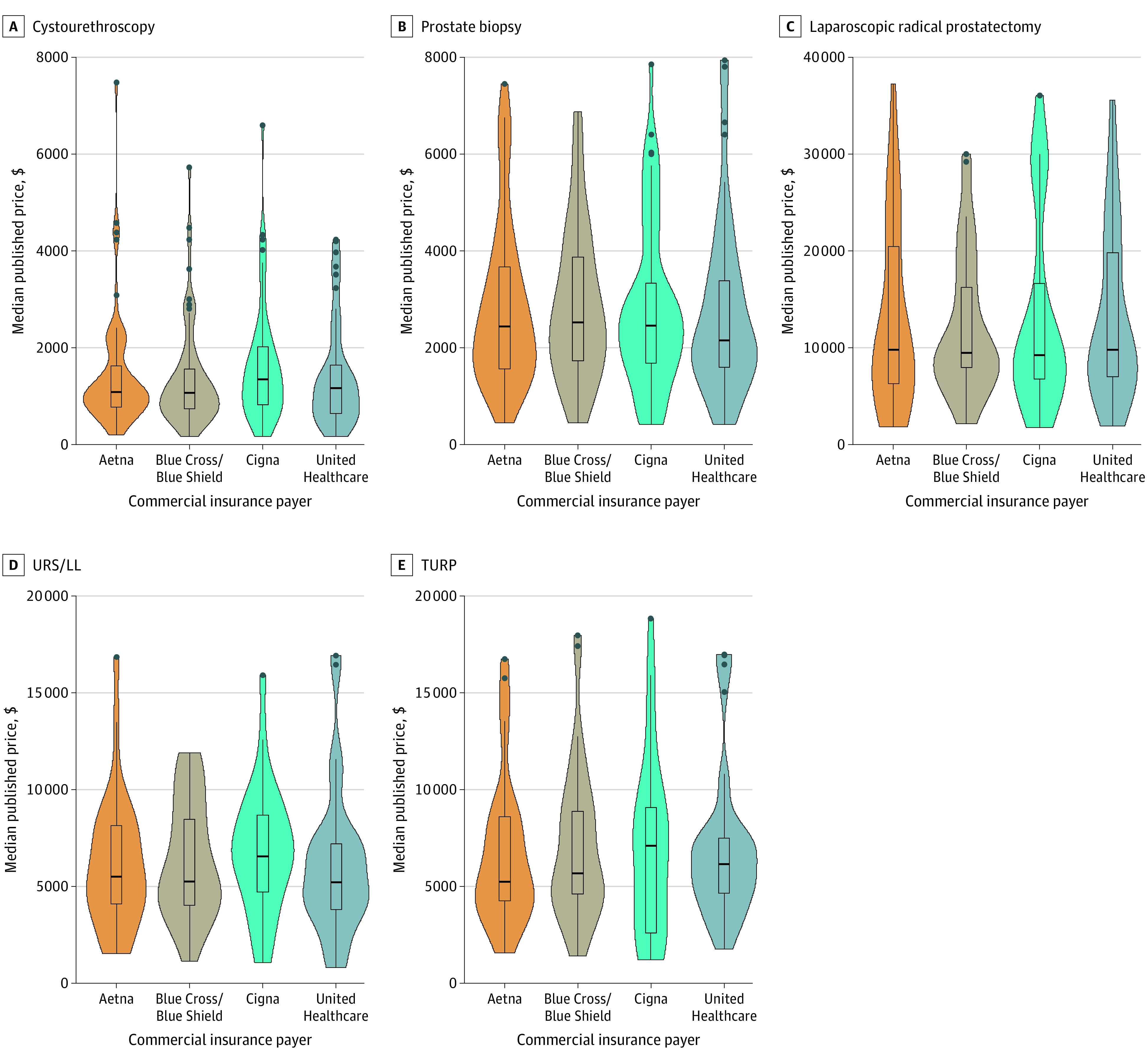
TURP indicates transurethral resection of the prostate; URS/LL, ureteroscopy with laser lithotripsy.
Discussion
This cross-sectional analysis of 153 academic hospitals found that compliance with the Price Transparency Final Rule remains below 30% and that there are large variations in the price of procedures among hospitals. There were also significant differences in price among the different insurance classes for all 5 common urologic procedures. Most strikingly, the cash price was lower than the Medicare, Medicaid, and commercial price at 16% of hospitals. In other words, in certain situations, health care costs would be reduced if patients omitted their insurance information and paid out of pocket. For all 5 procedures, there were no significant differences in prices among the 4 commercial insurance types.
The persistently large variations in the price of urologic procedures, among academic medical centers and by insurance class, reveal that the Price Transparency Final Rule has not had its intended effect. One reason the Final Rule has fallen short is that compliance with the legislation is low. We found that only 29% of academic hospitals are compliant. These compliance rates are similar to those that have been previously reported, although 1 small study,12 which only included US News Top 21 Hospitals, found higher rates of price reporting.12,15,18 Among hospitals that are compliant, we found that prices are reported more often for lower cost procedures, and similar findings have been reported previously.15 The higher rates of price reporting for lower cost procedures, despite possible fines of up to $300 per day for noncompliance,7 suggests that some hospitals are purposefully omitting cost information. This implies that either fines are not being imposed or are not sufficiently costly to hospitals. We suspect that the primary issue is the former, because as of June 9, 2022, of the 5239 total hospitals registered with CMS, only 2 hospitals have been fined for noncompliance.19,20 To improve compliance with price transparency, fines actually need to be enforced and possibly increased.
Even if there were stricter enforcement and higher rates of compliance, cost differentials would be eliminated only by the competitive pressures of price shopping. Previous research21,22 has shown that even when pricing information is available, patients often do not shop for medical goods or services. Determining hospitals’ costs can be difficult and time intensive. For example, 1 study23 found that only 77% of academic hospitals’ websites presented consumer-friendly (not just machine readable) pricing information. Among these, 18% had usability issues, including long search times.23 Patients will price shop only if the associated cost savings are greater than the associated labor costs. For price transparency to be effective, new health care policy should address reducing this patient burden.
Limitations
Our findings should be interpreted in the context of several limitations. Most important are the limitations associated with the data and data reporting. In its current form, price transparency legislation only partially lifts the shroud of mystery surrounding patient billing. For example, the legislation applies to hospitals only, even though hospital care accounts for only approximately 30% of health care expenditures.24 Moreover, the costs hospitals disclose may be incomplete because they are not required to include the cost of independent practitioners, who often deliver hospital-based care and constitute a sizable portion of total care costs.25
Ambiguities in the legislation allow hospitals to omit potentially important pricing information without being obviously noncomplaint. One example is that hospitals must list both the inpatient and outpatient prices for services only if these prices are different. If only 1 price is listed, the patient cannot be sure whether prices are the same or whether the hospital is noncomplaint and is listing only the lower price. A similar equivocation requires hospitals to list the gross charge and the discounted cash price, but CMS notes that if hospitals have not yet “determined a discounted cash price for self-pay consumers…the hospitals’ cash price would simply be the gross charges.”7 As written, hospitals can either not offer a discounted cash price and instead use the gross charge, which is marked up to maximize hospital revenue, or conceal information from patients about lower prices and can technically appear compliant.26
Another limitation is the potential lack of generalizability to nonacademic centers and other specialties. A previous study17 of the hospital factors associated with price transparency found that teaching hospitals were more compliant in 1 of their 4 models. In addition, although payers with larger enrollment should theoretically be able to achieve better pricing, because we did not have information about insurer-level enrollment, we were unable to account for the impact of enrollment size on prices. It is also likely that there are inaccuracies associated with Turquoise Health’s automatic data compilation and that we are overestimating hospital compliance. The data were sourced from machine-readable files, and we did not assess whether hospitals also provided consumer-friendly pricing tools, both of which are required by the mandate. Despite these limitations, our findings reveal an opportunity to reduce health care spending as well as elucidate how future health care policies could improve price transparency.
Conclusions
More than 1 year after the implementation of the Price Transparency Final Rule, this cross-sectional study found that there are still large variations in the prices of urologic procedures among academic hospitals and by insurance class. To improve efficacy, CMS must enforce penalties for noncompliance, and new policies should emphasize easy accesses to pricing information.
eTable 1. Median of the Minimum Prices and Interquartile Range (IQR) of the Minimum Prices for the Commercial Price, Medicaid Price, Medicare Reference Price, and Cash Price for Cystourethroscopy, Prostate Biopsy, Prostatectomy, Transurethral Resection of the Prostate (TURP), and Ureteroscopy With Laser Lithotripsy (URS/LL)
eTable 2. Median of the Maximum Prices and Interquartile Range (IQR) of the Maximum Prices for the Commercial Price, Medicaid Price, Medicare Reference Price, and Cash Price for Cystourethroscopy, Prostate Biopsy, Prostatectomy, Transurethral Resection of the Prostate (TURP), and Ureteroscopy With Laser Lithotripsy (URS/LL)
Data Sharing Statement
References
- 1.Reinhardt UE. The disruptive innovation of price transparency in health care. JAMA. 2013;310(18):1927-1928. doi: 10.1001/jama.2013.281854 [DOI] [PubMed] [Google Scholar]
- 2.Kullgren JT, Cliff BQ, Krenz CD, et al. A survey of Americans with high-deductible health plans identifies opportunities to enhance consumer behaviors. Health Aff (Millwood). 2019;38(3):416-424. doi: 10.1377/hlthaff.2018.05018 [DOI] [PubMed] [Google Scholar]
- 3.Cha AE, Cohen RA. Demographic variation in health insurance coverage: United States, 2020. Accessed June 21, 2022. https://www.cdc.gov/nchs/products/index.htm [PubMed]
- 4.Fletcher SA, Cole AP, Lu C, et al. The impact of underinsurance on bladder cancer diagnosis, survival, and care delivery for individuals under the age of 65 years. Cancer. 2020;126(3):496-505. doi: 10.1002/cncr.32562 [DOI] [PubMed] [Google Scholar]
- 5.Yelorda K, Rose L, Bundorf MK, Muhammad HA, Morris AM. Association between high-deductible health plans and hernia acuity. JAMA Surg. 2022;157(4):321-326. doi: 10.1001/jamasurg.2021.7567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chhabra KR, Fan Z, Chao GF, Dimick JB, Telem DA. The role of commercial health insurance characteristics in bariatric surgery utilization. Ann Surg. 2021;273(6):1150-1156. doi: 10.1097/SLA.0000000000003569 [DOI] [PubMed] [Google Scholar]
- 7.Centers for Medicare and Medicaid Services . Medicare and Medicaid Programs: CY 2020 hospital outpatient PPS policy changes and payment rates and ambulatory surgical center payment system policy changes and payment rates—price transparency requirements for hospitals to make standard charges public. Fed Regist. 2019;84(229):65524-65606. Accessed November 21, 2022. https://www.federalregister.gov/documents/2019/11/27/2019-24931/medicare-and-medicaid-programs-cy-2020-hospital-outpatient-pps-policy-changes-and-payment-rates-and [Google Scholar]
- 8.Bhanvadia SK, Psutka SP, Burg ML, et al. Financial toxicity among patients with prostate, bladder, and kidney cancer: a systematic review and call to action. Eur Urol Oncol. 2021;4(3):396-404. doi: 10.1016/j.euo.2021.02.007 [DOI] [PubMed] [Google Scholar]
- 9.Au D, Starkey J, Thompson J, Parker W. PD25-10: Evaluation of urologic patient reported peri-operative financial toxicity. J Urol. 2022;207(suppl 5):e425. doi: 10.1097/JU.0000000000002567.10 [DOI] [Google Scholar]
- 10.Green B, Feiertag N, Gupta K, Donnelly J, Watts K, Small A. MP26-17: Financial toxicity of nephrolithiasis: an assessment of the economic burden of stone disease treatment in a diverse, urban population. J Urol. 2022;207(suppl 5):e446. doi: 10.1097/JU.0000000000002569.17 [DOI] [PubMed] [Google Scholar]
- 11.Agarwal A, Dayal A, Kircher SM, Chen RC, Royce TJ. Analysis of price transparency via National Cancer Institute–designated cancer centers’ chargemasters for prostate cancer radiation therapy. JAMA Oncol. 2020;6(3):409-412. doi: 10.1001/jamaoncol.2019.5690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sood A, Butaney M, Olson P, et al. The impact of the price transparency mandate on cost reporting for common urological services across the U.S. News top 21 hospitals. Urol Pract. 2021;8(6):657-660. doi: 10.1097/UPJ.0000000000000264 [DOI] [PubMed] [Google Scholar]
- 13.Silvestre J, Caruso VA, Hernandez JM, Lee DI. Longitudinal assessment of adult cases performed by graduating urology residents in the United States: 2010–2018. Urol Pract. 2020;7(1):53-60. doi: 10.1097/UPJ.0000000000000075 [DOI] [PubMed] [Google Scholar]
- 14.Turquoise Health . For patients. Accessed June 29, 2022. https://turquoise.health/patients
- 15.Jiang JX, Makary MA, Bai G. Comparison of US hospital cash prices and commercial negotiated prices for 70 services. JAMA Netw Open. 2021;4(12):e2140526. doi: 10.1001/jamanetworkopen.2021.40526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jiang JX, Makary MA, Bai G. Commercial negotiated prices for CMS-specified shoppable radiology services in U.S. hospitals. Radiology. 2022;302(3):622-624. doi: 10.1148/radiol.2021211948 [DOI] [PubMed] [Google Scholar]
- 17.Jiang JX, Polsky D, Littlejohn J, Wang Y, Zare H, Bai G. Factors associated with compliance to the hospital price transparency final rule: a national landscape study. J Gen Intern Med. 2022;(14):3577-3584. doi: 10.1007/s11606-021-07237-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gondi S, Beckman AL, Ofoje AA, Hinkes P, McWilliams JM. Early hospital compliance with federal requirements for price transparency. JAMA Intern Med. 2021;181(10):1396-1397. doi: 10.1001/jamainternmed.2021.2531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Haque W, Ahmadzada M, Janumpally S, et al. Adherence to a federal hospital price transparency rule and associated financial and marketplace factors. JAMA. 2022;327(21):2143-2145. doi: 10.1001/jama.2022.5363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roubein R. Two hospitals are being fined for disobeying price transparency rules. The Washington Post. June 9, 2022. Accessed June 22, 2022. https://www.washingtonpost.com/politics/2022/06/09/two-hospitals-are-being-fined-disobeying-price-transparency-rules/
- 21.Glied S. Price transparency: promise and peril. JAMA. 2021;325(15):1496-1497. doi: 10.1001/jama.2021.4640 [DOI] [PubMed] [Google Scholar]
- 22.Emanuel EJ, Diana A. Considering the future of price transparency initiatives: information alone is not sufficient. JAMA Netw Open. 2021;4(12):e2137566. doi: 10.1001/jamanetworkopen.2021.37566 [DOI] [PubMed] [Google Scholar]
- 23.Berkowitz ST, Siktberg J, Hamdan SA, Triana AJ, Patel SN. Health care price transparency in ophthalmology. JAMA Ophthalmol. 2021;139(11):1210-1216. doi: 10.1001/jamaophthalmol.2021.3951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hartman M, Martin AB, Washington B, Catlin A; The National Health Expenditure Accounts Team . National health care spending in 2020: growth driven by federal spending in response to the COVID-19 pandemic. Health Aff (Millwood). 2022;41(1):13-25. doi: 10.1377/hlthaff.2021.01763 [DOI] [PubMed] [Google Scholar]
- 25.Horný M, Shafer PR, Dusetzina SB. Concordance of disclosed hospital prices with total reimbursements for hospital-based care among commercially insured patients in the US. JAMA Netw Open. 2021;4(12):e2137390. doi: 10.1001/jamanetworkopen.2021.37390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bai G, Anderson GF. US hospitals are still using Chargemaster markups to maximize revenues. Health Aff. 2016;35(9). doi: 10.1377/hlthaff.2016.0093 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Median of the Minimum Prices and Interquartile Range (IQR) of the Minimum Prices for the Commercial Price, Medicaid Price, Medicare Reference Price, and Cash Price for Cystourethroscopy, Prostate Biopsy, Prostatectomy, Transurethral Resection of the Prostate (TURP), and Ureteroscopy With Laser Lithotripsy (URS/LL)
eTable 2. Median of the Maximum Prices and Interquartile Range (IQR) of the Maximum Prices for the Commercial Price, Medicaid Price, Medicare Reference Price, and Cash Price for Cystourethroscopy, Prostate Biopsy, Prostatectomy, Transurethral Resection of the Prostate (TURP), and Ureteroscopy With Laser Lithotripsy (URS/LL)
Data Sharing Statement


