Abstract
Background
Older people living with HIV (PLWH) are at increased risks of co-morbidities and polypharmacy. However, little is known about factors affecting their needs and concerns about medicines. This systematic review aims to describe these and to identify interventions to improve medicine optimisation outcomes in older PLWH.
Methods and Data Sources
Multiple databases and grey literature were searched from inception to February 2022 including MEDLINE, CINAHL, PsycInfo, PsychArticles, the Cochrane Database of Systematic Reviews and the Cochrane Controlled Register of Trials, Abstracts in Social Gerontology, and Academic Search Complete.
Eligibility Criteria
Studies reporting interventions/issues affecting older PLWH (sample populations with mean/median age ≥ 50 years; any aspect of medicine optimisation, or concerns). Quality assessments were completed by means of critical appraisal checklists for each study design. Title and abstract screening was led by one reviewer and a sample reviewed independently by two reviewers. Full-paper reviews were completed by one author and a 20% sample was reviewed independently by two reviewers.
Synthesis
Data were extracted by three independent reviewers using standardised data extraction forms and synthesised according to outcomes or interventions reported. Data were summarised to include key themes, outcomes or concerns, and summary of intervention.
Results
Seventy-nine (n = 79) studies met the eligibility criteria, most of which originated from the USA (n = 36). A few studies originated from Australia (n = 5), Canada (n = 5), Spain (n = 9), and the UK (n = 5). Ten studies originated from Sub-Saharan Africa (Kenya n = 1, South Africa n = 6, Tanzania n = 1, Uganda n = 1, Zimbabwe n = 1). The rest of the studies were from China (n = 1), France (n = 1), Germany (n = 1), Italy (n = 1), the Netherlands (n = 1), Pakistan (n = 1), Switzerland (n = 1), Saudi Arabia (n = 1) and Ukraine (n = 1). Publication dates ranged from 2002 to 2022. Sample sizes ranged from 10 to 15,602 across studies. The factors affecting older PLWH’s experience of and issues with medicines were co-morbidities, health-related quality of life, polypharmacy, drug interactions, adverse drug reactions, adherence, medicine burden, treatment burden, stigma, social support, and patient-healthcare provider relationships. Nine interventions were identified to target older persons, five aimed at improving medication adherence, two to reduce drug interactions, and two for medicine self-management initiatives.
Conclusion
Further in-depth research is needed to understand older PLWH’s experiences of medicines and their priority issues. Adherence-focused interventions are predominant, but there is a scarcity of interventions aimed at improving medicine experiences for this population. Multi-faceted interventions are needed to achieve medicine optimisation outcomes for PLWH.
Trial Registration
This study is registered with PROSPERO registration number: CRD42020188448.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40266-022-01003-3.
Key Points
| Older people living with HIV have various factors that impact on their needs and concerns about medicines (e.g., polypharmacy, treatment burden, adherence support, stigma, and social support). |
| Only a few interventions have been developed to improve medicines optimisation outcomes, but most of these are adherence-focussed. |
| There is a need for further studies to better understand the needs and concerns of older people living with HIV in the UK about their medicines and to design multi-faceted interventions to reflect these. |
Introduction
Globally, about 38 million people continue to live with HIV [1]. Advances in treatment have transformed HIV into a complex chronic condition [2] and more people living with HIV (PLWH) have a near-normal life expectancy [3]. New diagnoses among PLWH over the age of 50 years are on the rise [4]. In the UK, nearly two-thirds (65%) of late HIV diagnoses were among those aged ≥ 65 years [5]. It is estimated that by 2030 nearly 75% of all PLWH will be 50 years or older, with the median age expected to increase gradually over the years [6]. A number of age cut-offs have been used to define older PLWH, ranging from 45 to 55 years old with 50 years and older used frequently across most literature [4, 7, 8]. For the purposes of this review, an ‘older person’ will include anyone aged 50 years or older.
Ageing within the context of HIV is associated with multimorbidity and polypharmacy [9, 10]. Polypharmacy has widely been defined as the use of five or more medicines, [11] and is linked to adverse health outcomes [12]. A recent multinational patient survey conducted in 24 countries including North America, Europe, Australia and China (n = 2112), reported a significantly higher level of polypharmacy among older PLWH (54.6%) compared with younger participants (36.5%, p < 0.001) [10]. The survey also found that people experiencing polypharmacy used an average of 6.5 pills per day, and willingness to change antiretroviral (ARV) regimens to those with a fewer number of medicines was significantly higher among older adults (79.9%) than those under 50 years old (70.1%, p < 0.001) [10]. An earlier study on older PLWH found that participants were taking a median of 13 (range 9–17) medicines, of which eight (range 4–14) were non-ARV medicines [13]. Polypharmacy is associated with regimen complexity, medicine burden, lower treatment satisfaction, potential drug–drug interactions (PDDIs), adverse drug reactions (ADRs), hospitalisation, non-adherence, and contributes to poor health outcomes [9, 10, 12, 14, 15]. A study investigating polypharmacy among PLWH found a correlation between the number of non-ARV medicines used and adverse health outcomes in older individuals [15]. There is a need to understand treatment experiences of older PLWH.
NICE guidelines define medicines optimisation, as “a person-centred approach to safe and effective medicines use, to ensure people obtain the best possible outcomes from their medicines”, which is fundamental in tackling the challenges presented by polypharmacy among older adults [16]. Medicine experiences are the summation of events involving drug therapy that one has encountered in their lives [17]. According to the UK’s Royal Pharmaceutical Society, medicines optimisation aims to understand patients’ experiences and to improve patient outcomes from a holistic perspective [18]. Across the literature, medicines optimisation is implemented through various interventions including medicine reviews [19], deprescribing [14], medicine reconciliations [11, 19], identifying potentially inappropriate prescribing (PIP) [19, 20], providing social support, and increasing antiretroviral therapy (ART) adherence [11]. A recent systematic review of interventions for frail older persons focused on medicines optimisation in secondary care settings [21], but was not specific to PLWH. Moreover, little is known about medicines optimisation interventions targeted at older PLWH. In some studies, older PLWH have reported concerns around stigma. Older PLWH may experience stigma twofold due to HIV-positive status and ageing [22]. It is therefore vital to understand the needs and concerns of older PLWH and to investigate interventions aimed at improving medicines optimisation outcomes for this population.
The aim of this review was to investigate medicines optimisation needs and interventions for older PLWH. The specific objectives were to determine: (a) the priority issues and concerns of older PLWH about their medicines, and (b) the types of medicines optimisation interventions developed for older PLWH, how they are implemented, and their effectiveness.
Methods
The systematic review was conducted and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines. The review was registered with the international Prospective Register of Systematic Reviews PROSPERO prior to data abstraction (CRD42020188448) [23].
Study Eligibility—Inclusion and Exclusion Criteria
We included various study designs, including but not limited to randomised, controlled trials (RCTs), before and after experimental studies (controlled and non-controlled), observational studies (cohort studies, case-control, cross-sectional surveys), qualitative research studies, and retrospective and prospective reviews of prescription and/or dispensing records. Case reports and case series were excluded regardless of age composition. Service evaluations and audits conducted to improve medicine-related outcomes in a specific health facility or organisation were excluded. We included studies composed of HIV-positive older adults as the main participants or where the vast majority of participants were of mean/median age 50 years or older. Studies focusing on other age groups besides older persons were excluded (i.e., children, adolescents and younger adults under the age of 50 years). Abstracts did not always report participants’ age, and therefore extra screening of full texts was done to determine if studies met the age eligibility criterion. For studies not reporting the mean/median age of participants within the abstract, the full text was reviewed to ascertain age composition of participants [see Online Supplementary Material (OSM): Appendix 1]. Studies of HIV-negative older adults were excluded from the review. Studies relating to any aspect of medicines optimisation, medicine reviews, medicine reconciliation, deprescribing, or strategies being undertaken to support older PLWH with safe and effective use of ART and/or non-HIV medicines were included. Studies that did not discuss any aspect of medicines optimisation or issues relating to medicines experience or that concerned older persons’ needs in relation to their medicines were also excluded. The search was limited to studies published in English.
Information Sources and Search Strategy
A range of electronic databases were searched from date of inception to February 2022. We searched MEDLINE, CINAHL, PsycInfo, PsychArticles, the Cochrane Database of Systematic Reviews, the Cochrane Controlled Register of Trials, Abstracts in Social Gerontology, and Academic Search Complete. We also searched grey literature via OpenGreyTM, including doctoral theses, research reports and other publications. We searched reference lists of included studies and relevant systematic reviews to identify additional studies. A digital referencing manager, Zotero (5.0.89), was used to manage all searches and to remove duplicates. To answer the research question, our Population Intervention Comparison Outcome (PICO) search strategy [24] included key words to maximise our ability to find relevant articles (OSM: Appendix 2). Examples of search terms used include: HIV, AIDS, ageing/aging, older/elderly, medicines, antiretrovirals, HAART/ART, optimis*, intervention, pharmaceutical, medicine-related problems, concerns, needs, issues, outcome. A full list of search terms is provided in the OSM (Appendix 3). The same search strategy was adapted for all databases, with minor changes to the wildcard symbols and truncations for searching different words with similar prefixes.
Selection of Studies
Titles were screened for eligibility by one author (PS). Abstracts and full texts were then independently reviewed by three authors (PS, RC, BK) using pre-specified screening criteria (OSM: Appendix 4). Each study was then categorised into: ‘definitely include’, ‘possibly include’ and ‘definitely exclude’. Full texts for all studies in the ‘definitely include’ and ‘possibly include’ categories were retrieved for assessment against eligibility criteria by PS and then a sample (20%) independently reviewed (RC, SC, BK) [25]. Disagreements at any stage of screening were resolved through discussions among the research team.
Data Extraction, Synthesis Methods, and Risk of Bias Assessment
Data from eligible articles were extracted using a standardised data extraction form (OSM: Appendix 5). One reviewer (PS) led data extraction and a sample of the results (20%) were independently reviewed by two reviewers (RC, SC). Discrepancies in data extracted were resolved by discussion and consensus among the research team.
Synthesis- research papers were categorised thematically (e.g., polypharmacy, treatment burden, medicine burden, adherence) and by the interventions reported (OSM: Appendix 5, Part 2).
The Critical Appraisal Skills Programme (CASP) checklist and the Appraisal tool for Cross-Sectional Studies (AXIS) were used to assess the risk of bias in and quality of the studies included in the final pool. Specific checklists were used as appropriate for each study design. Any disagreements were resolved through discussion with the team. Each question in the appraisal tool was graded as 1 or 0 for meeting or not meeting predefined criteria, respectively; scores and percentages were then calculated to assess overall quality. Overall, studies achieving 0–49% were defined as poor quality, 50–69% were fair quality and 70–100% were of excellent quality.
Results
Study Selection
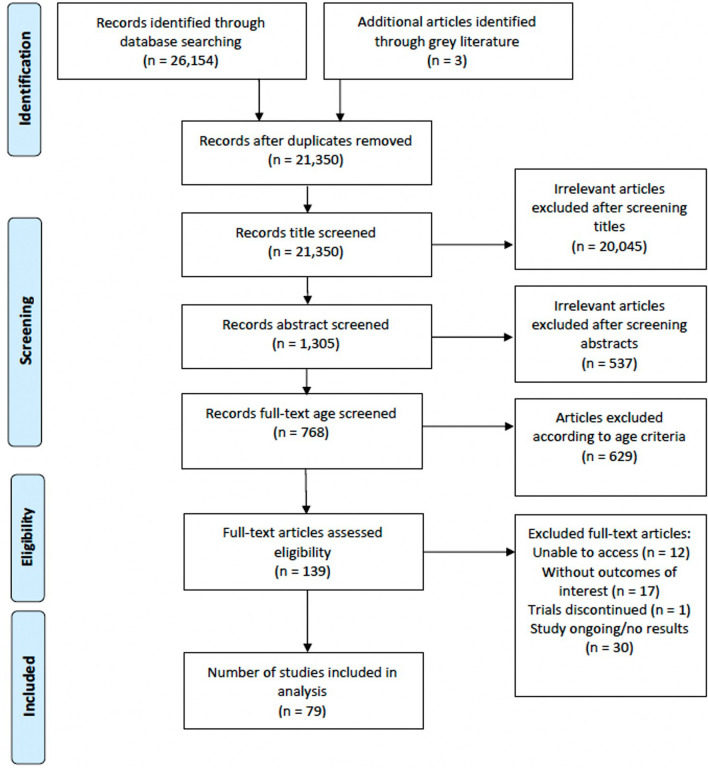
The search identified 26,154 articles from electronic databases and three articles from grey literature. After duplicate removal, 21,350 articles were title screened, of which 1305 were found to be eligible for abstract screening. Of the 1305 abstracts, 768 full texts were searched to determine whether they met the age criterion. 139 remaining articles were then assessed for other eligibility criteria, of which 60 articles were excluded due to either the study not having outcomes of interest (n = 17), the trial being discontinued (n = 1), incomplete study/no results (n = 30), and unable to access due to journal restrictions (n = 12). Overall, 79 (n = 79) studies were included in this review (Fig. 1).
Fig. 1.
PRISMA flow diagram of the systematic review
Study Characteristics
The review included 46 cross-sectional studies, 20 qualitative studies, five cohort studies, four RCTs, and four mixed-methods studies. Overall, all articles included were of excellent quality (70–100%). The mean score for the cross-sectional studies was 84% (range 73–90%) based on the AXIS quality assessments. Mean quality scores of 91% (range 70–100%), 91% and 79% (range 71–93%) were obtained for qualitative studies, RCTs and cohort studies, respectively.
The 79 studies that met the inclusion criteria were largely from the USA (n = 36). A few studies originated from Australia (n = 5), Canada (n = 5), Spain (n = 9) and the UK (n = 5). Ten studies originated from Sub-Saharan Africa (Kenya n = 1, South Africa n = 6, Tanzania n = 1, Uganda n = 1 and Zimbabwe n = 1). The rest of the studies were from China (n = 1), France (n = 1), Germany (n = 1), Italy (n = 1), the Netherlands (n = 1), Pakistan (n = 1), Switzerland (n = 1), Saudi Arabia (n = 1) and Ukraine (n = 1). Publication dates ranged from 2002 to 2022. Sample sizes ranged from 10 to 15,602 across individual studies.
Issues Affecting Older People Living with HIV (PLWH)
The studies reviewed showed a wide range of issues affecting older PLWH that impacted on their needs for and experiences of using medicines including co-morbidities, polypharmacy, drug interactions, adverse drug reactions, adherence, stigma, medicine burden, treatment burden, health-related quality of life (HRQOL), and patient and healthcare provider relationships (Table 1).
Table 1.
Characteristics of included studies
| First author, year (country) | Participant characteristics and study setting | Methods | Intervention reported or tools used for medicine optimisation | Key findings | Limitations |
|---|---|---|---|---|---|
| Ahmed et al., 2021 (Pakistan) [65] |
n = 602 32.9% > 50 years Hospital |
Participants were given a validated generic HRQOL questionnaire | EuroQol quality of life scale EQ-5D-3L and Visual Analogue Scale | 59.5% of participants reported no impairment in self-care, however, 63.1% were extremely anxious/depressed. Overall, the mean EQ-5D utility and Visual Analogue Scale scores were 0.388 (SD = 0.41) and 66.20 (SD = 17.22), respectively. Multiple regression analysis has shown that age over 50, the female gender, primary or secondary education, less than a year since HIV diagnosis, having a detectable viral load, and a longer time to ART were all factors significantly associated with HRQOL | The results cannot be generalised to non-adherent PLWH as participants who failed to show up regularly according to their dispensing records were excluded from the study. Moreover, the cross-sectional study design does not allow for causality analysis and there is a possibility of social desirability bias as participants are likely to under-report socially undesirable behaviours |
| Ventuneac et al., 2020 (USA) [53] |
n = 406 M = 50.7 Community |
Intervention study: This study consisted of a single-arm prospective study design with assessments at baseline and 6 months | Rango (mobile health application) | 95% of participants returned for a follow-up visit, with 59% (38/65) of those who were unsuppressed at baseline achieving viral suppression. Viral suppression among Rango participants and those receiving usual care were similar (p = 0.84) and increased in both groups at six months (p < 0.001). Significant difference in the number of unsuppressed participants (n = 65) at baseline who were suppressed (n = 38) at 6 months (p = 0.006) | The findings are limited by the short study duration and a lack of useability data. Usage changes were not analysed over the 6 months |
| Nguyen et al., 2018 (USA) [62] |
n = 176 M = 58.7 years (SD = 5.4) Community |
Data pertaining to HIV-positive participants was obtained from the 2012 baseline cohort from the Research Core of the Rush Centre of Excellence on Disparities in HIV and Aging | The CESD-10, the 30-item MMSE, the 5-item De Jong-Gierveld Loneliness Scale, and the Everyday Discrimination Scale | Participants with good/excellent health showed greater purpose in life, fewer depressive symptoms, more education, and less loneliness than those with poor fair health. Less depressive symptoms, disabilities, adverse life events, and loneliness were associated with higher healthy days index scores. Health-related quality of life was linked to disabilities, smoking status, depression, race/ethnicity, and purpose in life | The cross-sectional study design does not allow for causality interpretations, and self-reported data may include response bias. The participants in this study had good virologic control and thus generalisability to those with less virological control may be reduced |
| DeFulio et al., 2021 (USA) [98] |
n = 50 M = 52.4 years (SD = 10.7) Community |
Intervention study: Medication Event Monitoring System (MEMS) cap were given to participants attached to their primary ART medication bottle to measure adherence. Participants were placed into either the intervention or control group. Participants were given smart phones that had the intervention app and had to submit videos of medication consumption. At the beginning and every month after surveys were given to participants | Medication Event Monitoring System (MEMS) cap and smartphone-based intervention app ("SteadyRX") | Participants in the intervention group submitted 75% of required videos, of which 81% met validity criteria, thus indicating a high usability level. Over the study duration the percentage of adherent participants decreased in the control group (p = 0.031). The control group self-reported an average adherence of 91.10% adherence and 94.34% was reported by the intervention group, but this was not a significant difference | A limitation of this study is the small sample size and single site recruitment, reducing generalisability of the findings. Another study limitation could be the lack of requiring a detectable viral load. Finally, the biometric data collecting procedure was flawed, creating another study limitation |
| Lopez-Centeno et al., 2020 (Madrid) [20] |
n = 1292 Median = 69 years (67–73) Community and Hospital pharmacies |
Dispensation registries of community and hospital pharmacies from the Madrid Regional Health Service was analysed between January to June 2017. The Beers criteria was used to identify potentially inappropriate medications among older PLWH | The 2019 American Geriatrics Society Beers criteria | Polypharmacy was observed in 65.9% of older PLWH. Cardiovascular (69.7%), gastrointestinal and metabolism (68.2%), and nervous system (61.0%) drugs were among the most prescribed co-medications among participants. At least one potentially inappropriate medication was identified in 37.3% (482) participants. 667 potentially inappropriate medications were identified in 482 participants, 60.8% (293) involved benzodiazepines, and 27.2% (131) involved nonsteroidal anti-inflammatory drugs | One limitation to the study is that over-the-counter medicines were not included, this may have led to an under-estimation of potentially inappropriate medications. Moreover, the study is limited by a lack of information on participants co-morbidities, medical managements, such as potential dosage adjustments, and the absence of information on the clinical outcomes of patients with potentially inappropriate medication |
| Jakeman et al., 2021 (Switzerland) [74] |
n = 1019 Median = 70 years Nationwide |
Prescriptions of eligible participants from the Swiss HIV Cohort Study (SHCS) were reviewed to assess anticholinergic (ACH) medication | An average of 5 (± 3.6) non-HIV drugs were taken by participants. 20% of participants were on one ACH medication, reporting average ACH scores of 1.7 (± 1.3). Self-reported neurocognitive impairment was associated with depression and being on one ACH medication | A limitation to this study includes that adherence to ACH medications were not assessed so it cannot be determined if participants were taking their prescribed medications. Dose or duration of ACH medication and history of CNS infection was not evaluated, which all impacts neurocognitive impairment. Self-reported depression rating scales were not available; thus, the diagnosis of depression may have been missed in some of the cohort | |
| Fischetti et al., 2022 (USA) [51] |
n = 1144 Median = 52 years Community |
Data were collected retrospectively via medical chart reviews | Most participants (48%) had one or two co-morbidities, with two participants having 5 co-morbidities. 80% of participants had an undetectable viral load. Higher viral suppression was seen in participants with more co-morbidities (p = 0.009). It was reported that participants with psychiatric disorders had the lowest viral suppression compared to other co-morbidities | Generalisability of the study findings is reduced due to recruitment being from a single site. The number of medications taken per disease and data on disease control was not taken | |
| Hartzler et al., 2019 (USA) [60] |
n = 44 M = 52.3 years Hospital and Community |
Data were collected through focus groups and a survey for demographic information | The study found an emerging theme across staff focus groups of wanting therapy to be patient centred, adaptable, and mission-congruent. Patients reported desiring therapy to have patient autonomy in illness management and fairness among service users. Staff perceived higher compatibility for motivation interviewing than cognitive behavioural therapy or contingency management, this was similar among patients albeit a less robust or reliable pattern | A limitation of the study includes potential bias in participant responses within the focus groups due to social desirability. The generalisability of the study findings is reduced due to the small sample size | |
| Furlotte et al., 2017 (Canada) [92] |
n = 11 Age: 52–67 years Community |
Semi-structured interviews, a checklist of health and social services, and a demographic questionnaire were used to collect data | Three main themes emerged from the interviews: uncertainty, stigma, and resilience. Uncertainty impacting on mental health was reported due to unexpected survival, medical uncertainty, and perception of one's symptoms. Stigma experiences were caused by discrimination in health care interactions, being stigmatised due to physical appearance, anticipated stigma, misinformation, and compounded stigma. Individual approaches to resilience helped participants cope with these experiences, examples include decreasing the space that HIV consumes in their life, making lifestyle changes around the condition, and using social supports | Limitations to the study include that recruitment was of participants attending their local clinic service and the results cannot be generalised to those not attending care services. Full mental health histories were not taken; thus, it is not possible to determine whether participants had mental health concerns before or after their HIV diagnosis | |
| Lee, 2019 (USA) [82] |
n = 97 M ≥ 50 years for all groups Community |
Self-report measures were used to collect data on demographics, ART medication information and medication adherence. Pharmacy and medical records were also used for data collection | Medication adherence, both self-reported and pharmacy-based, or executive functioning was not significantly associated with cigarette smoking. Poor self-reported medication adherence was associated with symptoms of clinical and subclinical levels of anxiety and depression | Generalisability of the study findings are reduced due to recruitment being from a single site. Overall status of health was not measured, which may have impacted the findings. Some participants found the self-reported adherence questionnaire to be difficult to understand, this may have affected the findings, also pharmacy-based adherence data was based on pharmacy refill data, which may not always mean participants are taking the medications they collect | |
| Jacomet et al., 2020 (France) [59] |
n = 1137 M = 50.2 years Hospital and community |
Data were collected through surveys | The presence of co-morbidities was reported in 64.2% of participants and 90% had a undetectable viral load. 58% of participants knew of the medication file, however, only 40% of pharmacists reported to offering it systematically. 32% of participants would like to use the medication file programme, particularly those with shorter ARV duration, a less often undetectable viral load and those who experience anxiety more often | Generalisability of the study results are reduced due to the sample population being predominantly male | |
| Zheng et al., 2022 (China) [61] |
n = 185 M = 58 years (SD = 7.5) Hospital and community |
Data were collected using questionnaires | The Chinese version of the Living with Medicines Questionnaire version 3 (LMQ-3) and the Centre for Adherence Support Evaluation (CASE) Adherence Index | Polypharmacy was reported in 40% of participants. A higher level of medicine-related burden was reported in females, who took more drugs and had a lower monthly income. ART adherence was negatively associated with medicine-related burden (p = 0.001) | Limitations include that data were collected via self-report and was not verified using medical records, prevalence of PDDI in this study may have been underestimated as the Liverpool interaction database does not include information on traditional Chinese medicines or herbal drugs, and as recruitment occurred only at two sites in the Hunan province, findings may not be generalisable elsewhere |
| Uphold et al., 2004 (USA) [46] |
n = 19 (≥ 50 years) and n = 18 (< 40 years) Older group: M = 58 years (SD = 7) Hospital |
Data were collected using electronic medical records | Adverse side effects from highly active antiretroviral therapy (HAART) were uncommon in the two age groups, with only 4 participants stopping HAART due to adverse effects. Viral load improved significantly for both groups on HAART (p = 0.0001) | Generalisability of the study results are reduced due to the sample population being predominantly male | |
| McInnes et al., 2013 (USA) [81] |
n = 1871 36% = 45–54 years, 43% = 55–64 years and 11.7% ≥ 65 years Community clinics |
Data collected via the Veterans Aging Cohort Study was used to investigate an association between patient electronic personal health record use and ARV adherence. Pharmacy-refill data was used to assess adherence | Personal health record: My HealtheVet | The study found that younger participants (under 45 years) were less adherent than older participants (over 55 years). Participants ≥ 65 years old were less likely to use the personal health record than those < 45 years old. Personal health record use was linked to better adherence | The cross-sectional study design limits the ability to establish a causal relationship between personal health records and adherence. Moreover, there may be unmeasured confounding factors. Pharmacy refill data may overestimate adherence as patients may be collecting their medications without administering them |
| Rosenfeld et al., 2020 (UK) [41] |
n = 100 Median = 56 years (50–87) Hospital and community |
Focus groups, life-history interviews, and surveys were used to collect data | Distinguishing support from HIV-negative (Goffman's 'the wise') people and support based on experiences of PLWH themselves (Goffman's 'the wise'), participants viewed the former as requiring supplementation by the later. Experientially based support varied across groups | A limitation to this study is that focus groups may have led to social desirability bias or moderator bias | |
| Gardenier et al., 2010 (USA) [80] |
n = 56 M = 50.5 years (SD = 8.5) Community (AIDS day health care program) |
Information was extracted from medical records then reviewed and corrected by participants. Participants also completed the Social Provision Scale and the AIDS Clinical Trial Group adherence follow-up instrument | Social Provision Scale (SPS) and the AIDS Clinical Trial Group (ACTG) adherence follow-up instrument | There was a statistical significance between adherence and social support (p = 0.02). Out of the 51 participants who were prescribed ART, 28 (55%) were adherent. There was a statistically significant difference between CD4 T-cell counts between the adherent and non-adherent group, with the latter being lower (p = 0.004) | The study is limited due to the sample size, recruitment not being randomised, and the participants being recruited at two New York city locations from the AIDS Day Health programme |
| Bosire, 2021 (South Africa) [57] |
n = 15 40–70 years Hospital and community |
Data were collected using an ethnographic approach and through 90-min interviews | Participants access to care to manage their co-morbidities were impeded by fragmentation of care, having multiple clinic appointments, conflicting information, and poor patient-provider communication | The small sample size and single site for recruitment reduces the generalisability of the study findings. Language barriers and the use of an interpreter may have changed the meaning of statements reported by participants | |
| Frazier et al., 2018 (USA) [79] |
n = 3672 over 50 years old Hospital and community |
Matched interview and medical record abstraction data from a surveillance system, the Medical Monitoring Project (MMP), was analysed | Women living with HIV over 50 years old were more likely to be prescribed antiretroviral therapy, be virally supressed, be dose adherent, and are less likely to have received sexually transmitted infection prevention information from a healthcare provider, have condomless sex with a negative or unknown partner and report depression compared to women under 50 years old | The limitations to this study are that generalisability of findings are reduced due data being collected from HIV positive women who are in care and not those who are not receiving medical care and the cross-sectional study design does not allow for causality analysis of findings | |
| Schatz et al., 2021(South Africa) [48] |
n = 23 Age ≥ 50 years Community |
In-depth semi-structured interviews | Perceived shame of sexuality and disrespect by clinical staff, disclosing serostatus to others, affording transport to clinics and co-morbidities were key age-related barriers to ART access. Age-related facilitators were financial and moral support from families and access to social grants | Limitations to this study include the small sample size and recruitment of participants who were already tested and linked to care, reducing the generalisability of the findings. Moreover, there may be other barriers or difficulties relating to not testing, late testing, and failing to attend care services that the study was unlikely to identify due to the sample population | |
| Schatz et al., 2022 (South Africa) [84] |
n = 161, PLWH > 40 years Community |
Focus group discussions | Participants reported fewer negative consequences of discloser in 2018 compared to 2013. Participants reported positive outcomes such as building trust, and greater support with adherence and medication collection | A limitation of the study is that participants in the 2013 focus group were different to those in 2018, which may have influenced the findings | |
| Contreras-Macias et al., 2020 (Spain) [73] |
n = 19 M = 69.4 years Outpatient |
Data were obtained from medical records, the electronic prescription programme, and the outpatient dispensing programme | Medication Regimen Complexity Index (MRCI), The European AIDS Clinical Society (EACS) guideline of “Selected Top 10 Drug Classes To Avoid (Top-10-A) in elderly PLWHIV”, and the STOPP-Beers criteria | Polypharmacy was reported in 84.2% (16) of participants and a Top-10-A potentially inappropriate prescription was evident in 47.4% (9) of participants. The most prevalent group of prescribed drugs were benzodiazepines, reported in 30% (6) of participants. 57.9% of participants were complex patients with a MRCI index above 11.25. A higher sum of STOPP-Beers criteria was identified in older patients. Analysis using the t-student test showed a statistically significant relationship between MRCI score and the sum of the STOPP-Beers criteria with increasing age (p < 0.05) | The generalisability of the study findings is reduced by the single-centre study design and small sample size. Moreover, the STOPP-Beers criteria were validated to non-HIV patients 65 years or older |
| Contreras-Macias et al., 2021 (Spain) [70] |
n = 428 M = 50 years (SD = 10.9) Outpatient |
Data were collected using the Capacity-Motivation-Opportunity pharmaceutical care model at routine follow-up appointments | Medication Regimen Complexity Index (MRCI) and the EQ-5D-5L questionnaire | Polypharmacy was identified in 25.9% (111) of participants, with 5.4% (23) being on 11 or more medications. A negative correlation between ED-5D and MRCI scores was identified (p = 0.0002). The relationship between co-morbidity and quality of life was statistically significant in the thyroid-mechanic (p = 0.002) and geriatric-depressive (p = 0.003) patterns | Although the study had a large sample size, the generalisability of the findings is limited due to the study being based at a single urban safety net hospital. Moreover, participants included in the study were those engaged in the care and cannot be generalised to patients who fail to attend care |
| Engelhard et al., 2018 (The Netherlands) [26] |
n = 331 (HIV positive) M = 51 years (SD = 11.2) Outpatient |
HRQOL was measured using a survey in a nationwide sample of PLWH. Data from studies in diabetes and rheumatoid arthritis were added | Medical Outcomes Study Short Form 36-item Health Survey | The HIV sample had the lowest mental health score, with the odds of poor mental HRQOL being higher in HIV patients than other groups. The chances of poor physical HRQOL were similar in both the HIV and diabetes groups, but lower in the rheumatoid arthritis group. Poor physical HRQOL among PLWH was linked to a history of AIDS, longer time on combination ART and severe co-morbidity. Being of Sub-Saharan African descent and having CD4+ counts of less than 350 was linked to poor mental HRQOL | A limitation of this study is that comparing HRQOL between different datasets may lead to findings resulting from other unmeasured factors and not the diversity of the diseases. Socioeconomic status, substance use, and sexual orientation were potential confounders that the study was unable to adjust for, due to inconsistent recording across data sets. Other limitations include that disease severity was not corrected for and participant samples of the other diseases were not a national cross-section of the patient populations |
| Moitra et al., 2011 (USA) [87] |
n = 16 M = 52.5 years (SD = 5) Community clinic |
Intervention study: 3–5 weekly 60-min acceptance-based behaviour sessions were conducted in groups of 3–5 participants. Discussions included overall acceptance-based principles, with each session being a stand-alone intervention | Acceptance-based behaviour therapy | 37.5% (6) participants found the groups to be very helpful and another 37.5% (6) found them to be moderately helpful, whilst 25% (4) found them minimally helpful. The study reported that qualitative observations suggested that the acceptance-based intervention strategies were well suited in the target population. A significant point made in every session was that avoiding the realities of living with HIV can lead to worsened health | The small sample size reduces the generalisability of the study. Group formats for each session may have impeded recruitment or undermined treatment acceptability for potential participants |
| Farahat et al., 2020 (Saudi Arabia) [47] |
n = 13 M = 50.1 years Hospital |
Data were collected retrospectively via medical chart reviews | Out of 130 participants that were included, 48.5% had one or more co-morbidities. Diabetes (15.4%), dyslipidaemia (10.8%), hypertension (10.8%) and lymphoma (10.0%) being the most common co-morbidities. An increase in co-morbidities was seen with an increase in age, with 40.7% of participants aged 60 years or older having three or more co-morbidities. Logistic regression analysis showed that only patients aged 50 years and older were more likely to have at least one co-morbidity | The generalisability of the study is limited by the small sample size. Also, the cross-sectional study design does not allow for causality analysis. Moreover, the study did not look at adherence and medical records were reviewed over an 18-year period, but several ART medication doses and durations were missing | |
| Guaraldi et al., 2017 (Italy) [28] |
n = 482 M = 53.9 years (SD = 6.9) Multidisciplinary clinic |
Patients were evaluated using two frailty tools as part of routine protocol | The Frailty Index and frailty phenotype | The frailty phenotype categories were: 51.9% pre-frail, 3.1% frail, and 45% robust. The mean Frailty Index score was 0.28±0.1. Falls and disability were linked to the Frailty Index but not the frailty phenotype | Due to the cross-sectional study design, the Frailty Index could not be assessed over time for the prediction of adverse outcomes. The lack of a HIV-negative control group and more objective tools to assess disability are further limitations |
| Owen et al., 2012 (UK) [71] |
n = 10 Median = 57 (52–78) years Hospital and community |
A biographical narrative approach was used to collect data | Findings showed that some participants were positive about ageing regarding it as progressing towards valued life goals, whereas others were more conflicted with future prospects. The individual's biographic relationship with the HIV epidemic history rather than their age influenced the differences in views of the future. Participants who were involved with HIV for longer were more likely to have interrupted careers due to illness, depend on state benefits, and have damaged social networks | The study findings were limited by the small sample size and recruitment location | |
| Date et al., 2022 (UK) [101] |
n = 164 Age: MOR: median = 59.5 (SD = 50–78) years; standard care: median = 60 (SD = 50–82) years Hospital |
Intervention study: Participants were randomized to either receive standard care or a Medicines Management Optimisation Review (MOR) | Medicines Management Optimisation Review toolkit, the University of Liverpool and Toronto General Hospital HIV drug interaction references, EuroQol five-dimension five-level (EQ-5D-5L) questionnaire and visual analogue scale (EQ-VAS) | Seventy participants were in the intervention group and ninety-four in the standard care group. Significantly more medicine-related problems were identified in the intervention group at baseline (p = 0.001) and 6 months (p = 0.001). There was a significant reduction in new medicine-related problems at 6 months in the intervention group compared to baseline (p = 0.001), with 44% being resolved at baseline and 51% at 6 months. There were no changes in HRQOL identified between groups or after the intervention. Participants and healthcare professionals found the MOR highly acceptable | The limitations to this study include the sample size, MORs required extra attendance to the clinic which may have precluded some participants, and as this was a feasibility study, it was not powered to measure the effectiveness of the intervention |
| Cho et al., 2018 (USA) [100] |
n = 36 Control group: M = 52 years (SD = 6.6) Intervention group: M = 51 years (SD = 13) Community |
Intervention study: Follow-up focus groups lasting 60–90 min were conducted using semi-structured discussion guides to allow participants to discuss their experiences and any issues with using the mVIP app, after the clinical trial had ended | mVIP (a web-app) | Focus groups revealed the five following themes related to predisposing factors: ease of using the app, being user-friendly, self-efficacy for management of symptoms, design preference of illustrated strategies with videos, and user-control. The four themes identified relating to enabling factors included: information requirements of symptom management, tracking symptoms, fit in lifestyle/living/schedule conditions, and more languages. The five themes reported relating to reinforcing factors included: communication with healthcare providers, information visualisation for each user, social networking, improvement in quality of life, and individual-tailored information quality | The generalisability of the findings may be limited due to the small sample size and the study sample being predominantly female. The app was only in English, therefore PLWH who are primary-Spanish speakers (an underserved population in the USA) were not included in the study |
| McNicholl et al., 2017 (USA) [38] |
n = 248 M = 57.8 years (SD = 5.1) Community |
Intervention study: Electronic medical records were used for medication reconciliations conducted by pharmacists | Pharmacist medication reconciliation, Beers and STOPP criteria, Patient Health Questionnaire-9, the Montreal Cognitive Assessment, and the Veterans Ageing Cohort Study (VACS) Index | Hypertension (56%), depression (52%), COPD/asthma (48%), dyslipidaemia (39%), coronary artery disease (27%), and diabetes (22%) were the most common co-morbidities found. 35% of participants were taking 16 or more medications and 16% were taking more than 20. Beers and STOPP criteria were present in 156 and 134 participants, respectively. 25 contraindicated drug interactions were identified in 20 participants. A mean of 2.2 medications were stopped after medication reconciliation | A limitation to this study is that only a subsample of the clinic’s population was included due to limited resources. Underestimations of the pharmacist’s role in correcting potentially inappropriate prescribing may have occurred as only medications that can be corrected without collaboration and conducted during the clinic visit were measured. Interventions undertaken after the clinic visit was not included |
| Hojilla et al., 2021 (USA) [95] |
n = 584 M = 50.5 years Hospital |
Secondary analysis of data collected from a RCT of behavioural interventions for reducing unhealthy alcohol use in PLWH | Berger HIV stigma scale, the 12-item short form survey (SF-12) | African American participants reported higher personalised stigma scores and disclosure concerns compared to Caucasians. Both Hispanic/Latinx and African American participants were more likely to report having concerns around public attitudes towards PLWH than Caucasians. Woman were more likely to have increased negative self-image scores than men | Sample size limited the studies ability to evaluate correlates of HIV stigma within sex and race/ethnicity subgroups. The generalisability of the results is reduced as participants are an insured cohort with well managed HIV |
| McAllister et al., 2013 (Australia) [88] |
n = 335 M = 52 years Hospital |
Data were collected via anonymous surveys | 19.6% (65) of participants reported meeting pharmacy dispensing costs as difficult or very difficult, 14.6% (49) stated that due to pharmacy dispensing costs they have delayed purchasing medications, and 9% (30) reported stopping medication due to pharmacy costs. Amongst the 19.6% of participants finding difficulty meeting pharmacy costs, 29.2% (19) had stopped medication compared to 4.1% (11) of the remaining 270 patients (p < 0.0001). 5.7% (19) patients found travel to the clinic difficult or very difficult. Difficulty meeting pharmacy and clinic travel costs were independently associated with treatment cessation and interruption. 4.9% of patients reported being asked if they were having difficulty with payments for medication | The study findings are limited due to a single-site recruitment, participants being mostly male, and the lack of viral load data meaning that clinical significance of patient responses could not be determined | |
| Heron et al., 2019 (Australia) [31] |
n = 2406 (HIV-positive) and n = 648,205 (HIV-negative) Age: 45–64 years = 58.9%; 65–74 years = 10.3%; over 75 years = 2.3% Community |
Data were collected directly from MedicineInsight—a national primary care data programme | HIV-positive males were less socioeconomically at a disadvantage than HIV-negative males. The HIV-positive males in this cohort were at an increased risk of cancer, chronic kidney disease, anxiety, depression, and osteoporosis. Younger PLWH are at risk of premature onset of osteoporosis, cancer, and cardiovascular disease. A high prevalence of depression and anxiety was reported among HIV-positive males | A limitation to this study includes the potential of duplicated patient records on MedicineInsight as it is not linked across practices, thus if a patient were to visit more than one practice it would be entered as separate records | |
| McMillan et al., 2019 (Canada) [67] |
n = 716 Age range = 50–92 years and M = 59.2 (SD = 6.5) Outpatient clinic |
Health data routinely collected at the Southern Alberta Clinic that included laboratory, self-reported and clinician-reported results | The 29-item Frailty Index developed for Southern Alberta Clinic | The mean Frailty Index, 0.303 (± 0.128), did not differ between genders. It was not linked to current CD4 counts or nadirs. Frailty Index increased with age, ART duration, and duration since HIV diagnosis. Higher Frailty Indexes was seen in those who died compared to the survivors | The cross-sectional design of the study limits the ability to draw conclusions of causality and directionality of the associations found. Another limitation is that the data used was collected for purposes other than calculating frailty, raising questions about accuracy and comprehensiveness |
| Kiplagat et al., 2019 (Kenya) [34] |
n = 57 Age: 50–59 years = 33.3%; 60–69 years = 49.2%; 70–79 = 17.5% Hospital and community |
In-depth interviews and four focus groups were used to collect data | Participants reported that co-morbidities and visiting multiple healthcare providers to manage their HIV as factors that impact their adherence to medication and clinic attendance. Other challenges included poor quality of facilities and patient-provider communications. Matched gender and older age for healthcare providers were reported as preferential by participants | The generalisability of the results is reduced as patients that had been lost to follow up or disengaged from care were not included, also participants included had been in care for at least a year, thus their views and experiences may have improved within that time | |
| Drewes et al., 2021 (Germany) [50] |
n = 897 M = 57 years (SD = 6.7) Community |
Data were collected using a self-administered questionnaire | An Adapted version of the negative self-image subscale of the HIV Stigma Scale, the Silver Lining Questionnaire (SLQ), the OSLO 3 Social Support Scale (OSSS-3), and the UCLA Loneliness Scale | 18% (165) of participants reported having one or more falls in the 12 months prior to the study. A higher risk of falling was significantly associated with a lower economic status, living alone and being single. Having one or more co-morbidity increased the risk of falls by 2.5 times. Diseases of the central nervous system, heart disease, rheumatism, osteoporosis, and chronic pain were strongly associated with fall risk. In addition, internalised and experienced HIV stigma, social support, and loneliness were significantly related to a fall risk | The cross-sectional study design does not allow for causality analysis. The self-administered questionnaires may have led to bias on recall and social desirability. The study was not able to fulfil a probability sample of people ageing with HIV in Germany, thus reducing the generalisability of the results. Moreover, several potential risk factors for falls were not included in the analysis of this study, for example, specific medication, problems with balance or gait, or mobility |
| Vinuesa-Hernando et al., 2021 (Spain) [49] |
n = 30 Median = 71 Hospital |
Observational study using data from patient hospital medical records | The Medication Regimen Complexity Index (MRCI), the Simplified Medication Adherence Questionnaire (SMAQ), the Screening Tool of Older People’s Prescriptions (STOPP) and List of Evidence-baSed depreScriing for CHRONic patients (LESS-CHRON) crtieria | The most common co-morbidities were dyslipidaemia (70%), hypertension (66.7%), diabetes (43.4%), mental health disorders (26.7%). 30% of participants were taking 10 or more medications and 70% were taking more than five. 66.7% of participants were adherent to their medications. The MRCI score of concomitant medications was higher than the score of ART at 18.3 points and 5.1 points, respectively. Potentially inappropriate prescribing was present in 70% of participants according to the STOPP or LESS-CHRON criteria. Polypharmacy was significantly associated with meeting deprescribing criteria (p = 0.008) | Limitations to this study include the use of dispensing records as some information may be missing and the reliability of the information depends on the inputting physician. Furthermore, the small sample size limits the generalisability of the data |
| Rozanova et al., 2020 (Ukraine) [97] |
n = 123 Age = 55–81 years Community |
Data were collected via telephone surveys | Older PLWH with substance misuse disorders maintained their HIV and substance use disorder therapies over the Covid-19 lockdown, however, social support was highlighted to be critical to avoid treatment interruptions | A limitation to this study is that telephone surveys may have led to social desirability bias in participant answers | |
| Chayama et al., 2021 (Canada) [55] |
n = 42 Age = 50+ years Community |
Semi-structured in-depth interviews were used to collect data | Participants viewed co-morbidities as more urgent and prioritised them over HIV. Access to care for co-morbidities were hindered by stigma and discrimination. Participants reported difficulty concurrently managing their co-morbidities and HIV due to poorly managed co-morbidities. Concerns and frustrations were stated regarding the potential impact of ART on the development of co-morbidities. Treatment approaches that integrated services aided engagement with care | The study was only conducted with English speaking participants, thus the opinions and experiences of marginalised individuals such as immigrants and refugees were not collected | |
| Siefried et al., 2017 (Australia) [85] |
n = 522 M = 50.8 years (SD = 12.3) Hospital and community clinics |
A study-provided laptop was used by participants to complete a 204-item questionnaire | University of Liverpool HIV drug interaction database, and the Charlson co-morbidity Index | 77 (14.8%) of participants reported being linked to one or more HIV community organisations or peer support groups. The median duration on ART was 11 years. 78 (14.9%) of participants missed an average of one or more ART medications per month in the 3 previous months | The self-reported nature of the questionnaire for adherence may overestimate true adherence levels. Due to recruitment strategies, there is a risk of selection bias. The study findings are less generalisable to patients without subsidised healthcare, community supports, those with virological failure, females, and heterosexual males |
| Siefried et al., 2018 (Australia) [44] |
n = 522 M = 50.8 years (SD = 12.3) Hospital and community clinics |
Participants were given a 204-item questionnaire on dedicated laptops | 204-question questionnaire incorporating other existing or pre-validated instruments | 292 (55.9%) participants reported having co-morbidities. 392 (75.1%) participants took at least one concomitant drug. The daily pill burden for concomitant drugs was 6 and the ART daily pill burden was 1.2. Cardiovascular, antidepressants, over the counter, endocrine agents and anti-effectives were the most common classes of concomitant medication. 122 (23.4%) participants were taking at least 5 concomitant medications. The concomitant medication taken in 17 participants were contraindicated with their ART. Overall, 730 ART-concomitant combinations were identified as being a potential drug–drug interaction. 178 participants reported adverse drug reactions | A majority of the participants were male and in a country with subsidised healthcare systems, thus reducing generalisability to females and those in countries without subsidisation. The cross-sectional study design does not allow for causality analysis. The study did not collect data on concomitant medication dosage, therefore it cannot report whether dose adjustments would mitigate potential drug–drug interactions |
| Bogart et al., 2021 (USA) [94] |
n = 76 Median = 52.9 (SD = 12.9) Community |
Intervention study: Individually randomised group-treatment trial using cognitive behavioural therapy. Participants were clustered into groups. Semi-structured interviews were conducted post intervention | Medication Event Monitoring System (MEMS) bottle cap | The intervention group showed improved adherence compared to the control group (electronically monitored: p = 0.06; Self-reported: p = 0.02). There was significantly lower medical mistrust amongst the intervention group compared to the control group (p = 0.02) | Generalisability of the study findings are reduced due to convenience sampling at one community site and the small sample size |
| Harris et al., 2020 (USA) [64] |
n = 35 M = 58.3 years (SD = 5.4) Community and hospital |
Data were collected through surveys, interviews, and focus groups | The Berger HIV Stigma Scale, Perceived Stress Scale, Engagement with Health Care Providers Scale, and the Composite of Engagement in HIV care | 54.3% of participants were reported to be moderately engaged in care. The overall stigma in participants were high and participants were reported to be moderately stressed. There was a significant correlation between engagement in care and the stigma subscales, including negative self-image stigma (p = 0.03). Perceived stress was also associated with overall stigma, disclosure stigma, personalised stigma, negative self-image stigma, and public attitudes stigma. Race was highlighted as an additional cause of stigmatisation among African Americans | Limitations include data collected from surveys being self-reported, and items related to engagement in care were not based on reviews of medical charts. Self-reports may have led to bias on recall and social desirability. The small sample size limits generalisability |
| Mao et al., 2018 (Australia) [37] |
n = 98 Median = 51.5 years (26–65) Community |
Intervention study: A 6-week randomised SMS reminder intervention for ART adherence was conducted, followed by a mixed-method evaluation consisting of one-to-one interviews and a self-completed online survey | SMS reminders to mobile phones | The most common reasons for previous ART interruption were experiencing side effects and attending to other life priorities. There were no statistically significant differences between the intervention and control arms at the end of the SMS campaign. A common suggestion for improvement of the intervention was that it should be tailored to each individual's needs and synchronised with their dosing regimens. The SMS campaign had several positive responses, describing impacts beyond ART adherence | The small sample size may reduce generalisability of the findings and limits the ability to find differences between the experiment groups. The cross-sectional mixed methods evaluation does not allow causal conclusions to be drawn. Moreover, evaluation consisted of self-reported data |
| Jiménez-Guerrero et al., 2018 (Spain) [77] |
n = 242 Median = 57.5 years (54–62) Hospital |
Data from electronic clinical records were used with a computer system (Diraya) to identify home treatment and an application for outpatient dispensing (Farmatools). Interactions were identified using four independent prescribers, product specification and an online database (http://www.drugs.com) | http://www.drugs.com | 61% (148) of participants were receiving concomitant treatment and 243 potential interactions were detected among 110 participants. 46 of the interactions were considered severe, whilst 197 were moderate. 76% (35) of the severe interactions were associated with boosted protease inhibitors. Statins and inhaled corticosteroids caused most severe interactions | The retrospective nature of the study could be a limitation, however, being merely descriptive, it may be considered irrelevant. Another limitation could be that over the counter and herbal medicines were not included |
| Knight et al., 2018 (South Africa) [35] |
n = 23 PLWH ≥ 50 years Community |
In-depth semi-structured interviews | Participants received care for both HIV and other conditions provided by different healthcare professionals and at different health facilities. Older PLWH and non-communicable diseases experience several physical and structural barriers to accessing care. These difficulties can worsen health outcomes | A limitation to this study is that recruitment was conducted via referrals from the HIV service, thus this may have led to participants with more or less barriers being missed | |
| Halloran et al., 2019 (UK/Ireland) [14] |
n = 698 PLWH ≥ 50 years and 374 PLWH ≤ 50 years 304 HIV-negative participants≥ 50 years old Hospital |
Potential drug–drug interactions were analysed using two interaction checking tools. The Pharmacokinetic and Clinical Observations in People Over 50 (POPPY) study is a prospective, observational, multicentre study that collected data over a three-year period from 2013 to 2016 | The Lexicomp database and the Liverpool drug interaction database (wwwhiv-druginteractionsorg) | Polypharmacy was prevalent in 65.8, 48.1 and 13.2% in older PLWH, younger PLWH and the HIV-negative group, respectively. This reduced to 29.8% of the older group and 14.2% of the younger group when ARVs were excluded. 36.1% of older PLWH, 20.3% of younger PLWH and 16.4% of the HIV-negative group had a prevalence of ≥ 1 PDDI involving non-ARV medications. The prevalence of ≥ 1 PDDI between ARV and non-ARV medication was 57.3% in older PLWH and 32.4% in younger PLWH | One limitation of this study was a lack of data on dosing information of most medications, leading to some interactions being overestimated. Another limitation is that the medication lists were self-reported by participants, which may have been under-reported. Lexicomp is a sensitive interaction checker and some of the interactions flagged may not be clinically relevant in daily practice |
| John et al., 2016 (USA) [32] |
n = 359 Median = 57 years (50–80) Hospital |
The following four domains were evaluated using a questionnaire: social support, physical health and function, mental health, and behavioural and general health | The Lubben Social Network Scale-6, the Social Provisions Scale, the UCLA 8-item Loneliness Scale, the Patient Health Questionnaire-9), the Generalised Anxiety Disorder-7, the Breslau 7-item PTSD screen, and the Montreal Cognitive Assessment | Participants experienced the burden of ageing related conditions over the domains evaluated. Nearly 60% reported mild symptoms of loneliness, 50% showed low social support, 41% had a fall in the last year and 34% met the criteria for possible mild cognitive impairment. Participants 60 years old or over had higher frequencies of balance issues compared to the group aged 50–59 years old. Fewer participants reported "very good" or "excellent" HRQOL in the 50–59 years old age group compared to the older group | The cross-sectional study design meant that changes were not measured over time. The findings may not be generalisable as the participants were largely male and from one city. Patients in long-term care facilities were not included. Most of the participants were diagnosed over 10 years prior, thus results may not be generalisable to newly diagnosed older PLWH |
| Townsend et al., 2007 (USA) [63] |
n = 58 M = 51.5 years (SD = 8.8) Hospital |
Data were collected using electronic medical records | Findings showed a non-significant correlation between viral loads and 6-month pharmacy medication refill-based adherence (r = 0.1). Adherence rates lower or equal to 70% led to CD4+ levels progressively declining. AIDS-related events incidence or past ARV experience did not significant affect the distribution of participant CD4+ levels or adherence | Limitations to this study include that pharmacy refill data was used to measure adherence as patients may have collected their medications but not taken them, the small sample size, and short study duration | |
| Levy et al., 2017 (USA) [36] |
n = 7018 Median = 50 years (39–57) Hospital and community |
Electronic medical records were used for data collection | Half of the participants reported having hypertension, 48% had dyslipidaemia, and 35% had obesity. A higher prevalence of co-morbidities was seen in older PLWH (p < 0.001). Hypertension was reported more in black patients, diabetes and obesity were reported more in female and black patients, and dyslipidaemia was reported more in male and white patients (all p < 0.001). Metabolic co-morbidities were associated with controlled immunovirological factors, longer time since HIV diagnosis, and a greater duration of ART | Limitations to this study include the cross-sectional study design does not allow for temporality or causality analysis, electronic medical records may have missing information, thus this may affect the results. Information on ARV adherence was not collected | |
| Gimeno-Gracia et al., 2014 (Spain) [76] |
n = 130 M = 56.7 years (SD = 6.2) Hospital |
Data were collected from out-patient pharmacy records at a University Hospital in Spain | At the end of the study, 90% of participants had an undetectable viral load and 58% had a CD4 count over 500 cells/mm3. Treatment that was based on protease inhibitors were used by 51.5% of older patients and 54.4% of the younger patients, whilst nonnucleoside reverse transcriptase inhibitors were used by 43.8 and 39.8%, respectively. The older group used treatments with abacavir more frequently (p = 0.054) and with tenofovir less frequently (0.105) compared to the younger group | Due to the retrospective nature of this study, some data was incomplete. Also, the varying number of years since diagnosis among patients could have influenced their degree of adherence, the ART received, etc. | |
| Gimeno-Gracia et al., 2016 (Spain) [72] |
n = 119 Median = 52 years (51–56) Hospital |
Data were collected retrospectively to compare polypharmacy, percentage of patients that collected each therapeutic drug class, and the median duration of each drug class between older PLWH and the general population | A higher percentage of HIV-positive males had polypharmacy than males from the general population (8.9 vs 4.4%, p = 0.01). This was also true for females from each group, with older and younger groups having 11.3 and 3.4% of polypharmacy, respectively (p = 0.002). HIV-positive participants recieved more gastrointestinal drugs, analgesics, anti-infectives, central nervous system (CNS) agents, and respiratory drugs than the general population. No differences was observed between both groups for cardiovascular drugs. HIV-positive participants had a higher estimated number of treatment days than the males in the general population for CNS agents (p = 0.02), anti-infectives (p < 0.001) and more were receiving sulphonamides (p < 0.001), quinolones (p = 0.009) and macrolides (p = 0.02) | Generalisability of the study is reduced due to single-site recruitment and only a small number of female participants being included | |
| Greene et al., 2014 (USA) [13] |
n = 89 (HIV positive) Median = 64 years (60–82) Community |
Structured interviews were used to obtain demographic data, HIV history and co-morbidity data. Medication lists were reviewed during interviews to obtain medication usage information. Participants were asked to complete a questionnaire before the interview with all their prescribed and over-the-counter medication | Lexi-Interact drug interaction software, Beers criteria 2012, and the Anticholinergic Risk Scale | Common co-morbidities amongst the participants were identified as hypertension, hyperlipidaemia, and depression. An average of 13 medications (2–38) were taken by PLWH, with only an average of four being ARVs, whereas non-HIV participants took an average of six (3–10) medications. There was at least one potentially inappropriate medicine prescribed in 46 (52%) of PLWH. Ten (11%) of the HIV participants had a Category X (avoid combination) interaction and 62 (70%) had at least one Category D (consider modification), with a third of these interactions being between two non-ARV medications. Fifteen (17%) PLWH were identified as having an anticholinergic risk scale ≥ 3 | The study population consisted of highly educated, Caucasian, men who have sex with men, therefore the findings may be less generalisable. The participants were also diagnosed for an average of 20 years, so the data may not be generalisable to older patients diagnosed more recently. Information about dosing was not obtained, therefore drug–drug interactions may have been overestimated, although the findings are consistent with other studies |
| Greene et al., 2018 (USA) [68] |
n = 356 Median = 56 years (53–62) Hospital |
Survey data were collected at two clinics to assess participants social, physical, mental, and cognitive health | The UCLA eight item loneliness scale, the Montreal Cognitive Assessment, the Lubben Social Network Scale, and the Patient Health Questionnaire | Symptoms of loneliness was reported in 58% of participants, with the majority having mild loneliness. Lonely participants were more likely to have depressive symptoms, poor or fair HRQOL, have fewer physical supports, be current smokers or at-risk drinkers and/or drug users | The study participants were predominantly male, urban, were 57% white, and had long durations since diagnosis, therefore generalisability is limited. As the study was cross-sectional, temporal relationships between loneliness and depression with HRQOL and functional impairment was not examined. The HRQOL measure used was due to ease of administration but did not have a mental health measure. Also, a measure of stigma was not included, previous research has shown links between loneliness, stigma, and depression |
| Greene et al., 2018 (USA) [27] |
n = 77 surveyed and n = 31 focus groups Median = 58 years (50–77) Hospital |
Data were collected through focus groups and a survey | Findings highlighted the need for greater focus on the following: (1) the need for knowledge expertise in HIV and ageing, (2) a focus on determinants of health (e.g., marginal housing) and on medical conditions, (3) locating speciality services together, and (4) social isolation. These findings informed the creation and design of a multidisciplinary care model for PLWH (the Golden Compass programme) | A limitation of this study includes single-site recruitment and that generalisability of the findings is reduced as non-English-speaking participants were excluded | |
| Kuteesa et al., 2012 (Uganda) [86] |
n = 40 Median = 65 years (50–80) Hospital |
Individual in-depth interviews and focus groups were used to collect data. Observations of clinic interactions were also recorded | Key themes that emerged from the qualitative interviews highlighting distinctive healthcare needs in older PLWH were: difficulty disclosing (8%), stigma (43%), access to care (80%), delayed diagnosis and care-seeking (55%), quality of patient = provider relationship (75%), serodiscordance (20%), adherence support (25%), continuity of care (14%), end-of-life issues (13%) and other issues (20%). Participants reported experiencing stigma due to HIV and ageism. Concerns and anxiety regarding securing future healthcare and the lack of social services was expressed by participants. Problems with transport and food compromised adherence to ART for many participants | Limitations to this study affecting generalisability of the findings include recruitment from a limited geographic area and purposive sampling. Duration since diagnosis may have affected individual perspectives reducing generalisability of the findings as interviews did not indicate any participant to be newly diagnosed | |
| Philbin et al., 2021 (USA) [91] |
n = 59 M = 51 years Hospital and community |
In-depth interviews were used to collect data | Four main groups emerged from those interviewed, firstly, those with few long-acting injection related worries who received episodic injections, secondly, those who had regular injections and did not want anymore, thirdly, those with a history of injection drug use that were worried long-acting injections would trigger a reoccurrence, and lastly, those who currently inject drugs and have few worried around long-acting injections. Most participants who have a history of using injectable medication would prefer long-acting injectable ART, but participants with regular injections already and a history of injection drug use may not | The generalisability of the study findings are limited as they are based on the individual women's experiences and concerns, which may not be relatable to other subpopulations | |
| Katende-Kyenda et al., 2008 (South Africa) [75] |
n = 8999 (HIV-positive) 59.42% = 40–60 years and 1.58% ≥ 60 years National medicine claims database |
Data were collected directly from Interpharm Data systems and analysed. Prescriptions were used to determine if combinations of ARVs could cause possible drug–drug interactions | A clinical significance rating of potential drug–drug interactions as described by Tatro [Drug Interaction Facts 2005 St Louis, MO: Facts and Comparisons (2005)] | Participants received a mean of 2.36 ARVs per prescription. 960 drug–drug interactions were identified. Patients aged 40–60 years old had the highest number of ARV prescriptions and the highest number of drug–drug interactions. The most drug–drug interactions were seen between Indinavir and ritonavir, efavirenz and indinavir, efavirenz and lopinavir/ritonavir | A limitation to the study was that demographic and clinical information was not available on the database. Moreover, dosage information was also not supplied |
| Schreiner et al., 2019 (USA) [42] |
n = 103 M = 53.16 years (SD = 7.2) Community |
Data from a parent study examining physical activity patterns in PLWH was used for secondary analysis to evaluate treatment burden. The parent study used one-to-one interviews and entered responses directly into Research Electronic Data Capture | The Treatment burden Questionnaire-13, the Bullen and Onyx (2007) Social Capital Measurement Tool | Overall, a low level of treatment burden was reported among participants, however, 16% of participants reported experiencing high treatment burden. Treatment burden was significantly associated with number of chronic conditions (p ≤ 0.01) and social capital (p = 0.03). The most prevalent co-morbidities were hypertension, asthma, arthritis, diabetes, hepatitis B/C, and hyperlipidaemia. Remembering to take medications at certain times during the day, paperwork, the limitations linked to taking medications and maintaining a prescribed exercise regimen were items causing the highest treatment burden | Due to treatment burden not being the primary focus of the parent study, the reanalysis could not collect data on other variables of interest. The sampling technique used may have allowed for potential sampling bias, effecting the generalisability of the study findings. PLWH who are not insured or able to afford regular medical care were not represented in this study |
| Hastain et al., 2020 (USA) [29] |
n = 99 Median = 54 years (49–61) Community clinic |
Electronic medical records were used to evaluate ART simplification. Drug–drug interaction scores pre- and post- simplification were calculated. Concomitant medications were identified and evaluated for drug–drug interactions with pre- and post- simplification ART regimens | A drug–drug interaction incidence and severity score was developed and validated and the University of Liverpool's HIV Drug Interaction Checker | A median of 3 ART pills were taken a day. After simplification, the median number of ART pills taken was 2. Discontinuing protease inhibitors and nonnucleoside reverse transcriptase inhibitors occurred frequently and ART changes to integrase strand transfer inhibitor-based regimens were common. Average interaction scores reduced from 3 (1–6) to 1 (0–2) from pre- to post- simplification. The median number concomitant medication taken was 4.5 | The results may not be generalisable due to the sample size and recruitment from only one urban site. Also, not all ART simplification strategies and HIV medications could be thoroughly evaluated. As the study relied on the completeness and accuracy of electronic medical records, it is possible that over the counter, herbal and non-prescriptions items were not included. Lastly, the scoring system does not reflect the clinical significance of drug–drug interactions, for example, some interactions may need dose adjustments or close monitoring |
| Foster et al., 2009 (USA) [93] |
n = 24 Age range = 50–76 years (M = 57) Community |
Four focus groups were conducted, and supplementary data was obtained using two stigma instruments | The Stigma Impact of HIV scale and the Self-Perceptions of HIV Stigma Scale | Participants reported rarely or not experiencing stigma as they had not disclosed their HIV diagnosis to others. Stigma was reported by participants on the Internalised Shame scale. Qualitative data found four themes associated with stigma: (1) disclosure; (2) stigma experiences; (3) need for HIV/AIDS education; and (4) acceptance of the disease | Limitations to this study include that the focus group setting may have led to response-bias and participants who have been stigmatised not wanting to participate in group discussions, data on sexual orientation and mode of sexual transmission was not collected, and the time since diagnosis ranged broadly between participants, which may have affected perceptions on stigma and disclosure |
| Halkitis et al., 2014 (USA) [66] |
n = 180 M = 55.4 years (SD = 4.6) Community |
Data were drawn from Project Gold, a study of ageing HIV-positive men who have sex with men in New York City. Self-report data was collected for sociodemographic characteristics and clinical markers | The AIDS Clinical Trials Group (ACTG) Adherence Questionnaire, the 21-item Beck Depression Inventory-II, the HIV Stigma Scale | 109 (57.2%) participants reported at least one suboptimal adherence behaviour, with 36 (20%) missing doses in the 4 days prior to the assessment; 97 (48.3%) failing to take medication on schedule; 40 (24.1%) failing to follow instructions; and 33 (18.3%) missing doses in the weekend prior. Participants who missed a dose in the four days prior had experienced higher levels of HIV-related stigma compared to those who did not miss doses in those days. Depression and HIV-related stigma was associated with failing to take medication on schedule in the four days before (p = 0.05 and p = 0.01, respectively). These factors were also associated with failing to follow instructions on how to take ARVs | Data on adherence and psychosocial factors were collected using self-reports, which could have resulted in under-reporting. The cross-sectional study design limits the studies ability to find causal conclusions and evidence of a history of adherence behaviours and psychosocial behaviours |
| Shippy et al., 2005 (USA) [43] |
n = 160 Age: 50–59 = 85%; 60+ = 15% Community |
A survey was used to collect variables of interest | The increasing group of ageing PLWH are facing isolation from informal networks due to HIV stigma and ageism. 71% of participants lived alone. Family members and partners are critical for informal support, however, only a third of participants had a partner. 86% of participants used Medicaid | The cross-sectional study design does not allow for causality analysis among mental health indicators, social networks, and support needs of older PLWH | |
| Zepf et al., 2020 (USA) [54] |
n = 281 M = 57.9 Hospital |
Self-reported questionnaires were used to collect data | Symptoms of depression (p = 0.008), stimulant use (p < 0.0001), and PTSD (p = 0.002) were significantly associated with reduced medication adherence. Intimate partner violence, binge drinking and past physical or sexual abuse were not significantly associated with lower medication adherence | Due to the study cross-sectional study design, causality or determination of the sequence of events could not be determined. Self-administered questionnaire answers are subject and may have led to desirability bias in findings | |
| Morillo-Verdugo et al., 2019 (Spain) [39] |
n = 223 Median = 53 years (52–57) Hospital |
Data were collected from an electronic medical record. Questionnaires and hospital dispensing records were used to measure medication adherence | The SMAQ questionnaire, the Morisky-Green questionnaire, and the Medication regimen complexity index | The median number of concomitant medications prescribed per participant was 3 (1–5) and the median number of co-morbidities was also 3 (2–4). Polypharmacy was noted in 56.1% of participants and 9.4% had higher polypharmacy. The polypharmacy was 60% cardiovascular, 27.1% was depression-anxiety, 7.1% was mixed and 5.8% was COPD. Participants with high pharmacotherapy complexity indices had a 50 times greater chance of polypharmacy. It was demonstrated that 11.25 was the best cut-off point to predict polypharmacy in older PLWH | A minor limitation is that private prescription and alternative medicines were not included. Another limitation is that the Medication regimen complexity index tool used is imperfect and has trade-offs between sensitivity and specificity. Also, some dosing options were missed, such as monthly doses |
| Schnall et al., 2018 (Australia) [99] |
n = 80 Control group: M = 51 years (SD = 9) Intervention group: M = 50 years (SD = 11.7) Community |
Intervention study: Symptom burden when using a mobile app with self-care strategies to manage symptoms was compared to a mobile app without the self-care strategies between 2016 and 2017. The study used mVIP, a web-app, that was created to help users self-manage their symptoms. Surveys were given weekly on the app. The study lasted 12 weeks | mVIP (a web-app) | Participants in the intervention group had a significantly higher improvement than the control group in the following 5 symptoms: depression (p = 0.001), anxiety (p = 0.001), neuropathy (p = 0.002), weight loss/wasting (p = 0.020), and fever/chills/sweat (p = 0.037). The intervention group also showed a higher improvement in adherence rates to ART medications than the control group (p = 0.017). Over the 12-week trial, mVIP was linked to improved symptom burden and adherence rates in PLWH | The study had limitations to the generalisability of study findings with a small sample size, and as participants with access to a smart-phone or tablet were required, PLWH who do not have or are unable to use this technology were marginalised |
| Gimenez et al., 2020 (Spain) [90] |
n = 42 Median = 70 years Hospital |
Observational, prospective study where data from hospital patient records were analysed using various tools | The Medication Regimen Complexity Index (MRCI), the Simplified Medication Adherence Questionnaire (SMAQ), the Morisky-Green questionnaire (MMAS) and the Revised Patients’ Attitudes Towards Deprescribing (rPATD) Questionnaire | A majority of participants agreed with the following three statements in relation to deprescribing, firstly, 91.9% agreed to “I have a good understanding of the reasons I was prescribed each of my medicines”, secondly, 89.2% reported that “Overall, I am satisfied with my current medicines” and finally, 89.2% agreed that “I like to be involved in making decisions about my medicines with my doctors” | The small sample size limits the generalisability of the data. Another limitation is the loss of information intrinsically in relation to the dichotomisation of the indices used for analysis |
| Patel et al., 2016 (UK) [40] |
n = 299 M = 58 years (SD = 2) Outpatient clinic |
Data were collected using self-reported questionnaires | One or more co-morbidities was present in 84% of participants and 61% had two or more. High cholesterol, hypertension, depression and sexual dysfunction were commonly reported. Multivariate analysis when adjusted for lifestyle factors, showed that number of years since HIV diagnosis, age, and duration of ART were significant predictors of co-morbidity. Multiple co-morbidities, polypharmacy and higher use of non-HIV services were reported in older PLWH | The self-reported nature of the questionnaire may have led to recall and self-presentation bias. As data was collected at a single timepoint, it was not possible to determine the direction of associations between co-morbidity and risk factors. Generalisability of findings are reduced to due single-site recruitment with a high prevalence of White men who have sex with men | |
| Kteily-Hawa et al., 2019 (Canada) [69] |
n = 1422 M = 55.81 years (SD = 5.25) in older women group Community |
Survey data from the Canadian HIV Women's Sexual and Reproductive Health Cohort Study was used. The questionnaire used in the study included the following nine sections: demographics and socioeconomic status, healthcare utilisation, medical and HIV disease information, stigma, and discrimination, HRQOL, and substance misuse | The 12-item Short Form Survey (SF-12), the Medical Outcome Trust scoring method, the 10-item Resiliency Scale, the Center for Epidemiologic Studies Depression 10-item scale, and the 4-item Abbreviated Social Support Instrument | Older participants had poorer physical HRQOL and less social support than younger participants. Mental HRQOL was similar between the groups. Better physical HRQOL was linked to resilience. Poorer physical health was linked to poorer mental HRQOL, food insecurity and depressive symptoms | The cross-sectional study design limits the ability to determine a causal relationship between correlates and causations of HRQOL. The self-report nature of the questionnaire may have been affected by social desirability biases. Recruitment may have been biased to include women already accessing HIV care, and thus experiencing higher physical functioning and resilience, lowering generalisability of results to those not accessing care |
| Sutton et al., 2016 (USA) [83] |
n = 15602 M = 52.1 years (SD = 9.5) Hospital and community |
Data were collected from the Veterans Health Administration electronic health record system from 2006 to 2012. Data included demographic details, vital signs, mortality, administrative claims, laboratory results, and pharmacy dispensing records | The Charlson co-morbidity index score | A significantly lower proportion of single-tablet regimen compared to multiple-tablet regimen participants had undetectable viral loads at baseline (p < 0.001). It was found that the single-tablet regimen participants had double the odds of being adherent, less chances of hospitalisation, and more chances of an undetectable viral load during follow-up, after controlling for baseline covariates | A limitation to the study was that pharmacy refill data was used as a measure of adherence, however, this may have overestimated adherence. The study was unable to exclude confounding factors that could have influenced the findings, as patients were not randomised to the two treatments. Despite attempting to control for some variables through multivariable models, residual confounding may have remained |
| McKetchnie et al., 2021 (USA) [58] |
n = 15 Age ≥ 50 years Community |
Data were collected using one-on-one interviews | The main themes highlighted from interview transcripts were firstly, the impact of chronic pain and its treatment on HIV care engagement, secondly, the impact of substance use on chronic pain, and lastly, interventions to target substance use and chronic pain. The results showcase the need for interventions addressing structural, physical, and psychological barriers to care engagement | The small sample size limits the generalisability of the data | |
| Heckman et al., 2002 (USA) [78] |
n = 83 M = 55.2 (SD = 5.1) Community clinics in two cities |
Self-administered assessment instruments were completed by participants | The Symptom Checklist-90-Revised, the Beck Depression Inventory, the Barriers to Care Scale, the Provision of Social Relations Scale, the HIV-related Life Stressor Burden Scale, and the Limitations Related to HIV symptoms question | 4% of participants had severe depression, 21% had moderate depression, 33% had mild depression, 42% had minimal or no depression. Participants reporting more psychological symptoms had higher HIV-related life stressor burden, less social support from friends, and experienced more barriers to services due to HIV-related stigma. Elevation of symptoms characteristic of somatisation was seen in participants | Due to recruitment being from only two sites, this may reduce the generalisability of the study findings. Also, the study used a self-selected sample. Participants were already connected to the AIDS service organisation; therefore they might already have their life-care needs met; study findings may underestimate the life chaos among participants |
| Haruna et al., 2021 (Tanzania) [56] |
n = 27 M = 54 years Hospital |
Data were collected through in-depth semi-structured interviews | Participants and healthcare workers held positive attitudes towards integration of services, they reported perceived benefits with this. Inconsistent and limited supplies, for example with screening equipment or medications, low awareness of non-communicable diseases among PLWH, insufficient training of healthcare workers on how to manage non-communicable diseases in PLWH, treatment costs and payment systems were factors hindering the integrations of services | Interviews being conducted within the clinic setting that participants usually received their care may have led to socially desirable answers. Recruitment from five large clinics in Dar es Salaam may not be representative of patients from other smaller clinics | |
| Fritsch, 2005 (Canada) [96] |
n = 22 under 50 years, n = 12 aged 50–65 years Hospital and community |
Data were collected via in-depth individual interviews | The majority of participants had positive experiences accessing medical services. PLWH over 50 years old reported being able to access the social and medical services they required to cope with HIV. Both the younger and older groups accessed a variety of medical services, although the later did slightly less. The older group utilised social and emotional supports and organisations to a similar or higher degree than the younger group | The generalisability of the study findings is limited due to the geographic location, sample size, non-random sampling and snowballing technique used | |
| Kim et al., 2017 (USA) [33] |
n = 250 Median = 50 years (44–56) Community |
Data were extracted from electronic medical records | Sedating medication and opioids were prescribed in 80 and 50% of participants, respectively. 51% of participants exceeded risky drinking limits. Illicit opioid use and illicit opioid sedative use was reported in 23% and 9% of participants, respectively, with 37% reporting lifetime non-fatal overdose and 7% past year non-fatal overdose. Participants were taking a median of 10 (7–14) medications and a median of 2 (1–3) sedating medications. The odds of a lifetime non-fatal overdose were increased with each additional sedation medication taken and any opioid medication. The prevalence of past year non-fatal overdose was higher with each additional sedating medication (p = 0.049) and non-ARV medication (p = 0.048) | Limitations to this study include the absence of a validated method to assess overdose history and the examination of only non-fatal overdose | |
| Shamu et al., 2021 (Zimbabwe) [52] |
n = 420 Median = 55 years Outpatient clinic |
Data were collected from electronic medical records | World Health Organization stage 3 or 4 conditions were present in 40% of participants at baseline. 15% of participants had hypertension at baseline and a further 27% reported incident hypertension at follow-up. 61.7% of participants had one or more chronic non-communicable disease. Results from the follow-up reported the most common incident co-morbidities to be hypertension, arthritis, and chronic kidney disease | The generalisability of the results is reduced due to the nature of the study being single-sited | |
| Hoang et al., 2009 (USA) [30] |
n = 1,018 M = 50.6 (SD = 9.4) Hospital and community |
Data were obtained from electronic medical records and by interviewing the Infectious Disease clinics chiefs at the five Veterans Affairs facilities | 93% of participants had co-morbidities with a mean of 3.2 co-morbidities (SD = 2). Viral suppression was achieved in a median of 231 days (SD = 411.6) by 52% of participants. Participants attending integrated clinics offering hepatitis, psychological, psychiatric, and social services were 3.1 times more likely to achieve viral suppression compared to those visiting clinics that only offered HIV care (Hazard ratio = 3.1, p < 0.001) | A limitation of this study includes that findings may be affected by the unmeasured differences between participants attending different clinics and healthcare providers skills varying, rather than the comprehensiveness of the care. Also, the potency of ART or its complexity was not measured. Duration of combined ART was not measured; therefore, it is not possible to determine whether this affected viral suppression | |
| Njie-Carr et al., 2021 (USA) [102] |
n = 20 completed baseline activities, n = 6 completed all activities, n = 7 included in focus group Age ≥ 50 years Community |
Intervention study: Participants were given The CARE intervention, a three-module intervention for three weeks followed by post intervention measures to test its utility | World Health Organization QOL BREF, Perceived Social Support Scale, Mood tracker, Geriatric Depression Scale, and HIV Self-Care for Symptom Management Survey | Participants found the CARE intervention useful and felt empowered utilising the app. Neuropathic pain (70%), anxiety (55%), fatigue (50%), and depressive symptoms (35%) were reported to cause high-intensity distress and negative impact on life to participants. It was reported that self-regulation and self-awareness improved, and there were positive trends in outcome measures | A small sample size limits the generalisability of the study results. Another limitation is the short intervention duration of three weeks. Also, the participants retained in the study may be healthier and more acquainted with technology |
| Singo et al., 2015 (South Africa) [45] |
n = 12 Age = 50–83 years Community |
Data were collected through interviews using an interview guide | The findings showed that HIV and AIDS can have negative effects on the lives of older PLWH. Socio-economic, household, psychological and emotional health burdens are critical areas in relation to older PLWH | The small sample size limits the generalisability of the data and the population recruited in may not be representative of other geographical areas |
ACH anticholinergic medication, ART antiretroviral therapy, ARV antiretroviral, CNS central nervous system, HAART highly active antiretroviral therapy, HRQOL health related quality of life, MOR medicines management optimisation review, PDDI potential drug-drug interaction, PLWH people living with HIV, PTSD post-traumatic stress disorder
Co-morbidities and Health-Related Quality of Life (HRQOL)
Most older PLWH are affected by multiple co-morbidities [14, 26–63]. One study reported 93% of participants having one or more co-morbidities, with a mean of 3.2 conditions per person [30]. Similarly, other studies have also shown the mean number of co-morbidities to range from 2.4 to 3.6 [39, 40, 42].
Older PLWH are more likely to be affected by anxiety, depression, cancer, chronic kidney disease (CKD), chronic pain, diabetes, hypertension, osteoporosis, hepatitis B/C infections than HIV-negative individuals [31, 32, 34, 36, 39, 42–45, 47, 51, 55, 58, 61]. A study comparing HIV-positive older males to their HIV-negative counterparts found that older participants were six times more likely to be diagnosed with osteoporosis [31]. Similarly, cardiovascular disease (CVD) and CKD are more common in older males living with HIV [31]. Other studies indicate a higher incidence of mental conditions in PLWH over the age of 50 years [30, 33, 36, 37, 43, 44, 64, 65]. One study [43] reported over half (58%) of participants experiencing depression, with a greater proportion having received treatment for depression in the year prior to the study. Poorer health outcomes have been associated with depression in ageing PLWH [66], and depression has also been linked non-adherence behaviour [66]. The duration since HIV diagnosis and time since ART initiation are predictors of co-morbidity, and both factors are associated with frailty [36, 40]. Frailty is linked to higher mortality rates among older PLWH, and its incidence increases with age, presence of co-morbidities, falls and disability [27, 28, 67]. The presence of one or more co-morbidities also increases the risk of falls in PLWH [50]. Among older PLWH, poor HRQOL is associated with co-morbidities, especially AIDS-defining illnesses, longer time since ART initiation, loneliness and a lower level of education [26, 54, 62, 65, 68–70]. A study focusing on women living with HIV showed that physical HRQOL was lower in older participants than in younger age groups [69]. Older PLWH are also more likely to have poor mental HRQOL than patients with other non-HIV conditions [26].
Concerns about co-morbidities and ageing have been reported by older PLWH in the qualitative studies reviewed [27, 41, 71]. One older participant expressed their frustration of having to manage HIV, ageing and co-morbidities, particularly when they do not know which is the cause of a health issue they are experiencing [41]. Another participant reported not knowing if they were tired due to getting older, their co-morbidities or side effects of their medicines [71]. Many PLWH who were diagnosed in the 1990s or just after the 2000s do not view HIV as their most pressing concern, but rather prioritise co-morbidities—their HIV is perceived to be under control due to adherence to ART [55].
Polypharmacy, Drug Interactions, and Adverse Drug Reactions
Polypharmacy
The average number of concomitant medicines used by older PLWH varies [13, 14, 32, 33, 38–40, 49, 52, 61, 70, 72–74]. Several studies have found that older PLWH experience more polypharmacy than HIV-negative participants [14, 29, 40, 72, 75]. One study reported 35% of participants received 16 or more medicines and 16% were using ≥ 20 long-term medicines. Two studies reported that 66% of participants experienced polypharmacy even when ARVs were excluded from the analysis [13, 20]. Co-morbidities are expectedly a precipitating factor for polypharmacy in older PLWH [38], and some studies have demonstrated a positive correlation between the number of conditions and the number of concomitant medicines used (p < 0.0001) [40]. Cardiovascular and gastrointestinal medicines were identified as the most common classes of concomitant medicines used by older PLWH in several studies [13, 14, 39, 40, 44, 52, 72]. Similarly, another study identified 667 potentially inappropriate medicines in 482 older PLWH with 60.8% (n = 293) involving benzodiazepines, 27.2% (n = 131) involving non-steroidal anti-inflammatory drugs, and 14.9% (n = 72) involving anticholinergic drugs [20].
Drug interactions
With higher prevalence of polypharmacy, drug interactions among older PLWH are common, including those occurring between ARV and non-ARV medicines, or between two or more non-ARV medicines [13, 14, 29, 31, 38, 40, 41, 44, 46, 48, 61, 64, 67, 71, 74–77]. A large number of drug–drug interactions have been identified in the ageing HIV population, as demonstrated in several studies reviewed, with up to 2552 potential drug–drug interactions (PDDIs) being identified in 1947 participants [13, 14, 29, 44, 61, 77]. A study comparing PDDIs between older and younger PLWH showed that a significantly higher proportion of older PLWH had at least one PDDI consisting of both an ARV and a non-ARV combination than those in the younger group (i.e., 913 compared to 201 potential interactions, respectively, p = 0.001) [14]. Moreover, older PLWH had a larger number of interactions that were classified as “Do not co-administer” than the older HIV-negative or younger HIV-positive groups [14].
In a study using the Beers criteria for PIP, the authors reported one or more potentially inappropriate medicines in half (52%) of all participants [13]. The most frequent drugs implicated were testosterone (n = 20), ibuprofen (n = 15), zolpidem (n = 9) and lorazepam (n = 5) [13]. Other studies measuring drug–drug interactions have listed the same drug groups, among others, as interacting with ART [13, 14, 29, 38, 40, 44, 49, 61, 73, 77]. PLWH were more likely to have a high anticholinergic burden, with 17% having a score of ≥ 3, in contrast to 4% seen among HIV-negative participants [13]. One study reported that statins have a high involvement in severe interactions (24%), followed by inhaled corticosteroids (15%) [77]. One study showed that 80% of participants were prescribed at least one sedating medicine, and the risk for a non-fatal overdose to occur in the past year was higher with each additional sedating medicine and non-ARV medicine, but this association was only marginally significant (p = 0.048) [33]. Another study assessing PIP and therapeutic complexity in older PLWH found at least one medication to deprescribe based on the STOPP criteria or the list of evidence-based deprescribing for chronic patients (LESS-CHRON) criteria in 70% of participants [49]. Meeting STOPP or LESS-CHRON criteria was significantly associated with the number of concomitant prescriptions (p = 0.008) [49].
Similarly, another study assessed the incidence and severity of drug interactions before and after ART simplification. In this study, the authors reported lower rates of PDDIs after regimen simplification, with median interaction scores being 3 (range 1–6) and 1 (range 0–2), respectively [29]. Moreover, this study showed that their participants were taking a median of three ARV pills a day, and discontinuing a protease inhibitor during ART simplification was a strong predictor for lowering the number of PDDIs [29]. Another study found that 70% of older participants had at least one drug–drug interaction that was categorised as ‘consider therapy modification’ and 11% had an interaction that was categorised as ‘avoid combination’ [13].
Adverse Drug Reactions
Adverse drug reactions such as cognitive impairment, delirium, dry mouth and constipation have all been reported among older PLWH [13, 20]. A study led by pharmacists in the USA to evaluate and reduce PIP identified an increase of 85% for the likelihood of an adverse drug event occurring with each inappropriate prescribing that occurs in older PLWH [38].
A mixed methods study with older African-American PLWH highlighted the effects caused by adverse drug reactions, with one participant explaining the stress caused by drug toxicity associated with her medicines on her body over time: “Even though I’m taking medicine to keep my immune system up and everything like that, it is still somewhat ‘wear and tear’ on my body” [64]. Long-term ART toxicity has been linked to early onset and/or a higher incidence of frailty among PWLH [67]. This uncertainty of adverse outcomes makes it difficult for older PLWH to predict their future care needs [27, 41]. In addition, physical changes experienced by PLWH relating to the condition, treatments and side effects can increase stigma levels and treatment burden, affect mental health and lower quality of life [26, 78].
Adherence
Several studies showed that older PLWH were more adherent to their ART than younger PLWH [32, 49, 54, 69, 76, 79–82]. Two studies found older women living with HIV were more likely to be adherent to ART, and subsequently be virally suppressed [69, 79]. McInnes et al. demonstrated that increasing age was associated with higher medicine adherence for PLWH. PLWH aged 55–64 years and those ≥ 65 years were twice or three times as likely to adhere than those under 45 years [81]. Two studies reported high adherence rates for ART among older PLWH but low adherence when taking their concomitant medicines [39, 44]. A study comparing adherence rates in older PLWH taking single-tablet or multiple-tablet ART regimens found that patients on a single-tablet regimen had significantly greater adherence than patients on a multiple-tablet regimen (p < 0.001) [83]. Simplifying medicine regimens can increase adherence in older PLWH [37, 48].
Several factors may explain higher rates of adherence to ART among older people, particularly longevity. It is likely that living longer allows older people to be better at taking their medicines throughout life and subsequently continue to live longer. Living longer with HIV may lead to many older PLWH experiencing HIV-related loss of friends/family, these experiences may have reinforced adherence behaviour [37], although newly diagnosed older people may not be affected by this concern. The association between social support and adherence to ART has been reported in studies [80, 84]. Older PLWH living with someone who knows their serostatus may increase their adherence rates due to increased social support (e.g., medicine reminders) [41, 45, 85, 86].
Nonetheless, barriers to achieving optimal adherence may affect older PLWH [66], including co-morbidities, regimen complexity and fatigue, mental health conditions and cognitive impairment, lack of social support and social isolation, and stigma [30, 36, 37, 54, 55, 61, 64, 66, 80, 82, 86, 87]. Practical difficulties (e.g., those associated with obtaining refills) can lead to medicine non-adherence among older PLWH [61, 81]. Some studies found that financial concerns, for instance costs of travel to clinic appointments, prescription costs or lacking basic necessities such as food, can lead to non-adherence in older PLWH [34, 57, 86, 88].
Treatment and Medicine Burden
Treatment burden is a broad concept and has been defined as the ‘work’ of being a patient, requiring significant investment of time, effort, attention and cognitive energy [89]. With a higher number of co-morbidities in older PLWH, polypharmacy can increase medicine burden [61]. Medicine burden is associated with regimen complexity, number, size and taste of daily pills, and side effects [13, 14, 17, 47, 74]. Side effects (e.g., diarrhoea, hyperlipidaemia) could result in additional prescribing cascades to manage symptoms, adding to the complexity of a treatment regimen [13, 33, 74].
Fragmentation of care can lead to missed diagnoses and inappropriate management of co-morbidities [27], and some patients may receive conflicting information from clinicians [57]. In another study, the desire for a comprehensive care programme for older PLWH including primary care, geriatric consultations and speciality care for co-morbidities was noted [27]. HIV-only clinics, which may not offer other services, may cause access challenges for older patients (e.g., poor co-ordination of appointments, travel difficulties, fatigue from prolonged waiting times at different facilities) [27, 35, 56, 57]. Many older PLWH may struggle with travel to and from clinic appointments due to physical difficulties, access to public transport or a personal vehicle/driving licence, or parking difficulties [27, 48, 58, 64]. A lack of transportation could lead to disengagement from care [57, 64]. Engagement in care is also related to everyday life demands and financial concerns [34, 45, 48, 57, 64, 88]. Older PLWH face significant burden with everyday tasks, such as shopping, managing medicines and keeping to daily treatment regimens, especially for those who require assistance with these tasks [32, 45].
One study measured treatment burden in older PLWH (mean age, 53 years) using a validated outcome measure (i.e., the Treatment Burden Questionnaire-13). Using a self-reported measure, Schreiner et al. found a mean treatment burden score of 22.8 (SD = 24.6) with overall findings indicating low level of treatment burden (58%, n = 60) in the sample population [42]. High levels of treatment burden were associated with remembering to take medicines throughout the day and associated limitations, and adhering to prescribed exercise regimens and administrative paperwork [42].
Medicine burden in older PLWH was measured using the Living with Medicines Questionnaire (Chinese version). Zheng et al. found that polypharmacy was associated with moderate-high levels of medicine burden [61]. Socioeconomic status, particularly lower income, was associated with higher medicine burden. Females were also reported to experience significantly more medicine burden than males (110.5 vs. 102.5, p = 0.002). Adherence levels were negatively associated with overall medicine burden (r = − 0.3, p = 0.001). Analyses of medicine burden domains showed similar correlations between adherence to ART and practical difficulties (r = − 0.3), communication/relationships with other HCPs (r = − 0.3) and interferences to day-to-day life (r = 0.2, p < 0.05). Nonetheless, the authors acknowledged challenges of self-reported data and small sample size (n = 185) recruited from two clinics within the Chinese Hunan province, limiting generalisability of findings from this study. Moreover, another study reported that 80% of caregivers strongly agreed/agreed that “My care recipient’s medicines are a burden to them” [90]. A study investigating women’s interest in long-acting injectable ART reported that the majority of participants preferred long-acting injectable ART (56%) over daily pills [91]. A participant in this study with a history of drug use indicated that injectable drugs users have unpredictable lifestyles that make daily pill taking challenging, whereas an appointment every 1 or 2 months would be more manageable [91].
Stigma and Need for Social Support
Stigma
Findings from the studies reviewed indicate that stigma is still prevalent among PLWH, and more so in older persons [27, 34, 37, 41, 43, 48, 50, 55, 64, 66, 71, 78, 84, 86, 92–95]. Several studies have reported that older PLWH experience more stigma than younger PLWH due to the HIV condition and age-related stigma [34, 41, 43, 64, 86, 96]. Many HIV-positive participants experience psychological burden arising from being stigmatised by partners, family members, friends, work colleagues, insurance companies, housing departments, law enforcement officials, and healthcare professionals [55, 92]. Studies have also suggested that poor mental wellbeing or anxiety among older PLWH may be linked to greater stigma levels [26, 95]. Older PLWH who are long-term survivors of HIV may also experience stigma from healthcare professionals, leading to instances of disengagement from care [55, 64]. HIV-related stigma can create barriers to accessing support and increase non-adherence rates [34, 37, 43, 55, 66, 86]. A study exploring stigma and engagement in HIV care among older PLWH found that there was a significant correlation between negative self-image stigma and engagement in care (r = − 0.38, p = 0.03) [64]. Similar to the general population, some older PLWH may worry about being recognised by a friend or family member while attending appointments at an HIV clinic [34, 64]. Stigma can affect an older person’s sense of self-worth and contributes to mental distress [92]. Moreover, many older PLWH want more support services to address mental health, stigma and isolation [27, 34]. Furthermore, studies exploring stigma in older African American PLWH found individuals experienced stigma due to ethnicity, gender identity, sexual orientation and socio-economic status [37, 64, 95, 96]. Another study comparing older and younger PLWH reported that participants over 55 years of age experienced less internalised stigma than the younger groups under the age of 40 years, possibly due to learning to cope and manage negative aspects of living with HIV and the associated stigma over time [64, 93].
Need for Social Support
Themes around social isolation, loneliness and a need for support among the ageing HIV population have been highlighted in the studies reviewed [27, 32, 34, 41, 48, 68, 69, 71, 78, 80, 84, 87, 93, 97]. A study focusing on geriatric assessments in older PLWH indicated that up to 50% had low social support and nearly 60% showed some form of loneliness [32]. One study reported lower levels of social support among older HIV-positive women than younger HIV-positive woman (p < 0.001) [69]. In another study, those who reported more instances of hostility, temper outbursts and arguments tended to alienate potential allies and therefore not receive vital sources of emotional support [69, 78]. Lower mean social support scores were reported among participants who had a high prevalence of mental conditions, psychosocial stressors and disrupted social systems [78, 80]. Older PLWH’s need for improved social support networks was evident in the studies reviewed, with one patient suggesting: “We should have. . .somewhere we can go and socialise. . .have lunch and have social workers there, if we need to get stuff done. For me, I live alone, I have friends but sometimes my friends work and I like to get out and be around other people socially during the day, I have groups but they are in the evening, but in the daytime I'm just stuck at home” [27, 32]. One study observed a statistically significant association between adherence and social support in older PLWH (p = 0.02) [80]. Similarly, other studies have shown that support from family members was highly rated as a facilitator for medicine adherence and engagement in care [34, 87].
A recent study on older PLWH and substance use disorders found that social support is critical to minimising treatment interruptions [97]. Studies have also suggested the usefulness of peer support groups, particularly to counteract the social isolation and stigma experienced by older HIV-positive people [34, 41]. One study showed that older adults accessed fewer HIV-related health information sources than the younger participants, including primary-care physicians, family/friends, the HIV clinic, support groups, and the Internet [96]. Moreover, one study found only 14.8% (n = 77) of participants reported being linked to one or more HIV support groups or communities [85]. Older adults living with HIV have suggested the need for age-specific peer support groups as some have felt out of place at support groups consisting of younger participants [34, 96]. One study suggested that social welfare programmes and primary health promotion should focus on educating older PLWH and their service providers on methods to cope with health and social difficulties of ageing with HIV [45].
A study conducted in Canada reported that all participants attended at least one mental health service, including local drop-in services, support and self-help groups, and visiting therapists [92]. Participants described achieving resilience by lowering the space that HIV occupies in their lives, creating lifestyle changes around the illness and engaging in social support [92]. Another study found that older and younger PLWH access a similar number of social and emotional supports, and the older group reported fewer barriers to accessing medical and social services than the younger groups, but this was not statistically significant [96].
Patient and Healthcare Provider Relationships
Older persons’ wants and desires for comprehensive and integrated care are noteworthy. Some older persons want healthcare professionals to consider different HIV- and age-related co-morbidities, with one participant describing concerns with their HIV doctor focusing on viral loads and not their co-morbidities as they aged [27]. Some older PLWH reported that provider perceptions may negatively impact HIV care and lead to late diagnoses. Perceptions about sexual activity among older people are associated with poorer care around sexually transmitted infections [79].
In addition, a study investigating the pharmacist’s role in HIV care in France reported that 21.6% (n = 233) of participants would agree to interviews with pharmacists during ARV dispensing to improve their knowledge and help manage their ART, and 18.9% (n = 204) would participate to improve their follow-up and compliance [59]. It was reported by 94% of pharmacists recruited in this study that more training would be required for them to manage and address the needs of PLWH [59]. One study using patient and provider focus groups found that healthcare providers need a deeper knowledge base to care for the ageing HIV population [27]. In another study, 83.8% of participants reported that they would be willing to stop one or more of their regular medicines if their doctor said it was possible [90].
Some older PLWH have reported concerns regarding fragmentation of HIV care services [14, 27, 30, 34, 35, 55, 57, 64]. A study evaluating the impact of integrated HIV care on patient health outcomes found that patients attending HIV clinics that also offered other services (e.g., hepatitis treatment, psychological and social services) were three times more likely to achieve better clinical outcomes (e.g., viral suppression) than patients attending HIV-only clinics (p < 0.001) [30].
Interventions Used in Studies of Older PLWH
A total of nine interventions were presented in the studies reviewed (Table 2) [37, 38, 53, 87, 94, 98–102]. Five of the interventions were designed to improve adherence to medicines, two utilised medicine reviews, and two interventions focussed on self-management apps.
Table 2.
Summary of intervention studies
| First author, year (country) | N | Age of participants | Study design | Mode of delivery | Intervention/s reported | Objectives | Effectiveness of the intervention and statistical significance |
|---|---|---|---|---|---|---|---|
| Ventuneac et al., 2020 (USA) [53] | 406 | M = 50.7 | Single-arm prospective trial | Mobile application: Assessments at baseline and six months for pre-post within-group comparisons, and between-group comparisons with matched sample patients not enrolled in the trial | Rango (mobile health application) |
Promote Care engagement and medication adherence by: • Addressing knowledge, skills, and motivation for HIV care engagement • Creating a sense of community via peer support • Coordinating care and other support services • Tailored medication and appointment reminders Access to integrated services within Rango for referrals to social services |
• The majority of Rango participants were engaged in care: 95% (387/406) returned for medical follow-up appointment • Significant difference in the number of unsuppressed participants (n = 65) at baseline who were suppressed (n = 38) at six months (p = 0.006) Viral suppression among Rango participants and those receiving usual care were similar (p = 0.84) and increased in both groups at six months (p < 0.001) |
| DeFulio et al., 2021 (USA) [98] | 50 | M = 52.4 (SD = 10.7) | Randomised controlled pilot study with a two-group parallel design | Mobile application: Videos had to be submitted of medication consumption. Surveys were given at baseline and monthly for six months | Medication Event Monitoring System (MEMS) cap and smartphone-based intervention app ("SteadyRX") |
Pilot clinical trial to demonstrate feasibility and acceptability of the SteadyRX app developed to increase adherence in PLWH with a substance use disorder The app consisted of: • The “PillWatch” section to record and submit selfie videos demonstrating ART adherence • The “MyRewards” section to monitor monetary incentive earnings of adherence The “InTouch” section for listings and contact information for community resources, adherence documents and app instructions |
• At six months the intervention group using SteadyRX, had a higher adherence than the control group (p = 0.037) The intervention had high acceptability and usability, with intervention participants submitting a mean of 75% of possible videos, with 81% of these meeting the validity criteria |
| Moitra et al., 2011 (USA) [87] | 16 | M = 52.5 (SD = 5) | Mixed methods |
Group sessions: Three to five weekly 60-min sessions. Treatment consisted of experiential group exercises, role-play, and homework |
Acceptance-based behaviour therapy |
Core principles of sessions included: • Developing “creative hopelessness”, highlighting issues relating to direct cognitive and emotional control strategies • Cultivating a willingness to accept HIV-related distress • Clarifying and focusing on life values This study focused on: • Feasibility and acceptability of the intervention Changes in CD4 counts and viral loads from baseline to the end of the intervention |
• Six (37.5%) participants found the intervention very helpful, six (37.5%) found them moderately helpful, and four (25%) found them minimally helpful • Mean CD4 counts increased from 372.3 (SD = 167.4) to 487.3 (SD = 225.3) and viral loads decreased from 148.8 (SD = 130.1) to 16.0 (SD = 24.8) from baseline to the end of the intervention • Participants enjoyed discussing which medicines worked, which were toxic to the body, and which tasted bad Familial and romantic relationships were discussed to be a key factor when troubleshooting life with HIV |
| Date et al., 2022 (UK) [101] | 164 |
MOR: Median = 59.5 (SD = 50–78) Standard care: Median = 60 (SD = 50–82) |
Randomised controlled study |
Medicines Management Optimisation Review (MOR): Participants were randomized to either receive standard care or the MOR intervention |
Medicines Management Optimisation Review toolkit, the University of Liverpool and Toronto General Hospital HIV drug interaction references, EuroQol five-dimension five-level (EQ-5D-5L) questionnaire and visual analogue scale (EQ-VAS) |
Core objective of the MOR toolkit: • Increase patient safety by identifying and reviewing patients at high risk for polypharmacy or drug–drug interactions This study focused on: • Examining the feasibility and acceptability of the MOR intervention The MOR toolkit consisted of: • A user guide • ‘My Clinic Companion’, a patient self-reported questionnaire of medicines and adherence The ‘MOR consultation form’ to assist with and provide a record of the patient consultation |
• Significantly more medicine-related problems were identified in the intervention group at baseline (p = 0.001) and 6 months (p = 0.001) • There was a significant reduction in new medicine-related problems at 6 months in the intervention group compared to baseline (p = 0.001), with 44% being resolved at baseline and 51% at 6 months • There were no changes in HRQOL identified between groups or after the intervention Participants and healthcare professionals found the MOR highly acceptable |
| McNicholl et al., 2017 (USA) [38] | 248 | M = 57.8 (SD = 5.1) | Prospective randomised interventional trial |
Medicine review: Pharmacists reviewed electronic drug charts |
Pharmacist medication reconciliation, Beers and STOPP criteria, Patient Health Questionnaire-9, the Montreal Cognitive Assessment, and the Veterans Ageing Cohort Study (VACS) Index | This study utilised the Beers Criteria and Screening Tool of Older Persons’ Potentially Inappropriate Prescriptions (STOPP) instruments to assess potentially inappropriate prescribing (PIP) |
• Participants were prescribed a mean of 11.6 ± 5.7 non-ARV medicines. 35% were receiving 16 or more medicines • PIP was identified in 54% and 63% of participants • 25 contraindicated drug interactions were found in 20 participants • At least 69% of participants had at least one medicine stopped, with almost 10% stopping six or more after reviewed by the pharmacist Over 40% of participants had at least one Beers or STOPP criteria that needed immediate correction |
| Bogart et al., 2021 (USA) [94] | 76 | Median = 52.9 (SD = 12.9) | Pilot randomised controlled trial | Cognitive behaviour therapy: Eight session group intervention. Data were collected at baseline, two-, four-, five-, and seven-months | Cognitive behaviour therapy, dialectical behaviour therapy, Medication Event Monitoring System (MEMS) bottle cap |
Sessions aimed to: • Improve coping with intersectional stigma • Address medical mistrust • Improve treatment adherence The intervention included psychoeducation on: • Discrimination • HIV disparities • Treatment adherence |
• Primary outcome (adherence): both electronically monitored (p = 0.06) and self-reported (p = 0.02) adherence increased in the intervention group compared to the control group from baseline Secondary outcome (coping, medical mistrust, and internalised stigma): Intervention participants showed slightly lower negative religious coping (p = 0.06) and significantly lower medical mistrust (p = 0.02) |
| Mao et al., 2018 (Australia) [37] | 98 | Median = 51.5 years (26–65) | Randomised controlled trial and mixed-method evaluation | Mobile phone reminders: The project consisted of two components, the six-week campaign (intervention arm with two groups and a control arm of one group) and a mixed-methods evaluation (online survey and interviews) | SMS reminders to mobile phones |
This study aimed to assess the following two topics: • Feasibility and acceptability of the SMS reminders for ARV adherence The potential impact of SMS reminders on adherence and disease self-management |
• SMS reminders were deemed acceptable and feasible • No statistically significant differences in adherence between intervention and control Lower perceived stigma was independently associated with better ARV adherence (p = 0.026) |
| Schnall et al., 2018 (Australia) [99] | 80 |
Control group: M = 51 (SD = 9) Intervention group: M = 50 (SD = 11.7) |
Randomised controlled trial | Mobile application: Participants were given surveys each week for 12 weeks. Both the intervention and control groups used the app, but only the intervention group received self-care strategies | mVIP (mobile health application) | The app provided 143 self-care strategies for 13 different symptoms |
• Participants in the intervention group showed significantly higher improvement that the control group in the following symptoms: anxiety (p = 0.001), depression (p = 0.001), neuropathy (p = 0.002), fever/sweat/chills (p = 0.037), and weight loss/wasting (p = 0.02) Greater adherence to ARV were reported in the intervention group compared to the control group (p = 0.017) |
| Njie-Carr et al., 2021 (USA) [102] | n = 20 baseline activities, n = 6 all activities, n = 7 focus group | ≥ 50 years | Mixed methods | Mobile application: Participants were given post intervention measures (Focus group and surveys) to complete after three weeks of using the app | ThE CARE Intervention (web-based app), World Health Organization QOL BREF, Perceived Social Support Scale, Mood tracker, Geriatric Depression Scale, HIV Self-Care for Symptom Management Survey, the Treatment Management Questionnaire, the Treatment Self-regulation Questionnaire (TSRQ) |
The app aimed to increase the autonomous motivation and perceived competence of individuals to self-manage disease symptoms and increase engagement with others The app included the following: • two 3–5 min videos on HIV transmission risk reduction • HIV and aging • Free text health promotion strategies • Mood tracker, reflective journal, self-efficacy measures, and links to resources for self-monitoring Remote individual clinician and peer support |
• Participants found the app useful and “felt empowered” using it • Self-awareness and self-regulation improved Increases in mean scores were reported for treatment confidence, help-seeking, and internal motivation for treatment entry and adherence |
ART antiretroviral therapy, ARV antiretroviral, HRQOL health related quality of life, PIP potentially inappropriate prescribing, PLWH people living with HIV
Adherence Interventions
SMS reminders were used as ART adherence support in one study [37]. This involved a 6-week campaign, where reminder messages were sent to each participant’s mobile phone by the study co-ordinator. The campaign randomly assigned participants to two intervention groups and one control group. Two intervention groups received two-way SMS reminders three and two times per week, respectively. Intervention groups were required to reply immediately, with the first SMS being “Stop, drop and pop. Take your ART meds now. Have you taken ART drugs on time in the last 48 h?”, if the response was “Yes”, the next SMS would be “Perfect med adherence. Great job!”, if the response was “No” or “Not yet”, the following SMS would be “Please take your meds ASAP. If you need any help, please contact BGF.” The control group received one-way non-specific greeting messages once weekly and were not required to respond and received a general SMS, such as “G’day, BGF wishes you a nice day!” The author reported no statistically significant differences between the intervention and control arms at the end of the SMS campaign [37]. The intervention was useful for adherence support and reassurance for some participants, but others perceived limited effectiveness especially those on established long-term ART.
In another adherence intervention, a Smartphone app (SteadyRX) was tested through an RCT. The intervention group received the smartphone app and usual care, whilst the control group received usual care only [98]. Each participant was given login details to access three sections of the app: (a) the “PillWatch” section allowed users to upload video recordings within in a 6-h dosing window with SMS notifications sent daily 30 min before the start of the dosing window, (b) The “MyRewards” section allowed users to view their monetary incentives for adherence, for example, the number of consecutive days of adherence, countdown to bonus earnings, total earnings, and current balance, (c) The “InTouch” section provided additional resources e.g. adherence-related documents, a user guide/manual, and contact information. Study participants were followed up monthly for 6 months, and adherence was measured by Medicine Event Monitoring System (MEMS) caps. The percentage of adherent participants in the control group reduced across the study duration, with a significant difference between the control and intervention group being evident at 6 months (p = 0.037), with the latter being more adherent [98].
A mobile health intervention app, Rango, designed to support care engagement and treatment adherence for PLWH, was evaluated in a pre-/post-intervention study [53]. The app consisted of three primary components. Firstly, a social network interface to facilitate social support, secondly, personalised medication and appointment reminders, and thirdly, access to services within the app for social services referrals based on each patient’s needs [53]. Participants responded positively to the app and found it acceptable. Lower patient activation of the app was associated with reports of missed doses [53]. A statistically significant difference was evident in the number of participants with unsuppressed viral loads becoming suppressed post-intervention with the Rango app (p = 0.006) [53].
Acceptance-based behaviour therapy was used in another study to promote ART adherence. This intervention used direct cognitive and emotional control strategies, for example encouraging participants to accept HIV-related distress, and to focus their own values [87]. Intervention activities included experiential group exercises, role playing, and homework completed in weekly sessions lasting 60 min. Most participants (75%) found the groups to be helpful [87]. The study reported that qualitative observations suggested that the acceptance-based intervention strategies were well suited to the target population [87]. The sessions emphasised psychological acceptance of the condition and medicines and avoiding denial. The participants reflected on medicine effectiveness, side effects, and taste [87]. The study emphasised social support when living with HIV. This intervention was perceived as less judgemental than compared to traditional approaches for increasing adherence [87].
An RCT using cognitive behavioural therapy utilised psychoeducation to discuss HIV disparities, discrimination and treatment adherence. Adherence was measured electronically using Medication Event Monitoring System (MEMS) bottle caps and through a self-reported questionnaire. A significant improvement in self-reported adherence was seen among participants (p = 0.02) [94]. Electronically monitored adherence showed an increase in adherence; however, this was not significant (p = 0.06) [94]. The study reported high intervention acceptability by participants.
Pharmacist-Led Medicine Reviews
Medicine reviews/reconciliations were conducted by pharmacists in a study evaluating polypharmacy and PIP in older PLWH (n = 248) [38]. This study found 54% and 63% of older people had PIP when using the Screening Tool of Older Persons’ Potentially Inappropriate Prescriptions (STOPP) and Beers criteria, respectively [38]. Pharmacist-led reviews led to discontinuation of PIP in older PLWH with two medicines stopped, on average, per patient. At least one medicine was stopped in over two-thirds (69%) of older PLWH, while six medicines were stopped in ≥ 10% of older persons [38]. Pharmacists play a big role in optimising medicines for older PLWH, and this study found that nearly half of participants had one or more medicine-related problems (e.g., drug interactions, duplication of medicines, high dosage, use of medicines with higher anticholinergic burden) that needed urgent attention by the pharmacist. The study provides useful insight regarding how pharmacist involvement in HIV care can potentially improve pharmaceutical care outcomes. Regardless, the authors recognised limitations around sample selection and excluding potentially inappropriate prescriptions that required a multidisciplinary approach. The study lacked a control/comparator and did not appear to report effectiveness of this pharmacist-led intervention.
A Medicines Management Optimisation Review (MOR) toolkit aids the identification and reviewing of patients that are high risk for polypharmacy and PDDIs to improve patient safety [101]. It consists of a user guide, a patient-orientated questionnaire promoting self-report and adherence to medications named ‘My Clinic Companion’, and the ‘MOR consultation form’ that is used to record the information elicited in the patient consultations and primary-care/hospital records, and to identify beneficial interventions, such as adherence education and smoking cessation [101]. An RCT evaluating the toolkit reported 93 medication-related problems (MRPs) (e.g., PDDIs, dose adjustments, and potential adverse drug reactions) in the intervention group and two in the standard-care control group at baseline. Six to 8 months later, 33 new MRPs were identified in the intervention group compared to three in the control group (r = 0.4, p = 0.001) [101]. More participants in the intervention group had polypharmacy compared to the control group. A reduction in non-ART drugs was evident at 6 months in the intervention arm; however, this was not significant (p = 0.217) [101]. There were no significant changes in HRQOL in both groups throughout the study. Thirty-eight patients completed patient satisfaction questionnaires, and all agreed that the service provided was excellent or very good, most agreed that they had an increased confidence in managing their medicines post intervention [101].
Self-Management Interventions
A self-management app (mVIP) covers 143 self-care strategies for different symptoms including anxiety, depression, sleeping difficulties, cough/shortness of breath, diarrhoea, memory difficulties, fatigue, dizziness, fever, chills/sweats, neuropathy, nausea/vomiting, skin issues and weight loss/wasting. App users are guided through questions relating to symptoms and based on their responses, self-care strategies are recommended [99, 100]. In an RCT, weekly surveys were given through the app asking participants if they had experienced one of the symptoms in the past 7 days and how much they were bothered by the symptoms [99]. For bothersome symptoms, the intervention group was given self-care strategies and illustrative videos. After the RCT was complete, the follow-up study used convenience sampling to recruit participants to focus groups [100]. Common symptoms reported by participants included difficulty sleeping, anxiety, neuropathy and depression [99]. The intervention group showed improvements in 12 out of 13 symptoms compared to the control group [99]. The RCT trial study did not find a significant difference in HRQOL between the groups; improvement in ART adherence was found in the intervention group [99, 100]. The intervention group found the app useful for self-care strategies to manage their HIV-related symptoms [99]. Participants suggested the addition of more languages to the app [99, 100]. The ability of the intervention group to review symptoms previously logged was reported as being useful and could potentially aid interactions with healthcare providers [100].
ThE CARE (Technology Enhanced Competence, Autonomy, and Relatedness Intervention for Elderly women with HIV) uses a web-based app to provide users with interactive features and functionality within modules to enhance physical and psychosocial functions and increase self-determination of older PLWH [102]. A study conducted a pre-/post-test intervention using ThE CARE app [102]. Overall, participants found the app and information useful, despite some encountering challenges navigating the contents of the modules. Participants found the social support aspect of the intervention positive, with one participant stating “…support groups are so important because I would die to have somebody to share with daily…” [102]. During the post-intervention focus group, all seven participants agreed that they would recommend the app to other PLWH [102]. Although not statistically significant, slight improvements were seen post intervention for treatment confidence, seeking help, and internal motivation for treatment entry and adherence [102].
Discussion
This systematic review was designed to identify the main issues and concerns in relation to medicines in the ageing HIV population, the interventions available to target these concerns and for medicines optimisation, and how effective the interventions are. There were a variety of tools used among the studies to identify and quantify issues, such as stigma, polypharmacy, drug–drug interactions, and frailty. However, the studies reviewed were largely descriptive, with only nine intervention studies reported out of the 79 appraised. A majority of the studies included were conducted in the USA, whereas only five were conducted in the UK, highlighting the need for further research in this population.
The priority issues and concerns identified in the studies reviewed were co-morbidities, HRQOL, polypharmacy, drug interactions, adverse drug reactions, adherence, medicine burden, treatment burden, stigma, social support and patient-healthcare provider relationships. The results of the review showed that these issues are interrelated with complex impacts on each other, and so must be considered holistically when optimising the medicines of older PLWH. A higher number of co-morbidities have been reported among the ageing HIV population compared to younger PLWH and the HIV-negative population of the same age. The studies reviewed have shown that older PLWH have an average of three co-morbidities, with duration since HIV diagnosis and ART initiation being predictors of co-morbidity. As the number of concomitant medicines taken by older PLWH increases with the number of presenting co-morbidities, this leaves this population vulnerable to potential drug–drug interactions. There is evidence from the included studies that the conditions that affect this population the most are gastrointestinal, mental health, cancer, CKD, diabetes, CVD, chronic pain and osteoporosis. It has been reported that this population hold uncertainty about the physical, psychological and social impacts of ageing with HIV. Moreover, there are concerns that certain conditions are being overlooked in older PLWH, this could lead to late diagnosis and the potential addition of medicines that could have been avoided if earlier screening occurred. A poor physical HRQOL can be observed in older PLWH, and has been associated with a history of AIDS, a longer duration since ART initiation, multiple co-morbidities, and loneliness [26, 68, 69]. Lower mental HRQOL has been observed in HIV-positive adults compared to HIV-negative adults [26]. Moreover, depression has been linked to poorer health outcomes in this population [66]. Mental health conditions in older PLWH have been mentioned as a concern across several studies in this review, including depression, anxiety and, although not as common, one study showed post-traumatic stress disorder (PTSD) in 12.5% of long-term survivors of the disease [32, 92]. A participant from one study described his fallout and anger that he experienced when unexpectedly surviving HIV with the term “reactive depression” [92]. This suggests support for further research in this area and in HIV survivorship [103, 104]. Moreover, one study reported mental disorders as being the most prevalent co-morbidity in older PLWH, with other studies also reporting high incidences of mental illness [30, 33, 36, 37, 43, 44, 64].
The studies reviewed have shown that older PLWH experience higher rates of polypharmacy than younger PLWH and HIV-negative people [14, 29, 40, 72, 75]. Several studies in this review have identified a high number of drug–drug interactions in the ageing HIV population. Commonly prescribed concomitant medicines in older PLWH have been reported to interact with ART; examples include statins, proton pump inhibitors, antidepressants, phosphodiesterase-5 inhibitors and inhaled corticosteroids. These interactions can result in negative and unpleasant effects for the patient. Older PLWH have expressed drug toxicity of medicines causing stress on their body over time. Adverse drug reactions and physical changes relating to their HIV disease can increase the stigma and treatment burden, affect mental health, and lower the quality of life experienced by older individuals with HIV. Long-term ART toxicity and the presence of co-morbidities has been reported to increase the incidence of frailty [27, 28, 67]. Frailty is an emerging concern among the ageing HIV population and can have a significant impact on clinical care and health outcomes [105]. The STOPP and Beers criteria are validated tools that are useful in identifying PIP, drug–drug interactions, drug-disease interactions, and medicine to avoid in older adults [106]. Several studies in this review highlighted the usefulness of using such tools and medicine reconciliations in older PLWH [13, 20, 38, 49, 73], with the Beers criteria evident in over 50% of participants in two studies and over 60% of participants with the STOPP criteria in one study [13, 38]. Moreover, medicine reconciliation leading to an average of two medicines being stopped per patient in one study is incredibly important, particularly when each PIP can increase the likelihood of ADRs by 85% [38]. Simplified medicine regimens leading to increased adherence rates and less adverse drug reactions of medicines can potentially reduce the number of further medicines needed. It is important that the cause of ADRs is identified and treated to prevent further inappropriate prescribing. Pharmacist reviews are therefore effective in reducing both polypharmacy and potentially inappropriate prescribing [38, 39]. The findings from this review suggest that using medicine reviews to target individuals affected by polypharmacy would have the highest yield and greatest impact in reducing PIP [38]. Medicine reviews can lead to ART simplification, reducing polypharmacy, pill burden and PDDIs, and improve health outcomes [29].
Co-morbidities, polypharmacy, regimen complexity, medicine refill difficulties, stigma, mental health disorders, poor finances and low social support are all factors that lead to suboptimal adherence in the ageing HIV population. Older adults who have been living with HIV for a long time and have witnessed the loss of friends and family to the disease have reported that the importance of medicine adherence has been reinforced within them through these experiences [37]. This may be the reason for higher adherence rates of ART reported in some studies among older PLWH compared to their younger counterparts. A higher adherence rate for ARTs compared to concomitant medicines suggests that some patients prioritise medicine based on their beliefs and perceptions of their importance [39, 44]. Medicine regimen complexity may leave patients confused about how to take their medicines, and this in addition to the number of medicines taken, pill size/shape, and dosing instructions can increase medicine burden. Co-morbidities, polypharmacy and adverse drug reactions increase the medicine burden experienced by older HIV-positive adults. Further to medicine burden, the difficulties experienced by older PLWH adhering to their medicines and treatment regimens can lead to treatment burden. This includes the time and effort taken to manage medicines, attending clinic appointments, laboratory tests, lifestyle changes and self-monitoring. A higher number of co-morbidities can lead to higher requirements to maintain the treatment of each condition, thus augmenting the treatment burden.
Despite the advances in HIV care, older PLWH are still facing stigmatisation not only for their serostatus but also due to ageism. In addition, race, gender identity, and sexual orientation have also been reported to cause stigmatisation [37, 64, 95, 96]. This has led to an increase in mental burden, decrease in mental wellbeing, and lower engagement in care [26, 64]. Stigma can create barriers to accessing care services and subsequently lower adherence in older PLWH [34, 37, 43, 66]. Moreover, previous mistreatment and stigmatisation from healthcare professionals and the anticipation of future instances can cause disengagement from care [64]. Other examples of stigma experienced include stigma due to misinformation, physical appearance, discrimination, and compounded stigma [66, 71, 78, 92].
The need for social support was a common theme across the studies reviewed. Lower levels of social support have been seen in older PLWH compared to younger PLWH [69]. Several studies have reported an association between social support and adherence to medicines [41, 45, 80, 85]. Social support has also proven critical for PLWH with substance use disorders to help them avoid treatment interruption [97]. Low social support has been observed among older PLWH who have a higher prevalence of psychiatric illness and psychosocial stressors [80]. Older HIV-positive individuals have expressed a need for more support services focusing on mental health, stigma and isolation [27, 34]. Targeting vulnerable individuals and providing this support could help to prevent negative health outcomes in this population. Current peer support groups for PLWH of all ages have left older HIV-positive adults feeling out of place and wanting age-specific groups [34, 96]. Social support among older PLWH is of particular interest within the UK as in 2017 it was reported that 82% of this population experienced moderate to high levels of loneliness [107]. Understanding the role of stigma and resilience is vital, since these factors may contribute to mental health co-morbidities and the addition of further medicines in older PLWH.
The fragmentation of services for PLWH is particularly of concern, due to difficulties involved in travelling between care facilities, time taken for visits, and finances [27, 30, 34, 35, 48, 56]. Older PLWH have expressed concerns of missed diagnoses of co-morbidities as they age due to fragmentation of care [27]. They have also suggested a need for specific care programmes tailored to their requirements. Studies have shown the effectiveness of integrated HIV care, with patients being three times more likely to be virally suppressed than clinics with HIV services alone [30]. Therefore, providing integrated care for the management and treatment of co-morbid conditions is vital for long-term care in this population [30, 34, 55, 56].
Implications for Research and Practice
The medicines optimisation interventions in the studies reviewed targeted medicine reviews, adherence, and physical and psychological self-management methods. Five interventions were technology based, requiring a mobile phone and/or internet accessibility. The interventions were well received by most of the participants, showing the desire and usability of medicines optimisation interventions among this population. The reported interventions exhibited positive outcomes in adherence among participants. For instance, SteadyRX, a Smartphone app, utilising daily SMS reminders, monetary incentives for adherence, and adherence-related documents reported increases in participant adherence [98]. Similarly, another mobile intervention app, Rango, providing daily reminders, access to social services referrals, and facilitating social support, demonstrated increases in suppressed viral loads among participants post-intervention [53]. Participants in one study using acceptance-based behaviour therapy to increase adherence found it helpful and perceived it as less judgemental than traditional adherence interventions [87]. In addition, increases in adherence were reported in participants using mVIP, a self-management app [99, 100]. The web-based app ThE CARE showed small improvements in treatment confidence and internal motivation for adherence among participants through modules to increase physical and psychosocial functioning with a social support aspect; however, the difference was not significant. Medicine reviews/reconciliations and a MOR toolkit to reduce PIP and PDDIs were effective among intervention studies, with an average of two medicines being discontinued per patient in one study [38], and significantly more MRPs being identified in intervention groups compared to the control (p = 0.001) in another study [101]. However, the majority of the key issues of concern for older PLWH regarding their medicines, as identified in this review, were not reflected in the few studies with interventions. The need for social support and its importance was highlighted in the studies included as a fundamental medicines optimisation intervention. The lack of medicines optimisation interventions targeted specifically for older PLWH reinforces the need for further research exploring these key issues within this population, utilising a variety of qualitative and quantitative methods. This would then inform subsequent work for the design, implementation, and evaluation of medicines optimisation interventions in older PLWH with the intention to improve patient health outcomes.
Study Limitations
Many of the studies included in our review had a small sample size. The adherence interventions reported in the studies reviewed focus on adherence of ART and have not considered concomitant medicine, which is prevalent in the older HIV population. A majority of the studies include people who have been living with HIV for many years and therefore the data may not be generalisable to newly diagnosed PLWH 50 years of age and over. Although searches of multiple databases and grey literature were conducted, it may be possible for some relevant papers to have been missed in this review.
Conclusion
This systematic review synthesised available data on the priority issues and concerns of older PLWH about their medicines, and the type and effectiveness of interventions developed to tackle optimising their medicines. Our findings provide evidence that the ageing HIV population are at high risk for co-morbidity, polypharmacy, drug interactions, adverse drug reactions, medicine burden, treatment burden and stigma. Mental health and social support have been identified as important factors that need attention to improve patient health-related outcomes. Moreover, the fragmentation of care diminishes the relationship between the patient and healthcare providers, creating several barriers and issues for the ageing HIV population. The interventions identified in this review, although sparse, show the potential for medicines optimisation to improve patient health-related outcomes in the ageing HIV population. The use of acceptance-based therapy, SMS reminders and apps for medicines optimisation interventions has high potential; however, the usability and acceptability need to be investigated further in older PLWH. There is a need for further medicines optimisation interventions and the involvement of targeted support groups in the ageing HIV population.
Supplementary Information
Below is the link to the electronic supplementary material.
Declarations
Funding
Open Access funding provided by The University of Kent.
Conflict of interest
Authors PS, RC, SC and BK declare that they have no conflicts of interest.
Ethics approval
This study did not require institutional ethics approval due to using secondary data (i.e., no direct involvement of human participants or their data).
Informed consent
Not applicable.
Data availability
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Author contributions
All authors contributed to study conception and design. PS conducted the literature search and data abstraction. RC, SC and BK contributed to all stages of the systematic review, including independent screening of titles, abstracts and/full articles. PS drafted preliminary versions of the manuscript. BK critically revised the manuscript and offered overall supervision of the project. All authors reviewed and agreed the final version of this paper.
References
- 1.Global HIV and AIDS statistics—2020 fact sheet [Internet]. [cited 2020 Aug 4]. Available from: https://www.unaids.org/en/resources/fact-sheet.
- 2.Deeks SG, Lewin SR, Havlir DV. The end of AIDS: HIV infection as a chronic disease. Lancet. 2013;382:1525–1533. doi: 10.1016/S0140-6736(13)61809-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Trickey A, May MT, Vehreschild J-J, Obel N, Gill MJ, Crane HM, et al. Survival of HIV-positive patients starting antiretroviral therapy between 1996 and 2013: a collaborative analysis of cohort studies. Lancet HIV. 2017;4:e349–e356. doi: 10.1016/S2352-3018(17)30066-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Date HL. Optimising the health and wellbeing of older people living with HIV in the United Kingdom. Clin Pharm. 2018;10:56–64. [Google Scholar]
- 5.Public Health England (PHE). Trends in new HIV diagnoses and in people receiving HIV-related care in the United Kingdom: data to the end of December 2018. 2019;13:8.
- 6.Smit M, Brinkman K, Geerlings S, Smit C, Thyagarajan K, van Sighem A, et al. Future challenges for clinical care of an ageing population infected with HIV: a modelling study. Lancet Infect Dis. 2015;15:810–818. doi: 10.1016/S1473-3099(15)00056-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Angus B, Brook G, Awosusi E, et al. BHIVA guidelines for the routine investigation and monitoring of adult HIV-1 positive individuals (2019 interim update). BHIVA. 2019. Available from: https://www.bhiva.org/monitoring-guidelines.
- 8.American Academy of HIV Medicine. The HIV and aging consensus project: recommended treatment strategies for clinicians managing older patients with HIV. [Internet]. Available from: https://aahivm.org/wp-content/uploads/2017/02/Aging-report-working-document-FINAL-12.1.pdf.
- 9.Gleason LJ, Luque AE, Shah K. Polypharmacy in the HIV-infected older adult population. Clin Interv Aging. 2013;8:749–763. doi: 10.2147/CIA.S37738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Okoli C. Relationship between polypharmacy and quality of life among people in 24 countries living with HIV. Prev Chronic Dis [Internet]. 2020 [cited 2021 Jul 4];17. Available from: https://www.cdc.gov/pcd/issues/2020/19_0359.htm. [DOI] [PMC free article] [PubMed]
- 11.Edelman EJ, Gordon KS, Glover J, McNicholl IR, Fiellin DA, Justice AC. The next therapeutic challenge in HIV: polypharmacy. Drugs Aging. 2013;30:613–628. doi: 10.1007/s40266-013-0093-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Back D, Marzolini C. The challenge of HIV treatment in an era of polypharmacy. J Int AIDS Soc. 2020;23:1–12. doi: 10.1002/jia2.25449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Greene M, Steinman MA, McNicholl IR, Valcour V. Polypharmacy, drug–drug interactions, and potentially inappropriate medications in older adults with human immunodeficiency virus infection. J Am Geriatr Soc. 2014;62:447–453. doi: 10.1111/jgs.12695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Halloran MO, Boyle C, Kehoe B, Bagkeris E, Mallon P, Post FA, et al. Polypharmacy and drug–drug interactions in older and younger people living with HIV: the POPPY study. Antivir Ther. 2019;24:193–201. doi: 10.3851/IMP3293. [DOI] [PubMed] [Google Scholar]
- 15.Justice AC, Gordon KS, Skanderson M, Edelman EJ, Akgün KM, Gibert CL, et al. Nonantiretroviral polypharmacy and adverse health outcomes among HIV-infected and uninfected individuals. AIDS Lond Engl. 2018;32:739–749. doi: 10.1097/QAD.0000000000001756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Introduction | Medicines optimisation | Quality standards | NICE [Internet]. NICE; [cited 2020 Aug 31]. Available from: https://www.nice.org.uk/guidance/qs120/chapter/Introduction.
- 17.Mohammed MA, Moles RJ, Chen TF. Medication-related burden and patients’ lived experience with medicine: a systematic review and metasynthesis of qualitative studies. BMJ Open. 2016;6:e010035. doi: 10.1136/bmjopen-2015-010035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Royal Pharmaceutical Society. Medicines optimisation: helping patients to make the most of medicines [Internet]. 2013 [cited 2021 Aug 3]. Available from: https://www.rpharms.com/Portals/0/RPS%20document%20library/Open%20access/Policy/helping-patients-make-the-most-of-their-medicines.pdf.
- 19.Marzolini C, Livio F. Prescribing issues in elderly individuals living with HIV. Expert Rev Clin Pharmacol. 2019;12:643–659. doi: 10.1080/17512433.2019.1627200. [DOI] [PubMed] [Google Scholar]
- 20.López-Centeno B, Badenes-Olmedo C, Mataix-Sanjuan A, Bellón J, Pérez-Latorre L, López J, et al. Potentially inappropriate medications in older adults living with HIV. HIV Med. 2020;21:541–546. doi: 10.1111/hiv.12883. [DOI] [PubMed] [Google Scholar]
- 21.Saeed D, Carter G, Parsons C. A systematic review of interventions to improve medicines optimisation in frail older patients in secondary and acute care settings. Int J Pharm Pract. 2021;29:i22–i23. doi: 10.1093/ijpp/riab015.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Emlet CA. ‘You’re awfully old to have this disease’: experiences of stigma and ageism in adults 50 years and older living with HIV/AIDS. Gerontologist. 2006;46:781–790. doi: 10.1093/geront/46.6.781. [DOI] [PubMed] [Google Scholar]
- 23.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ [Internet]. British Medical Journal Publishing Group; 2009 [cited 2020 Jul 21];339. Available from: https://www.bmj.com/content/339/bmj.b2535. [PMC free article] [PubMed]
- 24.da Costa Santos CM, de Mattos Pimenta CA, Nobre MRC. The PICO strategy for the research question construction and evidence search. Rev Lat Am Enfermagem. 2007;15:508–511. doi: 10.1590/S0104-11692007000300023. [DOI] [PubMed] [Google Scholar]
- 25.Mahtani KR, Heneghan C, Aronson J. Single screening or double screening for study selection in systematic reviews? BMJ Evid-Based Med. 2020;25:149–150. doi: 10.1136/bmjebm-2019-111269. [DOI] [PubMed] [Google Scholar]
- 26.Engelhard EAN, Smit C, van Dijk PR, Kuijper TM, Wermeling PR, Weel AE, et al. Health-related quality of life of people with HIV: an assessment of patient related factors and comparison with other chronic diseases. AIDS Lond Engl. 2018;32:103–112. doi: 10.1097/QAD.0000000000001672. [DOI] [PubMed] [Google Scholar]
- 27.Greene ML, Tan JY, Weiser SD, Christopoulos K, Shiels M, O’Hollaren A, et al. Patient and provider perceptions of a comprehensive care program for HIV-positive adults over 50 years of age: the formation of the Golden Compass HIV and aging care program in San Francisco. PLoS ONE. 2018;13:e0208486. doi: 10.1371/journal.pone.0208486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guaraldi G, Malagoli A, Theou O, Brothers TD, Wallace L, Torelli R, et al. Correlates of frailty phenotype and frailty index and their associations with clinical outcomes. HIV Med. 2017;18:764–771. doi: 10.1111/hiv.12527. [DOI] [PubMed] [Google Scholar]
- 29.Hastain NV, Santana A, Schafer JJ. The incidence and severity of drug interactions before and after antiretroviral therapy simplification in treatment-experienced patients with HIV infection. Ann Pharmacother. 2020;54:36–42. doi: 10.1177/1060028019867970. [DOI] [PubMed] [Google Scholar]
- 30.Hoang T, Goetz MB, Yano EM, Rossman B, Anaya HD, Knapp H, et al. The impact of integrated HIV care on patient health outcomes. Med Care. 2009;47:560–567. doi: 10.1097/MLR.0b013e31819432a0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Heron JE, Norman SM, Yoo J, Lembke K, O’Connor CC, Weston CE, et al. The prevalence and risk of non-infectious comorbidities in HIV-infected and non-HIV infected men attending general practice in Australia. PLoS ONE. 2019;14:e0223224. doi: 10.1371/journal.pone.0223224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.John MD, Greene M, Hessol NA, Zepf R, Parrott AH, Foreman C, et al. Geriatric assessments and association with VACS Index among HIV-infected older adults in San Francisco. J Acquir Immune Defic Syndr. 2016;72:534–541. doi: 10.1097/QAI.0000000000001009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim TW, Walley AY, Heeren TC, Patts GJ, Ventura AS, Lerner GB, et al. Polypharmacy and risk of non-fatal overdose for patients with HIV infection and substance dependence. J Subst Abuse Treat. 2017;81:1–10. doi: 10.1016/j.jsat.2017.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kiplagat J, Mwangi A, Chasela C, Huschke S. Challenges with seeking HIV care services: perspectives of older adults infected with HIV in western Kenya. BMC Public Health. 2019;19:929. doi: 10.1186/s12889-019-7283-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Knight L, Schatz E, Mukumbang FC. ‘I attend at Vanguard and I attend here as well’: barriers to accessing healthcare services among older South Africans with HIV and non-communicable diseases. Int J Equity Health. 2018;17:147. doi: 10.1186/s12939-018-0863-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Levy ME, Greenberg AE, Hart R, Powers Happ L, Hadigan C, Castel A. High burden of metabolic comorbidities in a citywide cohort of HIV outpatients: evolving health care needs of people aging with HIV in Washington, DC. HIV Med. 2017;18:724–735. doi: 10.1111/hiv.12516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mao L, Buchanan A, Wong HTH, Persson A. Beyond mere pill taking: SMS reminders for HIV treatment adherence delivered to mobile phones of clients in a community support network in Australia. Health Soc Care Community. 2018;26:486–494. doi: 10.1111/hsc.12544. [DOI] [PubMed] [Google Scholar]
- 38.McNicholl IR, Gandhi M, Hare CB, Greene M, Pierluissi E. A Pharmacist-led program to evaluate and reduce polypharmacy and potentially inappropriate prescribing in older HIV-positive patients. Pharmacotherapy. 2017;37:1498–1506. doi: 10.1002/phar.2043. [DOI] [PubMed] [Google Scholar]
- 39.Morillo-Verdugo R, Robustillo-Cortés MA, Abdel-Kader Martín L, ÁlvarezdeSotomayor Paz M, LozanodeLeón Naranjo F, Almeida González CV. Determination of a cutoff value for medication regimen complexity index to predict polypharmacy in HIV+ older patient. Rev Espanola Quimioter Publicacion Of Soc Espanola Quimioter. 2019;32:458–464. [PMC free article] [PubMed] [Google Scholar]
- 40.Patel R, Moore T, Cooper V, McArdle C, Perry N, Cheek E, et al. An observational study of comorbidity and healthcare utilisation among HIV-positive patients aged 50 years and over. Int J STD AIDS. 2016;27:628–637. doi: 10.1177/0956462415589524. [DOI] [PubMed] [Google Scholar]
- 41.Rosenfeld D, Anderson J. ‘The own’ and ‘the wise’ as social support for older people living with HIV in the United Kingdom. Ageing Soc. 2020;40:188–204. doi: 10.1017/S0144686X18000909. [DOI] [Google Scholar]
- 42.Schreiner N, Perazzo J, Currie J, Daly B, Webel A. A descriptive, cross-sectional study examining treatment burden in people living with HIV. Appl Nurs Res. 2019;46:31–36. doi: 10.1016/j.apnr.2019.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shippy RA, Karpiak SE. The aging HIV/AIDS population: fragile social networks. Aging Ment Health. 2005;9:246–254. doi: 10.1080/13607860412331336850. [DOI] [PubMed] [Google Scholar]
- 44.Siefried KJ, Mao L, Cysique LA, Rule J, Giles ML, Smith DE, et al. Concomitant medication polypharmacy, interactions and imperfect adherence are common in Australian adults on suppressive antiretroviral therapy. AIDS Lond Engl. 2018;32:35–48. doi: 10.1097/QAD.0000000000001685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Singo VJ, Lebese RT, Maluleke TX, Nemathaga LH. The views of the elderly on the impact that HIV and AIDS has on their lives in the Thulamela Municipality, Vhembe District, Limpopo province. Curationis [Internet]. South Africa: AOSIS Publishing; 2015;38. Available from: http://search.ebscohost.com/login.aspx?direct=true&db=cmedm&AN=26244455&site=ehost-live. [DOI] [PMC free article] [PubMed]
- 46.Uphold CR, Maruenda J, Yarandi HN, Sleasman JW, Bender BS. HIV and older adults: clinical outcomes in the era of HAART. J Gerontol Nurs. 2004;30:16–24. doi: 10.3928/0098-9134-20040701-06. [DOI] [PubMed] [Google Scholar]
- 47.Farahat FM, Alghamdi YS, Farahat AF, Alqurashi AA, Alburayk AK, Alabbasi AA, et al. The prevalence of comorbidities among adult people diagnosed with HIV infection in a tertiary care hospital in western Saudi Arabia. J Infect Public Health. 2020;13:1699–1704. doi: 10.1016/j.jiph.2020.08.009. [DOI] [PubMed] [Google Scholar]
- 48.Schatz E, Knight L, Mukumbang FC, Teti M, Myroniuk TW. ‘You Have to Withstand That Because You Have Come for What You Have Come for’: barriers and facilitators to antiretroviral treatment access among older South Africans living with HIV. Sociol Health Illn. 2021;43:624–641. doi: 10.1111/1467-9566.13243. [DOI] [PubMed] [Google Scholar]
- 49.Vinuesa-Hernando JM, Gimeno-Gracia M, Malo S, Sanjoaquin-Conde I, Crusells-Canales MJ, Letona-Carbajo S, et al. Potentially inappropriate prescriptions and therapeutic complexity in older HIV patients with comorbidities. Int J Clin Pharm. 2021;43:1245–1250. doi: 10.1007/s11096-021-01242-1. [DOI] [PubMed] [Google Scholar]
- 50.Drewes J, Ebert J, Langer PC, Kleiber D, Gusy B. Comorbidities and psychosocial factors as correlates of self-reported falls in a nationwide sample of community-dwelling people aging with HIV in Germany. BMC Public Health. 2021;21:1–9. doi: 10.1186/s12889-021-11582-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fischetti B, Sorbera M, Michael R, Njeim N. Evaluation of rates of virologic suppression in HIV-positive patients with varying numbers of comorbidities. Am J Health Syst Pharm. 2022;79:72–77. doi: 10.1093/ajhp/zxab346. [DOI] [PubMed] [Google Scholar]
- 52.Shamu T, Chimbetete C, Egger M, Mudzviti T. Treatment outcomes in HIV infected patients older than 50 years attending an HIV clinic in Harare, Zimbabwe: a cohort study. PLoS ONE. 2021;16:e0253000. doi: 10.1371/journal.pone.0253000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ventuneac A, Kaplan-Lewis E, Buck J, Roy R, Aberg CE, Duah BA, et al. A mobile health intervention in HIV primary care: supporting patients at risk for ART non-adherence. HIV Res Clin Pract. 2020;21:140–150. doi: 10.1080/25787489.2020.1862972. [DOI] [PubMed] [Google Scholar]
- 54.Zepf R, Greene M, Hessol NA, Johnson MO, Santos GM, John MD, et al. Syndemic conditions and medication adherence in older men living with HIV who have sex with men. AIDS Care. 2020;32:1610–1616. doi: 10.1080/09540121.2020.1772954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chayama KL, Ng C, Small W, Ivsins A, McNeil R. ‘It’s a burden, it’s a nuisance I wish I didn’t have these other ailments’: a qualitative exploration of comorbidities management among older people living with HIV who use drugs in Vancouver, British Columbia. J Int AIDS Soc. 2021;24:e25785. doi: 10.1002/jia2.25785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Haruna T, Somba M, Siril H, Mahiti G, August F, Minja A, et al. Factors hindering integration of care for non-communicable diseases within HIV care services in Dar es Salaam, Tanzania: the perspectives of health workers and people living with HIV. PLoS ONE. 2021;16:e0254436. doi: 10.1371/journal.pone.0254436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bosire EN. Patients’ experiences of comorbid HIV/AIDS and diabetes care and management in Soweto, South Africa. Qual Health Res. 2021;31:373–384. doi: 10.1177/1049732320967917. [DOI] [PubMed] [Google Scholar]
- 58.McKetchnie SM, Beaugard C, Taylor SW, O’Cleirigh C. Perspectives on pain, engagement in HIV care, and behavioral interventions for chronic pain among older sexual minority men living with HIV and chronic pain: a qualitative analysis. Pain Med. 2021;22:577–584. doi: 10.1093/pm/pnaa351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Jacomet C, Langlois J, Secher S, Coban D, Lambert C, Zucman D, et al. Pharmacist’s role in HIV care in France. Implication for clinical improvement of people living with HIV worldwide. Pharmacol Res Perspect. 2020;8:e00629. doi: 10.1002/prp2.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hartzler B, Dombrowski JC, Donovan DM. Contextual compatibility of three empirically supported behavior therapies for cART adherence among patients with substance use disorders. AIDS Care. 2019;31:19–24. doi: 10.1080/09540121.2018.1545985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zheng C, Meng J, Xiao X, Xie Y, Zhao D, Wang H. Polypharmacy, medication-related burden and antiretroviral therapy adherence in people living with HIV aged 50 and above: a cross-sectional study in Hunan, China. Patient Prefer Adherence. 2022;16:41–49. doi: 10.2147/PPA.S340621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nguyen AL, McNeil CJ, Han SD, Rhodes SD. Risk and protective factors for health-related quality of life among persons aging with HIV. AIDS Care. 2018;30:518–522. doi: 10.1080/09540121.2017.1381333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Townsend ML, Jackson GL, Smith R, Wilson KH. Association between pharmacy medication refill-based adherence rates and cd4 count and viral-load responses: a retrospective analysis in treatment-experienced adults with HIV. Clin Ther. 2007;29:711–716. doi: 10.1016/j.clinthera.2007.04.006. [DOI] [PubMed] [Google Scholar]
- 64.Harris LM, Crawford TN, Kerr JC, Thomas TA, Schmidt V. African American older adults living with HIV: exploring stress, stigma, and engagement in HIV care. J Health Care Poor Underserved. 2020;31:265–286. doi: 10.1353/hpu.2020.0022. [DOI] [PubMed] [Google Scholar]
- 65.Ahmed A, Saqlain M, Bashir N, Dujaili J, Hashmi F, Mazhar F, et al. Health-related quality of life and its predictors among adults living with HIV/AIDS and receiving antiretroviral therapy in Pakistan. Qual Life Res Int J Qual Life Asp Treat Care Rehabil. 2021;30:1653–1664. doi: 10.1007/s11136-021-02771-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Halkitis PN, Perez-Figueroa RE, Carreiro T, Kingdon MJ, Kupprat SA, Eddy J. Psychosocial burdens negatively impact HIV antiretroviral adherence in gay, bisexual, and other men who have sex with men aged 50 and older. AIDS Care. 2014;26:1426–1434. doi: 10.1080/09540121.2014.921276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.McMillan JM, Krentz HB, Gill MJ, Hogan DB. An emerging concern—high rates of frailty among middle-aged and older individuals living with HIV. Can Geriatr J. 2019;22:190–198. doi: 10.5770/cgj.22.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Greene M, Hessol NA, Perissinotto C, Zepf R, Hutton Parrott A, Foreman C, et al. Loneliness in older adults living with HIV. AIDS Behav. 2018;22:1475–1484. doi: 10.1007/s10461-017-1985-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kteily-Hawa R, Andany N, Wang Y, Logie CH, Tharao W, Conway T, et al. Quality of life of older women living with HIV: comparative assessment of physical and mental health-related markers using a large Canadian Sexual and Reproductive Health Cohort Study. HIV Res Clin Pract. 2019;20:35–47. doi: 10.1080/15284336.2018.1554373. [DOI] [PubMed] [Google Scholar]
- 70.Contreras-Macías E, Gutiérrez-Pizarraya A, RobustilloCortés MA, Morillo-Verdugo R. High level of medication regimen complexity index correlate with worse quality of life in people living with HIV. Rev Espanola Quimioter Publicacion Of Soc Espanola Quimioter. 2021;34:93–99. doi: 10.37201/req/097.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Owen G, Catalan J. ‘We never expected this to happen’: narratives of ageing with HIV among gay men living in London, UK. Cult Health Sex. 2012;14:59–72. doi: 10.1080/13691058.2011.621449. [DOI] [PubMed] [Google Scholar]
- 72.Gimeno-Gracia M, Crusells-Canales MJ, Armesto-Gómez FJ, Compaired-Turlán V, Rabanaque-Hernández MJ. Polypharmacy in older adults with human immunodeficiency virus infection compared with the general population. Clin Interv Aging. 2016;11:1149–1157. doi: 10.2147/CIA.S108072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Contreras Macías E, Serrano Giménez R, Morillo Verdugo R. Prevalence of prescription of the Top-10 drug classes to avoid in elderly people living with HIV in a real practice cohort. Rev Espanola Quimioter Publicacion Of Soc Espanola Quimioter. 2021;34:28–32. doi: 10.37201/req/087.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jakeman B, Scherrer A, Battegay M, Gunthard HF, Hachfeld A, Calmy A, et al. Anticholinergic medication use in elderly people living with HIV and self-reported neurocognitive impairment: a prospective cohort study. J Antimicrob Chemother. 2022;77:492–499. doi: 10.1093/jac/dkab386. [DOI] [PubMed] [Google Scholar]
- 75.Katende-Kyenda NL, Lubbe MS, Serfontein JHP, Truter I. Prevalence of possible drug–drug interactions between antiretroviral agents in different age groups in a section of the private health care sector setting in South Africa. J Clin Pharm Ther. 2008;33:393–400. doi: 10.1111/j.1365-2710.2008.00930.x. [DOI] [PubMed] [Google Scholar]
- 76.Gimeno-Gracia M, Crusells-Canales MJ, Rabanaque-Hernández MJ. Clinical characteristics and antiretroviral treatment of older HIV-infected patients. Int J Clin Pharm. 2014;36:1190–1195. doi: 10.1007/s11096-014-0015-x. [DOI] [PubMed] [Google Scholar]
- 77.Jiménez-Guerrero L, Núñez-Núñez M, Castañeda-Macías I, Sandoval-Fernández Del Castillo S. Potential interactions in a cohort of elderly hiv-positive patients. Farm Hosp Organo Of Expresion Cient Soc Espanola Farm Hosp. 2018;42:163–167. doi: 10.7399/fh.10921. [DOI] [PubMed] [Google Scholar]
- 78.Heckman TG, Heckman BD, Kochman A, Sikkema KJ, Suhr J, Goodkin K. Psychological symptoms among persons 50 years of age and older living with HIV disease. Aging Ment Health. 2002;6:121–128. doi: 10.1080/13607860220126709a. [DOI] [PubMed] [Google Scholar]
- 79.Frazier EL, Sutton MY, Tie Y, Collison M, Do A. Clinical characteristics and outcomes among older women with HIV. J Womens Health. 2018;27:6–13. doi: 10.1089/jwh.2017.6380. [DOI] [PubMed] [Google Scholar]
- 80.Gardenier D, Andrews CM, Thomas DC, Bookhardt-Murray LJ, Fitzpatrick JJ. Social support and adherence: differences among clients in an AIDS day health care program. JANAC J Assoc Nurses AIDS Care. 2010;21:75–85. doi: 10.1016/j.jana.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 81.Keith McInnes D, Shimada SL, Rao SR, Quill A, Duggal M, Gifford AL, et al. Personal health record use and its association with antiretroviral adherence: survey and medical record data from 1871 US veterans infected with HIV. AIDS Behav. 2013;17:3091–3100. doi: 10.1007/s10461-012-0399-3. [DOI] [PubMed] [Google Scholar]
- 82.Lee CJ. Executive functioning, cigarette smoking, and medication adherence in people living with HIV/AIDS [Internet]. ProQuest Information & Learning; 2019. Available from: http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2018-52510-087&site=ehost-live.
- 83.Sutton SS, Hardin JW, Bramley TJ, D’Souza AO, Bennett CL. Single- versus multiple-tablet HIV regimens: adherence and hospitalization risks. Am J Manag Care. 2016;22:242–248. [PubMed] [Google Scholar]
- 84.Schatz E, David I, Angotti N, Gómez-Olivé FX, Mojola SA. From ‘Secret’ to ‘Sensitive Issue’: shifting ideas about HIV disclosure among middle-aged and older rural South Africans in the era of antiretroviral treatment. J Aging Health. 2022;34:14–24. doi: 10.1177/08982643211020202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Siefried KJ, Mao L, Kerr S, Cysique LA, Gates TM, McAllister J, et al. Socioeconomic factors explain suboptimal adherence to antiretroviral therapy among HIV-infected Australian adults with viral suppression. PLoS ONE. 2017;12:e0174613. doi: 10.1371/journal.pone.0174613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kuteesa MO, Seeley J, Cumming RG, Negin J. Older people living with HIV in Uganda: understanding their experience and needs. Afr J AIDS Res. 2012;11:295–305. doi: 10.2989/16085906.2012.754829. [DOI] [PubMed] [Google Scholar]
- 87.Moitra E, Herbert JD, Forman EM. Acceptance-based behavior therapy to promote HIV medication adherence. AIDS Care. 2011;23:1660–1667. doi: 10.1080/09540121.2011.579945. [DOI] [PubMed] [Google Scholar]
- 88.McAllister J, Beardsworth G, Lavie E, MacRae K, Carr A. Financial stress is associated with reduced treatment adherence in HIV-infected adults in a resource-rich setting. HIV Med. 2013;14:120–124. doi: 10.1111/j.1468-1293.2012.01034.x. [DOI] [PubMed] [Google Scholar]
- 89.Tran V-T, Harrington M, Montori VM, Barnes C, Wicks P, Ravaud P. Adaptation and validation of the Treatment Burden Questionnaire (TBQ) in English using an internet platform. BMC Med. 2014;12:109. doi: 10.1186/1741-7015-12-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Serrano Giménez R, Gallardo Anciano J, Robustillo Cortés MA, Blanco Ramos JR, Gutiérrez Pizarraya A, Morillo Verdugo R. Beliefs and attitudes about deprescription in older HIV-infected patients: ICARD Project. Rev Espanola Quimioter Publicacion Of Soc Espanola Quimioter. 2021;34:18–27. doi: 10.37201/req/084.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Philbin MM, Parish C, Bergen S, Kerrigan D, Kinnard EN, Reed SE, et al. A qualitative exploration of women’s interest in long-acting injectable antiretroviral therapy across six cities in the Women’s Interagency HIV study: intersections with current and past injectable medication and substance use. AIDS Patient Care STDs. 2021;35:23–30. doi: 10.1089/apc.2020.0164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Furlotte C, Schwartz K. Mental health experiences of older adults living with HIV: uncertainty, stigma, and approaches to resilience. Can J Aging Rev Can Vieil. 2017;36:125–140. doi: 10.1017/S0714980817000022. [DOI] [PubMed] [Google Scholar]
- 93.Foster PP, Gaskins SW. Older African Americans’ management of HIV/AIDS stigma. AIDS Care. 2009;21:1306–1312. doi: 10.1080/09540120902803141. [DOI] [PubMed] [Google Scholar]
- 94.Bogart LM, Barreras JL, Gonzalez A, Klein DJ, Marsh T, Agniel D, et al. Pilot randomized controlled trial of an intervention to improve coping with intersectional stigma and medication adherence among HIV-positive Latinx sexual minority men. AIDS Behav. 2021;25:1647–1660. doi: 10.1007/s10461-020-03081-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hojilla JC, Santiago-Rodriguez EI, Sterling S, Williams EC, Leyden W, Hare CB, et al. HIV stigma and its associations with longitudinal health outcomes among persons living with HIV with a history of unhealthy alcohol use. AIDS Behav. 2021;25:215–224. doi: 10.1007/s10461-020-02963-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Fritsch T. HIV/AIDS and the older adult: an exploratory study of the age-related differences in access to medical and social services. J Appl Gerontol. 2005;24:35–54. doi: 10.1177/0733464804271452. [DOI] [Google Scholar]
- 97.Rozanova J, Shenoi S, Zaviryukha I, Zeziulin O, Kiriazova T, Rich K, et al. Social support is key to retention in care during Covid-19 pandemic among older people with HIV and substance use disorders in Ukraine. Subst Use Misuse. 2020;55:1902–1904. doi: 10.1080/10826084.2020.1791183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.DeFulio A, Devoto A, Traxler H, Cosottile D, Fingerhood M, Nuzzo P, et al. Smartphone-based incentives for promoting adherence to antiretroviral therapy: a randomized controlled trial. Prev Med Rep. 2021;21:101318. doi: 10.1016/j.pmedr.2021.101318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Schnall R, Cho H, Mangone A, Pichon A, Jia H. Mobile health technology for improving symptom management in low income persons living with HIV. AIDS Behav. 2018;22:3373–3383. doi: 10.1007/s10461-017-2014-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Cho H, Porras T, Baik D, Beauchemin M, Schnall R. Understanding the predisposing, enabling, and reinforcing factors influencing the use of a mobile-based HIV management app: a real-world usability evaluation. Int J Med Inf. 2018;117:88–95. doi: 10.1016/j.ijmedinf.2018.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Leake Date HA, Alford K, Hounsome N, Moore D, Ing K, Vera JH. Structured medicines reviews in HIV outpatients: a feasibility study (the MOR study) HIV Med. 2022;23:39–47. doi: 10.1111/hiv.13158. [DOI] [PubMed] [Google Scholar]
- 102.Njie-Carr VPS, Zhu S, Williams GC, Corless IB, Himelhoch S. Evaluation of a technology-enhanced intervention for older women with HIV infection: a proof of concept study. AIDS Care. 2021;33:983–992. doi: 10.1080/09540121.2020.1810617. [DOI] [PubMed] [Google Scholar]
- 103.Freeman R, Gwadz M, Wilton L, Collins LM, Dorsen C, Hawkins RL, et al. Understanding long-term HIV survivorship among African American/Black and Latinx persons living with HIV in the United States: a qualitative exploration through the lens of symbolic violence. Int J Equity Health. 2020;19:146. doi: 10.1186/s12939-020-01253-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Psaros C, Barinas J, Robbins GK, Bedoya CA, Park ER, Safren SA. Reflections on living with HIV over time: exploring the perspective of HIV-infected women over 50. Aging Ment Health. 2015;19:121–128. doi: 10.1080/13607863.2014.917608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Willig AL, Overton ET, Saag MS. The silent epidemic—frailty and aging with HIV. Total Patient Care HIV HCV. 2016;1:6–17. [PMC free article] [PubMed] [Google Scholar]
- 106.Duerden M, Avery T, Payne R. Polypharmacy and medicines optimisation: making it safe and sound. London: The King’s Fund; 2013. [Google Scholar]
- 107.Terrence Higgins Trust. Uncharted Territory: a report into the first generation growing older with HIV. 2017.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.