Abstract
Introduction
Infection prevention and control remains very key to safety in healthcare settings and community. The use of personal protective equipment is now more relevant especially with the advent of COVID-19 pandemic. This study aimed to assess the knowledge, attitude, practice and technique of wearing facemask among healthcare workers at Ekiti State University Teaching Hospital, Ado-Ekiti, Nigeria
Methods
A descriptive cross-sectional questionnaire-based study explored knowledge, attitude and reported practice on the use of facemask. Also, a checklist was used to directly observe how participants put on and remove facemasks.
Results
Of the 450 respondents, 316 (70.2%) had good knowledge score. Only 255 (56.7%) had good attitude and barely half of the respondents 229 (50.9%) had good practice. However, the majority of those who were observed had good technique of wearing facemask 387 (86.4%). Also, 188 (41.8%) of the healthcare workers believed that face shield alone offers adequate protection against transmission of COVID-19.
Conclusions
Our finding suggests that knowledge does not translate to good practice. Furthermore, the fact that two out of every five healthcare workers held erroneous belief about face shield, and another one-third had poor knowledge points to the need for training and retraining of healthcare workers with the aim of reinforcing the need for consistent and correct use of facemasks. This should have a salubrious effect on the community knowledge of COVID-19 prevention as healthcare workers are believed to be the most common sources of health information to the lay public
Keywords: Facemask usage, Healthcare workers, Nigeria
Introduction
Transmission of infections remains a serious problem in health care facilities especially in developing countries. Health care associated infections (HAI) are infections that occur in patients as a result of receiving care at a health care facility and were not present at the time of arrival at the facility [1,2]. This often impacts negatively on health care costs, patients’ outcome of care and health care delivery system [3,4]. Hospital acquired respiratory infection continues to contribute significantly to HAIs [5], [6], [7].
The use of personal protective equipment (PPE) is one of the measures of infection prevention and control [8]. The use of PPE is now more relevant especially with the advent of COVID-19 pandemic. Facemasks protect the mouth and nose from splashes or sprays of blood/body fluids, or respiratory secretions [9,10]. A systematic review by Barasheed et al. showed that facemasks are effective for prevention of disease transmission [11]. For COVID-19 pandemic, the World Health Organization recommends the use of standard facemasks (KN95 respirators, surgical and medical masks, etc.) of varying efficiencies depending on the situations for health care workers and the general public to prevent the transmission of COVID-19 disease [12]. However, for the general public only, when standard facemasks are not available, non-medical homemade multilayered mask could be an acceptable option [13].
However, to achieve the desired purpose of preventing transmission of infection between persons, facemasks must be worn correctly and consistently [10]. To wear a facemask correctly, there are steps that should be followed and these are; washing of hands with soap and water for at least 20 s or use of alcohol based sanitizer when soap and water are not available, thereafter place the facemask to cover your nose, mouth and chin. Also, it is important to avoid touching the facemask when wearing it. The proper technique to remove facemask involves performing hand hygiene, touching only the elastic bands, dispose of the used facemask in appropriate container and performing hand hygiene after disposing of the facemask [10,14].
There is paucity of data on healthcare workers’ knowledge, practice and appropriate technique for wearing a facemask. The few studies available did not assess correct technique for wearing facemask. A previous study among healthcare workers in Karachi, Pakistan found that barely half of the study participants knew about the correct method of wearing facemask [15]. Worse still, a study conducted among healthcare professionals in south eastern part of Nigeria observed that, only about 18% of them had good knowledge on the steps involved in the correct use of medical masks [16].
To prevent transmission of respiratory pathogens especially in the context of COVID-19, it is important for health workers to have good knowledge and practice of the use of facemasks. Success in infection prevention should contribute positively to achieving sustainable development goal 3 (SDG 3) especially the target of ending the epidemics of AIDS, tuberculosis, malaria, and other communicable diseases by 2030. The two hypotheses considered in this study were; there is a difference in the technique of wearing and removing facemask among different cadre of healthcare workers and there is a difference in the practice of wearing facemask among different cadre of healthcare workers. Hence, this study assessed the knowledge, attitude, practice and technique of wearing facemask among healthcare workers at Ekiti State University Teaching Hospital, Ado-Ekiti. It is expected that the findings from this study will help to identify the gap(s) in the knowledge and technique of wearing facemask among healthcare workers in the study site. Information from this study may also be useful in planning interventions aimed at improving the techniques and use of facemask among healthcare workers.
Methods
Study design
This study employed a descriptive cross-sectional design.
Study location
The study was conducted in Ekiti State University Teaching Hospital (EKSUTH), located in Ado Ekiti the capital city of Ekiti State in the South Western Nigeria between November and December 2020 which was after the general lockdown restriction was eased in Nigeria. EKSUTH is a tertiary and a referral hospital for primary and secondary health facilities in the state. It currently has about 1500 clinical and non-clinical staff.
Inclusion and exclusion criteria
It included any staff that has worked in the hospital for at least one year and consented to participate in the study. The study excluded those on annual or sick leave.
Sample size determination
The sample size was determined using the formula for calculation of single proportion Leslie Fischer's formula for > 10,000 [17]. A sample of 415 was derived, considering 5% precision, 95% confidence interval and 56.4% as correct knowledge of wearing mask, assuming 10% non-response rate [15].
Sampling technique
A stratified random sampling technique was applied. The staff were stratified based on their job designation/cadre (doctors, nurses, laboratory workers etc.). A proportionate allocation was done based on the sample frame containing the staff list that was obtained from the Establishment department of the hospital using systematic random sampling to select the participants. Each selected worker on the sample frame was visited and invited to participate. Anyone who declined was replaced with the next on the sample frame.
Data collection instrument and methods
A semi structured questionnaire which was self-administered, was deployed to get information on bio data, knowledge, attitude and reported practise on the use of facemask. An observational checklist was used to directly observe how participants put on and remove facemasks. The questionnaire and the observational checklist were adapted from a previous study [14] and the guidelines in ‘Use Mask Properly’, which was developed for use in Nigeria by the Nigeria center for Disease Control (NCDC) [18].
For each study participant, the questionnaire was administered first and later he/she was instructed to wear and take off the facemask using the provided cloth facemasks, hand sanitizers, and dust bins. There were four basic steps on how to put on a facemask and three basic steps on how to remove a facemask which research assistants scored using an observational checklist.
Four medical students of Ekiti State University served as research assistants and were trained on the objective of the study, methodology and relevant research ethics. Also, the research assistants were trained on the use of the questionnaire and the checklists. Twenty percent (83) of the total sample size calculated were pretested in a similar hospital in another local government area. After pre-testing, ambiguous questions were removed to improve the reliability of the questionnaire. The content validity of the questionnaire was done by a panel of physicians with good knowledge of infection prevention and control as well as a surgeon with over 20 years of practice versed in wearing and removing mask. Using test re-test method for two weeks for the questions on practice, Cronbach's alpha was 0.72 while for the questions on technique it was 0.70.
Assessment of knowledge
The knowledge section had nine questions. Each correct answer had a score of one. Total score obtainable was nine points. The median score of 7 was used to categorize the knowledge scores. A score of less than 7 was categorised as poor knowledge while individuals who had 7 or more points were adjudged to have good knowledge
Assessment of attitude
The attitude section had 17 questions in all. A five-point Likert scale format was used with responses ranging from “strongly agree” to “strongly disagree”. Nine of the questions were positively worded while the remaining eight were negatively worded. For the positively worded questions, options ranged from strongly agree to strongly disagree and the awarded points range from five to one respectively, while the reverse was true for the negatively worded questions. The maximum obtainable score was 85 and the median score of 61 was used to categorize the attitude scores as poor attitude (<61) and good attitude (≥ 61).
Assessment of practice
There were seven questions in this section. The questions were all positively worded and there were five options for each question. The highest obtainable point was 28 and the median score of 23 was used to categorize the practice scores into poor practice (<23) and good practice (≥23).
Assessment of facemask wearing technique
There were seven items on the checklist. Four items addressed the technique of wearing and three assessed the technique of removing the facemask. One point was awarded for each correct step taken. If done but not correctly, half a point was given. All the research assistants were trained to know the appropriate way of observing each of the steps in wearing and removing facemask. A score of four or more was categorised as good technique while a score of less than four was graded as poor technique.
Data analysis
Data analysis was conducted using SPSS version 25(SPSS Inc. 233 South Wacker Drive, 11th Floor, Chicago). Univariate analysis was done with mean and frequency tables to describe the demographic characteristics and knowledge, practice, and technique of the participants.
Bivariate analysis was used to assess the association between independent variables (age, sex, and job designation) and dependent/outcome variables (knowledge, attitude, practice, and technique) using chi square and independent t-test. A p-value of <0.05 was taken as statistically significant.
Ethical issues
Ethical clearance (EKSUTH/A67/2020/10/010) was obtained before commencement of the study from the Ethics and Research Committee of EKSUTH Ado-Ekiti. Verbal consent was obtained from the respondents.
Results
Socio-demographic characteristics of respondents
A total of 450 respondents participated. Majority of the respondents 253 (56.2%) were aged between 20 and 40 years, 195 (43.3%) were 41–60 years and only 2 (0.4%) were 60 years and above. Majority of the respondents were females 371 (70.4%), while 280 (62.2%) had tertiary education. Different categories of health worker participated: nurses were 149 (33.1%), doctors 93 (20.7%), administrative staff 39(8.7%), laboratory scientists 20(4.4%), pharmacists 14 (3.1%) and others (Dental technicians, Health attendants, Community Health Extension Workers, Record officers) 135(30.0%) (Table 1 ).
Table 1.
Social-demographic characteristics of respondents.
| Variables | Frequency | Percentage (%) |
|---|---|---|
| Age | ||
| 21–40 | 253 | 56.2 |
| 41–60 | 195 | 43.3 |
| 60 and above | 2 | 0.5 |
| Sex | ||
| Male | 133 | 29.6 |
| Female | 317 | 70.4 |
| Educational Level | ||
| Secondary and below | 74 | 16.5 |
| Tertiary | 376 | 83.5 |
| Religion | ||
| Christianity | 396 | 88.0 |
| Islam | 50 | 11.1 |
| Others | 4 | 0.9 |
| Profession | ||
| Nurse | 149 | 33.1 |
| Doctor | 93 | 20.7 |
| Administrative staff | 39 | 8.7 |
| Laboratory scientist | 20 | 4.4 |
| Pharmacist | 14 | 3.1 |
| Others (Dental Technicians, H/Atendants, CHEW, Records) | 135 | 30.0 |
H/Attendants – Health Attendant, CHEW – Community Health Extension Worker.
Knowledge of the use of face mask, type of mask used and respondent's potential exposure to COVID-19
Majority of the participants 433 (96.2%) believed that putting on facemask is a measure of infection prevention and control, 315 (70%) believed that cloth facemask protects the person wearing it from getting infected with COVID-19. Almost nine out of ten 400 (88.9%) believed that facemasks should be washed every day after use. The commonest type of face mask used in the preceding week by healthcare workers was surgical mask, 216 (48.0%) used only surgical, while 109 (24.3%) used surgical mask in combination with either cloth mask or N 95. Only 11 (2.4%) used only N 95 masks (Table 2 ).
Table 2.
Knowledge on the use of face mask, type of mask used and respondent's potential exposure to COVID-19.
| VARIABLES | Yes n (%) | No n (%) |
|---|---|---|
| Putting on of facemask is a measure of infection prevention and control | 433(96.2) | 17 (3.8) |
| Facemask can be worn incorrectly | 370 (82.2) | 80 (17.8) |
| To wear a face mask correctly, the mask should cover mouth and nose | 425 (94.4) | 25 (5.6) |
| When wearing a face mask, there is no need to cover your mouth when sneezing or coughing | 311 (69.1) | 139 (30.9) |
| A cloth facial mask protects the person wearing the mask from getting infected with COVID-19 | 315 (70.0) | 135 (30.0) |
| A cloth facial mask protects others from getting infected with COVID-19 | 281 (62.4) | 169 (37.6) |
| A cloth mask must be washed every day | 400 (88.9) | 150 (11.1) |
| You do not need to wear a face mask if you are wearing a face shield | 188 (41.8) | 262 (58.2) |
| A face mask should be kept in a secluded place after use | 390 (86.7) | 60 (13.3) |
| Commonest type of mask used by respondent in the last one week | ||
| Surgical mask | 216(48.0) | 0(0.0) |
| Cloth mask | 112(24.9) | 0(0.0) |
| Cloth & Surgical mask | 97(21.6) | 0(0.0) |
| Cloth, Surgical and N95 masks | 12(2.7) | 0(0.0) |
| N-95 mask | 11(2.4) | 0(0.0) |
| Others | 2(0.4) | 0(0.0) |
| Someone close had COVID-19 | ||
| Yes | 78(17.3) | 0(0.0) |
| No | 321(71.3) | 0(0.0) |
| Don't Know | 51(11.4) | 0(0.0) |
| Had Contact with a COVID-19 patient | ||
| Yes | 95(21.1) | 0(0.0) |
| No | 281(62.4) | 0(0.0) |
| Don't Know | 74(16.5) | 0(0.0) |
Attitudes towards the use of facemask
Some health workers expressed positive attitude and some negative attitude. Some of the positive attitudes expressed were: 262 (58.2%) agreed that they were more susceptible to COVID-19 indoor than outdoor and 29 (6.4%) agreed that there was a higher possibility of contacting COVID-19 in a crowd. Regarding negative attitude to COVID-19, almost half of the participants 202 (44.8%) agreed that wearing facemask makes them uncomfortable and does not allow them to breathe properly. Forty-three (9.5%) felt that COVID-19 does not exist (Table 3 ).
Table 3.
Respondents’ attitudes towards the use of facemask.
| Characteristic | Strongly Agree n (%) | Agree n (%) | Uncertain n (%) | Disagree n (%) | Strongly Disagree n (%) |
|---|---|---|---|---|---|
| I am confident that I know the proper steps to wear a facemask correctly | 3(0.7) | 11(2.4) | 7(1.6) | 202(44.9) | 227(50.4) |
| I am more susceptible to COVID-19 in indoor than outside | 89(19.8) | 173(38.4) | 39(8.7) | 84(18.7) | 65(14.4) |
| There is a high chance of having COVID-19 transmitted to me when I am in a crowd | 6(1.3) | 23(5.1) | 18(4.0) | 173(38.4) | 230(51.2) |
| Buying a facemask is expensive. | 31(6.9) | 76(16.9) | 33(7.3) | 264(58.7) | 46(10.2) |
| Wearing a facemask is troublesome because I cannot breathe properly | 47(10.4) | 155(34.4) | 22(4.9) | 189(42.0) | 37(8.3) |
| I feel ashamed if I am the only person wearing a facemask | 33(7.3) | 55(12.2) | 28(6.2) | 264(58.7) | 70(15.6) |
| It is easier to wear a facemask if everyone else is wearing one too | 14(3.1) | 89(19.8) | 16(3.5) | 234(52.0) | 97(21.6) |
| Because of the facemask law in Ekiti, I now wear facemask more often | 89(19.8) | 227(50.4) | 28(6.2) | 81(18.0) | 25(5.6) |
| I believe that getting COVID-19 is serious | 24(5.3) | 47(10.4) | 27(6.0) | 207(46.1) | 145(32.2) |
| Wearing a facemask cannot fully prevent the transmission of COVID-19 | 4(0.9) | 51(11.3) | 25(5.6) | 264(58.7) | 106(23.5) |
| I feel that if I get COVID-19, I will recover quickly | 121(26.9) | 226(50.2) | 48(10.7) | 46(10.2) | 9(2.0) |
| I believe that wearing a facemask is a good way to protect myself against COVID-19 | 8(1.8) | 10(2.2) | 14(3.1) | 251(55.8) | 167(37.1) |
| Having COVID-19 will be troublesome for me as I may spread it to loved ones | 14(3.1) | 25(5.6) | 23(5.1) | 259(57.5) | 129(28.7) |
| I feel that since the Lockdown is over, I no longer need to worry about contracting COVID-19 | 30(6.7) | 70(15.6) | 27(6.0) | 201(44.6) | 122(27.1) |
| I feel facemask hinder communication | 49(10.9) | 120(26.7) | 48(10.6) | 179(39.8) | 54(12.0) |
| COVID-19 does not exist | 23(5.1) | 20(4.4) | 16(3.6) | 154(34.2) | 237(52.7) |
| I believe that wearing a facemask is a good way to protect myself against flu and tuberculosis | 23(5.1) | 33(7.3) | 31(6.9) | 221(49.1) | 142(31.6) |
Practice of using facemask
One hundred and seventy-three (38.4%) of the respondents frequently wear facemasks in public places when they were not ill while 149(33.1%) always wore it in public places even when they were ill. Among the respondents, 81 (18.0%) always wore facemask at home when they had respiratory symptoms and 123 (27.3%) never remove their facemask when they need to talk with people (Table 4 ).
Table 4.
PRACTICE OF USING FACE MASK among the respondents.
| Characteristic | Never n (%) | Rarely n (%) | Sometimes n (%) | Frequently n (%) | Always n (%) | Not Applicable n (%) |
|---|---|---|---|---|---|---|
| I wear a face mask in public venues even when I am NOT ill | 17(3.8) | 37(8.2) | 90(20.0) | 173(38.4) | 128(28.4) | 5(1.2) |
| I wear a face mask in public venues when I am ill | 23(5.1) | 58(12.9) | 68(15.2) | 123(27.3) | 149(33.1) | 29(6.4) |
| I wear a face mask when in the hospital even when I am NOT ill | 10(2.2) | 26(5.8) | 48(10.7) | 123(27.3) | 236(52.4) | 7(1.6) |
| I wear a face mask when in the hospital when I am ill | 25(5.5) | 25(5.5) | 67(14.9) | 106(23.6) | 197(43.8) | 30(6.7) |
| I wear a face mask at home if I have fever or respiratory symptoms | 117(26.0) | 88(19.6) | 79(17.6) | 47(10.4) | 81(18.0) | 38(8.4) |
| I wear a face mask at home when family members have respiratory symptoms | 111(24.7) | 97(21.5) | 99(22.0) | 35(7.8) | 84(18.7) | 24(5.3) |
| I remove my facemask when I need to talk to people | 123(27.3) | 86(19.1) | 144(32.0) | 41(9.1) | 43(9.6) | 13(2.9) |
Technique of wearing facemask
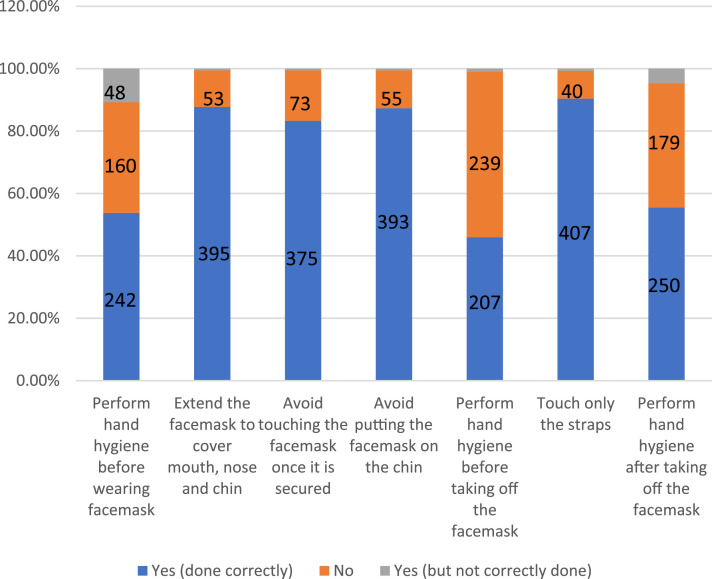
Hand hygiene was assessed if correctly done or not, 242 (53.8%) performed hand hygiene correctly before wearing the mask while 160 (35.6%) did not perform hand hygiene at all before wearing facemask. Two hundred and seven (46.0%) performed hand hygiene correctly before removing the facemask and 250 (55.6%) performed it after taking off the facemask (Fig. 1 ).
Fig. 1.
Technique of wearing and removal of face mask by the respondents.
Association between respondents’ socio-demographic characteristics and knowledge of use and type of facemask and attitude to facemask use
Overall, 316 (70.2%) of the participants had good knowledge while 134 (29.8%) had poor knowledge. Laboratory scientists were more knowledgeable than other healthcare workers (p = 0.021). Those with tertiary education appeared to be more knowledgeable compared with those with secondary school education (p = 0.001) More respondents who had not had contact with someone with COVID 19 had good knowledge compared with respondents who have had contact with someone with COVID 19 (p = 0.001) (Table 5 ).
Table 5.
Association between respondents’ socio-demographic characteristics and knowledge of use and type of facemask.
| Poor Knowledge n (%) | Good Knowledge n (%) | Statistical comparison | p value | |
|---|---|---|---|---|
| Age | ||||
| 21 – 40 | 71 (28.1) | 182 (71.9) | Fisher's exact | 0.405 |
| 40 - 60 | 62 (31.8) | 133 (68.2) | ||
| >60 | 1 (50.0) | 1 (50.0) | ||
| Profession | ||||
| Doctors | 32 (34.4) | 61 (65.6) | χ[2]=13.261 | 0.021 |
| Nurses | 42 (28.2) | 107 (71.8) | ||
| Pharmacy | 5 (35.7) | 9 (64.3) | ||
| Lab Scientist | 1 (5.0) | 19 (95.0) | ||
| Admin Staff | 6 (15.4) | 33 (84.6) | ||
| Others | 48 (35.6%) | 87 (64.4) | ||
| Sex | ||||
| Male | 37 (27.8) | 96 (72.2) | χ[2]=0.346 | 0.556 |
| Female | 97 (30.6) | 220 (69.4) | ||
| Educational Level | ||||
| Secondary and below | 31(41.9.9) | 43 (58.1) | χ[2]=22.51 | 0.001 |
| Tertiary | 103 (27.4) | 273(72.6) | ||
| Religion | ||||
| Christianity | 106 (26.8) | 290 (73.2) | Fisher's exact | 0.001 |
| Islam | 26 (52.0) | 24 (48.0) | ||
| Others | 2 (50.0) | 2 (50.0) | ||
| Someone close had COVID-19 | ||||
| Yes | 32 (41.0) | 46 (59.0) | χ[2] =6.150 | 0.046 |
| No | 86 (26.8) | 235 (73.2) | ||
| Don't know | 16 (31.4) | 35 (68.6) | ||
| Contact with COVID-19 Patient | ||||
| Yes | 50 (52.6) | 45 (47.4) | χ[2] = 30.265 | p<0.001 |
| No | 68 (24.2) | 213 (75.8) | ||
| Don't Know | 16 (21.6) | 58 (78.4) |
Association between respondents’ socio-demographic characteristics and knowledge of use and type of facemask and attitude to facemask use
Out of all the respondents, 195 (43.3%) had poor attitude while 255 (56.7%) had good attitude. More laboratory scientists (75.0%) had good attitude (p = 0.009) and more respondents with secondary school as their highest level of education (53.7%) had poor attitude (p<0.001). The relationship between knowledge on the use of facemask and attitude to facemask use was not statistically significant (χ[2]= 2.724, p = 0.099) (Supplementary Table 1).
Association between respondents’ socio-demographic characteristics and practice of using facemask
Overall, 229 (50.9%) of the respondents had good practice in the use of face mask. Level of practice among different professions was different (p<0.001). More male respondents (63.2%) had good practice of using the face mask compared with their female counterparts (45.7%) (p = 0.001). There was no statistically significant relationship between respondents’ practice of using facemask and respondents’ knowledge on the use of facemask (χ[2]= 2.199, p = 0.138) and attitude towards facemask use (χ[2]= 3.087, p = 0.079) (Supplementary Table 2).
Association between respondents’ socio-demographic characteristics and technique of wearing facemask
Overall, 389 (86.4%) of the respondents had good technique. Those with good technique among the medical doctors were more compared with other professionals and this difference was statistically significant (p = 0.001). There was a significant association between educational level and technique of wearing facemask (p = 0.043). (Supplementary Table 3).
Discussion
This study aimed to assess the knowledge, attitude, practice of wearing facemask among healthcare workers in a tertiary health facility. It observed that most healthcare workers had good knowledge of and attitude to facemask. However, barely one-half had good practice of the use of facemask while about four-fifth had good technique of wearing facemask.
Surgical and cloth masks were the most commonly used masks by respondents in the week preceding the survey and very few persons used N95 masks in this study. This may be because surgical and cloth masks were both cheaper and more commonly available than N95 masks at the time of the study. In addition, those working directly with patients are also provided with surgical masks by the hospital. However, the use of cloth mask is not recommended for use by health workers while on duty as the cloth mask was only recommended for use in community settings during that early phase of the pandemic when there was general gross scarcity of medical and surgical masks in our country [19].
Most healthcare workers had good knowledge of the use of facemask. However, about two-fifth of respondents indicated that the use of face shield obviates the need for a facemask. This is an erroneous belief that will need to be corrected via training and retraining of these health workers. This becomes imperative because the use of face shield instead of facemask is not recommended as a COVID-19 preventive measure [3,20]. The knowledge on the use of facemask varied significantly across the professional groups of respondents as more nurses and laboratory scientists had good knowledge. This is in consonance with a similar study conducted among health workers in southwestern and northwestern Nigeria [21]. The above cited study reported that nurses were more knowledgeable about personal protective equipment (PPE) needed to prevent COVID-19 than other cadres of workers [21]. However, an Ethiopian study found that knowledge on the use of facemask/PPE may be higher in other cadres of health workers [22].
Although the attitude of healthcare workers to the use of facemask was generally good, there exist some gaps that need to be addressed. For instance, most of the respondents were not confident about their knowledge of the proper steps in donning a mask correctly. This is in contrast with the results from a Ugandan study where the majority (69.4%) were confident that they can correctly put on a facemask [23]. In addition, there appears to be a poor perception of the risk of acquiring COVID among respondents as majority of them disagreed that they were more susceptible to COVID-19 when in a crowd despite clear evidence from the literature that crowding favours the spread of respiratory pathogens like COVID-19 [24,25].
The attitude of respondents varied among professional groups of healthcare workers as laboratory scientists and doctors had good attitude towards the use of facemask. It is expected that all cadre of workers should have good attitude to the use of facemask especially since it is an effective means of limiting the transmission of SARs-CoV2 particularly in resource poor settings like Nigeria. In addition, educational attainment was significantly associated with health workers’ attitude; as individuals with post tertiary and postgraduate education had good attitude toward the use of facemask. This is not surprising as it is expected that higher educational attainments should confer an advantage of improved attitudes and perceptions for positive health behavior. This has been corroborated by other studies [23,26]. This finding suggests that targeted continuing professional education is indicated to improve the attitude of professional groups to the proper use of facemasks and other PPE.
Although only about half of health workers had good practice of using facemasks, some respondents’ characteristics such as gender, professional cadre, educational attainment and history of contact with persons who had COVID-9 were significantly associated with facemask use. Males had good practice of facemask use in our study and this finding is in consonance with a study among the Vietnamese where males were also found to have good practice of use of facemask [23]. However, other studies reported that females were more likely to use facemask and comply with COVID-19 preventive measures [27,28].
Individuals with history of contact with COVID-19 cases (patients or close acquaintances) had good practice. This may not be unexpected because such persons are more likely to perceive the risk of acquiring COVID-19 to be high and hence adhere more to the proper use of facemask.
It is encouraging to note that the proportions who demonstrated good technique of putting on facemask was higher than the proportions who showed good knowledge, attitude and practice for all professions apart from laboratory scientists. It showed that when most of the health workers decided to use facemasks, they tended to do it the right way.
Healthcare workers are the most trusted and source of health information for many people [29,30]. That two-fifth of the respondents in this study held erroneous belief about face shield and close to one-quarter had poor knowledge of COVID-19 is rather unacceptable. These suggest the need for training and education of the hospital workforce. This study was conducted in a teaching hospital. Teaching hospitals are supposed to have the most knowledgeable workforce. This may imply that the COVID-19 knowledge base of the health workers in the lower tiers of healthcare is probably poorer than in this hospital. The implication for educating the lay public about COVID-19 is dire.
Study limitations
This study cannot be generalized to all health care workers because this was a single center study. Also, that the current study used a mixed method approach involving both questionnaire and direct observation has the potential for certain biases. For example, our study instrument has a self-report component which is prone to social desirability report bias. In addition, the direct observation component is prone to the possibility of Hawthorne effect where people will strive to do what is right which may not be their usual practice.
Conclusion
This study has demonstrated that healthcare workers in this study had good knowledge of the use of facemask as a preventive measure for COVID-19 (70.2%), however this did not translate to an appreciable level of practice of facemask use. Also, barely one-half of the respondents had positive attitude towards facemask use. This study concludes by recommending training and retraining of health workers with the aim of reinforcing the need for consistent and correct use of facemasks and positive attitude towards the use of facemask as a preventive measure for COVID-19.
Authors’ contributions statement
AB, OS, TO, OO and KO designed and supervised the study and did the initial draft of the manuscript. AB and OS supervised collection of the data. AB, OS and TO analyzed the data and performed the background literature review for the manuscript. OS, OS, TO and JF drafted the manuscript. All authors reviewed and approved the final version of the manuscript.
Funding
None to declare.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
We thank all our research assistants and study participants for their cooperation.
TOO was supported by the African Academy of Sciences (AAS) under a DELTAS Africa Initiative grant [107768/Z/15/Z] as part of the Consortium for Advanced Research Training in Africa (CARTA). The views expressed in this publication are those of the authors and not necessarily those of AAS or other partners in the consortium.
Editor Name: DR B Gyampoh
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.sciaf.2023.e01559.
Appendix. Supplementary materials
References
- 1.Monegro A.F., Muppidi V., Regunath H. StatPearls Publishing; 2020. Hospital Acquired Infections [Internet]https://www.ncbi.nlm.nih.gov/books/NBK441857/ [cited 2020 Oct 5]. Available from: [PubMed] [Google Scholar]
- 2.World Health Organization. Prevention of hospital-acquired infections: a practical guide. 2nd edition 2002. [cited 2020 Sep 29]. Available from: https://www.who.int/csr/resources/publications/drugresist/WHO_CDS_CSR_EPH_2002_12/en/.
- 3.Akinboyo I.C., Young R.R., Smith M.J., Smith B.A., Lewis S.S., Anderson D.J. Burden of Healthcare-Associated Infections among Hospitalized Infants within Community Hospitals. Open Forum Infect. Dis. 2019;23:S279–S280. [Google Scholar]
- 4.World Health Organization. The burden of health care-associated infection worldwide 2010 [cited 2020 Sep 23]. Available from: http://www.who.int/infection-prevention/publications/burden_hcai/en/.
- 5.Chow E.J., Mermel L.A. Hospital-acquired respiratory viral infections: incidence, morbidity, and mortality in pediatric and adult patients. Open Forum Infect. Dis. 2017;4(1) doi: 10.1093/ofid/ofx006. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5414085/ [cited 2020 Sep 29]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cardoso T., Lopes L.M., Carneiro A.H. Hospital-acquired respiratory infection in patients admitted in ICU. Critical Care. 2001;5(Suppl 1):P041. [Google Scholar]
- 7.Wang L., Zhou K.H., Chen W., Yu Y., Feng S.F. Epidemiology and risk factors for nosocomial infection in the respiratory intensive care unit of a teaching hospital in China: a prospective surveillance during 2013 and 2015. BMC Infect. Dis. 2019;19(1):145. doi: 10.1186/s12879-019-3772-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. Personal protective equipment [Internet]. 2020 [cited 2020 Sep 23]. Available from: http://www.who.int/medical_devices/meddev_ppe/en/.
- 9.Wisconsin Department of Health Services Infection Control and Prevention - Personal Protective Equipment (PPE) 2014 [Internet]. [cited 2020 Sep 23]. Available from: https://www.dhs.wisconsin.gov/ic/ppe.htm.
- 10.Desai A.N., Masks Mehrotra P.Medical. JAMA. 2020;323(15):1517–1518. doi: 10.1001/jama.2020.2331. [DOI] [PubMed] [Google Scholar]
- 11.Barasheed O., Alfelali M., Mushta S., et al. Uptake and effectiveness of facemask against respiratory infections at mass gatherings: a systematic review. Int. J. Infect. Dis. 2016;47:105–111. doi: 10.1016/j.ijid.2016.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coronavirus disease (COVID-19): masks [Internet]. [cited 2022 May 9]. Available from: https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-covid-19-masks.
- 13.World Health Organization. Advice on the use of masks in the community, during home care and in healthcare settings in the context of the novel coronavirus (COVID-19) outbreak 2020 [cited 2020 Oct 6]. Available from: https://www.who.int/publications-detail-redirect/advice-on-the-use-of-masks-in-the-community-during-home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-outbreak.
- 14.Lee L.Y., Lam E.P., Chan C., et al. Practice and technique of using facemask amongst adults in the community: a cross-sectional descriptive study. BMC Public Health. 2020;20(1):948. doi: 10.1186/s12889-020-09087-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kumar J., Katto M.S., Siddiqui A.A., et al. Knowledge, Attitude, and Practices of Healthcare Workers Regarding the Use of Facemask to Limit the Spread of the New Coronavirus Disease (COVID-19) Cureus. 2020;12(4) doi: 10.7759/cureus.7737. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7241223/ [cited 2020 Aug 31]; Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ozioko U.S., Iyidobi E.C., Ozioko O.M., Ozor I.I., Mbaeze C.O., Abireh I.E. The pattern of use of medical masks among health care professionals during covid 19 pandemic in South East Nigeria University Teaching Hospitals. Int. J. Infect. Dis. Ther. 2020;5(3):81. [Google Scholar]
- 17.Araoye M.O. Nathadex Publishers; Ilorin: 2003. Sample Size determination: In research Methodology With Statistics For Health and Social Sciences. [Google Scholar]
- 18.Centre for Disease Control and Prevention. Advisory on Use of Cloth Facemasks. 2019. Accessed on 18/08/21 Available at: https://covid19.ncdc.gov.ng/media/files/UseOfClothFaceMasks.pdf.
- 19.World Health Organization. Advice on the use of masks in the context of COVID-19: interim guidance, 6 April 2020 [Internet] 2020 (Cited 2021 August 18) Available at: https://apps.who.int/iris/handle/10665/331693.
- 20.Centers for Disease Control and Prevention. 2019. Guidance for wearing masks. Help slow the spread of COVID-19. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cloth-face-cover-guidance.html.
- 21.Alao M.A., Durodola A.O., Ibrahim O.R., Asinobi O.A. Assessment of Health Workers’ Knowledge, Beliefs, Attitudes, 2020. Available from: https://doi.org/10.1155/2020/4619214.
- 22.Tadesse T., Tesfaye T., Alemu T., Haileselassie W. Healthcare worker knowledge, attitude, and practice of proper facemask utilization, and associated factors in police health facilities of Addis Ababa. Ethiopia J. Multidiscip. Healthc. 2020;13:1203–1213. doi: 10.2147/JMDH.S277133. https://www.dovepress.com/healthcare-workerrsquos-knowledge-attitude-and-practice-of-proper-face-peer-reviewed-fulltext-article-JMDH020 [Internet][cited 2021 Jul 18] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sikakulya F.K., Ssebuufu R., Mambo S.B., et al. Use of facemasks to limit the spread of the COVID-19 among western Ugandans: knowledge, attitude and practices. PLoS One. 2021;16(3) doi: 10.1371/journal.pone.0248706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Adam D.C., Wu P., Wong J.Y., Lau E.H.Y., Tsang T.K., Cauchemez S., et al. Clustering and superspreading potential of SARS-CoV-2 infections in Hong Kong. Nat. Med. 2020;26(11):1714–1719. doi: 10.1038/s41591-020-1092-0. [DOI] [PubMed] [Google Scholar]
- 25.Chen Q., Toorop M.M.A., de Boer M.G.J., Rosendaal F.R., Lijfering W.M. LUMC-COVID-19 Research Group. Why crowding matters in the time of COVID-19 pandemic? - A lesson from the carnival effect on the 2017/2018 influenza epidemic in the Netherlands. BMC Public Health. 2020;20(1):1516. doi: 10.1186/s12889-020-09612-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Duong M.C., Nguyen H.T., Duong B.T. A cross-sectional study of knowledge, attitude, and practice towards facemask use amid the COVID-19 pandemic amongst university students in Vietnam. J. Commun. Heal. 2021:1–7. doi: 10.1007/s10900-021-00981-6. https://link.springer.com/article/10.1007/s10900-021-00981-6 [cited 2021 Jul 18] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Haischer M.H., Beilfuss R., Hart M.R., et al. Who is wearing a mask? Gender-, age-, and location-related differences during the COVID-19 pandemic. PLoS One [cited 2021 Jul 18];15(10). Available from: /pmc/articles/PMC7561164/. [DOI] [PMC free article] [PubMed]
- 28.Howard M.C. Gender, facemask perceptions, and facemask wearing: are men being dangerous during the COVID-19 pandemic? Pers. Individ. Dif. 2021;170 doi: 10.1016/j.paid.2020.110417. [Internet]. [cited 2021 Jul 18] Available from: /pmc/articles/PMC7543707/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Livingston G., Minushkin S., Cohn D. M-sources of information on health and health care [Internet]. Pew Research Center's Hispanic Trends Project. 2008 [cited 2021 Jul 24]. Available from: https://www.pewresearch.org/hispanic/2008/08/13/iv-sources-of-information-on-health-and-health-care/.
- 30.Citilli C.C. Seeking health information: what sources do your patients use? Orthop. Nurs. 2010;(3):214–219. doi: 10.1097/NOR.0b013e3181db5471. PMID: 20505493. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.