This qualitative study assesses the utility values, or quality of life burden measures, for the various thyroid eye disease health states.
Key Points
Question
What are utility values, or quality of life (QoL) burden measures, for the various thyroid eye disease (TED) health states?
Findings
In this qualitative study of 111 participant interviews, the lowest mean value (representing the worst QoL outcome) was observed for the most severe health state (large proptosis and constant diplopia), and the highest mean value was observed for the least severe health state (low proptosis and no diplopia).
Meaning
These findings suggest moderate-severe TED is associated with worse utility values, with increasing severities of proptosis and diplopia having greater association.
Abstract
Importance
Thyroid eye disease (TED) results in varying degrees of proptosis and diplopia negatively affecting quality of life (QoL), producing possibly substantial visual changes, disfigurement, and disability.
Objective
To determine the association of varying TED severities with QoL in a non-TED population by assessing health state utility scores.
Design, Setting, and Participants
This qualitative study, conducted from April 20, 2020, to April 29, 2021, assessed health states for active, moderate-severe TED, and values were elicited using time trade-off methods. Six health states of varying severity were determined from 2 placebo-controlled clinical trials (171 patients with TED and clinical activity score ≥4, ±diplopia/proptosis) and refined using interviews with US patients with TED (n = 6). Each health state description was validated by interviews with additional TED patient advocates (n = 3) and physician experts (n = 3). Health state descriptions and a QOL questionnaire were piloted and administered to a general population. Visual analog scales (VASs) were also administered to detect concurrence of the findings.
Main Outcomes and Measures
TED health state utility scores and whether they differ from one another were assessed using Shapiro-Wilk, Kruskal-Wallis, pairwise Wilcoxon rank sum, and paired t tests.
Results
A total of 111 participants completed time trade-off interviews. The mean (SD) utility value was 0.44 (0.34). The lowest (worse) mean utility value was observed in the most severe disease state (constant diplopia/large proptosis) with 0.30 (95% CI, 0.24-0.36), followed by constant diplopia/small proptosis (0.34; 95% CI, 0.29-0.40), intermittent or inconstant diplopia/large proptosis (0.43; 95% CI, 0.36-0.49), no diplopia/large proptosis (0.46; 95% CI, 0.40-0.52), and intermittent or inconstant diplopia/small proptosis (0.52; 95% CI, 0.45-0.58). The highest (best) mean value, 0.60 (95% CI, 0.54-0.67), was observed for the least severe disease state (no diplopia/small proptosis).
Conclusions and Relevance
These findings suggest that patients with active, moderate-severe TED may have substantial disutility, with increasing severity of proptosis/diplopia more likely to have detrimental associations with QoL. These health state scores may provide a baseline for determining QoL improvement in these TED health states (utility gains) treated with new therapies.
Introduction
Thyroid eye disease (TED) is an inflammatory autoimmune condition most often presenting with Graves disease. In the US, TED prevalence is between 0.16% and 0.25%.1,2 Those at risk for more severe disease include male individuals, those older than 65 years, tobacco users, and those with a high level of thyroid autoantibodies.1,3,4
TED begins with orbital and periocular inflammation typically followed by a less active but still symptomatic chronic disease course.5,6,7 Active TED, defined by a clinical activity score (CAS), includes orbital/periocular pain, swelling, and redness with proptosis and diplopia present in more severe disease.5,6,7
Increasing levels of proptosis and diplopia are associated with worsening QoL.8,9 These manifestations may prevent carrying out daily tasks such as driving and reading and have been associated with substantial psychosocial distress, most notably anxiety and depression from changes in appearance and visual function.10,11
Health state utilities are cardinal values that reflect an individual’s preference for different health outcomes, such as trading off a shorter period of time in perfect health vs a longer time with a disease that reduces QoL. Utility values play an important role in cost-effectiveness analyses as well as health technology appraisals. They allow comparisons of QoL impact among differing diseases. To our knowledge, published utility values have not been defined for TED-induced health states with varying levels of proptosis and diplopia, against a backdrop (anchor health state) of heightened inflammation. Therefore, the primary objective of this study was to elicit utility values for health states associated with moderate-severe active TED of varying severities. These were assessed by magnitude of proptosis and diplopia (separately and combined), to demonstrate QoL burden associated with TED and allow for future assessment of QoL gains with treatments.
Methods
Overview of Study Design
This qualitative analysis, including the collection and evaluation of protected health information, was compliant with the Health Insurance Portability and Accountability Act and adhered to the ethical principles outlined in the Declaration of Helsinki as amended in 2013. This study was conducted from April 20, 2020, to April 29, 2021. Institutional review board approval was not required for this study as it is defined as market research and is exempt. Patients agreed to participate in the interview and were assured confidentiality. All patients, health care professionals, and members of the public voluntarily participated in this study following identification from a patient advisory council, an expert panel, and a general population US proprietary panel, respectively. Participants were identified using a predefined screening questionnaire. All respondents provided written consent before study recruitment. All respondents participating in interview development or validation remained anonymous according to regulations and practice guidelines of market research governing bodies. These included the Council of American Survey Research Organizations and followed the Standards for Reporting Qualitative Research (SRQR) reporting guidelines for qualitative studies. Respondents were remunerated for their time according to fair market values.
Health states were developed using results from 2 placebo-controlled clinical trials in patients with active, moderate-severe TED with differing severities of proptosis and diplopia and interviews with patients with TED.12,13,14 The health state descriptions were validated through expert TED physician and patient advocate interviews. Utility scores were elicited using time trade-off (TTO) methods with a finite 10-year horizon.15 TTO methodology is widely accepted for valuing preference-based health-related QoL. The Measurement and Valuation of Health TTO protocol was used, involving the respondent trading off years with a poor QoL for a shorter period of life in full health.16 A utility score (decimalized) was then calculated using the interviewee’s value from the TTO interview between perfect health (1) and death (0) based on these trade-offs. Lower utility score represents worse QoL. The TTO interviews were conducted by 2 trained TTO interviewers who were independent of the study authors.
Health State Development
Each health state description represents patients with active TED with varying severities of proptosis and diplopia. Six health states (Box) were defined through a development and validation process (eFigure in Supplement 1) according to baseline clinical features of patients participating in the 2 clinical trials (171 patients with TED, CAS ≥4, ±diplopia/proptosis).12,13,14 Individual patient data were reviewed and categorized by proptosis degree (<3 mm or ≥3 mm [above upper limit of normal for race and sex]) and diplopia (none, intermittent, inconstant, or constant). These health state descriptions were further refined using telephone interviews (1 hour) with 6 US patients with TED. A semistructured interview guide was used subsequently to explore how the disease was associated with patient QoL (eAppendix 1 in Supplement 1).
Box. TED Health States in Order of Severitya.
1. No diplopia, small proptosis (<3 mm)
2. No diplopia, large proptosis (≥3 mm)
3. Intermittent or inconstant diplopia, small proptosis (<3 mm)
4. Intermittent or inconstant diplopia, large proptosis (≥3 mm)
5. Constant diplopia, small proptosis (<3 mm)
6. Constant diplopia, large proptosis (≥3 mm)
Descriptive language development focused on how each health state was associated with physical, mental, and social QoL. All of these health state descriptions incorporated QoL outcomes, including limitations on daily activities, problems with self-image, reduced social activities and interactions with others, inability to work/reduced productivity, anxiety about the future, coping mechanism, and treatments. Photographs of patients with CAS scores of 4 or greater with varying proptosis levels and language (with imaging) describing the association with diplopia were also used to aid the respondents’ understanding the outcome of each health state (eAppendix 2 in Supplement 1).
Health State Validation
To confirm the validity and ensure that each health state was representative of patients with TED and its association with QoL, interviews were conducted with 1 oculoplastic surgeon (G.L.), 1 comprehensive ophthalmologist (K.C.), and 1 endocrinologist (T.J.S.) with more than 4 years in practice, and 3 interviews were conducted with members of a patient advisory council, each with moderate-severe TED.
TTO Valuation Phase
Participants
Recruitment of a demographically representative sample comprising 100 interviewees (without TED) in the US was accomplished using a general population US proprietary panel identified by a third-party recruitment agency. Participants from the following race and ethnicity groups were included: Asian, Black or African American, Hispanic, and White. Race and ethnicity data were obtained from the screener questionnaire used for the TTO study. Based on existing guidance for health utility studies, a sample size of 100 was deemed adequate for achieving demographically representative sampling of the US general population.17 General population interviews were used to minimize bias because this cohort does not have a vested interest in the treatment of particular health states, as opposed to patients with TED.18 A 10% dropout rate was assumed before the interview stage. The selection criteria included (1) adult US residents 18 years or older willing to give explicit informed written consent to participate and have their answers audio-recorded, (2) no participation in market research within the past 6 months, and (3) no conflict of interest (defined as employment in health care or market research). In addition, recruitment quotas were applied to ensure a geographically and demographically representative sample.
Pilot Study
Pilot interviews with members of the public were conducted for linguistic validation, using the same methodology intended for formal interviews. These interviews validated the approach and were included in the final analysis.
Utility Interview Procedures and Scoring
The standard TTO method of eliciting utilities was used in this study and included a 10-year time horizon.19 A time horizon beyond 10 years lacks comparability with other utility values previously reported using this methodology.15,20
The TTO assessment was chosen because the most common QoL measure from which utilities can be derived, the EuroQol 5 Dimension 5 Level (EQ-5D-5L) questionnaire, includes domains not adequately capturing all relevant dimensions of TED QoL. TED disease-specific measures, such as the Graves ophthalmopathy QoL (GO-QoL) questionnaire, have good validity, reliability, and responsiveness; however, that questionnaire has not been mapped previously or correlated with specific TED utility values.
To prevent bias during the utility study, each health state was titled with different geometric shapes. This allowed each health state to be referred to without any implication of progression and/or severity.
The visual analog scale (VAS) interviews were conducted first to familiarize participants with the health state descriptions and the concept of evaluating health states. The VAS exercise provided additional data to the TTO analysis for comparison and confirmation purposes, as well as valuing their own health at the time of analysis. The VAS method used a scale between 0 (worst health) and 100 (best health). Both TTO and VAS interviews were conducted using the health state descriptions in a randomized order in the general US population (without TED).16
Statistical Analysis
Data were analyzed in the statistical software environment CRAN R using the packages dplyr, tidyr, and ggpubr (Kurt Hornik, Friedrich Leisch).21 Continuous variables (TTO scores and VAS scores by health state and the interviewee’s own health) were analyzed descriptively, and the sample size, mean, median, SD, SE, and 95% CIs were presented for each variable. Histograms of continuous variables were developed to visually represent the distribution of each variable. A Shapiro-Wilk test was performed to assess distribution of each variable and determine the optimal test for significance (paired t test for normal data or Kruskal-Wallis test for nonnormal data).
The Kruskal-Wallis test was used to determine the presence of overall significant difference between utility values of multiple health states (2-sided P value; cutoff .05 for significance). A pairwise Wilcoxon rank sum test assessed utility values and VAS scores to determine whether individual health states differed (2-sided P value). P values were not adjusted to multiple comparisons. Exploratory subgroup analyses were conducted using a Kruskal-Wallis test if the subpopulation sample size was greater than 25, to determine the differences across health states or between multiple subgroups.
A weighted analysis was performed to test whether differing proportions of health states would affect the results and whether utility values in this study are generalizable to the US TED population. Because the prevalence of these health states within TED is unknown, we estimated the percentage of each health state at baseline from the 2 trials.13,14
Results
Participant Baseline Characteristics
A total of 111 participants (pilot, n = 10; main study, n = 101) completed the TTO interviews. The largest proportion of participants were 55 to 64 years old (47 [42.0%]), female individuals (75 [68.0%]), wore glasses (90 [81.0%]), and 46 (41%) self-identified as having received a visual impairment diagnosis, including near or farsightedness (19 [17.0%]). Participants from the following race and ethnicity groups were included: 4 Asian (3.6%), 11 Black or African American (9.9%), 4 Hispanic (3.6%), and 92 White (82.9%). Some characteristics differed from the aggregate US population, such as older age, higher percentage of female individuals, lower income level, and higher percentage of visual impairment; however, these differences more closely resembled those reported in the US TED population (eTable 1 in Supplement 1).12,13,14
Utility Values
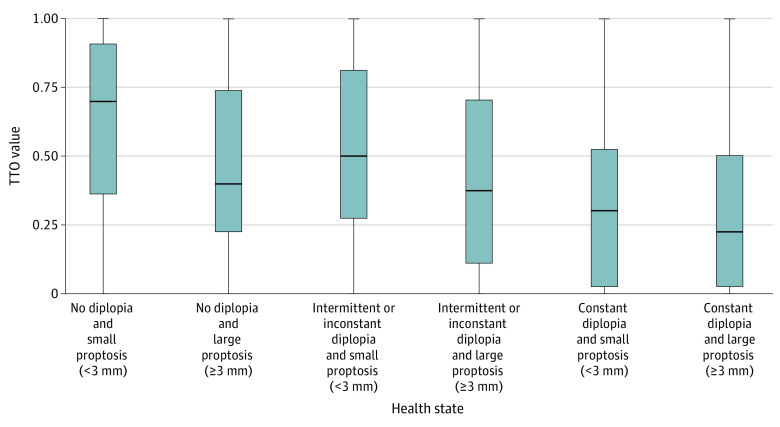
Overall, mean utility values were found to decrease with increasing severity of the health states (Box). As would be expected, the highest mean utility values (least association with QoL) were reported for the least severe health state of no diplopia and small proptosis (0.60; 95% CI, 0.54-0.67) (Table 1). However, a smaller decrease in utility was detected when the severity of proptosis remained constant, and there was minimal change in those with lower diplopia states (ie, no diplopia or intermittent/inconstant diplopia) as highlighted by overlapping CIs in an analysis of variability and central tendency shown in the Figure. The lowest (worse) mean utility value was observed in the most severe disease state (constant diplopia/large proptosis) with 0.30 (95% CI, 0.24-0.36), followed by constant diplopia/small proptosis (0.34; 95% CI, 0.29-0.40), intermittent or inconstant diplopia/large proptosis (0.43; 95% CI, 0.36-0.49), no diplopia/large proptosis (0.46; 95% CI, 0.40-0.52), and intermittent or inconstant diplopia/small proptosis (0.52; 95% CI, 0.45-0.58).
Table 1. Utility Values for Each Health Statea.
| Health state | Total No. of respondents | Mean (SD) | Median | 95% CI | IQR |
|---|---|---|---|---|---|
| No diplopia and small proptosis | 111 | 0.60 (0.34) | 0.70 | 0.54-0.67 | 0.36-0.91 |
| No diplopia and large proptosis | 111 | 0.46 (0.32) | 0.40 | 0.40-0.52 | 0.22-0.73 |
| Intermittent or inconstant diplopia and small proptosis | 111 | 0.52 (0.33) | 0.50 | 0.45-0.58 | 0.28-0.81 |
| Intermittent or inconstant diplopia and large proptosis | 111 | 0.43 (0.33) | 0.38 | 0.36-0.49 | 0.11-0.70 |
| Constant diplopia and small proptosis | 111 | 0.34 (0.31) | 0.30 | 0.29-0.40 | 0.03-0.53 |
| Constant diplopia and large proptosis | 111 | 0.30 (0.31) | 0.23 | 0.24-0.36 | 0.03-0.5 |
| Average TED utility value | 111 | 0.44 (0.34) | 0.40 | 0.42-0.47 | NA |
Abbreviations: NA, not applicable; TED, thyroid eye disease.
Scores rounded to 2 decimal places.
Figure. Distribution of Utility Values by Health State.
Figure displays median Q1, Q3. TTO indicates time trade-off.
Differences Between Health States
The pairwise Wilcoxon rank sum test indicated significant differences in utility values in 9 of 15 possible health state comparisons (Table 2). The other 6 comparisons were neighboring health states with small incremental differences in disease severity, with 1 comparison (intermittent/inconstant with small proptosis vs no diplopia/small proptosis) approaching significance. The weighted analysis of utility values produced a very similar utility value (0.45) to the mean (SD) utility value calculated in this study of 0.44 (0.34) (Table 3).
Table 2. Overview of Significance Between Health Statesa.
| Health state | No diplopia and small proptosis | No diplopia and large proptosis ptosis | Intermittent or inconstant diplopia and small proptosis | Intermittent or inconstant diplopia and large proptosis | Constant diplopia and small proptosis |
|---|---|---|---|---|---|
| No diplopia and large proptosis | .001 | NA | NA | NA | NA |
| Intermittent or inconstant diplopia and small proptosis | .053 | .21 | NA | NA | NA |
| Intermittent or inconstant diplopia and large proptosis | <.001 | .40 | .053 | NA | NA |
| Constant diplopia and small proptosis | <.001 | .001 | <.001 | .10 | NA |
| Constant diplopia and large proptosis | <.001 | <.001 | <.001 | <.001 | .27 |
Abbreviation: NA, not applicable.
Utility values from Table 1 were compared.
Table 3. Weighted Analysis of Utility Values by Health State.
| Health state | Total No. of respondents | % Samplea | Weighted utility score |
|---|---|---|---|
| No diplopia and small proptosis | 22 | 12.9 | 0.080 |
| No diplopia and large proptosis | 24 | 14 | 0.064 |
| Intermittent or inconstant diplopia and small proptosis | 33 | 19.3 | 0.099 |
| Intermittent or inconstant diplopia and large proptosis | 57 | 33.3 | 0.142 |
| Constant diplopia and small proptosis | 14 | 8.2 | 0.028 |
| Constant diplopia and large proptosis | 21 | 12.3 | 0.037 |
| Average weighted utility value | 171 | 100 | 0.45 |
Health state percentages taken from the 2 randomized trials.7
Analysis of Subpopulations
Most subgroups large enough to test (ie, n >25) demonstrated an overall significant difference between health states (Kruskal-Wallace test). Using the no diplopia/small proptosis health state, these included participants aged 55 to 64 years (mean [SD], 0.65 [0.34]; 95% CI, 0.03-1.00); female individuals (mean [SD], 0.61 [0.34], 95% CI, 0-1.00); male individuals (mean [SD], 0.59 [0.34], 95% CI, 0.03-1.00); White race (mean [SD], 0.64 [0.31]; 95% CI, 0.03-1.00); working full-time (mean [SD], 0.53 [0.34]; 95% CI, 0.03-1.00); eyeglass wearers (mean [SD], 0.61 [0.35]; 95% CI, 0-1.00); individuals with visual impairment (mean [SD], 0.59 [0.34]; 95% CI, 0-1.00); those without visual impairment (mean [SD], 0.61 [0.33], 95% CI, 0-1.00); those who previously smoked (mean [SD], 0.61 [0.32], 95% CI, 0-1.00); and those who never smoked (mean [SD], 0.60-0.35; 95% CI, 0-1.00) (eTables 2-10 in Supplement 1).
Results From the VAS Exercise
As with utility values, highest and lowest VAS scores were associated with no diplopia/small proptosis (51.71; 95% CI, 47.67-55.74) and constant diplopia/large proptosis (27.42; 95% CI, 24.41-30.44), respectively (Table 4).
Table 4. Visual Analog Scale (VAS) Scores for Each Health State (n = 111)a.
| Health state | Mean (SD) | Median (95% CI) |
|---|---|---|
| No diplopia and small proptosis | 51.71 (21.44) | 50.00 (47.67-55.74) |
| No diplopia and large proptosis | 38.95 (17.63) | 40.00 (35.64-42.27) |
| Intermittent or inconstant diplopia and small proptosis | 45.38 (17.74) | 45.00 (42.04-48.72) |
| Intermittent or inconstant diplopia and large proptosis | 36.52 (18.14) | 35.00 (33.11-39.94) |
| Constant diplopia and small proptosis | 30.56 (17.83) | 25.00 (27.20-33.91) |
| Constant diplopia and large proptosis | 27.42 (16.04) | 25.00 (24.41-30.44) |
| Average VAS score | 38.41 (19.94) | 40.00 (36.90-39.94) |
| Own health | 77.64 (80.00) | 1.54 (74.59-80.69) |
Scores rounded to 2 decimal places; 0 = worst health; 100 = perfect health.
Differences in VAS scores were found within the constant diplopia and large proptosis health state, when participants in the highest quartile (80.69) for their own health score were compared with those in the lowest quartile (74.59) (lowest quartile mean = 21.59 vs highest quartile mean = 33.61; P = .01).
There was no difference between own health VAS scores (mean [SD], 77.64 [80.00]) and VAS scores for the US general population (mean [SD], 80.4 [not reported]; 95% CI, 74.59-80.69; P = .08), supporting the hypothesis that the population interviewed was similar in general health to the overall population.22 Differences existed between TED health state VAS scores and the mean VAS score for the US general public across all health states (eTable 11 in Supplement 1). This emphasizes the disutility associated with the TED health states. The mean (SD) VAS score (when converted to the utility scale) was 0.38 (.20) vs an average mean (SD) utility value of 0.44 (.34).
Discussion
To our knowledge, based on a thorough literature search (eAppendix 3 in Supplement 1), this was the first study validating health states of moderate-severe TED and assessing utility values from the US general population using the TTO approach. Rationale for using the general population to value health states in TED derives from an assumption that these individuals harbor no investment in the disease, unlike those with TED. Patient valuation could potentially bias study results because these individuals could adapt to their health state over time and therefore assign higher values to their own health state.18 These higher values may be associated with patients developing coping mechanisms, allowing for improved functioning in daily activities.17 Further, ethical concerns regarding patient valuation of health states may arise given the potential for emotional distress provoked by imagining hypothetical situations that they are unable to experience.23
Each TTO exercise followed the standard Measurement and Valuation of Health protocol, which is one of the most widely adopted techniques for TTO valuation and was used by EuroQol for the valuation of the EQ-5D-3L questionnaire.15 It is acknowledged that EuroQoL has introduced another protocol, the EuroQoL Valuation Technology (EQ-VT), which includes a discrete choice component. Although utilities for quality-adjusted life-year calculations cannot be generated from discrete choice as a stand-alone technique, this represents an alternative approach to the complementary VAS scoring used in this study.15 The EQ-VT was deemed to be more difficult to administer due to the time required to complete and keep interviewees engaged during the peak of the COVID-19 lockdown.
The mean utility value derived across these 6 health states of patients with active, moderate-severe TED was 0.44. This indicates a substantial level of disutility as compared with the value of 0.88 found in a study investigating QoL in hyperthyroid Graves disease and a chronic, mild TED subgroup.24 These utility values highlight the substantial impact TED imposes when compared with the US general population (0.85).22 Further, this mean utility value was nearly identical to that calculated with a weighted analysis using proportions of these health states found in 2 controlled trials. Results found here might thus be validly generalized to the population with active, moderate-severe TED.12
The calculated overall utility value in this study (0.44) allows contextualizing the results to other diseases. It is similar to or lower (worse) than values reported for several severely debilitating conditions, such as blindness with no light perception (0.26; CI, 0.19-0.33), noninfectious uveitis (median, 0.975; IQR, 0.8-1.0), and age-related macular degeneration (mean, 0.81; 95% CI, 0.76-0.86) (all comparisons used the TTO methodology).25,26,27 This congruence highlights the severe burden moderate-severe active TED places on patients as perceived by an unbiased unaffected population.
Severity of proptosis and diplopia emerged as the key variables associated with utility values for the 6 health states studied here. These values decreased (worsened) as severity of diplopia increased; however, the decrement in those health states with large proptosis and milder diplopia was more modest. Both the presence of large proptosis and constant diplopia drove health state scores lower. Constant diplopia appears to produce a floor effect because scores clustered at their lowest when present in a health state, regardless of proptosis magnitude. This finding underscores the particular burden imposed by both large proptosis and constant diplopia.
No major differences emerged from 6 comparisons of the mostly neighboring middle health states. This may relate to a general similarity of association observed in these health states with daily life or our inability to discriminate differences. For instance, changes from intermittent/inconstant diplopia to no diplopia may be difficult to detect, thus resulting in only small utility value changes. As observed, moderate-severe TED health states were associated with worse utility values. This finding highlights the need for further identification of each health state characteristics having the greatest association with QoL. Furthermore, ongoing studies are attempting to bridge and validate these utility findings with the Graves Orbitopathy-Specific Quality of Life (GO-QOL) questionnaire, a specific TED QoL instrument.
Limitations
This study had some limitations. Despite best recruitment efforts, our cohort was older and included more women and more individuals with visual impairment than the US general population. However, the differences in our sample more closely approximated the known demographic characteristics of the US TED population.28 These differences serendipitously increased our confidence in the findings emanating from the interviewed population.
Although TED persists throughout life, the fixed time interval of 10 years used for health state assessment in this TTO may not represent a large subset of patients with active disease whose inflammatory symptoms are shorter lived. Primary progressive symptoms driving disutility identified here (proptosis and diplopia) can persist for extended time periods with variable severity over a lifetime, as was assessed here. Further, the 10-year time horizon is recommended by Health Technology Assessment as facilitating comparisons across treatments and diseases, despite very different patterns of disease manifestations.15,20 The TED health state descriptions studied here were based on patients with highly active, moderate-severe disease and thus may not represent individuals with milder or less active disease.
Conclusions
Results of this qualitative study suggest that patients with moderate-severe, active TED may have substantial disutility. The association of TED with negative QoL has been well documented; however, using the unbiased TTO method in a general US population to assess this association (health score utility scoring) is novel, to the best of our knowledge. The results suggest that utility values decrease with increasing severity of TED symptoms as is reflected by the presence of diplopia and/or proptosis in 6 different health states. Substantial differences were found between nonneighboring health states and in certain subpopulations. These very low utility values suggest the substantial QoL burden potentially confronting patients with TED and highlight the need for additional studies in this area. These data might now serve as baseline for prospectively assessing improvements (utility gains) with therapies.
eFigure. Health State Development and Validation Process
eTable 1. Demographic Characteristics of the Study Population (n=111)
eTable 2. Utility Values for Each Health State by Ethnicity
eTable 3. Utility Values for Each Health State by Annual Household Income
eTable 4. Utility Values for Each Health State in Participants With or Without Glasses
eTable 5. Utility Values for Each Health State by Employment Status
eTable 6. Utility Values for Each Health State by Age
eTable 7. Utility Values for Each Health State by Vision Impairment Diagnosis
eTable 8. Utility Values for Each Health State by Smoking Status
eTable 9. Utility Values for Each Health State by Gender
eTable 10. Utility Values for Each Health State by Education Level
eTable 11. Comparison of VAS Scores for Each Health State vs US General Population VAS
eAppendix 1. Interview Guide Example Questions
eAppendix 2. Large Proptosis and Constant Diplopia Description With Pictures
eAppendix 3. Literature Search
eReferences
Data Sharing Statement
Footnotes
In order of increasing severity.
Abbreviation: TED, thyroid eye disease.
References
- 1.Lazarus JH. Epidemiology of Graves’ orbitopathy (GO) and relationship with thyroid disease. Best Pract Res Clin Endocrinol Metab. 2012;26(3):273-279. doi: 10.1016/j.beem.2011.10.005 [DOI] [PubMed] [Google Scholar]
- 2.Hyman L, Penne R, Fujino D, et al. Prevalence and associated factors for thyroid eye disease (TED) in the AAO IRIS registry. Invest Ophthalmol Vis Sci. 2020;61(7):5425. [Google Scholar]
- 3.Sikder S, Weinberg RS. Thyroid eye disease: pathogenesis and treatment. Ophthalmologica. 2010;224(4):199-203. doi: 10.1159/000260224 [DOI] [PubMed] [Google Scholar]
- 4.Manji N, Carr-Smith JD, Boelaert K, et al. Influences of age, gender, smoking, and family history on autoimmune thyroid disease phenotype. J Clin Endocrinol Metab. 2006;91(12):4873-4880. doi: 10.1210/jc.2006-1402 [DOI] [PubMed] [Google Scholar]
- 5.Bahn RS. Graves’ ophthalmopathy. N Engl J Med. 2010;362(8):726-738. doi: 10.1056/NEJMra0905750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang Y, Padnick-Silver L, Francis-Sedlak M, Holt RJ, Foley C, Douglas RS. Inflammatory and noninflammatory thyroid eye disease: comparison of disease signs, symptoms, and quality of life in US patients. Endocr Pract. 2022;28(9):842-846. doi: 10.1016/j.eprac.2022.06.003 [DOI] [PubMed] [Google Scholar]
- 7.Cook LD. Oxford handbook of ophthalmology. J Neuroophthalmol. 2009;29(1):81-82. doi: 10.1097/01.wno.0000347033.35456.80 [DOI] [Google Scholar]
- 8.Egle UT, Kahaly GJ, Petrak F, et al. The relevance of physical and psychosocial factors for the quality of life in patients with thyroid-associated orbitopathy (TAO). Exp Clin Endocrinol Diabetes. 1999;107(suppl 5):S168-S171. doi: 10.1055/s-0029-1212177 [DOI] [PubMed] [Google Scholar]
- 9.Ponto KA, Pitz S, Pfeiffer N, Hommel G, Weber MM, Kahaly GJ. Quality of life and occupational disability in endocrine orbitopathy. Dtsch Arztebl Int. 2009;106(17):283-289. doi: 10.3238/arztebl.2009.0283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Farid M, Roch-Levecq A-C, Levi L, Brody BL, Granet DB, Kikkawa DO. Psychological disturbance in graves ophthalmopathy. Arch Ophthalmol. 2005;123(4):491-496. doi: 10.1001/archopht.123.4.491 [DOI] [PubMed] [Google Scholar]
- 11.Kahaly GJ, Hardt J, Petrak F, Egle UT. Psychosocial factors in subjects with thyroid-associated ophthalmopathy. Thyroid. 2002;12(3):237-239. doi: 10.1089/105072502753600205 [DOI] [PubMed] [Google Scholar]
- 12.Kahaly GJ, Douglas RS, Holt RJ, Sile S, Smith TJ. Teprotumumab for patients with active thyroid eye disease: a pooled data analysis, subgroup analyses, and off-treatment follow-up results from 2 randomised, double-masked, placebo-controlled, multicentre trials. Lancet Diabetes Endocrinol. 2021;9(6):360-372. doi: 10.1016/S2213-8587(21)00056-5 [DOI] [PubMed] [Google Scholar]
- 13.Douglas RS, Kahaly GJ, Patel A, et al. Teprotumumab for the treatment of active thyroid eye disease. N Engl J Med. 2020;382(4):341-352. doi: 10.1056/NEJMoa1910434 [DOI] [PubMed] [Google Scholar]
- 14.Smith TJ, Kahaly GJ, Ezra DG, et al. Teprotumumab for thyroid-associated ophthalmopathy. N Engl J Med. 2017;376(18):1748-1761. doi: 10.1056/NEJMoa1614949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oppe M, Rand-Hendriksen K, Shah K, Ramos-Goñi JM, Luo N. EuroQol protocols for time trade-off valuation of health outcomes. Pharmacoeconomics. 2016;34(10):993-1004. doi: 10.1007/s40273-016-0404-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gudex C. Time Trade-off User Manual: Props and Self-Completion Methods. Centre for Health Economics University of York; 1994. [Google Scholar]
- 17.Tolley K. What are health utilities? Accessed June 1, 2021. http://www.bandolier.org.uk/painres/download/What%20is%202009/What_are_health_util.pdf
- 18.Whitehead SJ, Ali S. Health outcomes in economic evaluation: the QALY and utilities. Br Med Bull. 2010;96(1):5-21. doi: 10.1093/bmb/ldq033 [DOI] [PubMed] [Google Scholar]
- 19.Dolan P. Modeling valuations for EuroQol health states. Med Care. 1997;35(11):1095-1108. doi: 10.1097/00005650-199711000-00002 [DOI] [PubMed] [Google Scholar]
- 20.Brazier J, Rowen D. NICE decision support unit technical support documents. In: NICE DSU Technical Support Document 11: Alternatives to EQ-5D for Generating Health State Utility Values. National Institute for Health and Care Excellence (NICE); 2011. [PubMed] [Google Scholar]
- 21.R Core Team . The R project for statistical computing. Accessed June 1, 2021. http://www.R-project.org/
- 22.Jiang R, Janssen MFB, Pickard AS. US population norms for the EQ-5D-5L and comparison of norms from face-to-face and online samples. Qual Life Res. 2021;30(3):803-816. doi: 10.1007/s11136-020-02650-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brazier J, Rowen D, Karimi M, Peasgood T, Tsuchiya A, Ratcliffe J. Experience-based utility and own health state valuation for a health state classification system: why and how to do it. Eur J Health Econ. 2018;19(6):881-891. doi: 10.1007/s10198-017-0931-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mladenovic M, Buchberger M, Qerimi V, Puntscher S, Siebert U, Rochau U. Health state utilities in individuals with goiter, hypothyroidism, hyperthyroidism and Graves’ disease as an example for thyroid disorders: a systematic review. Value Health. 2017;20(9):A483. doi: 10.1016/j.jval.2017.08.479 [DOI] [Google Scholar]
- 25.Brown GC, Sharma S, Brown MM, Kistler J. Utility values and age-related macular degeneration. Arch Ophthalmol. 2000;118(1):47-51. doi: 10.1001/archopht.118.1.47 [DOI] [PubMed] [Google Scholar]
- 26.Brown MM, Brown GC, Sharma S, Kistler J, Brown H. Utility values associated with blindness in an adult population. Br J Ophthalmol. 2001;85(3):327-331. doi: 10.1136/bjo.85.3.327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Niemeyer KM, Gonzales JA, Doan T, Browne EN, Rao MM, Acharya NR. Time trade-off utility values in noninfectious uveitis. Am J Ophthalmol. 2019;208:47-55. doi: 10.1016/j.ajo.2019.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang Y, Sharma A, Padnick-Silver L, et al. Trends in treatment of active, moderate-to-severe thyroid eye disease in the US. J Endocr Soc. 2020;4(12):bvaa140. doi: 10.1210/jendso/bvaa140 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure. Health State Development and Validation Process
eTable 1. Demographic Characteristics of the Study Population (n=111)
eTable 2. Utility Values for Each Health State by Ethnicity
eTable 3. Utility Values for Each Health State by Annual Household Income
eTable 4. Utility Values for Each Health State in Participants With or Without Glasses
eTable 5. Utility Values for Each Health State by Employment Status
eTable 6. Utility Values for Each Health State by Age
eTable 7. Utility Values for Each Health State by Vision Impairment Diagnosis
eTable 8. Utility Values for Each Health State by Smoking Status
eTable 9. Utility Values for Each Health State by Gender
eTable 10. Utility Values for Each Health State by Education Level
eTable 11. Comparison of VAS Scores for Each Health State vs US General Population VAS
eAppendix 1. Interview Guide Example Questions
eAppendix 2. Large Proptosis and Constant Diplopia Description With Pictures
eAppendix 3. Literature Search
eReferences
Data Sharing Statement