Abstract
Spending more time outdoors can improve children’s social and cognitive development, physical activity, and vision. Our systematic review summarized the determinants of outdoor time (OT) based on the social-ecological model. We searched nine databases: MEDLINE, APA PsycINFO, Web of Science, Cochrane Central Register of Controlled Trials (CENTRAL), CINAHL, SPORTDiscus, ERIC, SocINDEX, and ProQuest Dissertations and Theses. To be included, studies needed to be quantitative and longitudinal, include ≥1 potential determinant of OT among 0- to 17-year-olds, and be published in English, French, Japanese, or Spanish. We extracted the authors, publication year, country, design, sample size, OT measures, follow-up period, potential determinants, main results, and potential moderators or mediators. Fifty-five studies examining 119 potential determinants met the inclusion criteria. OT was consistently higher in warmer seasons and among participants reporting more OT at baseline. All three interventions that included both parent sessions and additional resources to promote OT (e.g., specific advice and community guides) were effective. COVID-19 restrictions and sun safety interventions discouraging midday outdoor activities led to less OT. The quality of evidence was rated as weak for 46 studies. Most potential determinants were examined in ≤3 studies; thus, more longitudinal studies are needed to enable stronger conclusions about the consistency of evidence and meta-analyses.
Keywords: outdoor play, social-ecological model, adolescents, physical activity, nature
1. Introduction
Evidence from large systematic reviews indicates that children and youth who are more physically active reap multiple benefits, including better motor and cognitive development, greater cardiovascular fitness, reduced cardiometabolic risk, and improved bone health [1,2]. However, the majority of children and youth worldwide do not meet current physical activity (PA) guidelines [3,4]. For example, Guthold et al. [4] estimated that, among 1.6 million 11- to 17-year-olds from 146 countries, 77.6% of boys and 84.7% of girls were insufficiently active. This underscores a need for interventions targeting important determinants of PA. Systematic reviews have consistently identified positive associations between time spent outdoors and children’s PA [5,6,7,8]. Yet, previous research suggests that outdoor play (OP) has declined substantially over the last few decades, likely at the expense of increasing screen time [9,10], emphasizing a need to promote outdoor activities.
Given that COVID-19 restrictions were associated with a decline in PA and limited access to opportunities such as physical education and sports, promoting outdoor activities may be even more salient in pandemic and post-pandemic contexts [11]. Unfortunately, cross-sectional studies included in the scoping review by Paterson et al. [11] reported that children spent limited time outdoors during the pandemic.
Beyond PA, a growing body of evidence shows that spending more time outdoors is beneficial for social-emotional and cognitive development, psychosocial health, and vision [12,13,14]. Exposure to nature has been shown to prevent myopia [12], improve the management of attention-deficit/hyperactivity disorder [15,16], and foster pro-environmental behaviours among children [17]. Based on some of the abovementioned benefits, the Position Statement on Active Outdoor Play recommends that “Access to active play in nature and outdoors—with its risks— is essential for healthy child development. We recommend increasing children’s opportunities for self-directed play outdoors in all settings—at home, at school, in child care, the community and nature” [14]. It is worth noting that the phrases outdoor time (OT) and OP have been used interchangeably in the literature, even though the former concept is broader [18]. Specifically, the Play, Learn, and Teach Outdoors Network defined play as “Voluntary engagement in activity that is fun and/or rewarding and usually driven by intrinsic motivation” and OP as a form of play that occurs outdoors [18]. Conversely, OT refers to the amount of time spent outdoors [18], regardless of what people are doing while outdoors.
Although previous systematic reviews have examined the correlates of OT and/or OP [19,20,21], most included studies were cross-sectional, precluding conclusions about the direction of observed associations. One of these reviews focused only on parental correlates [19], and another focused only on the built environment [20]. In addition, two of these reviews excluded adolescents [19,21]. A systematic review that focuses specifically on longitudinal studies that can establish a temporal sequence would help identify key determinants that could be targeted in future interventions. Such information would be particularly useful for researchers, practitioners, and policymakers to develop evidence-informed interventions to increase OT.
To address these research gaps, we conducted a systematic review of longitudinal studies on the determinants of OT in children and youth (aged 0–17 years). Guided by the social-ecological model [22], we considered potential correlates representing the individual, interpersonal, community, built and natural environment, and policy levels of influence. In an effort to inform future interventions, we also examined the potential moderators and mediators of the determinants of OT.
2. Materials and Methods
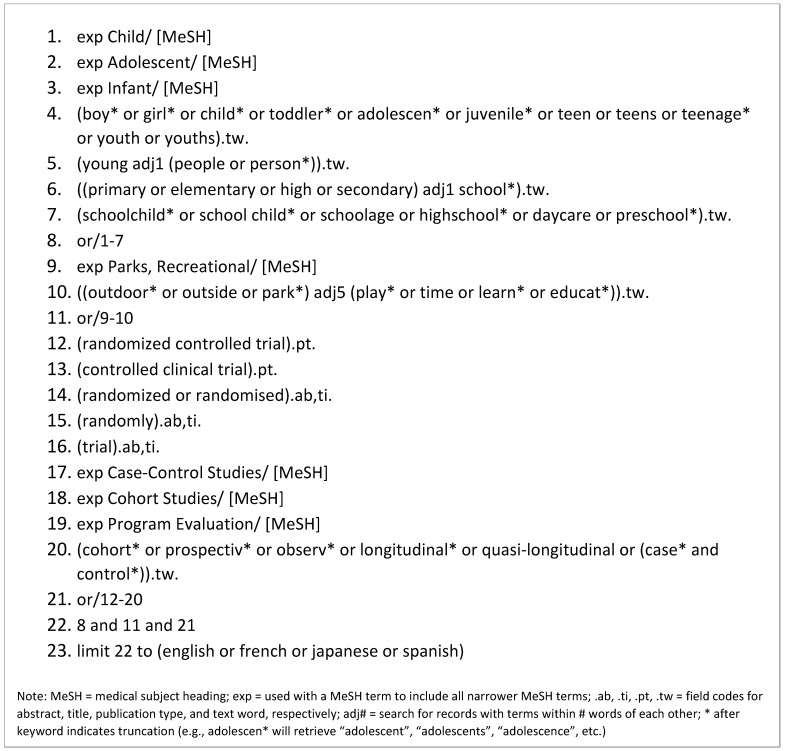
We conducted this systematic review in accordance with the PRISMA 2020 statement [23] (see Supplementary Material File S1 for the PRISMA checklist). A health sciences librarian (DS) searched nine databases (MEDLINE, APA PsycINFO, Web of Science, the Cochrane Central Register of Controlled Trials (CENTRAL), CINAHL, SPORTDiscus, ERIC, SocINDEX, and ProQuest Dissertations and Theses) on 9 and 10 March 2021. The search was updated on 6 July 2022. Search terms were identified through consultations between the lead author (RL) and the librarian, a scan of the titles and subject headings of preliminary search results, and a review of the titles and abstracts of nine seed articles collected by RL. Elements of search strings developed for previously published reviews also informed the search strategy [24,25,26]. To optimize the precision of searches while maintaining high sensitivity, the search string was revised several times in accordance with feedback from RL. The search strategy was first developed for MEDLINE (Figure 1) and adapted for the eight other databases (Supplementary Material File S2). When possible, subject headings from controlled vocabularies (e.g., MeSH) were used in the search. To increase sensitivity, concepts were also entered in the search string as keywords, with truncation (e.g., child*) and proximity operators (e.g., adj5) used when appropriate. Boolean operators connected subject headings and keywords, as shown in Figure 1 and Supplementary Material File S2. No limits were placed on publication date, but language filters were applied to capture articles published in either English, French, Japanese, or Spanish. Searches of reference lists of previous systematic reviews [19,20,21] and included studies were completed by VH, MK, and FS. The review is registered in PROSPERO (ID: CRD42021243959).
Figure 1.
MEDLINE search strategy.
See Supplementary Material File S2 for search strategies implemented in other databases.
2.1. Inclusion and Exclusion Criteria
To be eligible for the review, published studies needed to include (1) participants aged 0–17 years (or parents/guardians reporting on behalf of children); (2) a measure of OT; (3) data on at least one potential determinant in relation to OT; and (4) a longitudinal and quantitative design (i.e., including intervention studies, prospective studies, and retrospective studies). Studies published in English, French, Japanese, or Spanish were eligible. Eligible measures of OT included child- or parent-reported measures, direct observation, devices (e.g., accelerometers equipped with lux sensors), and any other relevant methods. No restrictions were placed on study location(s) or type of determinants examined. Studies that did not include data for children were excluded. Literature reviews, commentaries, editorials, cross-sectional studies, qualitative studies, and articles not in the aforementioned languages were excluded.
2.2. Screening Process
Titles and abstracts of each record identified were screened independently by two reviewers (MK, UCR, CH, VH, HS, LB, or OKO) trained by RL. Next, full-text copies of each record that passed the first stage of screening were obtained and screened independently by two research assistants. In this second stage, reasons for exclusion were collated in an Excel spreadsheet. Disagreements were resolved in discussions with RL.
2.3. Data Extraction
RL developed a data extraction form in Microsoft Excel. Data extracted included lead author, publication year, country, study design, analytical sample size, measures of OT, follow-up period, potential determinants examined, main results, and information about any moderators or mediators examined. For potential determinants, main results, and moderators or mediators, data about all reported longitudinal associations relevant to our review were extracted. For the first eight articles, data extraction was conducted independently by RL and all five reviewers, who then met via Zoom to discuss the extracted data. Subsequently, data extraction was conducted independently by two review team members. Any substantive disagreement was resolved in discussions with RL. When information to be extracted was missing, RL contacted the corresponding author of the original study via email. Any information that remained missing or unclear from the articles is identified as such in the results and tables.
2.4. Study Quality
We assessed study quality with the Effective Public Health Practice Project Tool (EPHPP) [27], a well-established method used in public health reviews that include few randomized controlled trials [28,29,30,31]. The tool addresses eight components: (1) selection bias; (2) study design; (3) confounders; (4) blinding; (5) validity and reliability of measurement tools; (6) withdrawals and drop-outs; (7) intervention integrity; and (8) analyses. Following recommended procedures, we graded the first six components as “strong”, “moderate”, or “weak” [27]. Next, we rated studies as “strong” if there were no “weak” ratings, “moderate” if there was only one “weak” rating, or “weak” if there were two or more “weak” ratings [27]. As in previous PA systematic reviews using the EPHPP, we made some adaptations to the tool [28,29,30,31]. First, for group-level interventions such as cluster randomized controlled trials, wherein all members of a school or preschool were assigned to a control or experimental group, we assessed participation rate at the group level for the first component [28,30]. Second, for the component on confounders, we expected studies to control for sex/gender, age, and socio-economic status, given that these variables were identified as correlates of PA and OT in previous reviews [5,7,19,21]. Third, like Dietz et al. [29], we considered the blinding component non-applicable in observational studies, as there are no interventions that participants/staff can be blinded to. After performing quality assessments independently for all articles, RL and MK met to discuss their assessments and resolve any discrepancies. When insufficient information was provided in the article to assess a component, we consulted previous articles or protocols from the study (when available) and/or contacted the author for correspondence. If no response was obtained, the component was conservatively rated as “weak”.
2.5. Summary of Findings
Due to the methodological heterogeneity of included studies (e.g., large differences in study designs, measures of OT, potential determinants, follow-up period, and analyses; see Table 1), we considered meta-analyses inappropriate. Instead, we present a narrative synthesis, and we tabulated measures of effect size (e.g., regression coefficients and odds ratios) and statistical significance as presented in the articles. To synthesize the consistency of associations investigated in ≥3 studies as an indicator of confidence in the body of evidence for a particular determinant, we adopted a classification system used in previous systematic reviews of correlates of PA and OT [8,21,32,33]. Variables positively or negatively associated with OT in ≥60% of studies were considered “consistent” correlates and coded as + or −. When 34–59% of associations were positive or negative, we coded the variable as (+) or (−), representing a “possible” correlate. Finally, when <34% of studies supported an association, we coded the variable as 0, indicating no relationship [8]. All studies that met inclusion criteria were included in the summary of findings. As per our PROSPERO record, we intended to stratify results by gender and age group; however, because most potential determinants were examined in a few studies, we were only able to investigate gender and age by age group.
Table 1.
Descriptive characteristics of included studies.
| Lead Author (Year) | Location | N | Age/Grade at Baseline (Mean ± SD or Range) | Gender | Setting | Follow-Up Length | Measure of Outdoor Time |
|---|---|---|---|---|---|---|---|
| Studies Beginning in Early Childhood (<5 Years) | |||||||
| Arcury (2017) [34] | United States (North Carolina) | 221 | 2–3 years | 52% girls | Community | 2 years | Parent-reported. 24 h recall: number of minutes child spent (1) at playground and (2) in the yard |
| Cameron (2019) [35] | Australia (Melbourne) | 307 | 3.61 years (range: 3.2–4.5) | Not stated | Cohort | 2 years | Parent-reported OT on an average day in last week |
| Davison (2011) [36] | United States (New York State) | 1322 | 2–5 years | 51.0% girls | Women and children clinics | 1 year | Parent-reported OT (dichotomized as ≥60 min/day vs. less) |
| Essery (2008) [37] | United States (Texas) | 90 | 3.1 ± 1.1 years | 53% girls | Home | 3 months | Parent-reported. Time spent in OP per day |
| Händel (2017) [38] | Denmark (Copenhagen) | 307 | 4 years (median) | 42.2% girls | Municipality (birth registry) | 15 months | Parent-reported OP in min/week |
| Hesketh (2015) [39] | Australia (Melbourne) | 542 | 3.9 ± 1.5 months | 47.4% girls | Maternal and Child Health service | 16 months | Parent-reported OT per day |
| Hnatiuk (2013) [40] | Australia (Melbourne) | 206 | 3.5 ± 1 months | 46.6% girls | First-time parent groups | 5 months | Parent-reported OT in min/week |
| Honda-Barros (2019) [41] | Brazil (Recife, Pernambuco) | 700 | 3–5 years | 47.9% girls | Schools | 2 years | Standardized interview (parent-reported OP in min/day) |
| Huang (2021) [42] | China (Longhua) | 26,611 | 1 year | 45.7% girls | Schools | 2 years | Parent-reported frequency and duration of OT |
| Li (2022) [43] | China (Changsha) | 953 | 12 months | 48.4% girls | Clinics/hospitals | 4 years | Parent-reported OT (hours/day) |
| Lumeng (2017) [44] | United States (Michigan) | 697 | 4.1 ± 0.5 years | 51% girls | Head Start programs (preschool) | 7 months | Parent-reported OT on weekdays and weekend days |
| Sääkslahti (2004) [45] | Finland (Turku) | 228 | Intervention: 4.6 ± 0.5 years; control: 4.4 ± 0.4 | 48.2% girls | Clinic | 3.5 years | Parent-reported. Diary reporting time spent in OP (hours/weekend) |
| Shah (2017) [46] | United Kingdom (Avon) | 2833 | 2 years | 50.2% girls | Cohort | 13 years (6.5 years for OT) | Parent-reported OT per day |
| Tandon (2019) [47] | United States (Seattle, Washington) | 82 | Active play group: 4.5 ± 0.6 years; outdoor play group: 4.6 ± 0.4 | 56.1% girls | Preschools | 12 weeks | Direct observation of outdoor activities (child-initiated and teacher-initiated) |
| Thiering (2016) [48] | Germany | 837 | Birth | 49% girls | Birth cohorts | 15 years | Child-reported OT: h/day |
| Xu (2016) [49] | Australia (Sydney) | 369 | 2 years | 50% girls | Birth cohort | 3 years | Mother-reported. Hours of OP per weekday and weekend day |
| Studies beginning in childhood (5–11 years) | |||||||
| Avol (1998) [50] | United States (Southern California) | 195 | 10–12 years | 48.7% girls | Cohort (hospital) | Mid-spring–late summer (~4–5 months) | Child-reported (diary). Location recorded hourly for four days |
| Bacha (2010) [51] | United States (10 sites) | 868 | Grade 3 | 50.8% girls | Birth cohort | 2 years (for main exposure) | Child-reported OT in the neighbourhood on weekdays between school dismissal and 6 pm (dichotomized as any vs. none) |
| Bagordo (2017) [52] | Italy (5 towns) | 1164 | 6–8 years | 49.1% girls | Schools | ~5 months (winter 2014–2015 to late spring 2015) | Parent-reported OP for >1 h per day (yes/no) |
| Buller (2020) [53] | United States (California) | 1758 | 8.16 ± 2.04 years | 49.1% girls | Schools | 20 months a | Parent-reported. OT between 10 am and 4 pm during the week (none, 30 min or less, or 31 min or more) |
| Christiana (2017) [54] | United States (Western North Carolina) | 70 | 5–13 years | 44.3% girls | Pediatric clinics | 3 months | Parent-reported frequency of OT |
| Cleland (2008) [55] | Australia (Melbourne) | 548 | Two cohorts: 5–6 years and 10–12 years | 53% girls | Schools | 3 years | Parent-reported OT on weekdays and weekend days for warmer and cooler months |
| Cleland (2010) [56] | Australia (Melbourne) | 421 | Two cohorts: 5–6 years and 10–12 years | 51.5% girls | Schools | 5 years | Parent-reported OT on weekdays and weekend days for warmer and cooler months |
| Cortinez-O’Ryan (2017) [57] | Chile (Santiago) | 100 | 4–12 years | 51% girls | Neighbourhood | 12 weeks | Parent-reported frequency and duration of OP |
| Flynn (2017) [58] | United States (Southeast region) | 27 | 10.7 ± 3.3 years | 51.9% girls | Neighbourhoods | 4 weeks | Parent-reported. Total minutes of outdoor PA/week |
| Ford (2002) [59] | United States (Atlanta, Georgia) | 28 | 7–12 years | 53.4% girls | Community clinic | 4 weeks | Parents and children reported together: typical amount of OT per day |
| Gerards (2015) [60] | Netherlands (Limburg) | 56 | 7.2 ± 1.4 years | 55.8% girls | Public health services | 12 months | Parent-reported. Days per week and number of hours playing outside |
| Handy (2008) [61] | United States (Northern California) | 272 | <16 years | Not stated | Neighbourhoods | 1 year (retrospective) | Parent-reported. Frequency of OP in previous week |
| He (2015) [12] | China (Guangzhou) | 1848 | 6–7 years | 46% girls | Schools | 3 years | Parent-reported OT in min/day |
| Kemp (2022) [62] | Australia (national) | 2971 | 10.4 ± 0.5 years | 49.2% girls | Home | 2 years | Child-reported time-use diaries with a category for non-organized outdoor/nature PA in min/day |
| Li (2021) [63] | Canada (Toronto) | 265 | 5.5 ± 2.5 years | 47.5% girls | Clinics/hospitals | 3 months | Parent-reported OT (hours and min/day) |
| Milne (2000) [64] | Australia (Perth) | 1386 | 5–6 years | 48% girls | Schools | 17 months | Parent-reported. Average time each day that the children were outdoors between 8 am and 4 pm and between 11 am and 2 pm |
| Milne (2007) [65] | Australia (Perth) | 1116 | 5–6 years | 49.8% girls | Schools | 4 years | Parent-reported. Average time each day that the children were outdoors between 8 and 11 AM, between 11 AM and 2 PM, and between 2 and 5 PM |
| Nigg (2021) [66] | Germany | 570 | 5.3 ± 0.8 years | 54.7% girls | Community | 11 years | Participant-reported OP frequency in a typical week (from 0 to 7 days) |
| Ngo (2009) [67] | Singapore | 285 | 6–12 years | 45.9% girls | Program/community | 9 months | Parent-reported OT on weekdays and weekend days (questionnaire and diary) |
| Nordvall-Lassen (2018) [68] | Denmark (Aarhus) | 4941 | 9–11 years | 49.6% girls | Birth cohort | 9–11 years | Parent-reported OT (h/week) |
| Ostrin (2018) [69] | United States (Houston, Texas) | 60 | 7.6 ± 1.8 years | 40% girls | Cohort | 1 year | Parent-reported OT and Actiwatch-measured ambient light exposure |
| Remmers (2014a) [70] | Southern Netherlands | 1317 | 5.0 ± 0.5 years | 49% girls | Cohort | 2 years | Parent-reported OP. Frequency and duration in an average week for the last 4 weeks |
| Remmers (2014b) [71] | Netherlands | 2007 | 5.75 ± 0.42 years | 49.5% girls | Healthcare cohort | 2 years | Parent-reported. Total duration of unstructured OP in an average week |
| Sadeh-Sharvit (2020) [72] | United States | 7 | 5.95 ± 3.57 years | Not available | Hospital | 8 weeks | Parent-reported. OP checklist |
| Sanchez-Tocino (2019) [73] | Spain (Valladolid and Burgos, Castilla y León) | 82 | 10 ± 3 years | 52.4% girls | Hospitals | 1.5 years | Parent-reported OT. Hours/week |
| Schneor (2021) [74] | Israel (central) | 19 | 10.2 ± 0.9 years | 0% girls | Clinics | 21 months | Actiwatch-measured ambient light exposure |
| Shepherd-Banigan (2014) [75] | United States (Eastern Washington State) | 99 | 6–12 years (median: 9.5) | 48% girls | Farming setting | 9 months | Parent-reported. Daily diary reporting children’s OT |
| Sum (2022) [76] | Singapore | 604 | 7.1 ± 3.6 years | 50.8% girls | Clinics | 3–5 months (retrospective) | Parent-reported frequency of OP or exercise |
| Van Griecken (2014) [77] | Netherlands | 293 | 5.8 ± 0.4 years | 61.9% girls | Healthcare centres | 2 years | Parent-reported (dichotomized as playing outside <1 h vs. ≥1 h per day) |
| Van Stralen (2012) [78] | Netherlands (Amsterdam) | 600 | 9.8 ± 0.7 years | 51% girls | Schools | 20 months | Child-reported frequency of OP |
| Walker (2021) [79] | United States (Texas) | 13 | 5–10 years | 46% girls | University (OP room) | 8 weeks | Parent-reported OT (hours/day) on weekdays and weekend days |
| Wolters (2022) [80] | Belgium, Cyprus, Estonia, Germany, Hungary, Italy, Spain, and Sweden | 2094 | 6.2 ± 1.8 years | 49% girls | School | 6 years | Child- or parent-reported OT (hours/day) for weekdays and weekend days |
| Studies beginning in adolescence (12–17 years) | |||||||
| Dunton (2007) [81] | United States (Southern California) | 524 | 14.5 ± 0.5 years | 49% girls | Schools | 4 years | Electronic ecological momentary assessment: proportion of entries in outdoor context |
| Evenson (2018) [82] | United States (California and Minnesota) | 265 | Grades 10–11 | 100% girls | Parks | 1 year | GPS-measured. Minimum park visit duration of 3 min to count as time spent in parks |
| French (2013) [83] | Australia (Sydney) | 1739 | 6.7 (younger cohort) and 12.7 (older cohort) | 47.3% girls | Cohort | 5–6 years | Parent-reported (and child-reported if 12+ years old). Sum of weekly time spent in outdoor leisure and sport |
| Gopinath (2013) [84] | Australia (Sydney) | 752 | 12.7 years at baseline | 53.3% girls | Cohort | 5 years | Sum of youth-reported time spent in different outdoor sporting activities in an average week |
| Lin (2017) [85] | China (Beijing) | 217 | 8.4 ± 1.1 and 14.2 ± 1.7 years for the primary and secondary students | 51.2% girls | Clinics | 3 years | Child-reported (parental help if needed). Sum of hours spent in outdoor sports and leisure after school |
| Miller (2017) [86] | United States (Chicago, Illinois) | 250 | Mean age of 12 years | 59% girls | Neighbourhoods | 1 year | Child-reported (ecological momentary assessment). Location reported ~7 times throughout the day. |
| Watowicz (2012) [87] | United States (Midwest) | 135 | 12.8 ± 2.8 years | 60% girls | Hospital (patients of a pediatric weight management centre) | 45 months (range = 8 to 86 months) [retrospective] | Children and parents completed questionnaire together (OP dichotomized as <1 vs. ≥1 h/day) |
Note: N = Sample size (only participants with outdoor time data were included); OP = outdoor play; OT = outdoor time; PA = physical activity; SD = standard deviation. a For the Buller et al. [33] study, the time period between pretest and post-test was not clear, but the intervention lasted 20 months.
3. Results
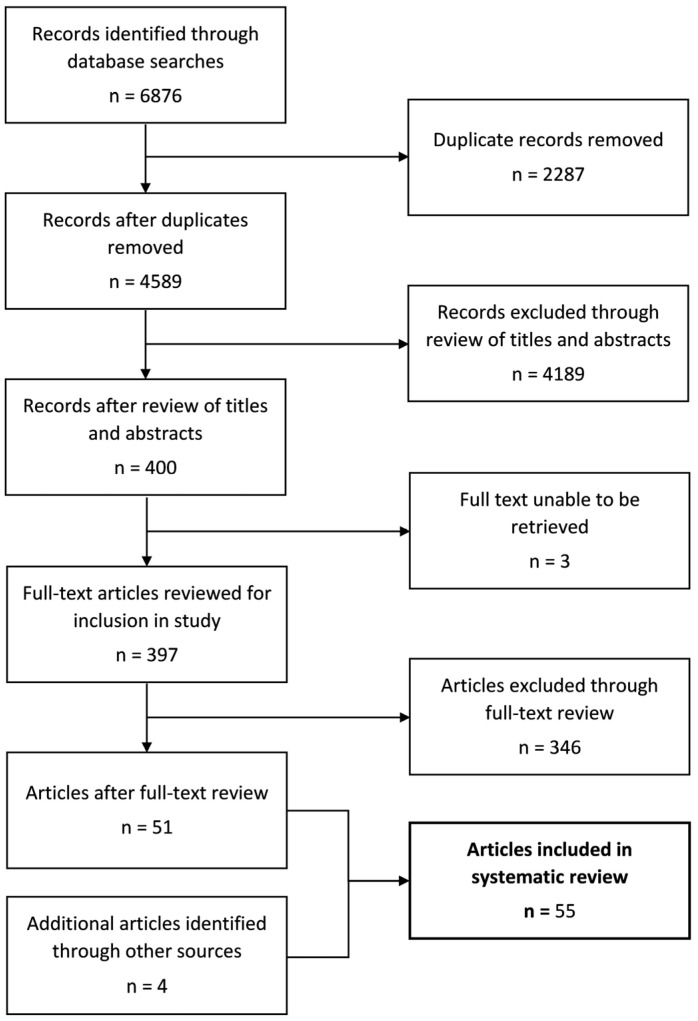
Figure 2 depicts the flow of the review process. Briefly, 4589 records were identified after the exclusion of duplicates. Of these, 4189 were excluded based on title and abstract screening. There were 3 full texts that could not be retrieved, and 346 were excluded based on inclusion/exclusion criteria, leaving 51 included articles. Three additional articles were included from twenty-six potentially relevant records identified by scanning the reference lists of included articles, and one was added from a narrative review of park prescription schemes [88]. Based on EPHPP guidelines, 16 of the 55 included papers were considered randomized controlled trials (RCTs) or controlled trials [12,37,38,39,44,45,47,53,57,59,60,64,65,67,77,78], 3 were quasi-experimental studies [36,54,58], 32 were prospective observational studies [34,35,40,41,42,43,46,48,49,50,51,52,55,56,62,63,66,68,69,70,71,72,73,74,75,80,81,82,83,84,85,86], 3 were retrospective longitudinal studies [61,76,87], and 1 was an uncontrolled pilot study [79]. Some studies combined data from control and experimental groups [35,40,82] and were considered observational because exposure to the intervention was not of substantive interest in the analyses. Table 1 summarizes the descriptive characteristics of the included studies categorized by age group at baseline (preschoolers (<5 years), children (5–11 years), and adolescents (12–17 years)) based on the mean, grade level, or midpoint of the reported age range. We classified studies that included distinct cohorts based on the highest mean age/grade reported. At baseline, the majority of cohorts had a mean age of <12 years. Only seven studies included a cohort of participants aged ≥ 12 years at baseline [81,82,83,84,85,86,87]. One study was conducted in boys only [74], and one was performed in girls only [82], whereas other studies included boys and girls. The sample size varied from 7 to 26,611, and the follow-up duration ranged from 8 weeks to 15 years. Almost all studies (n = 50) were conducted in high-income countries (e.g., USA (n = 21), Australia (n = 11), the Netherlands (n = 5), Denmark (n = 2), Singapore (n = 2), Canada (n = 1), Chile (n = 1), Finland (n = 1), Germany (n = 1), Israel (n = 1), Italy (n = 1), Spain (n = 1), and the UK (n = 1)), whereas 5 studies were conducted in upper-middle-income countries (China (n = 4) and Brazil (n = 1)). One study was conducted in eight European countries [80].
Figure 2.
Flow diagram for the review process.
3.1. Determinants of OT
Table 2 summarizes the potential determinants of OT and the main findings for each individual study stratified by age group. Table 3 presents the summary of associations between potential determinants (organized by levels of influence of the social-ecological model) and OT. Overall, the included studies investigated 119 potential determinants representing the personal, interpersonal, community, built and natural environment, and policy levels. Table 3 is not stratified by age group, as most included studies focused on 5- to 11-year-olds, and few determinants were investigated in ≥3 studies, limiting our ability to draw conclusions about the consistency of associations. It is also noteworthy that only four studies assessed policies in relation to OT [57,63,74,76].
With twenty studies, age was the most frequently examined variable. Overall, the association between age and OT is equivocal, with six studies reporting an increase with age [34,39,40,45,49,71], five showing a decrease [42,66,80,83,85], five showing mixed/inconsistent findings [43,55,70,81,82], and four reporting no associations [41,46,62,73]. However, five of the six studies reporting an increase involved younger cohorts (<5 years at baseline) [34,39,40,45,49], one of the studies coded as “mixed” reported an increase from 12 to 18 months of age followed by a steady decline until the last follow-up at 5 years [43], and one reported no changes in their younger cohort (ages 5–6 years at baseline), but a decrease in their older cohort (ages 10–12) [55]. Conversely, the average age was ≥5 years for four of the five studies reporting a decline in OT [66,80,83,85]. Five of the eleven studies that examined the association between gender and OT found that boys spent more time outdoors [50,71,81,83,85], one found similar findings in older but not younger children [55], and five found no gender differences [34,41,46,70,73]. Notably, all three studies examining gender differences in cohorts beginning in adolescence found significant differences [81,83,85]. Only two studies examined sex, reporting no differences between males and females [39,43].
Of the six studies examining parental education as a potential determinant, two found that children with more educated parents accumulated more OT [39,52], one found the opposite [70], two found no associations [41,61], and one found that children of more educated fathers increased their OT over time, whereas the mother’s education was not associated with OT [43]. For household income, two studies found no association [43,61], and one study found that higher income was associated with lower odds of eliminating OP or exercise during the COVID-19 lockdown in Singapore [76]. All seven studies that examined seasonal differences found that children spent significantly more time outdoors in warmer seasons [45,52,54,55,69,71,75]. Similarly, all three studies that assessed whether OT at a previous time point predicted current OT (i.e., past behaviour) reported significant positive associations [41,70,78]. Exposure to an intervention that included both sessions with parents and additional resources promoting OP (e.g., specific advice and community guide) was consistently associated with more OT (n = 3 interventions) [36,37,58]. In contrast, exposure to a school-based sun safety intervention that discouraged OT around midday was associated with lower midday OT among intervention groups in two out of three studies [53,64,65]. Lastly, all three studies that investigated the effect of the implementation of COVID-19 restrictions found decreases in OT [63,74,76], and one of these studies also reported that OT returned to pre-COVID levels after restrictions were lifted [74].
The criteria for consistency were not satisfied for any other potential determinant. It is worth noting that two of the three school-based curricular interventions that aimed to increase OT did not yield significant differences between experimental and control groups. In general, interventions that primarily focused on other health behaviours (e.g., PA in general and obesity) were less effective, with only 2/6 showing positive results. However, small sample sizes may have limited researchers’ ability to detect significant intervention effects. For example, the study by Ford et al. [59] included 28 participants, and despite a medium-to-large increase in OT following the intervention (Cohen’s d = 0.71), the effect was not statistically significant (p = 0.057). Similarly, Christiana et al. [54] found that an outdoor PA prescription scheme at a single pediatric practice did not result in increased OT at the 3-month follow-up, but the intervention was very small (n = 32) and took place from August to December, and the measure of OT was very crude (frequency assessed with a Likert scale). Still, 70% of parents reported using intervention materials, and 44% believed that the prescription encouraged their child to participate in outdoor activities [54].
3.2. Moderators and Mediators
As summarized in Table 4, twelve studies examined potential moderators. Child age (n = 3), sex (n = 3), and gender (n = 2) were the only potential moderators examined in at least two studies. Age was a significant moderator in two studies [46,63]. First, Shah et al. [46] found an interaction between age and the future risk of myopia and OT. Before the age of four, there were no differences in OT between children who later became myopic and those who remained non-myopic. Then, from 4 to 8.5 years, there was a larger decline in OT among children who became myopic. Second, Li et al. [63] examined whether age, sex, and household income moderated the effect of adherence to four preventive public health measures for COVID-19 on OT. Limiting the number of visitors was associated with a significant decline in OT in children under five years of age, but not in older children [63]. Two of the three studies examining sex as a moderator found no evidence of moderation [38,63]. Conversely, van Grieken et al. [77] found that males in the intervention group had a non-significant decrease in OP, whereas females demonstrated a significant and meaningful increase (>30 min/day). Regarding gender, French et al. [83] found no evidence of moderation, whereas Miller [86] claimed that there was a significant moderation effect but did not report the direction and magnitude of the association. However, Miller [86] did report that youth with lower levels of parental monitoring perceived their neighbourhood as more supportive and reported more OT, whereas youth with high parental monitoring perceived their neighbourhood as more dangerous and reported less OT. These findings suggest that parental monitoring may be a response to a perceived lack of safety that could instill in youth concerns about neighbourhood safety.
Remmers et al. [71] examined parent-perceived responsibility towards their child’s PA as a potential moderator. They noted that parent-perceived neighbourhood functionality was associated with more OP in children of parents with high perceived responsibility, while among parents with low perceived responsibility, functionality was related to less OP. They also found that the association between traffic safety and OP was stronger when parents perceived high vs. low responsibility. They suggested that “parents who feel responsible for the amount of their child PA may deliberately provide their child with the autonomy to play outside at spaces that they think are appropriate and safe” [71]. Handy et al. [61] found that the presence of children aged 6–12 in the household moderated the relationship between living in a cul-de-sac and the frequency of OP. Specifically, the presence of cul-de-sacs was supportive of OT for younger children compared to older children. However, the relationship between eleven other characteristics and OT was not modified by the presence of younger children [61]. Examining income as a potential moderator, Li et al. [63] noted that practising physical distancing led to a significant decrease in OT among children from families earning ≥ CAD 80,000, but not in those earning less. Finally, Schneor et al. [74] observed a larger decrease in OT during a full vs. partial COVID-19 lockdown. Only one study planned to examine potential mediators; however, their intervention was not effective, so the criteria for demonstrating mediation were not satisfied [78].
3.3. Study Quality
Table 5 summarizes the results of our quality appraisal with the EPHPP tool. Overall, 9 studies were rated as “moderate” [34,41,42,51,68,71,77,78,87], and the remainder (n = 46) were rated as “weak”. The components most frequently rated as “weak” were data collection tools (n = 43), selection bias (n = 30), confounders (n = 19), blinding (n = 18), and withdrawals (n = 15). Because we excluded cross-sectional studies, all included studies were rated as “moderate” or “strong” for their study design. The components most commonly rated as “strong” were withdrawals (n = 22), confounders (n = 18), study design (n = 16), data collection tools (n = 6), selection bias (n = 4), and blinding (n = 2).
Table 2.
Determinants of outdoor time in children and youth.
| Author (Year) | Potential Determinants Examined | Main Results |
|---|---|---|
| Studies Beginning in Early Childhood (<5 Years) | ||
| Arcury (2017) [34] | Gender, age, people per bedroom, number of inappropriate media (having a TV in view at meals and having a TV in the child’s bedroom), number of age-appropriate toys, limiting screen time, frequency of visits to play spaces | Compared to baseline, the mean time mothers estimated their child playing in the yard or park was 29.9 min/day greater at year 1 and 20.1 min/day greater at year 2 (both p = 0.001). For each additional month of age at baseline (B = 1.0 min/day, p = 0.049) and each age-appropriate toy (B = 12.3, p = 0.001), children spent more time playing in the yard or park. Each unit increase in the limiting screen time score was associated with less OP: B = −6.4, p = 0.016. |
| Cameron (2019) [35] | Influence of peer groups (i.e., partner, friends, mothers’ group, and family) on child’s nutrition, TV time, and PA | No association between influence of any peer group and time spent outside (all p > 0.05). |
| Davison (2011) [36] | Exposure to community guide and group sessions | Odds of playing outdoors > 60 min per day for the intervention site at follow-up compared to baseline was OR = 1.68 (95% CI = 1.19–2.37, p = 0.003). The adjusted OR for the intervention site at follow-up vs. comparison sites was 2.79 (95% CI = 1.94–4.02, p < 0.001). |
| Essery (2008) [37] | Effect of newsletter or booklet intervention on child feeding practices and physical activity | There was a significant increase in OP reported by the newsletter (p < 0.01) and booklet (p < 0.01) groups between baseline and post-test. |
| Händel (2017) [38] | Healthy Start Intervention, focused on changing diet, PA, sleep, and stress management | Participants in the intervention group spent more time on sports and outdoor activities combined at follow-up (intervention: 400 min/wk (95% CI: 341, 459) vs. control group: 321 min/wk (95% CI: 277, 366); p = 0.02). OP did not differ between groups post-intervention (intervention: 316 min/wk (95% CI: 264, 368) vs. 265 (95% CI: 209, 321); p = 0.19). |
| Hesketh (2015) [39] | Age, child sex, and mother’s education | OT increased from 25.7 to 90.0 min/day from 4 to 20 months of age (p < 0.001). Children of university-educated mothers engaged in more OT at all 3 time points (all p < 0.05). |
| Hnatiuk (2013) [40] | Age | Outdoor time increased from 46.93 ± 46.64 to 61.10 ± 48.35 min/week (p < 0.001). |
| Honda-Barros (2019) [41] | Age, gender, maternal education, school type (private vs. public), school shift (afternoon vs. morning), parent participation in PA with children, excess weight, and OP at baseline | Children who participated in PA with their parents were more likely to spend ≥60 min/day in OP (OR = 1.79; 95% CI = 1.27–2.54, p < 0.01). Children who spent ≥ 60 min/day in OP at baseline were more likely to maintain this behaviour after reaching school age (OR = 1.45; 95% CI = 1.02–2.07; p = 0.04). Children with excess weight at baseline engaged in less OP (OR = 0.56; 95% CI = 0.39–0.80; p < 0.01). |
| Huang (2021) [42] | Age | Over 2 years, the proportion of children who played outdoors ≥ 7 times a week decreased from 67.4 to 62.1%, and the proportion who played outdoors ≥ 60 min decreased from 53.3 to 38.8% (both p < 0.001). |
| Li (2022) [43] | Age, child sex, household size and income, pregnancy depression score, screen use, phone use, maternal and parental age, race, education level, and occupation | OT varied significantly with age (p < 0.001), with an increase from 12 to 18 months followed by a gradual decrease. Children from older and more educated fathers had an increase in OT over time (p < 0.05). |
| Lumeng (2017) [44] | Exposure to 1 of 3 interventions: (1) Head Start program + Preschool Obesity Prevention Series (targeting obesity prevention behaviours) + Incredible Years Series (IYS) (program to improve children’s self-regulation); (2) Head Start + Preschool Obesity Prevention Series; or (3) Head Start only | There were no differences in OT between children assigned to different interventions (intervention 2 vs. 3: change from baseline = −0.08 h/day, p = 0.48; intervention 1 vs. 3: change from baseline = 0.12 h/day, p = 0.25; intervention 2 vs. 1: change from baseline = 0.19 h/day, p = 0.06). |
| Sääkslahti (2004) [45] | Age, season, and exposure to intervention (parents of children in the intervention group received information and concrete suggestions on how, when, and where to encourage their child’s PA) | OP varied with intervention (p = 0.041), age (p = 0.016), and season (=12.72, p < 0.001). There were also combined relationships with age and season (p < 0.001), as well as intervention, age, and season (p < 0.001). The age-dependent increase was stronger in the intervention group. Children in the intervention group played more outdoors (p = 0.041) and less indoors (p = 0.049) than controls. |
| Shah (2017) [46] | Age, gender, future likely myopia, and number of myopic parents | Girls spent less time outdoors than boys (β = −0.04), but the difference was not significant (p = 0.14). Through the study period, children with one or two myopic parents spent an average of ~0.1 SD units per day less time outdoor than children whose parents were both non-myopic (p < 0.01). OT decreased with age, but the difference was not significant (β = 0.007; p = 0.073). |
| Tandon (2019) [47] | Exposure to interventions (Active Play! and Outdoor Play!) | In the preschool childcare centres receiving the Active Play! intervention, increases in outdoor child-initiated activity (18.8 min/day; 95% CI: 12.6, 25.0; p < 0.001), teacher-led activity (2.5 min/day; 0.1, 4.9; p = 0.04), and total OT (21.4 min/day; 14.6, 28.3; p < 0.001) were found. In the Outdoor Play! intervention group, OT increased by 24 min/day (95% CI: 19.3, 28.6; p < 0.001). Outdoor child-initiated activity increased (23.8 min/day; 19.1, 28.4), and outdoor teacher-initiated activity did not change significantly. The only significant post-intervention difference between interventions favoured Active Play! and was for outdoor teacher-led time (2.6 min/day; 4.5, 0.7; p = 0.008). |
| Thiering (2016) [48] | Birth in a rural (Wesel) vs. urban area (Munich) | Adolescents born in Wesel spent more time outside in the summer than those in Munich (χ2 = 46.94; p < 0.00001) a based on the frequencies reported in Table 1. |
| Xu (2016) [49] | Age, sleep patterns (bedtime, sleep duration, sleep latency, sleep time > 10 h/day, and waking at night) | Over time, there was an increase in children’s mean OP time (p < 0.0001). |
| Studies beginning in childhood (5–11 years) | ||
| Avol (1998) [50] | Gender and ambient ozone concentration | On average, boys spent ~37 min longer outside in the spring than girls (p < 0.001) and ~22 min more outside in the summer (p = 0.04). |
| Bacha (2010) [51] | Parent-perceived neighbourhood safety (classified in tertiles) | No difference in OT between tertiles of parent-perceived neighbourhood safety (p = 0.90). |
| Bagordo (2017) [52] | Season, parental education, and father’s occupational level | 70.3% of children played outdoors for >1 h/day at follow-up (spring) vs. 33% at baseline (winter) (p < 0.001). Children whose parents had <26 combined years of education were more likely (59.7% vs. 48.7%) to engage in >1 h/day of OP (p < 0.001). Children whose fathers had level III or IV occupations (service worker or unemployed, respectively) were more likely (57.4% vs. 48.1%) to engage in >1 h/day of OP (p < 0.001). |
| Buller (2020) [53] | Exposure to intervention on sun safety | In schools where principals implemented sun safety practices, parents reported that children spent less time outdoors between 10 am and 4 pm over one week (mean = 14.78 vs. 16.32 h; p = 0.033). |
| Christiana (2017) [54] | Exposure to outdoor PA prescription intervention and season | No difference in frequency of OT between groups and frequency of achieving ≥60 min of outdoor PA (p ≥ 0.29). OT declined from baseline (August) to follow-up (November/December; p < 0.01); authors attributed this finding to seasonality. |
| Cleland (2008) [55] | Seasons, age, and gender | OT was higher during warmer vs. cooler months at Time 1 and Time 2 (p < 0.01). OT was higher in older boys vs. older girls in both seasons at both time points. OT during warmer months declined between Time 1 and 2 among older boys (p < 0.01), OT on weekends in the warmer months declined among older girls (p < 0.01), and OT on weekdays in the colder months increased among older girls (p < 0.01). |
| Cleland (2010) [56] | Outdoor tendencies, indoor tendencies, parental encouragement, social opportunities, rules and restrictions, parental belief that child must be supervised when playing outside, parent report that there are no adults to supervise child while playing outside after school, dog ownership, number of siblings, yard size, home PA opportunities, access to local destinations, and weather as barrier (individual items: cold/dark in the winter; heat in the summer) | For younger boys, “high” indoor tendencies were associated with less OT (−168 min/wk; 95% CI = −324, −13), while “high” social opportunities were associated with more OT over 5 years (170 min/wk; 95% CI = 26, 314). Among older boys, higher indoor tendencies (“medium”: −215 min/wk; 95% CI = −311, −119; “high”: −324; 95% CI = −472, −176) and a lack of adult supervision (−47 min/wk; 95% CI = −91, −3) were associated with less OT, while “high” outdoor tendencies were associated with more OT over 5 years (123 min/wk; 95% CI = 40, 207). Among younger girls, higher indoor tendencies were associated with less OT (“medium”: −188 min/wk; 95% CI = −356, −21; “high”: −247 min/wk; 95% CI = −374, −120), while “high” parental encouragement was associated with more OT over 5 years (234 min/wk; 95% CI = 30, 438). Among older girls, “medium” outdoor tendencies (200 min/wk; 95% CI = 27, 374) and “high” parental encouragement were associated with more OT (151 min/wk; 95% CI = 67, 236), while a lack of adult supervision was associated with less OT (−34 min/wk; 95% CI= −60, −9). |
| Cortinez-O’Ryan (2017) [57] | Exposure to an evening street closure intervention (twice a week for 12 weeks) | There were significant increases in median number of weekdays with OP (from 2 to 3; p < 0.01), after-school OP time (from 60 to 90 min; p = 0.02), and weekly after-school OP time in the experimental neighbourhood (from 120 to 300; p = 0.01). No changes were observed in the control neighbourhood. |
| Flynn (2017) [58] | Exposure to intervention: family resource workbook and 3 group sessions | During the program, families increased their time spent being active together by an average of 111 min/week above baseline. Outdoor PA time was higher than baseline in 3 out of 4 weeks (p < 0.05). Mean length of a family outdoor PA bout was significantly greater than at baseline for all 4 weeks of the program. Families increased the mean length of their family outdoor PA bouts by ~41 min/bout. Frequency of family outdoor PA bouts did not change significantly. |
| Ford (2002) [59] | Behavioural vs. counselling (control) intervention to reduce children’s television viewing | Compared to the control group, the behavioural intervention led to a medium-to-large increase in OT (change of 1.0 ± 5.9 vs. −4.7 ± 9.4 h/wk; Cohen’s d = 0.71); however, this difference was not statistically significant (p = 0.057). |
| Gerards (2015) [60] | Exposure to the “Lifestyle Triple P” intervention | The increase in OT between baseline and first follow-up (4 months) was not significant (B = 2.85; 95% CI= −0.16, 5.86; p = 0.063; Cohen’s d = 0.56). Significant increase was found at the final (12 month) follow-up (B = 1.94; 95% CI = 0.04, 3.84; p < 0.05; Cohen’s d = 0.55). |
| Handy (2008) [61] | Parental preference for and perceptions of neighbourhood characteristics ((1) nearby amenities; (2) neighbourhood upkeep; (3) large back yard; (4) large front yard; (5) living in a cul-de-sac rather than on a through street; (6) low traffic on neighbourhood streets; (7) parks and open spaces nearby; (8) sidewalks through neighbourhood; (9) lots of interaction among neighbours; (10) lots of people out and about in the neighbourhood; (11) low crime rate in neighbourhood; (12) safe neighbourhood for children to play). Perceived changes in abovementioned characteristics, age of children in the household, parental education, household income, changes in household size, changes in number of children in household, changes in income, type of housing (apartment vs. other) suburban vs. traditional neighbourhood | After residential relocation, 52.7% of parents reported no change in OP frequency, 15.7% reported a decline, and 31.5% reported an increase. Preference for a safe neighbourhood for kids to play was associated with more OP (β = 0.147; p = 0.028). Changes in 4 perceived neighbourhood characteristics were also associated with more OP: cul-de-sac interacted with the presence of children ages 6–12 years (β = 0.170 p = 0.014), large front yards (β = 0.200; p = 0.005), low crime (β = 0.290; p = 0.002), and interaction among neighbors (β = 0.189; p = 0.008). Parents with children aged 12–16 were more likely to report no change in OP vs. those with younger children. Households with children aged 5–12 were more likely to report an increase in OP (β = 0.234; p = 0.001) than households with older children. |
| He (2015) [12] | Exposure to outdoor play intervention (additional outdoor activity class; 40 min/school day) | No difference in OT between children in intervention and control schools at baseline and 1-, 2-, and 3-year follow-ups (all p > 0.20). |
| Kemp (2022) [62] | Age | Time spent in “other outdoor/nature activities” (the time use category that included OT) did not change with age (all p > 0.05). |
| Li (2021) [63] | COVID-19 (number of days/week that children practised 4 preventive public health measures) | For each additional day/week that children adhered to public health measures, OT decreased by 17.2 min/day in the unadjusted model (95% CI = −22.07, −12.40; p < 0.001) and by 12.5 min/day in the adjusted model (95% CI = −18.25, −6.79; p < 0.001). Adherence to each individual measure was associated with less OT in both the unadjusted and adjusted models (p < 0.05), except for limiting the number of visitors. |
| Milne (2000) [64] | Exposure to school-based multicomponent intervention with specially designed curriculum (“medium” intervention) vs. exposure to multicomponent intervention plus program materials over the summer holidays and low-cost sun-protective swimwear (“high” intervention) compared to standard health curriculum (“control”) | Adjusted mean OT during the summer holidays between 11 am and 2 pm was highest in the control group (28.4 h) vs. the high intervention group (22.3 h) and the moderate group (24.1 h) (p = 0.01). Children in the moderate group tended to spend less time outside in both periods. Adjusted mean OT between 8 am and 4 pm was 111 h for the control group (95% CI: 103.9, 118.5), 113 h for the moderate group (104.6, 121.6), and 108.7 h for the high group (99.4, 118.5), with no differences between groups (p = 0.8). |
| Milne (2007) [65] | School-based sun protection curriculum over 4 years; children were encouraged to reduce sun exposure by staying indoors during the middle of the day, when solar ultraviolet radiation is highest, and to protect themselves when outdoors by using shade, clothing, hats, and sunscreen | The median OT in each group (control, “moderate” intervention, and “high” intervention) was similar after 2 years. There was no association between study group and total OT at either age 10 or age 12. |
| Nigg (2021) [66] | Age, OP (past behaviour), MVPA, TV, and computer/gaming time in previous survey waves | OP decreased from 5.93 ± 1.43 days/week at Time 1 to 1.14 ± 1.85 days/week at Time 3. OP at Time 1 was associated with more OP at Time 2, which was positively associated with OP at Time 3 (p < 0.05). |
| Ngo (2009) [67] | Exposure to intervention: structured weekend outdoor activities and incentives for children to increase their daily steps via pedometers | At the 6-month follow-up, a mean of 14.75 h/wk of OT was reported in the questionnaire for the intervention group vs. 12.40 h/wk for the control group (p = 0.04). At the 9-month follow-up, parents in the intervention and control groups reported 15.95 vs. 14.34 h/wk outdoors (p = 0.29). Mean OT from the diary was 6.98 h/wk and 7.93 h/wk for the control and intervention groups, respectively (p = 0.12). |
| Nordvall-Lassen (2018) [68] | “Moderate” preterm (32–36 weeks of gestation) vs. term birth | No difference in odds of reporting different weekly durations of OT based on birth status (OR for 4–6 h = 1.13 (95% CI = 0.59–1.74), OR for 7–13 h = 1.14 (0.61–1.70), OR for 14–20 h = 1.15 (0.52–1.67), and OR for 21–60 h = 1.20 (0.35–2.22)). |
| Ostrin (2018) [69] | Seasons (spring, summer, and fall) and parental outdoor time | Children were more exposed to outdoor light (lux) in the summer (110.5 ± 45.8 min/day) vs. spring (94.2 ± 30.4 min/day) or fall (72.2 ± 31.0 min/day, p < 0.0001). Children received the highest mean daily light exposure during the summer vs. spring and fall seasons (p < 0.0001). Parent and child OT were significantly correlated (r = 0.76, p = 0.0002). |
| Remmers (2014a) [70] | Gender, age, and parental and environmental factors, including accessibility of PA-related places, attitude towards child PA, concern regarding child PA, restriction of screen time, social capital, functionality, traffic safety, attractiveness, perceived responsibility, pressure, and monitoring | Children spent on average ~60 more minutes in OP per week at 7 vs. 5 years of age (both boys and girls) (p < 0.01). At both time points, boys spent significantly more time in OP than girls (p < 0.01), and there were significant differences in OP duration between all seasons (p < 0.01; but season was examined as a random effect, and the direction of association was not reported). Significant regression coefficients (β) for parental factors were accessibility of PA-related places within 10 min walking distance of home with 0.05 (95% CI = 0.01, 0.09), positive parental attitude towards child PA with 0.09 (0.05, 0.13), concern regarding child PA with −0.04 (−0.09, −0.001), restriction of screen time with −0.21 (−0.26, −0.17), and social capital with 0.07 (0.03, 0.11). |
| Remmers (2014b) [71] | Socio-demographic characteristics (child age, gender, ethnicity, and BMI and parental age, ethnicity, BMI, and education), family environment (parental attitude, family attitude, perceived difficulty, habit strength and intention to improve OP, presence of rules, presence of monitoring, presence of active encouragement, and child autonomy), and parent-perceived physical environment (safety perception during daytime and evenings, friendliness for children, attractiveness for children, and safety of OP without supervision) | Parents with high vs. low education reported that their child played outside 28.40 min/day less (95% CI = −55.66, −1.14) at age 7. Parents who indicated difficulty towards improving OP reported 22.11 (−33.41, −10.81) less minutes of OP. Parents with a habit towards improving OP (23.99; 95% CI = 14.61, 33.61), the presence of rules regarding OP (16.46; 95% CI = 9.26 to 23.67), and modelling from the respondent’s partner (1.85; 95% CI = 0.27, 3.42) were associated with more min/day of OP. Parental active encouragement of OP at baseline was associated with 8.91 (−17.33 to −0.48) less minutes of OP at age 7. Higher child age was related to more OP at baseline, but this attenuated significantly over time (p[interaction] < 0.01). |
| Sadeh-Sharvit (2020) [72] | Exposure to intervention (online 6-session parent-based prevention program after bariatric surgery) | Children spent less time outdoors at follow-up as reported by parents with bariatric surgery (baseline: 125.63 (58.88) min/day; follow-up: 103.00 (61.40); Hedges’ g = 0.36 (−0.64, 1.35)) or partners (baseline: 102.86 (58.71) min/day; follow-up: 97.50 (102.10); Hedges’ g = 0.06 (−1.05, 1.18)). As 95% CIs cross 0, differences were not significant. |
| Sanchez-Tocino (2019) [73] | Age and gender | There were no significant differences in hours spent on outdoors activities by age or gender (p > 0.05). |
| Schneor (2021) [74] | COVID-19 restrictions | Daily OT decreased from 1.8 ± 1.0 h to 0.7 ± 0.7 h (p = 0.001). In the subsample followed up after restrictions were removed, OT returned to pre-pandemic levels (1.8 ± 0.8 h). |
| Shepherd-Baniga (2014) [75] | Farmworker vs. non-farmworker status and agricultural seasons (thinning vs. pre-thinning) | Children spend 9 h/wk more outside during the thinning (summer) vs. pre-thinning season (spring) (95% CI: −13.0, −5.1, p < 0.001). In the thinning season, mean OT was 30.2 ± 20.8 h/wk for farmworker children vs. 24.2 ± 16.7 h/wk for non-farmworker children (p = 0.004). |
| Sum (2022) [76] | COVID-19 restrictions and household income | 64.1% of parents reported significant decreases in OP or exercise due to the COVID-19 lockdown (p < 0.001). Each 1,000-Singapore-dollar decrease in income before the lockdown was associated with higher odds of reporting the elimination of all OP or exercise (OR = 1.09; 95% CI = 1.01, 1.19; p = 0.03). |
| Van Griecken (2014) [77] | Exposure to a healthy lifestyle counselling intervention to parents of overweight 5-year-olds | Proportion of children playing outside ≥ 1 h/day decreased in the intervention (93.3 to 77.1%; p < 0.001) and control groups (94.3 to 77.1%; p < 0.001), with no difference between groups (OR = 1.11; 95% CI = 0.60, 2.06). There was no significant difference in OP, expressed in min/day, at follow-up (β = 8.22; 95% CI = −15.77, 32.22) between groups. |
| Van Stralen (2012) [78] | Exposure to JUMP-in school-based intervention targeting sports participation and outdoor play. Also examined the effect of OP at baseline and child-perceived pros and cons, social pressure, social support, social modelling, self-efficacy, planning skills, barriers, enjoyment, and habit strength related to OP | No significant intervention effect in the weekly frequency of OP (B= −0.30; 95% CI= −0.79, 0.19). Significant positive associations were found between social support (b = 0.04; 95% CI: 0.01–0.08), self-efficacy (b = 0.15; 95% CI: 0.00–0.30), enjoyment (b = 0.21; 95% CI: 0.14–0.28), and habit strength (b = 0.38; 95% CI: 0.18–0.58) and OP. In their Figure 3, the authors show that OP at Time 1 (b = 0.17) and planning skills (b = 0.15) were significantly associated with more OP at Time 2 (but did not provide the p-value). |
| Walker (2021) [79] | Participation in a child-centred play therapy intervention | There were no differences in OT on weekdays and weekend days between baseline and the end of the intervention (all p > 0.20) |
| Wolters (2022) [80] | Age | OT was higher at baseline vs. the last follow-up: 2.41 ± 1.39 vs. 1.80 ± 1.29 h/day (t = 13.63; p < 0.0001 based on the values reported in Table 2) b |
| Studies beginning in adolescence (12–17 years) | ||
| Dunton (2007) [81] | Gender, age, time of week, and season | Compared with girls, boys were more likely to report exercising in outdoor settings (p = 0.002) and walking in outdoor settings (p < 0.001). Walking in an outdoor setting decreased during high school (7% per year, p = 0.019), but outdoor exercising did not (p = 0.189). Students were more likely to exercise or walk outdoors on weekend days vs. weekdays (p < 0.001). Students were more likely to walk or exercise outdoors in the fall and spring seasons vs. the winter (all p < 0.05) and to walk outdoors in the spring vs. fall season (p = 0.010). |
| Evenson (2018) [82] | Age | The number of park visits identified by GPS during the 6-day monitoring period increased from 73 to 83 (p < 0.02). Mean duration of park visits decreased from 63.9 to 38.4 min (p < 0.03). |
| French (2013) [83] | Age, ethnicity, and gender | In the young cohort, OT decreased by just over 1 h/wk from baseline to follow-up, accompanied by a decline in outdoor leisure (both p ≤ 0.001). Time spent on organized outdoor sports increased (p < 0.0001). In the older cohort, there was a significant decrease in OT and outdoor sporting activities (p < 0.0001), but not in outdoor leisure time (p = 0.06). Boys spent ~2.5 h/wk more outdoors than girls in both cohorts at baseline and follow-up (all p < 0.0001). The decrease in OT between baseline and follow-up was significant for girls in both cohorts (younger, p = 0.006; older p < 0.0001) and for boys in the older cohort (p = 0.001), but not in the younger cohort (p = 0.052). The decline in OT with age was seen in European Caucasian participants (younger cohort: p = 0.001; older cohort: p < 0.0001), but not in East Asian participants (younger cohort: p = 0.7; older cohort: p = 0.07). |
| Gopinath (2013) [84] | Birth weight (categorized in quartiles) | In 12-year-olds, an increase in outdoor PA (~1 h/wk) was observed with increasing birth weight after adjustment for covariates (from the lowest to highest quartile; ptrend = 0.02). Among 17- to 18-year-olds, higher birth weight was associated with higher outdoor PA (~1 h/wk, p = 0.04). In multivariable models, each SD (573.5 g) increase in birth weight was associated with a 15 min/wk increase in outdoor PA (p = 0.01). Twelve-year-olds in the high- vs. very-low-birth-weight group (>4000 vs. <2000 g) spent ~1.3 h/wk more in outdoor PA (ptrend = 0.02). |
| Lin (2017) [85] | Age and gender | Among all students combined, there was a decrease in leisure OT (8.5 ± 7.7 vs. 9.9 ± 7.0 h/wk, p = 0.02). For primary students, there was an increase in outdoor sports time (3.5 ± 4.3 vs. 2.4 ± 3.0 h/wk, p = 0.02). For secondary students, there was a non-significant decrease in total OT (10.9 ± 8.8 vs. 12.7 ± 9.8 h/wk, p = 0.09). Girls spent less time outdoors than boys (baseline: 11.9 ± 7.9 vs. 14.4 ± 9.5 h/wk, p = 0.03; follow-up: 10.5 ± 8.2 vs. 13.9 ± 9.6 h/wk, p = 0.005) and less time in outdoor sports (baseline: 2.4 ± 2.8 vs. 4.0 ± 5.2 h/wk, p = 0.006; follow-up: 2.3 ± 3.1 vs. 5.1 ± 5.0 h/wk, p < 0.001). |
| Miller (2017) [86] | Parental perceptions of neighbourhood danger, perceived neighbourhood support, parental monitoring (in general), and OT at baseline | There was a positive correlation between the percent time spent outside at Times 1 and 2 (r = 0.480). Increased levels of parental monitoring at Time 1 was associated with increased OT at Time 2 (coeff = 0.7508, p = 0.0109). |
| Watowicz (2012) [87] | Recent parental weight loss surgery | Control group participants were significantly more likely than those whose parents underwent weight loss surgery to report ≥1 h/day of OP (55.8 vs. 31.6%, p = 0.01). |
Note: When potential determinants are not mentioned in the third column, this means that they were not significantly associated with outdoor time. B = unstandardized regression coefficient; β = standardized regression coefficient; CI = confidence interval; coeff = coefficient; OP = outdoor play; OR = odds ratio; OT = outdoor time; PA = physical activity; SE = standard error. a Chi-square test performed by the review team based on reported frequencies using an online calculator (https://www.socscistatistics.com/tests/chisquare2/default2.aspx, accessed on 1 December 2022). b t-test performed by the review team based on reported means and standard deviations using an online calculator (https://www.graphpad.com/quickcalcs/ttest1/, accessed on 1 December 2022).
Table 3.
Summary of the determinants of outdoor time in children and youth.
| Variable | Level of Influence | Number of Studies | Positive (%) | Negative (%) | Mixed (%) | Null (%) | Summary Code |
|---|---|---|---|---|---|---|---|
| Child sex (male) | Individual | 2 | 0 (0%) | 0 (0%) | 0 (0%) | 2 (100%) | N/A |
| Child gender (boy) | Individual | 11 | 5 (45.5%) | 0 (0%) | 1 (9%) | 5 (45.5%) | (+) |
| Child age (older) | Individual | 20 | 6 (30%) | 5 (25%) | 5 (25%) | 4 (20%) | Equivocal |
| Child ethnicity (dominant vs. other) | Individual | 2 | 0 (0%) | 1 (50%) | 0 (0%) | 1 (50%) | N/A |
| Birth weight (higher) | Individual | 1 | 1 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | N/A |
| Preterm birth (yes vs. no) | Individual | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Child weight status (overweight/higher BMI vs. normal weight) | Individual | 2 | 0 (0%) | 1 (50%) | 0 (0%) | 1 (50%) | N/A |
| Child moderate- to vigorous-intensity PA (higher) | Individual | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Child screen time (higher) | Individual | 2 | 0 (0%) | 0 (0%) | 0 (0%) | 2 (100%) | N/A |
| Number of age-appropriate toys (higher) | Individual | 1 | 1 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | N/A |
| Frequency of visits to play spaces (higher) | Individual | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Outdoor tendencies score (higher) | Individual | 1 | 0 (0%) | 0 (0%) | 1 (100%) | 0 (0%) | N/A |
| Indoor tendencies score (higher) | Individual | 1 | 0 (0%) | 1 (100%) | 0 (0%) | 0 (0%) | N/A |
| OP at baseline (higher) | Individual | 3 | 3 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | + |
| Child-perceived neighbourhood danger (greater danger) | Individual | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Child autonomy (higher) | Individual | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Child-perceived pros and cons of OP (higher) | Individual | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Child-perceived social support for OP (higher) | Individual | 1 | 1 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | N/A |
| Child-perceived social modelling of OP (higher) | Individual | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Child-perceived self-efficacy for OP (higher) | Individual | 1 | 1 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | N/A |
| Child-perceived habit strength for OP (higher) | Individual | 1 | 1 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | N/A |
| Child planning skills for OP (higher) | Individual | 1 | 1 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | N/A |
| Child-perceived barriers to OP (higher) | Individual | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Child enjoyment of OP (higher) | Individual | 1 | 1 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | N/A |
| Child likely to develop myopia in the future (yes vs. no) | Individual | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Child sleep patterns | Individual | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Participation in a child-centred play therapy intervention | Individual | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Parent-perceived neighbourhood safety (safer) | Interpersonal | 2 | 0 (0%) | 0 (0%) | 0 (0%) | 2 (100%) | N/A |
| Parental education (higher vs. lower) | Interpersonal | 6 | 2 (33.3%) | 1 (16.7%) | 1 (16.7%) | 2 (33.3%) | Equivocal |
| Household income (higher) | Interpersonal | 3 | 1 (33.3%) | 0 (0%) | 0 (0%) | 2 (66.7%) | 0 |
| Father’s occupation (service workers/unemployed vs. higher class) | Interpersonal | 1 | 1 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | N/A |
| Parental occupation | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Family size | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Changes in household income (increase) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Changes in household size (increase) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Changes in the number of children in household (increase) | Interpersonal | 1 | 1 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | N/A |
| Type of housing (apartment vs. other) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Number of people per bedroom (higher) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Number of “inappropriate” media (higher) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Limiting screen time (more restriction) | Interpersonal | 2 | 0 (0%) | 2 (100%) | 0 (0%) | 0 (0%) | N/A |
| Rules and restrictions related to OP (more vs. less) | Interpersonal | 2 | 1 (50%) | 0 (0%) | 0 (0%) | 1 (50%) | N/A |
| Parental concern with child’s PA (more concern) | Interpersonal | 1 | 0 (0%) | 1 (100%) | 0 (0%) | 0 (0%) | N/A |
| Parental attitude towards child’s PA (more positive) | Interpersonal | 1 | 1 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | N/A |
| Parental and family attitude towards OP (more positive) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Perceived difficulty of increasing OP (higher) | Interpersonal | 1 | 0 (0%) | 1 (100%) | 0 (0%) | 0 (0%) | N/A |
| Parental habit strength to improve OP (higher) | Interpersonal | 1 | 1 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | N/A |
| Parental intention to improve OP (higher) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 1 (100%) | 0 (0%) | N/A |
| Parental encouragement of OP (more encouragement) | Interpersonal | 2 | 0 (0%) | 1 (50%) | 1 (50%) | 0 (0%) | N/A |
| Parent participation in PA with children (higher) | Interpersonal | 1 | 1 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | N/A |
| Parent OT (higher) | Interpersonal | 1 | 1 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | N/A |
| Parent age (higher) | Interpersonal | 2 | 0 (0%) | 0 (0%) | 1 (50%) | 1 (50%) | N/A |
| Parent BMI (higher) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Parent race/ethnicity (dominant vs. other) | Interpersonal | 2 | 0 (0%) | 0 (0%) | 0 (0%) | 2 (100%) | N/A |
| Social opportunities score (higher) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 1 (100%) | 0 (0%) | N/A |
| Dog ownership (yes vs. no) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Number of siblings (higher) | Interpersonal | 2 | 0 (0%) | 0 (0%) | 0 (0%) | 2 (100%) | N/A |
| Home PA opportunities (higher) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Parental belief that child must be supervised when playing outside (higher agreement) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Parent report that there are no adults to supervise child while playing outside after school (higher agreement) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 1 (100%) | 0 (0%) | N/A |
| Perceived influence of peer groups (i.e., partner, friends, mother, and family) on child’s nutrition, TV time, and PA (higher) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Parental preference for access to nearby amenities (higher) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Parental preference for high level of neighbourhood upkeep (higher) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Parental preference for large back or front yard (higher) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Parental preference for living in a cul-de-sac vs. on a through street (higher) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Parental preference for low traffic on neighbourhood streets (higher) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Parental preference for parks and open spaces nearby (higher) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Parental preference for sidewalks throughout neighbourhood (higher) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Parental preference for lots of interaction among neighbours or lots of people out and about in the neighbourhood (higher) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Parental preference for low crime rate in neighbourhood (higher) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Parental preference for a safe neighbourhood for kids to play (higher) | Interpersonal | 1 | 1 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | N/A |
| Parental monitoring, not specific to OP (higher) | Interpersonal | 2 | 1 (50%) | 0 (0%) | 0 (0%) | 1 (50%) | N/A |
| Parental monitoring of PA (higher) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Parent-perceived responsibility for child PA (higher) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Parental pressure for child to be active (higher) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Number of myopic parents (1 or 2 vs. 0) | Interpersonal | 1 | 0 (0%) | 1 (100%) | 0 (0%) | 0 (0%) | N/A |
| Farmworker parent (yes vs. no) | Interpersonal | 1 | 1 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | N/A |
| Pregnancy depression score | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Pregnancy screen time (higher) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Recent parental weight loss surgery (yes vs. no) | Interpersonal | 1 | 0 (0%) | 1 (100%) | 0 (0%) | 0 (0%) | N/A |
| Sessions with parents with additional resources (e.g., specific advice and community guide) promoting OP (yes vs. no) | Interpersonal | 3 | 3 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | + |
| Newsletter or booklet intervention on healthy eating and PA (yes vs. no) | Interpersonal | 1 | 1 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | N/A |
| Counselling intervention to reduce TV viewing (yes vs. no) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Lifestyle Triple P intervention (focused on nutrition, PA, and positive parenting strategies; yes vs. no) a | Interpersonal | 1 | 1 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | N/A |
| Intervention—structured weekend outdoor activities and incentives for children to increase steps counts via pedometers (yes vs. no) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 1 (100%) | 0 (0%) | N/A |
| Intervention—parent-based prevention program after parental bariatric surgery (yes vs. no) | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Intervention—pediatrician outdoor PA prescription | Interpersonal | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Parent-perceived interactions among neighbours (higher) | Community | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Parent-perceived change in interactions among neighbours (increase) | Community | 1 | 1 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | N/A |
| Parent-perceived people out and about in the neighbourhood or changes in the number of people out and about (more) | Community | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Parent-perceived low crime rate in neighbourhood (increase) | Community | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Parent-perceived change in crime rate in neighbourhood (lower) | Community | 1 | 1 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | N/A |
| School type (private vs. public) | Community | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| School shift (afternoon vs. morning) | Community | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Parent-perceived social capital (higher) | Community | 1 | 1 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | N/A |
| Youth-perceived neighbourhood support (higher) | Community | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Parent-perceived neighbourhood friendliness or attractiveness for children (higher) | Community | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| School-based sun safety intervention discouraging outdoor activities at certain times of the day (yes vs. no) | Community | 3 | 0 (0%) | 2 (66.7%) | 0 (0%) | 1 (33.3%) | - |
| Preschool interventions focused on health behaviours and stress management/self-regulation (yes vs. no) | Community | 2 | 0 (0%) | 0 (0%) | 0 (0%) | 2 (100%) | N/A |
| School curriculum intervention to increase OP (yes vs. no) | Community | 3 | 1 (33.3%) | 0 (0%) | 0 (0%) | 2 (66.7%) | 0 |
| Parent-perceived access to local destinations for PA (higher or increase over time) | Built environment | 2 | 0 (0%) | 0 (0%) | 0 (0%) | 2 (100%) | N/A |
| Parent-perceived neighbourhood upkeep (higher or increase over time) | Built environment | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Parent-perceived back or front yard size (larger) | Built environment | 2 | 0 (0%) | 0 (0%) | 0 (0%) | 2 (100%) | N/A |
| Parent-perceived change in large back or front yard size (increase) | Built environment | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Living in a cul-de-sac vs. on a through street (or moving to a cul-de-sac) | Built environment | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Parent-perceived traffic on neighbourhood streets (low or decrease) | Built environment | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Parent-perceived parks and open spaces nearby (higher or increase) | Built environment | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Parent-perceived sidewalks through neighbourhood (higher or increase) | Built environment | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Parent-perceived neighbourhood functionality (higher) | Built environment | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Parent-perceived neighbourhood attractiveness (higher) | Built environment | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Parent-perceived traffic safety (higher) | Built environment | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Living in suburban vs. traditional neighbourhood | Built environment | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Living in an urban vs. rural area | Built environment | 1 | 0 (0%) | 1 (100%) | 0 (0%) | 0 (0%) | N/A |
| Ambient ozone concentration (higher) | Natural environment | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Season (warmer) b | Natural environment | 7 | 7 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | + |
| Weather perceived as a barrier by parent (higher) | Natural environment | 1 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | N/A |
| Time of the week (weekdays vs. weekend days) | Chronosystem | 1 | 1 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | N/A |
| Street closure intervention (yes vs. no) | Policy | 1 | 1 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | N/A |
| COVID-19 restrictions (adoption) | Policy | 3 | 0 (0%) | 3 (100%) | 0 (0%) | 0 (0%) | - |
| COVID-19 restrictions (removal) | Policy | 1 | 1 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | N/A |
Note: BMI: body mass index; OP: outdoor play; OT: outdoor time; PA: physical activity. a The intervention effect was significant at 12 months and close to significance at 4 months (p = 0.063; Cohen’s d = 0.56) [60], so the intervention effect was deemed positive. b Sääkslahti et al. [45] also found significant difference between spring and fall seasons, but it is not included in this table because it was not clear which season was warmer. Due to the small number of studies that were not rated as “weak” based on the Effective Public Health Practice Project tool (see Table 5), the risk of bias remains high for most potential determinants.
Table 4.
Moderators and mediators examined in relation to outdoor time.
| Author (Year) | Moderators or Mediators Examined | Results |
|---|---|---|
| Avol (1998) [50] | Asthma status (healthy, “wheezy”, or asthmatic) as potential moderator | Asthma status did not moderate the relationship between peak hourly ambient ozone (O3) concentration and OT (all p > 0.10). |
| French (2013) [83] | Gender and ethnicity as potential moderators | Gender and ethnicity did not moderate the relationship between age and outdoor time (all p ≥ 0.2). |
| Händel (2017) [38] | Sex, age, mother’s BMI, mother’s education, and mother’s PA level were examined as potential moderators of the effect of the intervention. | No significant interactions were found (all p ≥ 0.2). |
| Handy (2008) [61] | The presence of children aged 6 to 12 was examined as a potential moderator between 12 perceived neighbourhood characteristics ((1) nearby amenities; (2) neighbourhood upkeep; (3) large back yard; (4) large front yard; (5) living in a cul-de-sac rather than on a through street; (6) low traffic on neighbourhood streets; (7) parks and open spaces nearby; (8) sidewalks through neighbourhood; (9) lots of interaction among neighbours; (10) lots of people out and about in the neighbourhood; (11) low crime rate in neighbourhood; (12) safe neighbourhood for children to play) and weekly frequency of OP. | The only significant interaction in longitudinal analyses was between the change in cul-de-sac and the presence of children aged 6–12 in the household (β = 0.170; p = 0.014), suggesting that the presence of cul-de-sacs is supportive of OP for younger children. |
| Li (2021) [63] | Child age, sex, and household income as potential moderators | The effect of limiting the number of visitors on OT was significant in children < 5 years (β = −9.94, 95% CI = −17.18, −2.71, p = 0.01), but not in older children. The effect of practising physical distancing was significant for children for families earning ≥ CAD 80,000 (β = −5.00, 95% CI: −9.47, −0.53, p = 0.03), but not in those earning less. Age, sex, and household income did not moderate any other associations. |
| Miller (2017) [86] | Gender and parental monitoring as potential moderators | The effect of youth-perceived neighbourhood danger at Time 1 on OT at Time 2 was moderated by both gender (coefficient = −0.0718, SE = 0.1392, t = −0.5157) and parental monitoring at Time 1 (coefficient = −0.0157, SE = 0.0195, t = −0.8077). The effect of youth-perceived neighbourhood support at Time 1 on OT at Time 2 was also moderated by parental monitoring (coefficient = −0.1153, SE = 0.1130, t = −1.0200) and gender (coefficient = −0.9064, SE = 0.8646, t = −1.0484). The author reported that “youth with lower levels of parental monitoring perceived their neighbourhood to be more supportive and spent more time outside. In contrast, youth with high parental monitoring, who perceived their neighbourhood to be more dangerous, spent less time outside”. The author did not clearly discuss the moderating effect of gender. |
| Remmers (2014a) [70] | Perceived responsibility regarding child PA as potential moderator | Perceived responsibility moderated the effect of perceived functionality on OP (Table 3). When stratified, functionality was related to more OP in children of parents with high perceived responsibility (β = 0.04; 95% CI = −0.07, 0.15), while among parents with low responsibility, functionality was related to less OP (β = −0.03; 95% C = −0.09, 0.04). Traffic safety interacted with perceived responsibility, but this effect was only significant after adjustment for main effects (Model 3) and became non-significant after adjustment for the other interaction (Model 4). Stratification showed that the association between traffic safety and OP was marginally stronger when parents perceived high (β = 0.10; 95% CI = −0.03, 0.23) vs. low responsibility (β = 0.06; 95% CI = −0.003, 0.12). |
| Schneor (2021) [74] | Full vs. partial COVID-19 lockdown as potential moderator | A larger reduction in OT was observed with a full lockdown vs. a partial lockdown (−93 vs. −30 min/day; p = 0.008). |
| Shah (2017) [46] | Age as potential moderator | Age moderated the association between future risk of myopia and OT (p = 0.002), such that, before the age of 4, there was little difference in OT between children who later became myopic and those who remained non-myopic. Between the ages of 4 and 8.5 years, children who later became myopic spent progressively less time outdoors than their peers who remained non-myopic (0.1 SD unit per day difference in OT by age 8.5 years). |
| van Grieken (2014) [77] | Sex as potential moderator | The interaction between sex and group was significant (p = 0.019). Males in the intervention group had a change in OP of −13.99 min/day (95% CI: −46.11, 18.13) vs. 31.65 min/day for females (95% CI: 4.32, 58.98). |
| Van Stralen (2012) [78] | This study investigated several hypothesized personal and environmental mediators, which included perceived pros and cons, social pressure, social support, social modelling, self-efficacy, planning skills, perceived barriers, enjoyment, and habit strength related to OP. | No statistically significant intervention effects on potential mediators were seen at Time 2; thus, criteria for mediation were not satisfied. |
| Watowicz (2012) [87] | Length of time since parental weight loss surgery as potential moderator | There were no differences in reported lifestyle behaviours (including OP) in an analysis of the subset of subjects (n = 33) for whom length of time since surgery was available (by Watowicz et al.). |
| Xu (2016) [49] | Time as a potential moderator of sleep patterns (bedtime, sleep duration, sleep latency, sleep > 10 h/day, and waking at night) | Interactions were excluded from the final model, as they were not statistically significant (p > 0.05). |
Note: OP: outdoor play; OT: outdoor time; PA: physical activity.
Table 5.
Summary of the quality assessment using the Effective Public Health Practice Project Tool [25].
| Lead Author (Year) | Selection Bias | Study Design | Confounders | Blinding | Data Collection Tools | Withdrawals | Summary Rating |
|---|---|---|---|---|---|---|---|
| Arcury (2017) [34] | Moderate | Moderate | Moderate | N/A | Weak | Strong | Moderate |
| Avol (1998) [50] | Weak | Moderate | Moderate | N/A | Weak | Strong | Weak |
| Bacha (2010) [51] | Moderate | Moderate | Strong | N/A | Weak | Moderate | Moderate |
| Bagordo (2017) [52] | Weak | Moderate | Moderate | N/A | Weak | Moderate | Weak |
| Buller (2020) [53] | Weak | Strong | Weak | Weak | Weak | Strong | Weak |
| Cameron (2019) [35] | Weak | Moderate | Moderate | N/A | Weak | Moderate | Weak |
| Christiana (2017) [54] | Moderate | Moderate | Weak | Weak | Weak | Strong | Weak |
| Cleland (2008) [55] | Weak | Moderate | Strong | N/A | Strong | Weak | Weak |
| Cleland (2010) [56] | Weak | Moderate | Strong | N/A | Strong | Weak | Weak |
| Cortinez-O’Ryan (2017) [57] | Moderate | Strong | Weak | Weak | Strong | Strong | Weak |
| Davison (2011) [36] | Weak | Moderate | Moderate | Weak | Moderate | Moderate | Weak |
| Dunton (2007) [81] | Weak | Moderate | Weak | N/A | Moderate | Weak | Weak |
| Essery (2008) [37] | Weak | Strong | Strong | Weak | Weak | Strong | Weak |
| Evenson (2018) [82] | Weak | Moderate | Weak | N/A | Strong | Strong | Weak |
| Flynn (2017) [58] | Weak | Moderate | Weak | Weak | Weak | Weak | Weak |
| Ford (2002) [59] | Weak | Strong | Strong | Weak | Weak | Strong | Weak |
| French (2013) [83] | Moderate | Moderate | Moderate | N/A | Weak | Weak | Weak |
| Gerards (2015) [60] | Moderate | Strong | Strong | Weak | Weak | Moderate | Weak |
| Gopinath (2013) [84] | Moderate | Moderate | Strong | Weak | Weak | Moderate | Weak |
| Händel (2017) [38] | Weak | Strong | Strong | Weak | Weak | Weak | Weak |
| Handy (2008) [61] | Weak | Moderate | Moderate | N/A | Weak | Moderate | Weak |
| He (2015) [12] | Strong | Strong | Moderate | Weak | Weak | Strong | Weak |
| Hesketh (2015) [39] | Strong | Strong | Weak | Weak | Weak | Strong | Weak |
| Hnatiuk (2013) [40] | Moderate | Moderate | Weak | N/A | Weak | Moderate | Weak |
| Honda-Barros (2019) [41] | Strong | Moderate | Strong | N/A | Weak | Moderate | Moderate |
| Huang (2021) [42] | Moderate | Moderate | Strong | N/A | Weak | Moderate | Moderate |
| Kemp (2022) [62] | Moderate | Moderate | Weak | N/A | Weak | Strong | Weak |
| Li (2021) [63] | Weak | Moderate | Strong | N/A | Weak | Weak | Weak |
| Li (2022) [43] | Moderate | Moderate | Strong | N/A | Weak | Weak | Weak |
| Lin (2017) [85] | Weak | Moderate | Moderate | N/A | Weak | Moderate | Weak |
| Lumeng (2017) [44] | Moderate | Strong | Strong | Weak | Moderate | Strong | Moderate |
| Miller (2017) [86] | Weak | Moderate | Weak | N/A | Weak | Strong | Weak |
| Milne (2000) [64] | Strong | Strong | Moderate | Weak | Weak | Strong | Weak |
| Milne (2007) [65] | Moderate | Strong | Moderate | Weak | Weak | Moderate | Weak |
| Nigg (2021) [66] | Moderate | Moderate | Weak | N/A | Weak | Weak | Weak |
| Ngo (2009) [67] | Weak | Strong | Strong | Weak | Moderate | Strong | Weak |
| Nordvall-Lassen (2018) [68] | Moderate | Moderate | Strong | N/A | Weak | Moderate | Moderate |
| Ostrin (2018) [69] | Weak | Moderate | Weak | N/A | Strong | Strong | Weak |
| Remmers (2014a) [70] | Moderate | Moderate | Strong | N/A | Weak | Strong | Moderate |
| Remmers (2014b) [71] | Weak | Moderate | Strong | N/A | Weak | Weak | Weak |
| Sääkslahti (2004) [45] | Moderate | Strong | Weak | Weak | Weak | Moderate | Weak |
| Sadeh-Sharvit (2020) [72] | Weak | Moderate | Weak | N/A | Moderate | Moderate | Weak |
| Sanchez-Tocino (2019) [73] | Weak | Moderate | Moderate | N/A | Weak | Moderate | Weak |
| Schneor (2021) [74] | Weak | Moderate | Weak | N/A | Strong | Moderate | Weak |
| Shah (2017) [46] | Moderate | Moderate | Moderate | N/A | Weak | Weak | Weak |
| Shepherd-Baniga (2014) [75] | Weak | Moderate | Weak | N/A | Weak | Strong | Weak |
| Sum (2022) [76] | Weak | Moderate | Weak | N/A | Weak | Weak | Weak |
| Tandon (2019) [47] | Weak | Strong | Moderate | Weak | Weak | Strong | Weak |
| Thiering (2016) [48] | Moderate | Moderate | Moderate | N/A | Weak | Weak | Weak |
| Van Griecken (2014) [77] | Weak | Strong | Moderate | Strong | Weak | Weak | Weak |
| Van Stralen (2012) [78] | Moderate | Strong | Strong | Strong | Weak | Strong | Moderate |
| Walker (2021) [79] | Weak | Moderate | Weak | N/A | Weak | Strong | Weak |
| Watowicz (2012) [87] | Moderate | Moderate | Moderate | N/A | Weak | Moderate | Moderate |
| Wolters (2022) [80] | Weak | Moderate | Weak | N/A | Weak | Strong | Weak |
| Xu (2016) [49] | Weak | Moderate | Moderate | N/A | Moderate | Weak | Weak |
Note: Blinding was rated as non-applicable (N/A) for observational studies given the absence of intervention.
4. Discussion
Our systematic review summarized previous longitudinal and intervention studies examining the determinants of OT in children and youth. Overall, 119 determinants spanning the social-ecological model were examined across the 55 included studies (including 35 observational and 20 intervention studies). Illustrating the rapid growth in this field of research, the largest and most recent previous review on this topic included only 12 longitudinal studies [21]. Although we found that few potential determinants were included in a sufficient number of studies to draw conclusions about the consistency of associations, we identified some consistent positive or negative determinants of OT at multiple levels of influence.
4.1. Individual Level
About half of the included studies found that boys accumulated more OT than girls, with other studies reporting no gender differences. When examining findings by age group, all three cohorts that began in adolescence found that boys spent more time outdoors than girls. In the broader literature on correlates of PA, boys are usually more active than girls [8,22], with longitudinal studies suggesting that the age-related decline in PA tends to begin earlier in girls [89]. Hence, additional efforts may be needed to promote OT among girls. In our review, five studies examined sex or gender as potential moderators, and two found significant interactions. Notably, the intervention by van Grieken et al. [77] achieved a substantial increase in females’ (but not in males’) OT. Our findings suggest that the determinants of OT may vary according to sex and gender, and a better understanding of such differences could help guide future interventions.
Like the previous review by Lee et al. [21], we initially found mixed associations between age and OT. However, when considering the direction of age-related changes in OT by age group, we noted that increases were only reported in studies beginning in early childhood (≤5 years old), whereas decreases were common among older cohorts. These observations suggest that the relationship between age and OT may be curvilinear. If confirmed by future research, this would suggest a need for interventions to promote sustained engagement in outdoor activities in an effort to minimize the well-known age-related decline in PA [8,22,89] and increase in myopia prevalence [12]. In addition to promoting OT, interventions with youth may need to address important barriers to outdoor activities. For example, a large Canadian mixed-methods study indicated that the addictive nature of electronic screen devices and the belief that being indoors is safer and more comfortable were key factors associated with reduced connection to nature [90]. Echoing these findings, a quantitative study with Ecuadorian children found that connection to nature was negatively associated with screen time [91]. Conversely, connection to nature and OT are both associated with PA [5,6,7,8,91], suggesting that increasing outdoor activities could improve individual health [1,2] while helping to address the United Nations’ Sustainable Development Goals [17,92].
All three studies that examined the association between OT at baseline and subsequent OT found positive associations. These findings are consistent with previous research in the fields of PA epidemiology and health psychology, showing that past behaviour is an important determinant of current behaviour [93,94,95,96]. In this regard, our findings suggest that promoting OT may yield lasting benefits, though intervention studies are needed to test this hypothesis.
4.2. Interpersonal Level
The important role of parents in supporting their child’s PA is well established [97,98]. In our review, different aspects of parental influence (e.g., encouragement, co-participation, attitude, and intention) were examined as potential determinants of OT in no more than two studies, precluding strong conclusions. Yet, we found preliminary evidence that parent participation in PA/OP [41,69] and parental habit strength to increase OP [70] were associated with higher OT among primary school children. Ostrin et al. [69] notably reported a strong correlation within child–parent dyads in device-measured outdoor light exposure (i.e., lux) (r = 0.76). These findings are consistent with previous research showing consistent positive correlations in PA within parent–child dyads—especially in studies using device-based measures of PA [98].
In general, we found insufficient or inconclusive evidence regarding the associations between parental socio-demographic variables (e.g., education, income, occupation, and ethnicity) and OT (Table 3). Mostly relying on cross-sectional findings, previous reviews concluded that children from ethnic minorities and more educated parents played outside less [19,21]. It is also important to bear in mind that, in line with social-ecological theory [22], parental socio-demographic variables may interact with other levels of influence. Such interactions were not investigated in previous reviews, and we found only one study that examined income as a potential moderator [63]. Hence, more research is needed to unpack the potential role(s) of socio-demographic variables in influencing OT, as this may help in tailoring interventions to different groups.
Extending previous reviews, we were able to include 20 intervention studies. We found that all three interventions that included sessions with parents augmented by additional resources to promote outdoor activities (e.g., specific advice and community guide) were associated with higher OT [36,45,58]. While promising, two of these studies did not include a control group [36,58], and thus, further research is needed to confirm these findings.
Within the realm of interpersonal influences, nature/outdoor PA prescriptions from pediatricians and other health professionals, such as the US National ParkRx Initiative (https://www.parkrx.org/, accessed on 7 December 2022) and the Canadian PaRx (https://www.parkprescriptions.ca/, accessed on 7 December 2022), are gaining popularity to address physical inactivity and excessive screen time [88]. One outdoor PA prescription intervention met our inclusion criteria, but it was limited by a small sample size, seasonal changes, and a crude outcome measure [54]. Conversely, pilot studies from Kondo and colleagues’ [88] narrative review of nature prescription programs found positive intervention effects on the park visit frequency [99,100] but did not measure OT per se. Notwithstanding the potential benefits of park prescriptions, the currently insufficient evidence of effectiveness represents a barrier for healthcare providers to dedicate their limited time [88]. This underscores a need for larger outdoor activity prescription interventions using stronger study designs and measures.
4.3. Community Level
In contrast, school-based sun safety interventions that discouraged OT during midday were generally associated with lower OT [53,65]. Well-intended public health campaigns focusing on different issues have collectively recommended keeping children indoors for most of the day to avoid (1) sun exposure between 10:00 am and 4:00 pm to prevent skin melanoma; (2) ozone exposure, which tends to be highest in commuting periods immediately before and after school; and (3) exposure to insect-borne diseases from dusk to dawn [7]. Notwithstanding these issues, researchers have called for a better balance between risks and benefits and identified often overlooked risks associated with being indoors, including physical inactivity, excess screen time, an increased risk of myopia, exposure to an obesogenic food environment, indoor air pollution, allergens, and cyberpredators [7,14]. Parents, educators, pediatricians, and other health professionals could play an important role in reframing perceptions of risks associated with OT [14,101].
4.4. Natural Environment Level
We found that children consistently spent more time outside during the warmer months. These findings are consistent with previous reviews on PA and OT [21,102]. While seasonal variations cannot be modified in the short term, interventions could be developed to promote outdoor activities in colder seasons with appropriate clothing. Such interventions may be particularly useful for new or recent immigrants who may be at higher risk of physical inactivity [103].
4.5. Policy Level
Only four studies examined policy-level determinants, but all of them found significant associations with OT. Cortinez-O’Ryan et al. [57] found that an evening street closure intervention occurring twice a week for 12 weeks was associated with significant increases in measures of frequency and duration of OP. In contrast, all three studies that examined the effect of COVID-19 restrictions found a significant decrease in OT. Furthermore, in a small sample of Israeli boys, Schneor et al. [74] reported that the effect of a full lockdown was greater than that of a partial lockdown and that device-measured OT returned to pre-pandemic levels after restrictions were removed. Our findings are consistent with reviews that reported large decreases in PA and increases in screen time during the pandemic [9,104]. Given the potential of PA to reduce the risk and severity of COVID-19 infections [105] and the lower risk of transmission in outdoor environments, more efforts should be invested in promoting OT and PA during future pandemics.
4.6. Limitations of Included Studies
Based on the EPHPP tool, quality was rated as “weak” for most included studies. It is worth noting that some components of the EPHPP are rated quite severely [27,30]. For example, the withdrawals component is rated as “weak” whenever attrition exceeds 40%, regardless of the follow-up duration. Similarly, a participation rate below 60% is considered “weak” for the selection bias component, regardless of the complexity and/or length of the study. The blinding of participants was impossible or impractical in most intervention studies. Hence, the summary quality ratings should be interpreted with caution. That said, given the large number of “weak” ratings for data collection tools, future studies should use measures of OT that have been shown to be reliable and valid. In our review, most studies used child or parent reports and did not provide information about the psychometric properties of their measures. Some studies also appeared underpowered to examine determinants of OT. Finally, most of the studies were conducted in high-income countries, so the transferability of the findings to lower- and middle-income countries is unclear.
4.7. Strengths and Limitations of the Review
The strengths of the review include the focus on longitudinal studies that can establish a temporal sequence, the consideration of the entire pediatric population, and the robust screening and quality assessment process. Furthermore, we were able to consider articles published in English, French, Japanese, and Spanish, although we may still have missed articles published in other languages. Given that most potential determinants have been examined in only one or two studies, we could not conduct the planned analysis of determinants stratified by gender and age group. Similarly, the heterogeneity of the exposure and outcome measures among the included studies precluded meta-analyses. Future studies examining the same potential determinants are needed to draw stronger conclusions. We also noted that OT was measured in a variety of ways, with some studies focusing only on OP, others on outdoor PA, and others on all activities that took place outdoors (Table 1 and Table 2). Standard definitions of terms related to OT and play have recently been proposed [18], and their uptake in future studies could help minimize methodological heterogeneity.
5. Conclusions
Previous studies have examined 119 potential determinants of OT representing multiple levels of influence of the social-ecological model, but few determinants have been examined frequently enough to draw strong conclusions. Nevertheless, we found consistent evidence that children spend more time outdoors in warmer seasons, that OT at baseline predicted subsequent OT, and that COVID-19 restrictions and sun safety interventions discouraging midday outdoor activities were associated with less OT. The association between age and OT appears to be curvilinear, with most increases reported in early childhood, followed by decreases in late childhood and adolescence. About half of studies examining gender differences reported that boys spent more time outdoors (especially in adolescence), and the remainder found no differences. Interventions that include both parent sessions and additional resources to promote OT seem promising, but more robust research is needed to confirm their effectiveness. Given that most included studies were rated as “weak”, there remains a need for stronger studies to improve the quality of evidence. Longitudinal studies investigating the determinants of OT among underrepresented populations, notably adolescents and children and youth living in low- and middle-income countries, are also needed. Finally, future studies should consider using both subjective and device-based measures of OT, such as accelerometers and other devices equipped with light sensors that can reduce social desirability and recall biases associated with subjective measures [69,74,106].
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph20021328/s1, File S1: PRISMA checklist; File S2: Systematic review search terms.
Author Contributions
Conceptualization, R.L.; methodology, R.L. and D.R.S.; software, R.L. and D.R.S.; validation, R.L., M.K., U.C.R., V.H., C.H., L.M.B., O.K.O., F.S. and H.S.; formal analysis, R.L.; investigation, R.L., M.K., U.C.R., V.H., C.H., L.M.B., O.K.O., F.S. and H.S.; data curation, R.L.; writing—original draft preparation, R.L.; writing—review and editing, R.L., M.K., U.C.R., V.H., C.H., D.R.S., L.M.B., O.K.O., F.S. and H.S.; supervision, R.L.; project administration, R.L.; funding acquisition, R.L. and L.M.B. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Template data collection forms can be requested via email to R.L.
Conflicts of Interest
R.L. is a Board Member of Outdoor Play Canada and a founding member of the Play, Learn, and Teach Outdoors Network (PLaTO-Net) but receives no payment for these roles. Other authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Funding Statement
This research was funded by the University of Lethbridge via start-up research funds held by R.L., Graduate Assistantships from the University of Lethbridge’s School of Graduate Studies and an Alberta Innovates Summer Studentship award held by L.M.B.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Carson V., Lee E.Y., Hewitt L., Jennings C., Hunter S., Kuzik N., Stearns J.A., Powley Unrau S., Poitras V.J., Gray C., et al. Systematic review of the relationships between physical activity and health indicators in the early years (0–4 years) BMC Public Health. 2017;17((Suppl. S5)):854. doi: 10.1186/s12889-017-4860-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Poitras V.J., Gray C.E., Borghese M.M., Chaput J.-P., Janssen I., Katzmarzyk P.T., Pate R.R., Connor Gorber S., Kho M.E., Sampson M., et al. Systematic review of the relationships between objectively measured physical activity and health indicators in school-aged children and youth. Appl. Physiol. Nutr. Metabol. 2016;41:S197–S239. doi: 10.1139/apnm-2015-0663. [DOI] [PubMed] [Google Scholar]
- 3.Aubert S., Barnes J.D., Abdeta C., Abi Nader P., Adeniyi A.F., Aguilar-Farias N., Andrade Tenesaca D.S., Bhawra J., Brazo-Sayavera J., Cardon G., et al. Global matrix 3.0 physical activity report card grades for children and youth: Results and analysis from 49 countries. J. Phys. Act. Health. 2018;15((Suppl. S2)):S251–S273. doi: 10.1123/jpah.2018-0472. [DOI] [PubMed] [Google Scholar]
- 4.Guthold R., Stevens G.A., Riley L.M., Bull F.C. Global trends in insufficient physical activity among adolescents: A pooled analysis of 298 population-based surveys with 1·6 million participants. Lancet Child Adolesc. Health. 2020;4:23–35. doi: 10.1016/S2352-4642(19)30323-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Biddle S.J., Atkin A.J., Cavill N., Foster C. Correlates of physical activity in youth: A review of quantitative systematic reviews. Int. Rev. Sport Exerc. Psychol. 2011;4:25–49. doi: 10.1080/1750984X.2010.548528. [DOI] [Google Scholar]
- 6.Ferreira I., Van Der Horst K., Wendel-Vos W., Kremers S., Van Lenthe F.J., Brug J. Environmental correlates of physical activity in youth–a review and update. Obes. Rev. 2007;8:129–154. doi: 10.1111/j.1467-789X.2006.00264.x. [DOI] [PubMed] [Google Scholar]
- 7.Sallis J.F., Prochaska J.J., Taylor W.C. A review of correlates of physical activity of children and adolescents. Med. Sci. Sport. Exerc. 2000;32:963–975. doi: 10.1097/00005768-200005000-00014. [DOI] [PubMed] [Google Scholar]
- 8.Gray C., Gibbons R., Larouche R., Sandseter E.B.H., Bienenstock A., Brussoni M., Chabot G., Herrington S., Janssen I., Pickett W., et al. What is the relationship between outdoor time and physical activity, sedentary behaviour, and physical fitness in children? A systematic review. Int. J. Environ. Res. Public Health. 2015;12:6455–6474. doi: 10.3390/ijerph120606455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bassett D.R., John D., Conger S.A., Fitzhugh E.C., Coe D.P. Trends in physical activity and sedentary behaviors of United States youth. J. Phys. Act. Health. 2015;12:1102–1111. doi: 10.1123/jpah.2014-0050. [DOI] [PubMed] [Google Scholar]
- 10.Clements R. An investigation of the status of outdoor play. Contemp. Issues Early Child. 2004;5:68–80. doi: 10.2304/ciec.2004.5.1.10. [DOI] [Google Scholar]
- 11.Paterson D.C., Ramage K., Moore S.A., Riazi N., Tremblay M.S., Faulkner G. Exploring the impact of COVID-19 on the movement behaviors of children and youth: A scoping review of evidence after the first year. J. Sport Health Sci. 2021;10:675–689. doi: 10.1016/j.jshs.2021.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.He M., Xiang F., Zeng Y., Mai J., Chen Q., Zhang J., Smith W., Rose K., Morgan I.G. Effect of time spent outdoors at school on the development of myopia among children in China: A randomized clinical trial. JAMA. 2015;314:1142–1148. doi: 10.1001/jama.2015.10803. [DOI] [PubMed] [Google Scholar]
- 13.Larouche R., Garriguet D., Gunnell K.E., Goldfield G.S., Tremblay M.S. Outdoor time, physical activity, sedentary time, and health indicators at ages 7 to 14: 2012/2013 Canadian Health Measures Survey. Health Reps. 2016;27:3–13. [PubMed] [Google Scholar]
- 14.Tremblay M.S., Gray C., Babcock S., Barnes J., Costas Bradstreet C., Carr D., Chabot G., Choquette L., Chorney D., Collyer C., et al. Position statement on active outdoor play. Int. J. Environ. Res. Public Health. 2015;12:6475–6505. doi: 10.3390/ijerph120606475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Faber Taylor A., Kuo F.E. Children with attention deficits concentrate better after walk in the park. J. Atten. Disord. 2009;12:402–409. doi: 10.1177/1087054708323000. [DOI] [PubMed] [Google Scholar]
- 16.Kuo F.E., Faber Taylor A. A potential natural treatment for attention-deficit/hyperactivity disorder: Evidence from a national study. Am. J. Public Health. 2004;94:1580–1586. doi: 10.2105/AJPH.94.9.1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Otto S., Pensini P. Nature-based environmental education of children: Environmental knowledge and connectedness to nature, together, are related to ecological behaviour. Glob. Environ. Chang. 2017;47:88–94. doi: 10.1016/j.gloenvcha.2017.09.009. [DOI] [Google Scholar]
- 18.Lee E.Y., De Lannoy L., Li L., De Barros M.I.A., Bentsen P., Brussoni M., Fiskum T.A., Guerrero M., Hallås B.O., Ho S., et al. Play, learn, and teach outdoors—Network (PLaTO-Net): Terminology, taxonomy, and ontology. Int. J. Behav. Nutr. Phys. Act. 2022;19:66. doi: 10.1186/s12966-022-01294-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Boxberger K., Reimers A.K. Parental correlates of outdoor play in boys and girls aged 0 to 12—A systematic review. Int. J. Environ. Res. Public Health. 2019;16:190. doi: 10.3390/ijerph16020190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lambert A., Vlaar J., Herrington S., Brussoni M. What is the relationship between the neighbourhood built environment and time spent in outdoor play? A systematic review. Int. J. Environ. Res. Public Health. 2019;16:3840. doi: 10.3390/ijerph16203840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee E.Y., Bains A., Hunter S., Ament A., Brazo-Sayavera J., Carson V., Hakimi S., Huang W.Y., Janssen I., Lee M., et al. Systematic review of the correlates of outdoor play and time among children aged 3-12 years. Int. J. Behav. Nutr. Phys. Act. 2021;18:41. doi: 10.1186/s12966-021-01097-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bauman A.E., Reis R.S., Sallis J.F., Wells J.C., Loos R.J., Martin B.W., Lancet Physical Activity Series Working Group Correlates of physical activity: Why are some people physically active and others not? Lancet. 2012;380:258–271. doi: 10.1016/S0140-6736(12)60735-1. [DOI] [PubMed] [Google Scholar]
- 23.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Telzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kido A., Masahiro M., Watanabe M. Interventions to increase time spent outdoors for preventing incidence and progression of myopia in children. Cochrane Database Syst. Rev. 2020;20:CD013549. doi: 10.1002/14651858.CD013549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vinceti M., Filippini T., Del Giovane C., Dennert G., Zwahlen M., Brinkman M., Zeegers M.P.A., Horneber M., D’Amico R., Crespi C.M. Selenium for preventing cancer (review) Cochrane Database Syst. Rev. 2018;1:CD005195. doi: 10.1002/14651858.CD005195.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wilczynski N.L., McKibbon K.A., Haynes R.B. Response to Glanville et al.: How to identify randomized controlled trials in MEDLINE: Ten years on. J. Med. Libr. Assoc. 2007;95:117–118. doi: 10.3163/1536-5050.95.2.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thomas B.H., Ciliska D., Dobbins M., Micucci S. A process for systematically reviewing the literature: Providing the research evidence for public health nursing interventions. Worldviews Evid. Based Nurs. 2004;1:176–184. doi: 10.1111/j.1524-475X.2004.04006.x. [DOI] [PubMed] [Google Scholar]
- 28.Chillón P., Evenson K.R., Vaughn A., Ward D.S. A systematic review of interventions for promoting active transportation to school. Int. J. Behav. Nutr. Phys. Act. 2011;8:10. doi: 10.1186/1479-5868-8-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dietz P., Watson E.D., Sattler M.C., Ruf W., Titze S., van Poppel M. The influence of physical activity during pregnancy on maternal, fetal or infant heart rate variability: A systematic review. BMC Pregnancy Childbirth. 2016;16:326. doi: 10.1186/s12884-016-1121-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Larouche R., Mammen G., Rowe D.A., Faulkner G. Effectiveness of active school transport interventions: A systematic review and update. BMC Public Health. 2018;18:206. doi: 10.1186/s12889-017-5005-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Oja P., Titze S., Bauman A., De Geus B., Krenn P., Reger-Nash B., Kohlberger T. Health benefits of cycling: A systematic review. Scand. J. Med. Sci. Sport. 2011;21:496–509. doi: 10.1111/j.1600-0838.2011.01299.x. [DOI] [PubMed] [Google Scholar]
- 32.D’Haese S., Vanwolleghem G., Hinckson E., De Bourdeaudhuij I., Deforche B., Van Dyck D., Cardon G. Cross-continental comparison of the association between the physical environment and active transportation in children: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2015;12:145. doi: 10.1186/s12966-015-0308-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ding D., Sallis J.F., Kerr J., Lee S., Rosenberg D.E. Neighborhood environment and physical activity among youth: A review. Am. J. Prev. Med. 2011;41:442–455. doi: 10.1016/j.amepre.2011.06.036. [DOI] [PubMed] [Google Scholar]
- 34.Arcury T.A., Suerken C.K., Ip E.H., Moore J.B., Quandt S.A. Residential environment for outdoor play among children in Latino farmworker families. J. Immigr. Minor. Health. 2017;19:267–274. doi: 10.1007/s10903-016-0473-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cameron A.J., Charlton E., Walsh A., Hesketh K., Campbell K. The influence of the maternal peer group (partner, friends, mothers’ group, family) on mothers’ attitudes to obesity-related behaviours of their children. BMC Pediatr. 2019;19:357. doi: 10.1186/s12887-019-1726-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Davison K.K., Edmunds L.S., Wyker B.A., Young L.M., Sarfoh V.S., Sekhobo J.P. Feasibility of increasing childhood outdoor play and decreasing television viewing through a family-based intervention in WIC, New York State, 2007–2008. Prev. Chron. Dis. 2011;8:A54. [PMC free article] [PubMed] [Google Scholar]
- 37.Essery E.V., DiMarco N.M., Rich S.S., Nichols D.L. Mothers of preschoolers report using less pressure in child feeding situations following a newsletter intervention. J. Nutr. Educ. Behav. 2008;40:110–115. doi: 10.1016/j.jneb.2007.02.008. [DOI] [PubMed] [Google Scholar]
- 38.Händel M.N., Larsen S.C., Rohde J.F., Stougaard M., Olsen N.J., Heitmann B.L. Effects of the Healthy Start randomized intervention trial on physical activity among normal weight preschool children predisposed to overweight and obesity. PLoS ONE. 2017;12:e0185266. doi: 10.1371/journal.pone.0185266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hesketh K.D., Crawford D.A., Abbott G., Campbell K.J., Salmon J. Prevalence and stability of active play, restricted movement and television viewing in infants. Early Child Dev. Care. 2015;185:883–894. doi: 10.1080/03004430.2014.963066. [DOI] [Google Scholar]
- 40.Hnatiuk J., Salmon J., Campbell K.J., Ridgers N.D., Hesketh K.D. Early childhood predictors of toddlers’ physical activity: Longitudinal findings from the Melbourne InFANT Program. Int. J. Behav. Nutr. Phys. Act. 2013;10:123. doi: 10.1186/1479-5868-10-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Honda Barros S.S., Nahas M.V., Menêses Hardman C., Bezerra J., Gomes de Barros M.V. Longitudinal follow-up of physical activity from preschool to school age: The ELOS-Pré study. Rev. Bras. Cineantropometria Desempenho Hum. 2019;21:e59242. doi: 10.1590/1980-0037.2019v21e59242. [DOI] [Google Scholar]
- 42.Huang L., Schmid K.L., Yin X.N., Zhang J., Wu J., Yang G., Ruan Z.-L., Jiang X.-Q., Wu C.-A., Chen W.Q. Combination effect of outdoor activity and screen exposure on risk of preschool myopia: Findings from Longhua Child Cohort Study. Front. Public Health. 2021;9:607911. doi: 10.3389/fpubh.2021.607911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Li C., Cheng G., He S., Xie X., Tian G., Jiang N., Min X., Shi Y., Li R., Zhou T., et al. Prevalence, correlates, and trajectory of screen viewing among Chinese children in Changsha: A birth cohort study. BMC Public Health. 2022;22:1170. doi: 10.1186/s12889-022-13268-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lumeng J.C., Miller A.L., Horodynski M.A., Brophy-Herb H.E., Contreras D., Lee H., Sturza J., Kaciroti N., Peterson K.E. Improving self-regulation for obesity prevention in head start: A randomized controlled trial. Pediatrics. 2017;139:e20162047. doi: 10.1542/peds.2016-2047. [DOI] [PubMed] [Google Scholar]
- 45.Sääkslahti A., Numminen P., Salo P., Tuominen J., Helenius H., Välimäki I. Effects of a three-year intervention on children’s physical activity from age 4 to 7. Pediatr. Exerc. Sci. 2004;16:167–180. doi: 10.1123/pes.16.2.167. [DOI] [Google Scholar]
- 46.Shah R.L., Huang Y., Guggenheim J.A., Williams C. Time outdoors at specific ages during early childhood and the risk of incident myopia. Investig. Ophthalmol. Vis. Sci. 2017;58:1158–1166. doi: 10.1167/iovs.16-20894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tandon P.S., Downing K.L., Saelens B.E., Christakis D.A. Two approaches to increase physical activity for preschool children in child care centers: A matched-pair cluster-randomized trial. Int. J. Environ. Res. Public Health. 2019;16:4020. doi: 10.3390/ijerph16204020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Thiering E., Markevych I., Brüske I., Fuertes E., Kratzsch J., Sugiri D., Hoffmann B., von Berg A., Bauer C.-P., Koletzko S., et al. Associations of residential long-term air pollution exposures and satellite-derived greenness with insulin resistance in German adolescents. Environ. Health Perspect. 2016;124:1291–1298. doi: 10.1289/ehp.1509967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Xu H., Wen L.M., Hardy L.L., Rissel C. A 5-year longitudinal analysis of modifiable predictors for outdoor play and screen-time of 2- to 5-year-olds. Int. J. Behav. Nutr. Phys. Act. 2016;13:96. doi: 10.1186/s12966-016-0422-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Avol E.L., Navidi W.C., Rappaport E.B., Peters J.M. Acute effects of ambient ozone on asthmatic, wheezy, and healthy children. Res. Rep. Health Eff. Inst. 1998;82:1–30. [PubMed] [Google Scholar]
- 51.Bacha J.M., Appugliese D., Coleman S., Kaciroti N., Bradley R.H., Corwyn R.F., Lumeng J.C. Maternal perception of neighborhood safety as a predictor of child weight status: The moderating effect of gender and assessment of potential mediators. Int. J. Pediatr. Obes. 2010;5:72–79. doi: 10.3109/17477160903055911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bagordo F., De Donno A., Grassi T., Guido M., Devoti G., Ceretti E., Zani C., Feretti D., Villarini M., Moretti M., et al. Lifestyles and socio-cultural factors among children aged 6-8 years from five Italian towns: The MAPEC_LIFE study cohort. BMC Public Health. 2017;17:233. doi: 10.1186/s12889-017-4142-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Buller D.B., Reynolds K.D., Buller M.K. Parent reports of sun safety communication and behaviour for students in a randomised trial on a school policy implementation intervention. Aust. N. Z. J. Public Health. 2020;44:208–214. doi: 10.1111/1753-6405.12987. [DOI] [PubMed] [Google Scholar]
- 54.Christiana R.W., Battista R.A., James J.J., Bergman S.M. Pediatrician prescriptions for outdoor physical activity among children: A pilot study. Prev. Med. Rep. 2017;5:100–105. doi: 10.1016/j.pmedr.2016.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cleland V., Crawford D., Baur L.A., Hume C., Timperio A., Salmon J. A prospective examination of children’s time spent outdoors, objectively measured physical activity and overweight. Int. J. Obes. 2008;32:1685–1693. doi: 10.1038/ijo.2008.171. [DOI] [PubMed] [Google Scholar]
- 56.Cleland V., Timperio A., Salmon J., Hume C., Baur L.A., Crawford D. Predictors of time spent outdoors among children: 5-year longitudinal findings. J. Epidemiol. Community Health. 2010;64:400–406. doi: 10.1136/jech.2009.087460. [DOI] [PubMed] [Google Scholar]
- 57.Cortinez-O’Ryan A., Albagli A., Sadarangani K.P., Aguilar-Farias N. Reclaiming streets for outdoor play: A process and impact evaluation of “Juega en tu Barrio” (Play in your Neighborhood), an intervention to increase physical activity and opportunities for play. PLoS ONE. 2017;12:e0180172. doi: 10.1371/journal.pone.0180172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Flynn J.I., Bassett D.R., Fouts H.N., Thompson D.L., Coe D.P. Active Families in the Great Outdoors: A program to promote family outdoor physical activity. J. Adventure Educ. Outdoor Learn. 2017;17:227–238. doi: 10.1080/14729679.2017.1291355. [DOI] [Google Scholar]
- 59.Ford B.S., McDonald T.E., Owens A.S., Robinson T.N. Primary care interventions to reduce television viewing in African-American children. Am. J. Prev. Med. 2002;22:106–109. doi: 10.1016/S0749-3797(01)00410-X. [DOI] [PubMed] [Google Scholar]
- 60.Gerards S.M.P.L., Dagnelie P.C., Gubbels J.S., Van Buuren S., Hamers F.J., Jansen M.W., van der Goot O.H.M., de Vries N.K., Sanders M.R., Kremers S.P.J. The effectiveness of lifestyle triple P in the Netherlands: A randomized controlled trial. PLoS ONE. 2015;10:e0122240. doi: 10.1371/journal.pone.0122240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Handy S., Cao X., Mokhtarian P. Neighborhood design and children’s outdoor play: Evidence from northern California. Child. Youth Environ. 2008;18:160–179. [Google Scholar]
- 62.Kemp B.J., Parrish A.M., Batterham M., Cliff D.P. Changes in subdomains of non-organized physical activity between childhood and adolescence in Australia: A longitudinal study. Int. J. Behav. Nutr. Phys. Act. 2022;19:73. doi: 10.1186/s12966-022-01311-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Li X., Vanderloo L.M., Maguire J.L., Keown-Stoneman C.D., Aglipay M., Anderson L.N., Tombeau Cost K., Charach C., Vanderhout S.M., Birken C.S., et al. Public health preventive measures and child health behaviours during COVID-19: A cohort study. Can. J. Public Health. 2021;112:831–842. doi: 10.17269/s41997-021-00549-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Milne E., Johnston R., Cross D., Borland R., Costa C., Giles-Corti B. Improved sun protection behaviour on children after two years of the Kidskin intervention. Aust. N. Z. J. Public Health. 2000;24:481–487. doi: 10.1111/j.1467-842X.2000.tb00497.x. [DOI] [PubMed] [Google Scholar]
- 65.Milne E., Simpson J.A., Johnston R., Giles-Corti B., English D.R. Time spent outdoors at midday and children’s body mass index. Am. J. Public Health. 2007;97:306–310. doi: 10.2105/AJPH.2005.080499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Nigg C., Niessner C., Nigg C.R., Oriwol D., Schmidt S.C., Woll A. Relating outdoor play to sedentary behavior and physical activity in youth—Results from a cohort study. BMC Public Health. 2021;21:1716. doi: 10.1186/s12889-021-11754-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ngo C., Pan C.W., Finkelstein E.A., Lee C.F., Wong I.B., Ong J., Ang M., Wong T.-Y., Saw S.M. A cluster randomised controlled trial evaluating an incentive-based outdoor physical activity programme to increase outdoor time and prevent myopia in children. Ophthal. Physiol. Opt. 2014;34:362–368. doi: 10.1111/opo.12112. [DOI] [PubMed] [Google Scholar]
- 68.Nordvall-Lassen M., Hegaard H.K., Obel C., Lindhard M.S., Hedegaard M., Henriksen T.B. Leisure time physical activity in 9- to 11-year-old children born moderately preterm: A cohort study. BMC Pediatr. 2018;18:163. doi: 10.1186/s12887-018-1141-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ostrin L.A., Sajjadi A., Benoit J.S. Objectively measured light exposure during school and summer in children. Optom. Vis. Sci. 2018;95:332–342. doi: 10.1097/OPX.0000000000001208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Remmers T., Van Kann D., Gubbels J., Schmidt S., de Vries S., Ettema D., Kremers S.P.J., Thijs C. Moderators of the longitudinal relationship between the perceived physical environment and outside play in children: The KOALA birth cohort study. Int. J. Behav. Nutr. Phys. Act. 2014;11:150. doi: 10.1186/s12966-014-0150-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Remmers T., Broeren S.M.L., Renders C.M., Hirasing R.A., van Grieken A., Raat H.A. Longitudinal study of children’s outside play using family environment and perceived physical environment as predictors. Int. J. Behav. Nutr. Phys. Act. 2014;11:76. doi: 10.1186/1479-5868-11-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sadeh-Sharvit S., Runfola C.D., Welch H.A., Gibbs E.L., Dickens C.E., Lock J., Safer D.L. Parent-based prevention after parental weight loss surgery: A pilot case-series trial. Surg. Obes. Relat. Dis. 2020;16:1321–1327. doi: 10.1016/j.soard.2020.05.016. [DOI] [PubMed] [Google Scholar]
- 73.Sanchez-Tocino H., Gómez A.V., Bolaños C.G., Alonso I.A., Alvarez A.V., Zamora M.G., Francés Caballero E., Marcos-Fernández M.A., Schellini S., Galindo-Ferreiro A. The effect of light and outdoor activity in natural lighting on the progression of myopia in children. J. Fr. Ophtalmol. 2019;42:2–10. doi: 10.1016/j.jfo.2018.05.008. [DOI] [PubMed] [Google Scholar]
- 74.Shneor E., Doron R., Levine J., Zimmerman D.R., Benoit J.S., Ostrin L.A., Gordon-Shaag A. Objective Behavioral Measures in Children before, during, and after the COVID-19 Lockdown in Israel. Int. J. Environ. Res. Public Health. 2021;18:8732. doi: 10.3390/ijerph18168732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Shepherd-Banigan M., Ulrich A., Thompson B. Macro-activity patterns of farmworker and non-farmworker children living in an agricultural community. Environ. Res. 2014;132:176–181. doi: 10.1016/j.envres.2014.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sum K.K., Cai S., Law E., Cheon B., Tan G., Loo E., Lee Y.S., Yap F., Chan J.K.Y., Daniel M., et al. COVID-19–related life experiences, outdoor play, and long-term adiposity changes among preschool-and school-aged children in Singapore 1 year after lockdown. JAMA Pediatr. 2022;176:280–289. doi: 10.1001/jamapediatrics.2021.5585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.van Grieken A., Renders C.M., Veldhuis L., Looman C.W., Hirasing R.A., Raat H. Promotion of a healthy lifestyle among 5-year-old overweight children: Health behavior outcomes of the ‘Be active, eat right’ study. BMC Public Health. 2014;14:59. doi: 10.1186/1471-2458-14-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.van Stralen M.M., de Meij J., te Velde S.J., Van der Wal M.F., Van Mechelen W., Knol D.L., Chinapaw M.J. Mediators of the effect of the JUMP-in intervention on physical activity and sedentary behavior in Dutch primary schoolchildren from disadvantaged neighborhoods. Int. J. Behav. Nutr. Phys. Act. 2012;9:131–142. doi: 10.1186/1479-5868-9-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Walker K. Ph.D. Dissertation. University of North Texas; Denton, TX, USA: 2021. Outdoor Child-Centered Play Therapy with Attention and Social-Emotional Competencies in Children. [Google Scholar]
- 80.Wolters M., Intemann T., Russo P., Moreno L.A., Molnár D., Veidebaum T., Tornaritis M., De Henauw S., Eiben G., Ahrens W., et al. 25-Hydroxyvitamin D reference percentiles and the role of their determinants among European children and adolescents. Eur. J. Clin. Nutr. 2022;76:564–573. doi: 10.1038/s41430-021-00985-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Dunton G.F., Whalen C.K., Jamner L.D., Floro J.N. Mapping the social and physical contexts of physical activity across adolescence using ecological momentary assessment. Ann. Behav. Med. 2007;34:144–153. doi: 10.1007/BF02872669. [DOI] [PubMed] [Google Scholar]
- 82.Evenson K.R., Cho G.-H., Rodríguez D.A., Cohen D.A. Park use and physical activity among adolescent girls at two time points. J. Sports Sci. 2018;36:2544–2550. doi: 10.1080/02640414.2018.1469225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.French A.N., Morgan I.G., Mitchell P., Rose K.A. Patterns of myopigenic activities with age, gender and ethnicity in Sydney schoolchildren. Ophthal. Physiol. Opt. 2013;33:318–328. doi: 10.1111/opo.12045. [DOI] [PubMed] [Google Scholar]
- 84.Gopinath B., Hardy L.L., Baur L.A., Burlutsky G., Mitchell P. Birth weight and time spent in outdoor physical activity during adolescence. Med. Sci. Sports Exerc. 2013;45:475–480. doi: 10.1249/MSS.0b013e3182752b95. [DOI] [PubMed] [Google Scholar]
- 85.Lin Z., Vasudevan B., Ciuffreda K.J., Zhou H.J., Mao G.Y., Wang N.L., Liang Y.B. Myopigenic activity change and its risk factors in urban students in Beijing: Three-year report of Beijing myopia progression study. Ophthal. Epidemiol. 2017;24:388–393. doi: 10.1080/09286586.2017.1307994. [DOI] [PubMed] [Google Scholar]
- 86.Miller K.M. Ph.D. Dissertation. Loyola University; Chicago, IL, USA: 2016. Examining Urban African American Adolescent Perceptions of Neighborhood and Time Spent in Risky Contexts: Cross-Sectionally and Longitudinally. [Google Scholar]
- 87.Watowicz R.P., Taylor C.A., Eneli I.U. Lifestyle behaviors of obese children following parental weight loss surgery. Obes. Surg. 2013;23:173–178. doi: 10.1007/s11695-012-0752-7. [DOI] [PubMed] [Google Scholar]
- 88.Kondo M.C., Oyekanmi K.O., Gibson A., South E.C., Bocarro J., Hipp J.A. Nature prescriptions for health: A review of evidence and research opportunities. Int. J. Environ. Res. Public Health. 2020;17:4213. doi: 10.3390/ijerph17124213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Dumith S.C., Gigante D.P., Domingues M.R., Kohl H.W., III Physical activity change during adolescence: A systematic review and a pooled analysis. Int. J. Epidemiol. 2011;40:685–698. doi: 10.1093/ije/dyq272. [DOI] [PubMed] [Google Scholar]
- 90.Michaelson V., King N., Janssen I., Lawal S., Pickett W. Electronic screen technology use and connection to nature in Canadian adolescents: A mixed methods study. Can. J. Public Health. 2020;111:502–514. doi: 10.17269/s41997-019-00289-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Molina-Cando M.J., Escandón S., Van Dyck D., Cardon G., Salvo D., Fiebelkorn F., Andrade S., Ochoa-Avilés C., García A., Brito J., et al. Nature relatedness as a potential factor to promote physical activity and reduce sedentary behavior in Ecuadorian children. PLoS ONE. 2021;16:e0251972. doi: 10.1371/journal.pone.0251972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Salvo D., Garcia L., Reis R.S., Stankov I., Goel R., Schipperijn J., Hallal P.C., Ding D., Pratt M. Physical activity promotion and the United Nations Sustainable Development Goals: Building synergies to maximize impact. J. Phys. Act. Health. 2021;18:1163–1180. doi: 10.1123/jpah.2021-0413. [DOI] [PubMed] [Google Scholar]
- 93.Aarts H., Verplanken B., Van Knippenberg A. Predicting behavior from actions in the past: Repeated decision making or a matter of habit? J. Appl. Soc Psychol. 1998;28:1355–1374. doi: 10.1111/j.1559-1816.1998.tb01681.x. [DOI] [Google Scholar]
- 94.Ouellette J.A., Wood W. Habit and intention in everyday life: The multiple processes by which past behavior predicts future behavior. Psychol. Bull. 1998;124:54–74. doi: 10.1037/0033-2909.124.1.54. [DOI] [Google Scholar]
- 95.Telama R., Yang X., Viikari J., Välimäki I., Wanne O., Raitakari O. Physical activity from childhood to adulthood: A 21-year tracking study. Am. J. Prev. Med. 2005;28:267–273. doi: 10.1016/j.amepre.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 96.Telama R. Tracking of physical activity from childhood to adulthood: A review. Obes. Facts. 2009;2:187–195. doi: 10.1159/000222244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Yao C.A., Rhodes R.E. Parental correlates in child and adolescent physical activity: A meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2015;12:10. doi: 10.1186/s12966-015-0163-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Petersen T.L., Møller L.B., Brønd J.C., Jepsen R., Grøntved A. Association between parent and child physical activity: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2020;17:67. doi: 10.1186/s12966-020-00966-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Coffey J.S., Gauderer L. When pediatric primary care providers prescribe nature engagement at a state park, do children “fill” the prescription? Ecopsychology. 2016;8:207–214. doi: 10.1089/eco.2016.0019. [DOI] [Google Scholar]
- 100.Zarr R., Cottrell L., Merrill C. Park prescription (DC Park Rx): A new strategy to combat chronic disease in children. J. Phys. Act. Health. 2017;14:1–2. doi: 10.1123/jpah.2017-0021. [DOI] [PubMed] [Google Scholar]
- 101.Brussoni M., Han C.S., Lin Y., Jacob J., Pike I., Bundy A., Faulkner G., Gardy J., Fisher B., Mâsse L. A web-based and in-person risk reframing intervention to influence mothers’ tolerance for, and parenting practices associated with, children’s outdoor risky play: Randomized controlled trial. JMIR. 2021;23:e24861. doi: 10.2196/24861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Tucker P., Gilliland J. The effect of season and weather on physical activity: A systematic review. Public Health. 2007;121:909–922. doi: 10.1016/j.puhe.2007.04.009. [DOI] [PubMed] [Google Scholar]
- 103.Lane G., Nisbet C., Johnson S., Candow D., Chilibeck P.D., Vatanparast H. Barriers and facilitators to meeting recommended physical activity levels among new immigrant and refugee children in Saskatchewan, Canada. Appl. Physiol. Nutr. Metabol. 2021;46:797–807. doi: 10.1139/apnm-2020-0666. [DOI] [PubMed] [Google Scholar]
- 104.Stockwell S., Trott M., Tully M., Shin J., Barnett Y., Butler L., McDermott D., Schuch F., Smith L. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: A systematic review. BMJ Open Sport Exerc. Med. 2021;7:e000960. doi: 10.1136/bmjsem-2020-000960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Lee S.W., Lee J., Moon S.Y., Jin H.Y., Yang J.M., Ogino S., Song M., Hong S.H., Ghayda R.A., Kronbichler A., et al. Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: A nationwide cohort study. Br. J. Sports Med. 2022;56:901–912. doi: 10.1136/bjsports-2021-104203. [DOI] [PubMed] [Google Scholar]
- 106.Bhandari K.R., Mirhajianmoghadam H., Ostrin L.A. Wearable sensors for measurement of viewing behavior, light exposure, and sleep. Sensors. 2021;21:7096. doi: 10.3390/s21217096. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Template data collection forms can be requested via email to R.L.