Abstract
This case-control study uses a radiotracer and positron emission tomography to assess N-methyl-d-aspartate receptor (NMDAR) density changes during recovery from NMDAR-antibody encephalitis.
N-methyl-d-aspartate receptor (NMDAR) autoantibodies are a common cause of autoimmune encephalitis.1 In vitro and animal studies indicated that NMDAR internalization is a major mechanism underlying NMDAR-antibody encephalitis,2 but direct support in humans is limited to a reduction of NMDAR staining in postmortem hippocampi.2,3
Methods
In this case-control study, we performed cross-sectional resting-state positron emission tomography (PET) of NMDARs in vivo using radioligand [18F]GE-179, which binds within the ion channel of open, activated NMDARs. We included 5 patients recovering from definite NMDAR-antibody encephalitis1 (eTable in the Supplement) and 29 healthy volunteers (HVs) who took no medications that interfere with NMDARs and underwent PET–magnetic resonance scanning. Four patients with NMDAR-antibody encephalitis had persistent GluN1 autoantibodies in serum and mild symptoms, were scanned 2 to 8 months after discharge, and were classified as persistently seropositive. One patient had undetectable serum GluN1 antibodies, was scanned 16 months after discharge, and was classified as seroreverted. The study was reviewed and approved by the local ethical committees, and all participants gave written informed consent. The study followed the STROBE reporting guideline.
From preprocessed data,4 we used [18F]GE-179 total volume of distribution (VT) to quantify open, activated NMDAR density. We assessed gray matter atrophy using magnetic resonance voxel-based morphometry and compared regional and voxelwise data using a general linear model adjusting for age, sex, and site. A cluster-level voxelwise P < .05 corrected for multiple comparisons (pFWE) was considered significant. SPM, version 12 (UCL Queen Square Institute of Neurology) and SPSS, version 27 (IBM) were used for statistical analyses.
Results
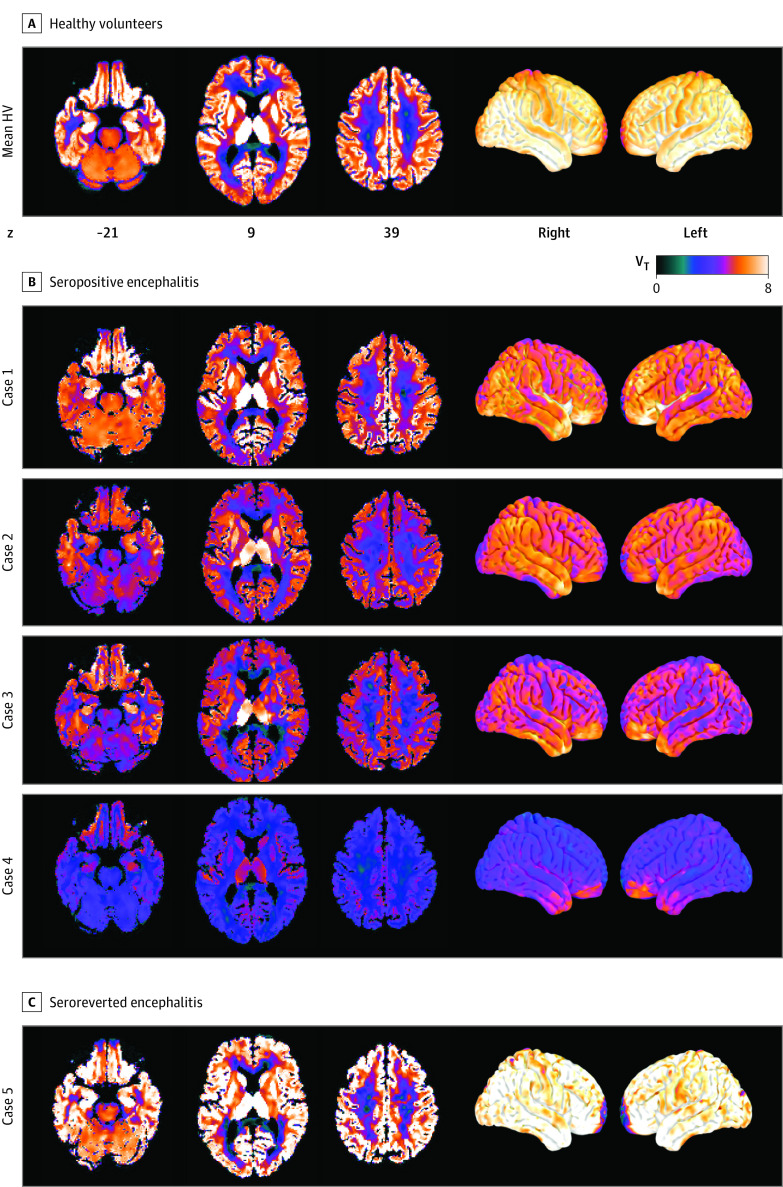
The sample comprised 4 seropositive cases (all women; mean [SD] age, 28 [6] years), 1 seroreverted case (female aged 25-30 years), and 29 HVs (21 [72%] men; 8 [28%] women; mean [SD] age, 41 [13] years). Seropositive cases 1 to 4 had lower gray matter VT (estimated marginal mean, 6.2; 95% CI, 4.4-8.0) compared with HVs (mean, 8.8; 95% CI, 8.1-9.4; F = 6.5; P = .02) and the seroreverted case 5 (9.7) (Figure). Voxel-based analysis showed reduced VT in seropositive cases within bilateral anterior temporal lobes (left: t = 4.5, pFWE = 0.02; right: t = 4.9, pFWE = 0.05) and a large cluster involving bilateral superior parietal lobes, paracentral lobules, left posterior cingulate gyrus, and left precuneus (t = 5.8; pFWE < .001). Volume-of-interest analyses corroborated regional VT reductions in seropositive temporal (34% reduction; F = 8.3; P = .008) and parietal (31% reduction; F = 7.3; P = .01) lobes and mesial temporal region (40% reduction; F = 8.9; P = .006).
Figure. Radioligand [18F]GE-179 Uptake in Autoantibody Seropositive or Seroreverted Patients With N-Methyl-d-Aspartate Receptor (NMDAR)-Antibody Encephalitis and Healthy Volunteers (HVs).
The figure shows the spatial distributions of [18F]GE-179 total volume of distribution (VT) on brain slices and surface projections.
Gray matter VT was not associated with higher serum GluN1 antibody levels, shorter time since discharge and episode onset, cognition at the time of scanning, or symptom severity at discharge. Areas of decreased gray matter volume in cerebellar hemispheres and regions with significantly reduced VT did not overlap.
Discussion
We found a mean 30% regional reduction in the density of open, active NMDARs, most prominently in anterior temporal and superior parietal cortices, in patients with persisting serum GluN1 autoantibodies recovering from NMDAR-antibody encephalitis. Patients had mild cognitive symptoms, indicating the considerable compensatory capacity of the brain. In contrast, a recovered, seroreverted patient had slightly elevated NMDAR density, indicating a rebound of NMDAR function.
NMDAR hypofunction has been observed in patients with depression5 or first-episode psychosis.6 Our results are not explained by brain atrophy or perfusion.4 The potential of [18F]GE-179 PET as a biomarker for NMDAR-antibody encephalitis severity and recovery should be further evaluated.
Limitations include the small sample size; different age and sex distributions among participants; and lack of intrathecal GluN1 autoantibody titers on scanning day, detailed cognitive testing, and a comparison group with other inflammatory or encephalopathic central nervous system diseases. Findings may be more prominent during the acute phase vs recovery, but logistical barriers exist to scanning patients with severe disease. Our study supports the hypothesis of NMDAR internalization and indicates involvement of large cortical areas beyond the limbic system.
eTable. Characteristics of Patients With N-Methyl-d-Aspartate Receptor-Antibody Encephalitis
References
- 1.Graus F, Titulaer MJ, Balu R, et al. A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol. 2016;15(4):391-404. doi: 10.1016/S1474-4422(15)00401-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hughes EG, Peng X, Gleichman AJ, et al. Cellular and synaptic mechanisms of anti-NMDA receptor encephalitis. J Neurosci. 2010;30(17):5866-5875. doi: 10.1523/JNEUROSCI.0167-10.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zrzavy T, Endmayr V, Bauer J, et al. Neuropathological variability within a spectrum of NMDAR-encephalitis. Ann Neurol. 2021;90(5):725-737. doi: 10.1002/ana.26223 [DOI] [PubMed] [Google Scholar]
- 4.Galovic M, Erlandsson K, Fryer TD, et al. ; NEST investigators . Validation of a combined image derived input function and venous sampling approach for the quantification of [18F]GE-179 PET binding in the brain. Neuroimage. 2021;237:118194. doi: 10.1016/j.neuroimage.2021.118194 [DOI] [PubMed] [Google Scholar]
- 5.McGinnity CJ, Koepp MJ, Hammers A, et al. NMDA receptor binding in focal epilepsies. J Neurol Neurosurg Psychiatry. 2015;86(10):1150-1157. doi: 10.1136/jnnp-2014-309897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beck K, Arumuham A, Veronese M, et al. N-methyl-D-aspartate receptor availability in first-episode psychosis: a PET-MR brain imaging study. Transl Psychiatry. 2021;11(1):425. doi: 10.1038/s41398-021-01540-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Characteristics of Patients With N-Methyl-d-Aspartate Receptor-Antibody Encephalitis