Abstract
Background/Objectives:
The benefits of laparoscopic surgery such as swifter recovery and fewer wound complications, elude much of the developing world. Nigeria, a lower middle-income country, is the most populous sub-Saharan nation; an excellent model for studying the impact of laparoscopy in resource-constrained environments. The Department of Surgery at the Obafemi Awolowo University Teaching Hospital and the University of Utah’s Center for Global Surgery present a study of laparoscopic surgery cases in sub-Saharan Africa.
Methods:
A retrospective chart review of 261 patients compared open and laparoscopic surgical outcomes for three common general surgery procedures: open versus laparoscopic cholecystectomy and appendectomy, and open laparotomy versus diagnostic laparoscopy for biopsy of intra-abdominal mass. The primary outcome was total length of stay (LOS); secondary outcomes included wound complications, analgesia and antibiotic use, time to oral intake, and patient charges.
Results:
Total LOS for laparoscopic surgery was significantly shorter compared to analogous open procedures (4.7 vs 11.5 days). Postoperative LOS was also shorter (2.6 vs 8.2 days). There were no differences in wound complications. Median charges to patients were lower for laparoscopic versus open procedures ($184 vs $217 USD).
Conclusions:
The introduction of laparoscopy allows for significantly shorter LOS and equivalent wound complications in the context of a sub-Saharan teaching hospital. Concerns regarding higher costs of care for patients do not appear to be a significant issue. Further work is needed to evaluate costs to the hospital system as a whole, including procurement and maintenance of laparoscopic equipment.
Keywords: General surgery, Laparoscopy, LMIC, Outcomes
INTRODUCTION
Access to safe and timely surgery in the developing world is a growing subject of interest.1 One area of focus is laparoscopic surgery, which has demonstrated shorter recovery times compared to open surgery in both high- and low-income populations. Shorter recovery allows for faster return to daily activities and work, which is crucial for families in lower-middle income countries (LMICs) reliant upon day-to-day income.2 Incision-related complications occur in greater numbers and have a larger financial and personal impact in LMICs. Furthermore, antibiotics may be challenging to procure and administer and access to specialist care for complications can be extremely limited and costly. Laparoscopy allows for smaller incisions, less risk of hernia, wound separation, and infection.3,4 These findings support access to laparoscopic surgery as vital to modern global healthcare. New modalities may also strengthen nascent health systems; encouraging centralized organization of training, outcomes monitoring, and maintenance of technology, as seen in Mongolia and elsewhere.5,6
Publication on laparoscopy in LMICs began in the 1980s, with the longest series published by Udwadia et al. in India, and Johns Hopkins’ Jhpiego in 40 countries.7–9 Most laparoscopic data published in sub-Saharan populations are small case series focused on one procedure type, with little data regarding outcomes and costs related to the introduction of laparoscopy.
The most populous country in Africa, Nigeria is experiencing rapid economic and technological advancement but remains an LMIC, making it an ideal location to study the impact of laparoscopy and surgical infrastructure.10 It is home to 88% of Western Africa’s 44 surgical training programs. Most trainees report a desire for more training in laparoscopy.11 In recent years, the surgical department at the Obafemi Awolowo University Teaching Hospital (OAUTH) has embraced laparoscopic surgery. One surgeon was able to travel abroad for a laparoscopy fellowship and has since procured equipment and staff to open a laparoscopy unit in the hospital. Cases selected for this unit are based on surgeon, staff, and equipment availability. Unreliable electricity and insufflation gas sometimes determine operative approach. Since their first procedure in 2007, laparoscopic cases have included appendectomy, cholecystectomy, colectomy, and various diagnostic surgeries. We sought to evaluate outcomes and costs associated with the most commonly performed laparoscopic and open general surgery procedures at OAUTH since the adoption of laparoscopy. We hypothesize patient outcomes to be superior in the laparoscopic group, while open procedures will demonstrate cost savings.
The goals laparoscopy seeks to achieve appear attainable, based on earlier published experiences from OAUTH, which demonstrated decreased length of stay (LOS) by almost half (1.8 days vs 3.0) with the first series of 139 appendicitis patients after introducing laparoscopic appendectomy.12 Cases were completed for as little as $95 to $285 US. More recent experience from 2017 shows a progressive increase in the rate and number of laparoscopic cholecystectomies between 2005 and 2015, from 2.7% of all elective major general surgery procedures to 9.1%, with similar LOS trends.13
METHODOLOGY
A retrospective chart review was carried out at OAUTH in Fall 2016, for all available laparoscopic general surgery cases performed between January 1, 2005 and December 31, 2016, as well as analogous open cases. Initially, 419 patients were identified via the operative log as having received laparoscopic surgery during this period. Of these, 290 were one of the three laparoscopic procedures included in this study: appendectomy, cholecystectomy, or diagnostic biopsy of intra-abdominal mass (referred to as “diagnostic laparoscopy” and “mini-laparotomy” for laparoscopic and open approaches, respectively). These three procedures were chosen because they were the most frequently performed by the OAUTH General Surgery Division. Of those 290, 151 laparoscopic cases could be found in the medical records department, as well as 110 analogous open surgery cases. Cases were not organized by year, and the records department system had challenges such as duplicate and missing files that increased difficulty of retrieval, thus distribution between 2005 and 2016 was random. Inclusion criteria included patients between the ages of 14 and 80 years who underwent one of the three procedures in either open or laparoscopic fashion. All case files that met inclusion criteria and were retrievable were included, producing a convenience sample. Data were deidentified by numerical key, collected, and managed using REDCap electronic data capture tools hosted at the University of Utah.14 Statistical analysis was carried out with assistance from the University of Utah’s Study Design and Biostatistics Center using Stata (StataCorp, Texas), and included χ2, student’s T-test, Wilcoxon rank sum, and Fisher test as appropriate for continuous and categorical variables.15
Prior to data collection, power analysis indicated that a minimum of 260 total patients would be required to detect outcomes differences between laparoscopic versus open procedures, assuming a maximum of 70% laparoscopic cases (α 0.05, β 00.1), and p < 0.05 was statistically significant. Data were reported in terms of most statistically meaningful measure, either mean or median; both were included where possible.
The primary outcome was total length of stay (TLOS); secondary outcomes included postoperative length of stay (PLOS), surgical site infection (SSI), skin separation, fascial dehiscence, incisional hernia, hypertrophic scar, analgesic use, time to oral intake, antibiotic use, length of follow-up (in weeks), and cost to the patient. Analgesics and antibiotics were categorized for simplification (i.e. narcotic versus non-narcotic, cephalosporin versus metronidazole) and total doses per patient were counted, both pre- and postoperatively. Narcotic dosing conversions to morphine equivalents were not feasible, as exact dosage given was not always available. Post-discharge occurrences were obtained from patient charts based on documentation from follow-up clinic visits. The date of last surgical visit was used to calculate length of follow-up in weeks. Return to the operating room and reason for reoperation were also recorded, if applicable. For patients undergoing cholecystectomy, biliary tree injuries were recorded based on documented incidence of bile leak or other evidence of biliary injury. All patients whose procedures were converted from laparoscopic to open remained in the laparoscopic cohort, per intention-to-treat analysis.
Total in-patient costs to the hospital system were unavailable; thus, total charges to the patient upon discharge from the initial surgical procedure were used as a surrogate for cost. These costs included surgical materials purchased by the patient, surgeon and anesthesia fees, and in-patient care including medications, meals, and nursing. Cost data were sorted by fiscal year, converted to US dollars based on year-specific exchange rates, and converted to 2017 US dollar values.16 Insurance status in the Nigerian National Health Insurance Scheme (NHIS) was also noted.
The University of Utah’s Internal Review Board (#00093980) and the Ethics Committee at the Obafemi Awolowo University Teaching Hospital (ERC/2016/09/02) approved this study. The University of Utah Study Design and Biostatistics Center supported this investigation.
RESULTS
Two hundred sixty-one patients met inclusion criteria and had charts available in medical records, including 151 who underwent one of the three laparoscopic procedures of interest, and 110 having had analogous open surgeries. The most common reasons for exclusion were age outside of inclusion criteria and inability to locate the chart. Demographics analysis revealed equivalent mean age between groups (39.1 years vs 37.9, standard deviation [SD] 15.4 vs 15.0, P = .55). The laparoscopic cohort had a lower proportion of male patients than the open cohort (32% male vs 51%, P = .003). There was a slightly higher percentage of insured patients in the open group, 33% versus 23% insured in the laparoscopic group; this was not statistically significant (Table 1).
Table 1.
Patient Demographics Stratified by Laparoscopic Versus Open Procedures
| Laparoscopic (N = 151) | Open (N = 110) | P-Value | |
|---|---|---|---|
| Age | |||
| Mean (SD) | 39.1 (15.4) | 37.9 (15) | 0.55 |
| Median (IQR) | 37 (27, 50) | 34 (24, 50) | - |
| Range | (14, 79) | (18, 72) | - |
| Sex | |||
| Male (%) | 49 (32%) | 56 (51%) | 0.003 |
| Insured through NHIS | 35 (23%) | 36 (33%) | 0.09 |
Abbreviations: SD, standard deviation; IQR, interquartile range; NHIS, National Health Insurance Scheme.
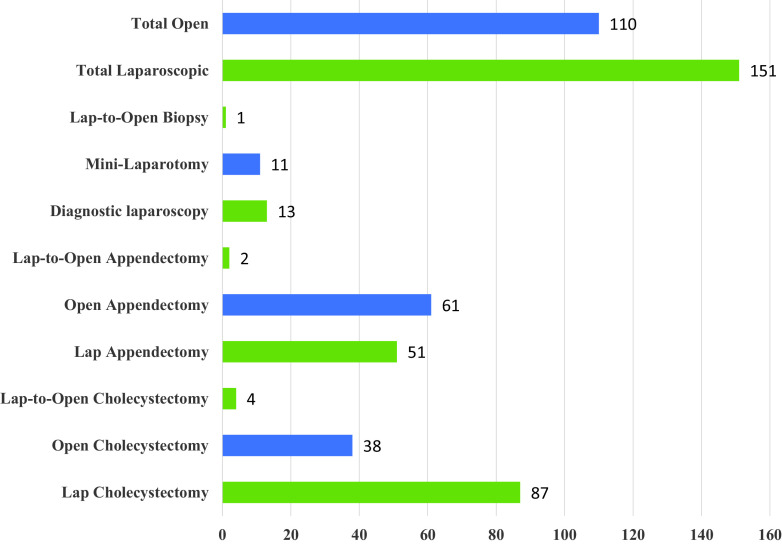
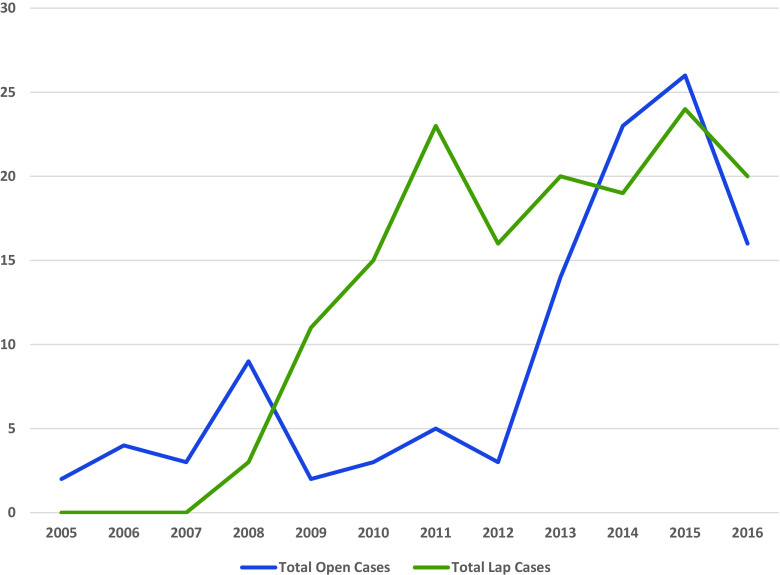
Procedural distribution varied based on departmental practices with regard to adoption of laparoscopy. For instance, more cholecystectomies were performed laparoscopically versus open, whereas open appendectomies were almost equal to laparoscopic. Biopsies for intra-abdominal masses were likewise fairly equal between open and laparoscopic (Figure 1). All laparoscopic cases were performed by one surgeon, while open cases were performed by all general surgeons within the division. Discharge criteria were similar between the laparoscopic and open surgical units. All laparoscopic cases were performed during daytime hours; nighttime (urgent) cases done open. The number of laparoscopic cases quickly increased between 2007 and 2011 and has since leveled off at a rate approximately equal to open cases. Total case volume for both approaches increased substantially since the mid-2000s (Figure 2).
Figure 1.
Patient distribution by procedure type.
Figure 2.
Total case volume by year.
The primary outcome, TLOS was significantly shorter for patients undergoing laparoscopic procedures compared with their open counterparts (mean TLOS 3.9 days vs 10.7, SD 4.7 vs 12.1; median TLOS 2.8 days vs 5.7, P < .001). PLOS followed a similar trend, at a median of 1.9 days for laparoscopic cases versus 4.0 for open (P < .001). Additional secondary outcomes, including in-hospital death, return to operating room, time to oral intake, SSI, fascial dehiscence, wound separation, hypertrophic scar, incisional hernia, and bile duct injury for cholecystectomy patients were also compared (Table 2).
Table 2.
Primary and Secondary Outcomes Stratified by Operative Approach
| Outcome Measure | Laparoscopic (N = 151) | Open (N = 110) | P-Value |
|---|---|---|---|
| Total LOS | |||
| Mean (SD) | 4.7 (5.9) | 11.5 (12) | - |
| Median (IQR) | 2.8 (2, 4.2) | 6.5 (3.7, 14.3) | <0.001 |
| Range | (1.1, 42.1) | (1.7, 55.4) | - |
| Postoperative LOS | |||
| Mean (SD) | 2.6 (4.3) | 8.2 (8.8) | - |
| Median (IQR) | 1.9 (1.1, 2.2) | 4.5 (2.7, 9.8) | <0.001 |
| Range | (0.2, 41.1) | (1.3, 48.6) | - |
| Bile duct injury | 2 (1%) | 2 (2%) | 1 |
| In-hospital death | 1 (1%) | 7 (6%) | 0.011 |
| Return to Operating Room | 7 (5%) | 5 (5%) | 0.97 |
| Time to Oral Intake (days) | |||
| Mean (SD) | 0.9 (0.7) | 2 (1.2) | - |
| Median (IQR) | 0.9 (0.6, 1) | 1.8 (1.1, 2.5) | <0.001 |
| Range | (0.2, 8) | (0, 6.1) | - |
| Surgical Site Infection | 19 (13%) | 11 (10%) | 0.52 |
| Hypertrophic scar | 11 (7%) | 12 (11%) | 0.31 |
| Wound separation | 2 (1%) | 4 (4%) | 0.24 |
| Incisional hernia | 0 (0%) | 0 (0%) | - |
| Fascial dehiscence | 0 (0%) | 2 (2%) | 0.18 |
Abbreviations: LOS, length of stay; SD, standard deviation; IQR, interquartile range.
The only statistically significant findings were a lower rate of in-hospital death and faster return to oral intake for the laparoscopic group. All other secondary outcomes were equivalent. There were a total of 12 returns to the operating room for short-term postoperative complications: seven in the laparoscopic group and five in the open.
Fewer patients in the laparoscopic group received pre-operative antibiotics versus the open group (Table 3).
Table 3.
Pre- and Postoperative Antibiotics Given Stratified by Operative Approach
| Laparoscopic (N = 151) | Open (N = 110) | P-Value | |
|---|---|---|---|
| Pre-operative antibiotics administered (Y/N) | 78 (52%) | 102 (93%) | <0.001 |
| Ciprofloxacin | 26 (35%) | 68 (67%) | <0.001 |
| Metronidazole | 49 (65%) | 93 (91%) | <0.001 |
| Cephalosporin | 49 (65%) | 36 (35%) | <0.001 |
| Other | 1 (1%) | 0 (0%) | 0.42 |
| Postoperative antibiotics administered (Y/N) | 149 (99%) | 110 (100%) | 0.51 |
| Ciprofloxacin | |||
| Mean (SD) | 2.7 (6) | 10.9 (12.3) | - |
| Median (IQR) | 0 (0, 0) | 10 (0, 16.8) | <0.001 |
| Range | (0, 31) | (0, 80) | - |
| Metronidazole | |||
| Mean (SD) | 11.9 (14.5) | 24.2 (15.7) | - |
| Median (IQR) | 7 (0, 21) | 22 (15, 29) | <0.001 |
| Range | (0, 106) | (0, 90) | - |
| Cephalosporin | |||
| Mean (SD) | 13.8 (10.2) | 8.4 (11.4) | - |
| Median (IQR) | 14 (10, 18) | 0 (0, 15.8) | <0.001 |
| Range | (0, 76) | (0, 54) | - |
| Gentamycin | |||
| Mean (SD) | 0 (0) | 0.1 (0.8) | - |
| Median (IQR) | 0 (0, 0) | 0 (0, 0) | 0.043 |
| Range | (0, 0) | (0, 6) | - |
| TMP/SMX | |||
| Mean (SD) | 0 (0) | 0.3 (3.1) | - |
| Median (IQR) | 0 (0, 0) | 0 (0, 0) | 0.25 |
| Range | (0, 0) | (0, 33) | - |
| Doxycycline | |||
| Mean (SD) | 0 (0) | 0 (0.1) | - |
| Median (IQR) | 0 (0, 0) | 0 (0, 0) | 0.25 |
| Range | (0, 0) | (0, 1) | - |
Abbreviations: SD, standard deviation; IQR, interquartile range; TMP/SMX, trimethoprim/sulfamethoxazole.
Postoperative antibiotics demonstrated an overall similar trend in three of six antibiotic types; however, this difference was not statistically significant when all doses of postoperative antibiotics were totaled (99% vs 100%, P = .51). Of note, several second and third generation cephalosporins were utilized; these were combined into a single category for simplicity.
Postoperative inpatient analgesic use was fairly equivalent. Three of the five nonnarcotic medications available at OAUTH (pentazocine, tramadol, and pethidine) were used more often by patients who underwent an open procedure versus a laparoscopic procedure, and these differences were statistically significant. However, morphine, fentanyl, and the remaining nonnarcotic analgesics were utilized equally regardless of operative approach (Table 4).
Table 4.
Number of Doses of Postoperative Analgesia, Stratified by Operative Approach
| Analgesic Type | Laparoscopic (N = 151) | Open (N = 110) | P-Value |
|---|---|---|---|
| Morphine | 3 (2%) | 5 (5%) | 0.29 |
| Fentanyl | 4 (3%) | 1 (1%) | 0.4 |
| Pentazocine | 58 (38%) | 56 (51%) | 0.044 |
| Tramadol | 14 (9%) | 24 (22%) | 0.005 |
| Paracetamol | 29 (19%) | 26 (24%) | 0.39 |
| Diclofenac | 51 (34%) | 25 (23%) | 0.052 |
| Pethidine | 6 (4%) | 13 (12%) | 0.016 |
A subgroup analysis of cholecystectomy patients evaluated the rate of biliary tree injuries. There were 38 open and 83 laparoscopic cholecystectomies; four conversions to open were analyzed as laparoscopic cases. Biliary tree injuries were equivalent for both groups, with two injuries each.
The number of patients who underwent surgery for a diagnosis of cancer, either biopsy-proven or presumed, was low in both groups. Thirteen (9%) patients in the laparoscopic group and 11 (10%) in the open group had a cancer diagnosis at time of surgery (P = 0.7). Lastly, cost comparisons between laparoscopic and open cases also demonstrated a statistically significant trend toward cost savings, from the patient’s perspective, with laparoscopic surgery (Table 5).
Table 5.
Costs to Patients for Initial Inpatient Hospital Stay and Perioperative Care
| Laparoscopic (N = 151) | Open (N = 110) | P-Value | |
|---|---|---|---|
| Total cost (Naira) | |||
| Mean (SD) | 31980.3 (20019) | 44673.7 (28558.8) | - |
| Median (IQR) | 27827.5 (15917.5, 40538.8) | 39830 (26162.5, 50685) | <0.001 |
| Range | (2960, 97250) | (755, 158990) | - |
| Total cost (USD*) | |||
| Mean (SD) | 191.5 (108.4) | 256 (140.8) | - |
| Median (IQR) | 184.9 (106.3, 225.8) | 217.2 (184.5, 285.7) | <0.001 |
| Range | (11.8, 636.3) | (4, 750.1) | - |
2017 U.S. Dollars
Abbreviations: SD, standard deviation; IQR, interquartile range.
However, a multivariate analysis controlling for age and total LOS negated any cost difference, resulting in a mean savings of US $4.88 for laparoscopic cases. This was not statistically significant.
DISCUSSION
The introduction of laparoscopy has been shown to promote faster recovery, with fewer complications such as wound infections and hernias, in many settings worldwide. These findings appear to be consistent at OAUTH in Ile-Ife, Nigeria. Most striking were differences in LOS, both total and postoperative. The advent of laparoscopic general surgery at OAUTH in 2007 had been noted by faculty and trainees to decrease LOS, which is supported by our findings and consistent with previous literature.17,18 Lack of data related to severity of illness limited our ability to adjust for confounding factors such as pre-operative selection bias, which may have influenced operative approach. It is possible that patients who underwent a laparoscopic procedure were healthier at baseline and less acutely ill compared to those who underwent an analogous open procedure. Prior to our data analysis, it was assumed that a large percentage of patients with prolonged LOS had a pre-operative cancer diagnosis. However, cancer diagnoses were relatively few in both groups, thus a cancer diagnosis did not serve as an accurate surrogate for severity of illness. A number of factors may influence TLOS, but with a limited set of diagnoses and surgical procedures, patient factors would be expected to be similar enough for comparison, despite multiple surgeons managing the units.
It is unclear why a significantly higher percentage of women underwent laparoscopic surgery, as compared with a relatively even sex distribution in the open group. It is possible that more female patients requested minimally invasive procedures, either due to cosmetic concerns or perhaps the length of recovery and the needs of their families. Similar trends have been reported for laparoscopic cholecystectomy in the Nigerian setting, with speculation that cosmesis increased acceptance of laparoscopy by female patients.17 Other than sex differences, the other demographic features studied suggest fairly even allocation between the two operative approaches. Insurance status did not appear to drive decision-making, nor did age.
Incision complications (i.e. SSI, wound dehiscence or separation, hernia) were equivalent. Patients who underwent open surgery were significantly more likely to suffer a postoperative mortality, although some selection bias is inherent in this finding, which could not be controlled for due to lack of information regarding pre-operative severity of illness. Overall utilization of antibiotics and analgesics was equivalent between the two surgical approaches.
We examined the rate of biliary tree injuries in the cholecystectomy subgroup as an indicator of quality and the surgeon’s learning curve. Reassuringly, rates of recognized biliary injuries were not only equal for both laparoscopic and open cases but were approximately equivalent to accepted average rates for the procedure.18 However, we are cautious in our interpretation of subgroup analysis, as our study was not adequately powered for this. Rates of injury were also too low to gain meaningful understanding of whether they are changing over time. This may become clearer with lengthier retrospective analysis, or with future prospective data.
Laparoscopic cases trended less costly for patients in terms of hospital charges. Lower charges were attributed primarily to TLOS, which drove up charges based on a small number of outliers in which TLOS was nearly two months. Of the 37 patients whose TLOS exceeded 14.3 days (placing them in the highest quartile for the open group), eight had laparoscopic surgery and 29 had an open operation. This assumption was confirmed by our multivariate analysis: controlling for patient age and TLOS equalized cost differences. The more notable conclusion is that laparoscopy does not appear cost-prohibitive to this patient population, despite an insurance coverage rate of less than 25%.
Limitations of this study include difficulty obtaining records from all patients who underwent laparoscopy during the study period; we obtained complete records for 151 out of 290 (52%) possible relevant laparoscopic cases. While meeting our requirements for power analysis, case number limitations precluded detailed subgroup analysis. Additionally, information regarding severity of illness was not available, making case matching and propensity analysis impossible.
In summary, postoperative complications between laparoscopic and open surgery at OAUTH were equivalent, suggesting that laparoscopy is safe in this setting. Dramatically shorter LOS supports its expansion at OAUTH. Concerns regarding higher charges for patients treated laparoscopically were also disproven, as laparoscopy was slightly less costly from a patient perspective. Further work is needed to evaluate costs to the hospital system, including procurement and maintenance of equipment. Later publications will report ongoing outcomes as additional laparoscopic surgeons join the institution.
Footnotes
Acknowledgements: The authors wish to thank the surgical department and residents at the Obafemi Awolowo University Teaching Hospitals Complex for hosting representatives of the University of Utah, and for sharing data, opinions, and ideas. They also extend gratitude to the University of Utah’s Center for Global Surgery for financially supporting this project.
Funding sources: This investigation was supported by the University of Utah Population Health Research (PHR) Foundation. Statistical analysis was supported by the University of Utah Study Design and Biostatistics Center with funding from the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant 5UL1TR001067-05 (formerly 8UL1TR000105 and UL1RR025764).
Conflict of interests: none.
Disclosure: none.
Informed consent: Dr. Katherine E. Smiley declares that written informed consent was obtained from the patient/s for publication of this study/report and any accompanying images.
Contributor Information
Katherine E. Smiley, University of Utah Hospital, Salt Lake City, Utah..
Funmilola Wuraola, Department of Surgery, Obafemi Awolowo University Teaching Hospitals Complex, Obafemi Awolowo University, Osun State, Nigeria..
Bolanle O. Mojibola, Department of Surgery, Obafemi Awolowo University Teaching Hospitals Complex, Obafemi Awolowo University, Osun State, Nigeria..
Adewale Aderounmu, Department of Surgery, Obafemi Awolowo University Teaching Hospitals Complex, Obafemi Awolowo University, Osun State, Nigeria..
Raymond R. Price, University of Utah Hospital, Salt Lake City, Utah..
Adewale O. Adisa, Department of Surgery, Obafemi Awolowo University Teaching Hospitals Complex, Obafemi Awolowo University, Osun State, Nigeria..
References:
- 1.Meara JG, Leather AJM, Hagander L, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386(9993):569–624. [DOI] [PubMed] [Google Scholar]
- 2.Chao T, Mandigo M, Opoku-Anane J, et al. Systematic review of laparoscopic surgery in low- and middle-income countries: benefits, challenges and strategies. Surg Endosc. 2016;30(1):1–10. [DOI] [PubMed] [Google Scholar]
- 3.Aimaq R, Akopian G, Kaufman HS. Surgical site infection rates in laparoscopic versus open colorectal surgery. Am Surg. 2011;77(10):1290–1294. [DOI] [PubMed] [Google Scholar]
- 4.Al Chalabi H, Larkin J, Mehigan B, et al. A systematic review of laparoscopic versus open abdominal incisional hernia repair, with meta-analysis of randomized controlled trials. Int J Surg. 2015;20:65–74. [DOI] [PubMed] [Google Scholar]
- 5.Straub CM, Price RR, Matthews D, et al. Expanding laparoscopic cholecystectomy to rural Mongolia. World J Surg. 2011;35(4):751–759. [DOI] [PubMed] [Google Scholar]
- 6.Kayumba K, Nsanzimana S, Binagwaho A, et al. TRACnet internet and short message service technology improves time to antiretroviral therapy initiation among HIV-infected infants in Rwanda. Pediatr Infect Dis J. 2016;35(7):767–771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jhpiego. Jhpiego in Nigeria. Available at: https://www.jhpiego.org/wp-content/uploads/2015/08/Nigeria-Country-Profile.pdf. Accessed October 4, 2022.
- 8.Udwadia TE, Udwadia RT, Menon K, et al. Laparoscopic surgery in the developing world. An overview of the Indian scene. Int Surg. 1995;80(4):371–375. [PubMed] [Google Scholar]
- 9.Castadot RG, Magarick RH, Sheppard L, et al. A review of ten years’ experience with surgical equipment in international health programs. Int J Gynaecol Obstet. 1986;24(1):53–60. [DOI] [PubMed] [Google Scholar]
- 10.World Bank. 2019. Data for Nigeria. Available at: http://data.worldbank.org/?locations=NG-XN. Accessed October 4, 2022.
- 11.Ojo EO, Chirdan OO, Ajape AA, et al. Post-graduate surgical training in Nigeria: the trainees’ perspective. Niger Med J. 2014;55(4):342–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Adisa AO, Alatise OI, Arowolo OA, et al. Laparoscopic appendectomy in a Nigerian teaching hospital. JSLS. 2012;16(4):576–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adisa AO, Lawal OO, Adejuyigbe O. Trend over time for cholecystectomy following the introduction of laparoscopy in a Nigerian tertiary hospital. Niger J Surg. 2017;23(2):102–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.StataCorp. 2009. Stata Statistical Software: Release 11. College Station, TX: StataCorp LP. [Google Scholar]
- 16.Oanda Solutions for Business. Historical Currency Converter. Available at: https://www.oanda.com/currency/average https://www.oanda.com/currency/average Accessed October 4, 2022.
- 17.Perron-Burdick M, Calhoun A, Idowu D, et al. Minilaparotomy vs. laparoscopic hysterectomy: comparison of length of hospital stay. J Minim Invasive Gynecol. 2014;21(4):619–623. [DOI] [PubMed] [Google Scholar]
- 18.Ayandipo O, Afuwape O, Olonisakin R. Laparoscopic cholecystectomy in Ibadan, southwest Nigeria. J West Afr Coll Surg. 2013;3(2):15–26. [PMC free article] [PubMed] [Google Scholar]